Abstract
Studies of religious/spiritual behavior frequently rely on self-reported questionnaire data, which is susceptible to bias. The Daily Phone Diary (DPD) was developed to minimize bias in reporting activities and behavior across a 24-hour period. A cross-sectional study of 126 parents of children with cystic fibrosis was used to establish the validity of the DPD to study religious/spiritual behaviors. Longitudinal models were used to determine the odds of improved mood during religious/spiritual activities. Convergent validity was found. Participants had increased odds of improved mood during religious/spiritual activities compared to non-religious/spiritual activities. Associations with gender and religious affiliations were found. The DPD is a valid tool for studying religious/spiritual activities and opens novel avenues for chaplaincy research and the development of chaplaincy interventions incorporating these findings.
Keywords: religiosity, cystic fibrosis, parents, mood, Daily Phone Diary
Having a child with a chronic illness is stressful for the family (Herzer et al., 2010), members of which may draw on various coping responses (Folkman, Lazarus, Dunkel-Schetter, DeLongis, & Gruen, 1986). Religion and spirituality are effective coping strategies for some patients and family members (Cotton, Grossoehme, & McGrady, 2012; Grossoehme, Ragsdale, Wooldridge, Cotton, & Seid, 2010; Pargament, 1997). The stress-buffering effects of religion and spirituality has been proposed as one of several potential mechanisms by which these behaviors may affect health outcomes (Oman & Thoresen, 2005). Parents of children with CF and other chronic diseases use religion and spirituality to cope with their experiences (Dollahite, Marks, & Olson, 1998; Grossoehme, Ragsdale, Wooldridge, Cotton, & Seid, 2010). The use of religious and or spiritual beliefs or practices to decrease stress may also contribute to improved mood states. Mahoney and colleagues have shown that family members often participate in religious or spiritual activities as a group activity to cope with stress (Mahoney, Pendleton, & Ihrke, 2006). Religious behaviors have also been associated with less distressed marriages among parents of children who have cystic fibrosis (Grossoehme, Szczesniak, Dodd, & Opipari-Arrigan, 2014).
A relationship between religion and emotion has long been noted. Silberman describes three ways in which religion influences emotions (Emmons, 2005). First, religion makes claims about the appropriateness of certain emotions. Second, religious beliefs may dispose a person towards particular emotions as well as influence one’s emotional well-being. Third, religious practices create opportunities to powerfully experience intimacy with the Divine. Many people use religion to cope with illness (Pargament, 1997), and religious coping affects health outcomes. Engaging in some types of religious coping lead to improved mental health outcomes (Gall, Kristjansson, Charbonneau, & Florack, 2009; Koenig, Pargament, & Nielsen, 1998; Yangarber-Hicks, 2004). Engaging in other types of religious coping is associated with poorer mental health outcomes (Bickel et al., 1998; Exline, Park, Smyth, & Carey, 2011; Krause, 2006; Mohr, Brandt, Borras, Gilliéron, & Huguelet, 2006). Much work has been done on the relationship between religion and psychopathology, most notably regarding religion and spirituality and depressive symptoms. A meta-analytic study by Smith and colleagues of 147 studies showed an inverse relationship between religious involvement and depression that was not moderated by a person’s age, gender, or ethnicity (Miller & Kelley, 2005). Krause (Krause, 2010) noted a bimodal onset of depressive symptoms in early and late adulthood, and explored the possibility that meaning in life was a missing element in religion-mood research. He found that church-based social support bolstered older adults’ sense of meaning in life, and that persons with a sense of meaning were less likely to have depressive symptoms. Although approximately 16% of adults will have a diagnosis of depression once in their lifetime and there is an 8.7% incidence of depressive symptoms at any one time (Strine et al., 2015), some of which may have a spiritual dimension, there is also a strong association between daily spiritual experiences and psychological well-being (Yonker, Schnabelrauch, & DeHaan, 2012), and between daily spiritual experiences and better mental health status (Rippentrop, Altmaier, Chen, Found, & Keffala, 2005). Common everyday spiritual experiences have been shown to buffer the effects of stress on negative affect while exerting a direct effect on positive affect (Whitehead & Bergeman, 2011).
Examining the ways in which religious or spiritual behaviors affect health outcomes requires overcoming several obstacles. The first is the absence of a uniform definition of these terms. Hill and colleagues, in an attempt to generate consensus, proposed the following definitions, which were utilized in this study. Spirituality is defined as those, “feelings, thoughts, experiences, and behaviors that arise from a search for the sacred.” Using that definition as its base, religion is more narrowly defined as the, ‘‘means and methods (e.g., rituals or prescribed behaviors) of the search receive validation and support from within an identifiable group of people” (Hill et al., 2000). Religiosity refers, even more narrowly, to “involvement in religious activities, such as prayer” (Saroglou, 2002).
The second obstacle is the multi-dimensional nature of religion and spirituality. Religion and spirituality encompass a number of aspects—behavior and belief—as well as social, cognitive and developmental aspects. Conceptualizing religion and spirituality is important. Single-item measures, typically of religious affiliation, have little variance (McCullough & Larson, 1999) and are simplistic (Masters et al., 2009). The Fetzer Institute and the National Institute on Aging sponsored the development of a multi-dimensional means to address this issue, leading to the development of measures across twelve domains (Fetzer/National Institute on Aging, 1999).
The third obstacle is rigorous measurement of these behaviors. Most often, studies of religious/spiritual behavior have relied on self-reported data on various questionnaires, which have several limitations (Hill, 2005). Questionnaires may not capture the multidimensional nature of religious/spiritual behaviors because they generally utilize only closed-ended items. They may also be written at a higher reading level than the general population, making them more difficult to complete and interpret. Finally, self-report measures may elicit more socially desirable responding.
The Daily Phone Diary (DPD) was developed as an unobtrusive measure of events and behaviors that people engage in on a daily basis (Quittner et al., 1998). It provides an ecological momentary assessment (EMA) of all activities, companions and mood ratings over a 24-hour period. The DPD is administered by phone, taking about 15 minutes to assess a 24-hour period and asks about all activities lasting 5 minutes or longer in the previous 24 hours, “blinding” the respondent to the behavior of interest that is the focus of the analyses. Telephone interviews are preferable to in-person interviews for topics are sensitive in nature, such as adherence to recommended therapies or religious and spiritual matters (Midanik, Greenfield, & Rogers, 2001). The DPD has established psychometric properties (Quittner, et al., 1998; Quittner & Opipari, 1994), although it has not been used to study religious/spiritual behaviors.
Given the role of religious/spiritual beliefs and experiences on depression and stress, the aim of this study was to determine whether the DPD is a valid measure of religious/spiritual behaviors reported by parent caregivers of children who have cystic fibrosis. Cystic fibrosis is a useful exemplar because of its life-shortening nature, the prevalence of depressive symptoms and the relationship between depressive symptoms and poorer child health outcomes (Quittner et al., 2014). If the DPD is indeed a valid measure for religious/spiritual behaviors, it would be a useful tool for describing family spiritual/religious behaviors and their effects on psychological functioning. The hypotheses were that the DPD would demonstrate convergent validity, and that engaging in a religious/spirituality activities would be associated with improved mood reported throughout the day.
Methods
Participants
Data used in these analyses were collected in the course of a larger study focused on parental adherence to their child’s prescribed treatments (Grossoehme et al., 2015). This two-site study was approved by the institutional review boards at both hospitals. We recruited caregivers of children with CF ages 13 years and younger who were followed at accredited CF Centers. The pediatric, academic medical centers were in the Midwest (Site 1) and the South (Site 2), drawing on patients from 7 US states. A total of 142 caregivers were enrolled (42% participation rate; Site 1 n=83 and Site 2 n=59) in two phases of the study: the first was an online collection of measures (described below) using the Research Electronic Data Capture (REDCap) database and the second was data collection using the DPD by phone. Of those enrolled, 130 (N = 73, Site 1 and N = 57, Site 2) completed at least 1 of the 3 scheduled DPD interviews within three weeks of completing the online questionnaires.
Procedures
Caregivers at both sites were informed of the study in a letter from their child’s pulmonologist or a phone call from a member of the research team, followed by an outpatient clinic encounter to answer any questions or concerns, opt out, or obtain consent. Both parents were given an opportunity to participate if they wanted to. Caregivers were given a URL address to complete the study measures, separately, in REDCap using their own computers if the initial measures were not completed during the child’s clinic visit. REDCap is a web-based application designed to securely capture data and export it to statistical packages for analysis (Harris et al., 2009). At the time of enrollment, participants agreed to receive a follow-up contact if they had not completed their measures online within a month. Follow-up contacts were made to remind parents, provide the URL address again in case it was misplace, and to resolve any systems issues.
Measures
Symptoms of depression
The Center for Epidemiologic Studies Depression scale (CES-D) is a 20-item scale used to measure depressive symptoms in community samples (Radloff, 1977). Respondents indicate the frequency of feelings such as, “I talked less than usual” and “I had crying spells” on a scale ranging from 0-3. Internal consistency, measured as Cronbach’s alpha, is strong (0.78). In accordance with published thresholds, participants who scored below 16 were classified as “not depressed” and participants who scored at or above 16 were classified as “depressed.”
Religiosity
The Duke University Religiosity Index (DUREL) is a five-item scale that measures three constructs: organizational, non-organizational, and intrinsic religiosity (Koenig, Parkerson, & Meador, 1997). The organizational religiosity item is, “How often do you attend church or other religious meetings?” Nonorganizational religiosity is measured with the item, “How often do you spend time in private religious activities, such as prayer, meditation, or Bible study?” Three items measure intrinsic religiosity; an example is, “I try hard to carry my religion over into all other dealings in life.” Cronbach’s alpha for this scale was 0.84.
Spiritual coping
Spiritual coping was measured using the Brief R-COPE (Pargament, Koenig, & Perez, 2000). This widely-used 18-item scale measures spiritual coping styles (Pargament, 1999). There are three subscales for positive spiritual coping, negative spiritual coping, and spiritual coping for control. The terms “positive” and “negative” refer to the associations that certain spiritual coping styles have with health outcomes, with positive coping styles associated with improved outcomes and negative coping styles with poorer health outcomes (Bosek, Lowry, Lindeman, Burck, & Gwyther, 2003; Burker, Evon, Sedway, & Egan, 2005; Grossoehme et al., 2016; Pargament, 1997). The positive and negative coping subscales have seven items each. An example positive spiritual coping item is, “Looked for a stronger connection with God”; an example of negative spiritual coping is, “Questioned the power of God.” Responses are made on a 4-point Likert-style scale indicating how frequently the style was used, ranging from “not at all” to “a great deal.” Five items comprise the subscale for spiritual coping for control, with one item each for collaborative, active surrender, deferring, self-directed, and pleading. For example, the pleading item reads, “Pleaded with God to make things turn out okay.” Cronbach’s alpha for the Brief R-COPE scale was 0.80.
Spiritual activities
Once the measures were completed, participants were contacted to schedule and complete three DPD calls over the phone within three weeks and when possible, at least one DPD was conducted on a Monday to obtain weekend data from Sunday. The DPD asks participants to recall the events over the last 24 hours which lasted 5 minutes or longer; they also report on the number and types of companions present for that activity, its duration, their mood (described below), and whether the activity was considered “instrumental” (necessary activities) or “recreational”(activities for fun). The DPD is an unobtrusive measure because participants are not aware of which variables across the 24-hour period are the focus of the study. This reduces social desirability responding. The DPD has been used extensively to measure adherence in CF, asthma (Modi & Quittner, 2006), and HIV-Aids (Wiener, Riekert, Ryder, & Wood, 2004). Test-retest reliability of the DPD over a 3-week period have been shown(Quittner & Opipari, 1994). Interrater reliability of greater than 90% has been documented(Quittner, Espelage, Opipari, Carter, & Eigen, 1998); this well-established measure has also shown convergent validity with electronic monitors and viral load. Control activities were defined as any activities on the DPD that were not classified as religious/spiritual activities.
Mood
Self-reported mood data is gathered using the DPD as described above. At enrollment, the content of the DPD call is described to the participants, which includes providing them with a one-page document depicting a 5-point Likert rating scale anchored at either end with the words “negative” and “positive”, with higher values corresponding to better mood. For each activity they describe during their DPD calls, they are asked to refer to this page in order to respond to the interviewer’s question about their mood while engaged in that activity.
Analytic Approach
Preliminary analysis
Only participants with at least one religious/spiritual activity were included in the analysis. Aggregate outcomes for daily duration and frequency were calculated for each participant and type of religious/spiritual activity, as follows. The duration of each religious/spiritual activity of the same type was summed over each day and then averaged over the total number of days to provide an average daily frequency and duration for descriptive and correlation analyses. For longitudinal modeling, all available data were included and organized as follows for analysis. An index variable was created to track time across each daily diary. To examine duration of improved mood, a separate index variable was created to measure the time since religious/spiritual activity (in hours) for each individual participant and religious/spiritual activity within the same DPD day. Participants’ multiple activities were represented via multiple corresponding time series.
Comparison of religious, spiritual, and control activities
To determine whether parents had increased odds of improved mood while performing religious/spiritual activities, compared to control activities, ordinal multinomial logistic regressions were calculated using generalized estimating equations, with adjustment for longitudinal correlation, imbalance in the number of control and religious/spiritual activities, and parent dyad effects (Park & Lee, 2002) with mood level as the outcome. Mood ratings of 3-5 were collapsed into “positive mood” due to the absence of mood ratings above 3 for religious/spiritual activities, which violate the proportional odds assumption of the model. The resulting mood variable in each model consisted of three levels, where a higher rating indicated better mood. Each parent could have multiple religious/spiritual activities on each day. Covariates initially included in the model were: parent gender, education level and religious affiliation, and CES-D and DUREL scores. An interaction term for parent gender and religious/spiritual activity was included to assess the moderating effect of parent gender on the relationship between religious/spiritual activity and mood. A final model was developed, retaining only the statistically significant interaction and lower level terms (P<0.1), through backward elimination.
Comparison of instrumental and recreational activities
To examine whether participants had increased odds of describing religious/spiritual activities as instrumental vs. recreational, logistic regressions were conducted using the previously described estimation procedures, adjustments, and model selection.
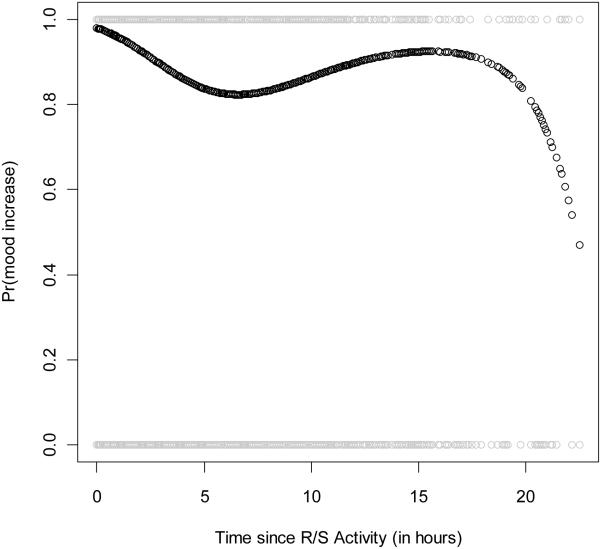
Sustaining/improving mood after religious/spiritual and control activities
Sustained or improved mood change after completing religious/spiritual activities was examined using a mixed effects, logistic regression with similar correlation structure. Improved mood at a given time was defined as the current mood rating being higher than the mood rating immediately preceding it. A binary outcome variable was created to indicate better or worse mood by comparing the mood level from the previous religious/spiritual activity within a DPD day. In this model, mood ratings were not collapsed. Time since religious/spiritual activity for each individual and his or her religious/spiritual activity was included as a covariate in the model and calculated as the time difference in hours since previous religious/spiritual activity until the next religious/spiritual activity within 24-hour period, or until the end of the day if no additional religious/spiritual activities occurred. A cubic polynomial was selected after fitting a logistic regression to represent the shape of probability of improved mood over time. The estimated probability or odds ratio (OR) and 95% confidence interval (CI), along with corresponding effect sizes expressed as Cohen’s d (Borenstein, Hedges, Higgins, & Rothstein, 2009), are reported for each effect of interest from the longitudinal models. All analyses were implemented using SAS 9.3 (SAS Institute, Cary, NC).
Results
Preliminary analysis
A total of 126 participants, 71 from Site 1 (56%) and 55 from Site 2 (44%) completed the DPDs, with 95 parents reporting at least one religious/spiritual activity (75%). A total of 540 religious/spiritual activities were reported across all diaries; 218 (40%) were individual activities, 316 (59%) were group activities and three (1%) were complementary-alternative medicine activities. A list of activity codes is included as an appendix. The mean and median frequency and duration of individual and group spiritual activities is presented in Table 1. These results did not significantly differ by religious affiliation or depression status. There was limited concordance between religious/spiritual activities on the DPD and the use of spiritual coping measured by the Brief R-COPE (see Table 2). Passive Deferring spiritual coping was positively correlated with the duration of individual spiritual activities. The use of positive spiritual coping as measured by the Brief R-COPE was significantly correlated with the frequency of participating in group spiritual activities. There was a non-significant relationship between the use of negative spiritual coping and either frequency or duration of individual or group spiritual activities.
Table 1.
Daily frequency and duration of religious/spiritual activities*
| N | Mean (SD) | Median (Range) | ||
|---|---|---|---|---|
| Individual spiritual | Frequency | 74 | 1.46 (0.91) | 1 (1-1.67) |
| activities | Duration (min) | 21.51 (28.81) | 10 (5-28.33) | |
| Group spiritual | Frequency | 77 | 1.81 (1.10) | 1.5 (1-2) |
| activities | Duration (min) | 49.48 (71.04) | 13.33 (5-73.33) |
Daily value per participant and activity type (individual or group) is based on aggregate calculation (see Methods)
Table 2.
Concordance between Daily Phone Diary, DUREL, and religious coping scale items (Spearman correlation coefficient)
| DPD religious/spiritual activity | Religiosity | Non- organizational religiosity |
Organizational religiosity |
Positive spiritual coping |
Passive Deferring spiritual coping |
|---|---|---|---|---|---|
| individual (frequency) | 0.29* | 0.31** | 0.22t | 0.09 | 0.009 |
| individual (duration) | 0.37** | 0.33** | 0.22t | 0.12 | 0.25* |
| Group (frequency) | 0.30** | 0.095 | 0.38** | 0.25* | −0.037 |
| Group (duration) | 0.18 | −0.02 | 0.31** | 0.17 | 0.016 |
p<0.01;
p< 0.05,
p<0.10
As hypothesized, there was evidence that the DPD has convergent validity. Convergent validity was operationalized as the extent of concordance between religious/spiritual activities on the DPD activity and religiosity as measured by the DUREL items of non-organizational and organizational religiosity. We found a positive, moderate correlation between both the frequency and duration of time spent in individual religious/spiritual activities on the DPD with these religious variables, including the total DUREL score; there was a trend towards significance with organizational religiosity (see Table 2). There was a positive, moderate correlation between the frequency and duration of time spent in group religious/spiritual activities and organizational religiosity.
Comparison of religious/spiritual and control activities
The final longitudinal model checking the odds of improved mood with covariate adjustment is shown in Table 3. Parents had an increased probability of having an improved mood during religious/spiritual activities compared to control activities (OR: 2.09, 95% CI: 1.45 to 3.02, Cohen’s d=0.41). Mothers exhibited greater improvements in mood during religious/spiritual vs. control activities than fathers, although the impact of these religious activities was positive for both. Religious affiliation was retained in the model. Parents with Protestant and Roman Catholic affiliations had greater odds of improved mood than those with non-denominational Christian affiliations (OR: 2.24, 95% CI: 1.38 to 3.62 and OR: 2.16, 95% CI: 1.35 to 3.45, respectively, Cohen’s d= 0.44 and 0.42, respectively).
Table 3.
Odds of improved mood during religious/spiritual activity, adjusted for confounders
| OR* | 95% CI | P Value | |
|---|---|---|---|
| Activity | |||
| Religious/Spiritual | 2.09 | 1.45 to 3.02 | <.0001 |
| Control | 1 | ||
| Parent Gender | |||
| Female | 0.81 | 0.48 to 1.38 | 0.042 |
| Male | 1 | ||
| Activity × Parent Gender | 0.041 | ||
| Female, Religious/Spiritual vs. Control | 3.32 | 2.61 to 4.21 | <0.0001 |
| Male, Religious/Spiritual vs. Control | 2.09 | 1.45 to 3.02 | <0.0001 |
| Religious Affiliation | 0.0015 | ||
| Protestant | 2.24** | 1.38 to 3.62 | 0.001 |
| Roman Catholic | 2.16** | 1.35 to 3.45 | 0.0013 |
| Other | 0.69 | 0.43 to 1.11 | 0.12 |
| Non-denominational Christian | 1 |
Each odds ratio refers to a comparison between each category and reference level of the covariate (denoted by OR = 1) with respect to mood level. An OR > 1 (< 1) corresponds to participants having higher (lower) odds of improved mood when comparing a given category to the reference level. Model includes covariance terms (see Methods).
P < .05.
Comparison of instrumental and recreational activities
Religious/spiritual activities were more likely to be categorized as instrumental vs. recreational based on the results of the longitudinal models for each type of religious/spiritual activity; the probabilities that participants regarded religious/spiritual activities as instrumental were 0.71 (95% CI: 0.65 to 0.76), 0.72 (95% CI: 0.63 to 0.79) and 0.71 (95% CI: 0.64 to 0.77) for all, individual and group religious/spiritual activities. The odds ratios of participants categorizing religious/spiritual activities as instrumental after adjusting for covariates are shown in Table 4 for all and group religious/spiritual activities. Those with Roman Catholic, non-denominational Christian, and other religious affiliations were less likely to endorse these activities as instrumental when compared to Protestant affiliations with odds ratios of 0.17 (95% CI: 0.06 to 0.49), 0.14 (95% CI: 0.06 to 0.32) and 0.26 (95% CI: 0.10 to 0.65), respectively. Corresponding effect sizes were 0.97, 1.08 and 0.75. In the final model, no covariate effects were retained for individual religious/spiritual activities. The final model for group religious/spiritual activities included adjustment for religious affiliation, education level, and DUREL score. Religious affiliations demonstrated a similar pattern across all religious/spiritual activities; All other affiliations were less likely than Protestant to label group religious/spiritual activities as instrumental with separate odds ratios of 0.10 (95% CI: 0.02 to 0.50), 0.13 (95% CI: 0.03 to 0.47) and 0.11 (95% CI: 0.03 to 0.42) with corresponding effect sizes of 1.24, 1.14, and 1.20.
Table 4.
Odds of describing religious/spiritual activity as instrumental compared to recreational, adjusted for confounders
| Religious/spiritual activities | All OR* (95% CI) |
Group OR* (95% CI) |
|
|---|---|---|---|
| Religious Affiliation | |||
| Roman Catholic | 0.17** (0.06, 0.49) | 0.10** (0.02, 0.50) | |
| NDC^ | 0.14** (0.06, 0.32) | 0.13** (0.03, 0.47) | |
| Other | 0.26** (0.10, 0.65) | 0.11**(0.03, 0.42) | |
| Protestant | 1 | 1 | |
| Education Level | |||
| High school | 0.17** (0.055, 0.56) | ||
| Some college | 0.10** (0.039, 0.36) | ||
| College graduate | 0.24** (0.093, 0.64) | ||
| Graduate school | 1 | ||
| Religiosity | 0.89 t (0.80, 1.00) |
Each odds ratio refers to a comparison between each category and reference level of the covariate (denoted by OR = 1) with respect to describing religious/spiritual activity as instrumental compared to recreational. An OR > 1 (< 1) corresponds to participants having higher (lower) odds describing religious/spiritual activity as instrumental compared to recreational when comparing a given category to the reference level. For continuous variable, OR indicated odds ratio with covariate increasing one unit. Model includes covariance terms (see Methods).
P < .05;
P<0.10.
NDC denotes Non-denominational Christian.
In terms of education, compared to a graduate degree, participants with high school up through college degree were less likely to consider group religious/spiritual activities as instrumental vs. recreational, with odds ratios of 0.17 (95% CI: 0.055 to 0.56), 0.10 (95% CI: 0.039 to 0.36) and 0.24 (95% CI: 0.093 to 0.64) respectively. Cohen’s d values were −0.98, −1.27 and −0.79, respectively. The odds of treating group religious/spiritual activities as instrumental would decrease 11% for each one unit increase in DUREL scores, with an odds ratio of 0.89 (95% CI: 0.80 to1.00).
Sustaining/improving mood after religious/spiritual and control activities
The estimated probability of improved mood after completing a religious/spiritual activity was relatively high (> 0.80) for most of the remaining 24-hour following the activity (see Figure 1). An estimated probability for each post-religious/spiritual activity mood rating was analyzed. As expected and shown by the number of gray points in the plot, the number of observations decreased as the time since the initial religious/spiritual activity increases. The first inflection point in the probability curve occurred around 6 hours after the religious/spiritual activity was completed, creating a local minimum. The estimated probability increased slightly to 0.90, then trailed downward toward the end of the 24-hour period.
Figure 1. Probability of Improved Mood with Time Since Spiritual Activity*.
*Estimated probability of improved mood over time since initiating religious/spiritual activity (black curve with points). The mood at a given time is compared to the mood observed during the religious/spiritual activity. The x-axis represents the hours since the activity. Gray points that equal zero on the plot correspond to worse mood after the activity; gray points that equal 1 correspond to a level of mood that is the same or higher than the mood during the activity.
Discussion
This study provided strong evidence that the DPD is a valid measure of religious and spiritual activities in parents of children with CF. Evidence of convergent validity was obtained and further, positive effects of religious/spiritual behaviors were documented. A benefit of improving one’s mood may accrue, and be sustainable for at least one hour after the spiritual activity. The analyses also show that engaging in a spiritual activity is likely to be regarded as instrumental rather than a recreational activity. These findings are important for chaplaincy for several reasons.
First, we have shown that the DPD is a valid tool for use in research about religion and spirituality—a topic important to the practice of chaplaincy. The DPD requires some training to use, and is then a straightforward tool which chaplains can use in their own studies. Secondary data analysis of DPD data from other investigators’ studies which include religious and spiritual activities may also be done. Chaplains may encourage collaborators to customize the activity codes to include the breadth of religious/spiritual behaviors permitting a more fine-grained analysis than the seven default activity codes for religious and spiritual behaviors. An important advantage of using the DPD over direct questions is that it minimizes the pressure which some respondents may feel to provide socially desirable answers (Midanik, Greenfield, & Rogers, 2001), especially to persons with greater perceived power such as a chaplain. As Oman and Thoresen argue, there is a need to move beyond questionnaire data to learn about the role of religion, spirituality and health, and this is especially true of religious and spiritual behaviors (Oman & Thoresen, 2005). Validity of the DPD opens a novel avenue for chaplaincy research. As the number and quality of studies on which chaplains are principal or co-investigators and participation in religious or spiritual activities is a variable hypothesized to relate to health outcomes, the need for valid tools such as the DPD increases.
The mood increases following religious/spiritual activities that were found in this study contribute to existing knowledge on the relationships between religion, spirituality, and health outcomes. Although these findings do not necessarily imply a causal effect, the results suggest that chaplains may be able to promote improved mood states by utilizing religious or spiritual interventions in their clinical encounters, or by encouraging the development and use of such activities by patients, families, or staff outside of those encounters. The improved mood was not a brief phenomenon which decreased rapidly after the activity; rather, it persisted over time, suggesting that the benefit remained between 6 and 24 hours afterwards, despite parents’ participation in other, non-religious/spiritual activities.
Persons who engaged in religious/spiritual activities understood them to be instrumental rather than recreational. This suggests that engaging in such activities was not an optional extra part of life, but a necessary component which was expected to provide them something other than pleasure or relaxation. The increased odds of Protestants viewing religious/spiritual activities as instrumental may reflect beliefs inculcated from within their faith tradition. The results suggest that persons who are Protestant may understand engaging in religious/spiritual activities as “being a good Christian”
This study has the following limitations. First, DPD is a form of self-report data collection, which is open to reporting bias. Participants were informed that the focus of the study was their adherence to their child’s cystic fibrosis treatments; it is unlikely that they would self-censor on the topic of religious or spiritual behaviors. The DPD itself seeks to minimize the related construct of recall bias by inquiring about all activities lasting more than five minutes rather than only the behaviors of interest. Second, participants were those affiliated with two cystic fibrosis centers in US regions with higher religious participation than others (Newport, 2010). It is possible that these participants reported more religious/spiritual activities than a nationwide sample would. Third, the sample size, while adequate for analyses, is relatively small, with 95 participants reporting a religious/spiritual activity. Fourth, the list of activity codes may not adequately capture the breadth of religious/spiritual activities. Fifth, participants were primarily Christian, and the experience of engaging in religious/spiritual activities may differ between Christianity and other faith traditions. Nevertheless, important conclusions may be drawn. Future research directions should lead to increased understanding of the religious/spiritual activities related to improved mood; feasibility/acceptability studies of chaplain interventions related to mood; and extending the present study to different populations, including adults with chronic disease. As professional chaplaincy seeks to move beyond simple Rogerian non-directive listening and towards more outcome-oriented interventive care (Perry, 2012; VandeCreek & Lucas, 2001), inquiry about a change in spiritual activities may be a question of clinical relevance to chaplains. The loss of religious/spiritual beliefs and practices has been theorized as one way to operationalize spiritual struggle (Fitchett & Risk, 2009). The present study does not contradict that hypothesis. The non-significant relationship between experiencing spiritual struggle (operationalized as the use of negative religious/spiritual coping styles as measured by the Brief R-COPE) and participation in spiritual activities suggests exploration of this area in the future. Inquiry about a decrease in religious/spiritual activities may be questions clinical chaplains may integrate into encounters early in the relationship as a means of identifying persons with spiritual struggle.
Acknowledgements
This study was partially funded by grants from the NIH/NICHD K23HD062642 (PI: Grossoehme), NIH/NHLBI K25 HL125954 (PI: Szczesniak), and NIH 8UL1 TR000077 (REDCap database). The authors acknowledge with appreciation the participation of the parents in this study; LaCrecia Britton and Stephanie Gamble for data collection at Alabama Children’s Hospital’s CF Center; the following individuals for their contributions with data collection and entry: Nicole Dalessandro, Cody Hanson, and Sarah Harrelson; and Alexis Teeters for her assistance with the manuscript.
Appendix
Daily Phone Diary Spiritual Activity Codes
| Level 1 | Level 2 | Level 3 | Activity |
|---|---|---|---|
| 1 | 0 | 0 | Spiritual Activities |
| 1 | 1 | 0 | Individual spiritual activities |
| 1 | 1 | 1 | Praying |
| 1 | 1 | 2 | Reading devotional materials |
| 1 | 1 | 3 | Watching religious programming on tv or internet |
| 1 | 1 | 4 | Sacrament/other ritual (confession, healing) |
| 1 | 1 | 5 | Visit cemetery by one’s self |
| 1 | 1 | 6 | Talk with religious leader about spiritual issue(s) |
| 1 | 1 | 7 | Talk with lay person about spiritual issue(s) |
| 1 | 1 | 8 | Drive to/from spiritual activity |
| 1 | 1 | 9 | Other individual spiritual activity |
| 1 | 2 | 0 | Group spiritual activities |
| 1 | 2 | 1 | Family prayer (incl. grace at meals) |
| 1 | 2 | 2 | Attend public worship |
| 1 | 2 | 3 | Drive to/from or drop off youth group for child |
| 1 | 2 | 4 | Drive to/from or drop off group spiritual activity (for self or family) |
| 1 | 2 | 5 | Attend bible study |
| 1 | 2 | 6 | Attend Sunday school/church school/Hebrew school/religious school |
| 1 | 2 | 7 | Attend wedding, baptism, funeral, bat mitzvah, festival, etc. |
| 1 | 2 | 8 | Watching religious programming on tv or internet |
| 1 | 2 | 9 | Participate in 12-step recovery program (meeting or call sponsor) |
| 1 | 2 | 10 | Attend social hour related to worship (coffee hour, breakfast) |
| 1 | 2 | 11 | Visit cemetery with others |
| 1 | 2 | 12 | Attend small group activity at place of worship |
| 1 | 2 | 13 | Other group spiritual activity |
| 1 | 2 | 14 | Reading religious/spiritual literature |
| 1 | 3 | 0 | Mind body spirit modalities |
| 1 | 3 | 1 | Drive to/from mind body spirit modality |
| 1 | 3 | 2 | Yoga |
| 1 | 3 | 3 | Massage |
| 1 | 3 | 4 | Chiropractic |
| 1 | 3 | 5 | Art therapy |
| 1 | 3 | 6 | Music therapy |
| 1 | 3 | 7 | Aroma therapy (incl. candles) |
| 1 | 3 | 8 | Acupuncture/acupressure |
| 1 | 3 | 9 | Healing touch/reiki |
| 1 | 3 | 10 | Other mind body spirit modality |
| 1 | 3 | 11 | Writing (journal, diary, creative, poetry, etc.) |
| 1 | 3 | 12 | Meditating |
References
- Bickel CO, Ciarrocchi JW, Sheers NJ, Estadt BK, Powell DA, Pargament KI. Perceived stress, religious coping styles, and depressive affect. Journal of Psychology and Christianity. 1998;17(1):33–42. [Google Scholar]
- Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Introduction to meta-analysis. Wiley; Chichester, West Sussex, UK: 2009. [Google Scholar]
- Bosek MS, Lowry E, Lindeman DA, Burck JR, Gwyther LP. Promoting a good death for persons with dementia in nursing facilities: family caregivers' perspectives. JONA'S Healthcare Law, Ethics, & Regulation. 2003;5(2):34–41. doi: 10.1097/00128488-200306000-00006. [DOI] [PubMed] [Google Scholar]
- Burker EJ, Evon DM, Sedway JA, Egan T. Religious and non-religious coping in lung transplant candidates: does adding God to the picture tell us more? Journal of Behavioral Medicine. 2005;28(6):513–526. doi: 10.1007/s10865-005-9025-4. [DOI] [PubMed] [Google Scholar]
- Cotton S, Grossoehme DH, McGrady ME. Religious coping and the use of prayer in children with sickle cell disease. Pediatric Blood and Cancer. 2012;58(2):244–249. doi: 10.1002/pbc.23038. doi: 10.1002/pbc.23038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dollahite DC, Marks LD, Olson MM. Faithful fathering in trying times: Religious beliefs and practices of Latter-day Saint fathers of children with special needs. The Journal of Men's Studies. 1998;7(1):71–93. [Google Scholar]
- Emmons RA. Emotion and religion. In: Paloutzian RF, Park CL, editors. Handbook of the psychology of religion and spirituality. 2005. pp. 235–252. [Google Scholar]
- Exline JJ, Park CL, Smyth JM, Carey MP. Anger toward god: social-cognitive predictors, prevalence, and links with adjustment to bereavement and cancer. Journal of Personality and Social Psychology. 2011;100(1):129–148. doi: 10.1037/a0021716. [DOI] [PubMed] [Google Scholar]
- Fetzer/National Institute on Aging, W. G. Mulitdimensional measurement of religiousness/spirituality for use in health research: A report of the Fetzer/National Insitute on Aging Working Group. Fetzer Institute; Kalamazoo, MI: 1999. [Google Scholar]
- Fitchett G, Risk JL. Screening for spiritual struggle. Journal of Pastoral Care and Counseling. 2009;63(1-2):1–12. [PubMed] [Google Scholar]
- Folkman S, Lazarus RS, Dunkel-Schetter C, DeLongis A, Gruen RJ. Dynamics of a stressful encounter: cognitive appraisal, coping, and encounter outcomes. Journal of Personality and Social Psychology. 1986;50(5):992–1003. doi: 10.1037//0022-3514.50.5.992. doi: 10.1037/0022-3514.50.5.992. [DOI] [PubMed] [Google Scholar]
- Gall TL, Kristjansson E, Charbonneau C, Florack P. A longitudinal study on the role of spirituality in response to the diagnosis and treatment of breast cancer. Journal of Behavioral Medicine. 2009;32(2):174–186. doi: 10.1007/s10865-008-9182-3. [DOI] [PubMed] [Google Scholar]
- Grossoehme D, Szczesniak R, Dodd C, Opipari-Arrigan L. Dyadic Adjustment and Spiritual Activities in Parents of Children with Cystic Fibrosis. Religions. 2014;5(2):385–401. doi: 10.3390/rel5020385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grossoehme DH, Ragsdale J, Wooldridge JL, Cotton S, Seid M. We can handle this: parents' use of religion in the first year following their child's diagnosis with cystic fibrosis. Journal of Health Care Chaplaincy. 2010;16(3-4):95–108. doi: 10.1080/08854726.2010.480833. doi: 10.1080/08854726.2010.480833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grossoehme DH, Szczesniak RD, Britton LL, Siracusa CM, Quittner AL, Chini BA, Seid M. Adherence Determinants in CF: Cluster Analysis of Parental Psychosocial and Religious/Spiritual Factors. Annals of the American Thoracic Society. 2015 doi: 10.1513/AnnalsATS.201408-379OC. doi: 10.1513/AnnalsATS.201408-379OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grossoehme DH, Szczesniak RD, Mrug S, Dimitriou SM, Marshall A, McPhail GL. Adolescents’ Spirituality and Cystic Fibrosis Airway Clearance Treatment Adherence: Examining Mediators. Journal of Pediatric Psychology. 2016 doi: 10.1093/jpepsy/jsw024. jsw024. [DOI] [PubMed] [Google Scholar]
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herzer M, Godiwala N, Hommel KA, Driscoll K, Mitchell M, Crosby LE, Modi AC. Family functioning in the context of pediatric chronic conditions. Journal of Developmental and Behavioral Pediatrics. 2010;31(1):26–34. doi: 10.1097/DBP.0b013e3181c7226b. doi: 10.1097/DBP.0b013e3181c7226b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill PC. Measurement in the psychology of religion and spirituality. In: Paloutzian RF, Park CL, editors. Handbook of the psychology of religion and spirituality. Guilford Press; New York, NY: 2005. pp. 43–61. [Google Scholar]
- Hill PC, Pargament KI, Hood RW, McCullough ME, Swyers JP, Larson DB, Zinnbauer BJ. Conceptualizing religion and spirituality: points of commonality, points of departure. Journal for the Theory of Social Behavior. 2000;30(1):51–77. [Google Scholar]
- Koenig HG, Pargament KI, Nielsen J. Religious coping and health status in medically ill hospitalized older adults. Journal of Nervous and Mental Disease. 1998;186(9):513–521. doi: 10.1097/00005053-199809000-00001. [DOI] [PubMed] [Google Scholar]
- Koenig HG, Parkerson GR, Jr., Meador KG. Religion index for psychiatric research. American Journal of Psychiatry. 1997;154(6):885–886. doi: 10.1176/ajp.154.6.885b. [DOI] [PubMed] [Google Scholar]
- Krause N. Religious doubt and psychological well-being: A longitudinal investigation. Review of Religious Research. 2006;47(3):287–302. [Google Scholar]
- Krause N. Religion and Depressive Symptoms in Late Life. In: Ellison CG, Hummer RA, editors. Religion, Families, and Health: Population-Based Research in the United States. Rutgers University Press; New Brunswick, NJ: 2010. p. 229. [Google Scholar]
- Mahoney A, Pendleton SM, Ihrke H. Religious coping by children and adolescents: unexplored territory in the realm of spiritual development. In: Roehlkepartain EC, Ebstyne King P, Wagener L, Benson PL, editors. The Handbook of spiritual development in childhood and adolescence. Sage Publications; Thousand Oaks, CA: 2006. pp. 341–354. [Google Scholar]
- Masters KS, Carey KB, Maisto SA, Caldwell PE, Wolfe TV, Hackney HL, Himawan L. Psychometric examination of the brief multidimensional measure of religiousness/spirituality among college students. The International Journal for the Psychology of Religion. 2009;19(2):106–120. [Google Scholar]
- McCullough ME, Larson DB. Religion and depression: a review of the literature. Twin Research. 1999;2(02):126–136. doi: 10.1375/136905299320565997. [DOI] [PubMed] [Google Scholar]
- Midanik LT, Greenfield TK, Rogers JD. Reports of alcohol-related harm: telephone versus face-to-face interviews. Journal of Studies on Alcohol and Drugs. 2001;62(1):74–78. doi: 10.15288/jsa.2001.62.74. doi: 10.15288/jsa.2001.62.74. [DOI] [PubMed] [Google Scholar]
- Miller L, Kelley BS. Relationships of religiosity and spirituality with mental health and psychopathology. In: Paloutzian RF, Park CL, editors. Handbook of the psychology of religion and spirituality. Guilford Press; New York, NY: 2005. pp. 460–478. [Google Scholar]
- Modi AC, Quittner AL. Barriers to treatment adherence for children with cystic fibrosis and asthma: what gets in the way? Journal of Pediatric Psychology. 2006;31(8):846–858. doi: 10.1093/jpepsy/jsj096. doi: 10.1093/jpepsy/jsj096. [DOI] [PubMed] [Google Scholar]
- Mohr S, Brandt P-Y, Borras L, Gilliéron C, Huguelet P. Toward an integration of spirituality and religiousness into the psychosocial dimension of schizophrenia. American Journal of Psychiatry. 2006;163(11):1952–1959. doi: 10.1176/ajp.2006.163.11.1952. [DOI] [PubMed] [Google Scholar]
- Newport F. Mississippians Go to Church the Most. Vermonters: 2010. Least Retrieved December 10, 2013, from http://www.gallup.com/poll/125999/mississippians-go-church-most-vermonters-least.aspx. [Google Scholar]
- Oman D, Thoresen CE. Do spiriituality and religion influence health? In: Paloutzian RF, Park CL, editors. Handbook of the psychology of religion and spirituality. Guilford Press; New York, NY: 2005. pp. 435–459. [Google Scholar]
- Pargament KI. Psychology of religious coping. Guilford Press; New York: 1997. [Google Scholar]
- Pargament KI. Religious/Spiritual coping. Fetzer Institute, National Institute on Aging Working Group; Kalamazoo, MI: 1999. pp. 43–56. [Google Scholar]
- Pargament KI, Koenig HG, Perez LM. The many methods of religious coping: development and initial validation of the RCOPE. Journal of Clinical Psychology. 2000;56(4):519–543. doi: 10.1002/(sici)1097-4679(200004)56:4<519::aid-jclp6>3.0.co;2-1. doi: 10.1002/(SICI)1097-4679. [DOI] [PubMed] [Google Scholar]
- Park T, Lee YJ. Covariance models for nested repeated measures data: Analysis of ovarian steroid secretion data. Statistics in Medicine. 2002;21(1):143–164. doi: 10.1002/sim.949. [DOI] [PubMed] [Google Scholar]
- Perry B. Outcome oriented chaplaincy: intentional caring. In: Roberts SB, editor. Professional spiritual & pastoral care. Skylight Paths Publishing; Woodstock, VT: 2012. pp. 342–361. [Google Scholar]
- Quittner AL, Espelage DL, Opipari LC, Carter B, Eid N, Eigen H. Role strain in couples with and without a child with a chronic illness: associations with marital satisfaction, intimacy, and daily mood. Health Psychology. 1998;17(2):112. doi: 10.1037//0278-6133.17.2.112. [DOI] [PubMed] [Google Scholar]
- Quittner AL, Espelage DL, Opipari LC, Carter BD, Eigen H. Role strain in couples with and without a chronically ill child: associations with marital satisfaction, intimacy and daily mood. Health Psychology. 1998;17:112–124. doi: 10.1037//0278-6133.17.2.112. doi: 10.1037//0278-6133.17.2.112. [DOI] [PubMed] [Google Scholar]
- Quittner AL, Goldbeck L, Abbott J, Duff AJ, Lambrecht P, Sole A, Barker D. Prevalence of depression and anxiety in patients with cystic fibrosis and parent caregivers: results of The International Depression Epidemiological Study across nine countries. Thorax. 2014;69(12):1090–1097. doi: 10.1136/thoraxjnl-2014-205983. doi: 10.1136/thoraxjnl-2014-205983. [DOI] [PubMed] [Google Scholar]
- Quittner AL, Opipari LC. Differential treatment of siblings: interview and diary analyses comparing two family contexts. Child Development. 1994;65(3):800–814. doi: 10.1111/j.1467-8624.1994.tb00784.x. doi: 10.1111/1467-8624.ep9408220881. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D Scale: a self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1(3):385–401. doi: 10.1177/014662167700100306. [Google Scholar]
- Rippentrop AE, Altmaier EM, Chen JJ, Found EM, Keffala VJ. The relationship between religion/spirituality and physical health, mental health, and pain in a chronic pain population. Pain. 2005;116(3):311–321. doi: 10.1016/j.pain.2005.05.008. [DOI] [PubMed] [Google Scholar]
- Saroglou V. Religion and the five factors of personality: A meta-analytic review. Personality and Individual Differences. 2002;32(1):15–25. [Google Scholar]
- Strine TW, Mokdad AH, Balluz LS, Gonzalez O, Crider R, Berry JT, Kroenke K. Depression and anxiety in the United States: findings from the 2006 behavioral risk factor surveillance system. Psychiatric Services. 2015 doi: 10.1176/ps.2008.59.12.1383. [DOI] [PubMed] [Google Scholar]
- VandeCreek L, Lucas AM, editors. The Discipline for pastoral care giving. Haworth Press; New York: 2001. [Google Scholar]
- Whitehead BR, Bergeman CS. Coping with daily stress: Differential role of spiritual experience on daily positive and negative affect. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2011 doi: 10.1093/geronb/gbr136. doi: 10/1093/geronb/gbr136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiener L, Riekert K, Ryder C, Wood LV. Assessing medication adherence in adolescents with HIV when electronic monitoring is not feasible. AIDS Patient Care & STDs. 2004;18(9):527–538. doi: 10.1089/apc.2004.18.527. [DOI] [PubMed] [Google Scholar]
- Yangarber-Hicks N. Religious coping styles and recovery from serious mental illness. Journal of Psychology & Theology. 2004;32(4):305–317. [Google Scholar]
- Yonker JE, Schnabelrauch CA, DeHaan LG. The relationship between spirituality and religiosity on psychological outcomes in adolescents and emerging adults: A meta-analytic review. Journal of adolescence. 2012;35(2):299–314. doi: 10.1016/j.adolescence.2011.08.010. [DOI] [PubMed] [Google Scholar]