Inhalational anesthetic agents (IAs) have been used for general anesthesia for more than 150 years. Since then, the safety profile of this class of anesthetics has improved markedly as drugs to control hypotension and techniques to secure the airway have been refined. However, it is only over the past few decades that we have begun to appreciate the versatility and benefits of using these agents for more than just anesthesia. We recently published a study reporting a dose-dependent protective effect of inhalational anesthetics against postoperative respiratory complications. These findings have generated great interest and discussion, and we thank Landoni et al. for their acknowledgement of and insight into the implications these findings may have for inhalational anesthetic use both within and outside of the operating room setting.
As stated by Landoni et al., the literature regarding the organ protective effects of IAs in non-cardiac surgery is sparse. In our quantitative effectiveness study, we found a strong, linear, dose-dependent, protective association between IA dose and respiratory complications, mortality and hospital costs (1). These outcomes have led us to speculate as to whether these protective effects could be utilized to tackle clinical challenges outside of the operating room, in critical care settings in particular.
Potential pharmacophysiological mechanisms underlying the preventive effects
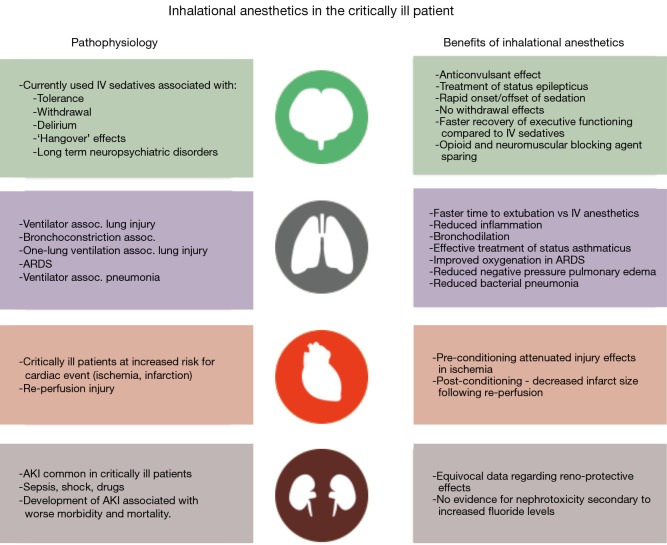
Inhalational anesthetics have pleiotropic effects on physiology with multiple likely mechanisms behind their organ protective properties (Figure 1). The immunomodulatory qualities of IAs are well reported in the literature. IAs decrease inflammation and attenuate lung injury by suppressing inflammatory responses (2,3). Mechanisms include modulation of alveolar macrophage responses and GABAA—receptor mediated anti-inflammatory effects at the level of lung epithelial cells. Moreover, IAs may exert protective effects on the lung via bronchodilation. These agents act directly to deplete calcium stores, leading to relaxation of airway smooth muscle. They also facilitate bronchodilation through neurally-mediated central effects that reduce vagal tone, whilst also altering circulating catecholamines and β receptor sensitivity (4).
Figure 1.
Organ specific effects of inhalational anesthetics in the critically ill patients. Organ art designed by freepik.com
How do the properties of volatile anesthetics improve outcomes?
The immunomodulatory and bronchodilative effects of IAs are associated with reduced airway resistance, reduced inflammation during one-lung ventilation, decreased risk of negative pressure pulmonary edema and reduced risk of bacterial pneumonia (5).
IAs have many advantages: they can be rapidly titrated, are cleared via exhalation, do not affect renal or hepatic laboratory markers, and do not cause development of tolerance or withdrawal in patients. Given these findings, we have begun to explore whether these organ protective attributes of IAs can be used to benefit critically ill patients outside the OR setting, a concept that is not without precedence.
IAs have been successfully used for their bronchodilatory effects in pediatric intensive care units to treat status asthmaticus. A case series by Carrie and Anderson has demonstrated the remarkable success these agents can have in treating refractory cases (6). Their review also sheds light on the unique challenges facing healthcare institutions in providing IAs for routine use outside the OR, as well as the co-ordination required between multidisciplinary teams, including anesthesia and critical care providers. They suggest that approaches to ensure safe and effective use of these agents in the critical care setting include provision of anesthesia delivery devices in the ICU, use of low flow techniques, provision of scavenger systems attached to vacuum systems and limitation of the use of other sedative agents, approaches that may help make provision of these agents in the adult ICU more common.
Current readily available intravenous sedative agents in the ICU are associated with adverse consequences. IAs provide shorter time to extubation, earlier recovery of executive function and opioid sparing effects after discontinuation of sedation when compared to propofol or midazolam (7). These findings were reciprocated in studies looking at both short term and long term sedation (8). Incidence of hallucination was also found to be significantly lower with IAs than with IV sedatives (8).
Furthermore, a randomized controlled pilot study has also demonstrated significantly improved oxygenation and reduced markers of epithelial injury and inflammation in ARDS patients on day 2 of treatment when an IA was used for sedation compared to IV midazolam (9).
Areas for future research
The maximum dose of IAs for anesthesia is limited in certain patients by cerebral vasodilation leading to increased intracranial pressure and the cost of specialized drug delivery and scavenger devices required to ensure safety. Indeed, we found in our study that titration of IAs to blood pressure is key, as hypotension for greater than 11 minutes obliterated the protective effects (1).
High doses of volatiles may be harmful. Whilst some studies point to a neuroprotective effect, others suggest neurodegeneration, apoptosis and cognitive dysfunction especially when high doses of volatile anesthetics are being given to elderly patients (7). Future studies will evaluate in disease entity-based subcohorts the optimal dose to be used in order to achieve the optimal protective effect.
In order to use IAs in the ICU, scavenger systems need to be installed to minimize pollution in compliance with local guidelines. Bedside IA administration has recently been simplified with the advent of miniature delivery devices such as the AnaConDa and MIRUS, both of which are not currently available in the US.
In conclusion, the proven organ protective effects of IAs make these a promising class of agents with great potential benefit to the critically ill population, both young and old. Furthermore, literature demonstrating the negative outcomes associated with opioids and neuromuscular blocking agents adds credence to the notion that IAs are much needed and viable alternatives (10,11). This is however a subject matter still in its infancy, with larger studies needed to resolve existing controversies and uncertainties, identify optimal methods of effectively delivering these agents outside the OR, and determine cost-effectiveness with consideration of outcomes.
Acknowledgements
None.
Provenance: This is an invited article commissioned by Section Editor Zhi Mao, MD (Department of Critical Care Medicine, Chinese People’s Liberation Army General Hospital, Beijing, China).
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Grabitz SD, Farhan HN, Ruscic KJ, et al. Dose-Dependent Protective Effect of Inhalational Anesthetics Against Postoperative Respiratory Complications: A Prospective Analysis of Data on File From Three Hospitals in New England. Crit Care Med 2017;45:e30-e39. 10.1097/CCM.0000000000002015 [DOI] [PubMed] [Google Scholar]
- 2.Faller S, Strosing KM, Ryter SW, et al. The volatile anesthetic isoflurane prevents ventilator-induced lung injury via phosphoinositide 3-kinase/Akt signaling in mice. Anesth Analg 2012;114:747-56. 10.1213/ANE.0b013e31824762f0 [DOI] [PubMed] [Google Scholar]
- 3.Stollings LM, Jia LJ, Tang P, et al. Immune Modulation by Volatile Anesthetics. Anesthesiology 2016;125:399-411. 10.1097/ALN.0000000000001195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mondoñedo JR, McNeil JS, Amin SD, et al. Volatile Anesthetics and the Treatment of Severe Bronchospasm: A Concept of Targeted Delivery. Drug Discov Today Dis Models 2015;15:43-50. 10.1016/j.ddmod.2014.02.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schilling T, Kozian A, Senturk M, et al. Effects of volatile and intravenous anesthesia on the alveolar and systemic inflammatory response in thoracic surgical patients. Anesthesiology 2011;115:65-74. 10.1097/ALN.0b013e318214b9de [DOI] [PubMed] [Google Scholar]
- 6.Carrié S, Anderson TA. Volatile anesthetics for status asthmaticus in pediatric patients: a comprehensive review and case series. Paediatr Anaesth 2015;25:460-7. 10.1111/pan.12577 [DOI] [PubMed] [Google Scholar]
- 7.Jerath A, Parotto M, Wasowicz M, et al. Volatile Anesthetics. Is a New Player Emerging in Critical Care Sedation? Am J Respir Crit Care Med 2016;193:1202-12. 10.1164/rccm.201512-2435CP [DOI] [PubMed] [Google Scholar]
- 8.Mesnil M, Capdevila X, Bringuier S, et al. Long-term sedation in intensive care unit: a randomized comparison between inhaled sevoflurane and intravenous propofol or midazolam. Intensive Care Med 2011;37:933-41. 10.1007/s00134-011-2187-3 [DOI] [PubMed] [Google Scholar]
- 9.Jabaudon M, Boucher P, Imhoff E, et al. Sevoflurane for Sedation in ARDS: A Randomized Controlled Pilot Study. Am J Respir Crit Care Med 2016. [Epub ahead of print]. 10.1164/rccm.201604-0686OC [DOI] [PubMed] [Google Scholar]
- 10.McLean DJ, Diaz-Gil D, Farhan HN, et al. Dose-dependent Association between Intermediate-acting Neuromuscular-blocking Agents and Postoperative Respiratory Complications. Anesthesiology 2015;122:1201-13. 10.1097/ALN.0000000000000674 [DOI] [PubMed] [Google Scholar]
- 11.Farhan H, Moreno-Duarte I, Latronico N, et al. Acquired Muscle Weakness in the Surgical Intensive Care Unit: Nosology, Epidemiology, Diagnosis, and Prevention. Anesthesiology 2016;124:207-34. 10.1097/ALN.0000000000000874 [DOI] [PubMed] [Google Scholar]