Abstract
AIM
To compare the repeatability/reproducibility of measurement by high-resolution Placido disk-based topography with that of a high-resolution rotating Scheimpflug camera and assess the agreement between the two instruments in measuring corneal power in eyes with keratoconus and post-laser in situ keratomileusis (LASIK).
METHODS
One eye each of 36 keratoconic patients and 20 subjects who had undergone LASIK was included in this prospective observational study. Two independent examiners worked in a random order to take three measurements of each eye with both instruments. Four parameters were measured on the anterior cornea: steep keratometry (Ks), flat keratometry (Kf), mean keratometry (Km), and astigmatism (Ks-Kf). Intra-examiner repeatability and inter-examiner reproducibility were evaluated by calculating the within-subject standard deviation (Sw) the coefficient of repeatability (R), the coefficient of variation (CoV), and the intraclass correlation coefficient (ICC). Agreement between instruments was tested with the Bland-Altman method by calculating the 95% limits of agreement (95% LoA).
RESULTS
In keratoconic eyes, the intra-examiner and inter-examiner ICC were >0.95. As compared with measurement by high-resolution Placido disk-based topography, the intra-examiner R of the high-resolution rotating Scheimpflug camera was lower for Kf (0.32 vs 0.88), Ks (0.61 vs 0.88), and Km (0.32 vs 0.84) but higher for Ks-Kf (0.70 vs 0.57). Inter-examiner R values were lower for all parameters measured using the high-resolution rotating Scheimpflug camera. The 95% LoA were -1.28 to +0.55 for Kf, -1.36 to +0.99 for Ks, -1.08 to +0.50 for Km, and -1.11 to +1.48 for Ks-Kf. In the post-LASIK eyes, the intra-examiner and inter-examiner ICC were >0.87 for all parameters. The intra-examiner and inter-examiner R were lower for all parameters measured using the high-resolution rotating Scheimpflug camera. The intra-examiner R was 0.17 vs 0.88 for Kf, 0.21 vs 0.88 for Ks, 0.17 vs 0.86 for Km, and 0.28 vs 0.33 for Ks-Kf. The inter-examiner R was 0.09 vs 0.64 for Kf, 0.15 vs 0.56 for Ks, 0.09 vs 0.59 for Km, and 0.18 vs 0.23 for Ks-Kf. The 95% LoA were -0.54 to +0.58 for Kf, -0.51 to +0.53 for Ks and Km, and -0.28 to +0.27 for Ks-Kf.
CONCLUSION
As compared with Placido disk-based topography, the high-resolution rotating Scheimpflug camera provides more repeatable and reproducible measurements of Ks, Kf and Ks in keratoconic and post-LASIK eyes. Agreement between instruments is fair in keratoconus and very good in post-LASIK eyes.
Keywords: keratoconus, post-LASIK, corneal power measurement, Placido disk-based topography, Scheimpflug camera
INTRODUCTION
Accurate measurement of corneal power is required for diagnosis and follow-up in patients with keratoconus. With the advent of corneal cross-linking, precise measurement of corneal power over time is crucial for patient selection[1]. Reliable measurement of corneal power is also important after refractive surgery for several reasons: to monitor post-operative stability, assess the onset of complications such as corneal ectasia, and calculate intraocular lens (IOL) power accurately.
Placido disk-based topography and the rotating Scheimpflug camera are widely used by clinicians to measure corneal power. However, the systems are based on different technologies. In Placido disk-based topography (or reflection topography), corneal power is determined from a series of concentric rings (or mires) projected on the anterior corneal surface, whereas the rotating Scheimpflug camera measures corneal power from cross-sectional scans of the cornea. The reliability of the two technologies and their agreement in measuring corneal power has been compared in normal corneas[2]–[6]. A recent Meta-analysis[7] showed similar intra-examiner repeatability and inter-examiner reproducibility between these technologies; as regards the agreement, they were found to be equivalent. In eyes with keratoconus and after laser in situ keratomileusis (LASIK), measurement reliability might be lower due to the corneal irregularities and the changes in corneal shape induced by excimer laser. In this study, we compared the repeatability/reproducibility of measurement by high-resolution Placido disk-based topography (Antares, Costruzione Strumenti Oftalmici, Florence, Italy) with that of a high-resolution rotating Scheimpflug camera (Pentacam HR, Oculus, Wetzlar, Germany) and assessed the agreement between these instruments in measuring corneal power in eyes with keratoconus and post-LASIK.
SUBJECTS AND METHODS
Subjects
Two groups of patients were prospectively recruited: patients with a diagnosis of keratoconus based on classic slitlamp and corneal topography findings and patients who had undergone LASIK. Patients were examined at the Cornea Service of the Eye Clinic, University of Torino, between September 2013 and February 2014. If both eyes were elegible for the study, the eye to be examined was randomly selected (fair coin toss). Exclusion criteria were history of corneal cross-linking or ocular surgery, use of contact lenses in the previous 30d, presence of corneal scars, ocular surface diseases or other ocular comorbidities. The study was conducted in accordance with the Declaration of Helsinki and approved by the local clinical research Ethics Committee. All participants provided informed consent.
Measurements
Measurement repeatability and reproducibility were defined according to the International Organization for Standardization[8]–[9]. To assess repeatability, all factors (examiner, instrument, calibration, setting, time between measurements) were kept constant. To assess reproducibility, only one factor (examiner) was changed.
The Antares is a 24-ring Placido disk-based topographer that uses a white light source and a high resolution (1024×960 pixels) color digital camera to measure 6144 corneal points. The software version was Phoenix 3.0. The Pentacam HR uses a monochromatic slit-light source [blue light-emitting diode (LED)] operating at 475 nm wavelength) and a high-resolution (1.45 megapixel) 360-degree rotating Scheimpflug camera to measure 138 000 true elevation points of the cornea. The software version was 1.19r11. Both instruments were calibrated by the manufacturer at the beginning of the study.
Two expert examiners worked in a random order to take three measurements of each eye with both instruments. Measurements were taken during a single session between 2 and 4 p.m. following the manufacturer's guidelines. The patient's head was carefully aligned in the chin rest and against the forehead strap. He/she was asked to open both eyes, stare at the fixation target, and blink before each scan. The devices were defocused and realigned before each measurement.
Using the Placido disk-based topographer, the examiner focused the rings on the corneal surface and aligned the instrument with the corneal vertex. The instrument was moved away from the eye to obtain a “little defocus”, then slowly towards the eye, and the image was captured automatically by the high-resolution digital camera. The procedure was repeated until a good-quality image was obtained. Using the high-resolution rotating Scheimpflug camera, the examiner adjusted the joystick until perfect alignment was achieved. Then the automatic release mode was used to capture 25 images per scan. The scan was accepted if the quality expressed by the software was “OK”.
The tangential curvature map was displayed on the instrument monitor and the following parameters were recorded. 1) Flat keratometry (Kf) and steep keratometry (Ks). Using the default setting of the instruments, the Kf and Ks are calculated automatically 90 degrees apart from the steepest and flattest radius of curvature (r) of the 3.00 mm central cornea based on the paraxial formula: K=(n2-n1)/r, where n2 is the standard refraction index of the cornea (1.3375) and n1 is the refraction index of air (1). 2) Mean keratometry (Km). This parameter is calculated from the arithmetic average of the steepest and flattest radius of curvature of the 3.00 mm central cornea based on the paraxial formula. 3) Astigmatism (Ks-Kf). This parameter is the arithmetic difference between Ks and Kf.
Statistical Analysis
All data were exported in an Excel spreadsheet (Microsoft Corp., Redmond, WA, USA), and statistical analysis was performed using IBM SPSS Statistics (version 19.0, IBM, Inc. Armonk, NY, USA). Continuous variables were expressed as mean±standard deviation. They were compared with non parametric tests for k matched distributions: Wilcoxon's signed-rank test for k=2 and Friedman's test for k>2. Statistical significance was set at P<0.05. Repeatability and reproducibility were assessed using the following methods and parameters. 1) Within-subject standard deviation (Sw) which is derived from the square root of the residual mean square from the analysis of variance (ANOVA)[10]. 2) The coefficient of repeatability (R), which is calculated by multiplying the Sw by 2.77. For 95% of all pairs of measurements, the absolute difference between two measurements may be as much as this value[10]. This coefficient is an indicator of repeated measurement error. The lower the coefficient, the better the repeatability. 3) Coefficient of variation (CoV), which is the Sw/mean ratio (%). This coefficient gives an idea of the Sw proportionality with respect to the mean and allows to compare data sets with different units or widely different means. The lower the CoV, the higher the repeatability. 4) Intraclass correlation coefficient (ICC), which is the ratio of the between-subject variance to the sum of the pooled within-subject variance and the between-subject variance. The closer the ICC is to 1, the better the measurement consistency (very good if ICC>0.90, moderate if 0.75≤ICC≥0.90, poor if ICC<0.75). The coefficient is quoted with 95% confidence interval (95% CI).
Agreement between the two instruments was tested using Bland-Altman plots, where differences between the instrument measurements were plotted against mean values[11]. The mean difference and 95% limits of agreement (95% LoA) were calculated for each corneal parameter from the mean difference ±1.96 standard deviation. They represent the limits of the range for the 95% of differences between the two instruments.
Sample size was calculated to determine the minimum number of patients that had to be included in the study in order to detect a statistical difference between repeated intrasubject measurements. Previous studies[7] report that the standard deviation of multiple corneal power measurements with the rotating Scheimpflug camera and Placido-disk topography is about 0.10 diopters (D). Hence, to detect a difference in corneal power of 0.25 D, with a significance level of 0.05 and a power of 0.95, a minimum sample size of five eyes per group was computed to be needed.
RESULTS
Keratoconic Eyes
One eye of 32 patients (20 women and 12 men) with keratoconus was analyzed. The mean age was 36.9±13.1y. According to the collaborative longitudinal evaluation of keratoconus (CLEK) study group classification[12], mild keratoconus (Km<45 D) was present in 10/32 eyes (31.25%) and moderate keratoconus (Km ≥45 and ≤52 D) in 22/32 eyes (68.75%).
Intra-examiner Repeatability
Table 1 shows the intra-examiner repeatability of measurements with each method by examiner 1, as assessed by Sw, R, CoV, and ICC, as well as the results of Friedman's test on the three sets of measurements obtained for each parameter (Kf, Ks, Km, Ks-Kf). For Kf, Ks and Km measurements, the Sw, R and CoV were lower using high-resolution rotating Scheimpflug camera compared to Placido disk-based topography (Table 1). In contrast, for Ks-Kf measurement, the Sw, R and CoV were slightly lower using the Placido disk-based topography compared to high-resolution rotating Scheimpflug camera (Table 1). The ICC between measurements by both instruments repeated by the same examiner were >0.90 for all parameters (Table 1). Similar results were obtained for examiner 2.
Table 1. Intra-examiner repeatability of corneal power measurements by Placido disk-based topography and high-resolution rotating Scheimpflug camera in eyes with keratoconus.
| Parameters | 1P | Sw (D) | R (D) | CoV (%) | ICC (95% CI) |
| Kf | |||||
| Placido | 0.86 | 0.32 | 0.88 | 0.72 | 0.962 (0.932-0.980) |
| Scheimpflug | 0.31 | 0.11 | 0.32 | 0.25 | 0.996 (0.993-0.998) |
| Ks | |||||
| Placido | 0.80 | 0.32 | 0.88 | 0.67 | 0.987 (0.978-0.993) |
| Scheimpflug | 0.74 | 0.22 | 0.61 | 0.46 | 0.995 (0.990-0.997) |
| Km | |||||
| Placido | 0.99 | 0.30 | 0.84 | 0.65 | 0.980 (0.965-0.990) |
| Scheimpflug | 0.79 | 0.11 | 0.32 | 0.25 | 0.996 (0.992-0.998) |
| Ks-Kf | |||||
| Placido | 0.37 | 0.21 | 0.57 | 6.60 | 0.987 (0.977-0.993) |
| Scheimpflug | 0.90 | 0.25 | 0.70 | 8.55 | 0.973 (0.952-0.986) |
Kf: Flat keratometry; Ks: Steep keratometry; Km: Mean keratometry; Ks-Kf: Astigmatism; D: Diopters; Sw: Within-subject standard deviation; R: Coefficient of repeatability; CoV: Coefficient of variation; ICC: Intraclass correlation coefficient. 1Friedman's test.
Inter-examiner Reproducibility
Since all sets of three measurements proved to be statistically equivalent (P>0.30), they were averaged to yield for each examiner an ensemble of series relative to each of the four parameters for the two instruments. Table 2 presents the results of Wilcoxon's test on all matched measurements by the two examiners and shows no statistically significant differences between examiners. The Sw, R, and CoV of all parameters measured by the high-resolution rotating Scheimpflug camera were lower as compared with Placido disk-based topography (Table 2). The ICC between examiners were >0.90 for all parameters measured by both instruments (Table 2).
Table 2. Inter-examiner reproducibility of corneal power measurements by Placido disk-based topography and high-resolution rotating Scheimpflug camera in eyes with keratoconus.
| Parameters | 1P | Sw (D) | R (D) | CoV (%) | ICC (95% CI) |
| Kf | |||||
| Placido | 0.06 | 0.29 | 0.81 | 0.65 | 0.968 (0.936-0.984) |
| Scheimpflug | 0.56 | 0.08 | 0.21 | 0.17 | 0.998 (0.996-0.999) |
| Ks | |||||
| Placido | 0.05 | 0.35 | 0.98 | 0.74 | 0.986 (0.972-0.993) |
| Scheimpflug | 0.74 | 0.14 | 0.40 | 0.30 | 0.998 (0.995-0.999) |
| Km | |||||
| Placido | 0.06 | 0.31 | 0.87 | 0.68 | 0.980 (0.959-0.990) |
| Scheimpflug | 0.58 | 0.09 | 0.26 | 0.20 | 0.998 (0.996-0.999) |
| Ks-Kf | |||||
| Placido | 0.27 | 0.19 | 0.52 | 5.97 | 0.990 (0.981-0.995) |
| Scheimpflug | 0.34 | 0.14 | 0.38 | 4.70 | 0.993 (0.986-0.997) |
Kf: Flat keratometry; Ks: Steep keratometry; Km: Mean keratometry; Ks-Kf: Astigmatism; D: Diopters; Sw: Within-subject standard deviation; R: Coefficient of repeatability; CoV: Coefficient of variation; ICC: Intraclass correlation coefficient. 1Wilcoxon's signed-rank test.
Agreement Between Instruments
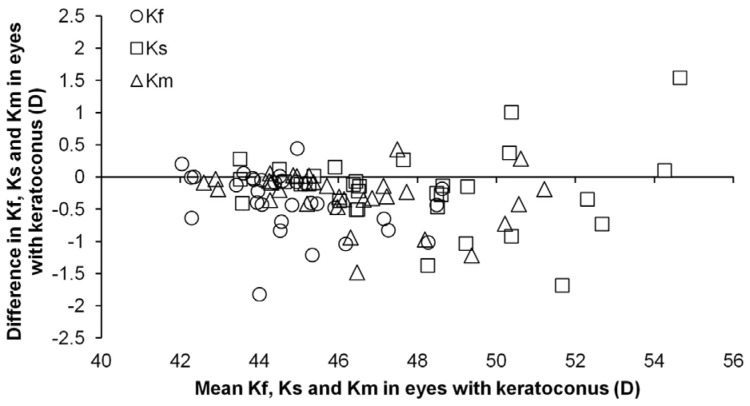
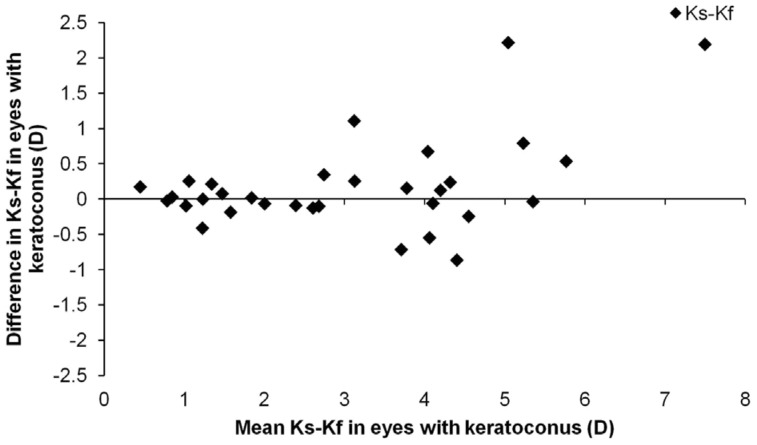
Table 3 reports the outcome of the comparison of measurement of the four parameters by the two instruments. Since good inter-examiner reproducibility was found in the previous step of the analysis, the table presents details of the evaluation only for examiner 1. Wilcoxon's test indicated that Placido disk-based topography significantly underestimated Kf and Km, and Ks to a minor extent. The Bland-Altman plots (Figures 1, 2) confirmed these results, as far as mean difference and width of the region of agreement. It follows that Ks-Kf was slightly (P=0.26) overestimated by Placido disk-based topography, with small mean difference and large region of agreement.
Table 3. Agreement between Placido disk-based topography and high-resolution rotating Scheimpflug camera in measuring corneal power in eyes with keratoconus.
| Instruments | Kf | Ks | Km | Ks-Kf |
| Placido | 44.63±1.65 | 47.76±3.06 | 46.12±2.23 | 3.14±1.92 |
| Scheimpflug | 44.99±1.81 | 47.95±3.05 | 46.41±2.33 | 2.96±1.63 |
| 1P | <0.01 | 0.03 | <0.01 | 0.26 |
| Difference between instruments | -0.37±0.47 | -0.19±0.60 | -0.29±0.40 | 0.18±0.66 |
| 95% LoA | -1.28 to +0.55 | -1.36 to +0.99 | -1.08 to +0.50 | -1.11 to +1.48 |
Kf: Flat keratometry; Ks: Steep keratometry; Km: Mean keratometry; Ks-Kf: Astigmatism; 95% LoA: 95% limits of agreement. 1Wilcoxon's signed-rank test.
x±s
Figure 1. Scatterplot demonstrating the differences between Placido disk-based topography and the high-resolution rotating Scheimpflug camera in measuring Kf, Ks, and Km in eyes with keratoconus, plotted against the mean value obtained with the two instruments.
Figure 2. Scatterplot demonstrating the differences between Placido disk-based topography and the high-resolution rotating Scheimpflug camera in measuring Ks-Kf in eyes with keratoconus, plotted against the mean value obtained with the two instruments.
Post-LASIK Eyes
One eye of 20 patients (mean age 34.4±7.1y; 16 women and 4 men) were analyzed on average 1.2±0.3y after LASIK. Eighteen had undergone myopic and 2 hyperopic LASIK. The mean preoperative spherical equivalent was -3.9±2.1 D (range +2.50 to -6.00 D).
Intra-examiner Repeatability
Table 4 shows the measurement repeatability by both instruments for examiner 1, as assessed by Sw, R, CoV, and ICC, as well as the results of Friedman's test on the three sets of measurements by the two instruments obtained for each parameter. The Sw, R, and CoV for measurement of all parameters by the high-resolution rotating Scheimpflug camera were lower as compared with Placido disk-based topography (Table 4). The ICC between measurements repeated by the same examiner were >0.90 for all parameters, except for Ks-Kf measured by the Placido disk-based topography (ICC=0.876, Table 4). Similar results were obtained for examiner 2.
Table 4. Intra-examiner repeatability of corneal power measurements by Placido disk-based topography and high-resolution rotating Scheimpflug camera in post-LASIK eyes.
| Parameters | 1P | Sw (D) | R (D) | CoV (%) | ICC (95% CI) |
| Kf | |||||
| Placido | 0.86 | 0.32 | 0.88 | 0.77 | 0.989 (0.976-0.995) |
| Scheimpflug | 0.79 | 0.06 | 0.17 | 0.15 | 1 (0.999-1) |
| Ks | |||||
| Placido | 0.68 | 0.32 | 0.88 | 0.77 | 0.989 (0.976-0.995) |
| Scheimpflug | 0.37 | 0.08 | 0.21 | 0.18 | 0.999 (0.999-1) |
| Km | |||||
| Placido | 0.86 | 0.31 | 0.86 | 0.75 | 0.989 (0.978-0.995) |
| Scheimpflug | 0.37 | 0.06 | 0.17 | 0.15 | 1 (0.999-1) |
| Ks-Kf | |||||
| Placido | 0.45 | 0.12 | 0.33 | 16.10 | 0.876 (0.760-0.944) |
| Scheimpflug | 0.07 | 0.10 | 0.28 | 13.54 | 0.909 (0.820-0.960) |
Kf: Flat keratometry; Ks: Steep keratometry; Km: Mean keratometry; Ks-Kf: Astigmatism; D: Diopters; Sw: Within-subject standard deviation; R: Coefficient of repeatability; CoV: Coefficient of variation; ICC: Intraclass correlation coefficient. 1Friedman's test.
Inter-examiner Reproducibility
Since all sets of the three measurements proved to be statistically equivalent (P>0.06), they were averaged to yield for each examiner an ensemble of series relative to each of the four parameters for the two instruments. Table 5 presents the results of Wilcoxon's test on all matched measurements by the two examiners and shows no statistically significant differences between examiners. The Sw, R, and CoV for all parameters measured by the high-resolution rotating Scheimpflug camera were lower as compared with Placido disk-based topography (Table 5). The ICC between examiners were >0.90 for all parameters measured by both instruments (Table 5).
Table 5. Inter-examiner reproducibility of corneal power measurements by Placido disk-based topography and high-resolution rotating Scheimpflug camera in post-LASIK eyes.
| Parameters | 1P | Sw (D) | R (D) | CoV (%) | ICC (95% CI) |
| Kf | |||||
| Placido | 0.99 | 0.23 | 0.64 | 0.56 | 0.994 (0.985-0.998) |
| Scheimpflug | 0.80 | 0.03 | 0.09 | 0.08 | 1 (1-1) |
| Ks | |||||
| Placido | 0.73 | 0.20 | 0.56 | 0.48 | 0.995 (0.988-0.998) |
| Scheimpflug | 0.07 | 0.05 | 0.15 | 0.13 | 1 (0.999-1) |
| Km | |||||
| Placido | 0.72 | 0.21 | 0.59 | 0.52 | 0.995 (0.986-0.998) |
| Scheimpflug | 0.99 | 0.03 | 0.09 | 0.08 | 1 (0.999-1) |
| Ks-Kf | |||||
| Placido | 0.58 | 0.08 | 0.23 | 11.43 | 0.935 (0.844-0.974) |
| Scheimpflug | 0.06 | 0.06 | 0.18 | 8.28 | 0.970 (0.919-0.987) |
Kf: Flat keratometry; Ks: Steep keratometry; Km: Mean keratometry; Ks-Kf: Astigmatism; D: Diopters; Sw: Within-subject standard deviation; R: Coefficient of repeatability; CoV: Coefficient of variation; ICC: Intraclass correlation coefficient. 1Wilcoxon's signed-rank test.
Agreement Between Instruments
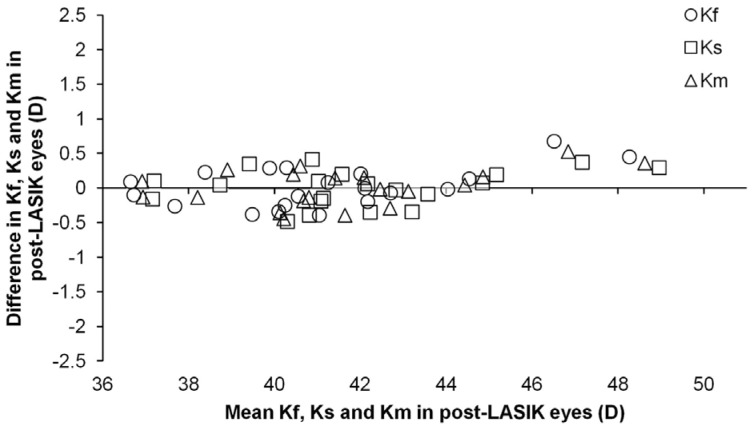
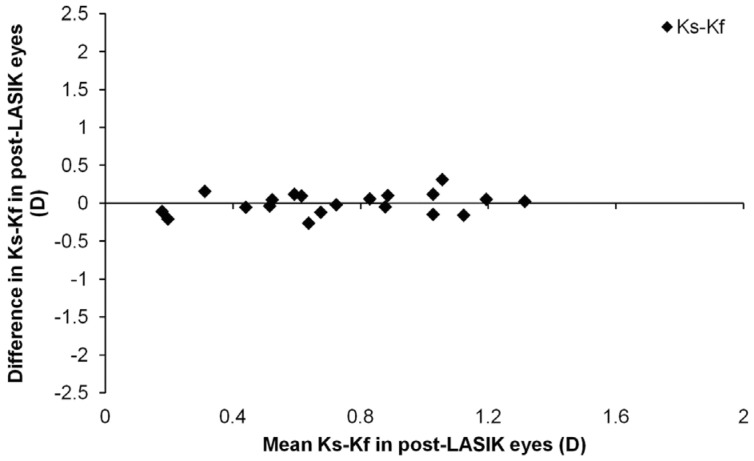
Table 6 reports the outcome of the comparison between the two instruments. Since good inter-examiner reproducibility was found in the previous step of the analysis, the details of the comparison are shown only for examiner 1. Wilcoxon's test indicated excellent agreement between the devices in the evaluation of Kf, Ks, Km, and Ks-Kf. The Bland-Altman plots (Figures 3, 4) confirmed these results, as far as mean difference and reduced width of the region of agreement.
Table 6. Agreement between Placido disk-based topography and high-resolution rotating Scheimpflug camera in measuring corneal power in post-LASIK eyes.
| Instruments | Kf | Ks | Km | Ks-Kf |
| Placido | 41.23±3.07 | 41.97±3.03 | 41.60±3.05 | 0.73±0.35 |
| Scheimpflug | 41.22±2.93 | 41.96±2.96 | 41.59±2.94 | 0.74±0.32 |
| 1P | 0.98 | 0.86 | 0.84 | 0.94 |
| Difference between instruments | 0.02±0.29 | 0.01±0.27 | 0.01±0.27 | 0.00±0.14 |
| 95% LoA | -0.54 to +0.58 | -0.51 to +0.53 | -0.51 to +0.53 | -0.28 to +0.27 |
Kf: Flat keratometry; Ks: Steep keratometry; Km: Mean keratometry; Ks-Kf: Astigmatism; 95% LoA: 95% limits of agreement. 1Wilcoxon's signed-rank test.
x±s
Figure 3. Scatterplot demonstrating the differences between Placido disk-based topography and the high-resolution rotating Scheimpflug camera in measuring Kf, Ks, and Km in post-LASIK eyes, plotted against the mean value obtained with the two instruments.
Figure 4. Scatterplot demonstrating the differences between Placido disk-based topography and the high-resolution rotating Scheimpflug camera in measuring Ks-Kf in post-LASIK eyes, plotted against the mean value obtained with the two instruments.
DISCUSSION
Keratoconic Eyes
Both Placido disk-based topography and the high-resolution rotating Scheimpflug camera provided repeatable and reproducible measurements in keratoconic eyes. The accuracy of the instruments was slightly lower than that reported in normal corneas [2]–[4]. Using both instruments, the intra-examiner/inter-examiner differences were not statistically significant (P>0.05), and the ICC were >0.90 for all parameters. The Sw, R, and CoV values showed that the intra-examiner/inter-examiner variability in measuring Ks-Kf by the two instruments was similar. The intra-examiner/inter-examiner variability for the Kf, Ks, and Km measurements by the high-resolution rotating Scheimpflug camera was lower as compared with Placido disk-based topography. The intra-examiner R had differences >0.25 D for Ks (0.61 vs 0.88 D), >0.50 D for Kf (0.32 vs 0.88 D), and Km (0.32 vs 0.84 D). Similarly, the inter-examiner R had differences >0.50 D for Kf (0.21 vs 0.81 D), Ks (0.40 vs 0.98 D), and Km (0.26 vs 0.87 D). These findings suggest that different thresholds for Placido disk-based topography and high-resolution rotating Scheimpflug camera should be used to define disease progression. Indeed, a higher instrument variability involves higher thresholds to define disease progression. Based on our results, the threshold for Kf, Ks, and Km should be 0.50 D when the high-resolution rotating Scheimpflug camera and 0.8 - 1 D when Placido disk-based topography is used.
Of note, however, is that since these thresholds were obtained in eyes with mild and moderate keratoconus, they might be not appropriate for evaluating eyes with advanced keratoconus. In eyes with advanced keratoconus, variability of measurements may increase[13]–[16]. In their study, Hashemi et al[13] reported that the variability of Kf and Ks was significantly increased in eyes with steep corneas. Comparison of keratoconic corneas with Ks<50 D versus >55 D showed that the R value of Kf increased by more than fourfold (from 0.36 to 1.66 D) and that of Ks by sevenfold (from 0.40 to 2.80 D). In keratoconic corneas with high astigmatism, the variability of curvature measurements may increase because patients find it difficult to fixate accurately during examination[14]. Moreover, small differences in instrument alignment between repeated scans can lead to wide variations of curvature measurements in eyes with very steep and irregular corneas.
As mentioned above, we observed that Placido disk-based topography was less reliable in measuring Kf, Ks, and Km than the high-resolution Scheimpflug camera. However, many instruments based on Placido disk principle are available. Using the Keratograph (Oculus Optikgeräte GmbH, Wetzlar, Germany), a Placido disk-based topographer, Ortiz-Toquero et al[17] found a better reliability of Kf and Ks measurements compared to our results. In 25 eyes with mean Kf of 45.30 and mean Ks of 47.84 D, the CoV values of these parameters were 0.36 and 0.47 D respectively. In our study, they were higher, being 0.72 and 0.67 D respectively.
The measurements taken with the two instruments were statistically different for Kf, Ks, and Km but not for Ks-Kf. On average, Placido disk-based topography underestimated Kf, Ks, and Km (-0.37, -0.19, and -0.29, respectively) and overestimated Ks-Kf (+0.18) as compared with high-resolution rotating Scheimpflug camera. Although these differences were clinically mild, the width of the region of agreement showed that the differences in measuring Kf, Ks, Km, and Ks-Kf by the two instruments ranged from 1.50 to 2.50 D. These data suggest that the two instruments are not interchangeable for corneal power measurements in keratoconus.
Post-LASIK Eyes
Also in the post-LASIK eyes, measurements by Placido disk-based topography and high-resolution rotating Scheimpflug camera were repeatable and reproducible. There were no statistically significant intra-examiner/inter-examiner differences with either instrument (P>0.05), and the ICC were >0.90 for all parameters except for Ks-Kf measured by Placido disk-based topography in the intra-examiner analysis. However, considering the Sw, R, and CoV values for Kf, Ks and Km, the variability of measurements by the high-resolution rotating Scheimpflug camera was considerably lower as compared with Placido disk-based topography. In the post-LASIK eyes, the reliability of the high-resolution rotating Scheimpflug was comparable with that found in normal corneas, but that of Placido disk-based topography was lower[2]–[4]. Furthermore, the intra-examiner and inter-examiner differences between instruments were high in the post-LASIK eyes. Intra-examiner R had differences >0.70 for Kf (0.17 vs 0.88 D) and >0.60 D for Ks (0.21 vs 0.88 D) and Km (0.17 vs 0.86 D). The inter-examiner R had differences >0.50 D for Kf (0.09 vs 0.64 D) and >0.40 for Ks (0.15 vs 0.56 D) and Km (0.09 vs 0.59 D). Based on our results, the corneal power variability between measurements in post-LASIK eyes should be 0.20 D with the high-resolution rotating Scheimpflug camera and 0.60-0.90 D with Placido disk-based topography for Kf, Ks, and Km. The variability between measurements by both instruments was similar for Ks-Kf (about 0.30 D).
A number of studies[18]–[22] have reported on the reliability of corneal power measurements in post-LASIK eyes. Two studies[18],[21] used the high-resolution rotating Scheimpflug camera and no studies have compared Placido disk-based topography and the high-resolution rotating Scheimpflug camera. Jain et al[18] obtained a repeatability coefficient of 0.29 for Km, that was slightly higher as compared with what we found in the current study (R=0.17). Ho wever, because Jain et al[18] performed 5 (not 3) consecutive measurements and measured the radius of curvature in millimeters (instead of corneal power in diopters) no direct comparison between their study and ours can be made. Also in the study by Chan et al[21] the repeatability coefficients of Ks, Kf and Km were slightly higher than in our study (0.55, 0.42, and 0.28 respectively). This difference may be due to the characteristics of the included eyes. In the study by Chan et al[21], the preoperative spherical equivalent was higher (-6.27±1.67) and the post-LASIK keratometric values were lower (39.49, 38.74 and 39.11 for Ks, Kf, and Km, respectively ) as compared to our study.
Agreement between the two technologies in measuring Kf, Ks, Km, and Ks-Kf was very good. As compared with the high-resolution rotating Scheimpflug camera, Placido disk-based topography slightly overestimated Kf, Ks, and Km, but the differences between the instruments (0.02, 0.01, 0.01 D, respectively) were not statistically significant. Moreover, no difference was found in measuring Ks-Kf. Although these differences were clinically negligible, the width of the region of agreement showed that the differences between the two instruments were about 1 D for Kf, Ks, Km and about 0.50 D for Ks-Kf. These data suggest that the two instruments are not completely interchangeable for corneal power measurements in post-LASIK eyes.
The present study has some limitations. First, the threshold values found in this study need to be confirmed in a larger sample of patients. Second, the study did not test the differences between instruments in eyes with advanced keratoconus and in those with poor tear film stability. In such cases, the difference might increase. Third, the study did not include a control group.
In conclusion, we found that high-resolution rotating Scheimpflug camera has higher reliability compared to Placido disk-based topography in measuring most of corneal power parameters in keratoconic and post-LASIK eyes. The reliability of both instruments for measuring astigmatism was similar. Agreement between the two instruments was fair in keratoconus and very good in post-LASIK eyes, although they were not completely interchangeable in measuring corneal power parameters in these eyes.
Acknowledgments
Prof. Laura Bergamasco provided assistance with statistical analysis revision.
Conflicts of Interest: Penna RR, None; de Sanctis U, None; Catalano M, None; Brusasco L, None; Grignolo FM, None.
REFERENCES
- 1.Wollensak G, Spoerl E, Seiler T. Riboflavin/ultraviolet-a-induced collagen crosslinking for the treatment of keratoconus. Am J Ophthalmol. 2003;135(5):620–627. doi: 10.1016/s0002-9394(02)02220-1. [DOI] [PubMed] [Google Scholar]
- 2.Hidalgo IR, Rozema JJ, Dhubhghaill SN, Zakaria N, Koppen C, Tassignon MJ. Repeatability and inter-device agreement for three different methods of keratometry: Placido, Scheimpflug, and color LED corneal topography. J Refract Surg. 2015;31(3):176–181. doi: 10.3928/1081597X-20150224-01. [DOI] [PubMed] [Google Scholar]
- 3.Klijn S, Reus NJ, Sicam VA. Evaluation of keratometry with a novel Color-LED corneal topographer. J Refract Surg. 2015;31(4):249–256. doi: 10.3928/1081597X-20150212-01. [DOI] [PubMed] [Google Scholar]
- 4.Laursen JV, Jeppesen P, Olsen T. Precision of 5 different keratometry devices. Int Ophthalmol. 2016;36(1):17–20. doi: 10.1007/s10792-015-0069-3. [DOI] [PubMed] [Google Scholar]
- 5.Delrivo M, Ruiseñor Vázquez PR, Galletti JD, Garibotto M, Fuentes Bonthoux F, Pfortner T, Galletti JG. Agreement between placido topography and Scheimpflug tomography for corneal astigmatism assessment. J Refract Surg. 2014;30(1):49–53. doi: 10.3928/1081597X-20131217-06. [DOI] [PubMed] [Google Scholar]
- 6.Mehravaran S, Asgari S, Bigdeli S, Shahnazi A, Hashemi H. Keratometry with five different techniques: a study of device repeatability and inter-device agreement. Int Ophthalmol. 2014;34(4):869–875. doi: 10.1007/s10792-013-9895-3. [DOI] [PubMed] [Google Scholar]
- 7.Rozema JJ, Wouters K, Mathysen DG, Tassignon MJ. Overview of the repeatability, reproducibility, and agreement of the biometry values provided by various ophthalmic devices. Am J Ophthalmol. 2014;158(6):1111–1120.e1. doi: 10.1016/j.ajo.2014.08.014. [DOI] [PubMed] [Google Scholar]
- 8.International organization for standardization . Part 1: General principles and definitions. Geneva, Switzerland: 1994. Accuracy (trueness and precision) of measurement methods and results. ISO 5725-1. [Google Scholar]
- 9.International organization for standardization . Part 2: Basic methods for the determination of repeatability and reproducibility of a standard measurement method. Geneva, Switzerland: 1994. Accuracy (trueness and precision) of measurement methods and results. ISO 5725-2. [Google Scholar]
- 10.Bland JM, Altman DG. Measurement error. BMJ. 1996;312(7047):1654. doi: 10.1136/bmj.312.7047.1654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bland JM, Altman DG. Measuring agreement in method comparison studies. Stat Methods Med Res. 1999;8(2):135–160. doi: 10.1177/096228029900800204. [DOI] [PubMed] [Google Scholar]
- 12.Zadnik K, Barr JT, Gordon MO, Edrington TB. Biomicroscopic signs and disease severity in keratoconus. Collaborative Longitudinal Evaluation of Keratoconus (CLEK) Study Group. Cornea. 1996;15(2):139–146. doi: 10.1097/00003226-199603000-00006. [DOI] [PubMed] [Google Scholar]
- 13.Hashemi H, Yekta A, Khabazkhoob M. Effect of keratoconus grades on repeatability of keratometry readings: comparison of 5 devices. J Cataract Refract Surg. 2015;41(5):1065–1072. doi: 10.1016/j.jcrs.2014.08.043. [DOI] [PubMed] [Google Scholar]
- 14.Hashemi K, Guber I, Bergin C, Majo F. Reduced precision of the Pentacam HR in eyes with mild to moderate keratoconus. Ophthalmology. 2015;122(1):211–212. doi: 10.1016/j.ophtha.2014.08.026. [DOI] [PubMed] [Google Scholar]
- 15.Vianna LM, Muñoz B, Hwang FS, Gupta A, Jun AS. Variability in Oculus Pentacam tomographer measurements in patients with keratoconus. Cornea. 2015;34(3):285–289. doi: 10.1097/ICO.0000000000000344. [DOI] [PubMed] [Google Scholar]
- 16.Flynn TH, Sharma DP, Bunce C, Wilkins MR. Differential precision of corneal Pentacam HR measurements in early and advanced keratoconus. Br J Ophthalmol. 2016;100(9):1183–1187. doi: 10.1136/bjophthalmol-2015-307201. [DOI] [PubMed] [Google Scholar]
- 17.Ortiz-Toquero S, Rodriguez G, de Juan V, Martin R. Repeatability of placido-based corneal topography in keratoconus. Optom Vis Sci. 2014;91(12):1467–1473. doi: 10.1097/OPX.0000000000000421. [DOI] [PubMed] [Google Scholar]
- 18.Jain R, Dilraj G, Grewal SP. Repeatability of corneal parameters with Pentacam after laser in situ keratomileusis. Indian J Ophthalmol. 2007;55(5):341–347. [PMC free article] [PubMed] [Google Scholar]
- 19.Savini G, Barboni P, Carbonelli M, Hoffer KJ. Repeatability of automatic measurements by a new Scheimpflug camera combined with Placido topography. J Cataract Refract Surg. 2011;37(10):1809–1816. doi: 10.1016/j.jcrs.2011.04.033. [DOI] [PubMed] [Google Scholar]
- 20.Savini G, Carbonelli M, Barboni P, Hoffer KJ. Repeatability of automatic measurements performed by a dual Scheimpflug analyzer in unoperated and post-refractive surgery eyes. J Cataract Refract Surg. 2011;37(2):302–309. doi: 10.1016/j.jcrs.2010.07.039. [DOI] [PubMed] [Google Scholar]
- 21.Chan TC, Biswas S, Yu M, Jhanji V. Longitudinal evaluation of cornea with swept-source optical coherence tomography and Scheimpflug imaging before and after Lasik. Medicine (Baltimore) 2015;94(30):e1219. doi: 10.1097/MD.0000000000001219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kanellopoulos AJ, Asimellis G. Color light-emitting diode reflection topography: validation of keratometric repeatability in a large sample of wide cylindrical-range corneas. Clin Ophthalmol. 2015;9:245–252. doi: 10.2147/OPTH.S68371. [DOI] [PMC free article] [PubMed] [Google Scholar]