Abstract
AIM
To evaluate the distribution of refractive error in young subjects in a rural area of Paraguay in the context of an international cooperation campaign for the prevention of blindness.
METHODS
A sample of 1466 young subjects (ranging from 3 to 22 years old), with a mean age of 11.21±3.63 years old, were examined to assess their distance visual acuity (VA) and refractive error. The first screening examination performed by trained volunteers, included visual acuity testing, autokeratometry and non-cycloplegic autorefraction. Inclusion criteria for a second complete cycloplegic eye examination by an optometrist were VA <20/25 (0.10 logMAR or 0.8 decimal) and/or corneal astigmatism ≥1.50 D.
RESULTS
An uncorrected distance VA of 0 logMAR (1.0 decimal) was found in 89.2% of children. VA <20/25 and/or corneal astigmatism ≥1.50 D was found in 3.9% of children (n=57), with a prevalence of hyperopia of 5.2% (0.2% of the total) in this specific group. Furthermore, myopia (spherical equivalent ≤-0.5 D) was found in 37.7% of the refracted children (0.5% of the total). The prevalence of refractive astigmatism (cylinder ≤-1.50 D) was 15.8% (0.6% of the total). Visual impairment (VI) (0.05≤VA≤0.3) was found in 12/114 (0.4%) of the refracted eyes. Main causes for VI were refractive error (58%), retinal problems (17%, 2/12), albinism (17%, 2/12) and unknown (8%, 1/12).
CONCLUSION
A low prevalence of refractive error has been found in this rural area of Paraguay, with higher prevalence of myopia than of hyperopia.
Keywords: refractive error, blindness, visual impairment, myopia, hyperopia
INTRODUTION
Uncorrected refractive errors are the main cause of visual impairment (VI) in developing countries (43%), followed by cataract (33%)[1]. Refractive errors were not considered as a cause of blindness until recently, with the increasing use of the concept of presenting visual acuity (VA) for defining blindness[2].
The global magnitude of low vision caused by uncorrected refractive error (nearsightedness, farsightedness or astigmatism) published in the Bulletin of the World Health Organization in 2010 is estimated to be 103 million[1].
The distribution of blindness is not homogeneous throughout the world, with 90% of blindness being present in developing countries[3]. Blindness due to refractive error in a specific country suggests that its access to eye care services are in general poor because the management of a refractive error is probably the easiest and most effective eye care service[4]–[5].
The overall prevalence of blindness in the American and the Caribbean regions was found to be of 0.45/1000, with the majority of these regions (67%) in countries with under 5 death rates above 30/1000 live births[6].
Children are the most fragile social stratum for VI and blindness, although the incidences of these conditions are lower than in adults. Given the potential life of a child, a refractive error at the young age may have a lifelong impact[7]. In many middle-income and low-income countries, 30%-72% of childhood blindness is avoidable, and refractive error, which is easily correctable with glasses, is the most common cause of bilateral VI[8]–[9].
Although there is a growing interest in the elimination of avoidable blindness due to uncorrected refractive error[10], and the eye care services for children have improved[11], a recalculation of global estimates of prevalence, incidence, and cause of children's eye problems is needed.
Paraguay is a Latin America country of middle development, with a human development index of 0.665. The gross domestic product per capita in purchasing power parity (PPP) terms is $4107. Population living below $1.25 PPP per day is 5.1%[12].
In this study, we evaluated the distribution of the refractive error in young subjects of the rural area of San Roque González de Santa Cruz (also called Tavapy) around 100 km south Paraguay's capital Asuncion, in the context of an international cooperation campaign for the prevention of blindness. The district of San Roque Gonzalez de Santa Cruz, is located in the center of the Department of Paraguarí. The economy is based in livestock and farming and has a density of 26 people per km2. Although access to a general practitioner is almost universal in the area, access to a vision specialist is not easily available. People from this rural area have to travel to the capital city, Asuncion, to have a comprehensive eye exam. The patient must assume the travel and specialist consultation expenses with the additional cost of the glasses, which is not affordable by most of people living in this rural area. To this date, there is only one study evaluating the refractive error in a school age population in Paraguay, only including 324 children[13].
SUBJECTS AND METHODS
Sample Selection
All school-age children from preschool (ages three to five), primary (ages six to eleven) and secondary (ages twelve to eighteen) in the rural area of San Roque González de Santa Cruz were contacted and informed about the campaign of eye examinations. Due to the discontinuity in the studies, some students were up to 22 years old.
We consider all those children attending school in August 2011 between age 3 and 22 years old whose parents signed the informed consent for examination. Table 1 shows the name of the schools visited and the number of children tested in each one. A specific date for performing the eye examinations was defined according to the preferences and possibilities of each school. The study was cross-sectional, and aimed at evaluating the prevalence of refractive errors and its contribution to VI in this middle income area of Latin America. The parents gave written consent for the study that adhered to the tenets of the Declaration of Helsinki.
Table 1. Distribution of children screened and examined by school.
| School name | No. of children screened | No. of children examined |
| Avelino Delvalle-Arazaty | 62 | 4 |
| Calle-Simbrón | 100 | 9 |
| Cañada-Simbrón | 162 | 10 |
| Cap. Benítez | 41 | 5 |
| Cerrito | 101 | 9 |
| EE.UU | 196 | 14 |
| Fidelino González-Moquete | 78 | 6 |
| Loma-Simbrón | 101 | 5 |
| Martin Molinas-Moquete | 93 | 4 |
| Mbocayaty | 112 | 11 |
| Niño Jesús-Matachi | 96 | 6 |
| Puerta del Ypoa | 39 | 3 |
| Rep. Venezuela | 106 | 15 |
| San Alfonso-Rincón | 64 | 5 |
| San Blas-Arazaty | 62 | 4 |
| Valle Pucu-Mbocayaty | 34 | 3 |
| Yvypytandy-Simbrón | 19 | 1 |
| Total | 1466 | 114 |
Examination Protocol
The examination protocol of the campaign was divided in two parts. A previous visual screening was performed on all children by a trained non-eye care group of volunteers. This exam included presenting or uncorrected distance visual acuity (UCDVA) (E Snellen chart at 5 m), autokeratometry and non-cycloplegic autorefraction (Retinomax, K-3 plus) in both eyes. Patient name, address, age and sex were also recorded. All data were entered into a customized Excel (Microsoft Windows) page to select those children that met one or both of the following inclusion criteria for an additional comprehensive examination: VA of 20/25 or worse and corneal astigmatism (CA) of 1.50 D or higher. This second eye examination was performed on those children meeting the criteria mentioned and included the following tests performed by three experienced optometrists: ocular motility, retinoscopy, cycloplegic and subjective refraction and dilated fundus examination. Cycloplegic refraction was performed 30min after instilling 1% cyclopentolate administered two times at intervals of 5min. Additionally, anterior segment integrity was explored by means of a portable slit lamp.
Myopia was defined as the presence of a spherical equivalent (SE) of -0.50 D or more and hyperopia as an SE of +1.50 D or more. Children were considered as myopic if one or both eyes were myopic (including antimetropic patients), hyperopic if one or both eyes were hyperopic as long as neither eye was myopic, and emmetropic if neither eye was myopic or hyperopic[14]. The prevalence of astigmatism was investigated at the following ranges: cylinder ≥1.00 D and ≥1.50 D. The prevalence of refractive error was calculated assuming that eyes with normal or near-normal vision (VA≥0.8) were emmetropic. This assumption was made considering the fact that subjective refraction data were not available for this type of eyes. According to WHO definitions, a logMAR UCDVA between 0.5 and 1.0 (between 0.05 and 0.3 in decimal notation) was considered as VI and logMAR UCDVA lower than 0.5 (0.05) as blindness[15].
Refraction Notation
The spherocylindrical refractions obtained were converted to vectorial notation using the power vector method described by Thibos and Horner. Using this procedure, any spherocylindrical refractive error can be expressed by 3 dioptric powers: M, J0 and J45, being M a spherical lens equal to the SE of the given refractive error, and J0 and J45 two Jackson crossed cylinders equivalent to the conventional cylinder. These numbers are the coordinates of a point in a three-dimensional dioptric space (M, J0, J45). The length of this vector is a measure of the overall blurring strength B of a spherocylindrical refractive error.
According to the power vector method, manifest refractions in conventional script notation [S (sphere), C (cylinder)×φ (axis)] were converted to power vector coordinates and overall blurring strength (B) by the following formulas: M=S+C/2; J0=(-C/2) cos (2 φ); J45=(-C/2) sin (2 φ); and B=(M2+J02+J452)1/2.
Statistical Analysis
Data analysis was performed using the software SPSS for Windows version 19.0 (IBM, Armonk, NY, USA). Mean, standard deviation (SD) and range for each of the parameters evaluated were calculated. Normality of data samples was confirmed by means of the Kolmogorov-Smirnov test. The degree of correlation between different clinical variables was assessed by means of the coefficient of correlation (Pearson or Spearman depending if the condition of normality could be assumed or not). Correlations were considered to be statistically significant when the associated P-value was <0.05.
RESULTS
A total of 1466 young subjects (age range, 3 to 22 years old) of a mean age of 11.21±3.63 years old were screened. A total of 2932 eyes were autorefracted with 114 (3.9%) undergoing a second complete eye examination because they had a VA<20/25 (0.10 logMAR) and/or CA ≥1.50 D. The gender distribution of the sample analyzed was even, with 50.1% of women. A total of 86% of subjects were 15 years old or younger.
Visual Outcomes
Mean logMAR UCDVA for the 1466 children screened was 0.016±0.074 (range 1.00 to 0.00 logMAR). The UCDVA was 20/25 (0.1 logMAR, 0.8 decimal) or worse and 20/250 (1.30 logMAR, 0.05 decimal) or worse in the better eye in 96.3% and 0% of eyes, respectively. 89.2% of subjects had UCDVA of 0 logMAR (1 decimal). 1.9% had an UCDVA of 20/40 or worse.
VI, considered as a logMAR UCDVA between 0.5 and 1.0 (between 0.05 and 0.3 decimal), was found in 12/114 (0.4%) of the refracted eyes. Refractive error was the main cause of VI in the analyzed sample. Indeed, 7 (58%) of the 12 eyes with VI achieved with refractive correction a best corrected distance visual acuity (BCDVA) of 20/25 or better in both eyes. Other causes of VI found in our sample were retinal problems in 2/12 (17%), albinism in 2/12 (17%) and unknown causes 1/12 (8%). Amblyopia, defined as a difference of two lines or more between the two eyes or a BCDVA of 20/30 or worse, was found in 14 eyes (12.3%). The UCDVA was better than 0.8 and worse than or equal to 0.3 in 3.3% of eyes.
Keratometric and Refractive Outcomes
Mean keratometric outcomes for the whole sample are summarized and displayed in Table 2.
Table 2. Distribution of the keratometric measures obtained in the analyzed study.
| Keratometric parameters (n=2932) | Mean (SD) | Range |
| K1 (mm) | 7.86 (0.27) | 7.07 to 8.88 |
| K2 (mm) | 7.67 (0.28) | 6.82 to 9.85 |
| KM (mm) | 7.77 (0.27) | 6.96 to 8.91 |
| Astig (D) | 0.19 (0.10) | 0 to 1.89 |
K1: Flattest keratometric reading; K2: Steepest keratometric reading; KM: Mean keratometry; Astig: Keratometric astigmatism.
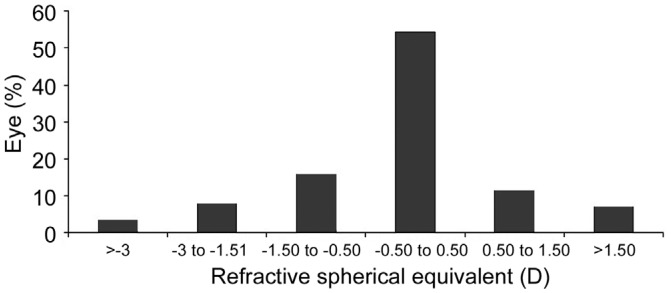
The proportion of myopic patients (SE≤-0.50 D) was 37.7% (43/114) of the refracted children that corresponded with a 1.5 % of whole sample (2932 eyes). Mean magnitude of myopia was -1.42±1.41 D. The percentage of myopia in the sample of eyes refracted according to these other definitions was SE≤-1.00 D 21.9% (25/114) and SE≤-3.00 3.5% (4/114). The proportion of hyperopic patients defined as SE≥+2.00 D was 5.2% (6/114), a 0.2% of the total, decreasing to 1.7% (2/114) when a SE≥+3.00 D was considered. Mean magnitude of hyperopia was +3.4±1.3 D (Figure 1).
Figure 1. Distribution of the SE in the group of eyes from the sample that were refracted (n=114).
Refractive astigmatism (RA) of 1.50 D or more was present in 15.8% (18/114) of eyes (0.6% of the total) and of 1.00 D or more in 34.2% of eyes (39/114) which corresponds with 1.3% of the total. Mean magnitude of RA was -3.4±1.7 D. Table 3 summarizes the refractive data in conventional format as well as in vector notation.
Table 3. Mean values of refractive parameters and of its power vector components in the sample of eyes in which manifest refraction was performed in the current study (114 children).
| Refractive parameters | Mean (SD) | Range |
| Sphere (D) | +0.14 (1.55) | -6.50 to +5.50 |
| Cylinder (D) | -0.77 (1.31) | -6.75 to 0.00 |
| SE (D) | -0.25 (1.44) | -6.75 to +3.75 |
| J0 (D) | -0.08 (0.70) | -1.64 to +3.32 |
| J45 (D) | -0.02 (0.29) | -0.98 to +1.17 |
| B (D) | 1.07 (1.25) | 0.00 to 6.89 |
SE: Spherical equivalent; J0 and J45: Power vector components of manifest cylinder; B: Overall blurring strength of the manifest spherocylindrical error.
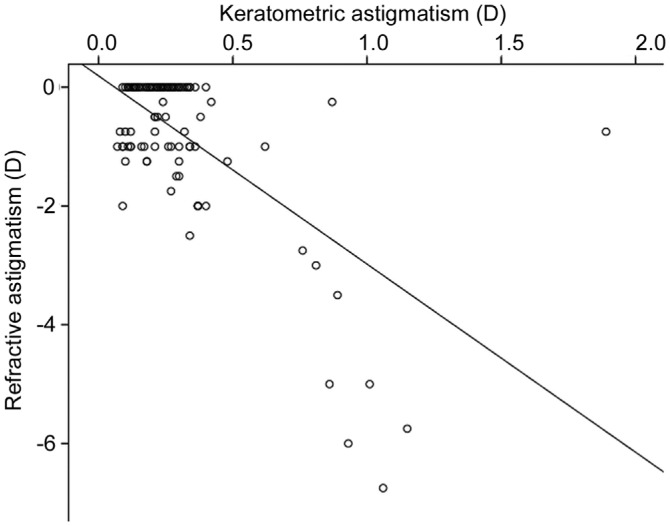
No significant correlation of SE in refracted patients with age was found (r=-0.21, P=0.11). In addition, manifest SE did not correlate with mean keratometry (r=0.09, P=0.37) and keratometric astigmatism (r=0.11, P=0.25). In contrast, a significant correlation between manifest and keratometric cylinder was found (r=-0.64, P<0.01) (Figure 2).
Figure 2. Scattergram showing the relationship between the magnitude of the RA and the magnitude of CA for 114 eyes.
The adjusting line to the data obtained by means of the least squares fit is shown (R2=0.40) and the RA is correlated with the CA with this formula: RA=0.19-3.17×CA.
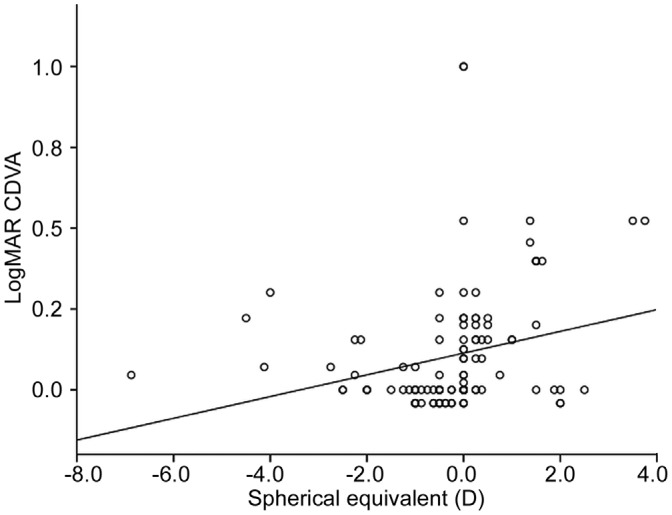
Likewise, a statistically significant but weak correlation was found between SE and BCDVA (r=0.26, P<0.01) (Figure 3).
Figure 3. Scattergram showing the relationship between the SE and the logMAR CDVA for 114 eyes.
The adjusting line to the data obtained by means of the least-squares fit is shown (R2=0.06). The spherical equivalent is correlated with the corrected distance visual acuity with this formula: SE=0.11+0.03×CDVA.
DISCUSSION
The south American population encompasses an extremely diverse set of nations. In Paraguay, the social differences in the population are significant, with the presence of highly educated and wealthy people who have access to the most developed eye care systems, to very poor people with limited access to any type of eye care service[16]. In addition, Paraguay has a scarce scientific production in Ophthalmology and Vision[17]. Therefore, there was a need for the study and characterization of the refractive error in different regions of this specific country.
In our sample from a rural area of Paraguay, a total of 89.2% of subjects had UCDVA of 0 logMAR (1 decimal), a percentage very close to the 85.3% found in a urban school children of low-income families in Kolkata (India)[18], and worse than that found in Nigeria (97.7%)[19]. Only 1.9% of subjects had an UCDVA of 20/40 or worse compared to the 4.82% found in Brazil[20]. Keratometric mean values found in our sample were normal and similar to those reported in other young populations[21].
Regarding refraction, the mean vector parameters obtained in the current study (J0: -0.08±0.70 D, J45: -0.02±0.29 D, B: 1.07±1.25 D) were very similar to those found by our research group in a rural population of Kenya (J0: -0.10±0.30 D, J45: -0.01± 0.07 D, B: 1.12±0.73 D)[22]. In a study with a Malaysian young population, Choong et al[23] found a mean binocular subjective refraction of -0.62±2.51 D (95% CI -1.07 to -0.16), a slightly more myopic result than our mean SE (-0.25±1.44 D).
Refractive error was the main cause of VI in our series (58%), as in another study performed in Chile in which the percentage of decreased VA due to uncorrected refractive error in children was of 55%[24]. In low-middle income school children of Brazil, refractive error was the cause of VI in one or both eyes in 76.8% of children. Regarding amblyopia, the percentage found in our study (12.3%) was similar to that found by Salomao et al[25] (11.4%) in a total of 2441 Brazilian children.
We found a prevalence of myopia (SE≤-0.5 D) of 37.7% (1.5% of the total) and a prevalence of hyperopia (SE ≥+2 D) of 5.2% (0.2% of the total) in the sample of refracted children. The proportion of myopic patients in our series is similar to the one reported by Carter et al[13] (from 1.2% to 1.4% depending on the ethnicity) in a study conducted at the capital city of Paraguay, Asuncion. In contrast, these authors found a higher prevalence of hyperopia (from 34.2% to 46.3%, depending on the ethnicity). This high hyperopia prevalence also contrasts with the results of a recent study from India, in which myopia and hyperopia was present in 11.9% and 2.5% of children, respectively[18]. In India, Bagchi et al[26] reported in a population of 45 087 urban students a prevalence of myopia of 2.85%.
A great number of factors may have accounted for the significant differences in the prevalence of myopia and hyperopia between studies, such as the type of population selected from the country evaluated (rural or urban), the development of the country, the quality of the eye services of each country, or even the tests and conditions used for evaluating the VA. There was a trend of a higher proportion of myopia than hyperopia in our evaluated population which contrasts with the mildly hyperopic children found in the refractive error study[27].
The proportion of RA in our study (1.00 D or more) was 34.2% (1.3% of the total). This finding is consistent with the proportion of astigmatism found in a population of children in Nepal[28], but higher than the one found in Brazil[29] and Asuncion (Paraguay)[13].
Regarding the relationship of SE with other clinical factors, no significant correlations were found with age, mean keratometry and keratometric astigmatism. In a study among children in Brazil, myopic VI (SE<-0.50 D in one or both eyes) was not associated with age or sex as well as hyperopic VI (SE≥2.00 D)[25]. A significant inverse correlation was found in our sample between refractive and keratometric astigmatism, suggesting that eyes with significant RA (high negative cylinder) had large levels of CA. This is coherent considering the optical relevance of the first corneal surface. Remón et al[30] determined in an adult population by means of regression analysis a linear model relating corneal and RA expressed in their power vector components (J0 and J45).
This study presents some drawbacks, such as its design. A population-based design would have been a more suitable design for this type of study. In any case, given the lack of information about the refractive error distribution of the area evaluated, we believe that our data can be of interest for the scientific community.
In conclusion, refractive error seems to be a not very common disorder among the children of the rural area of San Roque González de Santa Cruz-Tavapy of Paraguay, with a low proportion of patients with VI due to refractive error in comparison with other studies evaluating the visual function in rural areas of other low-income countries. Refractive error is the main cause of VI in this specific population, which can be avoided, with the establishment of an effective eye care service in this rural area.
Acknowledgments
Conflicts of Interest: Signes-Soler I, None; Hernández-Verdejo JL, None; Estrella Lumeras MA, None; Tomás Verduras E, None; Piñero DP, None.
REFERENCES
- 1.Pascolini D, Mariotti SP. Global estimates of visual impairment: 2010. Br J Ophthalmol. 2012;96(5):614–618. doi: 10.1136/bjophthalmol-2011-300539. [DOI] [PubMed] [Google Scholar]
- 2.Murthy GV, Gupta SK, Ellwein LB, Muñoz SR, Pokharel GP, Sanga L, Bachani D. Refractive error in children in an urban population in New Delhi. Invest Ophthalmol Vis Sci. 2002;43(3):623–631. [PubMed] [Google Scholar]
- 3.Cunningham ET., Jr World blindness-no end in sight. Br J Ophthalmol. 2001;85(3):253. doi: 10.1136/bjo.85.3.253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dandona R, Dandona L. Refractive error blindness. Bull World Health Organ. 2001;79(3):237–243. [PMC free article] [PubMed] [Google Scholar]
- 5.Naidoo KS, Jaggernath J. Uncorrected refractive errors. Indian J Ophthalmol. 2012;60(5):432–437. doi: 10.4103/0301-4738.100543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Munoz B, West SK. Blindness and visual impairment in the Americas and the Caribbean. Br J Ophthalmol. 2002;86(5):498–504. doi: 10.1136/bjo.86.5.498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Courtright P, Hutchinson AK, Lewallen S. Visual impairment in children in middle- and lower-income countries. Arch Dis Child. 2011;96(12):1129–1134. doi: 10.1136/archdischild-2011-300093. [DOI] [PubMed] [Google Scholar]
- 8.Nallasamy S, Anninger WV, Quinn GE, Kroener B, Zetola NM, Nkomazana O. Survey of childhood blindness and visual impairment in Botswana. Br J Ophthalmol. 2011;95(10):1365–1370. doi: 10.1136/bjo.2010.189068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Maida JM, Mathers K, Alley CL. Pediatric ophthalmology in the developing world. Curr Opin Ophthalmol. 2008;19(5):403–408. doi: 10.1097/ICU.0b013e328309f180. [DOI] [PubMed] [Google Scholar]
- 10.Naidoo KS, Wallace DB, Holden BA, Minto H, Faal HB, Dube P. The challenge of uncorrected refractive error: driving the agenda of the Durban Declaration on refractive error and service development. Clin Exp Optom. 2010;93(3):131–136. doi: 10.1111/j.1444-0938.2010.00455.x. [DOI] [PubMed] [Google Scholar]
- 11.Gogate P, Kalua K, Courtright P. Blindness in childhood in developing countries: time for a reassessment? PLoS Med. 2009;6(12):e1000177. doi: 10.1371/journal.pmed.1000177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.UNDP International Human Development Indicators. Human development reports for Paraguay 2011. 2011. Available at http://hdrstatsundp org/en/countries/profiles/PRY html.
- 13.Carter MJ, Lansingh VC, Schacht G, Rio Del AM, Scalamogna M, France TD. Visual acuity and refraction by age for children of three different ethnic groups in Paraguay. Arq Bras Oftalmol. 2013;76(2):94–97. doi: 10.1590/s0004-27492013000200008. [DOI] [PubMed] [Google Scholar]
- 14.Negrel AD, Maul E, Pokharel GP, Zhao J, Ellwein LB. Refractive error study in children: sampling and measurement methods for a multi-country survey. Am J Ophthalmol. 2000;129(4):421–426. doi: 10.1016/s0002-9394(99)00455-9. [DOI] [PubMed] [Google Scholar]
- 15.World Health Organization Subjective assessment of visual functioning and disability weights. WHO; Document WHO_PBL_03 91 2003. Geneva. Ref Type: Generic. Available at http://www.who.int/blindness/Final1stMonitoringCttee2006.pdf.
- 16.Limburg H, Barria von-Bischhoffshausen F, Gomez P, Silva JC, Foster A. Review of recent surveys on blindness and visual impairment in Latin America. Br J Ophthalmol. 2008;92(3):315–319. doi: 10.1136/bjo.2007.125906. [DOI] [PubMed] [Google Scholar]
- 17.Ragghianti CP, Martinez R, Martins J, Gallo JE. Comparative study of scientific publications in Ophthalmology and Visual Sciences in Argentina, Brazil, Chile, Paraguay and Uruguay (1995-2004) Arq Bras Oftalmol. 2006;69(5):719–723. doi: 10.1590/s0004-27492006000500019. [DOI] [PubMed] [Google Scholar]
- 18.Ghosh S, Mukhopadhyay U, Maji D, Bhaduri G. Visual impairment in urban school children of low-income families in Kolkata, India. Indian J Public Health. 2012;56(2):163–167. doi: 10.4103/0019-557X.99919. [DOI] [PubMed] [Google Scholar]
- 19.Opubiri I, Pedro-Egbe CN. Screening of primary school children for refractive error in South-South Nigeria. Ethiop J Health Sci. 2012;22(2):129–134. [PMC free article] [PubMed] [Google Scholar]
- 20.Moraes Ibrahim F, Moraes Ibrahim M, Pomepo de Camargo JR, Veronese Rodrigues Mde L, Scott IU, Silva Paula J. Visual impairment and myopia in Brazilian children: a population-based study. Optom Vis Sci. 2013;90(3):223–227. doi: 10.1097/OPX.0b013e31828197fd. [DOI] [PubMed] [Google Scholar]
- 21.Ubolsing S, Charoensri A. Keratometry in Thai children from newborn to the age of ten: a retrospective study. J Med Assoc Thai. 2006;89(Suppl 3):S196–S199. [PubMed] [Google Scholar]
- 22.Signes-Soler I, Pinero DP, Javaloy J. Prevalence of visual problems in a rural population of Kenya. Acta Ophthalmol. 2013;91(2):e165–166. doi: 10.1111/j.1755-3768.2012.02507.x. [DOI] [PubMed] [Google Scholar]
- 23.Choong YF, Chen AH, Goh PP. A comparison of autorefraction and subjective refraction with and without cycloplegia in primary school children. Am J Ophthalmol. 2006;142(1):68–74. doi: 10.1016/j.ajo.2006.01.084. [DOI] [PubMed] [Google Scholar]
- 24.Maul E, Barroso S, Munoz SR, Sperduto RD, Ellwein LB. Refractive error study in children: results from La Florida, Chile. Am J Ophthalmol. 2000;129(4):445–454. doi: 10.1016/s0002-9394(99)00454-7. [DOI] [PubMed] [Google Scholar]
- 25.Salomao SR, Cinoto RW, Berezovsky A, Mendieta L, Nakanami CR, Lipener C, Muñoz Ede H, Ejzenbaum F, Belfort R, Jr, Pokharel GP, Ellwein LB. Prevalence and causes of visual impairment in low-middle income school children in Sao Paulo, Brazil. Invest Ophthalmol Vis Sci. 2008;49(10):4308–4313. doi: 10.1167/iovs.08-2073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bagchi K, Sarkar SN, Chattopadhyaya T, Dan A. Vision screening programme among school children-evaluation of the outcome in a selected urban locality. J Indian Med Assoc. 2008;106(5) [PubMed] [Google Scholar]
- 27.Morgan IG, Rose KA, Ellwein LB, Refractive Error Study in Children Survey Group Is emmetropia the natural endpoint for human refractive development? An analysis of population-based data from the refractive error study in children (RESC) Acta Ophthalmol. 2010;88(8):877–884. doi: 10.1111/j.1755-3768.2009.01800.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rai SK, Thapa HB, Sharma MK, Dhakhwa K, Karki R. The distribution of refractive errors among children attending Lumbini Eye Institute, Nepal. Nepal J Ophthalmol. 2012;4(1):90–95. doi: 10.3126/nepjoph.v4i1.5858. [DOI] [PubMed] [Google Scholar]
- 29.Caca I, Cingu AK, Sahin A, Ari S, Dursun ME, Dag U, Balsak S, Alakus F, Yavuz A, Palanci Y. Amblyopia and refractive errors among school-aged children with low socioeconomic status in southeastern Turkey. J Pediatr Ophthalmol Strabismus. 2013;50(1):37–43. doi: 10.3928/01913913-20120804-02. [DOI] [PubMed] [Google Scholar]
- 30.Remon L, Benlloch J, Furlan WD. Corneal and refractive astigmatism in adults: a power vectors analysis. Optom Vis Sci. 2009;86(10):1182–1186. doi: 10.1097/OPX.0b013e3181baac2c. [DOI] [PubMed] [Google Scholar]