Abstract
The number of deaf children has dramatically increased in the past few decades. These children present to the pediatric dentist a unique set of challenges mostly pertaining to the establishment of communication with them. There have been very few attempts in the past to break down these challenges and formulate a strategy on how to manage them effectively. This is a case report of a child who was successfully managed using two different modes of communication. Finally, the advantages and disadvantages are mentioned, and a common strategy incorporating the positives of both the methods has been devised.
How to cite this article
Renahan N, Varma RB, Kumaran P, Xavier AM. Unique Approach to Dental Management of Children with Hearing Impairment. Int J Clin Pediatr Dent 2017;10(1):107-110.
Keywords: Behavior management, Communication, Deaf child, Sign language.
INTRODUCTION
When a deaf child walks into the dental clinic, the normal management protocol will not be appropriate. Literature does not provide specific management strategy for such children. A total of 63 million people in India have hearing impairment, which is a common cause of disability.1 There is no structured program to impart knowledge on how to manage such children.2 Sign language and treatment under general anesthesia are the routinely employed management methods. In the United Kingdom, there was an incidence of 1/1,000 births of deaf in the year 2000.3 Derelioglu and Yilmaz4 suggest that deaf children will have to be treated under general anesthesia as there is difficulty in communication. Nunn5 suggested the use of some basic actions for management. However, in most cases, we fall short of a definite plan of action for chairside behavior management of these children.
CASE REPORT
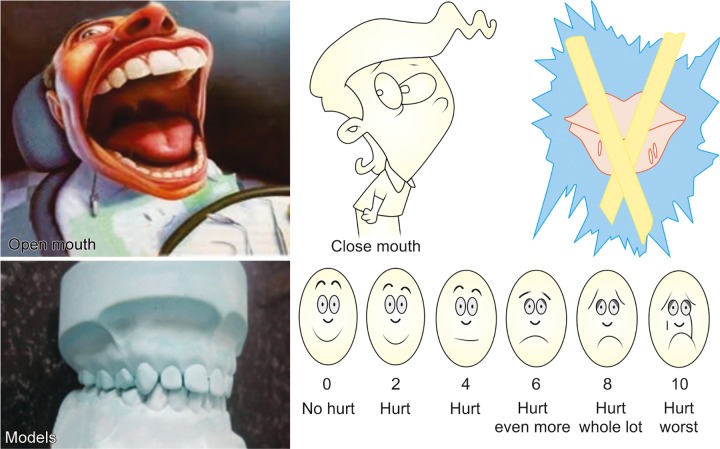
A 6-year-old child presented to the Pediatric Dental Clinic with caries lesions. The child was classified as having class III deafness according to the World Health Organization (WHO) classification.6 He was uncooperative and had a phobia toward medical practitioners, which could be attributed to prior bad experiences. Parents could not afford the child’s treatment under general anesthesia. So, chairside management was chosen, which presented a scenario encompassing all the challenges of treating a conscious special child. We devised two modes of management. The first mode was using sign language with actions (Fig. 1) and the second mode was using models, pictures, and rating scales (Fig. 2). Examination revealed arrested caries on all quadrants, so we addressed two quadrants at a time. The first method was used in the first appointment, and the second method was used in the second appointment (Fig. 3). Prior to this, an appointment was used to orient the child to both methods (Fig. 4). Restorations were successfully done (Fig. 5), and the advantages and disadvantages of both methods were unraveled. He has now developed a positive attitude toward dentistry (Fig. 6).
Fig. 1:
Sign language
Fig. 2:
Models, pictures, rating scale
Fig. 3:
Applying second mode of management
Fig. 4:

Orientation appointment
Fig. 5:
Pretreatment and posttreatment
Fig. 6:
Attitude change
DISCUSSION
Hearing impaired children are facing a similar situation of not being able to undergo treatment under general anesthesia due to socioeconomic conditions and treatment at chairside being denied due to lack of awareness of management methods. Parents from low socioeconomic group do not often enroll their children in special schools at an early age, thereby affecting their communication skills.7,8 The sign language method was comforting for the patient, but being a child he himself was in the learning stages of sign language. The pictures and models were swift to attract the child’s attention, but distracted the child from the treatment at times. In general, the child was highly uncooperative and had increased salivation. After the management of the child who developed a positive attitude and certain key features presented themselves in managing such a child, which can be abbreviated to “I STUMBLED” (Fig. 7), the pedodontist would henceforth be prevented from stumbling while managing a deaf child. A well-constructed protocol will serve in the successful management of deaf children and is an attempt in that noble direction, which may invoke many more attempts to fabricate a concrete protocol, which will ultimately benefit deaf children.
Fig. 7:
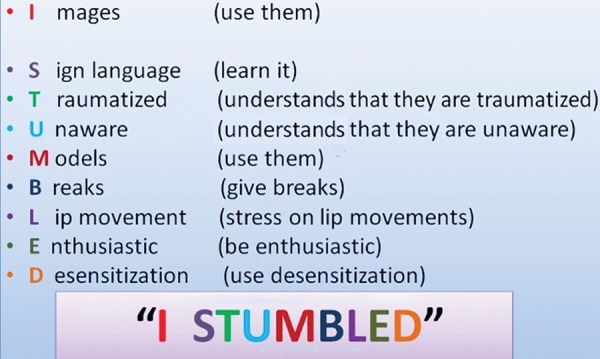
Novel strategy formulated
Footnotes
Source of support: Nil
Conflict of interest: None
REFERENCES
- 1.Naik SM, Naik MS. Rehabilitation of hearing impaired in India-an update. Online J Otolaryngol. 2013 Jan;3(1):20–31. [Google Scholar]
- 2.Kleinert HL, Sanders C. Improving student dentist competencies and perception of difficulty in delivering care to children with developmental disabilities using a virtual patient module. J Dent Educ. 2007 Feb;71(2):279–286. [PubMed] [Google Scholar]
- 3.Fortnum HM, Summerfield AQ. Prevalence of permanent childhood hearing impairment in the UK and implications for universal neonatal hearing screening: questionnaire based ascertainment study. BMJ. 2001 Sep;323(7312):536–540. doi: 10.1136/bmj.323.7312.536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Derelioglu SS, Yilmaz Y. Dental treatment under the general anesthesia in a child with keratitis, ichthyosis and deafness syndrome. Case Rep Dent. 2013;2013:618468. doi: 10.1155/2013/618468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nunn JH. Paediatric dentistry: are we dealing with hearing-impaired children correctly? Br Dent J. 2000 Aug;189:151. [Google Scholar]
- 6.Available from: www.who.int/healthinfo/statistics/bod_hearingloss.pdf. or Colin Mathers, Andrew Smith, Marisol Concha. Global burden of hearing loss in the year 2000;2000:1-27.
- 7.Moeller MP. Early intervention and language development in children who are deaf and hard on hearing. Pediatrics. 2000 Sep;106(3):1–9. doi: 10.1542/peds.106.3.e43. [DOI] [PubMed] [Google Scholar]
- 8.Watkin P, McCann D. Language ability in children with permanent hearing impairment: the influence of early management and family participation. Pediatrics. 2007 Sep;120(3):e694–e701. doi: 10.1542/peds.2006-2116. [DOI] [PubMed] [Google Scholar]