Abstract
INTRODUCTION
Prolonged stay in acute hospitals increases the risk of hospital-acquired infections in older patients, and disrupts patient flow and access to care due to bed shortages. We aimed to investigate the factors associated with prolonged length of stay (pLOS) among older patients (aged ≥ 78 years) in a tertiary hospital, to identify the potentially modifiable risk factors that could direct interventions to reduce length of stay (LOS).
METHODS
During a three-month period from January 2013 to March 2013, we identified 72 patients with pLOS (LOS ≥ 21 days) and compared their demographic and clinical variables with that of 281 randomly selected control patients (LOS < 21 days) using univariate and multivariate logistic regression analyses.
RESULTS
The mean age of the patients was 85.30 ± 5.34 years; 54% of them were female and 72% were of Chinese ethnicity. Logistic regression revealed the following significant factors for increased LOS: discharge to intermediate and long-term care services (odds ratio [OR] 9.22, 95% confidence interval [CI] 3.56–23.89; p < 0.001); increased severity of illness (OR 2.41, 95% CI 1.12–5.21; p = 0.025); and presence of caregiver stress (OR 3.85, 95% CI 1.67–8.91; p = 0.002).
CONCLUSION
Presence of caregiver stress and nursing home placement are potential modifiable risk factors of pLOS among older patients. Early identification and management of caregiver stress, as well as expediting discharge planning, may help to reduce the length of stay for this cohort.
Keywords: caregiver stress, elderly, prolonged length of stay
INTRODUCTION
An ageing population can increase the burden(1) on the healthcare system, including greater utilisation of hospital beds, prolonged length of stay (pLOS) and an attendant rise in healthcare cost.(2) Therefore, ageing societies have attempted to innovate using novel care models,(3) with the dual goals of providing optimal healthcare for the elderly and minimising the fiscal burden on the system.
In 2013, statistics showed that 10.5% of the Singapore population were over 65 years of age.(4) Meanwhile, other studies suggest that older patients constitute an increased proportion of hospital occupancies, accounting for 31.8% of male and 35.1% of female admissions,(5) and tend to stay longer.(6) Prolonged stay in acute hospitals increases the risk of hospital-acquired infections, and disrupts patient flow and access to care due to bed shortages. The hospital bed crunch problem raises concerns about patient safety and the adequacy of healthcare infrastructure. It is therefore timely and pertinent to evaluate the factors underlying prolonged hospitalisation among older patients to guide the design of interventions that can be trialled to ameliorate the problem.
Extant literature has revealed several putative factors associated with the prolonged stay and delayed discharge seen among older patients in hospitals.(7) Demographic factors such as age, ethnicity, gender and income have been explored. According to Falcone et al, older age was associated with prolonged hospitalisation.(8) Interestingly, a study by Ohwaki et al found that women living with only their husband were associated with pLOS.(9)
A recent study by Bo et al revealed associations between prolonged hospital stay and cognitive impairment, functional dependence and higher comorbidity burden.(10) Other studies have also evidenced that poorer functional status,(11) the presence of cognitive impairment and walking difficulties(12) are associated with pLOS. Fick et al further identified that patients with delirium superimposed on dementia had a higher likelihood of delayed discharge from hospitals.(13) Among patients with dementia, caregiver support and burden(14) are important predictors of pLOS, just as poor nutritional status(15) is an important predictor for older adults. Expectedly, clinical factors,(16) such as the principal admitting diagnosis and burden of comorbidities, have been shown to be important.
Postdischarge care is a crucial determinant of acute hospital length of stay (LOS). Studies have revealed the importance of discharge destination(17,18) (particularly to community hospitals and nursing homes) and adequacy of care by caregivers following discharge in determining the duration of the patient’s hospital stay. In particular, the availability of caregiver assistance and support,(19) presence of dementia(20) and admission to intermediate and long-term care (ILTC) services(21) have emerged as the most significant factors.
Despite the considerable number of studies published, there have hitherto been very few local studies exploring this issue. In 2006, a study by Lim et al found that social factors, such as the absence of a caregiver, the wait for bed availability in nursing homes and medical factors (including septicaemia and cardiovascular disorders), were associated with delayed hospital discharge.(22) However, this earlier study was primarily descriptive in nature and no comparisons were made with patient groups that did not have prolonged stay. Also, as the study was conducted nearly a decade ago, it is likely that different factors may currently be at play.
In view of the above, the present study sought to explore the possible factors associated with pLOS among older patients in an acute tertiary hospital setting in Singapore. It was hoped that interventions(23) targeting the factors identified, especially those that are potentially modifiable, could help to ameliorate the problem of pLOS in older patients.
METHODS
Over a three-month period from January 2013 to March 2013, the medical case records of patients who were aged ≥ 78 years and admitted to the Department of Geriatric Medicine at Khoo Teck Puat Hospital, Singapore, were extracted from the hospital’s electronic medical records database; this constituted the sampling frame. Patients who were in the intensive care unit and isolation ward for infection control were excluded. Patients who died during the hospital stay were likewise not included in the study. The records of all patients with pLOS were reviewed. A random sample (50%) of patients who did not meet the criteria for pLOS was also selected using computer-generated random selection, to constitute the non-pLOS group. The final sample comprised 72 pLOS patients and 281 non-pLOS patients. Ethics approval was granted by the National Healthcare Group Domain Specific Review Board.
pLOS was defined as LOS ≥ 21 days, which is consistent with the local Health Ministry’s operational definition,(24) wherein the status of patients who are ‘medically fit for discharge’ but still not discharged at LOS ≥ 21 days are monitored and reported. However, patients with LOS ≥ 21 days were included in our study regardless of fitness for discharge. Two clinicians who were not involved in the care of patients during their hospital stay extracted the relevant data from the patients’ case records. Information obtained included demographic characteristics (e.g. age, gender and ethnicity), primary diagnosis, comorbidities, severity of acute illness, functional status, discharge destination, patient’s living arrangement (i.e. alone or with caregiver/relative) and presence of caregiver stress, as evidenced in the clinical notes or social worker’s reports. Key terms to indicate caregiver stress, which were used to search the clinical notes, included: stress, strain, burden, fatigue and burnout.
Severity of acute illness during hospitalisation was measured using the Severity of Illness Rating Scale (SIRS),(25) and categorised as low, moderate or high. SIRS evaluates the severity of illness based on patient symptoms, vital signs and the need for intensive care unit or high dependency unit admission. Patients’ functional status during the admission was determined using the Modified Barthel Index (MBI),(26) an 11-item scale assessing basic activities of daily living (total score = 100 points), on which higher scores indicate better function and independence. For patients with more than one MBI assessment during the course of hospitalisation, the last MBI score before eventual discharge was used for analysis. The Charlson Comorbidity Index (CCI)(27) was used to evaluate comorbidities. It assigns relative weights to different comorbidities, according higher weights to diseases with higher burden; the sum of the weights indicates the overall comorbidity burden.
Patient characteristics were reported using descriptive analysis. Univariate analysis was first performed to study the differences between pLOS patients and non-pLOS patients. Chi-square test was used for categorical independent variables. For continuous independent variables, Student’s t-test was used as the parametric test and Mann-Whitney U test as the non-parametric test. Logistic regression analysis was carried out to assess the likelihood of the factors’ contribution to pLOS. To prevent over-fitting the regression model, only factors with a probability (p-value) < 0.05 on univariate analysis were used as independent factors for logistic regression. Factors were retained or removed from the model following a forward selection design, based on the likelihood ratio test and using p < 0.05 as the entry criterion. All statistical data was analysed using IBM SPSS Statistics version 22.0 (IBM Corp, Armonk, NY, USA).
RESULTS
Among the 353 patient records included in the study, 72 patients had pLOS. Total LOS for all the patients was 2–128 days. Slightly more than half (54%) of the patients were female and most (72%) were of Chinese ethnicity. The mean age of the patients was 85.30 ± 5.34 years; 88% of the patients were aged > 80 years. 39% were married, with the remaining (61%) patients being single, divorced or widowed. A small number (9%) of patients lived alone. Most (86%) patients resided in their own homes and 14% of patients lived in ILTC institutions.
Only 65% of the Abbreviated Mental Test (AMT) scores were recorded, and the mean score was 5.49 ± 2.85 (range 0–10). The remaining 35% of scores were not assessed, as these patients were either uncommunicative or unable to cooperate with testing. Dementia was found in 26% of the patients and the mean score of age-adjusted CCI was 6.32 ± 1.99. The most common admitting diagnoses were pneumonia and urinary tract infection. The mean MBI score of our patients was 46.60 ± 28.90. Discharge placements included the patient’s own home (75%), nursing home (18%) and community hospital (7%). A large proportion of pLOS patients were discharged to nursing homes (38%). Caregiver stress was present in 22% of patients and 11% required financial aid.
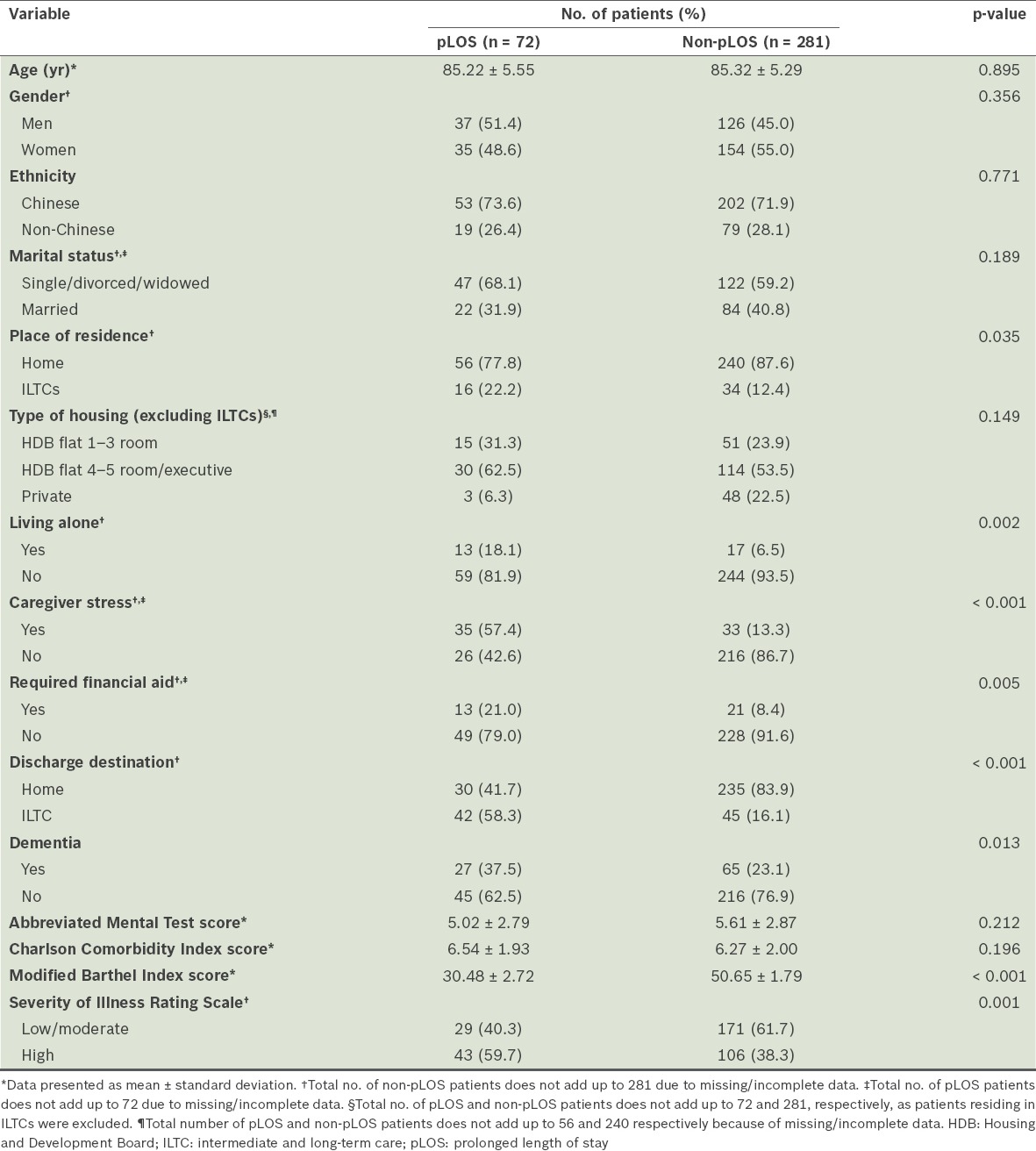
The results of univariate analysis of the sociodemographic and medical factors associated with pLOS are shown in Table I. A majority of the demographic variables, such as age, gender, ethnicity and type of housing, were not found to be significant. However, place of residence (p = 0.035) and discharge destination (p < 0.001), particularly discharge to community hospitals and nursing homes (collectively known as ILTC facilities), were significant factors. Caregiving and situational factors were also shown to have significant associations with pLOS, namely caregiver stress (p < 0.001), patient living alone (p = 0.002) and the need for financial aid (p = 0.005). Among the medical factors evaluated, CCI score was notably not associated with pLOS (p = 0.196). However, the diagnosis of dementia (p = 0.013), functional status based on MBI score (p < 0.001) and severity of acute illness as measured by SIRS (p = 0.001) were found to be significantly associated with pLOS.
Table I.
Univariate analysis of sociodemographic and medical factors associated with pLOS (n = 353).
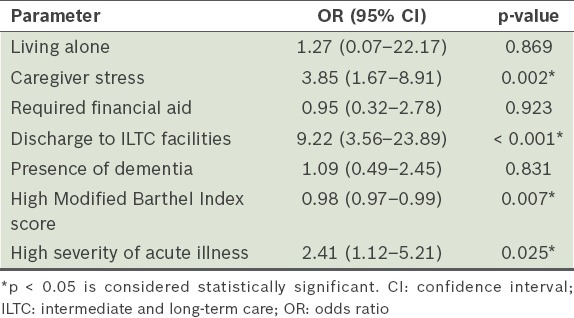
The results of multivariate logistic regression analysis are shown in Table II. The main sociodemographic predictors identified were presence of caregiver stress (odds ratio [OR] 3.85, 95% confidence interval [CI] 1.67–8.91; p = 0.002) and discharge to ILTC facilities (OR 9.22, 95% CI 3.56–23.89; p < 0.001). Two medical factors, severity of illness (OR 2.41, 95% CI 1.12–5.21; p = 0.025) and functional status (OR 0.98, 95% CI 0.97–0.99; p = 0.007), were associated with pLOS. Of note, discharge to ILTC facilities presented with the highest OR, followed by presence of caregiver stress.
Table II.
Results of multivariate logistic regression analysis.
DISCUSSION
In the present study, several factors were associated with pLOS on univariate analysis, including living alone, financial difficulties and a diagnosis of dementia. However, these factors did not remain statistically significant after adjustments for other covariates on multivariate logistic regression analysis. Dementia, for example, is known to be associated with poorer functional status, increased discharge disposition to nursing homes and increased caregiver stress.(28,29) Published studies have similarly highlighted the impact of dementia on lengthened LOS in hospitals.(30)
We surmise that dementia per se no longer emerged as significant because its contribution could have been mediated, through one or more of the independent predictors that surfaced subsequent to multivariate analysis. Patients with more severe acute illness and decreased functional ability, who were discharged to ILTC institutions and whose caregivers were under stress, were more likely to stay longer in acute hospitals. Intuitively, patients with dementia are more susceptible to impaired function and impose more strain on their caregivers, and are therefore more likely to be institutionalised. Similarly, living alone no longer emerged as significant after logistic regression, likely because it was not only being home alone, but also being functionally compromised and incapable of independent living, that had delayed hospital discharge in such patients. Therefore, it is necessary to step up efforts to improve the quality of care and community support available to elderly dementia patients and those who live on their own in spite of compromised independence.
Some factors associated with increased LOS may be potentially modifiable, but others can prove difficult to control. For instance, severity of acute illness is dependent on the nature of the acute illness, which directly affects the duration of treatment required and the overall duration of hospital stay. Nosocomial infections,(18) which are not uncommon in older patients, may complicate a patient’s hospital stay and further increase LOS.(31) Consistent with the extant literature, poorer functional status during hospitalisation was also associated with pLOS(32) in our study, although the effect was very modest. A patient’s functional well-being is closely associated with his premorbid condition as well as the impact of the acute illness. Given the reduced physiological reserves in frail older patients, functional recovery can be slow and, in some cases, limited. We should bear in mind that efforts to promote functional recovery among older patients may not necessarily produce an appreciable impact vis-à-vis LOS.
Published literature has shown that the wait for placement in ILTC institutions, such as nursing homes and community hospitals, can be associated with increased LOS.(6,33) Patient transfers to ILTC institutions may be delayed due to limited bed availability and administrative delays in the referral process. It is hoped that, as ILTC bed capacities increase in the foreseeable future,(34) the bed crunch situation in hospitals will be eased. Additionally, discharge delays due to delayed administration of referrals may be ameliorated by careful process analysis to identify bottlenecks, if any, in information flow, communication and coordination between staff.
Communication between hospital staff, patients and their families on discharge planning has been reported to be inadequate,(35) and some of this inadequacy is caused by the lack of engagement with patients and families during the discharge process. Therefore, early engagement with patients and families holds promise for facilitating smoother transfer between institutions. Nonetheless, given the realities of the tight bed situation in local nursing homes, increasing the availability and capability of home- and community-based interventions in home nursing and medical care, subsidies for employing foreign domestic workers and comprehensive centre-based care for seniors(36) are avenues that should be explored to alleviate the strain on nursing homes and, consequently, decrease overall hospital LOS.
Caregiver stress is a key, potentially modifiable factor identified in our study; this finding has been supported by other studies as well.(14,19) Caregiver stress and burden also increase the risk of institutionalisation, hospital readmission and patient abuse.(37) Stress in caregivers often arises from problems with coping with the patient’s physical care or behaviour, financial difficulties,(27) emotional strain and the negative impact of caregiving on the caregiver’s personal life.(38) If not addressed, caregiver strain can exert a negative impact on patients and may also lead to the development of psychiatric comorbidities among caregivers.(39)
Caregiver strain is usually present early during hospital admission and should hence be routinely screened for. It often arises from a mismatch between a patient’s needs and the caregiver’s ability to meet those needs, in addition to the caregiver’s own personal needs. Early intervention would allow social workers and counsellors to conduct in-depth assessments to better delineate the pain points and guide appropriate measures to address them. Specialised multidisciplinary teams(40) would help provide longitudinal support for family caregivers following discharge from hospitals. In addition, community-based care in the form of home-care and day-care centres can be very useful in supporting working adults who have to balance work commitments with caring for their parents. Caregiver-specific programmes, such as mindfulness training,(41) cognitive behavioural intervention(42) and caregiver support groups, can have significant benefits for reducing stress, improving mood(43) and enhancing quality of life for caregivers.
Our study has identified key factors associated with pLOS in hospitalised older patients; among these, at least two factors, i.e. caregiver stress and discharge to ILTC institutions, can potentially be addressed with appropriate interventions. However, this study was not without limitations. It was a review of case records of patients admitted over a three-month period, which may not necessarily be representative of all admissions. Moreover, as the study involved a retrospective case record analysis, the quality of data collected was largely dependent on the adequacy of documentation and thus susceptible to missing or incomplete information.
In conclusion, pLOS in hospitals for older patients is largely a result of multiple factors, and the main modifiable factors are the presence of caregiver stress and discharge to ILTC facilities. A pertinent follow-up initiative would be to address these factors through new service interventions and research initiatives.
REFERENCES
- 1.United Nations Department of Economic and Social Affairs, Population Division. World Population Ageing. 2013. [Accessed May 20, 2015]. Available at: http://www.un.org/en/development/desa/population/publications/pdf/ageing/WorldPopulationAgeing2013.pdf .
- 2.Hendy P, Patel JH, Kordbacheh T, Laskar N, Harbord M. In-depth analysis of delays to patient discharge: a metropolitan teaching hospital experience. Clin Med (Lond) 2012;12:320–3. doi: 10.7861/clinmedicine.12-4-320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Department of Health Government of the United Kingdom. National service framework: older people. [Accessed May 20, 2015]. Available at: www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4003066 .
- 4.Department of Statistics Singapore. Elderly, Youth and Gender Profile. [Accessed May 20, 2015]. Available at: http://www.singstat.gov.sg/statistics/browse-by-theme/elderly-youth-and-gender-profile .
- 5.Ministry of Health Singapore. Admissions and Outpatient Attendances. 2013. [Accessed May 20, 2015]. Available at: http://www.moh.gov.sg/content/moh_web/home/statistics/Health_Facts_Singapore/Admissions_and_Outpatient_Attendances.html .
- 6.Maguire PA, Taylor IC, Stout RW. Elderly patients in acute medical wards: factors predicting length of stay in hospital. Br Med J (Clin Res Ed) 1986;292:1251–3. doi: 10.1136/bmj.292.6530.1251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Victor CR, Healy J, Thomas A, Seargeant J. Older patients and delayed discharge from hospital. Health Soc Care Community. 2000;8:443–52. doi: 10.1046/j.1365-2524.2000.00270.x. [DOI] [PubMed] [Google Scholar]
- 8.Falcone D, Bolda E, Leak SC. Waiting for placement: an exploratory analysis of determinants of delayed discharges of elderly hospital patients. Health Serv Res. 1991;26:339–74. [PMC free article] [PubMed] [Google Scholar]
- 9.Ohwaki K, Hashimoto H, Sato M, Tokuda H, Yano E. Gender and family composition related to discharge destination and length of hospital stay after acute stroke. Tohoku J Exp Med. 2005;207:325–32. doi: 10.1620/tjem.207.325. [DOI] [PubMed] [Google Scholar]
- 10.Bo M, Fonte G, Pivaro F, et al. Prevalence of and factors associated with prolonged length of stay in older hospitalized medical patients. Geriatr Gerontol Int. 2016;16:314–21. doi: 10.1111/ggi.12471. [DOI] [PubMed] [Google Scholar]
- 11.Chin JJ, Sahadevan S, Tan CY, Ho SC, Choo PW. Critical role of functional decline in delayed discharge from an acute geriatric unit. Ann Acad Med Singapore. 2001;30:593–9. [PubMed] [Google Scholar]
- 12.Lang PO, Heitz D, Hédelin G, et al. Early markers of prolonged hospital stays in older people: a prospective, multicenter study of 908 inpatients in French acute hospitals. J Am Geriatr Soc. 2006;54:1031–9. doi: 10.1111/j.1532-5415.2006.00767.x. [DOI] [PubMed] [Google Scholar]
- 13.Fick DM, Steis MR, Waller JL, Inouye SK. Delirium superimposed on dementia is associated with prolonged length of stay and poor outcomes in hospitalized older adults. J Hosp Med. 2013;8:500–5. doi: 10.1002/jhm.2077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lang PO, Zekry D, Michel JP, et al. Early markers of prolonged hospital stay in demented inpatients: a multicentre and prospective study. J Nutr Health Aging. 2010;14:141–7. doi: 10.1007/s12603-009-0182-y. [DOI] [PubMed] [Google Scholar]
- 15.Chima CS, Barco K, Dewitt ML, et al. Relationship of nutritional status to length of stay, hospital costs, and discharge status of patients hospitalized in the medicine service. J Am Diet Assoc. 1997;97:975–8. doi: 10.1016/S0002-8223(97)00235-6. [DOI] [PubMed] [Google Scholar]
- 16.Lenzi J, Mongardi M, Rucci P, et al. Sociodemographic, clinical and organisational factors associated with delayed hospital discharges: a cross-sectional study. BMC Health Serv Res. 2014;14:128. doi: 10.1186/1472-6963-14-128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Elwood D, Rashbaum I, Bonder J, et al. Length of stay in rehabilitation is associated with admission neurologic deficit and discharge destination. PM R. 2009;1:147–51. doi: 10.1016/j.pmrj.2008.10.010. [DOI] [PubMed] [Google Scholar]
- 18.Jasinarachchi KH, Ibrahim IR, Keegan BC, et al. Delayed transfer of care from NHS secondary care to primary care in England: its determinants, effect on hospital bed days, prevalence of acute medical conditions and deaths during delay, in older adults aged 65 years and over. BMC Geriatr. 2009;9:4. doi: 10.1186/1471-2318-9-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tan WS, Chong WF, Chua KS, Heng BH, Chan KF. Factors associated with delayed discharges after inpatient stroke rehabilitation in Singapore. Ann Acad Med Singapore. 2009;39:435–41. [PubMed] [Google Scholar]
- 20.Challis D, Hughes J, Xie C, Jolley D. An examination of factors influencing delayed discharge of older people from hospital. Int J Geriatr Psychiatry. 2014;29:160–8. doi: 10.1002/gps.3983. [DOI] [PubMed] [Google Scholar]
- 21.Majeed MU, Williams DT, Pollock R, et al. Delay in discharge and its impact on unnecessary hospital bed occupancy. BMC Health Serv Res. 2012;12:410. doi: 10.1186/1472-6963-12-410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lim SC, Doshi V, Castasus B, Lim JK, Mamun K. Factors causing delay in discharge of elderly patients in an acute care hospital. Ann Acad Med Singapore. 2006;35:27–32. [PubMed] [Google Scholar]
- 23.Ministry of Health Singapore. MOH 2012 Committee of Supply Speech Healthcare 2020: Improving Accessibility, Quality and Affordability for Tomorrow’s Challenges (Part 1 of 2) [Accessed May 20, 2015]. Available at: http://www.moh.gov.sg/content/moh_web/home/pressRoom/speeches_d/2012/moh_2012_committeeofsupplyspeechhealthcare2020improvingaccessibi.html .
- 24.Lateef F. Long Stayers in restructured hospitals. In: Ministry of Health, Singapore. [Accessed May 20, 2015]. Available at: https://www.moh.gov.sg/content/moh_web/home/pressRoom/Parliamentary_QA/2013/long-stayers-in-restructured-hospitals-.html .
- 25.Horn SD, Horn RA. Reliability and validity of the Severity of Illness Index. Med Care. 1986;24:159–78. doi: 10.1097/00005650-198602000-00007. [DOI] [PubMed] [Google Scholar]
- 26.Mahoney FI, Barthel DW. Functional evaluation: the Barthel Index. Md State Med J. 1965;14:61–5. [PubMed] [Google Scholar]
- 27.Charlson M, Szatrowski T, Peterson J, Gold J. Validation of a combined comorbidity index. J Clin Epidemiol. 1994;47:1245–51. doi: 10.1016/0895-4356(94)90129-5. [DOI] [PubMed] [Google Scholar]
- 28.Zekry D, Herrmann FR, Grandjean R, et al. Does dementia predict adverse hospitalization outcomes? A prospective study in aged inpatients. Int J Geriatr Psychiatry. 2009;24:283–91. doi: 10.1002/gps.2104. [DOI] [PubMed] [Google Scholar]
- 29.Covinsky KE, Pierluissi E, Johnston CB. Hospitalization-associated disability: “She was probably able to ambulate, but I’m not sure”. JAMA. 2011;306:1782–93. doi: 10.1001/jama.2011.1556. [DOI] [PubMed] [Google Scholar]
- 30.King B, Jones C, Brand C. Relationship between dementia and length of stay of general medical patients admitted to acute care. Australas J Ageing. 2006;25:20–3. [Google Scholar]
- 31.Puisieux F, Defrennes R, Salomez-Granier F, Dewailly P. [Consequences of nosocomial infections in a geriatric short-stay department] Presse Med. 1997;26:1708–13. French. [PubMed] [Google Scholar]
- 32.Saxena SK, Koh GC, Ng TP, Fong NP, Yong D. Determinants of length of stay during post-stroke rehabilitation in community hospitals. Singapore Med J. 2007;48:400–7. [PubMed] [Google Scholar]
- 33.Ou L, Young L, Chen J, et al. Discharge delay in acute care: reasons and determinants of delay in general ward patients. Aust Health Rev. 2009;33:513–21. doi: 10.1071/ah090513. [DOI] [PubMed] [Google Scholar]
- 34.Ministry of Health Singapore. More facilities to help seniors age-in-place. [Accessed May 20, 2015]. Available at: https://www.moh.gov.sg/content/moh_web/home/pressRoom/pressRoomItemRelease/2012/more-facilities-to-help-seniors-age-in-place.html .
- 35.Bull MJ, Roberts J. Components of a proper hospital discharge for elders. J Adv Nurs. 2001;35:571–81. doi: 10.1046/j.1365-2648.2001.01873.x. [DOI] [PubMed] [Google Scholar]
- 36.Nikolaus T, Specht-Leible N, Bach M, Oster P, Schlierf G. A randomized trial of comprehensive geriatric assessment and home intervention in the care of hospitalized patients. Age Ageing. 1999;28:543–50. doi: 10.1093/ageing/28.6.543. [DOI] [PubMed] [Google Scholar]
- 37.Yan E, Kwok T. Abuse of older Chinese with dementia by family caregivers: an inquiry into the role of caregiver burden. Int J Geriatr Psychiatry. 2011;26:527–35. doi: 10.1002/gps.2561. [DOI] [PubMed] [Google Scholar]
- 38.Fianco A, Sartori RD, Negri L, et al. The relationship between burden and well-being among caregivers of Italian people diagnosed with severe neuromotor and cognitive disorders. Res Dev Disabil. 2015;39:43–54. doi: 10.1016/j.ridd.2015.01.006. [DOI] [PubMed] [Google Scholar]
- 39.Russo J, Vitaliano PP, Brewer DD, Katon W, Becker J. Psychiatric disorders in spouse caregivers of care recipients with Alzheimer’s disease and matched controls: a diathesis-stress model of psychopathology. J Abnorm Psychol. 1995;104:197–204. doi: 10.1037//0021-843x.104.1.197. [DOI] [PubMed] [Google Scholar]
- 40.Bakker TJ, Duivenvoorden HJ, van der Lee J, et al. Benefit of an integrative psychotherapeutic nursing home program to reduce multiple psychiatric symptoms of psychogeriatric patients and caregiver burden after six months of follow-up: a re-analysis of a randomized controlled trial. Int Psychogeriatr. 2012;25:34–46. doi: 10.1017/S1041610212001305. [DOI] [PubMed] [Google Scholar]
- 41.Paller KA, Creery JD, Florczak SM, et al. Benefits of mindfulness training for patients with progressive cognitive decline and their caregivers. Am J Alzheimers Dis Other Demen. 2015;30:257–67. doi: 10.1177/1533317514545377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fialho PP, Köenig AM, Santos MD, Barbosa MT, Caramelli P. Positive effects of a cognitive-behavioral intervention program for family caregivers of demented elderly. Arq Neuropsiquiatr. 2012;70:786–92. doi: 10.1590/s0004-282x2012001000007. [DOI] [PubMed] [Google Scholar]
- 43.Burgio LD, Collins IB, Schmid B, et al. Translating the REACH caregiver intervention for use by area agency on aging personnel: the REACH OUT program. Gerontologist. 2009;49:103–16. doi: 10.1093/geront/gnp012. [DOI] [PMC free article] [PubMed] [Google Scholar]


