Abstract
To successfully infect host cells and evade the host immune response, a type III secretion system (T3SS) is commonly used by enteric bacterial pathogens such as enteropathogenic Escherichia coli (EPEC). Recent findings have revealed that various effectors are injected into host cells through the T3SS and exert an inhibitory effect on inflammatory signaling pathways, subverting the immune responses to these pathogens. Here we review recent studies aimed at addressing the modulation of several important inflammatory signaling pathways modulated by EPEC effector proteins, such as the nuclear factor-κB (NF-κB) and mitogen-activated protein kinase (MAPK) pathways, which provides insight into the unfinished work in this unexplored field and helps to identify novel positions in inflammatory signaling networks for EPEC effectors.
Introduction
Anti-infection immunity is one of the most important roles of the immune system and contains a series of physiological defense mechanisms, including immune recognition, the immune response and immune elimination by the host immune system.1 Like all other higher organisms, humans have evolved a relatively perfect immune system, consisting of both innate immunity and adaptive immunity to fight against various microbes under diverse circumstances.2, 3 Four hours after infection, microbes can be cleared by mechanical barriers, phagocytosis by macrophages, killing by NK cells and degradation by small humoral molecules, among other mechanisms. From 4 to 96 h, innate immune cells are further activated through the recognition of pathogen-associated molecular patterns (PAMPs) by pattern recognition receptors (PRRs) and secrete effect molecules and proinflammatory cytokines, such as interferon-α/β (IFN-α/β), tumor necrosis factor-α (TNF-α), interleukin-6 (IL-6) and IL-12, to enhance the nonspecific killing activity of NK and γ/δT cells. Simultaneously, innate immune cells present pathogen-nonspecific antigens to T and B cells to induce adaptive immunity. Adaptive immunity mainly includes killing by T cells and antibody effects induced by B cells.
Humans have evolved sophisticated defense mechanisms; however, many pathogens can still evade the host immune responses and infect the host successfully, even remaining latent in the host for several decades. This is due to complex and efficient anti-immune strategies utilized by successful microbial pathogens to overcome innate and adaptive immune mechanisms, which can result in disease or chronic infection. Pathogens evade anti-infection immunity mainly through: (1) infecting the immune cells directly or remaining latent in places where the immune cells cannot reach them, (2) changes in structure to subvert host recognition of the pathogen and (3) inhibiting and interfering with host signal transduction via structural or non-structural mechanisms.
There are many reported examples of bacterial pathogens altering downstream signaling pathways and affecting the production of inflammatory cytokines; however, most of the exact underlying molecular mechanisms have not been fully elucidated.4 Because of the complexity of bacteria and the diverse array of effectors and other immune modulators produced by these organisms, it has been difficult to identify which components take roles.
The functions of bacterial components, whether triggering cytokines or selectively inhibiting cytokine production, are difficult to identify. However, there are now examples of pathogens that specifically target cytokine pathways to evade the immune response.5 For example, Shigella flexneri, a pathogen causing severe diarrhea, harbors a type III effector, OspG, that can prevent the NF-κB activation and cytokine production induced by TNF-α stimulation.6
The human pathogen EPEC has long been known as an important diarrheagenic agent in children, mainly in the first year of life in developing countries, and could lead to tens of thousands of deaths every year. EPEC colonizes the gut epithelium, causing attaching and effacing (A/E) lesions, characterized by the localized effacement of the intestinal brush border microvilli, reorganization of the host cytoskeletal proteins beneath the intimately attached bacteria and reorganization of the tight junctions, which is the central EPEC pathogenicity mechanism that can be detected both in vitro and in vivo. Moreover, A/E formation is utilized as an infection mechanism not only by EPEC, but enterohemorrhagic E. coli (EHEC) and Citrobacter rodentium, all of which harbor a conserved core genomic structure.7 Citrobacter rodentium can only infect mice but not humans and domestic animals; however, its pathogenicity is similar to EPEC targeting in humans, which makes the study of A/E lesion-forming pathogens, including EPEC, in vivo possible.
Bacteria use the secretion system to sense their environment within the host. The locus of enterocyte effacement (LEE) island is responsible for A/E lesion formation. The LEE island encodes a T3SS, the outer membrane adhesin intimin and its translocated receptor (Tir), and various effector proteins.8 T3SS has an essential role in immune subversion by pathogens. Various proteins translocate from EPEC to the eukaryotic cell cytoplasm through T3SS targeting of different cellular signaling pathways and modulate immune signals to help subvert the host responses.9 The functions of the effectors from EPEC are widely variable,10 and thus a relatively comprehensive description of the functions involved in the inflammatory response is given in the form of a table (Table 1). However, EPEC strains differ from each other in the aspect of island location and effector expression within a certain island location; the EPEC strain 2348/69 is taken as an example. Among various signaling events, the NF-κB and MAPK pathways are two main pro-inflammatory signaling pathways downstream of PRR activation.
Table 1. Summary of EPEC 2348/69 effectors engaged in modulating inflammatory signaling pathways.
| Effector | Island location | Subcellular target sites | Targeted host proteins | Functions |
|---|---|---|---|---|
| NleA | PP6 | Golgi | NLRP3 | Interrupts de-ubiquitination and activation of NLRP3; depresses the maturation and secretion of IL-1 |
| NleD | PP4 | Unknown | JNK, p38, p65 | Cleaves JNK, p38 as a metalloprotease, has a secondary role in IL-8 production; cleaves and inactivates the p65 subunit of NF-κB |
| Tir | LEE | Beneath the plasma membrane orcytoplasm | SHP-1, SHP-2 SHIP2, PI3K | Targets TRAF2 for proteasome degradation; inhibits TRAF6-mediated NF-κB activation in an ITIM-dependent manner |
| NleB1 | IE6 | Cytoplasm | GADPH, DD | Suppresses TRAF2 polyubiquitination by glycosylating GADPH; glycosylates FADD and TRADD death domains |
| NleE | IE2/6 | Nucleus | TAB2, TAB3 | Stabilizes IκB by methylating TAB2/3 and subsequently inhibiting TAK activation |
| NleC | PP4 | Cytoplasm and nucleus | P65, p50, c-Rel and p300 | Directly cleaves the NF-κB subunits as a metalloprotease; minimizes the enhancing activity of p300 and RPS3; dampens p38 MAPK phosphorylation |
| NleH1 | PP2 | Cytoplasm | RPS3 and v-Crk sarcoma virus CT10 oncogene-like protein (NleH1) | Prevents the nuclear translocation of RPS3 and dampens RPS3-dependent NF-κB expression |
| NleH2 | PP6 | Cytoplasm | RPS3 | Counterbalances the effect of NleH1; regulates MAPK activity by enhancing AP-1-dependent transcription |
Here we review evidence indicating different functions and mechanisms for EPEC proteins in host cell signaling subversion during infection. We discuss the current understanding of the mechanisms underlying these different effects on different signaling pathways, including NF-κB and MAPK. In this context, we outline gaps between the current understanding and future research and discuss the implications of these findings for therapeutic strategies targeting EPEC infection.
The NF-κB inflammatory signaling pathway and its modulation by EPEC effector proteins
When innate immune cells detect foreign antigens via TLRs or cytokines via tumor necrosis factor receptor (TNFR) and interleukin receptor, a cascade of phosphorylation and ubiquitination is triggered in these cells. As the initiator of MAPK pathways, the activation of the IκB kinase (IKK) complex (with a regulatory subunit, named NEMO/IKKγ) takes place at the receptor much faster. The adaptor protein kinase receptor-interacting protein 1 (RIP1) or TNF receptor-associated factor2/6 (TRAF2/6) facilitate the recruitment of IKKγ and complex formation.11 TRAF6 can also catalyze lysine (K) 63 polyubiquitination of the TGFβ-activated kinase 1(TAK1) complex. TAK1-binding proteins 1, 2 and 3 (TAB1/TAB2/TAB3), which strongly interact with K63-linked polyubiquitin chains, form a heterotrimeric complex with TAK1. Afterwards, TAK1 is modified by ubiquitination and autophosphorylation for full activation12 and then further phosphorylates and activates the primed IKK complex.13 After that, Lys48-linked ubiquitin (Ub) chains are attached to the phosphorylated inhibitor of kB (IκB) for proteasome-dependent degradation, thereby releasing NF-κB for translocation into the nucleus, targeting immune response genes for transcription.14
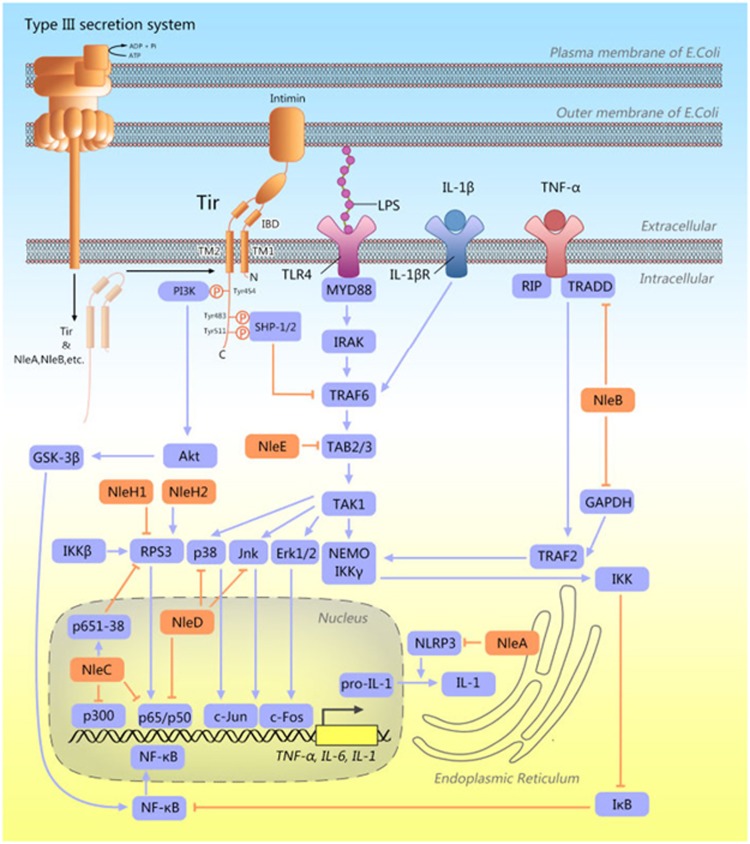
To date, the NF-κB signaling pathway was demonstrated to be regulated by EPEC proteins at different levels of signaling checkpoints, including kinases, phosphatases, ubiquitin ligases, de-ubiquitinases and adaptor proteins. It seems that modulation of the NF-κB signaling pathway is the key to subvert the host responses, especially the immune response by EPEC effectors (Figure 1).
Figure 1.
Diagram summarizing the effects of effector proteins on inflammatory signaling pathways in host cells. The nuclear factor-κB (NF-κB) and mitogen-activated protein kinase (MAPK) pathways are two main pro-inflammatory signaling pathways targeted and modulated by effector proteins translocated from EPEC into the host cells via the T3SS for immune subversion. Tir spans the host cell membrane with two predicted transmembrane (TM) domains. The central extracellular intimin-binding domain (IBD) is essential for binding to intimin. The phosphorylation of Tyr483/Tyr511 and Tyr 454 recruits SHP1/2 and PI3K, respectively. NleE stabilizes IκB by inactivating TAB2 and TAB3. NleC cleaves the NF-κB subunits and minimizes the activity of p300 and RPS3. NleH1/NleH2 control the activity of RPS3, which confers regulatory specificity on NF-κB-mediated gene expression. NleA blocks NLRP3 inflammasome activation downstream of the NF-κB pathway. NleD directly cleaves p38 and JNK, which are involved in the MAPK signaling pathway. These two pathways are not separated but are linked by certain intermediate proteins, such as TAK1, which means that a more extensive modulatory effect on inflammation may be present. See the text for explanation.
Inhibiting TRAF ubiquitination and activation
Tir is translocated into host cells and mediates the intimate attachment of bacteria to host cells by combining with intimin on the EPEC surface (Figure 1).15 Regarding the effect of Tir on the host immune response, TNF-α-induced NF-κB activation can be inhibited when TRAF2 is targeted for degradation independent of the proteasome upon interacting with Tir.16
The recruitment of Src-homology 2 (SH2) domain-containing phosphatases to immunoreceptor tyrosine-based inhibition motifs (ITIMs) is essential for the restriction of eukaryotic signaling pathways. The C-terminal regions in Tir, encompassing Tyr483 and Tyr511, share sequence similarity with cellular ITIMs.17 Tir has been demonstrated to interact with the host cellular SH2 domain-containing tyrosine phosphatase 1/2 (SHP-1, SHP-2) in an ITIM-dependent manner, requiring the phosphorylation of Tyr483 or Tyr511 of Tir. Interaction between Tir and SHP-1/2 contributed to the recruitment of SHP-1/2 to the adaptor TRAF6 and inhibited the ubiquitination of TRAF6. The ITIMs of Tir suppressed the EPEC-stimulated expression of proinflammatory cytokines and inhibited intestinal immunity to infection with Citrobacter rodentium.18, 19 However, the mechanism whereby Tir facilitates the interaction between SHPs and TRAF6 has not been elucidated. We speculated that a conformal change in SHPs upon interacting with Tir primed SHPs for the subsequent binding to TRAF6.19 The β-arrestin-TRAF6 complex prevents the autoubiquitination of TRAF6 and negatively regulates Toll-like receptor-interleukin 1 receptor signaling, including the activation of NF-κB and the activator protein 1 (AP-1).20 Meanwhile, the interaction of β-arrestin 2 with ITIMs within inhibitory receptors of NK cells mediates the recruitment of the tyrosine phosphatases SHP-1 and SHP-2.21 Recently, we also observed that β-arrestin 2 interacts with Tir and promotes the binding or Tir to SHP-1/2 (unpublished data).
TRAF2 polyubiquitination can also be suppressed by another EPEC effector, NleB, along with the participation of glyceraldehyde 3-phosphate dehydrogenase (GAPDH). GAPDH acts as a mediator of the TRAF2-dependent pro-inflammatory signaling cascade downstream of TNFR. NleB functions as a translocated N-acetyl-D-glucosamine (O-GlcNAc) transferase that modifies GAPDH. The glycosylation of GAPDH impedes binding to and activation of TRAF2, which impairs NF-κB activation.22 However, specific glycosylation of the death domains (DDs) of the protein was also reported.22, 23 Thus, it is doubted whether the NleB-mediated suppression of NF-κB is due to the modulation of DDs because it may recognize the binding site of the TNFR domain and recruit downstream adaptor proteins for NF-κB activation.14 Therefore, the glycosylation target responsible for the inhibitory signaling of the NF-κB pathway requires further investigation. Although NleB only suppresses NF-κB activation in response to TNF-α stimulation in a moderate manner, without AP-1 activation,24 the possibility that it can inhibit other unknown inflammatory signaling pathways cannot be ruled out and needs further elucidation.
Stabilizing IκB by inactivating TAB2 and TAB3
NleE prevents the proteasome-dependent degradation of IκB, the cytosolic inhibitor of p65. Stabilization of IκB in infected host cells blocks the nuclear translocation of p65 and c-Rel. In this manner, the TNF-α- and IL-1β-induced activation of NF-κB, including the expression of the pro-inflammatory cytokine IL-8, is inhibited.25 A six-amino-acid motif within the C-terminus of NleE, namely IDSY(M/I)K, was crucial for the inhibition of NF-κB activity.24 Recent studies show that TAB2 and TAB3, two ubiquitin-chain sensory proteins involved in NF-κB signaling, are directly inactivated by NleE, which harbors unprecedented S-adenosyl-l-methionine-dependent methyltransferase activity. In detail, the specific cysteine methylation results in the loss of the ubiquitin-chain binding activity of TAB2/3, which is required to activate TAK1.26 NleE-dependent methylation is suggested to account for the subsequent stabilization of IκB and reduction in inflammatory cytokine production.
The inhibitory effect of NleE on NF-κB signaling also extends to dendritic cells. The secretion of large amounts of IL-8, TNF-α, and IL-6 elicited in dendritic cells in response to PAMP recognition was dampened by NleE complementation in EPEC strains with pathogenicity island 4 deletions.27 In addition, the compromised costimulatory molecule expression may inhibit the activation of innate immunity.
Targeting NF-κB components
NleC acts as a zinc protease that compromises NF-κB activation by directly cleaving the NF-κB subunit p65. The decreased amount of p65 results in a decrease in the total nuclear entry of active p65.28 Other NF-κB components, c-Rel and p50, are also degraded in infected cells.29 As a result, NleC-mediated proteolysis suppresses NF-κB activation and subsequently impairs the secretion of IL-1β, IL-8 and TNF-α.28, 29, 30
The NF-κB component p65, recruited by NleC, is targeted for proteasomal-independent degradation, presumably via a consensus zinc metalloprotease motif. Early studies suggested that the site of p65 cleavage by NleC lies within its N-terminal Rel homology domain (RHD), which is involved in DNA binding by p65 on adjacent, parallel strands.28, 30 It has been further shown that two motifs, E22IIE25 and P177VLS180, within the RHD of p65 are needed for the recognition and binding of NleC.31
In spite of cleavage of a small percentage of p65, modulation of NF-κB-mediated gene expression is greatly amplified by a mechanism by which an NleC cleavage-generated p651–38 fragment interacts with p65 and ribosomal protein S3 (RPS3), which facilitates p65 binding to promoters and gene expression.32 Notably, the repression of IL-8 secretion is facilitated by a decrease in the acetyltransferase p300 in the nuclei, which enhances the activity of p65 and serves as a novel target for NleC.33 Overall, NleC blocks the secretion of inflammatory cytokines and inflammatory signaling by directly cleaving the NF-κB subunits, minimizing the activity of p300 and RPS3.
RPS3 is a non-Rel homology subunit of NF-κB complexes that regulates the selective transcription of NF-κB target genes. The regulatory specificity relies heavily on RPS3, especially in immediate cellular activation responses.34 However, RPS3 is also under the control of NleH1 and NleH2.35 It has been reported that phosphorylation of RPS3 Ser209 by the kinase IKKβ was crucial for the nuclear localization of RPS3. RPS3 fails to translocate into the nucleus if NleH1 dampens the activation of NF-κB signaling by blocking the phosphorylation of RPS3.36 NleH1/2 bind to the N terminus of RPS3 independent of their kinase activity, although they can act as autophosphorylated Ser/Thr protein kinases.35 Furthermore, the v-Crk sarcoma virus CT10 oncogene-like protein, an IKKβ interacting protein, was found to recruit NleH1 to IKKβ–RPS3 complexes for inhibition when phosphorylated by NleH1 independent of altering the kinetics of IκBα phosphorylation and degradation.37, 38 With regard to NleH2, the extent and duration of NF-κB activation after its T3SS-dependent translocation is suggested to be regulated by the relative proportion of heterodimers formed by NleH1/2, which downregulates the activity of NleH1.38 In other words, the NF-κB activity compromised by NleH1 is counterbalanced by NleH2. NleH1/2 from Escherichia coli O157:H7 may be expressed differentially due to their divergent promoter regions upstream of the genes encoding the effectors.39 This indicates that the total effect of effector proteins on the inflammatory response partly relies on the gene expression and regulation of host cells.
Altering the metabolism of phosphoinositide
Phosphatidylinositol 4,5-bisphosphate [PI(4,5)P2] and phosphatidylinositol 3,4,5-trisphosphate [PI(3,4,5)P3] are phosphoinositides (PIs) attached to the inner leaflet of the cells' plasma membrane lipid bilayer and are only present in small amounts. As mentioned above, Tir contains ITIMs, and Tyr483 and Tyr511 in the ITIM of Tir have been found to direct the actin reorganization of EPEC-induced actin pedestals with the help of recruited SH2 domain-containing inositol 5'-phosphatase (SHIP2).40 However, compared with the recruitment of SHP, the binding of SHIP2 is phosphorylation-independent because the elimination of all tyrosine residues due to substitution of Tyr 474 had no effect.41 In EPEC-adhered epithelial cells, actin-rich pedestal formation beneath the bacteria is usually triggered. SHIP2 recruited by Tir contributes to morphological changes by engaging the scaffolding protein SHC and the PI(3,4)P2-enriched lipid platform for the recruitment of the cytoskeletal regulator lamellipodin.
In contrast, a shift from PI(4,5)P2 to PI(3,4,5)P3 is initiated by EPEC Tir at the bacterial attachment site. The recruitment of phosphoinositide 3-kinase (PI3K) via Tir phosphorylation of Y454 is responsible for the phosphoinositide shift.42 Moreover, binding has been shown to be mediated by the SH2 domain of the PI3K regulatory p85 subunit, while the activation of PI3K requires the activation of receptor tyrosine kinases after EPEC infection.43, 44 However, PI3K inhibition was not correlated with actin rearrangement toward the sites of attachment, indicating the minor role of PIK3 in pedestal formation.42, 45
PI3K is a negative regulator of TLR signaling. The resulting activation of protein kinase B (PKB or Akt) and phosphorylation of glycogen synthase kinase (GSK)-3β indicates an inactive state. Along with regulating a series of transcription factors, activation of PI3K leads to depressed NF-κB activation and proinflammatory cytokine production.46 However, the mutant regulatory subunit, serving as a potential inhibitor of PI3K, downregulates NF-κB-dependent gene expression. In contrast, NF-κB activation is not regulated by PI3K alone but is accompanied by other TNF-α-inducible signals.44 PI3-kinase may have different targets and modulatory effects along the signaling cascade downstream of different receptors, such as TLR or TNFR, which are related to the subsequent NF-κB activation. TNF-α treatment induces the phosphorylation of Akt on serine 473. Data from cells uninfected or infected with the espA EPEC mutant (effector delivery-defective) demonstrated that EPEC inhibits PI3K pathways in differentiated Caco-2 cells. Cells infected with an eae mutant (intimin-defective) were unable to induce Akt phosphorylation after TNF-α treatment. Therefore, the compromised NF-κB activation may partly result from the suppression of PI3K activity; however, the exact effector proteins involved in the control of PI metabolism remain unidentified.47 Moreover, contradictory observations regarding the ability of EPEC to modulate PI3K activity42, 43, 47 may be due to variations in the responsiveness of different cell types infected by EPEC.
Blocking NLRP3 inflammasome activation downstream of the NF-κB pathway
Aside from blocking cytokine production through the NF-κB pathway, whether the inflammatory reaction can be fully elicited also depends on posttranslational modification, which has been demonstrated as a new target for EPEC immune subversion.48
The Nod-like receptor (NLR) inflammasome complex is a multimeric protein complex composed of NLR, the adapter apoptosis-associated speck-like protein containing a C-terminal caspase recruitment domain (ASC) and caspase-1. The inflammasome complex, and the cleaving activity of activated caspase-1 in particular, is responsible for the maturation and secretion of the proinflammatory cytokines IL-1β and IL-18.49 The NLRP3 inflammasome, which is the most characterized, it is thought to be regulated by two major signals. The first signal for priming is initiated by the Toll-like receptor (TLR)/ NF-κB pathway after the cells are exposed to a myriad of stimuli, including infection. The second signal relies on PAMPs and damage-associated molecular patterns and facilitates the assembly and activation of the functional NLRP3 inflammasome.50 Notably, post-translational modification, in particular the ubiquitination of the NLRP3 receptor, has a critical role in protein stability and inflammasome stability as well as activation.51
NleA was long thought to inhibit vesicle trafficking along the host cell secretory pathway by interacting with coatomer protein II (COPII) complex.52 Nevertheless, NleA has been demonstrated to subdue host IL-1β secretion not by inhibiting NF-κB activity but by suppressing NLRP3/caspase-1 activation. Further investigation showed that NleA interacted with NLRP3 and interrupted the de-ubiquitination of NLRP3, which is necessary for inflammasome activation. As NLRP3 inflammasome activation may result from ER stress mediated by thioredoxin-interacting protein53 and NleA blocks the ER secretory pathway, whether NLRP3 activation is inhibited by the failure of ER stress induction remains unclear.
MAPK inflammatory signaling pathways
TLR4 is a good example of a MAPK inflammatory signaling pathway. The initiation of TLR4 signaling requires the recruitment of adaptor proteins, such as MyD88 and toll-interleukin-1 receptor (TIR) domain-containing adaptor inducing interferon-beta, to the cytoplasmic portions of the receptors.54, 55 In a MyD88-dependent manner, cellular inhibitors of apoptosis (cIAPs) 1 and 2 are Ub ligases (E3s) that mediate canonical Lys48-linked ubiquitination and the subsequent degradation of TNFR-associated factor 3 (TRAF3). Thereafter, TRAF2/6:MAP3K signaling complexes responsible for MAPK activation escape the inhibition of TRAF3 and translocate from the cytoplasmic site of the receptor to the cytoplasm, where they activate MAPK phosphorylation.14 c-Jun N-terminal kinases (JNKs), extracellular signal-regulated kinases (ERK) and p38, members of the MAPK family, are phosphorylated within the region termed the activation loop when activated by several MAP3Ks after various stimuli. Afterwards, phosphorylated c-Jun and c-Fos form the AP-1 transcription factor, are transported into the nucleus and lead to inflammatory gene expression.56
IEC-specific p38 MAPK signaling has a major role in eliciting the inflammatory response to C. rodentium infection as an intestinal barrier defense.57, 58 The p38α protein in IECs promotes the recruitment of CD4+ cells by expressing chemokines, which are involved in the host immune defense against enteric pathogens.58 Recently, the central role of the MAPK family was established in host protein phosphorylation and signal transduction during EPEC infection using quantitative proteomics.59 NleD, a metalloprotease, directly cleaves p38, a crucial part of the MAPK signaling pathway, and JNK within the activation loop in EPEC-infected epithelial cells. The inactivation of the transcription factor c-Jun may account for the suppressed IL-8 secretion, although NleD may have a minor role. In addition, NleD can also specifically cleave and inactivate the p65 subunit of NF-κB.60 EPEC-derived NleC, as mentioned above, was predominantly localized at the site of bacterial attachment beneath the host cell membrane28 and had an effect on MAPK signaling in addition to NF-κB signaling.61 Significantly elevated p38 MAPK phosphorylation was detected in NleC-deleted EPEC infection. However, NleC failed to block flagellin-induced epithelial p38 MAPK signaling, which indicates a modest role in early immune subversion. Interestingly, NleH2 was also found to increase the activity of AP-1-dependent gene expression.35 The phosphorylation of multiple MAPKs, including ERK1/2, p38 and JNK, is induced upon EHEC infection, followed by AP-1 activation at later stages of infection.62 Moreover, the phosphorylation of the T42 residue of RPS3 by ERK facilitates its nuclear entry.63 The precise role of NleH2 in ERK/MAPK pathways, whether via the ERK substrate RPS3 or independent of RPS3, requires more investigation. Overall, NleD, NleC and NleH2 have been implicated in signaling regulation from the perspective of MAPK (Figure 1).
TAK1 is a key signaling component not only in the NF-κB pathway but also in MAPK signaling pathways, mediated by TLRs, the IL-1 receptor and the TNF receptor family.64 Lys562 of TAK1 is a novel Lys63-linked ubiquitination site. The loss of ubiquitination at Lys562 leads to reduced phosphorylation of TAK1 but has no effect on TAK1-containing complexes,65 which differentially regulate the NF-κB and MAPK pathways, since IKK activation might depend on the TAK1 protein as a platform for complex formation but does not depend on TAK1 activation.66 The activation of TAK1 is regulated by polyubiquitination and in turn inhibits further modification, indicating dynamic feedback regulation. EPEC effectors targeting the NF-κB pathway, especially TAK1 modification, may regulate the NF-κB and MAPK pathways with opposite effects. This may possibly account for the inconsistent activity of these two major signaling pathways in different stages of infection, which requires more supporting evidence (Figure 1).
In addition to the classical targets in MAPK signaling manipulated by EPEC effector proteins, Sonja et al. identified the interactions of effector proteins in EPEC with host proteins by performing yeast two-hybrid screens, among which small calcium-binding proteins, namely hippocalcin, encoded by the gene Hpcal1, and neurocalcin, δ encoded by the gene Ncald, are worthy of further evaluation.67 Hippocalcin and neurocalcin δ belong to the visinin-like protein subfamily, a highly homologous subfamily of neuronal calcium sensor proteins that may exert effects on signal transduction cascades.68 Hippocalcin may possibly interact with MLK2/3 (mixed-lineage Ser/Thr kinases), which is closely linked to the MAP3K family and in turn activates JNK, ERK and p38.69 In transgenic hippocalcin−/− mice, which have a malfunctioning MAP kinase cascade, a pathway upstream of cAMP-response element-binding protein (CREB) was proposed to be responsible for the suppression of CREB activation. Later, the phosphorylation of the MAP kinase ERK2 was demonstrated to be influenced by hippocalcin.70 In addition, these proteins co-localize in areas where EPEC colonize. Therefore, members of the superfamily of neuronal calcium sensors are likely to be unexplored targets engaged in Tir-dependent signaling complexes, especially in the MAP kinase signaling pathway, to participate in immune subversion by EPEC.
Notably, in a C. rodentium-induced transmissible murine colonic hyperplasia model, the inhibition of MEK1/2, ERK1/2 and p38 by specific siRNAs or MEK1/2 inhibitor was mimicked by blocking NF-κB activity. This indicates that MAPK regulates NF-κB signaling during C. rodentium infection, and thus effectors from the EPEC-target MAPK signaling pathway may exaggerate the inhibitory influence by engaging NF-κB signaling.71 However, work on effectors influencing MAPK signaling pathways is relatively limited, and further exploration is needed to determine the extent of the suppressive effects of the relevant functioning proteins.
Concluding remarks
It is increasingly accepted that multifunction, cooperation and redundancy are three vital features of various T3SS-pathogen effectors.10 With regard to cooperation, some effectors may dictate characteristic phenotypes during infection and be critical for virulence, while others may only have accessory or secondary roles, such as NleC and NleE, respectively. Compared with LEE effectors, non-LEE effectors are more highly conserved between A/E pathogens, suggesting that targeting highly conserved inflammatory proteins is the priority for pathogen survival. With regard to the apparent redundancy, effectors targeting different sequential points along a certain signaling pathway suppress host cell function at the same time in case any effector fails to work. Moreover, greater and longer-lasting subversion of the innate immune system can be attained in this manner.
Overall, the expanded repertoire of effectors from EPEC and newly explored functions of known EPEC effectors present us an opportunity to understand the pathogen's subversion strategies, based on which novel therapeutic targets against enteral infection can be identified. However, it is possible to discover a deeper perspective into vital eukaryotic processes using purified effectors targeting certain points of cellular signaling networks as tools.
Acknowledgments
This work was sponsored by the Program for Professor of Special Appointment (Eastern Scholar) at Shanghai Institutions of Higher Learning and Shanghai Pujiang Program.
Footnotes
The authors declare no conflict of interest.
References
- Vivier E, Malissen B. Innate and adaptive immunity: specificities and signaling hierarchies revisited. Nat Immunol 2005; 6: 17–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medzhitov R, Janeway CA. Innate immunity: the virtues of a nonclonal system of recognition. Cell 1997; 91: 295–298. [DOI] [PubMed] [Google Scholar]
- Bonilla FA, Oettgen HC. Adaptive immunity. J Allergy Clin Immunol 2010; 1252: S33–S40. [DOI] [PubMed] [Google Scholar]
- Tato CM, Hunter CA. Host-pathogen interactions: subversion and utilization of the NF-kappa B pathway during infection. Infect Immun 2002; 70: 3311–3317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finlay BB, McFadden G. Anti-immunology: evasion of the host immune system by bacterial and viral pathogens. Cell 2006; 124: 767–782. [DOI] [PubMed] [Google Scholar]
- Kim DW, Lenzen G, Page AL, Legrain P, Sansonetti PJ, Parsot C et al. The Shigella flexneri effector OspG interferes with innate immune responses by targeting ubiquitin-conjugating enzymes. Proc Natl Acad Sci USA 2005; 102: 14046–14051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mundy R, MacDonald TT, Dougan G, Frankel G, Wiles S. Citrobacter rodentium of mice and man. Cell Microbiol 2005; 7: 1697–1706. [DOI] [PubMed] [Google Scholar]
- Croxen MA, Law RJ, Scholz R, Keeney KM, Wlodarska M, Finlay BB. Recent advances in understanding enteric pathogenic Escherichia coli. Clin Microbiol Rev 2013; 26: 822–880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong AR, Pearson JS, Bright MD, Munera D, Robinson KS, Lee SF et al. Enteropathogenic and enterohaemorrhagic Escherichia coli: even more subversive elements. Mol Microbiol 2011; 80: 1420–1438. [DOI] [PubMed] [Google Scholar]
- Dean P, Kenny B. The effector repertoire of enteropathogenic E. coli: ganging up on the host cell. Curr Opin Microbiol 2009; 12: 101–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ea CK, Deng L, Xia ZP, Pineda G, Chen Z. Activation of IKK by TNF alpha requires site-specific ubiquitination of RIP1 and polyubiquitin binding by NEMO. Mol Cell 2006; 22: 245–257. [DOI] [PubMed] [Google Scholar]
- Ajibade AA, Wang HY, Wang R. Cell type-specific function of TAK1 in innate immune signaling. Trends Immunol 2013; 34: 307–316. [DOI] [PubMed] [Google Scholar]
- Gao M, Karin M. Regulating the regulators: control of protein ubiquitination and ubiquitin-like modifications by extracellular stimuli. Mol Cell 2005; 19: 581–593. [DOI] [PubMed] [Google Scholar]
- Karin M, Gallagher E. TNFR signaling: ubiquitin-conjugated TRAFfic signals control stop-and-go for MAPK signaling complexes. Immunol Rev 2009; 228: 225–240. [DOI] [PubMed] [Google Scholar]
- Mills E, Baruch K, Aviv G, Nitzan M, Rosenshine I. Dynamics of the type III secretion system activity of enteropathogenic Escherichia coli. mBio 2013; 4: e00303–e00313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruchaud-Sparagano M, Muehlen S, Dean P, Kenny B. The enteropathogenic E. coli (EPEC) tir effector inhibits NF-kappa B activity by targeting TNF alpha receptor-associated factors. PLoS Pathog 2011; 7: e1002414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blero D, Payrastre B, Schurmans S, Erneux C. Phosphoinositide phosphatases in a network of signalling reactions. Pflugers Arch 2007; 455: 31–44. [DOI] [PubMed] [Google Scholar]
- Yan D, Quan H, Wang L, Liu F, Liu H, Chen J et al. Enteropathogenic Escherichia coli Tir recruits cellular SHP-2 through ITIM motifs to suppress host immune response. Cell Signal 2013; 25: 1887–1894. [DOI] [PubMed] [Google Scholar]
- Yan D, Wang X, Luo L, Cao X, Ge B. Inhibition of TLR signaling by a bacterial protein containing immunoreceptor tyrosine-based inhibitory motifs. Nat Immunol 2012; 13: 1063–1071. [DOI] [PubMed] [Google Scholar]
- Wang Y, Tang Y, Teng L, Wu Y, Zhao X, Pei G. Association of β-arrestin and TRAF6 negatively regulates Toll-like receptor–interleukin 1 receptor signaling. Nat Immunol 2005; 7: 139–147. [DOI] [PubMed] [Google Scholar]
- Yu M, Su L, Zou L, Liu Y, Wu N, Kong L et al. An essential function for β-arrestin 2 in the inhibitory signaling of natural killer cells. Nat Immunol 2008; 9: 898–907. [DOI] [PubMed] [Google Scholar]
- Gao X, Wang X, Pham TH, Feuerbacher LA, Lubos M, Huang M et al. NleB, a bacterial effector with glycosyltransferase activity, targets GAPDH function to inhibit NF-κB activation. Cell Host Microbe 2013; 13: 87–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearson JS, Giogha C, Ong SY, Kennedy CL, Kelly M, Robinson KS et al. A type III effector antagonizes death receptor signalling during bacterial gut infection. Nature 2013; 501: 247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newton HJ, Pearson JS, Badea L, Kelly M, Lucas M, Holloway G et al. The type III effectors NleE and NleB from enteropathogenic E. coli and OspZ from Shigella block nuclear translocation of NF-kappa B p65. PLoS Pathog 2010; 6: e1000898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nadler C, Baruch K, Kobi S, Mills E, Haviv G, Farago M et al. The type III secretion effector NleE inhibits NF-kappa B activation. PLoS Pathog 2010; 6: e1000743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang L, Ding X, Cui J, Xu H, Chen J, Gong YN et al. Cysteine methylation disrupts ubiquitin-chain sensing in NF-kappa B activation. Nature 2012; 481: 204. [DOI] [PubMed] [Google Scholar]
- Vossenkämper A, Marchés O, Fairclough PD, Warnes G, Stagg AJ, Lindsay JO et al. Inhibition of NF-kappa B signaling in human dendritic cells by the enteropathogenic Escherichia coli effector protein NleE. J Immunol 2010; 185: 4118–4127. [DOI] [PubMed] [Google Scholar]
- Yen H, Ooka T, Iguchi A, Hayashi T, Sugimoto N, Tobe T et al. NleC, a type III secretion protease, compromises NF-κB activation by targeting p65/RelA. PLoS Pathog 2010; 6: 1001231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearson JS, Riedmaier P, Marches O, Frankel G, Hartland EL. A type III effector protease NleC from enteropathogenic Escherichia coli targets NF-kappa B for degradation. Mol Microbiol 2011; 80: 219–230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muehlen S, Ruchaud-Sparagano M, Kenny B. Proteasome-independent degradation of canonical NF kappa B complex components by the NleC protein of pathogenic Escherichia coli. J Biol Chem 2011; 286: 5100–5107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giogha C, Lung TWF, Muehlen S, Pearson JS, Hartland EL. Substrate recognition by the zinc metalloprotease effector NleC from enteropathogenic Escherichia coli. Cell Microbiol 2015; 17: 1766–1778. [DOI] [PubMed] [Google Scholar]
- Hodgson A, Wier EM, Fu K, Sun X, Yu H, Zheng W et al. Metalloprotease NleC suppresses host NF-kappa B/inflammatory responses by cleaving p65 and interfering with the p65/RPS3 interaction. PLoS Pathog 2015; 11: e1004705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shames SR, Bhavsar AP, Croxen MA, Law RJ, Mak SHC, Deng W et al. The pathogenic Escherichia coli type III secreted protease NleC degrades the host acetyltransferase p300. Cell Microbiol 2011; 13: 1542–1557. [DOI] [PubMed] [Google Scholar]
- Wan F, Anderson DE, Barnitz RA, Snow A, Bidere N, Zheng L et al. Ribosomal protein S3: a KH domain subunit in NF-kappaB complexes that mediates selective gene regulation. Cell 2007; 131: 927–939. [DOI] [PubMed] [Google Scholar]
- Gao XF, Wan FY, Mateo K, Callegari E, Wang D, Deng W et al. Bacterial effector binding to ribosomal protein S3 subverts NF-kappa B function. PLoS Pathog 2009; 5: e1000708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wan F, Weaver A, Gao X, Bern M, Hardwidge PR, Lenardo MJ et al. IKK beta phosphorylation regulates RPS3 nuclear translocation and NF-kappa B function during infection with Escherichia coli strain O157:H7. Nat Immunol 2011; 12: 119–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pham TH, Gao X, Singh G, Hardwidge PR. Escherichia coli virulence protein NleH1 interaction with the v-Crk sarcoma virus CT10 oncogene-like protein (CRKL) governs NleH1 inhibition of the ribosomal protein 53 (RPS3)/nuclear factor kappa B (NF-kappa B) pathway. J Biol Chem 2013; 288: 34567–34574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pham TH, Gao X, Tsai K, Olsen R, Wan F, Hardwidge PR et al. Functional differences and interactions between the Escherichia coli type III secretion system effectors NleH1 and NleH2. Infect Immun 2012; 80: 2133–2140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes A, Arlehamn C, Wang D, Mitchell TJ, Evans TJ, Roe AJ et al. Expression and regulation of the Escherichia coli O157:H7 Effector Proteins NleH1 and NleH2. PLoS One 2012; 7: e33408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith K, Humphreys D, Hume PJ, Koronakis V. Enteropathogenic Escherichia coli recruits the cellular inositol phosphatase SHIP2 to regulate actin-pedestal formation. Cell Host Microbe 2010; 7: 13–24. [DOI] [PubMed] [Google Scholar]
- Phillips N, Hayward RD, Koronakis V. Phosphorylation of the enteropathogenic E-coli receptor by the Src-family kinase c-Fyn triggers actin pedestal formation. Nat Cell Biol 2004; 6: 618–625. [DOI] [PubMed] [Google Scholar]
- Sason H, Milgrom M, Weiss AM, Melamed-Book N, Balla T, Grinstein S et al. Enteropathogenic Escherichia coli subverts phosphatidylinositol 4,5-bisphosphate and phosphatidylinositol 3,4,5-trisphosphate upon epithelial cell infection. Mol Biol Cell 2009; 20: 544–555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roxas JL, Koutsouris A, Viswanathan VK. Enteropathogenic Eschetichia coli-induced epidermal growth factor receptor activation contributes to physiological alterations in intestinal epithelial cells. Infect Immun 2007; 75: 2316–2324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reddy S, Huang J, Liao W. Phosphatidylinositol 3-kinase as a mediator of TNF-induced NF-B kappa activation. J Immunol 2000; 164: 1355–1363. [DOI] [PubMed] [Google Scholar]
- Campellone KG, Leong JM. Nck-independent actin assembly is mediated by two phosphorylated tyrosines within enteropathogenic Escherichia coli Tir. Mol Microbiol 2005; 56: 416–432. [DOI] [PubMed] [Google Scholar]
- Hazeki K, Nigorikawa K, Hazeki O. Role of phosphoinositide 3-kinase in innate immunity. Biol Pharm Bull 2007; 30: 1617–1623. [DOI] [PubMed] [Google Scholar]
- Ruchaud-Sparagano MH, Maresca M, Kenny B. Enteropathogenic Escherichia coli (EPEC) inactivate innate immune responses prior to compromising epithelial barrier function. Cell Microbiol 2007; 9: 1909–1921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yen H, Sugimoto N, Tobe T. Enteropathogenic Escherichia coli uses NleA to inhibit NLRP3 inflammasome activation. PLoS Pathog 2015; 11: e1005121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wen H, Miao EA, Ting JPY. Mechanisms of NOD-like receptor-associated inflammasome activation. Immunity 2013; 39: 432–441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jo EK, Kim JK, Shin DM, Sasakawa C. Molecular mechanisms regulating NLRP3 inflammasome activation. 2016. pp 13: 148–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bednash JS, Mallampalli RK. Regulation of inflammasomes by ubiquitination. Cell Mol Immunol 2016. e-pub ahead of print 11 April 2016 doi:10.1038/cmi.2016.15. [DOI] [PMC free article] [PubMed]
- Thanabalasuriar A, Bergeron J, Gillingham A, Mimee M, Thomassin JL, Strynadka N et al. Sec24 interaction is essential for localization and virulence-associated function of the bacterial effector protein NleA. Cell Microbiol 2012; 14: 1206–1218. [DOI] [PubMed] [Google Scholar]
- Lerner AG, Upton JP, Praveen P, Ghosh R, Nakagawa Y, Igbaria A et al. IRE1 alpha induces thioredoxin-interacting protein to activate the NLRP3 inflammasome and promote programmed cell death under irremediable ER stress. Cell Metab 2012; 16: 250–264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akira S, Takeda K. Toll-like receptor signalling. Nat Rev Immunol 2004; 4: 499–511. [DOI] [PubMed] [Google Scholar]
- Kawai T, Akira S. TLR signaling. Sem Immunol 2007; 19: 24–32. [DOI] [PubMed] [Google Scholar]
- Shaulian E, Karin M. AP-1 in cell proliferation and survival. Oncogene 2001; 20: 2390–2400. [DOI] [PubMed] [Google Scholar]
- Ruchaud-Sparagano M, Maresca M, Kenny B. Enteropathogenic Escherichia coli (EPEC) inactivate innate immune responses prior to compromising epithelial barrier function. Cell Microbiol 2007; 9: 1909–1921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang YJ, Otsuka M, van den Berg A, Hong L, Huang Z, Wu X et al. Epithelial p38alpha controls immune cell recruitment in the colonic mucosa. PLoS Pathog 2010; 6: e1000934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scholz R, Imami K, Scott NE, Trimble WS, Foster LJ, Finlay BB et al. Novel host proteins and signaling pathways in enteropathogenic E. coli pathogenesis identified by global phosphoproteome analysis. Mol Cell Proteomics 2015; 14: 1927–1945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baruch K, Gur-Arie L, Nadler C, Koby S, Yerushalmi G, Ben-Neriah Y et al. Metalloprotease type III effectors that specifically cleave JNK and NF-kappa B. EMBO J 2011; 30: 221–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sham HP, Shames SR, Croxen MA, Ma C, Chan JM, Khan MA et al. Attaching and effacing bacterial effector NleC suppresses epithelial inflammatory responses by inhibiting NF- B and p38 mitogen-activated protein kinase activation. Infect Immun 2011; 79: 3552–3562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dahan S, Busuttil VB, Imbert V, Peyron JF, Rampal P, Czerucka D et al. Enterohemorrhagic Escherichia coli infection induces interleukin-8 production via activation of mitogen-activated protein kinases and the transcription factors NF-kappa B and AP-1 in T84 cells. Infect Immun 2002; 70: 2304–2310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim HD, Lee JY, Kim J. Erk phosphorylates threonine 42 residue of ribosomal protein S3. Biochem Biophys Res Commun 2005; 333: 110–115. [DOI] [PubMed] [Google Scholar]
- Shim JH, Xiao CC, Paschal AE, Bailey ST, Rao P, Hayden MS et al. TAK1, but not TAB1 or TAB2, plays an essential role in multiple signaling pathways in vivo. Genes Dev 2005; 19: 2668–2681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen I, Hsu P, Hsu W, Chen N, Tseng P. Polyubiquitination of transforming growth factor β-activated kinase 1 (TAK1) at lysine 562 residue regulates TLR4-mediated JNK and p38 MAPK activation. Sci Rep 2015; 5: 12300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tseng P, Matsuzawa A, Zhang W, Mino T, Vignali DAA, Karin M et al. Different modes of ubiquitination of the adaptor TRAF3 selectively activate the expression of type I interferons and proinflammatory cytokines. Nat Immunol 2010; 11: 70–1819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blasche S, Arens S, Ceol A, Siszler G, Schmidt MA, Häuser R et al. The EHEC-host interactome reveals novel targets for the translocated intimin receptor. Sci Rep 2014; 4: 7531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braunewell K, Klein-Szanto AJ. Visinin-like proteins (VSNLs): interaction partners and emerging functions in signal transduction of a subfamily of neuronal Ca2+-sensor proteins. Cell Tissue Res 2009; 335: 301–316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tibbles LA, Woodgett JR. The stress-activated protein kinase pathways. Cell Mol Life Sci 1999; 55: 1230–1254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kobayashi M, Masaki T, Hori K, Masuo Y, Miyamoto M, Tsubokawa H et al. Hippocalcin-deficient mice display a defect in cAMP response element-binding protein activation associated with impaired spatial and associative memory. Neuroscience 2005; 133: 471–484. [DOI] [PubMed] [Google Scholar]
- Chandrakesan P, Ahmed I, Anwar T, Wang Y, Sarkar S, Singh P et al. Novel changes in NF- B activity during progression and regression phases of hyperplasia: role of MEK, ERK, and p38. J Biol Chem 2010; 285: 33485–33498. [DOI] [PMC free article] [PubMed] [Google Scholar]