Abstract
Addictive disorders, such as pathological gambling and alcohol use disorders, frequently co-occur at greater than chance levels. Substantive questions stem from this comorbidity regarding the extent to which shared variance between gambling and alcohol use reflects a psychological core of addictive tendencies, and whether this differs as a function of gender. The aims of this study were to differentiate both common and unique variance in alcohol and gambling problems in a bifactor model, examine measurement invariance of this model by gender, and identify substantive correlates of the final bifactor model. Undergraduates (N = 4475) from a large northwestern university completed an online screening questionnaire which included demographics, quantity of money lost and won when gambling, the South Oaks Gambling Screen, the AUDIT, gambling motives, drinking motives, personality, and the Brief Symptom Inventory. Results suggest that the bifactor model fit the data well in the full sample. Although the data suggest configural invariance across gender, factor loadings could not be constrained to be equal between men and women. As such, general and specific factors were examined separately by gender with a more intensive subsample of females and males (n = 264). Correlations with motivational tendencies, personality traits, and mental health symptoms indicated support for the validity of the bifactor model, as well as gender-specific patterns of association. Results suggest informative distinctions between shared and unique attributes related to problematic drinking and gambling.
Keywords: Pathological gambling, Risky drinking, College students, Bifactor model
Prevalence rates for problem and pathological gambling have fluctuated across time, changing definitions and criteria, and assessment instruments. Estimates for lifetime pathological gambling in the U.S. general population have ranged from about .4–3.5 % and sub-threshold (problem gambling) estimates have ranged from 2.9 to 4.8 % (Cunningham-Williams et al. 1998; Kessler et al. 2008; Lorains et al. 2011; Petry et al. 2005; Shaffer et al. 1999). Prevalence estimates are considerably higher for college students. Estimates from Shaffer et al. (1999) meta-analysis found the average prevalence rates among college students to be 4.67 % pathological and 9.28 % subthreshold. On the other hand, results from the 2013 National Survey on Drug Use and Health (N = 67,500; SAMHSA 2014) estimated past month prevalence of binge drinking (5+ on at least one occasion) in 23 % of the U.S. population over age 12. Heavy drinking, defined as at least five binge occasions in the past month was estimated to be 6.3 %. The general population estimate for alcohol abuse or dependence was 7.0 %. Rates were considerably higher among college-aged individuals (18–25) with estimates of 37.9 and 11.3 % binge and heavy drinking respectively. Estimated prevalence past year alcohol disorder was also higher in this group at 13 %. Thus, both problematic gambling and problematic alcohol use are fairly common problems, particularly among college student populations.
Consistent evidence has revealed comorbidity between problem gambling and substance related problems including alcohol. Relative to nongamblers, problem gamblers are approximately 7.2 times more likely to drink and 3.3 times more likely to have an alcohol use disorder (Cunningham-Williams et al. 1998). In Crockford and el-Guebaly’s (1998) review, between 25 and 63 % of pathological gamblers also had an alcohol use disorder whereas between 9 and 16 % of patients with substance disorders were also identified as probable pathological gamblers. In the National Epidemiologic Survey on Alcohol and Related Conditions (N = 43,093; NESARC; Grant et al. 2003), 73.2 % of individuals identified as pathological gamblers also had an alcohol use disorder (Petry et al. 2005) which is about 8 times higher than the 8.5 % population estimate (Grant et al. 2004) in that data-set. The prevalence of pathological gambling found in NESARC (0.42 %) was just over 2 times higher among individuals with a current alcohol use disorder (1.03 %). Thus, problem gambling and problem alcohol use also frequently co-occur at greater than chance levels (i.e., demonstrate robust patterns of comorbidity).
Increasing recognition of the overlap between gambling and substance use contributed to diagnostic changes in pathological gambling, which was previously classified as an impulse control disorder in the DSM-IV TR (APA 2000), to gambling disorder, now grouped among substance-related and addictive disorders in the DSM-5 (APA 2013). This change occurred in recognition of striking similarities between problem gambling and substance use in terms of symptoms, treatment approaches, and shared comorbidities as well as convergence in neurobiological correlates based on brain imaging, genetics and neurotransmitter studies (Gottheil et al. 2007). This taxonomic shift underscores the need to better understand such overlap, when it occurs, as well as unique aspects of both problem gambling and problem alcohol use (controlling for shared, or overlapping variance) as distinct diagnostic entities. This represented the primary goal of the present study.
Gender Differences in Gambling, Alcohol, and Comorbidity
Prevalence studies examining gender differences in gambling show that men are more likely to over report gambling and gamble at higher frequencies and quantities than do women (Kessler et al. 2008; Potenza et al. 2001; Shaffer and Hall 2001; Welte et al. 2002). Men also develop problem and pathological gambling at higher rates than women (Blanco et al. 2006; Cunningham-Williams et al. 1998; Kessler et al. 2008; Welte et al. 2001). However, research has also shown that men and women differ in their motives for gambling, suggesting that gambling among men occurs for excitement, thrill-seeking, and loss-chasing motives, whereas gambling among women occurs for regulation of negative affect (Blanco et al., 2006; Grant and Kim 2002; Ladd and Petry 2002; Lesieur and Blume 1991; Potenza et al. 2001). These findings help explain results from other studies demonstrating that associations between pathological gambling and DSM-IV psychiatric disorders, particularly internalizing disorders (e.g., dysthymia, major depression, generalized anxiety disorder, panic disorders), were stronger among women than men (Blanco et al. 2006; Desai and Potenza 2008; Petry et al. 2005; Potenza et al. 2001). With regard to gender differences in problematic drinking, research also shows that although men drink at a greater quantity and frequency than do women (Nolen-Hoeksema, 2004; SAMHSA 2014), problematic alcohol use is associated with consequences and affects health outcomes more strongly for women (Baraona et al. 2001; Greenfield 2002; Hill 1995; Nolen-Hoeksema 2004). Further, studies have shown that motivation for drinking is a stronger predictor of alcohol-related problems in men, whereas depressive symptomatology is a stronger predictor of problems in women (Harrell and Karim 2008).
Research examining gender differences in the comorbidity between gambling and alcohol use is limited. One study utilized the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) data to show that among respondents with subclinical pathological gambling, men were significantly more likely to be classified as heavy drinkers (Blanco et al. 2006). Similarly, another study found that for men, heavy drinkers were more likely to report gambling with friends, gambling with large amounts of money, and engaging in strategic forms of gambling; associations which were not present for women (Desai et al. 2006). Other work has demonstrated that associations between pathological gambling and alcohol dependence, nicotine dependence, and drug use disorders were stronger among women than men (Petry et al. 2005). While additional research is needed to understand these gender differences, it is possible that because women have lower rates of gambling and substance use overall, women who do evince problem levels of these may represent a distinct subgroup, displaying higher levels of comorbidity for problematic addictive behaviors, as well. In summary, gender differences suggest that men gamble and use alcohol more frequently and in greater quantities than do women, whereas drinking and gambling are more strongly associated with poorer psychological functioning among women. These findings emphasize the importance of considering gender in examinations of comorbidity of addictive problems, as in the present study.
Structural Models of Psychopathology Comorbidity
As described previously, a better understanding of the overlapping and nonoverlapping nature of gambling and alcohol problems is needed. Clearly, gambling and alcohol problems share an overall classification as addictive problems (Gottheil et al. 2007), which is now specifically embodied in DSM-5 (APA 2013). Furthermore, structural models of broadly defined psychopathology in adulthood differentiate between internalizing problems such as depression and anxiety versus externalizing problems reflecting disinhibition and sensation-seeking (e.g., Slade and Watson 2006). However, within the externalizing psychopathology domain, addictive disorders form a separate subfactor from other forms of antisocial behavior such as aggression and criminality (Krueger et al. 2007). Thus, precedent for grouping addictive problems together—including gambling and alcohol use—has been established. Yet, co-occurrence rates remain relatively low (Grant et al. 2004), raising important questions about the extent to which shared variance between gambling and alcohol use reflects a psychological core of addictive tendencies.
One particular modeling approach that has proven useful in differentiating sources of common and unique variance in psychological constructs, including psychopathology, is the bifactor model (Chen et al. 2012). The bifactor model has a long tradition in psy-chometric research, and serves to differentiate shared variance among constructs in a “general” factor, while simultaneously modeling unique variance in each construct in a “specific” factor. Traditionally, the bifactor model specifies that all shared variance between included constructs is captured in the general factor (i.e., correlations between specific factors are constrained at zero). The bifactor model has been useful in examining commonality and heterogeneity within specific domains, such as examinations of attention deficit/hyperactivity disorder subtypes (Martel et al. 2010; Toplak et al. 2012) and different variants of antisocial behavior (Tackett et al. 2013a, b). A bifactor model approach has also been used to examine larger scale comorbidity between distinct disorders, as well (Caspi et al. 2014; Lahey et al. 2011).
In addition to offering a structural understanding of common and specific variance, bifactor approaches to comorbidity offer an extremely useful opportunity to better understand the psychological nature of the substantive variance shared between disorders, as well as the psychological nature of the specific variance that each disorder does not share in common with the other. One example comes from research demonstrating that the personality trait of neuroticism is highly overlapping with shared variance among common childhood disorders, at both etiologic and phenotypic levels (Tackett et al. 2013a, b). Such findings extend our theoretical understanding of comorbidity by pointing to potential risk factors or mechanisms that can be more appropriately incorporated into working theories of psychopathology emergence and development. Thus, this approach may lend itself quite well to an empirically based, but theoretically rich, conceptualization of shared and unique variance in gambling and alcohol problems. The conceptual basis of such an approach is consistent with the idea of a general addiction syndrome (e.g., Shaffer et al. 2004), which has received empirical support regarding personality (Slutske et al. 2005) and genetic (Slutske et al. 2013) underpinnings. To the best of our knowledge, a bifactor model has not been used to conceptualize gambling and alcohol problems to date. This represented the primary goal of the present study.
The Present Study
The goals of the present study were to examine evidence for a bifactor conceptualization of co-occurring alcohol and gambling problems in a large sample (N >4000) of college students, and to further explore the nature of this model in a smaller subsample of college student gamblers. Specific goals of the present study were:
Test the fit of a bifactor model to college student alcohol and gambling problems. Compare fit to a single factor model and a correlated two-factor model. Examine evidence for measurement invariance of the best-fitting model across gender.
Begin constructing a nomological network for a bifactor conceptualization of problem gambling and alcohol use by differentiating motivational, personality, and health correlates of: the general factor, the specific alcohol problems factor, and the specific gambling problems factor.
Method
Participants
Undergraduate students (N = 12,944) from a large northwestern university were invited to complete a screening survey. Of those invited, 4751 (34.5 %) completed the survey. This sample was predominantly Caucasian (62.7 %) and Asian-American (22.6 %). A little over half of the sample was female (55.1 %), and participants were on average 20.34 (SD = 3.31) years old.
Procedures
Participants were invited via a mailed letter to complete a screening survey as part of a larger longitudinal study assessing physiological responses to photographic stimuli related to gambling, alcohol, and neutral content. A total of 12,944 students from a large northwestern university were invited to screen, and 4751 completed the brief screening survey. Compensation for completion of the screening survey was $10.00. All study procedures were approved by the university’s institutional review board. An additional subsample was then recruited (n = 264) to participate in a more intensive in-lab protocol.
Measures
Gambling behaviors and problems were measured using items from the South Oaks Gambling Screen (SOGS; Lesieur and Blume 1987) and two open-ended response question. Items from the SOGS that were used in this study related to 11 types of gambling behaviors individuals have participated in (e.g. machine gambling, card games, sports betting, etc.), as well as, five items assessing the type and frequency of a range of gambling behaviors, family history of gambling, and largest quantity lost while gambling. Two open response questions were used to assess the largest quantity of money participants had won and lost while gambling.
Participants drinking problems were assessed using the ten question Alcohol Use Disorder Identification Test (AUDIT; Saunders et al. 1993). Questions ask participants to report how often they had experienced behaviors or situations that are consistent with hazardous alcohol consumption. Response options were measured on three or five point scales ranging from Never/No to Daily or Almost Daily/Yes. Example items from the AUDIT include, “How often during the last year have you found that you were not able to stop drinking once you had started?” “How often during the last year have you been unable to remember what happened the night before because you had been drinking?” and “Have you or someone else been injured as a result of your drinking?”
Gambling motives were assessed using the Gambling Motives Questionnaire (GMQ; Neighbors et al. 2002). This measure is comprised of 48 items that represent 16 different gambling motives. These motives included boredom, competition, challenge, chasing, coping, drinking, escape, enjoyment, excitement, interest, luck, money, risk, skill, social, and winning. Items consist of statements ranging from “Something to do while drinking,” (boredom) to “A chance to get my money back,” (chasing). Participants reported how often they gambling for each of the listed reasons on a 5-point scale from 1-Never to 5-Always.
The Drinking Motives Questionnaire (DMQ; Cooper 1994) was used to assess participant motives for consuming alcohol. The DMQ assesses four types of drinking motives Conformity, Coping, Enhancement, and Social. Each subscale contains five items and response options are on a five-point scale from 1-Never/Almost Never to 5-Always/Almost Always. Questions about conformity motives include “To fit in with a group you like,” coping motives include “To forget about your problems,” enhancement motives include “Because I like the feeling,” and social motives include “Because it improves parties and celebrations.”
Personality constructs were measured using the Zuckerberg-Kuhlman Personality Questionnaire (ZKPQ; Zuckerman et al. 1993). The 99-item scale contains five subscales, Activity, Aggression/Hostility, Impulsiveness/Sensation Seeking, Neuroticism/Anxiety, and Sociability. Participants indicate whether each statement is true or false. Example items from each subscale are, “when I do things I do them with lots of energy” (Activity), “when people annoy me I do not hesitate to tell them so” (Aggression/Hostility), “I tend to begin a new job without much planning on how I will do it” (Impulsiveness/Sensation Seeking), “I sometimes feel edgy and tense” (Neuroticism/Anxiety), and “I tend to start conversations at parties” (Sociability).
Finally, the Brief Symptoms Inventory (BSI; Derogatis and Melisaratos 1983) was used to measure mental health constructs. The BSI consists of 53 items and measures nine mental health dimensions. The dimensions consist of anxiety, depression, hostility, interpersonal sensitivity, obsessive–compulsive behavior, paranoid ideation, phobic anxiety, psychoticism, and somatization. Participants rate how often, on a five-point scale from 0-not at all to 4-extremely, they have been bothered by in the past week by a list of symptoms. Example items include, “feeling tense or keyed up” (anxiety), “feeling lonely” (depression), “getting into frequent arguments” (hostility), “feelings of worthlessness” (interpersonal sensitivity), “having to check and double-check what you do” (obsessive–compulsive behavior), “others not giving you proper credit for your achievements” (paranoid ideation), “feeling very self-conscious with others” (phobic anxiety), “the idea that something is wrong with your mind” (psychoticism), and “feeling weak” (somatization).
Results
Structural equation modeling was performed in Mplus, Version 6 (Muthén and Muthén 1998–2010). Mplus utilizes a full information maximum likelihood (FIML) approach to handling missing data, which were minimal. The MLR estimator was used to estimate models, which is robust to non-normally distributed data. Fit statistics and criteria used to examine model fit include the root mean square error of approximation (RMSEA, <.08 considered good fit), the comparative fit index (CFI, >.95 considered good fit), and the square root mean residual (SRMR,<.08 considered good fit; Chen et al. 2012; Toplak et al. 2012). Factor analyses were conducted in the overall sample (N = 4472), as well as tests of measurement invariance (Female n = 2453, Male n = 2001). Correlational analyses to examine the substantive nature of the bifactor model were conducted in the intensive subsample (Female n = 65, Male n = 199).
Items 1A1-1A10 on the SOGS were summed to create one overall SOGS frequency item (SOGS1freq). In addition, parcels were created to increase model stability, rather than modeling items directly (Chen et al. 2012; Tackett et al. 2013a, b). Specifically, 4 parcels were made to reflect SOGS items: SOGSp1 (SOGS1freq, SOGS2, SOGS4); SOGSp2 (SOGS5, SOGS6, SOGS7); SOGSp3 (SOGS8, SOGS10); SOGSp4 (SOGS9, SOGS11, SOGS12, SOGS13, SOGS14). Item designations were determined following an exploration of item-level covariation (via exploratory factor analysis), which revealed heterogeneity among SOGS items. Specifically, a 4-factor EFA best fit the SOGS items (RMSEA = .035, CFI = .989, SRMR = .013), and items were subsequently allocated to parcels reflecting this 4-factor solution. Alternatively, a 2-factor EFA showed best fit for AUDIT items (RMSEA = .053, CFI = .981, SRMR = .022), with AUDIT items 5–10 all showing their highest loading on a second factor. Thus, to create three parcels for the AUDIT factor, the following designations were made: AUDITp1 (AUD1, AUD2, AUD3, AUD4); AUDITp2 (AUD5, AUD6, AUD7); AUDITp3 (AUD8, AUD9, AUD10). These parcels were used in subsequent analyses.
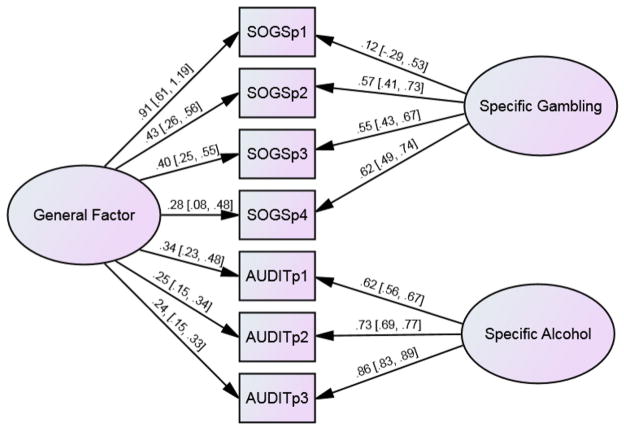
The bifactor model fit the data well in the full sample (RMSEA = .037, CFI = .987, SRMR = .024, see Fig. 1). All factor intercorrelations were constrained to zero, consistent with the traditional bifactor conceptualization. All parcels showed a significant loading on their respective factors, with the exception of SOGSp1 on the specific gambling factor. This loading was not significantly different from zero, indicating that all the variance in SOGSp1 was accounted for by the general factor. A 1-factor confirmatory factor analysis would not converge, which is not particularly surprising given the extent of non-overlapping variance in the alcohol and gambling measures. A 2-factor nonhierarchical CFA showed good fit to the data (RMSEA = .050, CFI = .959, SRMR = .041), but not superior fit to the bifactor model. In the 2-factor model, alcohol and gambling factors correlated at .278 (95 % CI .228, .329).
Fig. 1.
Final bifactor model with a general factor, specific gambling factor, and specific alcohol factor. Standardized factor loadings are presented with 95 % confidence intervals. Observed variables represent item parcels from the South Oaks Gambling Screen (SOGSp1-SOGSp4) and the Alcohol Use Disorder Identification Test (AUDITp1-AUDITp3)
The bifactor model was then fit separately in subsamples for men (RMSEA = .043, CFI = .987, SRMR = .018) and women (RMSEA = .005, CFI = 1.00, SRMR = .008), and fit well in both. Thus, the model demonstrated configural invariance across gender. Following this, nested models were created to examine evidence for weak invariance such that all factor loadings were constrained to be equal across men and women. A multi-group model was fit in which all parameters were free to vary across men and women (RMSEA = .026; CFI = .993) to compare with more stringent invariance constraints. Model comparisons followed the guidelines recommended in Toplak et al. (2012): a decrease of .01 or less in the CFI and an increase of not more than .01 in RMSEA were required to assume invariance. The model for weak invariance showed adequate fit to the data (RMSEA = .054, CFI = .945), but the change in RMSEA and CFI indicated that factor loadings could not be constrained across men and women. Thus, the following analyses examining correlates of the bifactor model were conducted separately for male and female subsamples in the intensive subsample.
Correlates of the Bifactor Model
Regression-based factor scores reflect individual standing on the general factor, the specific gambling factor, and the specific alcohol factor. Pearson correlations between these factor scores and other variables were examined to elucidate the overall nature of the general and specific factors, and to illustrate potential differences between the male and female subsamples.
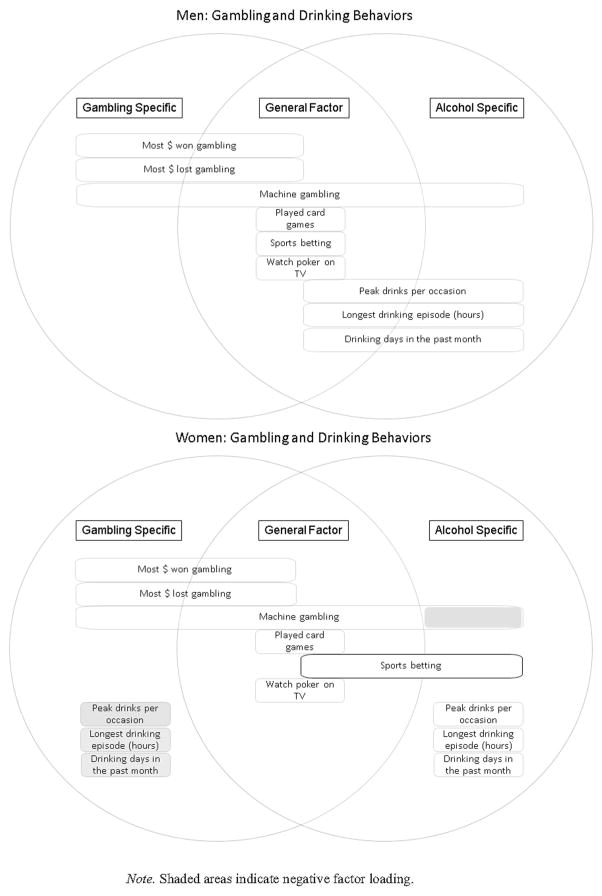
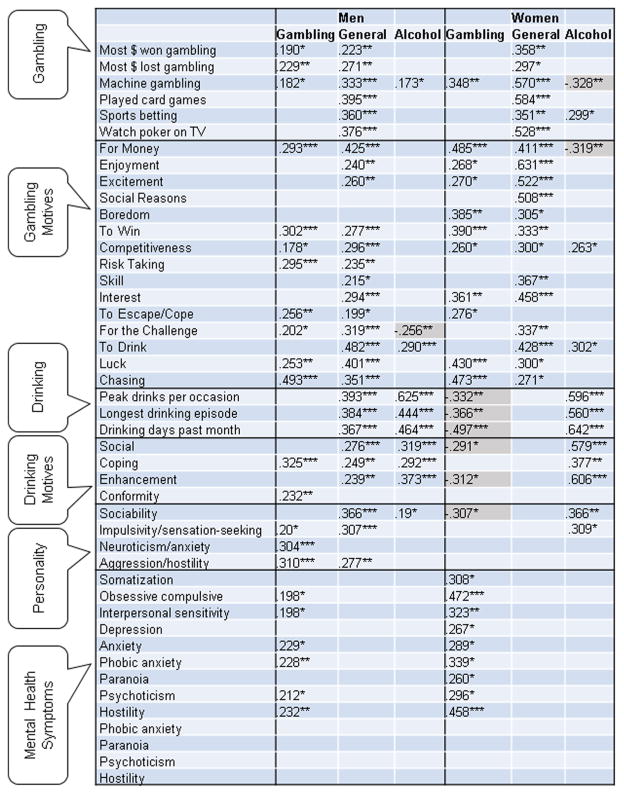
First, correlates were examined across a number of additional gambling and alcohol items (see Table 1; Fig. 2), to demonstrate convergent validity for the bifactor structure, but also to demonstrate its potential usefulness. Specifically, differential correlations with the general factor offer information about which gambling and alcohol behaviors are most relevant for gambling-alcohol co-occurrence (e.g., for women: machine gambling r = .570, p = .000, card games r = .584, p = .000, watching poker on TV r = .528, p = .000; for men: card games r = .395, p = .000, quantity of alcohol consumed in the largest episode r = .393, p = .000, hours of the largest alcohol consumption episode r = .384, p = .000). These findings indicate the different substantive nature of gambling-alcohol co-occurrence in women and men, such that problem drinking indicators overlap much more strongly with problem gambling indicators in men than they do in women.
Table 1.
Pearson correlations between the general factor, the specific gambling factor, the specific alcohol factor, and additional gambling and alcohol items
| General factor | Specific gambling | Specific alcohol | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| Men | Women | Men | Women | Men | Women | |
| Most $ won gambling | .223** | .358** | .190* | .209† | −.037 | −.114 |
| Most $ lost gambling | .271** | .297* | .229** | .095 | −.043 | −.230† |
| Machine gambling | .333*** | .570*** | .182* | .348** | .173* | −.328** |
| Played card games | .395*** | .584*** | .121 | .214† | .013 | .007 |
| Sports betting | .360*** | .351** | .009 | −.090 | .149† | .299* |
| Watch poker on TV | .376*** | .528*** | .131 | .216† | −.086 | .095 |
| Played tourn | .122 | .138 | .041 | .149 | .044 | .029 |
| Online gambling | .159† | .192 | .118 | .055 | .039 | .099 |
| Peak drinks per occasion | .393*** | .124 | −.102 | −.332** | .625*** | .596*** |
| Longest drinking episode (h) | .384*** | .047 | −.004 | −.366** | .444*** | .560*** |
| Drinking days in the past month | .367*** | −.053 | −.127 | −.497*** | .464*** | .642*** |
p <.001;
p <.01;
p <.05;
p <.1
Fig. 2.
Conceptual representation of primary markers for the general factor, specific gambling factor, and specific alcohol factor, estimated separately for men and women
Beyond convergent validity, correlations with the specific factors also offer information regarding divergent validity—for example, some items (e.g., days/week consuming alcohol over the past month) were positively correlated with one factor (specific alcohol r = .642, p = .000), negatively correlated with another (specific gambling r = −.497, p = .000), and share no overlapping variance with gambling-alcohol co-occurrence (general factor r = −.053, p = .676), at least for women. In other words, women who have spent many days drinking over the past month may be at especially low risk for problem gambling behaviors. However, the pattern for men is different, such that days/week consuming alcohol over the past month still reflect men’s scores on specific alcohol problems (r = .464, p = .000), but also reflect men’s likelihood of demonstrating gambling-alcohol co-occurrence (r = .367, p = .000) and do not show any association with specific gambling problems (r = −.127, p = .146). Thus, the same item, which indicates problematic alcohol use risk in both men and women, reflects a potential resiliency factor against problem gambling in women but a higher likelihood of gambling-alcohol co-occurrence in men.
Measures assessing both gambling and drinking motives offer further insight into the substantive nature of the general and specific factors (see Table 2). The pattern of associations once again showed gender differences. Unsurprisingly, endorsement of drinking motives during gambling behavior showed substantial correlations with the general factor in both women (r = .428, p = .000) and men (r = .482, p = .000). Otherwise, the pattern of strongest associations differed for men and women, as did patterns of divergent validity. For example, drinking motives related to coping and conformity predicted specific variance in gambling problems for men (r = .325 and .232, p = .000 and .008, respectively), above and beyond the general factor (gambling-alcohol co-occurrence) and specific variance in alcohol problems. However, coping and conformity drinking motives did not reflect specific variance in gambling problems in women.
Table 2.
Pearson correlations between the general factor, the specific gambling factor, the specific alcohol factor, and motives for drinking and gambling
| General factor | Gambling specific | Alcohol specific | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| Men | Women | Men | Women | Men | Women | |
| Drinking Motives | ||||||
| Social | .276*** | −.063 | .047 | −.291* | .319*** | .579*** |
| Coping | .249** | .023 | .325*** | −1.062 | .292*** | .377** |
| Enhancement | .239** | −.191 | −.016 | −.312* | .373*** | .606*** |
| Conformity | .165† | −.107 | .232** | −.081 | .068 | .218† |
| Gambling motives | ||||||
| For money | .425*** | .411*** | .293*** | .485*** | −.111 | −.319** |
| Enjoyment | .240** | .631*** | −.066 | .268* | −.076 | −.156 |
| Excitement | .260** | .522*** | .053 | .270* | −.024 | −.086 |
| Social reasons | .052 | .508*** | −.097 | .115 | .009 | −.029 |
| Boredom | .085 | .305* | .153† | .385** | .012 | .010 |
| To win | .277*** | .333** | .302*** | .390*** | −.160† | −.006 |
| Competitiveness | .296*** | .300* | .178* | .260* | −.042 | .263* |
| Conformity | −.009 | .170 | .070 | .162 | .025 | .022 |
| Risk taking | .235** | .205 | .295*** | .241† | −.053 | .116 |
| Skill | .215* | .367** | .115 | .230† | −.124 | .166 |
| Interest | .294*** | .458*** | .084 | .361** | −.060 | .089 |
| To escape/cope | .199* | .121 | .256** | .276* | .080 | −.012 |
| For the challenge | .319*** | .337** | .202* | .120 | −.256** | .144 |
| To drink | .482*** | .428*** | .118 | −.072 | .290*** | .302* |
| Luck | .401*** | .300* | .253** | .430*** | −.019 | −.118 |
| Chasing | .351*** | .271* | .493*** | .473*** | −.034 | −.245† |
p<.001;
p<.01;
p<.05;
p<.1
Fewer associations with personality traits were found for women than for men. In women, specific variance in gambling problems was associated with lower levels of sociability (r = −.307, p = .014), whereas specific variance in alcohol problems was associated with higher levels of impulsivity/sensation-seeking (r = .309, p = .014) and sociability (r = .366, p = .003). In men, the general factor was associated with higher levels of impulsivity/sensation-seeking (r = .307, p = .000), aggression/hostility (r = .277, p = .001), and sociability (r = .305, p = .000); specific variance in gambling problems was associated with impulsivity/sensation-seeking (r = .200, p = .022), neuroticism/anxiety (r = .304, p = .000), and aggression/hostility (r = .310, p = .000); specific variance in alcohol problems was associated with sociability (r = .190, p = .030).
Overarching associations with a measure of mental health demonstrated a different pattern—more associations were found for women than for men, although this pattern was reflected in associations with specific variance in gambling problems, in particular. That is, no mental health dimension showed a positive association with the general factor or with specific variance in alcohol problems, and this was true for women and men. In men, specific variance in gambling problems was associated with higher reports of obsessive compulsive behaviors (r = .198, p = .023), interpersonal sensitivity (r = .198, p = .023), anxiety, (r = .229, p = .008), phobic anxiety (r = .228, p = .009), psychoticism (r = .212, p = .015), and hostility (r = .232, p = .007). In women, however, specific variance in gambling problems was associated with higher levels of all symptom dimensions: somatization (r = .308, p = .013), obsessive compulsive behaviors (r = .472, p = .000), interpersonal sensitivity (r = .323, p = .009), depression (r = .267, p = .032), anxiety, (r = .289, p = .020), phobic anxiety (r = .339, p = .006), paranoia (r = .260, p = .037), psychoticism (r = .296, p = .017), and hostility (r = .458, p = .000). A summary of all significant associations by gender and by factor is presented in Fig. 3.
Fig. 3.
Correlational associations between validity indices and the general factor, specific gambling factor, and specific alcohol factor, estimated separately for men and women. Shaded areas indicate a negative factor loading
Discussion
The present study demonstrated that a bifactor model conceptualization can be a useful way of better understanding alcohol and gambling problem co-occurrence, and in delineating the substantive nature of both overlapping and distinct variance in these addictive problems. Specifically, we successfully fitted a bifactor model to alcohol and gambling problems in a large mixed-gender sample of college students. Assessment of measurement invariance revealed signficant differences in factor loadings between men and women. Evidence for the substantive nature of the general and specific factors was therefore examined separately by gender, with multiple associations with other constructs illustrating the psychological nature of the general and specific factors in this model. These results are discussed in more detail below.
Although the overall bifactor model fit the data well and showed successful fit in both male and female subsamples, factor loadings could not be constrained between genders. In both men and women, it is notable that the general factor (which captures shared variance between alcohol and gambling problems) was highly defined by the first parcel of gambling items, which comprised overall gambling frequency, and the extent to which the individual goes back to gamble more following a loss. Thus, this global composite of gambling frequency captured much of the shared variance between alcohol and gambling problems. The extent to which factor loadings differed between men and women could potentially reflect differential prevalence rates (Raylu and Oei 2002). Although differential prevalence rates would not necessarily result in measurement inequivalence, in the case where the underlying weighting and mechanisms are the same; however, differential prevalence rates in addictive behaviors may reflect other substantive and mechanistic differences such as social norms, expectancies, exposure, opportunity, and consequences (Brady et al. 2009; Byrnes et al. 1999; Iwamoto and Smiler 2013; Tyler et al. 2015; Wilsnack et al. 2000). In addition, the differential findings for substantive associations by gender suggest that such measurement inequivalence is meaningful, and future studies that do not explicitly test for measurement equivalence between genders may be adversely impacting study results.
To probe the substantive nature of the bifactor model, we examined associations (separately for males and females) with the general and specific factors in an intensive subsample of the overall sample which underwent a much more in-depth assessment protocol. A number of associations were demonstrated which provide further validity for a bifactor approach to gambling-alcohol co-occurrence. First, we examined associations with a number of other alcohol and gambling items, other than those used to model the bifactor structure directly. Many of these items were associated with the general factor, with stronger associations found for females than for males (also notable because the female subsample consisted of only 65 participants). This suggests that the general factor picks up on valid and reliable variance in addictive behaviors and tendencies. Associations with specific factors illustrate other ways that the bifactor model can be helpful. For example, for both males and females, the quantity of alcohol consumed during the last drinking episode was an extremely strong predictor of specific variance in alcohol problems, after accounting for shared variance with gambling problems. Furthermore, in females—but not in males—this variable was moderately associated with lower scores on specific gambling problems, suggesting a potentially gender-specific divergent predictor of gambling versus alcohol problems.
Moreover, when examining factor patterns of drinking and gambling related constructs (behavior and motives) by gender, we find support for the bifactor model but some interesting distinctions between men and women. For men, significant associations with the general factor are evident for almost all indices of behavior and motivation for gambling and drinking. For women the pattern is quite different. Almost all of the gambling indices and motives were associated with the general factor but none of the drinking indices or motives were associated with the general factor. Thus, we might suggest that a general factor placing women at risk for addictive behaviors is more likely to account for problematic gambling than for drinking. For men, the general factor appears to account relatively equally to indices of gambling and drinking. There is also a distinct difference in the association of gambling specific and alcohol specific factors between men and women. For men, where gambling specific indices (i.e., behaviors and motives) were associated with the alcohol specific factor and vice versa, these tended to be positive associations. For women they were more likely to be negative. In particular, for women, alcohol indices were only positively associated with the alcohol specific factor and were consistently negatively associated with the gambling specific factor. Taken together, these findings suggest that gambling and drinking are more strongly connected among men than women. These gender-specific findings could be very useful when trying to understand risk and resiliency factors as well as in directing intervention efforts, which would be masked if men and women were not examined separately.
Associations with personality and mental health also demonstrated gender-specific patterns. Specifically, personality traits were more strongly linked to the general and specific factors in men; whereas, mental health symptoms were more strongly linked to the general and specific factors in women. The overall patterns may reflect differences in normativity of these behaviors, such that personality traits are likely picking up on more normative variance in individual differences than do mental health symptoms. In conjunction with previous findings, these results suggesting that specific variance in gambling problems, after accounting for shared variance with alcohol problems, is especially strongly associated with psychopathology (thus potentially indicating a less normative addictive behavior in college students than is problematic alcohol use), and that these problematic associations are even stronger in female college students than in males.
As in all empirical research, it is also important to acknowledge some of the more salient limitations of the current study. The current research presents a novel examination of overlap and distinction of gambling and drinking among young adults, but results may not generalize to non-college samples or samples with more diverse demographic characteristics. In particular, when examining associations with a wide range of individual characteristics and behaviors, it is always important to keep in mind the base rate of the phenomena and the relative normativity in a given population. Associations with personality and psychopathology may manifest differently in samples where such behaviors are more, or less, normative. The data were also limited to only two addictive behaviors. Consideration of a bifactor model with larger number and wider range of addictive behaviors would be of interest for future work. The recent changes in the DSM-5 highlight the interesting question of how best to conceptualize the core of addictive behaviors, and such work should move forward by broadening the scope of addiction beyond the current work. In addition, information on situational factors relevant for drinking and gambling behaviors were not collected in the current study. Situational and contextual features, including aspects of the social environment, may further explicate gender differences in drinking and gambling. This remains an important topic for future research.
Conclusions
In conclusion, this research provided a novel examination of the overlap and distinction between two co-occuring addictive behaviors that are particularly common in college populations: gambling and alcohol use. Results of the bifactor model are consistent with the notion that there is a common factor underlying many addictive behaviors. Importantly, men and women have different profiles of gambling-alcohol co-occurrence, which are largely consistent with the broader literature. For men, gambling and drinking tend to co-occur with risk taking and are both associated with social functions. For women, gambling is more likely to serve as an escape and is more strongly associated with affective dis-regulation and psychopathology (Raylu and Oei 2002). Future research should expand our understanding of common and unique variance in addictive problems, and potential gender differences in addiction comorbidity.
Acknowledgments
This research was supported by grants from the National Center for Responsible Gaming to J.L.T., C.N., and G.E.
Footnotes
Compliance with Ethical Standards
Conflict of interest Authors have no additional conflicts of interest to report.
Ethical Approval All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or National Research Committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
References
- American Psychiatric Association (APA) Diagnostic and statistical manual of mental disorders, text revision (DSM-IV-TR) Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- American Psychiatric Association (APA) Diagnostic and statistical manual of mental disorders, (DSM-5®) Washington, DC: American Psychiatric Association; 2013. [Google Scholar]
- Baraona E, Abittan CS, Dohmen K, Moretti M, Pozzato G, Chayes ZW, et al. Gender differences in pharmacokinetics of alcohol. Alcoholism, Clinical and Experimental Research. 2001;25:502–507. [PubMed] [Google Scholar]
- Blanco C, Hasin DS, Petry N, Stinson FS, Grant BF. Sex differences in subclinical and DSM-IV pathological gambling: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Psychological Medicine. 2006;36:943–953. doi: 10.1017/S0033291706007410. [DOI] [PubMed] [Google Scholar]
- Brady KT, Back SE, Greenfield SF. Women and addiction: A comprehensive handbook. New York, NY: Guilford Press; 2009. [Google Scholar]
- Byrnes JP, Miller DC, Schafer WD. Gender differences in risk taking: A meta-analysis. Psychological Bulletin. 1999;125:367–383. [Google Scholar]
- Caspi A, Houts RM, Belsky DW, Goldman-Mellor SJ, Harrington H, Israel S, et al. The p factor one general psychopathology factor in the structure of psychiatric disorders? Clinical Psychological Science. 2014;2:119–137. doi: 10.1177/2167702613497473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen FF, Hayes A, Carver CS, Laurenceau JP, Zhang Z. Modeling general and specific variance in multifaceted constructs: A comparison of the bifactor model to other approaches. Journal of Personality. 2012;80:219–251. doi: 10.1111/j.1467-6494.2011.00739.x. [DOI] [PubMed] [Google Scholar]
- Cooper ML. Motivations for alcohol use among adolescents: Development and validation of a four-factor model. Psychological Assessment. 1994;6:117–128. [Google Scholar]
- Crockford DN, el-Guebaly N. Psychiatric comorbidity in pathological gambling: A critical review. Canadian Journal of Psychiatry. 1998;43:43–50. doi: 10.1177/070674379804300104. [DOI] [PubMed] [Google Scholar]
- Cunningham-Williams RM, Cottler LB, Compton WM, III, Spitznagel EL. Taking chances: Problem gamblers and mental health disorders–results from the St. Louis Epidemiologic Catchment Area Study. American Journal of Public Health. 1998;88:1093–1096. doi: 10.2105/ajph.88.7.1093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derogatis LR, Melisaratos N. The brief symptom inventory: An introductory report. Psychological Medicine. 1983;13:595–605. [PubMed] [Google Scholar]
- Desai RA, Maciejewski PK, Pantalon MV, Potenza MN. Gender differences among recreational gamblers: Association with the frequency of alcohol use. Psychology of Addictive Behaviors. 2006;20:145. doi: 10.1037/0893-164X.20.2.145. [DOI] [PubMed] [Google Scholar]
- Desai RA, Potenza MN. Gender differences in the associations between past-year gambling problems and psychiatric disorders. Social Psychiatry and Psychiatric Epidemiology. 2008;43:173–183. doi: 10.1007/s00127-007-0283-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gottheil E, Winters KC, Neighbors C, Grant JE, el-Guebaly N. Pathologic gambling: A nonsubstance, substance-related disorder? Journal of Addiction Medicine. 2007;1:53–61. doi: 10.1097/ADM.0b013e318066d5a8. [DOI] [PubMed] [Google Scholar]
- Grant JE, Kim SW. Gender differences in pathological gamblers seeking medication treatment. Comprehensive Psychiatry. 2002;43:56–62. doi: 10.1053/comp.2002.29857. [DOI] [PubMed] [Google Scholar]
- Grant BF, Moore TC, Shepard J, Kaplan K. Source and accuracy statement: Wave 1 national epidemiologic survey on alcohol and related conditions (NESARC) Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2003. [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, Kaplan K. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry. 2004;61:807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- Greenfield SF. Women and alcohol use disorders. Harvard Review of Psychiatry. 2002;10:76–85. doi: 10.1080/10673220216212. [DOI] [PubMed] [Google Scholar]
- Harrell ZA, Karim NM. Is gender relevant only for problem alcohol behaviors? An examination of correlates of alcohol use among college students. Addictive Behaviors. 2008;33:359–365. doi: 10.1016/j.addbeh.2007.09.014. [DOI] [PubMed] [Google Scholar]
- Hill SY. Mental and physical health consequences of alcohol use in women. Recent Developments in Alcoholism. 1995;12:181–197. doi: 10.1007/0-306-47138-8_10. [DOI] [PubMed] [Google Scholar]
- Iwamoto DK, Smiler AP. Alcohol makes you macho and helps you make friends: The role of masculine norms and peer pressure in adolescent boys’ and girls’ alcohol use. Substance Use and Misuse. 2013;48:371–378. doi: 10.3109/10826084.2013.765479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Hwang I, LaBrie R, Petukhova M, Sampson NA, Winters KC, Shaffer HJ. DSM-IV pathological gambling in the National Comorbidity Survey Replication. Psychological Medicine. 2008;38:1351–1360. doi: 10.1017/S0033291708002900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger RF, Markon KE, Patrick CJ, Benning SD, Kramer MD. Linking antisocial behavior, substance use, and personality: An integrative quantitative model of the adult externalizing spectrum. Journal of Abnormal Psychology. 2007;116:645–666. doi: 10.1037/0021-843X.116.4.645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ladd GT, Petry NM. Gender differences among pathological gamblers seeking treatment. Experimental and Clinical Psychopharmacology. 2002;10:302–309. doi: 10.1037//1064-1297.10.3.302. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Van Hulle CA, Singh AL, Waldman ID, Rathouz PJ. Higher-order genetic and environmental structure of prevalent forms of child and adolescent psychopathology. Archives of General Psychiatry. 2011;68:181–189. doi: 10.1001/archgenpsychiatry.2010.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lesieur HR, Blume SB. The South Oaks Gambling Screen (SOGS): A new instrument for the identification of pathological gamblers. American Journal of Psychiatry. 1987;144:1184–1188. doi: 10.1176/ajp.144.9.1184. [DOI] [PubMed] [Google Scholar]
- Lesieur HR, Blume SB. When lady luck loses: Women and compulsive gambling. In: Van Den Bergh N, editor. Feminist perspectives on treating addictions. New York: Springer; 1991. [Google Scholar]
- Lorains FK, Cowlishaw S, Thomas SA. Prevalence of comorbid disorders in problem and pathological gambling: Systematic review and meta-analysis of population surveys. Addiction. 2011;106:490–498. doi: 10.1111/j.1360-0443.2010.03300.x. [DOI] [PubMed] [Google Scholar]
- Martel MM, Von Eye A, Nigg JT. Revisiting the latent structure of ADHD: Is there a ‘g’factor? Journal of Child Psychology and Psychiatry. 2010;51:905–914. doi: 10.1111/j.1469-7610.2010.02232.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus user’s guide. 6. Los Angeles, CA: Muthén & Muthén; 1998–2010. [Google Scholar]
- Neighbors C, Lostutter TW, Cronce JM, Larimer ME. Exploring College Student Gambling Motivation. Journal of Gambling Studies. 2002;18:361–370. doi: 10.1023/a:1021065116500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nolen-Hoeksema S. Gender differences in risk factors and consequences for alcohol use and problems. Clinical Psychology Review. 2004;24:981–1010. doi: 10.1016/j.cpr.2004.08.003. [DOI] [PubMed] [Google Scholar]
- Petry NM, Stinson FS, Grant BF. Comorbidity of DSM-IV pathological gambling and other psychiatric disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. The Journal of Clinical Psychiatry. 2005;66:564–574. doi: 10.4088/jcp.v66n0504. [DOI] [PubMed] [Google Scholar]
- Potenza MN, Steinberg MA, McLaughlin SD, Wu R, Rounsaville BJ, O’Malley SS. Gender-related differences in the characteristics of problem gamblers using a gambling helpline. American Journal of Psychiatry. 2001;158:1500–1505. doi: 10.1176/appi.ajp.158.9.1500. [DOI] [PubMed] [Google Scholar]
- Raylu N, Oei TP. Pathological gambling: A comprehensive review. Clinical Psychology Review. 2002;22:1009–1061. doi: 10.1016/s0272-7358(02)00101-0. [DOI] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the alcohol use disorders screening test (AUDIT). WHO collaborative project on early detection of persons with harmful alcohol consumption. II. Addiction. 1993;88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Shaffer HJ, Hall MN. Updating and refining prevalence estimates of disordered gambling behavior in United States and Canada. Canadian Journal of Public Health. 2001;92:169–172. doi: 10.1007/BF03404298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaffer HJ, Hall MN, Vander Bilt J. Estimating the prevalence of disordered gambling behavior in the United States and Canada: A research synthesis. American Journal of Public Health. 1999;89:1369–1376. doi: 10.2105/ajph.89.9.1369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaffer HJ, LaPlante DA, LaBrie RA, Kidman RC, Donato AN, Stanton MV. Toward a syndrome model of addiction: Multiple expressions, common etiology. Harvard Review of Psychiatry. 2004;12:367–374. doi: 10.1080/10673220490905705. [DOI] [PubMed] [Google Scholar]
- Slade TIM, Watson D. The structure of common DSM-IV and ICD-10 mental disorders in the Australian general population. Psychological Medicine. 2006;36:1593–1600. doi: 10.1017/S0033291706008452. [DOI] [PubMed] [Google Scholar]
- Slutske WS, Caspi A, Moffitt TE, Poulton R. Personality and problem gambling: A prospective study of a birth cohort of young adults. Archives of General Psychiatry. 2005;62:769–775. doi: 10.1001/archpsyc.62.7.769. [DOI] [PubMed] [Google Scholar]
- Slutske WS, Ellingson JM, Richmond-Rakerd LS, Zhu G, Martin NG. Shared genetic vulnerability for disordered gambling and alcohol use disorder in men and women: Evidence from a national community-based Australian twin study. Twin Research and Human Genetics. 2013;16:525–534. doi: 10.1017/thg.2013.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2013 national survey on drug use and health: Summary of national findings. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2014. NSDUH Series H-48, HHS Publication No. (SMA) 14-4863. http://www.samhsa.gov/data/sites/default/files/NSDUHresultsPDFWHTML2013/Web/NSDUHresults2013.pdf. [Google Scholar]
- Tackett JL, Daoud SL, De Bolle M, Burt SA. Is relational aggression part of the externalizing spectrum? A bifactor model of youth antisocial behavior. Aggressive Behavior. 2013a;39:149–159. doi: 10.1002/ab.21466. [DOI] [PubMed] [Google Scholar]
- Tackett JL, Lahey BB, Van Hulle C, Waldman I, Krueger RF, Rathouz PJ. Common genetic influences on negative emotionality and a general psychopathology factor in childhood and adolescence. Journal of Abnormal Psychology. 2013b;122:1142. doi: 10.1037/a0034151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toplak ME, Sorge GB, Flora DB, Chen W, Banaschewski T, Buitelaar J, et al. The hierarchical factor model of ADHD: Invariant across age and national groupings? Journal of Child Psychology and Psychiatry. 2012;53:292–303. doi: 10.1111/j.1469-7610.2011.02500.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tyler KA, Schmitz RM, Adams SA. Alcohol expectancy, drinking behavior, and sexual victimization among female and male college students. Journal of Interpersonal Violence. 2015 doi: 10.1177/0886260515591280. [DOI] [PubMed] [Google Scholar]
- Welte JW, Barnes GM, Wieczorek W, Tidwell MC, Parker J. Alcohol and gambling pathology among U.S. adults: Prevalence, demographic patterns, and comorbidity. Journal of Studies on Alcohol. 2001;62:706–712. doi: 10.15288/jsa.2001.62.706. [DOI] [PubMed] [Google Scholar]
- Welte JW, Barnes GM, Wieczorek WF, Tidwell MC, Parker J. Gambling participation in the US—Results from a national survey. Journal of Gambling Studies. 2002;18:313–337. doi: 10.1023/a:1021019915591. [DOI] [PubMed] [Google Scholar]
- Wilsnack RW, Vogeltanz ND, Wilsnack SC, Harris TR. Gender differences in alcohol consumption and adverse drinking consequences: Cross-cultural patterns. Addiction. 2000;95:251–265. doi: 10.1046/j.1360-0443.2000.95225112.x. [DOI] [PubMed] [Google Scholar]
- Zuckerman M, Kuhlman DM, Joireman J, Teta P, Kraft M. A comparison of three structural models for personality: The Big Three, the Big Five, and the Alternative Five. Journal of Personality and Social Psychology. 1993;65:757–768. [Google Scholar]