Abstract
Behavior consultants conducted functional analyses (FAs) via telehealth with 20 young children with autism spectrum disorders between the ages of 29 and 80 months who displayed problem behavior and lived an average of 222 miles from the tertiary hospital that housed the behavior consultants. Participants’ parents conducted all procedures during weekly telehealth consultations in regional clinics located an average of 15 miles from the participants’ homes. Behavior consultants briefly trained parent assistants to provide on-site support for families during consultations. FAs completed within a multielement design identified environmental variables that maintained problem behavior for 18 of the 20 cases, and interrater agreement averaged over 90%. Results suggested that behavior analysts can conduct FAs effectively and efficiently via telehealth.
Keywords: functional analysis, telehealth, autism spectrum disorders
Many children with autism spectrum disorders (ASD) and other developmental disabilities engage in problem behavior (Oliver, Petty, Ruddick, & Bacarese-Hamilton, 2012), even at very early ages (Rogers & Wallace, 2011). Treatment packages that involve differential reinforcement programs matched to the function of problem behavior, such as functional communication training (FCT; Tiger, Hanley, & Bruzek, 2008; Wacker et al., 1998), can quickly reduce levels of problem behavior. This is important because, if left untreated, problem behavior often persists or increases over time and can negatively affect the child’s overall development and learning as well as the parents’ well-being (Baker et al., 2003).
One difficulty that many families experience is not having access to trained applied behavior analysts who can effectively implement procedures such as functional analysis (FA) or FCT. For example, less than 25 Board Certified Behavior Analysts (BCBAs) are listed in Iowa’s certificant registry (Behavior Analysis Certification Board, 2012), and there are an estimated 6,500 children with ASD in Iowa (Centers for Disease Control and Prevention, 2009). The lack of access to applied behavior analysis (ABA) services in rural states such as Iowa often results in long delays in receiving needed behavioral services, families having to absorb significant costs to obtain those services from out-of-state providers, or children going without needed services.
Since the seminal publication on FA by Iwata, Dorsey, Slifer, Bauman, and Richman (1982/1994), numerous studies have shown the clinical value of matching treatment to the identified function of problem behavior (e.g., Iwata et al., 1994). Other studies have shown that FA methods are learned easily (Iwata et al., 2000) and can be implemented in most applied settings. For example, brief versions of FAs (e.g., Cooper, Wacker, Sasso, Reimers, & Donn, 1990; Northup et al., 1991) were developed for outpatient clinic settings, and these versions were shown to be an effective way to identify the function of problem behavior. The correspondence between brief and more extended FAs is often very acceptable for clinical purposes (Kahng & Iwata, 1999; Wallace & Iwata, 1999), and FA procedures have been incorporated into many outpatient clinics (e.g., Kurtz et al., 2003; Watson & Sterling, 1998).
A second adaptation of FA procedures has involved conducting them in the homes of children with developmental disabilities who display problem behavior (Wacker et al., 1998). Wacker and colleagues have shown repeatedly that parents can conduct FAs in their homes when trained behavior analysts provide them with on-site coaching (Berg et al., 2007; Derby et al., 1997; Wacker et al., 2005). These studies also have shown that FCT programs that are matched to the results of FAs often decrease the occurrence of problem behavior by about 90%, even when every assessment and treatment session is conducted by a parent who has had no formal training in ABA. Equally important is that measures of the acceptability of these procedures consistently have shown that parents rate FA plus FCT as a highly acceptable intervention (Wacker et al., 1998, 2005).
Although the development of in-clinic and in-home services using FA procedures has been successful, demand for behavioral assessment and treatment far outpaces the availability of these services. For example, in-home services in Iowa can most often be delivered by our staff only within a 100-mile radius of the University of Iowa Children’s Hospital (UICH) due to time and travel constraints, and outpatient clinic appointments are routinely scheduled a minimum of 6 months from the day the appointment is requested. The limited availability of behavioral services for young children is of particular concern based on research that has shown that untreated problem behaviors tend to persist over time, can contribute to high levels of parent stress, and can have a negative impact on student learning (Baker et al., 2003; Carr, Taylor, & Robinson, 1991).
The use of telehealth services is one potential solution to the limited access to clinicians with training in FA procedures. Barretto, Wacker, Harding, Lee, and Berg (2006) reported that applied behavior analysts could implement FAs effectively via a telehealth system. Two children with problem behavior were evaluated in either a school setting by school staff or in a department of human services office by a physical therapist and a foster mother. For both evaluations, the behavior analysts were located at a tertiary-level hospital, and the child and staff were at the remote site approximately 100 miles from the hospital. Clear social functions were obtained for both children, thus showing that FAs could be delivered via telehealth by professional staff.
Machalicek et al. (2009) replicated these findings by showing that FAs could be conducted via telehealth. They reported that graduate students who had no previous training in FA could conduct the procedures in the children’s schools when supervised by advanced graduate students. Gibson, Pennington, Stenhoff, and Hopper (2010) showed that FCT conducted via telehealth could be implemented effectively to decrease elopement that had been assessed previously with a brief FA. Both studies showed that behavioral consultation could be provided in a very effective manner via telehealth.
To date, previous studies have demonstrated that FA procedures (a) are adaptable to most applied situations; (b) can be used by parents, teachers, and other educational and professional staff; and (c) are rated as highly acceptable. The purpose of this study was to evaluate the feasibility and effectiveness of conducting FAs via telehealth with 20 young children who had been diagnosed with ASD and who displayed problem behavior at home. All FAs were conducted by parents at regional medical clinics located a short distance from their homes. Parents received live coaching on FA procedures from a behavioral consultant who was housed at the UICH in Iowa City. The participants lived an average of 222 miles from the tertiary-level hospital, but they needed to travel only an average of 15 miles from their homes to obtain telehealth-based FA coaching at a regional clinic (Lindgren &Wacker, 2009). For the purposes of this study, our goal was to conduct FAs (Iwata et al., 1982/1994) as described in our previous in-home projects (Harding, Wacker, Berg, Lee, & Dolezal, 2009; Wacker et al., 1998). Specifically, we evaluated whether parents who had access to these services could conduct the same FA conditions of attention, tangible, escape, and free play effectively without the on-site presence of a skilled behavior analyst. We wanted to investigate whether the procedures would take comparable amounts of time, lead to comparable outcomes (i.e., identified social functions for the target behavior), and be as acceptable to parents as procedures conducted in person in home settings.
METHOD
Participants and Setting
All participants had been referred by clinical staff from the UICH or by nursing staff from one of the five regional Child Health Specialty Clinics (CHSC) that participated in this project. To be eligible for the study, all participants met the following four criteria: (a) They were between the ages of 18 and 83 months at the time of the diagnostic evaluation; (b) they lived within a 50-mile radius of one of five regional medical clinics participating in the study; (c) they displayed problem behavior such as aggression, self-injury, destruction, or disruption; and (d) they met the diagnostic criteria for an ASD. At the beginning of the study, a UICH psychologist completed a comprehensive diagnostic evaluation with each participant consisting of the Autism Diagnostic Observation Schedule (Lord, Rutter, DiLavore, & Risi, 2002), the Autism Diagnostic Interview-Revised (Rutter, Le Couteur, & Lord, 2003), the Vineland Adaptive Behavior Scales (Sparrow, Cicchetti, & Balla, 2005), and the Mullen Scales of Early Learning (Mullen, 1995) to confirm the presence of an ASD. Diagnosis of an ASD was made using the criteria of the Diagnostic and Statistical Manual of Mental Disorders (American Psychiatric Association, 2000) by UICH psychologists who were experienced in assessment of ASD.
Participant Demographic Information
Participants were 20 children between the ages of 29 and 80 months (M = 53.8 months) who lived with one or both of their birth parents. Thirteen participants had been diagnosed with pervasive developmental disorder not otherwise specified (PDD-NOS), and seven had been diagnosed with autistic disorder. All participants had language delays, and communication consisted primarily of gestures with no words for six participants, gestures with some single words for two participants, single words for three participants, phrase speech for eight participants, and fluent speech for one participant. At the time of their enrollment, 16 participants were receiving special education services (e.g., early childhood special education in a preschool, in a special education classroom, or at home), three were in general education preschools or Head Start, 16 were receiving speech and language therapy, 11 were receiving occupational therapy, one was receiving physical therapy, three were receiving respite services, one was receiving supported community living services, two were receiving play therapy, and three were receiving behavior therapy. Participants’ problem behaviors consisted of aggression (e.g., hitting, throwing items at people, kicking, pushing), property destruction (e.g., throwing items, hitting items, kicking items, ripping books), self-injury (e.g., head hitting, head banging, slapping legs, biting self ), disruption (e.g., screaming, elopement), dangerous behavior (e.g., climbing on furniture), and repetitive movements (e.g., dropping to floor and rocking, placing hands over or under clothes around the groin area). Parents reported that their child’s problem behavior affected the family’s ability to participate in many community activities such as eating at restaurants, going to parks, and attending family functions.
Parent Demographic Information
Participants’ parents (19 mothers and one father) served as therapists during all assessment procedures with coaching from a behavior consultant. Parents were an average of 34 years of age. Most parents had a degree beyond high school, and 16 were married or living with the participant’s other parent. Parents had no formal training in behavioral assessment or intervention prior to their participation in this study.
Parent Assistant Demographic Information
The on-site parent assistants were local individuals hired by the regional CHSC nurses to be “family navigators.” The parent assistants were selected based on a self-identified interest in working with young children with autism who engaged in problem behaviors. All parent assistants were female, and their educational background ranged from completion of high school to a master’s degree. None of them had a background in ABA before their participation in this study. They were present in the regional clinic rooms during the FAs to provide on-site support to the parents. They prepared session materials such as toys, conducted safety checks of the clinic room, and provided physical assistance with the participant as needed by the parents. The parent assistant and the behavior consultant met briefly via videoconferencing or telephone before and after each telehealth visit as needed to review the procedures to be conducted, to prepare the room and materials, to discuss the results obtained, and to plan for the next week’s telehealth visit.
Behavior Consultants
Behavior consultants were two trained behavior specialists (second and third authors) who had from 4 to 9 years of experience conducting FAs in children’s homes. One behavior consultant had a bachelor’s degree in special education, and the other was a doctoral candidate in a school psychology program. They were located at the UICH in Iowa City. They trained parent assistants to support parents during telehealth consultations and trained and coached parents to complete FA procedures. Both behavior consultants met with the first author weekly to discuss the results of the FAs.
Regional Clinics
Child Health Specialty Clinics are regional pediatric clinics located throughout Iowa that provide care coordination and health-care services to children and youth with special healthcare needs. Five CHSC sites were selected for inclusion in this study (Council Bluffs, Davenport, Ottumwa, Sioux City, and Spencer) based on the accessibility of reliable high-speed Internet, the availability of support staff, preexisting videoconferencing capabilities, and geographical proximity to rural and underserved communities. The dimensions of the rooms at the five clinics varied, but were approximately 5 m by 5 m. Behavior consultants provided each clinic site with appropriate toys, picture cards, micro-switches, and other materials needed to complete the FAs.
Telehealth Center
Hospital telehealth center site
The behavior consultants directed the FA sessions from the Teleconsultation Center located at the Center for Disabilities and Development, which is part of the UICH. The Teleconsultation Center had four partitioned teleconferencing workstations, with one Windows-based PC with video monitor at each station. Attached to each PC was a basic webcam and headset that could capture and transfer both audio and video from the behavior consultant to the CHSC sites. Prior to each visit, the behavior consultant reviewed feedback from the data-analysis team led by the first author. The consultant then connected through the Internet to the CHSC site prior to the family’s scheduled visit to speak with the parent assistant about room preparation. The desktop PCs used teleconferencing software to connect consultants to the CHSC sites as well as to view and record sessions for subsequent data coding and analysis. The software allowed the consultant to manipulate the camera at the CHSC clinic so that the child and parent remained visible at all times. Recorded sessions were subsequently edited to eliminate periods during which there were no recordable data (e.g., the child was too close to the video monitor for the camera to view). Recordings also had a 6-s interval audio track added to prompt data coding. Recordings were viewed for data coding using playback software that allowed coders to slow down the playback as needed to ensure reliability.
CHSC to Teleconsultation Center connectivity
The CHSC and the Teleconsultation Center were connected via a firewall-protected virtual private network (VPN), and all transmissions were encrypted for security (see Table 1 for a complete listing of equipment).
Table 1.
Telehealth Equipment at Each Clinic Site
| Child Health Specialty Clinic sites (remote clinics): |
| Sony PCS-1600 videoconferencing system with PTZ camera |
| Sony G520 video monitor |
| High-speed Internet connections |
| Teleconsultation Center at the University of Iowa Children’s Hospital: |
| Dell Windows XP workstations |
| 32-in. flat-panel LCD monitors |
| Logitech 600 Webcam |
| Logitech G330 headsets with microphones |
| Emblaze-VCON vPoint HD software |
| VideoLAN VLC media player |
| Windows Movie Maker |
| Internet configurations: |
| Firewalled VPN connection |
| H.235 AES encryption |
| H.323 compatible video connections |
Response Definitions and Data-Recording System
All procedures were recorded digitally using videoconferencing software for data collection and analysis. Trained data collectors at the UICH used a 6-s partial-interval recording system to code data on child behavior from the digital recordings. Problem behavior that was reinforced during the FA was combined and labeled target problem behavior for the purposes of this study. The children’s parents identified behaviors of most concern as target problem behavior; included were aggression, property destruction, self-injury, screaming, elopement, repetitive behavior, and dangerous behavior. Aggression was defined as any behavior that could result in tissue damage to another person (e.g., hitting, kicking, throwing items at the person). Property destruction was defined as any behavior that could result in damage to property (e.g., kicking items, throwing items, ripping books). Self-injury was defined as any behavior that could result in tissue damage to the participant (e.g., head banging, head hitting, biting self, throwing self on floor). Screaming was defined as loud vocalizations that were above conversational level. Elopement was defined as moving or attempting to move away from the parent when instructions were delivered and attempting to leave the clinic room. Repetitive behavior was defined as nonfunctional repetitive movements of body parts or repetitive movement of objects. Repetitive behavior was targeted for only one participant (Jill), for whom it was defined as dropping to the floor and rocking repeatedly and placing her hands over or under her clothing around her groin area. Dangerous behavior was defined as climbing and lying on furniture and leaning or jumping off high surfaces. Passive noncompliance was defined as two or more intervals of passively not completing a task without other problem behavior. Nontargeted problem behavior was recorded and included task refusal, screaming, elopement, passive noncompliance, repetitive behaviors, and dangerous behavior. Task refusal was defined as verbal or gestural refusal to complete a task. Independent manding was defined as requesting reinforcement appropriately without physical guidance or a specific prompt. Toy engagement was defined as physical contact with a toy or eye contact directed toward a book.
During the escape condition of the FA, trained data collectors used an event-recording procedure to record participants’ task completion. Each task was coded as either completed independently (when completed without physical guidance) or not completed independently.
Functional analysis outcomes were defined as the identified function of the FA (i.e., escape, tangible, attention, no function), the number of 5-min sessions to complete the FA, and the number of 1-hr telehealth visits to complete the FA. The focus of this project was on social functions; thus, no test (i.e., alone) condition was conducted to assess an automatic function. Because we wanted to compare the results to previously completed in-home projects, we always included attention, tangible, and escape test conditions.
All data were collected during scheduled weekly visits in which the parents traveled to their regional CHSC and received live coaching from the behavior consultant to assist in conducting the FA. The behavior consultants remotely recorded from three to five (M = 3.76), 5-min sessions during each visit.
Interobserver Agreement
Child behavior
Interobserver agreement of child behavior (6-s data) was collected using an exact interval-by-interval comparison in which the number of agreements was divided by the number of agreements plus disagreements and converting the result to a percentage. Interobserver agreement on child behavior was collected on 30% of sessions and averaged 97% (range, 95% to 99%) across participants.
Interobserver agreement for task completion (event recording) was collected using an exact trial-by-trial comparison in which the number of agreements was divided by the total number of trials and the result was converted to a percentage. Interobserver agreement for task completion was collected on 30% of sessions and averaged 99% (range, 92% to 100%) across participants.
Two trained observers independently inspected the FA data to determine the function of target problem behavior, the number of 5-min sessions to complete each FA, and the number of visits to complete the FA. The observers determined whether the FA identified escape, tangible, attention, or no function for the target problem behavior initially by visual inspection of the data and then according to the procedures described by Roane, Fisher, Kelley, Mevers, and Bouxsein (2013). Interobserver agreement of FA outcomes via visual inspection was assessed for 100% of participants’ FAs and was 100%.
Procedural integrity
Procedural integrity was defined by the following three conditions: (a) having the correct establishing operation (EO) present during the trial (i.e., the presentation of a demand during an escape condition, the removal of attention during an attention condition, the removal of the preferred tangible item during a tangible session, and the availability of attention and tangible item without the presentation of demands during free play); (b) providing the putative reinforcer contingent on target behavior when it occurred during test conditions and the absence of programmed consequences of behavior during free play; and (c) the absence of programmed consequences for any prosocial or nontargeted problem behaviors during test conditions and free play. Procedural integrity was scored if all three conditions were met during any given trial (trials are defined below for the various FA conditions). If any of these three conditions was not met, an integrity error was recorded. Observers also recorded if the parent assistant or consultant made a correction after an integrity error occurred. Correction was defined as any verbal prompt from the parent assistant or behavior consultant to the parent that indicated how to respond correctly to future behavior (e.g., “Next time, we are going to ignore any screaming”). For a correction to be recorded, it must have occurred after an integrity error and before the next instance of a target behavior.
For all participants, procedural integrity was coded for one session of each test and free-play condition (four sessions per participant). Thus, a total of 80 (24%) sessions were coded. Sessions chosen for procedural integrity were conducted approximately at the midpoint of the FA. For example, for conditions during which three sessions were conducted, the second session was used to evaluate procedural integrity. For conditions during which four or more sessions were conducted, a middle session (i.e., not the first or last session) was evaluated for procedural integrity. The beginning of a trial during test conditions (i.e., attention, tangible, escape) was defined as the presentation of the appropriate EO. During free-play sessions, the trials were predetermined arbitrarily; a total of 10 trials were conducted throughout each 5-min free-play session, at the rate of one trial per 30 s. Test condition trials ended following both the completion of the tested reinforcement period and the re-presentation of the EO. If a consequence was not provided for a target behavior, a new trial began during the subsequent 6-s interval when the relevant EO was still in place. Procedural integrity was evaluated by reviewing the digital recordings of each participant and examining the session data sheets. Procedural integrity averaged 96% without corrections and 97% with corrections.
Interobserver agreement on procedural integrity was calculated based on a trial-by-trial comparison in which the number of agreements during procedural integrity sessions was divided by the number of agreements plus disagreements and and the result was converted to a percentage. Interobserver agreement data were collected during two sessions per participant and 10 sessions per condition. Interobserver agreement of procedural integrity was assessed across 50% of the sessions (40 sessions) and was 100%.
Design
This study was conducted in four phases. During Phase 1, the behavior consultants trained the parent assistants via teleconferencing on the principles of behavior analysis, on the study’s purpose and procedures, and on the assistants’ role in supporting the behavior consultant and the parent. During Phase 2, the behavior consultant trained the participant’s parents via teleconferencing on the study’s purpose and procedures and explained that they would implement all procedures with live remote coaching from the behavior consultant and onsite support from the parent assistant. During Phase 3, the behavior consultant interviewed the parent via teleconferencing about the participant’s problem behavior, and the parent completed a daily behavior record for 1 week and implemented a preference assessment as described by Harding et al. (2009). The purpose of Phase 3 was to define the target problem behavior, to develop hypotheses of which situations occasioned problem behavior, and to identify preferred and nonpreferred items to use during the FA. During Phase 4, parents, with coaching from the behavior consultant and onsite support from the parent assistant, conducted an FA (Iwata et al., 1982/1994) within a multielement design as described by Wacker et al. (1998) to identify the maintaining variables of the target problem behavior. One difference in procedures from Wacker et al. (1998) was that parents conducted three or more free-play sessions before any test condition. This change in procedures was made (a) to identify preferred items for inclusion in subsequent conditions (Roane, Vollmer, Ringdahl, & Marcus, 1998) and (b) to acquaint the child and parent with the clinic room. In most cases, neither the parent nor the child had seen the clinic area previously, and thus both needed to acclimate to the area (e.g., become used to the toys, the presence of the parent assistant, and the presence of the video screen that showed the behavior consultant). Following the initial series of free-play sessions, subsequent free-play and test conditions (attention, tangible, and escape) were conducted in a counterbalanced order.
Procedure
Parent assistant training
Behavior consultants met with each parent assistant individually via teleconferencing on two occasions before the parent assistants worked with participants and their parents. During these two meetings, behavior consultants delivered two 1-hr presentations to the assistants on the principles of behavior analysis (e.g., operant behavior, reinforcement, punishment, functional vs. structural approach to problem behavior) and on the project’s specific procedures (i.e., descriptive assessment, preference assessment, FA, and FCT). Before the second training session, behavior consultants provided the parent assistants with a 39-page procedural manual (available from the first author). The manual included flowcharts that outlined the behavior assessment and intervention procedures and the expected timeline for completion of these procedures; one chapter on each assessment and intervention procedure (i.e., descriptive assessment, preference assessment, FA, FCT) including an explanation of the procedure, a rationale for the procedure, case examples, a checklist, and a script the parent assistants could follow during consultations; appendices that contained two forms (daily behavior record, preference assessment form) that assistants gave to parents during the assessment process; and a glossary to familiarize the assistants with the terms used by the behavior consultants.
Behavior consultants asked the parent assistants to read the manual before the second training session so that they would be familiar with the procedures during the presentation and could ask questions. They also explained the assistants’ roles in the project. Assistants were expected to be in the clinic room at all times when the participant was at the regional CHSC to provide on-site support. They were expected to become familiar with the steps and tentative schedule, to know what procedures would be conducted during each telehealth consultation, to ensure that they had the necessary materials (e.g., forms from the appendices, toys) before each telehealth consultation, to ensure that the environment was safe for the participant, to provide physical assistance to the parent as needed, to meet with the behavior consultant before and after each consultation as needed, and to send the behavior consultant needed documents (e.g., completed daily behavior record).
Parent training
Behavior consultants met individually with each participant’s parents during a 1-hr video visit to provide a brief introduction to the project’s procedures (i.e., indirect assessment, preference assessment, FA, FCT training) before conducting the FA. The parents received a 16-page procedural manual (available from the first author) during this meeting. The manual was an abridged version of the parent assistant’s manual and contained flowcharts that outlined the behavior assessment and intervention procedures and the expected timeline for completion of these procedures; one chapter on each assessment and intervention procedure with an explanation of the procedure and a rationale for the procedure; appendices that contained two forms (daily behavior record, preference assessment form); and a glossary to help parents become familiar with the terms used by the behavior consultants.
Parents were encouraged to review this manual before beginning the assessment process with their children to acquaint them with the steps and tentative schedule of the project. They could read about the procedures and their rationale throughout the project by referring to this manual but were not required to do so. They were encouraged to call their consultants if they had any questions about the procedures, the timeline, or any other aspect of the project. During subsequent visits, behavior consultants trained parents to conduct the FA by using the coaching procedures described by Harding et al. (2009).
General Procedure
After arrival at the CHSC clinic, the families were escorted by a parent assistant to a room equipped with videoconferencing equipment. The equipment, housed in a cabinet, consisted of a video monitor connected to a codec with a video camera, much like a home entertainment center. The parent and assistant used the monitor to view and listen to the behavior consultant. The codec and camera captured and transmitted the video and audio from the room. When the family entered the room, the behavior consultant greeted them. At the beginning of each visit, the behavior consultant talked with the parent about the focus of the visit. A common dialogue from the consultant to the parent might consist of the following: “Hello Ms. Smith and Johnny! How has your week been? First we will run the attention condition in which you will be asked to ignore Johnny for a while unless he exhibits the problem behaviors we discussed, at which time you will let Johnny know that he should not do that behavior. You will get him involved in play until I tell you to have him play by himself again.” During the FA sessions, the behavior consultant (on the monitor) was the source of live coaching to aid with procedural integrity as parents conducted the various conditions. A common dialogue from the consultant during an FA condition (e.g., demand) might consist of the following: “You can ask Johnny to point to a picture. Because Johnny is hitting, you can let him know he does not need to point and you can remove the book.” The dialogue needed to prompt the parent was reduced across visits. At the end of the visit, parents were informed of the results and were asked if they had any questions or concerns. When the “all done” and “goodbyes” were finished, the consultant disconnected the video conference.
Assessment procedures conducted prior to functional analyses
Before the FA, three assessments were completed. In the first assessment, the behavior consultant interviewed the parents via telehealth to obtain information about their concerns regarding their child’s behavior and to begin developing operational definitions for the target and nontarget problem behavior. The consultant also asked the parents about the child’s existing method of communication. Finally, the consultant asked the parents how their child’s problem behavior affected the family’s ability to engage in family and community activities to obtain a measure of the problem behavior’s severity. In the second assessment, the parents completed a daily behavior record for 7 days to develop hypotheses about the function of the target problem behavior. The parent assistant faxed these documents to the behavior consultant, and the parent and behavior consultant discussed the data via telehealth. Finally, a preference assessment was conducted to identify preferred and nonpreferred items to use during the FA. Detailed descriptions of the daily behavior record and preference assessment procedures can be found in Harding et al. (2009).
Functional analysis
During the FA, parents conducted four assessment conditions (free play, tangible, attention, and escape) in the CHSC room during an average of 4.9 (range, 4 to 8) 1-hr weekly telehealth visits. As stated previously, we included all three test conditions to compare the results with those obtained in previous in-home studies; this is also why 60-min sessions were scheduled with each family. Parents conducted an average of 3.7 (range, 1 to 6) 5-min sessions during each visit. The parent assistant and the behavior consultant were present during every session of the FA.
Before each 5-min session, the behavior consultant told the parent and parent assistant what condition to conduct, how to respond to target and nontarget problem behavior, how to respond to appropriate behavior, and what materials to present (e.g., task, preferred toy, less preferred toy).
Targeted problem behaviors were identified initially during the parent interview and daily behavior record (e.g., parent report of the child’s hitting) or behaviors that occurred during the FA (e.g., ripping books). Parents were instructed to ignore or to block and ignore nontargeted problem behavior across all conditions. They provided no programmed consequences for manding or other adaptive behavior.
During the free-play condition, the child had access to preferred toys and parent attention. Behavior consultants asked parents to play with their child and to refrain from restricting access to toys or delivering demands. Parents were asked to provide attention at least every 30 s. The behavior consultant instructed them to ignore target problem behavior or, using minimal attention, to block aggression, property destruction, self-injury, or dangerous behavior.
During the tangible condition, the child was allowed to play initially with a preferred toy identified during the preference assessment. After about 30 s of play, the parent removed the preferred toy and gave the child a less preferred toy. Parents were instructed to tell the child, for example, “We are done playing with the [high-preference toy], but you can play with the [low-preference toy]” as they removed the preferred toy. A low-preference toy was used so that the child and parent continued to have toys to play with. If the child engaged in target problem behavior, the parent returned the preferred toy for approximately 20 s. After the reinforcement period, the parent again removed the preferred item.
During the attention condition, the parent and parent assistant diverted their attention from the child. The parent was instructed to tell the child, “You play with the toys; I am going to—.” If the child engaged in target problem behavior, the parent provided both attention in the form of reprimands (e.g., “don’t kick”) and redirection to play for approximately 20 s. After the reinforcement period, the parent again diverted his or her attention from the child.
During the escape condition, the parent prompted the child to complete a task (e.g., point to a picture in a book). The task chosen for the escape condition was easy for the child to complete per parent report, but it was a less preferred activity as identified by the preference assessment. The behavior consultant instructed the parent to deliver the task using a three-step least-to-most prompting sequence: First, the parent verbally told the child what to do (e.g., “Point to the tree”) and then showed the child how to complete the task by modeling (e.g., “Point to the tree” while also gesturing to the tree). If the child did not complete the task after the initial two prompts, the parent physically guided him or her to complete the task (e.g., “Point to the tree” while gently holding the child’s hand and helping him or her point to the tree). If the child engaged in target problem behavior at any time during the prompting sequence, the task was removed for approximately 20 s. After the reinforcement period, the child was prompted to complete a new task.
RESULTS
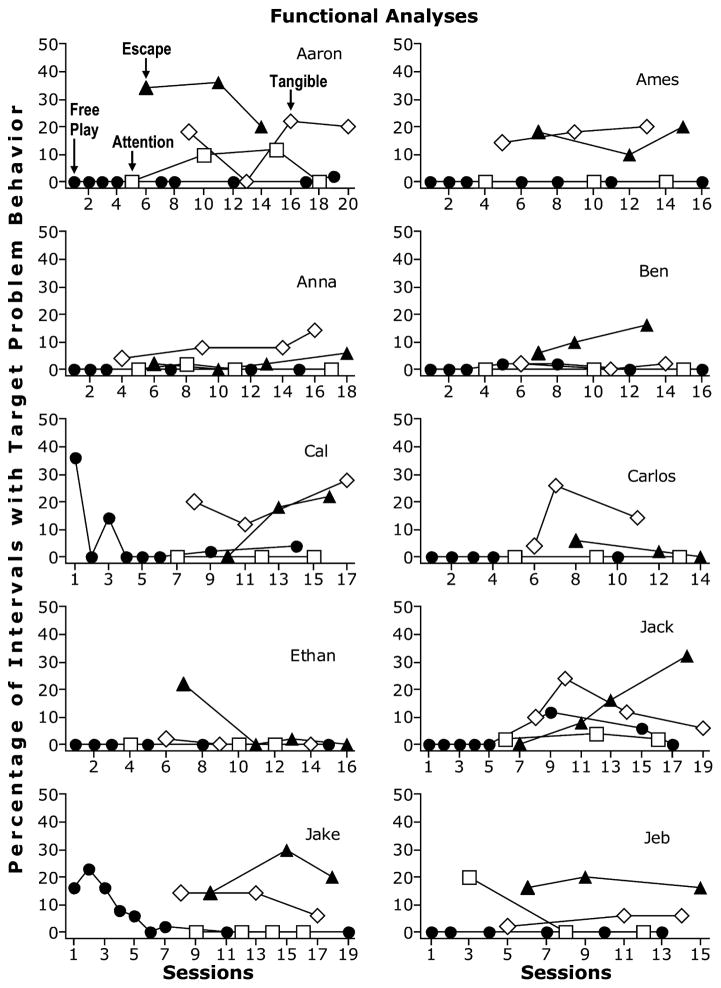
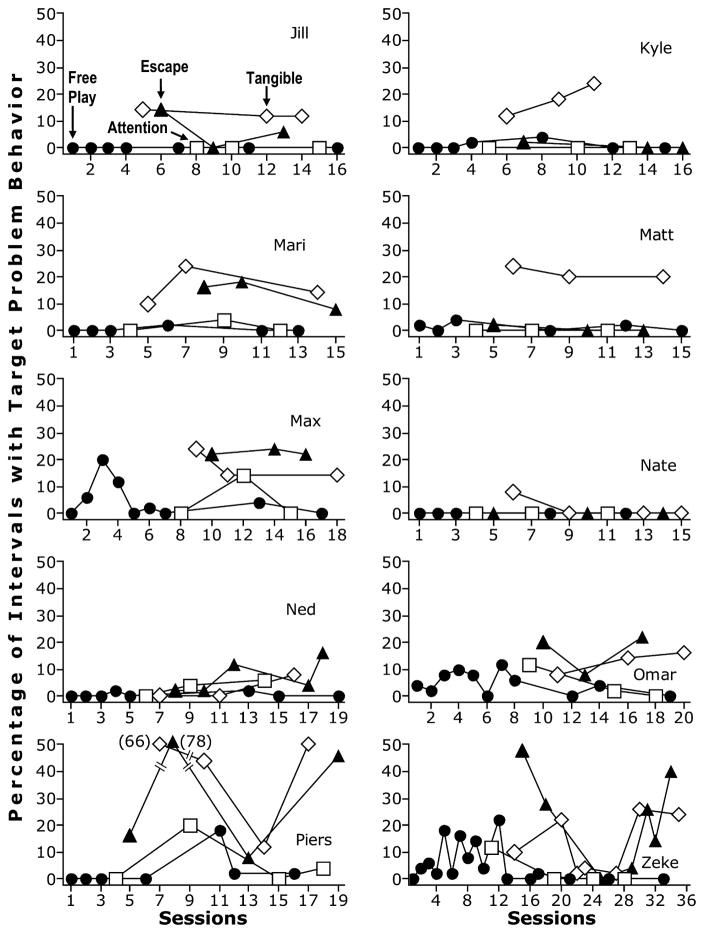
The results of individual FAs are shown in Figures 1 and 2. The average number of 5-min sessions to complete the FAs was 18.1 (range, 14 to 35), and the average number of 1-hr visits was 4.9 (range, 4 to 8). Total time to complete each assessment, including all preparation, follow-up, and graphing, was 270 to 380 min. Eighteen children (90%) had an identified social function during the initial FA. The majority of FAs (13) identified both escape and tangible functions (Aaron, Ames, Anna, Cal, Jack, Jake, Jeb, Jill, Mari, Max, Omar, Piers, and Zeke). An escape function was identified for Ben and Ned, and a tangible function was identified for Carlos, Kyle, and Matt. No functions were identified for Ethan and Nate because of lack of problem behavior. These results are very similar to the results obtained from our previous studies in which FAs were conducted directly in the parents’ homes (e.g., Wacker et al., 1998).
Figure 1.
Results of functional analyses for the first 10 participants.
Figure 2.
Results of functional analyses for the second 10 participants.
When factoring in transportation and clinicians’ time, the costs of delivering FAs via a telehealth delivery model to these 20 participants were significantly lower than if services had been delivered in the participants’ homes. The average weekly cost of delivering FAs via telehealth to these 20 participants was $57.95 per participant. It took approximately 1.5 hr of the parent’s time, 1 hr of the consultant’s time, and 1.5 hr of the parent assistant’s time to conduct FAs with each participant via telehealth. If the behavior consultant had delivered these services in the participants’ homes, the average weekly cost per participant would have been $335.09. On average, it would have taken 1 hr of the parent’s time and over 8 hr of the behavior consultant’s time to travel to and conduct an FA in the home of each participant. The total cost to set up a single video workstation (i.e., telehealth software, hardware, and equipment described in Table 1) at the Teleconsultation Center at UICH was approximately $1,800. The five CHSC sites that participated in this study had preexisting teleconferencing equipment; therefore, no additional costs were incurred for set-up at these remote sites.
In terms of the capacity to identify social functions of problem behavior and the length of assessment, the results of this study were comparable to direct service delivery of FAs in children’s homes. However, the telehealth service delivery model provided a cost-effective alternative strategy for delivering behavioral services.
DISCUSSION
Since the original publication of the FA methodology by Iwata et al. (1982/1994), the heuristic value of this methodology has been demonstrated repeatedly. Results of FA studies have been remarkably consistent across settings; these have included outpatient clinics (Northup et al., 1991), schools (Bloom, Iwata, Fritz, Roscoe, & Carreau, 2011; Sasso et al., 1992), homes (Wacker et al., 1998, 2011), and telehealth (Barretto et al., 2006). The procedures have been shown to be acquired quickly by both college students (Iwata et al., 2000) and parents (Wacker et al., 1998). FA results have led frequently to the identification of highly effective interventions (Asmus et al., 2004; Iwata et al., 1994; Kurtz et al., 2003; Wacker et al., 2011). Few (if any) other behavioral assessments or treatments have consistently demonstrated such direct application across virtually all clinical situations in which they have been applied.
With respect to conducting FAs with children with an ASD diagnosis, comparable findings have been obtained regardless of whether the FA was completed in the home or via telehealth. For example, of the seven children with an ASD in Wacker, Berg, and Harding (2004), social functions were identified for five (71%) when similar assessments were conducted in the home setting. The average number of sessions was approximately 13.7 (range, 10 to 17), and the average number of visits was approximately 4.4 (range, 3 to 6). It took an average of 69 min to complete the FAs for all seven children, and multiple functions were identified for each child. With minor changes, the FA procedures described by Iwata et al. (1982/1994) and others (e.g., Kurtz et al., 2003; Wacker et al., 1998) were completed successfully via telehealth. Of equal importance, parents who had no previous experience with behavior analysis completed the FAs. In addition, parent assistants, who likewise had no behavior analysis backgrounds, aided these parents. The parents and their assistants received only 1 to 2 hr of training prior to conducting the FAs. It is remarkable that, after such a limited amount of training, they successfully completed the analyses in combination with consultation from highly trained and experienced applied behavior analysts.
These results are important because they suggest that telehealth may be useful in increasing the accessibility of FA technology for underserved populations. In this study, we were able to identify a clear social function in the majority of cases while reducing barriers associated with travel and the availability of trained clinicians. These findings contribute to the ongoing clinical need to show the applicability of analogue FAs to a range of applied settings (including homes and schools) and to continue to identify the conditions under which FAs can be implemented most effectively (e.g., Bloom et al., 2011).
Although the current findings are comparable to previous results obtained in children’s homes, our results differed from other studies (e.g., Iwata et al., 1994) in that we found a higher incidence of problem behavior with multiple functions. These differences may be due to the subgroups evaluated, the test conditions included, or the inclusion of specific procedures (e.g., multiple topographies). It is also possible that one or more functions would have been ruled out if we had conducted more sessions (e.g., in the escape condition for Aaron). In addition, an alone condition might have identified an automatic function in some cases (e.g., for Jack). Rooker, Iwata, Harper, Fahmie, and Camp (2011) recommended the inclusion of a tangible condition only if a descriptive history suggested that access to tangible items might be maintaining problem behavior. If this suggestion is followed for all test conditions, it might be possible to make the FAs even more efficient and, thus, more applicable to different situations. However, in spite of these potential limitations, social functions were identified for the majority of the cases, and many of these cases showed tangible functions, either alone or in combination with escape.
Practical issues of cost, convenience, and access to trained professionals are likely to influence the extent to which FAs are implemented more widely. In the current project, although we provided some brief didactic training to the parents and their assistants, it is possible that this was not needed to achieve acceptable outcomes. As discussed by Harding et al. (2009), we provided no didactic training to parents in our in-home projects but instead completed the training via descriptive feedback during each trial. Also, the role of parent assistants in telehealth FAs should be evaluated more directly. Perhaps they were needed only during the first session of each condition or only for families under extreme stress.
Relative to costs, there is little doubt that telehealth is a less expensive alternative to personal consultation, especially when the clinician must travel to the patient’s home. However, the precise savings still need to be considered in each situation. We included only clinic settings that already had access to telehealth services. Factoring in the start-up costs for each clinic site would have increased the costs substantially, especially if newer high-definition teleconferencing equipment was required. In addition, we did not calculate the costs associated with having the consultants meet before and after each session with the parent assistants. Future analyses of telehealth consultation should include a more comprehensive economic analysis.
Finally, if the current results are replicated, the optimal conditions for conducting FAs in hospital, school, or home settings should be evaluated. For example, if a child’s problem behavior occurs in all settings, is there any particular reason to conduct the FA in any specific setting? Or should this decision be a matter of preference and convenience for the parents? In the current project, the greatest expertise in FA procedures was available in the hospital setting. Thus, it was important to have access to those experts even though many of the families who need assistance lived hundreds of miles away.
Each potential setting is likely to provide unique challenges that may require some procedural modifications. For example, Bloom et al. (2011) suggested conducting trial-based FAs in school settings. We also found that multiple free-play sessions were needed for several children before they appeared to adjust to the clinic setting. As FAs continue to be conducted in additional settings and situations, the procedures will need to evolve to adapt to those contexts.
The applied value of FAs in treating severe behavior disorders is difficult to overstate. The next generation of clinical studies needs to assess further the conditions under which FAs can be conducted most effectively and efficiently, and, ultimately, to determine how best to translate those results into interventions that can make a difference in people’s lives. In the current study, FCT was matched to the results of the FA for every child. In each case, FCT proved to be effective in reducing problem behavior, even though only parents conducted treatment procedures with remote consultation from the same behavioral consultants. Studies are now needed to evaluate the effects of treatments such as FCT when they are delivered via telehealth.
Acknowledgments
This investigation was supported by Grant R01-MH89607-02 from the National Institute of Mental Health of the National Institutes of Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Mental Health or the National Institutes of Health. The authors express their appreciation to the families who participated in this investigation, to the nurses and family support staff at the Child Health Specialty Clinics, and to Agnes DeRaad for her assistance with manuscript preparation.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author; 2000. text rev. [Google Scholar]
- Asmus JM, Ringdahl JE, Sellers JA, Call NA, Andelman MS, Wacker DP. Use of a short-term inpatient model to evaluate aberrant behavior: Outcome data summaries from 1996 to 2001. Journal of Applied Behavior Analysis. 2004;37:283–304. doi: 10.1901/jaba.2004.37-283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker BL, McIntyre LL, Blacher J, Crnic K, Edelbrock C, Low C. Preschool children with and without developmental delay: Behavior problems and parenting stress over time. Journal of Intellectual Disability Research. 2003;47:217–230. doi: 10.1046/j.1365-2788.2003.00484.x. [DOI] [PubMed] [Google Scholar]
- Barretto A, Wacker DP, Harding J, Lee J, Berg WK. The use of telemedicine to conduct brief functional analysis and behavioral consultation. Journal of Applied Behavior Analysis. 2006;39:333–340. doi: 10.1901/jaba.2006.173-04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Behavior Analysis Certification Board. Certificant registry. 2012 Retrieved from http://www.bacb.com/index.php?page=100155&by=state.
- Berg WK, Wacker DP, Cigrand K, Merkel S, Wade J, Henry K, Wang YC. Comparing functional analysis and paired choice assessment results in classroom settings. Journal of Applied Behavior Analysis. 2007;40:545–552. doi: 10.1901/jaba.2007.40-545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bloom SE, Iwata BA, Fritz JN, Roscoe EM, Carreau AB. Classroom application of a trial-based functional analysis. Journal of Applied Behavior Analysis. 2011;44:19–31. doi: 10.1901/jaba.2011.44-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carr EG, Taylor JC, Robinson S. The effects of severe behavior problems in children on the teaching behavior of adults. Journal of Applied Behavior Analysis. 1991;24:523–535. doi: 10.1901/jaba.1991.24-523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Prevalence of autism spectrum disorders. Autism and Developmental Disabilities Monitoring Network. 2009 Retrieved from http://www.cdc.gov/mmwr/preview/mmwrhtml/ss5810a1.htm.
- Cooper LJ, Wacker DP, Sasso GM, Reimers TM, Donn LK. Using parents as therapists to evaluate appropriate behavior of their children: Application to a tertiary diagnostic clinic. Journal of Applied Behavior Analysis. 1990;23:285–296. doi: 10.1901/jaba.1990.23-285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derby KM, Wacker DP, Berg W, DeRaad A, Ulrich S, Asmus J, … Stoner EA. The long-term effects of functional communication training in home settings. Journal of Applied Behavior Analysis. 1997;30:507–531. doi: 10.1901/jaba.1997.30-507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibson JL, Pennington RC, Stenhoff DM, Hopper JS. Using desktop videoconferencing to deliver interventions to a preschool student with autism. Topics in Early Childhood Special Education. 2010;29:214–225. doi: 10.1177/0271121409352873. [DOI] [Google Scholar]
- Harding JW, Wacker DP, Berg WK, Lee JF, Dolezal D. Conducting functional communication training in home settings: A case study and recommendations for practitioners. Behavior Analysis in Practice. 2009;2:21–33. doi: 10.1007/BF03391734. NIHMSID 134096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iwata BA, Dorsey MF, Slifer KJ, Bauman KE, Richman GS. Toward a functional analysis of self-injury. Journal of Applied Behavior Analysis. 1994;27:197–209. doi: 10.1901/jaba.1994.27-197. (Reprinted from Analysis and Intervention in Developmental Disabilities, 2, 3–20, 1982) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iwata BA, Pace GM, Dorsey MF, Zarcone JR, Vollmer TR, Smith RG, … Willis KD. The functions of self-injurious behavior: An experimental-epidemiological analysis. Journal of Applied Behavior Analysis. 1994;27:215–240. doi: 10.1901/jaba.1994.27-215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iwata BA, Wallace MD, Kahng S, Lindberg JS, Roscoe EM, Conners J, … Worsdell AS. Skill acquisition in the implementation of functional analysis methodology. Journal of Applied Behavior Analysis. 2000;33:181–194. doi: 10.1901/jaba.2000.33-181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahng S, Iwata BA. Correspondence between outcomes of brief and extended functional analyses. Journal of Applied Behavior Analysis. 1999;32:149–159. doi: 10.1901/jaba.1999.32-149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurtz PF, Chin MD, Huete JM, Tarbox RSF, O’Connor JT, Paclawskyj TR, Rush KS. Functional analysis and treatment of self-injurious behavior in young children: A summary of 30 cases. Journal of Applied Behavior Analysis. 2003;36:205–219. doi: 10.1901/jaba.2003.36-205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindgren SD, Wacker DP. Behavioral treatment for autismin community settings using a telehealth network. Washington, DC: Department of Health and Human Services, National Institute of Mental Health; 2009. [Google Scholar]
- Lord C, Rutter M, DiLavore PC, Risi S. Autism Diagnostic Observation Schedule (ADOS) Los Angeles, CA: Western Psychological Services; 2002. [Google Scholar]
- Machalicek W, O’Reilly MF, Chan J, Lang R, Rispoli M, Davis T, … Didden R. Using videoconferencing to conduct functional analysis of challenging behavior and develop classroom behavior support plans for students with autism. Education and Training in Developmental Disabilities. 2009;44:207–217. [Google Scholar]
- Mullen E. Mullen Scales of Early Learning. Bloomington, MN: Pearson Assessments; 1995. [Google Scholar]
- Northup J, Wacker D, Sasso G, Steege M, Cigrand K, Cook J, DeRaad A. A brief functional analysis of aggressive and alternative behavior in an outclinic setting. Journal of Applied Behavior Analysis. 1991;24:509–522. doi: 10.1901/jaba.1991.24-509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oliver C, Petty J, Ruddick L, Bacarese-Hamilton M. The association between repetitive, self-injurious and aggressive behavior in children with severe intellectual disabilities. Journal of Autism and Developmental Disorders. 2012;42:910–919. doi: 10.1007/s10803-011-1320-z. [DOI] [PubMed] [Google Scholar]
- Roane HS, Fisher WW, Kelley ME, Mevers JL, Bouxsein KJ. Using modified visual-inspection criteria to interpret functional analysis outcomes. Journal of Applied Behavior Analysis. 2013;46:131–146. doi: 10.1002/jaba.13. [DOI] [PubMed] [Google Scholar]
- Roane HS, Vollmer TR, Ringdahl JE, Marcus BA. Evaluation of a brief stimulus preference assessment. Journal of Applied Behavior Analysis. 1998;31:605–620. doi: 10.1901/jaba.1998.31-605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers S, Wallace K. Intervention for infants and toddlers with autism spectrum disorders. In: Amaral D, Dawson G, Geschwind D, editors. Autism spectrum disorders. Oxford, UK: Oxford University Press; 2011. pp. 1081–1094. [Google Scholar]
- Rooker GW, Iwata BA, Harper JM, Fahmie TA, Camp EM. False-positive tangible outcomes of functional analyses. Journal of Applied Behavior Analysis. 2011;44:737–745. doi: 10.1902/jaba.2011.44-737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutter M, Le Couteur A, Lord C. Autism Diagnostic Interview–Revised (ADI-R) Los Angeles, CA: Western Psychological Services; 2003. [Google Scholar]
- Sasso GM, Reimers TM, Cooper LJ, Wacker D, Berg W, Steege M, … Allaire A. Use of descriptive and experimental analyses to identify the functional properties of aberrant behavior in school settings. Journal of Applied Behavior Analysis. 1992;25:809–821. doi: 10.1901/jaba.1992.25-809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sparrow SS, Cicchetti DV, Balla DA. Vineland Adaptive Behavior Scales. 2. Bloomington, MN: Pearson Assessments; 2005. [Google Scholar]
- Tiger JH, Hanley GP, Bruzek J. Functional communication training: A review and practical guide. Behavior Analysis in Practice. 2008;1:16–23. doi: 10.1007/BF03391716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wacker DP, Berg WK, Harding JW. Maintenance effects of functional communication training. Washington, DC: Department of Health and Human Services, National Institute of Child Health and Human Development; 2004. [Google Scholar]
- Wacker DP, Berg WK, Harding JW, Barretto A, Rankin B, Ganzer J. Treatment effectiveness, stimulus generalization, and acceptability to parents of functional communication training. Educational Psychology. 2005;25(2–3):233–256. doi: 10.1080/0144341042000301184. [DOI] [Google Scholar]
- Wacker DP, Berg WK, Harding JW, Derby KM, Asmus JM, Healy A. Evaluation and long-term treatment of aberrant behavior displayed by young children with disabilities. Journal of Developmental and Behavioral Pediatrics. 1998;19:260–266. doi: 10.1097/00004703-199808000-00004. [DOI] [PubMed] [Google Scholar]
- Wacker DP, Harding JW, Berg WK, Lee JF, Schieltz KM, Padilla YC, … Shahan TA. An evaluation of persistence of treatment effects during long-term treatment of destructive behavior. Journal of the Experimental Analysis of Behavior. 2011;96:261–282. doi: 10.1901/jeab.2011.96-261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallace MD, Iwata BA. Effects of session duration on functional analysis outcomes. Journal of Applied Behavior Analysis. 1999;32:175–183. doi: 10.1901/jaba.1999.32-175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson TS, Sterling HE. Brief functional analysis and treatment of a vocal tic. Journal of Applied Behavior Analysis. 1998;31:471–474. doi: 10.1901/jaba.1998.31-471. [DOI] [PMC free article] [PubMed] [Google Scholar]