Abstract
Objective
We investigated the association between socioeconomic factors and the attainment of treatment goals and pharmacotherapy in patients with type 2 diabetes in Denmark.
Design
A cross-sectional population study.
Setting
The municipality of Naestved, Denmark.
Subjects
We studied 907 patients with type 2 diabetes identified from a random sample of 21,205 Danish citizens.
Main outcome measures
The proportion of patients who were not achieving goals for diabetes care based on their HbA1c, LDL-cholesterol, blood pressure, and lifestyle, and the proportion of patients who were treated with antihypertensive and cholesterol- and glucose-lowering medication.
Methods
We investigated the association of the socioeconomic factors such as age, gender, education, occupation, income, and civil status and attainment of treatment goals and pharmacotherapy in logistic regression analyses. We investigated effect modification of cardiovascular disease and kidney disease.
Results
Middle age (40–65 years), low education level (i.e. basic schooling), and low household income (i.e. less than 21,400 € per year) were associated with nonattainment of goals for diabetes care. The association of socioeconomic factors with attainment of individual treatment goals varied. Patients with low socioeconomic status were more often obese, physically inactive, smoking, and had elevated blood pressure. Socioeconomic factors were not associated with treatment goals for hyperglycemia. Socioeconomic factors were inconsistently associated with pharmacotherapy. There was no difference in contacts to general practitioners according to SES.
Conclusions
In a country with free access to health care, the socioeconomic factors such as middle age, low education, and low income were associated with nonattainment of goals for diabetes care.
Key points
Middle age, low education, and low income were associated with nonattainment of goals for diabetes care, especially for lifestyle goals.
Patients with low socioeconomic status were more often obese, physically inactive, smoking, and had elevated blood pressure.
Association of socioeconomic factors with pharmacotherapy was inconsistent.
Keywords: Type 2 diabetes mellitus, health care, general practice, socioeconomic status, lifestyle, Denmark
Introduction
Epidemiological studies have repeatedly confirmed association between incidence of type 2 diabetes mellitus (T2DM) and low socioeconomic status (SES) [1]. Mortality rates have fallen substantially, primarily due to effective pharmacotherapy and multifactorial diabetes interventions [2]. However, trends have been reported less favorable among patients with low SES even in countries with equal access to health care [3,4]. Associations between low SES and mortality in patients with T2DM have not been fully explained [5,6]. Reduced survival could be imputed to differences in the attainment of treatment goals and a lower level of pharmacotherapy among patients with low SES [6]. Patients with low SES may have difficulty bearing the costs of the multidrug regimens in T2DM [7], and medication adherence in general has been reported to be influenced by SES [7–9]. Adherence to recommended lifestyle changes could be a challenge for people with low SES [10]. Studies suggest that differences in clinical profiles between different SES groups are not the result of treatment, but rather that lifestyle factors are major contributors to these findings in Western countries [11]. It has been argued that drug coverage and differences in cardiovascular disease (CVD) burden are influenced by universal access to prescription drugs [3]. Despite the near universal health-care coverage in most European countries (including Denmark), income-related inequality in the use of physician services has been observed [12]. In a recent Danish study, the number of consultations for patients with diabetes with their general practitioner (GP) increased with decreasing SES [13]. Moreover social differences in the quality of diabetes care can be modified [10].
The aim of this study was to investigate how social disparity affects the attainment of treatment goals and pharmacotherapy in patients with T2DM in a country (Denmark) with universal health care.
Materials and methods
Setting
This study was part of the cross-sectional study named the Danish General Suburban Population Study (GESUS). GESUS was conducted in the Danish Naestved Municipality, with approximately 80,000 inhabitants and a mix of urban and rural settings. GESUS was implemented to facilitate epidemiological research, and analyzes the occurrence of comorbidities (e.g. T2DM), mortality, and to derive new knowledge of risk factors. The study design has been reported elsewhere [14].
The Danish health-care system is mainly tax-financed and based on the egalitarian principle of equal health-care access for equal health-care needs. In Denmark, patients with high expenditure on prescription drugs (e.g. patients suffering from T2DM) are for the most part compensated through the system. Diagnosis and routine care for T2DM are usually provided by GPs, who function as gatekeepers for specialist care and are responsible for more than 90% of all prescriptions [15].
Study population
GESUS recruited subjects from January 2010 through October 2013. The criteria for inclusion were Danish citizenship and residency in the Naestved Municipality. The GESUS researchers contacted all people over 30 years of age and a computer-generated 25% random selection of the population aged 20–30 years by mail and invited them to participate by attending a health examination. If individuals had not responded within 3 weeks of their scheduled attendance period, a reminder was sent with a new scheduled period. The total study population was 21,205 (43.2% of the 49,115 people invited to participate), and 20,876 individuals completed a health examination and a questionnaire. Participants were predominantly of Danish or other Scandinavian descent (98.9%) [14].
Questionnaire
A paper-form questionnaire, similar to those used for the Copenhagen City Heart Study (CCHS) and the Copenhagen General Population Study (CGPS) [16], was issued at the beginning of the examination and was a prerequisite for attending the health examination. The questionnaire was tested in a pilot-study involving 60 volunteers and it was reviewed and revised for understandability and relevance.
Patients with T2DM were identified as those participants who answered yes to one of the following questions: “Do you have diabetes?” or “Are you being treated with glucose-lowering medication?”. We excluded patients with Type 1 diabetes mellitus, which was defined as patients with insulin-treated diabetes diagnosed before the age of 30. Patients recorded age of onset of DM and whether they had been in contact with their GP or hospitalized in the prior 12 months. Patients with CVD were identified as people who reported a diagnosis of myocardial infarction, stroke, ischemic heart disease, or who suffered from angina pectoris. Information regarding treatment with antihypertensive, cholesterol, and glucose-lowering drugs was recorded in the questionnaire. Participants answered questions about lifestyle including current smoking status and level of physical activity. Physical activity was classified in accordance with international and national guidelines for patients suffering from T2DM [17,18]. Patients were labeled physically inactive if they answered: “Passive or less than 2 h of light activity per week” or “Light physical activity (i.e. walking, garden work) for 2–4 h per week”. Patients were classed as physically active if they answered: “More than 4 h of light physical activity” or “Strenuous workout (sweating and breathing hard) for 2–4 h per week”.
Information on socioeconomic factors was also collected in the questionnaire including highest attained educational level: Only basic schooling (<12 years of primary, secondary, and high-school); vocational training (1–3 years); short academic (1–3 years); long academic (>3 years e.g. university degree), civil status, total annual household-income, and occupation; working: Employed, self-employed or assisting spouse; welfare benefits: Unemployed, long-term sick leave, early retirement for health reasons, homemaker; and retired: senior citizen (the Danish retirement age was 67 years).
Health examination
All GESUS participants had their blood pressure (BP) measured after 5-min rest, two consecutive measurements performed on the left upper arm (apparatus type A&D UA-787, A&D Medical, Tokyo, Japan), and the second was registered. Weight and height were measured and BMI was calculated. Fresh blood samples were drawn in a nonfasting state and analyzed for HbA1c, estimated glomerular filtration rate (eGFR) [19] and low-density lipoprotein cholesterol (LDL) calculated from the Friedewald equation [20].
Outcome
We defined nonattainment of goals for T2DM based on the following six criteria: hyperglycemia (HbA1c >58 mmol/mol, or >7.5%), hyperlipidemia (LDL >2.5mmol/L), elevated BP (systolic-BP >140 mm Hg), obesity (BMI >30kg/m2) [21], current smoking, and physical inactivity as defined by responses in the corresponding questionnaire.
GESUS was approved by the appropriate Institutional Review Boards and Ethical Committees (SJ-113, SJ-114) and reported to the Danish Data Protection Agency. Written informed consent was obtained from all participants. The investigation conforms to the principles of the Declaration of Helsinki.
Statistics
We used the statistical program SAS 9.4 (SAS Institute, Cary, NC). Distribution of variables is shown as frequencies with percentages (categorical variables), or means with SD, (continuous variables).
We assessed the association between the socioeconomic variables and the various aspects of diabetes care and the use of pharmacotherapy as an odds ratio (OR) from logistic regression models. In these models, the socioeconomic factors were used, each in separate analyses, as independent variables, and each goal for diabetes care or the use of pharmacotherapy as binary dependent variable. These analyses were adjusted for gender and age (in three age groups as shown in Table 1). In analyses with household income, civil status was also adjusted for.
Table 1.
Characteristics, medication, and goals for diabetes care for 907 patients with T2DM.
| N (%) or {SD} | Missing | |
|---|---|---|
| Men, N (%) | 510 (56.2) | – |
| Age, mean {SD} | 64.7 {10.9} | – |
| 25–40 years, N (%) | 28 (3.1) | – |
| >40–65 years, N (%) | 398 (43.9) | |
| >65 years, N (%) | 481 (53.0) | |
| Treatment, N (%) | ||
| Lifestyle only | 165 (18.6) | – |
| Glucose-lowering medication not insulin | 543 (61.1) | 18 |
| Insulin | 181 (20.4) | 52 |
| Cholesterol-lowering medication, N (%) | 579 (65.4) | 22 |
| Antihypertensive medication, N (%) | 605 (68.3) | 21 |
| Cardiovascular disease, N (%) | 177 (20.5) | 43 |
| Kidney disease (eGFR <49 L/min/1.73 m2) | 95 (10.5) | 35 |
| Diabetes duration years {SD} | 9.0 {8.2} | 259 |
| Socioeconomic status | ||
| Education, N (%) | 14 | |
| Basic-schooling (<12 years)a | 247 (27.7) | |
| Vocational training (1–3years) | 358 (40.1) | |
| Short academic (<3 years) | 86 (11.6) | |
| Long academic (>3 years, e.g. university) | 202 (22.6) | |
| Occupation, N (%) | 21 | |
| Employed | 280 (31.6) | |
| Welfare benefits | 127 (14.3) | |
| Retired | 479 (54.1) | |
| Household income, N (%)c | 127 | |
| <21,400 € | 97 (12.4) | |
| 21,400–42,700 € | 240 (30.8) | |
| 42,700–85,570 € | 307 (39.4) | |
| >85,570 € | 136 (17.4) | |
| Civil status, N (%) | – | |
| Married/cohabiting | 658 (72.6) | |
| Living single | 249 (27.5) | |
| Goals for diabetes care | ||
| Smoking, N (%) | 156 (17.5) | 14 |
| Hyperglycemia | ||
| HbA1c, mean {SD} mmol/mol | 51.8 {12.4} | 11 |
| HbA1c not in goal (>58 mmol/mol), N (%) | 223 (24.6) | 11 |
| Hypertension | ||
| Systolic BP, mean {SD} mmhg | 145.5 {20.8} | 3 |
| Systolic BP not in goal (>140 mm hg), N (%) | 547 (60.3) | 3 |
| Hyperlipidemia | ||
| LDL, mean {SD} mmol/L | 2.3{0.84} | 57 |
| LDL not in goal (>2.5 mmol/L), N (%) | 328 (38.6) | 57b |
| Obesity | ||
| BMI, mean {SD} kg/m2 | 30.3{5.3} | 10 |
| Obese (BMI >30 kg/m2), N (%) | 421 (46.9) | 10 |
| Physically inactive, N (%) | 599 (69.9) | 50 |
| Number of treatment goals met (of 6), N (%) | 117 | |
| 6 (All treatment goals met) | 22 (2.8) | |
| 5 | 111 (14.0) | |
| 4 | 242 (30.6) | |
| 3 | 260 (32.9) | |
| 2 | 127 (16.1) | |
| 1 | 25 (3.2) | |
| 0 (No treatment goals met) | 3 (0.4) | |
Basic schooling includes primary, secondary, and high-school.
Blood sample missing, poor quality or too high triglyceride level (>4.4 mmol/L) to calculate LDL value using the Friedewald equation.
1 € = 7 dkr.
In order to investigate which of the socioeconomic factors were most detrimental for diabetes care, we calculated a measure for relative importance as the average increase in McFadden’s R2 [22], (i.e. the proportional reduction in error variance which corresponds to the addition of a factor to a logistic regression model across all multivariable logistic regression models that can be constructed from the remaining factors). This procedure partitions the R2 in a model with all factors into the contributions of the individual factors, and the relative importance is therefore reported as a percentage.
As a sensitivity analysis, we investigated the association between socioeconomic factors and missing values for specific treatment goals and diabetes duration. We investigated whether additional adjustment for CVD, the presence of kidney disease (eGFR <49 L/min/1.73 m2), and medication could explain an association between SES and nonattainment of goals. We also investigated effect modification by CVD or kidney disease on the association between SES and nonattainment of goals.
Finally, we investigated how contact to GP and hospitalization was associated with SES.
Results
Table 1 depicts baseline characteristics of the 907 patients with known T2DM. A small proportion of the patients met all (2.8%), or all but one (14%), of their treatment goals for T2DM care, while 415 (45.8%) did not meet three or more of the six treatment goals for diabetes care. Overall 50% of the patients were obese, 24.6% had HbA1c above 58 mmol/mol, 38.6% had LDL levels above 2.5 mmol/l, and 60.3% had elevated systolic BP.
There were few missing values (5.5%) among the clinical measurements (BMI, BP) and biochemical values (HbA1c, LDL), and these were not associated with socioeconomic factors (Supplementary Table S1). In comparison, the self-reported data had more missing values and we found missing values for physical exercise to be associated with education (p = 0.029) and income (p = 0.047) and missing information regarding cholesterol-lowering therapy to be associated with living single (Supplementary Table S2), but otherwise we could not demonstrate missing values to be associated with SES. Missing values for diabetes duration was overall high (29%), but not associated with SES, and the reported diabetes duration was significantly associated with age and occupation (Supplementary Table S3).
Attainment of treatment goals
Gender
Compared to men, women less physically active, had lower odds of attaining LDL goals, and higher odds of attaining glycemic (HbA1c) goals (Table 2) even though they were less likely to receive antidiabetic medication (Table 3), but overall men and women did not differ on goals for diabetes care.
Table 2.
Socioeconomic factors and not attaining goals for diabetes care, numbers, percentage, and odds ratio (OR).
| N = 907, OR (CI 95%) | Smoking,N (%) | SmokingOR (CI) | Hyperlipidemia(LDL >2.5 mmol/L),N (%) | HyperlipidemiaOR | Hyperglyce-mia(HbA1c>58 mmol/mol),N (%) | HyperglycemiaOR (CI) | Hypertension(systolicBP >140 mmHg),N (%) | HypertensionOR (CI) | Obese(BMI >30 kg/m2),N (%) | ObeseOR (CI) | Physicallyinactive,N (%) | Physicallyinactive,OR (CI) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Gender | ||||||||||||
| Male | 93 (15.9) | 1 | 165 (34.7) | 1 | 141 (28.0) | 1 | 312 (61.2) | 1 | 232 (45.9) | 1 | 320 (66.4) | 1 |
| Female | 63 (15.8) | 0.79 (0.55–1.14) | 163 (43.6) | 1.39 (1.05–1.83)c | 82 (20.9) | 0.69 (0.51–0.95)c | 235 (59.2) | 1.02 (0.77–1.34) | 189 (48.3) | 1.12 (0.86–1.46) | 279 (74.4) | 1.58 (1.16–2.14)c |
| Age | ||||||||||||
| >25–40 years | 8 (28.6) | 3.19 (1.34–7.66)c | 17 (60.7) | 3.01 (1.36–6.63)c | 3 (10.7) | 0.49 (0.15–1.67) | 4 (14.3) | 0.08 (0.03–0.23)c | 8 (28.6) | 0.50 (0.21–1.15) | 13 (46.4) | 0.30 (0.14–0.65)c |
| >40–65 years | 90 (22.6) | 2.15 (1.49–3.08)c | 160 (43.5) | 1.46 (1.11–1.93)c | 115 (29.4) | 1.47 (1.08–2.00)c | 216 (54.3) | 0.56 (0.42–0.74)c | 203 (51.4) | 1.34 (1.03–1.75)c | 273 (70.5) | 0.98 (0.72–1.32) |
| >65 years | 58 (12.1) | 1 | 151 (33.3) | 1 | 105 (22.0) | 1 | 327 (68.0) | 1 | 210 (44.3) | 1 | 313 (70.8) | 1 |
| Education | ||||||||||||
| Basic schooling | 41 (16.6) | 1.19 (0.71–2.00) | 101 (43.2) | 1.30 (0.88–1.93) | 59 (24.2) | 0.98 (0.64–1.53) | 157 (63.6) | 1.42 (0.96–2.10) | 128 (52.2) | 1.16 (0.80–1.69) | 173 (79.0) | 1.72 (1.10–2.67)c |
| Vocational training | 67 (18.7) | 1.18 (0.74–1.89) | 118 (34.9) | 0.87 (0.60–1.26) | 93 (26.2) | 1.04 (0.70–1.55) | 225 (62.9) | 1.60 (1.12–2.30)c | 152 (42.8) | 0.78 (0.55–1.11) | 229 (66.2) | 0.96 (0.66–1.40) |
| Short academic | 12 (14.0) | 0.86 (0.42–1.78) | 33 (41.8) | 1.10 (0.65–1.86) | 18 (20.9) | 0.79 (0.43–1.46) | 50 (58.1) | 1.25 (0.74–2.11) | 37 (44.1) | 0.78 (0.47–1.31) | 58 (69.1) | 1.04 (0.59–1.80) |
| Long academic | 32 (15.8) | 1 | 71 (38.2) | 1 | 51 (25.8) | 1 | 107 (53.0) | 1 | 97 (48.7) | 1 | 132 (66.7) | 1 |
| Incomea | ||||||||||||
| <21,400 € | 19 (19.6) | 3.04 (1.24–7.44)c | 37 (39.4) | 1.08 (0.57–2.06) | 25 (26.3) | 1.68 (0.83–3.41) | 72 (74.2) | 2.13 (1.08–4.17)c | 54 (55.7) | 2.21 (1.18–4.14)c | 67 (79.8) | 2.26 (1.09–4.71)c |
| 21,400–42,700 € | 38 (15.8) | 2.69 (1.26–5.73)c | 82 (36.4) | 1.03 (0.61–1.71) | 62 (25.9) | 1.39 (0.80–2.41) | 149 (62.1) | 1.11 (0.67–1.84) | 103 (43.5) | 1.22 (0.74–2.00) | 153 (67.7) | 1.21 (0.72–2.04) |
| 42,700–85,570 € | 61 (19.9) | 2.54 (1.32–4.89)c | 117 (41.3) | 1.08 (0.70–1.67) | 73 (24.1) | 0.89 (0.56–1.43) | 179 (58.3) | 1.15 (0.75–1.76) | 149 (49.2) | 1.32 (0.87–2.02) | 215 (70.7) | 1.47 (0.94–2.29) |
| >85,570 € | 13 (9.9) | 1 | 52 (40.3) | 1 | 39 (19.6) | 1 | 70 (51.5) | 1 | 59 (43.7) | 1 | 83 (61.9) | 1 |
| Occupationb | ||||||||||||
| Working | 52 (18.6) | 1 | 116 (44.1) | 1 | 76 (27.4) | 1 | 138 (49.3) | 1 | 141 (50.5) | 1 | 186 (67.6) | 1 |
| Welfare benefits | 33 (26.0) | 1.61 (0.97–2.68) | 56 (47.9) | 1.06 (0.68–1.63) | 35 (28.2) | 1.07 (0.66–1.73) | 74 (58.3) | 1.43 (0.93–2.21) | 67 (53.2) | 1.05 (0.69–1.62) | 92 (76.7) | 1.45 (0.88–2.40) |
| Retired | 62 (12.9) | 150 (33.2) | 105 (22.1) | 323 (67.4) | 204 (43.2) | 306 (68.9) | ||||||
| Civil status | ||||||||||||
| Married/cohabiting | 94 (14.3) | 1 | 222 (36.2) | 1 | 173 (26.5) | 1 | 392 (59.6) | 1 | 303 (46.5) | 1 | 427 (68.2) | 1 |
| Living single | 62 (24.9) | 2.40 (1.64–3.51)c | 106 (32.3) | 1.45 (1.06–1.97)c | 50 (20.5) | 0.78 (0.54–1.13) | 155 (62.3) | 1.06 (0.77–1.45) | 118 (48.0) | 1.06 (0.79–1.44) | 172 (74.5) | 1.25 (0.88–1.78) |
Percentages differ because of different numbers of missing. OR analysis: adjusted for gender and age (in the three age groups).
Analysis on income, adjusted in addition for civil status (1 € = 7 dkr).
In analysis “working vs. welfare benefits”, excluding retired people (n = 423).
p < 0.05.
Table 3.
Socioeconomic factors and odds ratio (or) for no pharmacotherapy.
| OR (CI 95%) | Not in glucose-loweringmedication, N = 889 | Not in insulin therapy, N = 855 | Not in antihypertensivemedication, N = 886 | Not in cholesterol-lowering medication, N = 885 |
|---|---|---|---|---|
| Gender | ||||
| Male | 1 | 1 | 1 | 1 |
| Female | 1.64 (1.13–2.35)c | 1.05 (0.74–1.48) | 1.15 (0.84–1.57) | 0.94 (0.69–1.27) |
| Age | ||||
| 25–40 years | 8.20 (3.57–18.87)c | 3.04 (0.70–13.17) | 22.50 (6.54–77.36)c | 18.43 (5.39–63.00)c |
| >40–65 years | 1.35 (0.93–1.96) | 0.84 (0.59–1.18) | 2.07 (1.51–2.84)c | 1.57 (1.15–2.13)c |
| >65 years | 1 | 1 | 1 | 1 |
| Education | ||||
| Basic schooling (<12 years) | 0.71 (0.43–1.18) | 1.16 (0.72–1.87) | 0.82 (0.53–1.27) | 0.84 (0.55–1.29) |
| Vocational training (1–3 years) | 0.76 (0.48–1.19) | 1.33 (0.86–2.07) | 0.81 (0.54–1.22) | 0.79 (0.54–1.17) |
| Short academic(<3 years) | 0.60 (0.30–1.21) | 1.06 (0.57–1.99) | 0.67 (0.37–1.23) | 0.95 (0.54–1.66) |
| Long academic (>3 years) | 1 | 1 | 1 | 1 |
| Household incomea | ||||
| <21,400 € | 0.79 (0.33–1.94) | 0.74 (0.34–1.64) | 0.76 (0.36–1.60) | 0.75 (0.37–1.53) |
| 21,400–42,700 € | 0.99 (0.51–1.94) | 0.74 (0.40–1.36) | 0.75 (0.43–1.32) | 0.83 (0.48–1.45) |
| 42,700–85,570 € | 1.06 (0.61–1.84) | 0.95 (0.56–1.61) | 0.58 (0.36–0.92)c | 0.74 (0.47–1.17) |
| >85,570 € | 1 | 1 | 1 | 1 |
| Occupationb | ||||
| Working | 1 | 1 | 1 | 1 |
| Welfare benefits | 0.54 (0.29–1.01) | 0.61 (0.36–1.06) | 0.53 (0.32–0.87)c | 0.76 (0.47–1.23) |
| Civil status | ||||
| Married/cohabiting | 1 | 1 | 1 | 1 |
| Living single | 0.94 (0.63–1.41) | 1.31 (0.89–2.02) | 0.99 (0.69–1.41) | 1.62 (1.15–2.29)c |
| Cardiovascular disease | ||||
| Yes | 1 | 1 | 1 | 1 |
| No | 1.20 (0.74–1.96) | 1.33 (0.81–2.00) | 3.93 (2.34–6.58)c | 3.68 (2.30–5.88)c |
| Kidney disease | ||||
| Yes | 1 | 1 | 1 | 1 |
| No | 1.28 (0.66–2.47) | 1.34 (0.78–2.29) | 1.59 (0.88–2.90) | 1.11 (0.65–1.88) |
OR analysis adjusted for gender, age (3 age groups), CVD and kidney disease (eGFR < 49 L/min/1.73 m2) (1 € = 7 dkr).
Analysis on income, adjusted in addition for civil status.
In the analysis “working vs. welfare benefits”, excluding retired people (n = 423).
p < 0.05.
Age
Compared to individuals >65 years, younger individuals had higher odds for smoking and LDL >2.5 mmol/l and lower odds for having elevated BP. Individuals in the age group 25–40 years were more physically active and had overall better regulated T2DM even though they were less likely to receive pharmacotherapy, whereas the age group 40–65 years were more obese and were less well regulated with attainment of the HbA1c-goal compared to patients above 65 years.
Education
Compared to individuals with long academic education, individuals with only basic schooling were less well regulated; however, odds ratios for individual goals or pharmacotherapy did not differ.
Income
Compared to individuals with the highest income, lower income groups were less well regulated, had higher odds ratios for smoking, had higher odds ratio for elevated blood pressure, were less likely to be physically active, and more likely to be obese. Inconsistent results were found for the association of income with pharmacotherapy.
Occupation
Compared to employed individuals, those unemployed did not differ on the diabetes goals or regulation, but were more likely to receive antihypertensive medication.
Civil status
Compared to married/cohabiting individuals, individuals living single were more often smokers, had higher odds ratios for LDL >2.5 mmol/l, and were less likely to receive cholesterol-lowering medication.
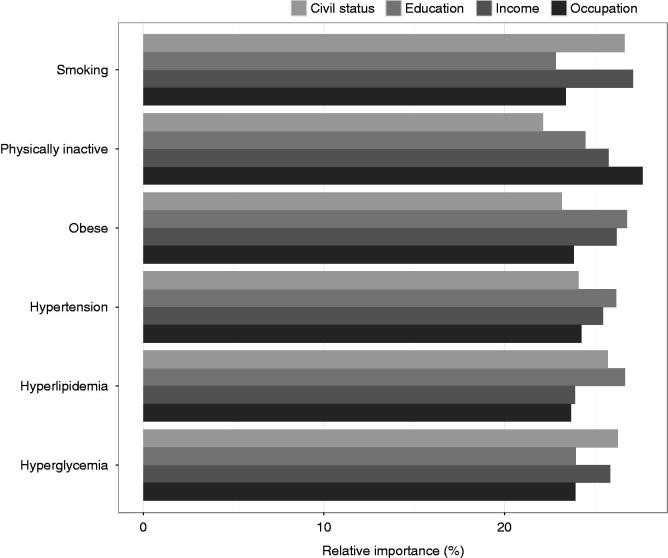
Overall, the relative importance of the socioeconomic factors such as civil status, education, income, and occupation for attainment of the different treatment goals was between 20% and 29% but varied according to specific treatment goal (Figure 1).
Figure 1.
Relative importance of socioeconomic factors in nonattainment of goals for diabetes care (e.g. the most important socioeconomic factor for smoking is income).Notes: A measure for relative importance was calculated as the average increase in McFadden’s R2 (see “Statistics” section), adjusted for gender and age. Smoking: Current smoker. Physically inactive (see text). Obese (BMI >30kg/m2). Hypertension (systolic BP >140 mmHg). Hyperlipidemia (LDL >2.5mmol/l). Hyperglycemia (HbA1c >58 mmol/mol (>7.5%)).
Additional adjustment for CVD and kidney disease Supplementary Table S4 or adjustment for medication (Supplementary Table S5) could not explain the association between SES and not attaining goals for diabetes care. Moreover could we not show any evidence of effect modification.
We could not show any significant difference according to socioeconomic group on whether the patients had been in contact with their GP the last year (Table 4). However, hospitalizations were increased among patients who were female, aged 25–40 years old, with low income, and with cardiovascular or kidney disease.
Table 4.
Socioeconomic factors, CVD, and kidney disease and association with hospitalization and contact with the GP in the last 12 months.
| Hospitalization in last 12 months N (174), 30 missing N (%) |
Hospitalization in last 12 months OR (CI 95%) |
Contact with GP in last 12 months N (836), 19 missing N (%) |
Contact with GP in last 12 months OR (CI 95%) |
|
|---|---|---|---|---|
| Gender | ||||
| Male | 83 (16.3) | 1 | 473 (92.8) | 1 |
| Female | 91 (22.9) | 1.61 (1.12–2.30)* | 363 (91.4) | 1.25 (0.68–2.29) |
| Age | ||||
| 25–40 years | 9 (32.1) | 2.62 (1.10–6.22)* | 23 (82.1) | 0.38 (0.10–1.42) |
| >40–65 years | 76 (19.1) | 1.30 (0.90–1.88) | 361 (90.7) | 0.65 (0.35–1.20) |
| >65 years | 89 (18.5) | 1 | 452 (94.0) | 1 |
| Education | ||||
| Basic schooling (<12 years) | 51 (20.7) | 1.12 (0.68–1.83) | 224 (90.7) | 1.23 (0.55–2.77) |
| Vocational training (1–3 years) | 64 (17.9 | 0.90 (0.57–1.43) | 332 (92.7) | 1.41 (0.68–2.92) |
| Short academic(<3 years) | 15 (17.4) | 0.97 (0.49–1.91) | 81 (94.2) | 1.23 (0.42–3.57) |
| Long academic (>3 years) | 40 (19.8) | 1 | 187 (92.6) | 1 |
| Household incomea | ||||
| <21,400 € | 20 (20.6) | 3.15 (1.26–7.85)* | 86 (88.7) | 1.15 (0.30–4.33) |
| 21,400–42,700 € | 53 (22.1) | 3.79 (1.78–8.07)* | 219 (91.3) | 0.99 (0.36–2.73) |
| 42,700–85,570 € | 61 (19.9) | 3.01 (1.54–5.88)* | 292 (95.1) | 1.76 (0.73–4.29) |
| >85,570 € | 13 (9.6) | 1 | 124 (91.2) | 1 |
| Occupationb | ||||
| Working | 43 (15.4) | 1 | 253 (90.4) | 1 |
| Welfare benefits | 32 (25.2) | 1.57 (0.89–2.77) | 119 (93.7) | 1.95 (0.71–5.38) |
| Retired | 97 (20.3) | – | 448 (93.5) | – |
| Civil status | ||||
| Married/cohabiting | 123 (18.7) | 1 | 613 (93.2) | 1 |
| Living single | 51 (20.5) | 1.05 (0.71–1.57) | 223 (89.6) | 0.55 (0.30–1.02) |
| Cardiovascular disease | ||||
| Yes | 50 (28.3) | 2.15 (1.42–3.25)* | 172 (97.2) | 2.79 (0.97–8.01) |
| No | 116 (16.9) | 1 | 628 (91.4) | 1 |
| Kidney disease | ||||
| Yes | 34 (35.8) | 2.80 (1.71–4.59)* | 89 (93.7) | 0.98 (0.34–2.86) |
| No | 140 (17.2) | 1 | 747 (92.0) | 1 |
Odds ratio (OR) from logistic regression models adjusted for gender, age (3 age groups), CVD and kidney disease.
*p < 0.05.
Income analysis also adjusted for civil status.
In the analysis “working vs. welfare benefits”, excluding retired people (n = 423).
CVD: cardiovascular disease; GP: general practitioner.
Discussion
Statement of principal findings
Our data show that among patients with T2DM, ascertained in a general population study in Denmark, approximately 50% are obese and hypertensive, but have on average good glycemic control. We showed that middle age (40–65 years), low education level (i.e. basic schooling), and low income were associated with nonattainment of goals for diabetes care. The association of socioeconomic factors with attainment of individual treatment goals varied. Patients with low SES were more often obese, physically inactive, smoking, and had elevated blood pressure patients. Socioeconomic factors were not associated with treatment goals for hyperglycemia. We could not show any consistent findings for the association between socioeconomic factors and pharmacotherapy. There were no effect modifications of CVD and kidney disease on the association of SES and nonattainment of goals. There was no difference in contacts to GPs according to SES.
Strengths and limitations
This study is a large, cross-sectional study, with a mixed invitation pattern (by gender, age, and residence) throughout the study period. The overall participation rate in GESUS (43%) resembles that of other general population studies in Europe that vary from 10% to 72% [23]. We have previously assessed selection bias among participants vs. nonparticipants [14] and found that nonparticipants had a higher prevalence of diabetes and CVD, higher percentage of men and individuals not living in a relationship being on average 4 years younger than participants. A recent, British investigation [24] has argued that there is a socioeconomic gradient on attendance, with socially deprived groups being less likely to attend. Thus, nonparticipants may be more diseased and have a worse SES status than participants, which could lead to conservative estimates in our study.
The paper used self-reported data both on socioeconomic factors, disease history, lifestyle, and medication, which in general might be difficult to report. This may cause risk of information bias and risk of both under- and overreporting. SES data, medication, and disease history might be difficult to report correct which may be a source of recall bias, selective bias, and social desirability [24]. We showed that for physical activity there is an increased number of missing values among patients with low education and low income. Also, in a cross-sectional study, we cannot tell if treatment was sufficient and if the patients adhere to all aspect of pharmacotherapy (time of day, dose, or take the medication every day). In comparison to the self-reported data, there were few missing values (5.5%) among the clinical measurements (BMI, blood pressure) and biochemical values (HbA1c, LDL). We did not have access to the Danish registries on diagnoses or medication, but this information could have improved especially details on pharmacotherapy (generic and brand names).
We used relatively conservative treatment goals for diabetes care, although these are fairly consistent with other studies [25]. Even so, we could demonstrate a relatively large proportion of patients not attaining goals. These findings must be viewed in light of the fact that participants included had no upper age limit and no limitations on comorbid disease, resembling patients in the general public treated in GP.
The association between achievement of treatment goals and higher income could be explained by a group of patients with a relatively low “disease burden” having the capacity to work and to earn more (“the healthy worker effect”). Cross-sectional studies, like this, only have a single time point estimate, and thus can only describe prevalence and not infer risk or causality or prediction.
Findings in relation to other studies
A comparison of the participants of GESUS, a mixed rural and urban population, with a more uniformly urban population (CGPS) showed that GESUS participants are less physically active, have fewer current smokers, higher anthropometric measures (BMI), and a higher prevalence of undiagnosed diabetes and hypertension [14]. This indicates that patients with T2DM in more rural areas could have a different risk profile compared to diabetes patients in more urban environments.
A study by Dalsgaard et al. found that consultation rates with the GP were higher for newly diagnosed T2DM-patients with the lowest SES [13]. In our study, we could not demonstrate any association between SES group and contact to the general practitioner. This result is in accordance with our finding that socioeconomic factors were inconsistently associated with pharmacotherapy could be interpreted as equality in the delivery of health care for patients with diabetes [6]. In this study, however, we did not have any information on why patients consulted the general practitioner, thus, there could be unexplained, hidden reasons for consulting GP varying according to SES groups.
We found that patients living single were more often smokers, had higher odds ratios for LDL >2.5 mmol/l, and were less likely to receive cholesterol-lowering medication. This finding is in accordance with previous studies, suggesting that living with a partner may provide support to the adaptation to lifestyle changes and adherence to medical treatment [9].
In particular, lifestyle factors differed between SES groups, which is in line with other studies [8,11]. We found that SES was not associated with attainment of goals for HbA1c and that 24% did not meet treatment goals for hyperglycemia; this is better than the results from a recent large European study finding that among people treated for T2DM 58.5% achieved the glycated hemoglobin (HbA1c) target of <7.0% [21]. Patients with low SES seem to have a similar ratio of drug treatment in concordance with other studies [11,26], although different observations have been made [13] – especially in other health-care systems.
Explanation of the findings and implications for future research on clinical practice
Our data show, that even in a country with a universal health-care system, socioeconomic factors such as education level and low income were associated with nonattainment of goals for diabetes care. The lack of attainment of treatment goals for diabetes care among patients with low SES may be interpreted as related to lifestyle factors and not delivery of health care as pharmacotherapy (a proxy for delivery of health care) overall and contact to GP were not associated with SES. However, other factors related to diabetes care – organization and treatment schemes [6,27] and adaption, which we did not assess, could also contribute to the results [10,26,28]. Our study emphasizes the need for future, prospective intervention studies [29] targeted on SES in patients with T2DM to improve glycemic control and cardiovascular risk factors.
Supplementary Material
Acknowledgements
The authors extend their appreciation to participants of GESUS, the board and executive committee, especially Jan Kvetny, MD, dr.med.sci; employees at Naestved Hospital, Region Zeeland. Ole Heltberg, MD, contributed in fruitful discussions.
Funding Statement
This study was supported Region Zealand Research Fund, Copenhagen University Faculty of Health Sciences and by University of Copenhagen 2016 Excellence program to LIFESTAT. The Danish General Suburban Population Study was founded by the Region Zealand Foundation; Naestved Hospital Foundation; Johan and Lise Boserup Foundation; TrygFonden; Johannes Fog’s Foundation; Region Zealand; Naestved Hospital; Naestved Kommune; The National Board of Health; and the Local Government Denmark Foundation.
Ethical approval
GESUS was approved by the appropriate Institutional Review Boards and Ethical Committees (SJ-113, SJ-114, SJ-147, SJ-278), and was reported to the Danish Data Protection Agency.
Disclosure statement
All authors declare they have no conflicts of interest.
References
- 1.Espelt A, Arriola L, Borrell C, et al. . Socioeconomic position and type 2 diabetes mellitus in Europe 1999–2009: a panorama of inequalities. Curr Diabetes Rev. 2011;7:148–158. [DOI] [PubMed] [Google Scholar]
- 2.Green A, Sortso C, Jensen PB, et al. . Incidence, morbidity, mortality, and prevalence of diabetes in Denmark, 2000–2011: results from the Diabetes Impact Study 2013. Clin Epidemiol. 2015;7:421–430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Booth GL, Bishara P, Lipscombe LL, et al. . Universal drug coverage and socioeconomic disparities in major diabetes outcomes. Diabetes Care. 2012;35:2257–2264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bachmann MO, Eachus J, Hopper CD, et al. . Socio-economic inequalities in diabetes complications, control, attitudes and health service use: a cross-sectional study. Diabet Med. 2003;20:921–929. [DOI] [PubMed] [Google Scholar]
- 5.Walker J, Halbesma N, Lone N, et al. . Socioeconomic status, comorbidity and mortality in patients with type 2 diabetes mellitus in Scotland 2004–2011: a cohort study. J Epidemiol Community Health. 2016;70:596–601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rawshani A, Svensson AM, Zethelius B, et al. . Association between socioeconomic status and mortality, cardiovascular disease, and cancer in patients with type 2 diabetes. JAMA Intern Med. 2016;176:1146–1154. [DOI] [PubMed] [Google Scholar]
- 7.Sundquist K, Chaikiat A, Leon VR, et al. . Country of birth, socioeconomic factors, and risk factor control in patients with type 2 diabetes: a Swedish study from 25 primary health-care centres. Diabetes Metab Res Rev. 2011;27:244–254. [DOI] [PubMed] [Google Scholar]
- 8.Walker RJ, Gebregziabher M, Martin-Harris B, et al. . Independent effects of socioeconomic and psychological social determinants of health on self-care and outcomes in Type 2 diabetes. Gen Hosp Psychiatry. 2014;36:662–668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Trivedi RB, Ayotte B, Edelman D, et al. . The association of emotional well-being and marital status with treatment adherence among patients with hypertension. J Behav Med. 2008;31:489–497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Baz L, Muller N, Beluchin E, et al. . Differences in the quality of diabetes care caused by social inequalities disappear after treatment and education in a tertiary care centre. Diabet Med. 2012;29:640–645. [DOI] [PubMed] [Google Scholar]
- 11.Rabi DM, Edwards AL, Svenson LW, et al. . Clinical and medication profiles stratified by household income in patients referred for diabetes care. Cardiovasc Diabetol. 2007;6:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.van Doorslaer E, Koolman X, Jones AM.. Explaining income-related inequalities in doctor utilisation in Europe. Health Econ. 2004;13:629–647. [DOI] [PubMed] [Google Scholar]
- 13.Dalsgaard EM, Vedsted P, Fenger-Gron M, et al. . Socioeconomic position and contact to general practice among persons with diabetes. Prim Care Diabetes. 2012;6:313–318. [DOI] [PubMed] [Google Scholar]
- 14.Bergholdt HK, Bathum L, Kvetny J, et al. . Study design, participation and characteristics of the Danish General Suburban Population Study. Dan Med J 2013;60:A4693. [PubMed] [Google Scholar]
- 15.Sorensen HT. Regional administrative health registries as a resource in clinical epidemiology: a study of options, strengths, limitations and data quality provided with examples of use. Int J Risk Saf Med. 1997;10:1–22. [DOI] [PubMed] [Google Scholar]
- 16.Ellervik C, Mandrup-Poulsen T, Andersen HU, et al. . Elevated transferrin saturation and risk of diabetes: three population-based studies. Diabetes Care. 2011;34:2256–2258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.de Backer G, Ambrosioni E, Borch-Johnsen K, et al. . European guidelines on cardiovascular disease prevention in clinical practice. Third Joint Task Force of European and Other Societies on Cardiovascular Disease Prevention in Clinical Practice. Eur Heart J 2003;24:1601–1610. [DOI] [PubMed] [Google Scholar]
- 18.Goff DC Jr., Lloyd-Jones DM, Bennett G, et al. . 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63:2935–2959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Levey AS, Coresh J, Greene T, et al. . Expressing the modification of diet in renal disease study equation for estimating glomerular filtration rate with standardized serum creatinine values. Clin Chem. 2007;53:766–772. [DOI] [PubMed] [Google Scholar]
- 20.Nordestgaard BG, Benn M.. Fasting and nonfasting LDL cholesterol: to measure or calculate? Clin Chem. 2009;55:845–847. [DOI] [PubMed] [Google Scholar]
- 21.Kotseva K, de Bacquer D, de Backer G, et al. . Lifestyle and risk factor management in people at high risk of cardiovascular disease. A report from the European Society of Cardiology European Action on Secondary and Primary Prevention by Intervention to Reduce Events (EUROASPIRE) IV cross-sectional survey in 14 European regions. Eur J Prev Cardiol. 2016. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 22.Mittlbock MMS. Explained variation in logistic regression. Statist Med. 1996;15:1987–1997. [DOI] [PubMed] [Google Scholar]
- 23.Hofman A, van Duijn CM, Franco OH, et al. . The Rotterdam Study: 2012 objectives and design update. Eur J Epidemiol. 2011;26:657–686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Marteau TM, Mann E, Prevost AT, et al. . Impact of an informed choice invitation on uptake of screening for diabetes in primary care (DICISION): randomised trial. BMJ. 2010;340:c2138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bedard D, Shatenstein B, Nadon S.. Underreporting of energy intake from a self-administered food-frequency questionnaire completed by adults in Montreal. PHN. 2004;7:675–681. [DOI] [PubMed] [Google Scholar]
- 26.Dalsgaard EM, Vestergaard M, Skriver MV, et al. . Socioeconomic position and cardiovascular risk factors among people with screen-detected Type 2 DM: six-year follow-up of the ADDITION-Denmark trial. Prim Care Diabetes. 2014;8:322–329. [DOI] [PubMed] [Google Scholar]
- 27.van Doorn-Klomberg AL, Braspenning JC, Wolters RJ, et al. . Organizational determinants of high-quality routine diabetes care. Scand J Prim Health Care. 2014;32:124–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Guthrie B, Emslie-Smith A, Morris AD.. Which people with Type 2 diabetes achieve good control of intermediate outcomes? Population database study in a UK region. Diabet Med. 2009;26:1269–1276. [DOI] [PubMed] [Google Scholar]
- 29.Thulesius H. Why are standardized lifestyle interventions for the metabolic syndrome not successful? Experiences from two RCTs and one mixed-methods study. Scand J Prim Health Care. 2015;33:55–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.