Abstract
Background:
Spine surgery in elderly with comorbidities is reported to have higher complication rates and increased cost. However, the surgical outcome is good irrespective of the complications. Hence, it is essential to identify the factors affecting the complication rates in such patients and the measures to reduce them. This retrospective observational study determines the perioperative complications, their incidence and the measures to reduce complications in the elderly with comorbidities, operated by instrumented multilevel lumbar fusion.
Materials and Methods:
Patients aged 60 years and above with one or more comorbidities operated by multilevel instrumented lumbar fusion in our center between January 2012 and December 2013 were included in the study. Perioperative complications and their incidence were calculated. Age, number of levels fused, operative time, blood loss, and complication rates were correlated with the duration of stay and the incidence of perioperative complications using SPSS software. Measures to reduce complications are determined by these results and by review of literature.
Results:
Fifty two patients were included in the study (28 females and 24 males) with an average age of 69 years (range 60-84 years). Hypertension was the most common comorbidity followed by diabetes. Spondylolisthesis was the most common indication. Eleven complications were noted with an incidence of 21%. Three were systemic complications which required transfer to Intensive Care Unit. Local complications were incidental durotomy (three), transient root deficits (two), wound infections (one), and persistent radicular pain (two). Operative time and blood loss were significantly higher in patients with complications.
Conclusion:
Complication rates strongly correlate with the blood loss and operative time. Reducing the operative time and blood loss by intraoperative tranexamic acid, laminectomy using osteotome, simultaneous bilateral exposure and instrumentation and reducing the number of interbody fusions can help in reducing the complications.
Keywords: Comorbidities, lumbar fusion, geriatrics, spine
MeSH terms: Geriatrics, spinal fusion, degenerative diseases, spondylolisthesis, lumbar vertebrae
INTRODUCTION
Geriatric population is on rise globally because of increasing life span. As per the US Census, people above 60 years constituted 6.4% of the total population in 1900, which increased to 18.4% in 2010 and predicted to go up to 25.5% by 2050.1 Spinal problems and spine surgeries in geriatric population are also showing a similar trend. Lumbar fusion surgeries in people aged 60 years and above have increased by 230% in a decade from 1991 to 2001.2 Desire to lead a more active life in advanced age, improved diagnostic techniques, and better operative results are some of the reasons for increasing spine surgeries in the elderly. In general, spine surgery in the elderly in the presence of comorbidities is feared among both patients and surgeon, as it is presumed to have higher perioperative complications and increased cost. However, surgical outcomes are good if complications are low. Many articles can be found in literature supporting this.3,4,5 A study by Daubs et al. involving adult spinal deformity in people over 60 years of age has reported that age and complication rates do not affect the surgical outcome.6 Similar studies have reported 91%–96% good to excellent results following surgical treatment of lumbar canal stenosis (LCS) by decompression and decompression with fusion on people aged above 65–70 years.7,8,9 This indicates that in the absence of complications, spinal decompression and fusion surgeries would result in a satisfied patient even in the elderly with comorbidities. Therefore, measures to reduced complications in such patients should be looked at rather than denying surgical management in symptomatic patients due to their old age or comorbidities. This study evaluates the perioperative complications and the contributing factors in patients over 60 years of age undergoing lumbar fusion surgeries.
MATERIALS AND METHODS
Patients aged 60 years and above with one or more comorbidities undergoing lumbar decompression and instrumented fusion at our institute between January 2012 and December 2013 (2-year period) were included in the study. In all these patients, perioperative complications (intraoperative and complications occurring within 3 weeks postoperative period) and their incidence were recorded. The technique was a standard open technique of pedicle screw instrumentation and fusion, either interbody by transforaminal approach or posterolateral using morcellized bone from the posterior elements or rarely with iliac crest. No minimally invasive, endoscopic, or paraspinal techniques were employed. Age, number of levels instrumented and fused, operative time, blood loss, comorbidities, and the duration of stay were correlated with the incidence of perioperative complications using SPSS software (IBM, SPSS Statistics V 23.0, New York, United States). Factors contributing to perioperative complications were noted and measures to reduce them were suggested by these results and compared with the available literature in discussion.
RESULTS
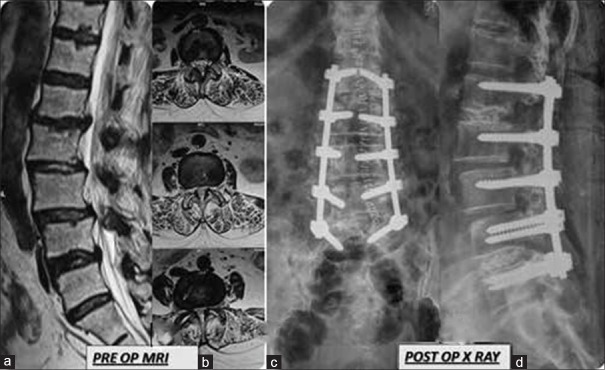
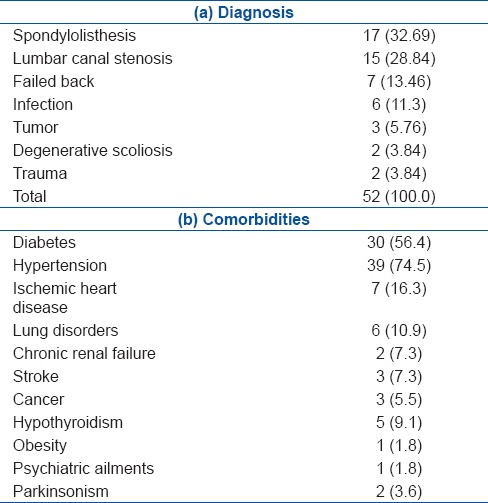
Analysis of our medical records revealed a total of 52 patients operated by lumbar fusions in the 2-year study period, who were aged 60 years and above and had one or more comorbidities. There were 28 females and 24 males [Figure 1]. The average age was 69 years (range 60-84 years). Most common indication for surgery was spondylolisthesis in 17 (32.7%) followed by LCS in 15 (28.8%) patients. Hypertension (HTN) was the most common comorbidity found in 39 patients (75%), followed by diabetes mellitus (Type 2) in thirty patients (56.4%). Twenty patients had single comorbidity while 18 patients had two comorbidities and 13 patients were found to have three comorbidities [Table 1].
Figure 1.
Preoperative MRI T2W, midsagittal (a) and axial (b) images showing multilevel listhesis and canal stenosis. Postoperative x-ray lumbosacral spine anteroposterior (c) and lateral (d) views showing implant (pedicle screws) in situ following instrumented fusion
Table 1.
Diagnosis and comorbidites of patients
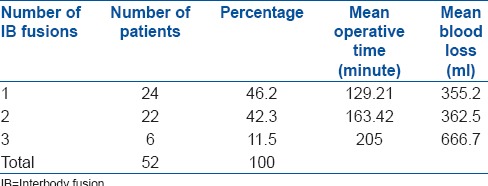
Forty six patients were operated under general anesthesia (GA) while the remaining six patients were operated in regional or spinal anesthesia. 3.8 levels were the average levels instrumented per patient while one patient underwent 9 levels instrumentation. Interbody fusions were performed at single level in 24, 2 levels in 22, and 3 levels in 6 patients. Posterolateral fusions were performed at the remaining instrumented levels [Table 2]. Average operative time and blood loss were 150 min (range 60–270 min) and 369 ml (range 90–1050 ml), respectively. Both operative time and blood loss increased with additional levels of instrumentation and interbody fusions [Table 3]. The levels of instrumentation and fusions were decided on segmental instability observed on dynamic radiographs. The interbody fusions were based on degree of segmental stenosis, disc degeneration, and instability.
Table 2.
Clinical details of patients
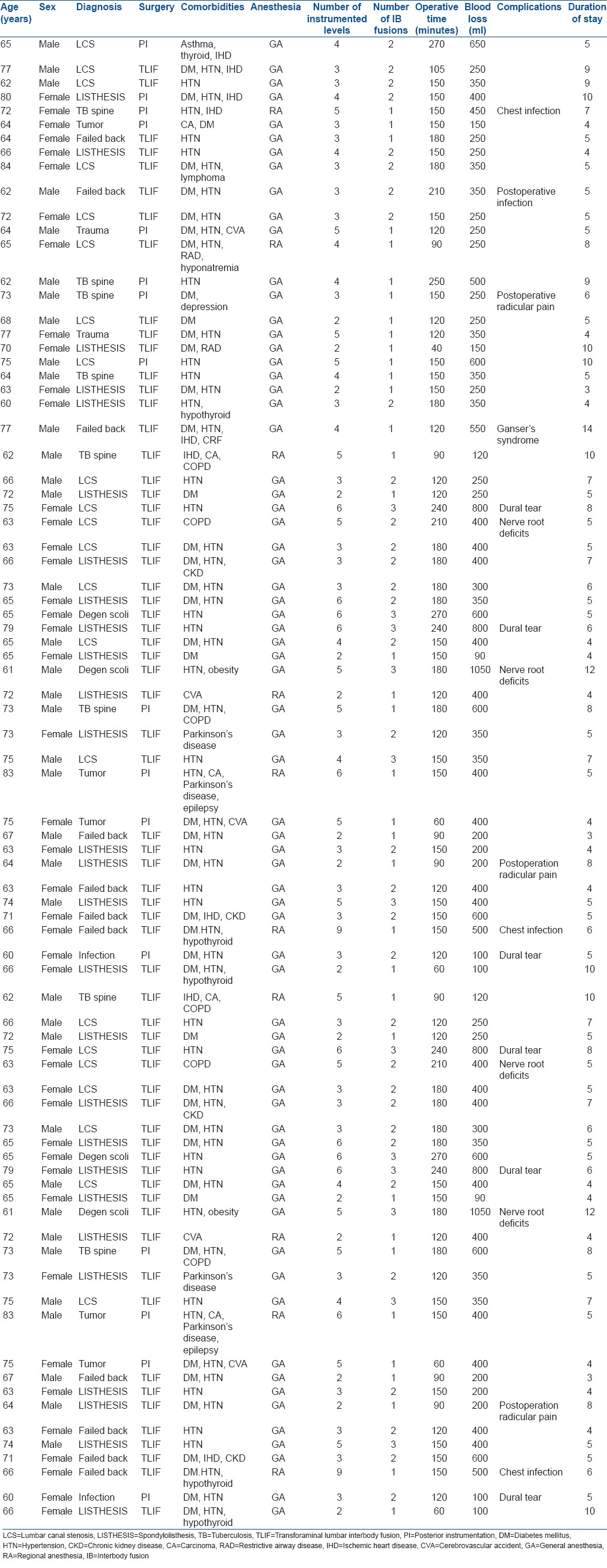
Table 3.
Operative time and blood loss with respect to the number of interbody fusion levels
A total of 11 complications were noted, 3 systemic and 8 local. Among the systemic complications, 2 were hypostatic pneumonia with secondary infection and one was a psychiatric illness called Ganser's syndrome. All the three patients required transfer to ICU and one patient with pneumonia expired due to septicemia and shock. The average total duration of stay in the hospital was 6.2 days (range 4-14 days). On comparing the complication rates with other variables, we found that the patients with complications had higher blood loss, operative time, number of instrumented levels, and number of interbody fusion levels [Tables 4 and 5]. Similarly, the duration of stay was longer in these patients. On analyzing these results statistically by ANOVA, the association of blood loss with complications was found to be statistically significant with P = 0.002. The duration of stay, operative time, and number of interbody fusion levels were close to significance with P = 0.63, 0.58, and 0.61, respectively, while number instrumented levels and the number of associated comorbidities showed no significance [Tables 4 and 5].
Table 4.
The complications and their incidence
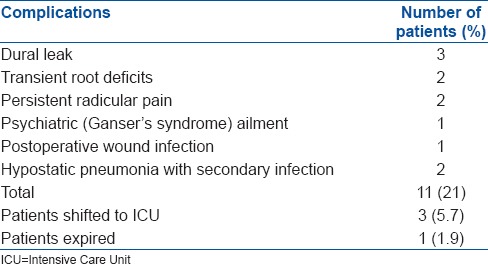
Table 5.
Comparisons of different variables in patients with and without complications
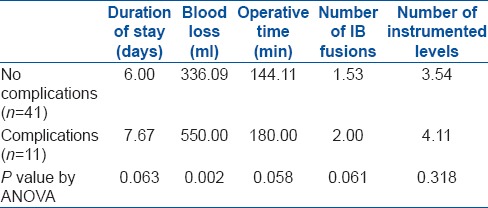
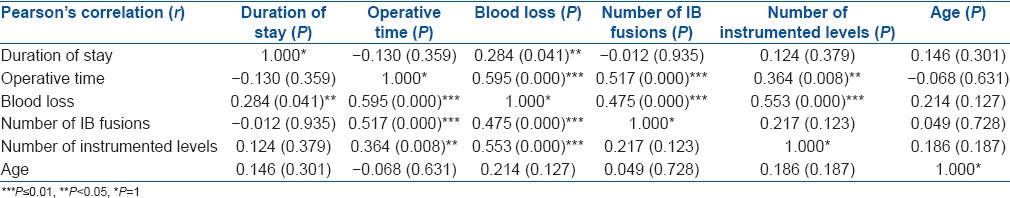
On analyzing the correlations between different variables, we found that there was a strong positive correlation of blood loss with operative time, number of instrumented levels, and number of interbody fusions which was statistically significant. Similarly, operative time showed a strong positive correlation with number of interbody fusions and a significant but a weaker positive correlation with number of instrumented levels [Table 6].
Table 6.
Correlations (±) between different variables and their statistical significance
DISCUSSION
The perioperative complication rates in the present study occurred in 11 of 52 patients with an incidence of 21%. Increased blood loss strongly correlated with the incidence of complications. Age, operative time, number of levels of fusion, and the duration of stay were also more in patients with complications and were close to statistical significance while number of instrumented levels and number of associated comorbidities were unrelated to the complication rates. Perioperative complication rates in instrumented lumbar fusions in patients above 60 years of age described in literature range from 29% to 62% [Table 7]. The factors influencing the incidence of complications are controversial. Cho et al. and Carreon et al. reported increased complications in patients with advanced age and surgeries with increased blood loss and number of levels of fusions.11,12 Carreon et al.11 found increased complication rates with increased operative time while Cho et al.12 found no such association. Guigui et al.10 found comorbidities to influence the complication rates and a similar study by Acosta et al.4 found ten times higher complication rates in patients with HTN while others found no association between comorbidities and the perioperative complications.6,12
Table 7.
The incidence of complications and factors affecting it described in the literature
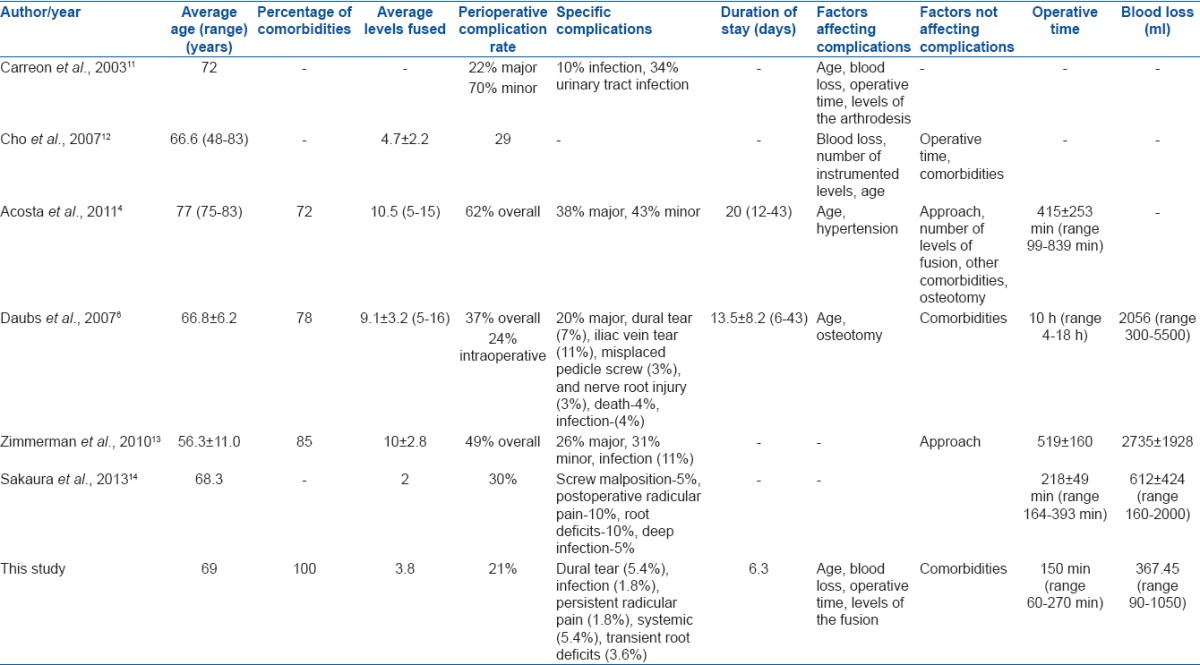
Considering the group of population included, the complication rate in our series was within the acceptable limits compared to literature [Table 7].4,6,11,12,13,14 Our patients were 60 years and above with the average age of 69 years, all of them had one or more comorbidities, and the average number of levels fused was 3.8, making this group more vulnerable for complications. Despite this, the complications in our series were about 21% with most of them being minor reversible complications such as dural tear, transient root deficits, and postoperative persistent radicular pain. Similarly, the operative time and blood loss, in our series, was lesser compared to that described in literature for multilevel fusions [Table 7].4,6,11,12,13,14 The blood loss in literature ranged from 206 ml in single level to 2056 ml in 9-level fusions and the operative time ranged from 145 min in single level to 415 min in 10.5-level fusions [Table 7].4,6,11,12,13,14 In comparison in our series with an average of 3.8 levels of fusion, the average operative time and blood loss were 150 min (range 60–270 min) and 367.45 ml (range 90–1050 ml), respectively. This could possibly explain the lesser complication rates in our study as the complications were strongly related to the operative time and blood loss.
On reviewing literature and analyzing our surgical technique, we found several strategies that helped in reducing the blood loss and operative time, and hence the complications. Injection tranexamic acid 1 g intravenous was given routinely preoperatively, immediately before skin incision in all cases. Literature describes that a single dose of tranexamic acid 15 mg/kg can effectively reduce blood loss without increasing the risk of deep vein thrombosis.15 The other technique employed in our surgeries was simultaneous exposure and instrumentation on either side by two trained spine surgeons [Figure 2]. This reduced the surgery time and also the blood loss as compared to a single surgeon exposing and instrumenting one side after the other. We employed a laminectomy technique described by Okuda et al.16 in which lamina was removed as a single fragment using osteotome and making cuts at pars on either side. This further reduced the operative time as compared to the classical technique of removing the lamina piecemeal by rongeurs.
Figure 2.
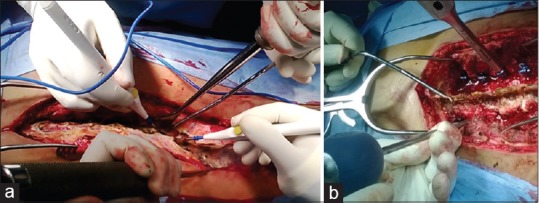
(a and b) Intraoperative images showing the technique of bilateral exposure and bilateral instrumentation
Operative time and blood loss were strongly related to the number of levels of vertebra instrumented and fused. Even though operative time and blood loss could be reduced by reducing the number of instrumented and fused levels, not instrumenting or fusing the levels when indicated would compromise the principles of surgery and therefore affect the clinical outcome. Hence, the number of vertebrae fused or instrumented should be restricted to the minimum indicated levels, without compromising on indications. We also found that the blood loss increased steeply with number of interbody fusion levels. The average blood loss in single level interbody fusion was 307 ml which increased to 362 ml in 2 levels and almost doubled in 3-level interbody fusions [Table 3]. The reason for this exponential increase being continued bleeding from the bed of prepared interbody levels while performing the next level. Performing interbody fusions at selected levels such as the most stenotic or unstable levels or at the bottom of the construct and posterolateral fusions at other levels also could reduce the blood loss and hence the complications [Figures 3 and 4].
Figure 3.
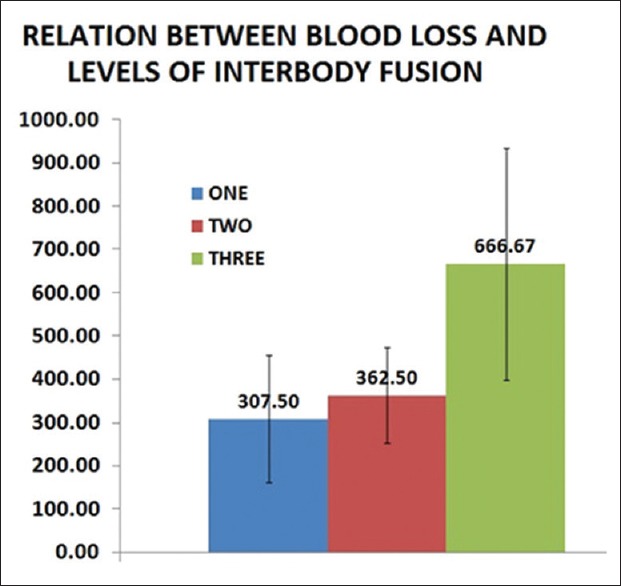
Bar diagram showing the relation between the intraoperative blood loss and number of interbody fusion levels
Figure 4.

Postoperative x-rays anteroposterior and lateral views of lumbosacral spine showing interbody fusions at L2L3, L4L5, L5S1 with posterolateral fusion at L3L4 images
Apart from reduction in operative time and blood loss, a thorough preoperative workup with concerned specialist consultations such as pulmonologist, cardiologist, and optimization of the medical conditions helped in reducing the anesthetic risks during surgery. Six of our patients in the series underwent surgery under spinal or combined spinal epidural anesthesia, due to poor pulmonary or cardiac status. Studies have shown regional anesthesia (RA) in spine surgery to have many advantages over GA in high-risk patients, like lesser anesthetic intraoperative complications, lesser postoperative HTN, respiratory and cardiovascular complications, lesser postoperative vomiting, longer postoperative analgesia, and shorter hospital stay.17,18 As surgeons we found spinal anesthesia to be satisfactory with reduced blood loss due to stable blood pressure one of these patients underwent surgery in sitting position which has shown in literature to be more convenient for the patient under RA, with the blood draining by gravity, resulting in clearer operative field and also reduce anesthesia complications by creating a hemodynamic status similar to that in othostasis.19 Early mobilization postoperatively with optimal control of medical comorbidities also helped in reducing the early postoperative complications.
CONCLUSION
Lumbar fusion surgeries in the elderly with comorbidities have higher complications rates. Increased intraoperative blood loss significantly correlated with the complication rates. Spinal decompression and fusion surgery when indicated should not be denied merely considering the age and comorbidities of the patients, fearing complications. Causes and measures to reduce complications should be considered as the outcome of surgeries in these patients in the absence of complications is good. The authors propose some of the measures to reduce the operative time, blood loss, and hence the complication rates in these patients.
Financial support and sponsorship
Mahesh - Research grant by Ulrich India and consultancy from Medtronic India ltd.
Upendra - Research grant from Medtronic India.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.U. S. Census Bureau DIS. 2008 National Population Projections: Summary Tables [Internet] [Last cited 2016 Oct 14]. Available from: http://www.census.gov/population/projections/data/national/2008/summarytables.html .
- 2.MCRC: Epidemiology of Spinal Surgery - Comparative Effectiveness, Cost and Outcomes Research Center - University of Washington [Internet] [Last cited 2016 Oct 14]. Available from: http://depts.washington.edu/ccor/studies/SpineSurgEpis.html .
- 3.Epstein NE. Spine surgery in geriatric patients: Sometimes unnecessary, too much, or too little. Surg Neurol Int. 2011;2:188. doi: 10.4103/2152-7806.91408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Acosta FL, Jr, McClendon J, Jr, O’Shaughnessy BA, Koller H, Neal CJ, Meier O, et al. Morbidity and mortality after spinal deformity surgery in patients 75 years and older: Complications and predictive factors. J Neurosurg Spine. 2011;15:667–74. doi: 10.3171/2011.7.SPINE10640. [DOI] [PubMed] [Google Scholar]
- 5.Campbell PG, Yadla S, Nasser R, Malone J, Maltenfort MG, Ratliff JK. Patient comorbidity score predicting the incidence of perioperative complications: Assessing the impact of comorbidities on complications in spine surgery. J Neurosurg Spine. 2012;16:37–43. doi: 10.3171/2011.9.SPINE11283. [DOI] [PubMed] [Google Scholar]
- 6.Daubs MD, Lenke LG, Cheh G, Stobbs G, Bridwell KH. Adult spinal deformity surgery: Complications and outcomes in patients over age 60. Spine (Phila Pa 1976) 2007;32:2238–44. doi: 10.1097/BRS.0b013e31814cf24a. [DOI] [PubMed] [Google Scholar]
- 7.Sanderson PL, Wood PL. Surgery for lumbar spinal stenosis in old people. J Bone Joint Surg Br. 1993;75:393–7. doi: 10.1302/0301-620X.75B3.8496206. [DOI] [PubMed] [Google Scholar]
- 8.Ragab AA, Fye MA, Bohlman HH. Surgery of the lumbar spine for spinal stenosis in 118 patients 70 years of age or older. Spine (Phila Pa 1976) 2003;28:348–53. doi: 10.1097/01.BRS.0000048494.66599.DF. [DOI] [PubMed] [Google Scholar]
- 9.Herkowitz HN, Kurz LT. Degenerative lumbar spondylolisthesis with spinal stenosis. A prospective study comparing decompression with decompression and intertransverse process arthrodesis. J Bone Joint Surg Am. 1991;73:802–8. [PubMed] [Google Scholar]
- 10.Guigui P, Devyver B, Rillardon L, Ngounou P, Deburge A, Ghosez JP. Intraoperative and early postoperative complications of lumbar and lumbosacral fusion: Prospective analysis of 872 patients. Rev Chir Orthop Reparatrice Appar Mot. 2004;90:5–15. doi: 10.1016/s0035-1040(04)70001-x. [DOI] [PubMed] [Google Scholar]
- 11.Carreon LY, Puno RM, Dimar JR, 2nd, Glassman SD, Johnson JR. Perioperative complications of posterior lumbar decompression and arthrodesis in older adults. J Bone Joint Surg Am. 2003;85-A:2089–92. doi: 10.2106/00004623-200311000-00004. [DOI] [PubMed] [Google Scholar]
- 12.Cho KJ, Suk SI, Park SR, Kim JH, Kim SS, Choi WK, et al. Complications in posterior fusion and instrumentation for degenerative lumbar scoliosis. Spine (Phila Pa 1976) 2007;32:2232–7. doi: 10.1097/BRS.0b013e31814b2d3c. [DOI] [PubMed] [Google Scholar]
- 13.Zimmerman RM, Mohamed AS, Skolasky RL, Robinson MD, Kebaish KM. Functional outcomes and complications after primary spinal surgery for scoliosis in adults aged forty years or older: A prospective study with minimum two-year followup. Spine (Phila Pa 1976) 2010;35:1861–6. doi: 10.1097/BRS.0b013e3181e57827. [DOI] [PubMed] [Google Scholar]
- 14.Sakaura H, Yamashita T, Miwa T, Ohzono K, Ohwada T. Outcomes of 2-level posterior lumbar interbody fusion for 2-level degenerative lumbar spondylolisthesis. J Neurosurg Spine. 2013;19:90–4. doi: 10.3171/2013.4.SPINE12651. [DOI] [PubMed] [Google Scholar]
- 15.Lykissas MG, Crawford AH, Chan G, Aronson LA, Al-Sayyad MJ. The effect of tranexamic acid in blood loss and transfusion volume in adolescent idiopathic scoliosis surgery: A single-surgeon experience. J Child Orthop. 2013;7:245–9. doi: 10.1007/s11832-013-0486-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Okuda S, Oda T, Miyauchi A, Haku T, Yamamoto T, Iwasaki M. Surgical outcomes of posterior lumbar interbody fusion in elderly patients. Surgical technique. J Bone Joint Surg Am. 2007;89(Suppl 2 (Pt 2)):310–20. doi: 10.2106/JBJS.G.00307. [DOI] [PubMed] [Google Scholar]
- 17.De Rojas JO, Syre P, Welch WC. Regional anesthesia versus general anesthesia for surgery on the lumbar spine: A review of the modern literature. Clin Neurol Neurosurg. 2014;119:39–43. doi: 10.1016/j.clineuro.2014.01.016. [DOI] [PubMed] [Google Scholar]
- 18.McLain RF, Bell GR, Kalfas I, Tetzlaff JE, Yoon HJ. Complications associated with lumbar laminectomy: A comparison of spinal versus general anesthesia. Spine (Phila Pa 1976) 2004;29:2542–7. doi: 10.1097/01.brs.0000144834.43115.38. [DOI] [PubMed] [Google Scholar]
- 19.Nicassio N, Bobicchio P, Umari M, Tacconi L. Lumbar microdiscectomy under epidural anaesthesia with the patient in the sitting position: A prospective study. J Clin Neurosci. 2010;17:1537–40. doi: 10.1016/j.jocn.2010.04.031. [DOI] [PubMed] [Google Scholar]