Abstract
Objective
Childhood sexual abuse (CSA) is linked to negative consequences, including insomnia. Few studies have examined enduring effects of CSA on adult insomnia. Given the relationship between sleep and poor health, a better understanding of these effects has clinical implications.
Method
We used a representative sample of adult twins. Both men and women were assessed with a broad variable representative of CSA, while a subset of females (n=424) were given additional items that captured escalating physical contact and abuse characteristics. A sum score of past month insomnia symptoms was calculated from the shortened version of the SCL-90. Logistic regression was used to estimate the effects of CSA on insomnia symptoms, as well as the effects of physical contact and incident characteristics.
Results
Of the full sample (n=8184), 9.8% reported broad CSA. CSA significantly predicted insomnia symptoms in the female sample (n=1407) (OR=1.67, 95% CI=1.35–2.06, p<0.0001). The continuum of physical contact did not predict sleep. On a univariate level, more than one perpetrator and feeling forced/threatened increased risk for sleep problems, while having a male perpetrator (vs. female or multiple perpetrators) decreased risk. These associations did not hold at a multivariate level. In the mixed-sex sample (n=6777), we replicated our CSA finding (OR=1.65, 95% CI=1.34–2.03, p<0.0001) and found that female gender (OR=1.16, 95% CI=1.03–1.30, p=0.0125) was significant. However, the female gender*CSA interaction was not significant.
Conclusion
CSA predicts insomnia symptoms in adults 25–30 years post-abuse, but the small sample size for incident characteristics (n=424) resulted in limited conclusions about associated risk.
Keywords: childhood, sexual, abuse, insomnia, sleep, epidemiology
Introduction
Childhood sexual abuse (CSA) is an important public health concern, as it can have a lasting impact on the victim’s mental and physical well-being well into adulthood (e.g., (Maniglio, 2009; Wegman & Stetler, 2009). Despite the definitions of CSA varying by the age of what is considered “childhood” (e.g., some studies have defined childhood events as occurring prior to the age of 16, and others include events up to age 18; (Fergusson & Mullen, 1999; Kendler & Prescott, 2006), the extant literature suggests that CSA is relatively common. The prevalence of CSA is reported to be around 20–25% for females and 5–10% for males (Centers for Disease Control and Prevention, 2014; Pereda, Guilera, Forns, & Gomez-Benito, 2009).
Although events included in most definitions of CSA are heterogeneous (e.g., ranging from unwanted kissing or fondling to completed intercourse (Fergusson & Mullen, 1999), there is a wealth of data implicating CSA as a risk factor for a broad array of mental and physical consequences (e.g., Maniglio, 2009; Wegman & Stetler, 2009). Specifically, a history of CSA has been associated with an increased risk for cardiovascular disease (Rich-Edwards et al., 2012), suicide (Devries et al., 2014; Harford, Yi, & Grant, 2014), revictimization (Barnes, Noll, Putnam, & Trickett, 2009; Widom, Czaja, & Dutton, 2008), and premature death (Brown et al., 2009; Felitti et al., 1998), among other medical consequences (Maniglio, 2009; Wegman & Stetler, 2009). CSA has also been associated with an increased risk for the development of many psychiatric disorders, including posttraumatic stress disorder, borderline personality disorder, major depression, generalized anxiety disorder, panic disorder, bulimia nervosa, alcohol dependence, and drug dependence (Bulik, Prescott, & Kendler, 2001b; Fergusson & Mullen, 1999). Generally, more severe forms of CSA (e.g., intercourse vs. non-genital CSA) are associated with higher risk of psychiatric outcomes (Bulik et al., 2001b), however, incident characteristics (e.g., age of the victim, relationship to the perpetrator) may differentially affect risk (Bulik, Prescott, & Kendler, 2001a).
Sleep disturbances, such as insomnia, are a less-studied correlate of CSA. Insomnia is defined in the DSM-V as sleep symptoms - which includes difficulty falling asleep, difficulty staying asleep, or early morning awakenings - present for at least three nights a week, lasting for at least three months and causing significant distress or impairment in normal activities (American Psychiatric Association, 2013). Although only an estimated 6–10% of the population will meet full criteria for insomnia, with more females than males experiencing this disorder (Morin & Jarrin, 2013; Zhang & Wing, 2006), the symptoms themselves are common, with one third of adults reporting at least one of the main nighttime insomnia symptoms (Morin & Jarrin, 2013; Ohayon, 2002; Roth, 2007). Child adversities in general have been associated with sleep problems in adulthood (e.g., Bader, Schafer, Schenkel, Nissen, Kuhl, et al., 2007; Bader, Schafer, Schenkel, Nissen, & Schwander, 2007; Hester, Squires, & Delaney; Koskenvuo, Hublin, Partinen, Paunio, & Koskenvuo, 2010). Moreover, the existing literature links sexual abuse (both child and adult) to sleep disturbances (see Steine et al. (2012) for a thorough review). Specific effects of CSA on sleep in these studies include: more sleep onset difficulties, decreased sleep efficiency, higher nocturnal activity, more nightmares, and more restless sleep, and general sleep disturbances (Steine et al., 2012).
There is a growing extant literature that specifically supports a relationship between CSA and subjective adult sleep disturbances (see Kajeepeta, Gelaye, Jackson, and Williams (2015) for a thorough review of the effects of different types of childhood adversity, including CSA, on sleep) . For example, in one of the few longitudinal studies to date of CSA and sleep disturbances, CSA resulted in more sleep disturbances in adolescent females 10 years after reported abuse, even after controlling for depression and PTSD, which include sleep problems in their diagnostic criteria (Noll, Trickett, Susman, & Putnam, 2006). However, there are still many gaps within this adult literature: Many of the studies have used small and non-representative samples (Kajeepeta et al., 2015; Steine et al., 2012), have not looked at CSA separate from other types of childhood abuse and adversity (Chambers & Belicki, 1998; Greenfield, Lee, Friedman, & Springer, 2011), or have not examined incident characteristics (Kajeepeta et al., 2015; Steine et al., 2012). There are also few studies addressing differences in sleep across gender, and those that have done so used larger numbers of females than males, resulting in low power to detect differences and leaving uncertainty over gender’s potential role in the relationship between CSA and sleep problems (Kajeepeta et al., 2015; Steine et al., 2012). As both sleep and CSA have their own negative influences on both mental and physical health, a better understanding of sleep disturbances in adults with CSA histories, which involves elucidating the effect of incident characteristics on sleep and determining gender differences, is important. Treatment of trauma-exposed individuals is complex, and as such, the effectiveness of interventions on sleep (and other related outcomes such as psychopathology) may differ based on CSA status (Cort et al., 2012; Lewis et al., 2010; Pigeon et al., 2009).
In order to address the limitations of the extant literature on CSA and adult sleep problems, the present analyses use one of the largest adult studies to date of CSA. Our primary aim was to examine the relationships between broad CSA, CSA continuum of physical contact, and CSA characteristics in a female subset of this sample. We hypothesized that CSA would significantly increase the risk of experiencing sleep disturbances, as well as that increasing levels of physical contact (i.e., genital or intercourse vs. non-genital, often used in the literature as a form of severity measurement) would be associated with higher reported occurrences of sleep problems. Further, we aimed to explore the relationships between incident characteristics and sleep problems. In an exploratory aim, we sought to replicate the initial CSA findings in a mixed-gender subset of our sample, which had a different CSA assessment, while also investigating potential gender differences.
Methods
Sample
Participants were taken from the Virginia Adult Twin Studies of Psychiatric and Substance Use Disorders (VATSPSUD) study of Caucasians (Kendler & Prescott, 2006), ascertained from the birth-certificate based Virginia Twin Registry. Female-female (FF) twin pairs, born 1934–1974, were eligible if both members responded to a mailed questionnaire in 1987–1988. Response rates across the four interview waves (FF1-FF4) ranged from 72–83%. All variables used in analysis came from questionnaires filled out during the fourth wave of data (FF4) conducted in 1995–1997. Of the individuals who responded, only those who filled out the CSA portion of the questionnaire at Wave 4 were included (n=1407 individual female twins, who were part of a monozygotic or dizygotic pair). The mean (SD) age and years of education of the twins were 35.1 (7.5) and 14.3 (2.2) at the FF4 interview. Male-male and male-female pairs (MMMF) came from a sample (birth years 1940–1974) initially ascertained, with a 72% cooperation rate, directly from registry records containing all twin births. Data from MMMF1 was used for the CSA variable, as questions about childhood sexual abuse were asked during this interview wave (n=6779 individuals responded). Sleep symptoms, age, and income were used from MMMF2 so that both twin samples’ (FF and MMMF) information was from the final wave. The mean (SD) age and years of education at MMMF2 wave was 37.0 (9.1) and 13.6 (2.6). The all-female (FF4) data was used in primary analyses, while the mixed-gender (MMMF1) data was used in the exploratory aim. Both twin pairs and singletons were included in all analyses, and the data was treated as an epidemiologic sample, with statistical corrections made for twin structure to account for the correlated nature of the sample.
Measures
Insomnia symptoms assessment
Participants completed a shortened version of the Symptom Checklist-90 (SCL-90; Derogatis, Lipman, & Covi, 1973). The SCL measure utilized a past month timeframe and included three symptoms of insomnia: trouble falling asleep, sleep that is restless or disturbed, and awakening in the early morning. Responses to all three items were recorded using a Likert-type format with five response options (scored as 0–4) reflecting frequency: not at all, a little bit, moderately, quite a bit, and extremely. The sleep items showed sufficient internal reliability (Cronbach’s alpha=0.80). These three items were summed up to create a sleep composite score.
Childhood sexual abuse assessment
The self-report questionnaire mailed to participants at wave FF4 included specific questions about childhood sexual abuse. The questionnaire included 6 items that assessed the occurrence and severity of CSA, in response to the following question: “Before the age of 16, did any adult, or another person older than yourself, involve you in any unwanted incidents like…” The 6 items included the following question stems: a) Inviting or requesting you to do something sexual; b) Kissing or hugging you in a sexual way; c) Touching or fondling your private parts; d) Showing their sex organs to you; e) Making you touch them in a sexual way; f) Attempting or having sexual intercourse. Response options to these questions included 0 (never), 1 (once), and 2 (more than once). These items were combined into CSA aggregate sum score variables, as done previously in this dataset (Bulik et al., 2001a, 2001b). A broad CSA variable was created, coded as 0 (did not indicate experiencing any of the items) and 1 (indicated experiencing at least one of the six items). An ordinal categorical continuum of physical contact CSA variable was also created: (1) no genital contact (sexual invitation, sexual kissing, exposing), (2) genital contact but no intercourse (fondling and sexual touching), and (3) intercourse. For the male and opposite-sex twin pair data (MMMF1), participants were asked two questions related to sexual victimization during a phone interview. Individuals who answered “Yes” to at least one of the two questions and reported that the event occurred before age 16 were counted as having reported broad “CSA” in this part of the sample.
CSA characteristics
A number of items assessing incident characteristics were included in the FF4 CSA assessment. Similar to prior analyses with this data (Bulik et al., 2001a), the present analyses included: intercourse vs. other types of abuse (coded as 1 and 0, respectively, using the continuum of physical contact variable created above), age at time of first abuse (continuous variable), more than one perpetrator (coded as 1 if this was indicated and 0 if not), age of perpetrator (5 categories: under 15 years old, 15–18, 19–24, 25–49, ≥ 50; each analyzed separately with 1 coding for that age group being reported and 0 if it was not), gender of perpetrator (with male coded as 1 and female or both genders coded as 0), relationship to the perpetrator (relative [1] vs. non-relative [0]), feeling forced or threatened by the person(s) involved (yes [2] and somewhat [1] vs. no [0], treated in the regression as a factor with three levels), and how much the incident affected the victim at the time (on a 7-point scale, with 1 indicating that the victim did not feel affected and 7 indicating that the experience affected the victim a great deal; if more than one incident occurred participants were asked to rate the worst one). For those individuals indicating that they reported the abuse, whether or not reporting put an end to the abuse (1 if it did and 0 if it did not) and whether or not the response from the person they told was negative (negative/mostly negative, coded as 1) vs. positive (positive/mostly positive/neutral, coded as 0) were also assessed and included in analyses.
Demographic variables
Age and income level (at FF4 for females and MMMF2 for males/opposite-sex twins) were used as covariates in all analyses.
Data Analytic Plan
Ordinal logistic regressions were conducted in SAS 9.3 (SAS Institute; Cary, NC). To account for the non-independence of the nested twin structure, we used the Generalized Estimating Equations (GEE) command of the SAS PROC GENMOD procedure. Primary aims: To test the initial hypothesis that CSA was related to insomnia severity in adults, the sleep composite score was regressed on broad CSA, with age and income included as covariates. To examine the relationship between the continuum of physical contact and sleep, sleep composite score was regressed on the 3-category physical contact variable, with age and income used as covariates again. To see if individual CSA characteristics were differential predictors of sleep problems, sleep composite score was regressed on each characteristic, with age and income as covariates. Finally, all CSA characteristics that were significant predictors of sleep problems on their own were then entered simultaneously into a regression analysis to see if they remained significant. Exploratory aim: Using the MMMF sample, the sleep composite score was regressed on broad CSA, with age, income, and gender as covariates, to replicate the first analysis and explore gender effects. In order to examine gender differences, an interaction effect (CSA*gender) was entered into the regression if gender alone was significant. For all analyses (primary and exploratory) odds ratios (ORs) with 95% confidence intervals (CIs) are reported.
Results1
Sample Characteristics
Among the full sample (n=8,179), mean (SD) age was 37 (9.11) for males and 36.5 (8.56) for females, while average income was $35,000–45,000 for both genders. CSA was reported by 9.8% of the full sample (n=802). Significantly more females (20.4%) than males (3.3%) reported a CSA history (X2=632, p<0.0001). Among the 424 participants who reported a CSA history for whom physical contact data was available 26.0% (n=110) indicated non-genital CSA, 46.7% (n=198) indicated genital CSA, and 27.4% (n=116) indicated attempted or completed intercourse. See Table 1 for the prevalence of the incident characteristics as well as CSA within the FF sample. The MMMF sample had n=6777 individuals.
Table 1.
CSA and Characteristics of Abuse Assessed in Females at Wave 4
| Item | Prevalence | Univariate regression (OR) | Multivariate regression (OR) |
|---|---|---|---|
| Childhood sexual abuse (CSA) | 424 (30.l%) | 1.67 (1.35–2.06)** | - |
|
| |||
| Attempted or completed intercourse vs. other forms of CSA | 116 (27.4%) | 1.215 (0.802–1.839) | - |
|
| |||
| Age at time of abuse | 10.2 ± 3.47 | 0.971 (0.926–1.018) | - |
|
| |||
| More than one perpetrator | 134 (32.7%) | 1.520 (1.054–2.192)* | 1.350 (0.892–2.042) |
|
| |||
| Age of perpetrator | |||
| Under 15 years | 108 (25.5%) | 1.174 (0.803–1.716) | - |
| 15–18 Years | 104 (24.5%) | 1.064 (0.885–1.278) | - |
| 19–24 years | 54 (12.7%) | 1.007 (0.858–1.182) | - |
| 25–49 years | 141 (33.3%) | 0.961 (0.875–1.055) | - |
| ≥ 50 years | 67 (15.8%) | 0.969 (0.886–1.061) | - |
|
| |||
| Gender of perpetrator(s) | |||
| Male vs. female or both | 378 (96.0%) | 0.476 (0.259–0.865)* | 0.553 (0.276–1.108) |
|
| |||
| Abuse by a relative | |||
| Relative vs. non-relative or stranger | 208 (51.6%) | 1.244 (0.879–1.762) | - |
|
| |||
| Forced or threatened | |||
| Maybe | 94 (22.6%) | 0.876 (0.580–1.323) | 0.881 (0.583–1.331) |
| Definitely | 53 (12.7%) | 2.055 (1.160–3.640)* | 1.745 (0.977–3.118) |
|
| |||
| How affected at the time | 3.79 ± 2.01 | 1.070 (0.980–1.169) | - |
|
| |||
| Negative response by someone they told | 31 (16.8%) | 0.670 (0.329–1.366) | - |
|
| |||
| If told, did abuse stop? | 116 (70.3%) | 0.644 (0.361–1.147) | - |
p<0.05.
p<0.001.
A phenotypic factor analysis showed that all three sleep items loaded onto one latent common factor. Estimated factor loadings were 0.78 (trouble falling asleep), 0.99 (restless/disturbed sleep), and 0.71 (early morning awakenings). These results suggest that the use of a composite score is appropriate, and following, the three sleep items were summed (range 0–12) and used in the analyses as an ordinal categorical variable. Although this sum score does not meet a formal definition of insomnia, here forward we refer to the sum score as ‘insomnia symptoms.’ Across the entire sample of males and females, the mean (± SD) insomnia symptom score was 2.24 ± 2.44. Mean (±SD) insomnia symptom score in males was 2.19 ± 2.39, while it was 2.30 ± 2.50 in females (t(df=6,818)=−1.97, p=0.05). Within all individuals who reported CSA, the average (± SD) insomnia symptom score was 2.84 ± 2.74.
Primary aims (FF sample)
CSA and Insomnia Symptoms
Broad CSA was significantly associated with increased odds for higher insomnia symptom severity (see Table 1, row 1 for this result). Age at the time of interview (OR=1.02, 95% CI=1.01–1.03, p=0.001) was significant in this regression but income (OR =0.96, 95% CI=0.92–1.00, p=0.067) was not.
Continuum of Physical Contact and Insomnia Symptoms
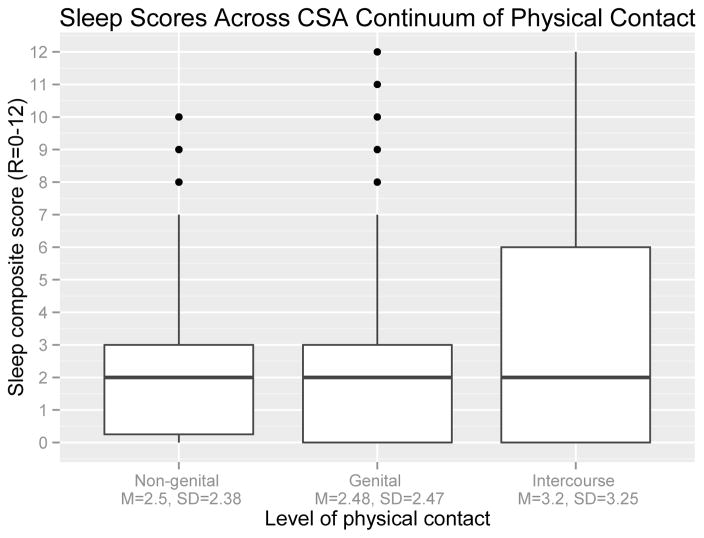
As shown in Figure 1 among the 424 females with physical contact data, the average insomnia symptom score did not differ across the defined levels physical contact (F(2, 420)=2.93, p=0.06). However, the variance for completed intercourse was also substantially higher. In the regression analysis, level of physical contact was not a significant predictor of insomnia symptoms: (genital vs. non-genital CSA, OR=0.90, 95% CI=0.61–1.32, p=0.57; intercourse vs. non-genital CSA, OR=1.13, 95% CI=0.70–1.83, p=0.62). In this model, age was significant (OR=1.04, 95% CI=1.01–1.06, p=0.0046) but income was not (OR=0.95, 95% CI=0.88–1.03, p=0.23).
Figure 1.
Boxplot of sleep composite scores across the three levels of physical contact for females assessed at wave 4.
CSA Characteristics and Insomnia Symptoms
Table 1 presents the results of the univariate regression models run for each of the CSA characteristics (among the 424 females with this data available). For the CSA characteristics, having more than one perpetrator compared to having only one perpetrator was associated with increased odds for higher severity of insomnia symptoms (OR=1.52, 95% CI=1.05–2.19, p=0.03), as was feeling forced or threatened during the abuse compared to not feeling forced or threatened (OR=2.06, 95% CI=1.16–3.64, p=0.01). Gender of the perpetrator was also significant, with having a male perpetrator(s) (compared to female or both genders) associated with a decreased likelihood of insomnia symptoms (OR=0.48, 95% CI=0.26–0.87, p=0.02). No other incident characteristics were associated with insomnia symptom severity. In all models, age was significant, with increasing age associated with an odds ratio slightly greater than 1 for experiencing more insomnia symptoms. Income was not significant in any of these models.
Multivariate analysis
Table 1 also shows the results of the multivariate regression with the significant predictors from the univariate analyses entered simultaneously. Indicating more than one perpetrator was no longer significant in the combined regression (OR=1.35, 95% CI=0.89–2.04, p=0.16). Feeling forced or threatened (OR=1.75, 95% CI=0.98–3.12, p=0.06) and gender of the perpetrator (OR=0.55, 95% CI=0.28–1.11, p=0.095) were also non-significant in the combined analysis. In this combined model, age was once again significant in the same direction as before, and income was not significant.
Exploratory aims (MMMF sample)
In the MMMF sample, CSA significantly predicted insomnia composite score (OR=1.65, 95% CI=1.34–2.04, p<0.0001). Gender was significant in this model (OR=1.16, 95% CI=1.03–1.30, p=0.014) but an interaction effect for gender*CSA was not significant (OR=0.76, 95% CI=0.50–1.15, p=0.19), so it was not included in the final model. Age (OR=1.01, 95% CI=1.01–1.02, p=0.0003) was significant as in other models, and here income (OR=0.93, 95% CI=0.91–0.95, p<0.0001) was a significant predictor, with higher income associated with less symptoms.
Discussion
Broad CSA (FF sample)
The primary purpose of this paper was to determine if exposure to a particularly potent form of childhood trauma, CSA, was associated with insomnia symptoms in adulthood. In the all female sample, having a history of CSA was associated with a 1.67 times increased risk for higher insomnia symptom severity in adulthood, which confirms that CSA is related to subjective sleep disturbances 25–30 years after abuse. Our results are consistent with the CSA literature among both youth and adults (Kajeepeta et al., 2015; Steine et al., 2012). Although outside of the scope of this paper, there are several possible explanations that may account for the relationship between CSA and sleep-related problems and represent future research directions. Potential models could be biological (e.g. sensitization of the HPA axis due to chronic stress early in life (Gillespie, Phifer, Bradley, & Ressler, 2009) and its relationship to sleep and arousal (Han, Kim, & Shim, 2012)) or conceptual (e.g., sleep serves as an important mediator between traumatic stress and poor health outcomes; (Spilsbury, 2009)) in nature.
Continuum of physical contact
Contrary to expectation, the continuum of physical contact of CSA (genital vs. non-genital and intercourse vs. non-genital) was not found to significantly predict insomnia symptom severity. This result is inconsistent with the extant literature (Heath, Bean, & Feinauer, 1996; Koskenvuo et al., 2010; Krakow, Tandberg, Barey, & Scriggins, 1995) as well as prior analyses with this sample (Bulik et al., 2001b) and others (i.e., Fergusson, Horwood, & Lynskey, 1996) in relation to other psychiatric phenotypes that suggests that more severe CSA is associated with increasingly worse outcomes. It is possible that we were underpowered, as only 424 females had data available on this physical contact continuum. The boxplot in Figure 1 shows that individuals who reported attempted or completed intercourse have greater variability in their insomnia scores with a slightly higher mean than the other two groups; however this did not reach statistical significance (p=0.06). Thus, we cannot conclude that there are underlying differences in how different levels of physical contact affect sleep. A recent analysis of CSA characteristics suggests that CSA severity can be broken down into two overall factors, physical and emotional, and that the physical aspects alone (like the continuum of physical contact analyzed here) may not be able to explain abuse severity (Young, Riggs, & Robinson, 2011).
CSA incident characteristics
Three CSA characteristics were found to have significant effects in the series of regressions conducted for the full set of variables shown in Table 1. The strongest predictor of insomnia symptom severity was feeling forced or threatened, conferring an approximately twofold increase in risk, followed closely by indicating more than one perpetrator. In contrast, when the perpetrator(s) was male, as compared to female or both genders, the risk for insomnia symptoms was reduced. Although some of the literature indicates that incident characteristics may differentially affect CSA outcomes (e.g., Heath et al., 1996 present a best-fit model that includes CSA severity, number of prepetrators, and physical abuse as predictors of depression and sleep disturbance in females), a meta-analysis that included type of abuse (severity), age at the time of abuse, relationship to the perpetrator, and number of abuse incidents found that none of these characteristics were mediators of the relationship between CSA and resulting consequences, including depression (Paolucci, Genuis, & Violato, 2001).
There have been several studies examining the effect of incident characteristics on sleep specifically (Noll et al., 2006; Rimsza et al., 1988), but there is mixed evidence as to whether or not these predictors are significant. Our finding that reporting a male perpetrator(s) vs. female or both genders increases insomnia symptoms may also be a reflection of multiple perpetrators; although Noll and colleagues (Noll et al., 2006) actually found the opposite: subgroups including single perpetrator, along with other characteristics representative of less severe abuse, actually reported more sleep disturbances and less sleep in general. Other research suggests the opposite, at least for depression: multiple perpetrators are associated with risk of increased depression symptoms (Liu, Jager-Hyman, Wagner, Alloy, & Gibb, 2012), implying that this could be indicative of more severe CSA, and thus result in experiencing more insomnia symptoms.
However, it is important to note that feeling forced or threatened, multiple perpetrators and gender of the perpetrator were not statistically significant in our sample when combined into a model together. A similar result was seen in Kendler et al. (2000), who used these incident characteristics to predict other psychiatric disorders. No significant predictors were retained for substance use, but depression and generalized anxiety disorder, which both have sleep problems included in their diagnostic criteria (American Psychiatric Association, 1987), retained one predictor each (attempted or completed intercourse and negative response by someone who was told, respectively) in the combined analysis (Bulik et al., 2001a).
Exploratory aims (MMMF sample)
In the MMMF sample, we found a similar association between CSA and insomnia symptom composite score: CSA resulted in a 1.65 times increased risk of insomnia symptoms, which is very close to the odds ratio of 1.67 found in the FF sample. This provides additional evidence for the lasting impact of CSA on insomnia symptoms and demonstrates that despite the use of fewer and less detailed questions to ascertain CSA status in the MMMF wave of the study, we appear to be capturing a similar phenotype. Additionally, gender was a significant predictor of insomnia symptoms in the MMMF sample (OR=1.16, for females), which is consistent with the literature that shows that insomnia is more prevalent in women (Zhang & Wing, 2006). However, gender did not interact with CSA to significantly predict insomnia symptom severity. This was somewhat surprising, as CSA rates are higher among women (Centers for Disease Control and Prevention, 2014; Pereda et al., 2009) and there is some evidence in the adolescent (Edgardh & Ormstad, 2000) and adult (Heath et al., 1996) CSA literatures that females may be more likely to experience sleep symptoms than males. However, both of these sample sizes were small and replication of these findings has not been reported. It should also be noted that although our study comprises one of the largest studies of CSA to date, we could still be underpowered to detect an interaction like this.
Conclusions and limitations
A number of limitations should be noted. A purely self-report methodology was employed, and this is particularly problematic for the assessment of sleep difficulties. Objective measures of sleep (such as polysomnography or actigraphy) would provide more detailed information and allow for a more in-depth analysis of the type of sleep disturbances associated with CSA. We were also limited to the sleep questions that were included in the questionnaire, which reflected past month insomnia symptoms. Our items clearly do not meet a DSM definition of insomnia, given that the items are asked over a 1 month (not 3 month) time span and there is no information on daytime consequences or clinical impairment (American Psychiatric Association, 2013). Additionally, there is no information available on sleep disorders, such as circadian rhythm disorders, in our sample. However, the three items used do parallel the main criteria in the DSM-V insomnia definition (e.g., trouble falling asleep). The assessment of CSA could affect the results as well, since this data relied on retrospective reporting of CSA and incident characteristics. As described in the methods, different questions were used to ascertain CSA status in the all-female and mixed gender data sets, with the all-female sample covering the abuse in greater detail and only two general questions asked to the mixed gender group. However, note that nearly identical odds ratios were obtained in separate regressions, supporting the use of both parts of the dataset.
The variance of insomnia accounted for by predictors across all models was modest (1–6%), yet similar to what is seen when studying psychiatric traits. This indicates that there are clearly other important influences on current insomnia symptoms, above and beyond CSA, that were not examined here. However, given that there is still a significant effect of CSA decades after this abuse, it is useful to focus on CSA. The small sample size of the group of individuals reporting CSA was problematic across all analyses, so future studies with larger sample sizes would be useful to better understand the enduring relationship between CSA and sleep. It is also important to note that we cannot determine causality with these methods. Using a co-twin control analysis, as in Bulik et al. (2001b), could help elucidate causal mechanisms.
Overall, we have demonstrated that CSA is a significant predictor of past month insomnia symptoms, even decades after the abuse. This was true in both our female sample that included a more-detailed CSA assessment and our mixed-gender sample that used only two questions related to abuse. Despite the fact that gender was a significant predictor in our mixed-gender sample, we were unable to show that gender and CSA interact to differentially predict insomnia symptom score. Thus, there are still many questions that remain regarding the enduring relationship between CSA and sleep. Although outside the scope of this particular paper, incident characteristics as related to insomnia symptoms are also of interest. Looking at potential mediators would be another way to delve more into the nature of this relationship. Stressful life events and current psychopathology could serve as mediators, and thus, examination of these relationships is an important future research direction. These mediators would likely account for more of the variance in insomnia symptoms than is seen with only CSA.
Our study adds to the literature on sleep problems as an adverse consequence of CSA, emphasizing that clinicians should be made aware of these results so that they can screen for and address sleep problems in patients (both male and female) reporting a history of CSA. Individuals who report attempted or completed intercourse (compared to other forms of CSA) may be more likely to experience sleep problems, when compared to other forms of CSA; however, this would need to be verified in a larger well-powered study. Other characteristics of the abuse, such as having more than one perpetrator or having felt forced or threatened may also be indicators of more severe sleep problems, so close attention should be paid to patients who report these particular experiences. Given that sleep problems are often symptoms of (American Psychiatric Association, 2013) or comorbid with (Ford & Kamerow, 1989; McCall, 2000; Roth et al., 2006) other psychopathology that may develop in individuals with a history of CSA (i.e., (Bulik et al., 2001b), addressing sleep in these patients could be beneficial in many aspects of their lives. There is also evidence that sleep disturbances are related to revicitimization (Noll et al., 2006), which underscores the importance of addressing sleep symptoms.
The emerging hypothesis that sleep plays a key role in resilience to future psychopathology highlights the importance of recognizing and resolving sleep problems in these patients and demonstrates the impact that treating sleep disturbances can have. Treatment with cognitive-behavioral therapy for insomnia has been found to reduce both depression and insomnia symptoms in individuals with both disorders when used in addition to antidepressants (Manber et al., 2011; Manber et al., 2008). Treatment of sleep problems in PTSD has also been shown to reduce PTSD symptoms in addition to improving sleep (Germain, 2013; Schoenfeld, Deviva, & Manber, 2012). However, the treatment of sleep disturbances in the context of these disorders may differ based on trauma history: A randomized clinical trial involving the use of interpersonal psychotherapy found that patients with current depression and a history of CSA showed less improvement in insomnia symptoms than those without CSA (Pigeon et al., 2009). Other studies corroborate the result that therapy may need to differ based on CSA history (Cort et al., 2012; Lewis et al., 2010). Thus, research into understanding sleep disturbances of CSA-exposed patients is important for both identifying the patients and informing therapy.
Acknowledgments
This work was supported in part by NIH grants R01 AA020179, P20 AA107828, R37 AA011408, K02 AA023239 and R01AG037986. The Mid-Atlantic Twin Registry is supported by NIH grant UL1RR031990. Dr. Amstadter is supported by grants R01AA020179, K02 AA023239, BBRF 20066, R01MH101518, and P60MD002256. The authors report no competing interests.
Footnotes
Note that in all regressions below, the predictors accounted for a modest proportion of the variance in insomnia symptoms (R2 range 0.01–0.06 for logistic regression models).
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 3. Washington, DC: American Psychiatric Association; 1987. Revised. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5. Arlington, VA: American Psychiatric Association; 2013. [Google Scholar]
- Bader K, Schafer V, Schenkel M, Nissen L, Kuhl HC, Schwander J. Increased nocturnal activity associated with adverse childhood experiences in patients with primary insomnia. Journal of Nervous and Mental Disease. 2007;195(7):588–595. doi: 10.1097/NMD.0b013e318093ed00. [DOI] [PubMed] [Google Scholar]
- Bader K, Schafer V, Schenkel M, Nissen L, Schwander J. Adverse childhood experiences associated with sleep in primary insomnia. Journal of Sleep Research. 2007;16(3):285–296. doi: 10.1111/j.1365-2869.2007.00608.x. [DOI] [PubMed] [Google Scholar]
- Barnes JE, Noll JG, Putnam FW, Trickett PK. Sexual and physical revictimization among victims of severe childhood sexual abuse. Child Abuse and Neglect. 2009;33(7):412–420. doi: 10.1016/J.Chiabu.2008.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown DW, Anda RF, Tiemeier H, Felitti VJ, Edwards VJ, Croft JB, Giles WH. Adverse childhood experiences and the risk of premature mortality. American Journal of Perventative Medicine. 2009;37(5):389–396. doi: 10.1016/j.amepre.2009.06.021. [DOI] [PubMed] [Google Scholar]
- Bulik CM, Prescott CA, Kendler KS. Features of childhood sexual abuse and the development of psychiatric and substance use disorders. British Journal of Psychiatry. 2001a;179(5):444–449. doi: 10.1192/bjp.179.5.444. [DOI] [PubMed] [Google Scholar]
- Bulik CM, Prescott CA, Kendler KS. Features of childhood sexual abuse and the development of psychiatric and substance use disorders. British Journal of Psychiatry. 2001b;179(10):444–449. doi: 10.1001/Archpsyc.57.10.953. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Prevalence of Indivdual Adverse Childhood Experiences. Violence Prevention 2014 May 13; [Google Scholar]
- Chambers E, Belicki K. Using sleep dysfunction to explore the nature of resilience in adult survivors of childhood abuse or trauma. Child Abuse and Neglect. 1998;22(8):753–758. doi: 10.1016/s0145-2134(98)00059-3. [DOI] [PubMed] [Google Scholar]
- Cort NA, Gamble SA, Smith PN, Chaudron LH, Lu N, He H, Talbot NL. Predictors of treatment outcomes among depressed women with childhood sexual abuse histories. Depression and Anxiety. 2012;29(6):479–486. doi: 10.1002/da.21942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derogatis LR, Lipman RS, Covi L. SCL-90: an outpatient psychiatric rating scale--preliminary report. Psychopharmacology Bull. 1973;9(1):13–28. [PubMed] [Google Scholar]
- Devries KM, Mak JY, Child JC, Falder G, Bacchus LJ, Astbury J, Watts CH. Childhood Sexual Abuse and Suicidal Behavior: A Meta-analysis. Pediatrics. 2014 doi: 10.1542/peds.2013-2166. [DOI] [PubMed] [Google Scholar]
- Edgardh K, Ormstad K. Prevalence and characteristics of sexual abuse in a national sample of Swedish seventeen-year-old boys and girls. Acta Paediatrica. 2000;89(3):310–319. [PubMed] [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, … Marks JS. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. American Journal of Preventive Medicine. 1998;14(4):245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Horwood LJ, Lynskey MT. Childhood sexual abuse and psychiatric disorder in young adulthood: II. Psychiatric outcomes of childhood sexual abuse. Journal of the American Academy of Child and Adolescent Psychiatry. 1996;35(10):1365–1374. doi: 10.1097/00004583-199610000-00024. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Mullen PE. Childhood sexual abuse: an evidence based perspective. Sage Publications; 1999. [Google Scholar]
- Ford DE, Kamerow DB. Epidemiologic study of sleep disturbances and psychiatric disorders. An opportunity for prevention? JAMA. 1989;262(11):1479–1484. doi: 10.1001/jama.262.11.1479. [DOI] [PubMed] [Google Scholar]
- Germain Anne. Sleep disturbances as the hallmark of PTSD: where are we now? American Journal of Psychiatry. 2013;170(4):372–382. doi: 10.1176/appi.ajp.2012.12040432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillespie CF, Phifer J, Bradley B, Ressler KJ. Risk and resilience: genetic and environmental influences on development of the stress response. Depression and Anxiety. 2009;26(11):984–992. doi: 10.1002/da.20605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenfield EA, Lee C, Friedman EL, Springer KW. Childhood abuse as a risk factor for sleep problems in adulthood: evidence from a U.S. national study. Annals of Behavioral Medicine. 2011;42(2):245–256. doi: 10.1007/s12160-011-9285-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han KS, Kim L, Shim I. Stress and sleep disorder. Experimental Neurobiology. 2012;21(4):141–150. doi: 10.5607/en.2012.21.4.141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harford TC, Yi HY, Grant BF. Associations between childhood abuse and interpersonal aggression and suicide attempt among U.S. adults in a national study. Child Abuse and Neglect. 2014:1873–7757. doi: 10.1016/j.chiabu.2014.02.011. (Electronic)) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heath V, Bean R, Feinauer L. Severity of childhood sexual abuse: Symptom differences between men and women. American Journal of Family Therapy. 1996;24(4):305–314. doi: 10.1080/01926189608251043. [DOI] [Google Scholar]
- Hester RK, Squires DD, Delaney HD. [Google Scholar]
- Kajeepeta S, Gelaye B, Jackson CL, Williams MA. Adverse childhood experiences are associated with adult sleep disorders: a systematic review. Sleep Med. 2015;16(3):320–330. doi: 10.1016/j.sleep.2014.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Prescott CA. Genes, environment, and psychopathology: understanding the causes of pyschiatric and substance use disorders. New York, New York: Guilford Press; 2006. [Google Scholar]
- Koskenvuo K, Hublin C, Partinen M, Paunio T, Koskenvuo M. Childhood adversities and quality of sleep in adulthood: A population-based study of 26,000 Finns. Sleep Medicine. 2010;11(1):17–22. doi: 10.1016/j.sleep.2009.03.010. [DOI] [PubMed] [Google Scholar]
- Krakow B, Tandberg D, Barey M, Scriggins L. Nightmares and Sleep Disturbance in Sexually Assaulted Women. Dreaming. 1995;5(3):199–206. [Google Scholar]
- Lewis CC, Simons AD, Nguyen LJ, Murakami JL, Reid MW, Silva SG, March JS. Impact of childhood trauma on treatment outcome in the Treatment for Adolescents with Depression Study (TADS) Journal of the American Academy of Child and Adolescent Psychiatry. 2010;49(2):132–140. doi: 10.1097/00004583-201002000-00007. [DOI] [PubMed] [Google Scholar]
- Liu RT, Jager-Hyman S, Wagner CA, Alloy LB, Gibb BE. Number of childhood abuse perpetrators and the occurrence of depressive episodes in adulthood. Child Abuse and Neglect. 2012;36(4):323–332. doi: 10.1016/j.chiabu.2011.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manber R, Bernert RA, Suh S, Nowakowski S, Siebern AT, Ong JC. CBT for insomnia in patients with high and low depressive symptom severity: adherence and clinical outcomes. Journal of Clinical Sleep Medicine. 2011;7(6):645–652. doi: 10.5664/jcsm.1472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manber R, Edinger JD, Gress JL, San Pedro-Salcedo MG, Kuo TF, Kalista T. Cognitive behavioral therapy for insomnia enhances depression outcome in patients with comorbid major depressive disorder and insomnia. Sleep. 2008;31(4):489–495. doi: 10.1093/sleep/31.4.489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maniglio R. The impact of child sexual abuse on health: a systematic review of reviews. Clinical Psychology Review. 2009;29(7):647–657. doi: 10.1016/j.cpr.2009.08.003. [DOI] [PubMed] [Google Scholar]
- McCall WV. A psychiatric perspective on insomnia. The Journal of Clinical Psychiatry. 2000;62(Suppl 10):27–32. [PubMed] [Google Scholar]
- Morin CM, Jarrin DC. Epidemiology of insomnia: prevalence, course, risk factors, and public health burden. Sleep Medicine Clinics. 2013;8(3):281–297. doi: 10.1016/j.jsmc.2013.05.002. [DOI] [PubMed] [Google Scholar]
- Noll JG, Trickett PK, Susman EJ, Putnam FW. Sleep disturbances and childhood sexual abuse. Journal of Pediatric Psychology. 2006;31(5):469–480. doi: 10.1093/jpepsy/jsj040. [DOI] [PubMed] [Google Scholar]
- Ohayon MM. Epidemiology of insomnia: what we know and what we still need to learn. Sleep Medicine Reviews. 2002;6(2):97–111. doi: 10.1053/Smrv.2002.0186. [DOI] [PubMed] [Google Scholar]
- Paolucci EO, Genuis ML, Violato C. A meta-analysis of the published research on the effects of child sexual abuse. Journal of Psychology. 2001;135(1):17–36. doi: 10.1080/00223980109603677. [DOI] [PubMed] [Google Scholar]
- Pereda N, Guilera G, Forns M, Gomez-Benito J. The prevalence of child sexual abuse in community and student samples: a meta-analysis. Clinical Psychology Review. 2009;29(4):328–338. doi: 10.1016/j.cpr.2009.02.007. [DOI] [PubMed] [Google Scholar]
- Pigeon WR, May PE, Perlis ML, Ward EA, Lu N, Talbot NL. The effect of interpersonal psychotherapy for depression on insomnia symptoms in a cohort of women with sexual abuse histories. Journal of Traumatic Stress. 2009;22(6):634–638. doi: 10.1002/jts.20456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rich-Edwards JW, Mason S, Rexrode K, Spiegelman D, Hibert E, Kawachi I, … Wright RJ. Physical and sexual abuse in childhood as predictors of early-onset cardiovascular events in women. Circulation. 2012;126(8):920–927. doi: 10.1161/CIRCULATIONAHA.111.076877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rimsza ME, Berg RA, Locke C. Sexual abuse: somatic and emotional reactions. Child Abuse and Neglect. 1988;12(2):201–208. doi: 10.1016/0145-2134(88)90028-2. [DOI] [PubMed] [Google Scholar]
- Roth T. Insomnia: definition, prevalence, etiology, and consequences. Journal of Clinical Sleep Medicine. 2007;3(5 Suppl):S7–10. [PMC free article] [PubMed] [Google Scholar]
- Roth T, Jaeger S, Jin R, Kalsekar A, Stang PE, Kessler RC. Sleep problems, comorbid mental disorders, and role functioning in the national comorbidity survey replication. Biological Psychiatry. 2006;60(12):1364–1371. doi: 10.1016/j.biopsych.2006.05.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schoenfeld FB, Deviva JC, Manber R. Treatment of sleep disturbances in posttraumatic stress disorder: a review. Journal of Rehabilitation Research and Development. 2012;49(5):729–752. doi: 10.1682/jrrd.2011.09.0164. [DOI] [PubMed] [Google Scholar]
- Spilsbury JC. Sleep as a Mediator in the Pathway From Violence-Induced Traumatic Stress to Poorer Health and Functioning: A Review of the Literature and Proposed Conceptual Model. Behavioral Sleep Medicine. 2009;7(4):223–244. doi: 10.1080/15402000903190207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steine IM, Harvey AG, Krystal JH, Milde AM, Gronli J, Bjorvatn B, … Pallesen S. Sleep disturbances in sexual abuse victims: a systematic review. Sleep Medicine Reviews. 2012;16(1):15–25. doi: 10.1016/j.smrv.2011.01.006. [DOI] [PubMed] [Google Scholar]
- Wegman HL, Stetler C. A meta-analytic review of the effects of childhood abuse on medical outcomes in adulthood. Psychosomatic Medicine. 2009;71(8):805–812. doi: 10.1097/PSY.0b013e3181bb2b46. [DOI] [PubMed] [Google Scholar]
- Widom CS, Czaja SJ, Dutton MA. Childhood victimization and lifetime revictimization. Child Abuse and Neglect. 2008;32(8):785–796. doi: 10.1016/j.chiabu.2007.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young TL, Riggs M, Robinson JL. Childhood sexual abuse severity reconsidered: a factor structure of CSA characteristics. Journal of Child Sexual Abuse. 2011;20(4):373–395. doi: 10.1080/10538712.2011.590124. [DOI] [PubMed] [Google Scholar]
- Zhang B, Wing YK. Sex differences in insomnia: a meta-analysis. Sleep. 2006;29(1):85–93. doi: 10.1093/sleep/29.1.85. [DOI] [PubMed] [Google Scholar]