Abstract
Case series summary
At different time points spanning 6 months, three adopted feral flea-infested cats, residing in the household of a veterinary technician, became acutely anorexic, lethargic and febrile. Enrichment blood culture/PCR using Bartonella alpha Proteobacteria growth medium (BAPGM) confirmed initial infection with the same Bartonella henselae genotype in all three cases. With the exception of anemia and neutropenia, complete blood counts, serum biochemical profiles and urinalysis results were within reference intervals. Also, tests for feline leukemia virus, feline immunodeficiency virus, Toxoplasma gondii and feline coronavirus antibodies were negative. Serial daily temperature monitoring in one case confirmed a cyclic, relapsing febrile temperature pattern during 1 month, with resolution during and after treatment with azithromycin. Bartonella henselae Western immunoblot (WB) results did not consistently correlate with BAPGM enrichment blood culture/PCR results or B henselae indirect fluorescent antibody (IFA) titers, and WB titration results were not informative for establishing antibiotic treatment failure. During the respective follow-up periods, no illnesses or additional febrile episodes were reported, despite repeat documentation of B henselae bacteremia in two cats available for follow-up (one with the same genotype and the other with a different B henselae genotype); one cat was, unfortunately, killed by dogs before follow-up testing.
Relevance and novel information
We conclude that microbiological diagnosis and treatment of B henselae infection in cats can be challenging, that antibody titration results and resolution of clinical abnormalities may not correlate with a therapeutic cure, and that fever and potentially neutropenia should be differential diagnostic considerations for young cats with suspected bartonellosis.
Cases 1 and 2, male domestic shorthair cats, were rescued from a shopping center parking area on 16 May 2012. Fleas were removed manually while bathing. On 16 June 2012, physical examinations (estimated age of the cats was 8 weeks and their body weight was 1 kg) were unremarkable. FRCP vaccination (Purevax Feline 3; Merial), empirical treatment for intestinal parasites (Profender; Bayer Animal Health) and a parasiticide (Frontline Plus; Merial) was applied every 25–30 days. Castrations, scheduled for 21 August 2012, were uneventful until 3 weeks later when case 1 became acutely lethargic with an elevated temperature (39.7°C).
Case 1’s complete blood count (CBC; Irvine, CA), serum chemistry profile and urinalysis values (ANTECH Diagnostics) were negative or were within the reference intervals (RIs). Feline leukemia virus (FeLV; indirect fluorescent antibody [IFA; National Veterinary Laboratory, Franklin Lakes, NJ]), feline immunodeficiency virus (FIV; Western blot [WB; National Veterinary Laboratory]), Toxoplasma gondii (ELISA; ANTECH Diagnostics), feline coronavirus (IFA; ANTECH Diagnostics) and a Bartonella henselae WB test (National Veterinary Laboratory) were negative. As summarized in Table 1, Bartonella alpha Proteobacteria growth medium (BAPGM) enriched blood culture/PCR (Galaxy Diagnostics, Research Triangle Park, NC) results were negative (ie, no Bartonella species DNA amplification) and B henselae WB (National Veterinary Laboratory) was again negative.1–3 Because of these negative test results, antibiotics were not administered and the owner (veterinary technician) recorded daily aural temperatures (Baby Braun ThermoScan 5 ear thermometer; Kaz US) for the next 30 days. Fever was defined as a temperature recording at or above 38.3°C. A relapsing, cyclic fever pattern was documented (Figure 1) with inactivity accompanying fever spikes.
Table 1.
Sequential clinical findings. Western immunoblot (WB), PCR, Bartonella alpha Proteobacteria growth medium (BAPGM) blood culture/PCR/DNA sequencing results and post-treatment Western blot antibody titration titers for three febrile Bartonella henselae-infected kittens
| Date | Clinical findings | Bartonella WB and titration titers | Blood PCR | BAPGM culture PCR |
|
|---|---|---|---|---|---|
| Case 1 | 3 September 2012 | Temperature 39.8°C, lethargy | Negative | Negative | Negative |
| 5 September 2012 | Negative | Negative | |||
| 7 September 2012 | Negative | Negative | |||
| 11 October 2012 | Temperature 40.8°C, lethargy | Negative | Bh * | Bh * | |
| Azithromycin 10 mg/kg for 21 days | Bh * | ||||
| 12 November 2012 | 1:256,000 | ||||
| 12 May 2013 | Titration testing | 1:16,000 (16-fold decrease) | |||
| 28 August 2014 | Follow-up testing |
ND | Negative | Bh † | |
| 30 August 2014 | ND | Negative | Negative | ||
| 1 September 2014 | 1:16,000 (no change) |
Negative | Negative | ||
| Case 2 | 21 August 2012 | Presurgery | 1:512,000 | ||
| 3 September 2012 | 40.0°C, lethargy | ND | Bh* | Bh* | |
| 5 September 2012 | ND | Bh* | Bh* | ||
| 7 September 2012 | Azithromycin 10 mg/kg for 21 days |
ND | Bh* | Bh* | |
| 2 March 2013 | 39.8°C, lethargy anorexia | 1:512,000 | Bh* | Bh* | |
| Pradofloxacin 7.5 mg/kg x 21 days | (no change) | Bh* | |||
| 5 September 2013 | Titration testing | 1:64,000 (eight-fold decrease) |
|||
| 30 May 2014 | Killed by dogs and lost to follow-up | ||||
| Case 3 | 23 August 2012 | 37.7°C, lethargy anorexia neutropenia Azithromycin 10 mg/kg for 21 days | 1:64,000 | Bh* | Bh* |
| 7 May 2013 | Titration testing | 1:8,000 (eight-fold decrease) |
|||
| 28 August 2014 | Follow-up BAPGM triple blood draw and titration testing |
ND | Bh* | Bh* | |
| 30 August 2014 | ND | Bh* | Bh* | ||
| 1 September 2014 | 1:32,000 (four-fold decrease) |
Negative | Bh* |
Bartonella henselae Houston-1 strain type based upon 16S-23S intergenic spacer DNA sequences
Bartonella henselae San Antonio-2 strain type based upon 16S-23S intergenic spacer DNA sequences
ND = not determined
Figure 1.
Sequential aural temperature recordings from case 1 prior to azithromycin therapy, documenting a fluctuating, cyclic fever pattern
Case 1 remained intermittently febrile through 11 October 2012, when lethargy, anorexia and fever (40.8°C) necessitated antibiotic therapy. CBC, serum biochemical profile and urinalysis results (ANTECH Diagnostics) were within the RIs. B henselae DNA was amplified and sequenced from the kitten’s blood in two laboratories (Galaxy Diagnostics and Vector Borne Disease Diagnostic Laboratory). By aligning DNA sequences, both laboratories amplified the same B henselae genotype. WB remained negative. Azithromycin suspension (40 mg/cc, 10 mg/kg/day) was administered orally for 21 days. Temperature, behavior and food intake normalized within 24 h. Aural temperatures remained normal for the next 30 days (Figure 2). On 12 November 2012, WB documented seroconversion. Six months later (7 May 2013), WB titration documented a 16-fold decrease in the titer of B henselae antibodies. Despite remaining healthy, B henselae DNA was again PCR amplified and sequenced from a BAPGM enrichment blood culture obtained on 28 August 2014, and WB titration indicated no decrease in antibodies, whereas a B henselae IFA titer (Vector Borne Disease Diagnostic Laboratory) was <1:16.
Figure 2.
Sequential aural temperature recordings from case 1 during and after azithromycin therapy, documenting resolution of the fluctuating, cyclic fever pattern
During the examinations of 15 June and 21 August 2012, case 2, presumably case 1’s littermate, was vaccinated, treated and tested identically. A B henselae WB was positive. There were no intra- or immediate postoperative complications. The owner was instructed to monitor and measure aural temperature if signs of illness occurred. Anorexia, lethargy and fever (40.0°C) developed 10 days postcastration. Laboratory abnormalities (ANTECH Diagnostics; 6 September 2012) included normocytic, normochromic anemia (hematocrit 26.1% [RI 29–48%], hemoglobin 8.2 g/dl [RI 9.3–15.9 g/dl]) and neutrophilia (12,456/µl [RI 2500–8500/µl]). B henselae DNA was amplified (Galaxy Diagnostics) and sequenced (GENEWIZ, Research Triangle Park, NC) from three BAPGM enrichment blood cultures. Azithromycin suspension (40 mg/cc, 10 mg/kg/day) was administered orally for 21 days. Temperature and food intake normalized within 24 h.
On 1 March 2013, case 2 became anorexic, lethargic and febrile (39.8°C). Body weight had increased (3.5 kg). Neutropenia (986/µl [RI 2500–8500/µl], confirmed by blood smear examination [ANTECH Diagnostics]) was the only hematological abnormality. Serum biochemical profile and urinalysis values were within the RIs. BAPGM enrichment blood culture/PCR (Galaxy Diagnostics) and FastPanel PCR Feline Flea and Tick Borne Profile (ANTECH Diagnostics) amplified B henselae DNA, whereas Anaplasma, Ehrlichia and hemotropic Mycoplasma species were not amplified from the cat’s blood. Azithromycin suspension (40 mg/cc, 10 mg/kg/day) was administered orally for 21 days, and again temperature and food intake normalized within 24 h. B henselae WB titration antibody levels (August 2012 vs March 2013) were unchanged. On 26 April 2013, case 2 was again febrile and lethargic and was treated with pradofloxacin (Veraflox, 7.5 mg/kg per day as an oral suspension; Bayer Animal Health) for 21 days. Within 6 h the cat appeared clinically improved. CBC values (5 September 2013) were within the RIs (neutrophil count 3060/µl) by WB titration (pretreatment and 5 months post-treatment), serum samples identified an eight-fold decrease in B henselae antibody levels; whereas, a B henselae IFA titer (Galaxy Diagnostics) was <1:16. Case 2 remained healthy until 30 May 2014, when the cat was killed by two dogs after escaping from the house. A necropsy was not performed.
On 15 August 2012, case 3, a female domestic shorthair cat, was found hiding under a car. Prior to introduction into the home, the flea-infested cat (weight 1.4 kg, aural temperature 37.8°C) was bathed, Frontline-Plus was applied, ear mites were treated (Acarexx; Boehringer Ingelheim Vetmedica) empirically with Profender and a vaccine (Nobivac: 1-HCP + FeLV; Merck Animal Health) was administered. Prior to comingling, case 3 was isolated from the other two kittens for 7 days. Cases 3 and 2 began playing and interacting immediately, whereas case 1 interacted minimally with case 3 for the initial month after introduction, after which all three cats interacted frequently.
On 23 August 2012, case 3 was lethargic and anorexic (aural temperature 37.7°C, body weight 1.38 kg). Physical examination was unremarkable. Neutropenia (930/μl [RI 2500–8500/μl]) was the only hematological abnormality. A serum biochemistry profile and urinalysis results were within the RIs. FeLV (National Veterinary Laboratory), FIV (National Veterinary Laboratory), T gondii, and feline coronavirus tests were negative. WB was positive and B henselae DNA was amplified (Galaxy Diagnostics) and sequenced (GENEWIZ) via BAPGM enrichment blood culture. Azithromycin suspension was administered (40 mg/cc, 10 mg/kg/day) for 21 days. Normal behavior and activities resumed within 5 h. WB titration (August 2012 and May 2013 serum) documented an eight-fold decrease in B henselae antibodies. Despite remaining clinically healthy, case 3 was bacteremic in August 2014, accompanied by a four-fold increase in B henselae WB antibodies, whereas a B henselae IFA titer (Galaxy Diagnostics) was <1:16.
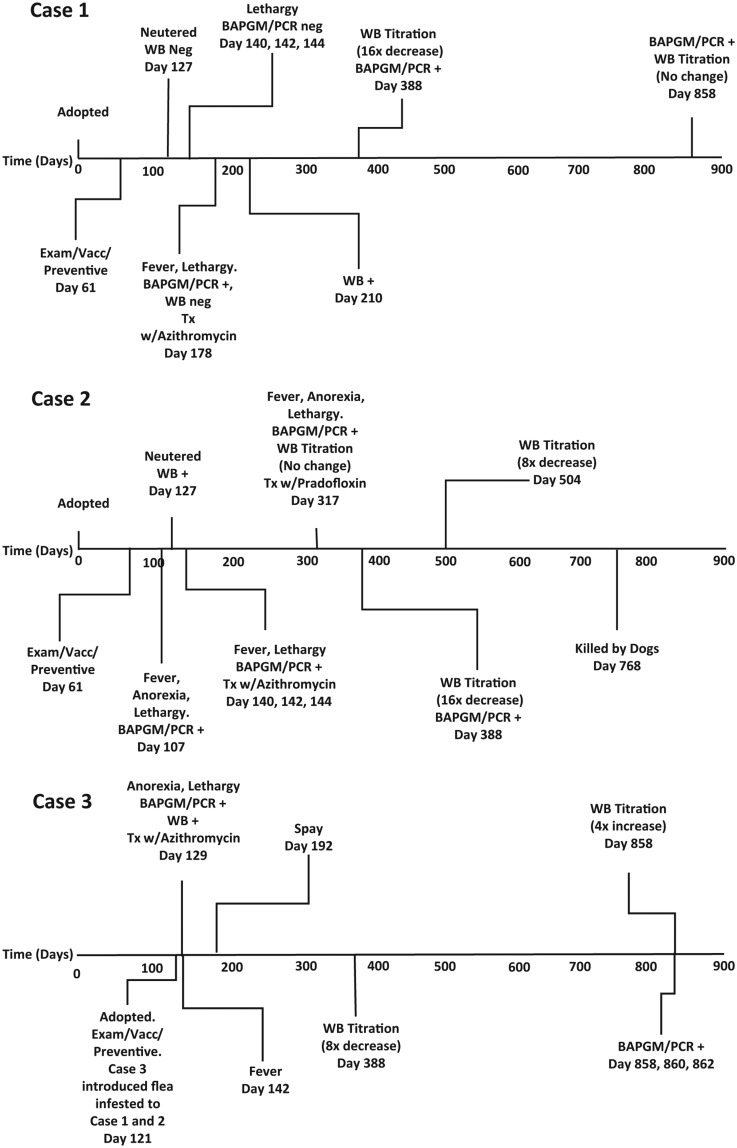
Fleas were not seen on the three kittens or the owner’s only dog following initial adoption. The time course for each of the three cases is summarized in Figure 3.
Figure 3.
Summary of the time course for each of the three cases.
WB Neg = Western blot negative; BAPGM = Bartonella alpha Proteobacteria growth medium; PCR neg = PCR negative; WB = Western blot; PCR (+) = PCR positive; Exam = examination; Vacc = vaccination; Tx w/ = treatment with; WB (+) = Western blot positive
Identical pretreatment B Henselae DNA sequences were obtained from all three cats. For each amplicon, there was 100% 16S–23S intergenic spacer region (ITS) sequence identity (ie, 360/360 nucleotides aligned [National Center for Biotechnology Information]), supporting infection with the same B Henselae ITS genotype (Houston-1, Genbank Accession L35101). This Houston-1 genotype was again documented at fever recrudescence 112 days later from case 2, and from case 3 2 years later, supporting failure of azithromycin to eliminate either infection. In contrast, case 1 was infected with a different ITS genotype (415/415 base pair identity to B Henselae San Antonio-2, Genbank accession AF369529) 2 years later, supporting co-infection with more than one genotype or a newly acquired infection.
Discussion
Although involving only three cases, these findings are unique for several reasons. The owner, a veterinary technician, worked for a veterinarian who systematically pursued an infectious disease diagnosis, in association with acute-onset lethargy and febrile illness. Additionally, there was consistency in preventive healthcare (vaccines and parasiticides), diagnostic testing, and the dose and duration of azithromycin administration. BAPGM enrichment blood culture/PCR followed by DNA sequencing documented B henselae infection in cases 2 and 3 at illness onset and at the time of case 2’s fever recrudescence, whereas case 1 initially tested PCR negative. Two possibilities for the negative BAPGM enrichment blood culture/PCR results seem most likely. Following experimental blood transfusion transmission of B henselae to cats, Kordick and Breitschwerdt documented prolonged periods of abacteremia (weeks to months) in some cats.4 Thus, it is possible that case 1 did not have circulating B henselae organisms at the time of specimen collections in September 2012. Alternatively, case 1 could have been infected by a flea, unknowingly introduced into the household, following case 3’s adoption in August 2012. This possibility could explain the negative WB results, the negative PCR results and the subsequent PCR positive results and documentation of seroconversion by WB. Based upon 16S–23S ITS DNA sequence alignments, all three kittens were initially infected with the same B henselae genotype.
Short-duration fever has been reported in cats experimentally infected with B henselae,4–10 and the bacterium causes relapsing fever in humans, particularly children.11–13 Cat scratch disease, caused by B henselae, is characterized by fever and lymphadenopathy,12,14 and recently B henselae bacteremia was documented in a dog with fever of unknown origin.15 Thus virulent strains of B henselae cause fever in cats, dogs and humans. Diagnostically, there were no consistent hematological, biochemical or urinalysis abnormalities, despite acute-onset febrile illness; however, case 2 was initially mildly anemic and had neutrophilia but was neutropenic when febrile illness reoccurred. The neutropenia in these two cats may have been related to B henselae infection or infection with another organism that was not tested for diagnostically. Unique sequential temperature data in case 1 documented a fluctuating, relapsing febrile pattern prior to illness onset.
An obvious limitation of this study is the inability to determine when and how B henselae transmission initially occurred and whether there was subsequent bacterial transmission within the household. Importantly, the onset of illness in cases 1 and 2 occurred months after presumptive flea transmission of B henselae, but shortly after the introduction of case 3. It is possible that fleas were unknowingly introduced into the household with case 3. In the context of disease causation, immediately following administration of azithromycin, all three cases became afebrile, supporting a diagnosis ex juvantibus (‘from that which helps’; medical definition: ‘a response to a narrow, specific therapy that strengthens the association with a suspected etiology’). Although B henselae bacteremia was documented in all three cats in conjunction with resolution of clinical signs following initiation of antibiotic therapy, it is possible that this response was related to another infectious agent (co-infection), or that spontaneous resolution of clinical signs occurred independently of antibiotic administration. However, based upon the results of this study and others published previously,4–9 B henselae may be an underestimated cause of fever of unknown origin in flea-exposed cats, particularly those with immature or naive immune systems.
In a study by Lappin et al, feline B henselae ELISA seroreactivity did not correlate with fever, whereas PCR positivity approached statistical significance (P = 0.0571).16 Also, Bartonella ELISA and WB did not correlate with positive Bartonella PCR.16 Because cats are natural reservoir hosts for Bartonella clarridgeiae, B henselae and Bartonella koehlerae, investigators have experienced difficulties establishing whether these Bartonella species are feline pathogens. Experimentally, the route of infection (intravenous or subcutaneous) and inoculum (culture grown, blood transfusion or flea transmission) substantially influence the duration and patterns of bacteremia (relapsing or non-relapsing), whether clinical signs were observed and, in those studies in which cats were necropsied, whether pathological lesions were found.4–9 Owing to the high seroprevalences among cats in flea-endemic regions, seroepidemiological studies have, for the most part, not found statistical associations between B henselae seroreactivity and disease manifestations.16–21 However, Whittemore et al found a correlation between Bartonella species antibodies and hypergammaglobulinemia in cats.22 Sykes et al found an association between gingivitis and stomatitis and culturing Bartonella species from bacteremic cats, whereas there was no statistical difference in seroprevalence between cases and controls.21 Also, a study from Switzerland, where the overall B henselae seroprevalence in 728 cats was low (8.3%) compared with many regions in North America where cat population seroprevalences are >40%, found a statistical correlation between seroreactivity and stomatitis.23 Collectively, these and other published studies serve to illustrate the evolutionary adaptation of most B henselae strains among cats as a natural reservoir host and the inherent difficulty in establishing disease correlations.
There is substantial genetic variation among B henselae strains,24 potentially contributing to different virulence characteristics, most likely mediated by genetic variation among B henselae type IV secretion systems,25 Bad A adhesion proteins and potentially other unknown virulence factors.26 Also, the strains most often isolated from healthy, non-clinical cats are not the genetic strains most often found in humans with bartonellosis.24,27 Thus, similar to other bacteria such as Escherichia coli (E coli 0157:H7 can induce hemolytic uremic syndrome and death), there are differences in virulence among B henselae strains. One might speculate that virulence differences, in conjunction with the robustness of the host immune response, determine the extent to which a B henselae genotype induces disease. For example, the CSU-1 strain, originally isolated from a shelter cat in Florida and used experimentally by Bradbury and Lappin in flea transmission studies, has induced acute myocarditis in young experimentally infected cats.9 Other feline experimental infection studies have also provided evidence to support virulence differences among B henselae strains.4,9 Granulomatous myocarditis was reported in young, naturally flea-infested cats, by direct bacterial visualization and PCR amplification of B henselae from the myocardial lesions.28 Thus, future field-based studies designed to address disease causation should incorporate bacterial isolation, B henselae genotyping, sequential serological testing, an enrichment culture/PCR approach to enhance the sensitivity of documenting infection with one or more Bartonella species and documentation of each cat’s clinical response to a defined antibiotic treatment regimen.
As recently reviewed, there is no ‘gold standard’ test for the diagnosis of bartonellosis in cats, dogs, horses or humans.29 A study involving canine vector-borne diseases (CVBDs) diagnosis provided support for obtaining serological, microbiological culture and PCR data when attempting to confirm a CVBD diagnosis.30 With the advent of PCR testing, some clinicians have abandoned serology in favor of vector-borne disease molecular diagnostic panels. As PCR testing has substantial sensitivity limitations (ie, false-negative test results),30 both modalities are recommended for diagnosis of feline vector-borne diseases, including bartonellosis.
In this study, WB results did not correlate with B henselae IFA titers, whereas in previous studies there were no correlations between ELISA and WB.9,16 Why WB, ELISA and IFA titers do not correlate deserves future research consideration. Also, WB titration results from case 3 were not informative for establishing antibiotic treatment failure. As cats (an unknown percentage), dogs (50–75% depending upon infecting Bartonella species),32 horses (100%)32 and humans (approximately 50–100% depending upon infecting Bartonella species)33,34 can be Bartonella bacteremic without detectable IFAs, IFA serology has substantial lack of sensitivity across several animal species. Similarly, case 1 was initially WB negative despite documentation of bacteremia, whereas case 2 was not initially treated (owing to lack of illness), despite being WB positive. As a result of stress-induced interference with premonition (infection immunity), one might speculate that hospitalization and castration contributed to the onset of febrile illness in cases 1 and 2, 10–21 days later. At the time of illness onset and at the time of recrudescent febrile illness, case 2 was BAPGM blood culture/PCR positive. Also, in order to determine antimicrobial susceptibility and resistance patterns, it is important for diagnostic laboratories to culture Bartonella species from cats and other animals whenever possible.
While there are multiple serologic assays, PCR assays and culture methods available for use to aid in the diagnosis of bartonellosis in cats, studies proving which are optimal are lacking. Despite these limitations, we recommend the use of serology, a Bartonella enrichment culture/PCR platform and subculture isolation to aid clinicians in making antibiotic treatment decisions or to advise clients relative to zoonotic concerns.
An optimal bartonellosis treatment regimen has not been established for bacteremic animals or humans.29,35 In a study involving naturally infected febrile cats, both doxycycline and orbifloxacin induced resolution of clinical abnormalities by day 5 of treatment; however, despite a 28 day treatment course, most cats remained Bartonella species PCR positive after antibiotic administration.10 Experimentally, cats inoculated with B henselae-infected blood remained culture positive despite treatment with 2 or 4 weeks of doxycycline.36 Relapses after antibiotic withdrawal have also been reported in B henselae-infected dogs and human patients treated with extended courses of doxycycline.37–39 Doxycycline treatment failure (6 week course) was also suspected in a febrile dog from France.15 Based upon the limited clinical and experimental evidence, we do not recommend doxycycline treatment protocols published to date as the sole antibiotic for treatment of feline bartonellosis, if therapeutic elimination is the primary goal.
By E-test and disk diffusion assays, pradofloxacin had greater antimicrobial activity against feline B henselae isolates than enrofloxacin and azithromycin40 and appeared to be an effective treatment for case 2; however, post-treatment BAPGM enrichment blood culture was not performed. Based upon negative culture and PCR results, cats treated with orbifloxacin appeared to clear their B henselae infections.9 A combination of antibiotics with different modes of action, such as doxycycline and a fluoroquinolone, may be required for therapeutic elimination of B henselae in cats; however, data confirming that a combination of doxycycline and pradofloxacin (as used in case 2) eliminates B henselae infections, rather than suppressing the infection, are currently lacking. Azithromycin has often been used to treat feline bartonellosis; however, based upon in vitro testing, cat and human B henselae strains rapidly developed genetic resistance to macrolides through a single nucleotide mutation in the 23S rRNA gene.41 Currently, no studies have investigated antimicrobial resistance in B henselae isolates obtained from azithromycin-treated cats, and there are no studies confirming the efficacy of azithromycin as a sole antibiotic for the treatment of feline bartonellosis.
Optimal monitoring of cats previously diagnosed with bartonellosis has not be established and further studies are needed. However, we recommend that follow-up serology and enrichment culture/PCR testing be considered to confirm therapeutic elimination of the infection. Post-treatment decreases in antibody levels seem to support elimination of infection in dogs.42 However, in a dog experimentally infected with B henselae, IFAs were no longer detectable after administration of corticosteroids (no antibiotic treatment administered), yet B henselae was isolated from the bone marrow.43 Based upon human case experiences, obtaining three specimens for enrichment blood culture/PCR within a 7 day period increased sensitivity of Bartonella species detection (odds ratio 3.4; P = 0.02),44 and in no instance was a patient enrichment culture/PCR positive in all three specimens and only 3/12 patients were positive for two specimens. This finding, potentially related to a relapsing bacteremia as reported in cats,4 indicates that diagnostic confirmation and subsequently proving therapeutic elimination of bartonellosis remains clinically and diagnostically challenging. Until additional studies define an optimal treatment regimen for feline bartonellosis, combination therapy is recommended for culture or PCR confirmed cases. As optimal treatment regimens, including dual therapy, are not proven to eliminate Bartonella species bacteremia in cats, it is important to attempt to lessen potential transmission by maintaining stringent flea control.8,9
Conclusions
We conclude that B henselae causes acute febrile illness in cats that resolves in conjunction with antibiotic therapy, which may or may not represent elimination of infection. Neutropenia may be an accompanying haematological abnormality in a subset of cats with bartonellosis. Additional laboratory and field studies are needed to define optimal treatment regimens and optimal follow-up testing procedures for cats with bartonellosis.
Acknowledgments
We wish to thank Tonya Lee for editorial assistance; Julie Bradley for assistance in generating Figure 3; and Kim Thomas, the owner, for obtaining the daily temperature measurements for case 1 and for facilitating the testing, treatments and follow-up evaluations of the three kittens reported in this manuscript. We also thank Dr William Hardy and Evelyn Zuckerman, National Veterinary Laboratory, for generating the Western blot and antibody titration data. EBB also thanks Dr Edward Wakem for helpful discussions related to the concept of diagnosis ex juvantibus.
Footnotes
Supplementary material: Indirect fluorescent antibody testing using a panel of Bartonella species antigens and the BAPGM enrichment blood culture/PCR platform, with DNA sequence confirmation of the infecting Bartonella species, is available for clinical diagnostic and research study purposes through Galaxy Diagnostics, Inc, Research Triangle Park, NC.
Conflict of interest: In conjunction with Dr Sushama Sontakke and North Carolina State University, Dr Breitschwerdt holds US Patent No. 7,115,385; Media and Methods for cultivation of microorganisms, which was issued 3 October 2006. He is the Chief Scientific Officer for Galaxy Diagnostics, a company that provides diagnostic testing for the detection of Bartonella species infection in animals and human patients. Dr Natalie Cherry is the Laboratory Supervisor/Research Specialist for Galaxy Diagnostic, Inc.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Duncan AW, Maggi RG, Breitschwerdt EB. A combined approach for the enhanced detection and isolation of Bartonella species in dog blood samples: pre-enrichment culture followed by PCR and subculture onto agar plates. J Microbiol Meth 2007; 69: 273–281. [DOI] [PubMed] [Google Scholar]
- 2. Maggi RG, Duncan AW, Breitschwerdt EB. Novel chemically modified liquid medium that will support the growth of seven Bartonella species. J Clin Microbiol 2005; 43: 2651–2655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Breitschwerdt EB, Maggi RG, Mozayeni BR, et al. PCR amplification of Bartonella koehlerae from human blood and enrichment blood cultures. Parasit Vectors 2010; 3: 76–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kordick DL, Breitschwerdt EB. Relapsing bacteremia following blood transmission of Bartonella henselae in cats. Am J Vet Res 1997; 58: 492–497. [PubMed] [Google Scholar]
- 5. O’Reilly KL, Bauer RW, Freeland RL, et al. Acute clinical disease in cats following infection with a pathogenic strain of Bartonella henselae (LSU16). Infect Immun 1999; 67: 3066–3072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Chomel BB, Kasten RW, Floyd-Hawkins K, et al. Experimental transmission of Bartonella henselae by the cat flea. J Clin Microbiol 1996; 34: 1952–1956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Guptill L, Slater L, Wu CC, et al. Experimental infection of young specific pathogen-free cats with Bartonella henselae. J Infect Dis 1997; 176: 206–216. [DOI] [PubMed] [Google Scholar]
- 8. Lappin MR, Davis WL, Hawley JR, et al. A flea and tick collar containing 10% imidacloprid and 4.5% flumethrin prevents flea transmission of Bartonella henselae in cats. Parasit Vectors 2013; 6: 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Bradbury CA, Lappin MR. Evaluation of topical application of 10% imidacloprid-1% moxidectin to prevent Bartonella henselae transmission from cat fleas. J Am Vet Med Assoc 2010; 236: 869–873. [DOI] [PubMed] [Google Scholar]
- 10. Lappin MR, Miller W, Sellins D. Effect of doxycycline or orbifloxacin administration on Bartonella spp. and Hemoplasma assay results in naturally exposed cats. Intern J Appl Res Vet Med 2012; 10: 225. [Google Scholar]
- 11. Myint KS, Gibbons RV, Iverson J, et al. Serological response to Bartonella species in febrile patients from Nepal. Trans R Soc Trop Med Hyg 2011; 105: 740–742. [DOI] [PubMed] [Google Scholar]
- 12. Boggs SR, Fisher RG. Bone pain and fever in an adolescent and his sibling. Cat scratch disease (CSD). Pediatr Infect Dis J 2011; 89: 93–94. [DOI] [PubMed] [Google Scholar]
- 13. Lin JW, Chen CM, Chang CC. Unknown fever and back pain caused by Bartonella henselae in a veterinarian after a needle puncture: a case report and literature review. Vector Borne Zoonotic Dis 2011; 11: 589–591. [DOI] [PubMed] [Google Scholar]
- 14. Zangwill KM. Cat scratch disease and other Bartonella infections. Adv Exp Med Biol 2013; 764: 159–166. [DOI] [PubMed] [Google Scholar]
- 15. Drut A, Bublot I, Breitschwerdt EB, et al. Comparative microbiological features of Bartonella henselae infection in a dog with fever of unknown origin and granulomatous lymphadenitis. Med Microbiol Immunol 2014; 203: 85–91. [DOI] [PubMed] [Google Scholar]
- 16. Lappin MR, Breitschwerdt E, Brewer M, et al. Prevalence of Bartonella species antibodies and Bartonella species DNA in the blood of cats with and without fever. J Feline Med Surg 2009; 11: 141–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Leibovitz K, Pearce L, Brewer M, et al. Bartonella species antibodies and DNA in cerebral spinal fluid of cats with central nervous system disease. J Feline Med Surg 2008; 10: 332–337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Fontenelle JP, Powell CC, Hill AE, et al. Prevalence of serum antibodies against Bartonella species in the serum of cats with or without uveitis. J Feline Med Surg 2008; 10: 41–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Powell CC, McInnis CL, Fontenelle JP, et al. Bartonella species, feline herpesvirus-1, and Toxoplasma gondii PCR assay results from blood and aqueous humor samples from 104 cats with naturally occurring endogenous uveitis. J Feline Med Surg 2010; 12: 923–928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Dowers KL, Hawley JR, Brewer MM, et al. Association of Bartonella species, feline calicivirus, and feline herpesvirus 1 infection with gingivostomatitis in cats. J Feline Med Surg 2010; 12: 314–321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Sykes JE, Westropp JL, Kasten RW, et al. Association between Bartonella species infection and disease in pet cats as determined using serology and culture. J Feline Med Surg 2010; 12: 631–636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Whittemore JC, Hawley JR, Radecki SV, et al. Bartonella species antibodies and hyperglobulinemia in privately owned cats. J Vet Intern Med 2012; 26: 639–644. [DOI] [PubMed] [Google Scholar]
- 23. Glaus T, Hofmann-Lehmann R, Greene C, et al. Seroprevalence of Bartonella henselae infection and correlation with disease status in cats in Switzerland. J Clin Microbiol 1997; 35: 2883–2885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Bouchouicha R, Durand B, Monteil M, et al. Molecular epidemiology of feline and human Bartonella henselae isolates. Emerg Infect Dis 2009; 15: 813–816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Quebatte M, Dehio M, Tropel D, et al. The BatR/BatS two-component regulatory system controls the adaptive response of Bartonella henselae during human endothelial cell infection. J Bacteriol 2010; 192: 3352–3367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Schmidgen T, Kaiser PO, Ballhorn W, et al. Heterologous expression of Bartonella adhesin A in Escherichia coli by exchange of trimeric autotransporter adhesin domains results in enhanced adhesion properties and a pathogenic phenotype. J Bacteriol 2014; 1960: 2155–2165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Gil H, Escudero R, Pons I, et al. Distribution of Bartonella henselae variants in patients, reservoir hosts and vectors in Spain. PLoS One 2013; 8: e68248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Varanat M, Broadhurst J, Linder KE, et al. Identification of Bartonella henselae in 2 cats with pyogranulomatous myocarditis and diaphragmatic myositis. Vet Pathol 2012; 49: 608–611. [DOI] [PubMed] [Google Scholar]
- 29. Breitschwerdt EB. Bartonellosis: one health perspectives for an emerging infectious disease. ILAR J 2014; 55: 46–58. [DOI] [PubMed] [Google Scholar]
- 30. Maggi RG, Birkenheuer AJ, Hegarty BC, et al. Comparison of serological and molecular panels for diagnosis of vector-borne diseases in dogs. Parasit Vectors 2014; 7: e127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Pérez C, Maggi RG, Diniz PP, et al. Molecular and serological diagnosis of Bartonella infection in 61 dogs from the United States. J Vet Intern Med 2011; 25: 805–810. [DOI] [PubMed] [Google Scholar]
- 32. Cherry NA, Jones SL, Maggi RG, et al. Bartonella spp. infection in healthy and sick horses and foals from the southeastern United States. J Vet Intern Med 2012; 26: 1408–1412. [DOI] [PubMed] [Google Scholar]
- 33. Maggi RG, Mascarelli PE, Pultorak EL, et al. Bartonella spp. bacteremia in high-risk immunocompetent patients. Diagn Microbiol Infect Dis 2011; 71: 430–437. [DOI] [PubMed] [Google Scholar]
- 34. Maggi RG, Mozayeni BR, Pultorak EL, et al. Bartonella spp. bacteremia and rheumatic symptoms in patients from Lyme Disease-endemic region. Emerg Infect Dis 2012; 18: 783–791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Angelakis E, Raoult D. Pathogenicity and treatment of Bartonella infections. Int J Antimicrob Agents 2014; 44: 16–25. [DOI] [PubMed] [Google Scholar]
- 36. Kordick DL, Papich MG, Breitschwerdt EB. Efficacy of enrofloxacin or doxycycline for treatment of Bartonella henselae or Bartonella clarridgeiae infection in cats. Antimicrob Agents Chemother 1997; 41: 2448–2255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Diniz PP, Wood M, Maggi RG, et al. Co-isolation of Bartonella henselae and Bartonella vinsonii subsp. berkhoffi from blood, joint and subcutaneous seroma from two naturally infected dogs. Vet Microbiol 2009; 138: 368–372. [DOI] [PubMed] [Google Scholar]
- 38. Sykes JE, Lindsay LL, Maggi RG, et al. Human co-infection with Bartonella henselae and two hemotropic mycoplasma variants resembling Mycoplasma ovis. J Clin Microbiol 2010; 48: 3782–3785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Maggi RG, Mascarelli PE, Havenga LN, et al. Co-infection with Anaplasma platys, Bartonella henselae and Candidatus Mycoplasma hematoparvum in a veterinarian. Parasit Vectors 2013; 6: e106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Biswas S, Maggi RG, Papich MG, et al. Comparative activity of pradofloxacin, enrofloxacin, and azithromycin against Bartonella henselae isolates collected from cats and a human. J Clin Microbiol 2010; 48: 617–618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Biswas S, Maggi RG, Papich MG, et al. Molecular mechanisms of Bartonella henselae resistance to azithromycin, pradofloxacin and enrofloxacin. J Antimicrob Chemother 2010; 65: 581–582. [DOI] [PubMed] [Google Scholar]
- 42. Breitschwerdt EB, Blann KR, Stebbins ME, et al. Clinicopathological abnormalities and treatment response in 24 dogs seroreactive to Bartonella vinsonii (berkhoffii) antigens. J Am Anim Hosp Assoc 2004; 40: 92–101. [DOI] [PubMed] [Google Scholar]
- 43. Balakrishnan N, Cherry NA, Linder KE, et al. Experimental infection of dogs with Bartonella henselae and Bartonella vinsonii subsp. berkhoffii. Vet Immunol Immunopathol 2013; 156: 153–158. [DOI] [PubMed] [Google Scholar]
- 44. Pultorak EL, Maggi RG, Mascarelli PE, et al. Serial testing from a 3-day collection period by use of the Bartonella Alpha proteobacteria growth medium platform may enhance the sensitivity of Bartonella species detection in bacteremic human patients. J Clin Microbiol 2013; 51: 1673–1677. [DOI] [PMC free article] [PubMed] [Google Scholar]