Abstract
PURPOSE
To distinguish between corneal ectasia and contact lens–related warpage by characteristic patterns on corneal topography and optical coherence tomography (OCT) epithelial thickness maps.
SETTING
Casey Eye Institute, Portland, Oregon, USA.
DESIGN
Prospective and retrospective case series.
METHODS
Axial and mean power maps were obtained on corneal topography systems. Epithelial thickness maps were generated using RTVue OCT. A sector divider was applied to all maps. The locations of the minimum epithelial thickness, maximum epithelial thickness, maximum axial power, and maximum mean power were determined based on sector averages. Agreement was defined as the extremums occurring in the same or adjacent sectors.
RESULTS
Twenty-one eyes with keratoconus, 6 eyes with forme fruste keratoconus (better eye of asymmetric keratoconus), and 15 eyes with contact lens–related warpage were identified. The keratoconus and forme fruste keratoconus eyes had coincident topographic steepening with epithelial thinning. The locations of minimum epithelial thickness and maximum axial power agreed in 90% of the keratoconic eyes, while the minimum epithelial thickness and maximum mean power agreed in 95% of them. Conversely, the warpage eyes had coincident topographic steepening with epithelial thickening and normal pachymetry maps. The locations of maximum epithelial thickness and maximum axial power agreed in 93% of the warpage eyes, while the maximum epithelial thickness and maximum mean power agreed in all warpage eyes.
CONCLUSION
Results show that epithelial thickness maps and corneal topographic maps are powerful synergistic tools in evaluating eyes with abnormal topography and can help differentiate between keratoconus and nonectatic conditions.
Forme fruste keratoconus is the single greatest risk factor for the development of iatrogenic ectasia after laser vision correction.1 As such, detection of this early pre-ectatic condition is beneficial when screening the refractive surgery population. Whereas frank keratoconus is easily identifiable, the findings in early keratoconus are more subtle and primarily based on corneal topography.2–4 Nonprogressive and nonectatic conditions, such as contact lens warpage, can give similar topographic appearances, making clinical decision-making difficult in these suspect cases.5
Fourier-domain optical coherence tomography (OCT) can map both corneal and epithelial thicknesses, which are altered in ectasia.6–9 The corneal epithelium has a great amount of plasticity and acts as a low-pass smoothing filter over corneal irregularities.10 It thins over areas of relative increases in corneal curvature and thickens over areas of relative flattening in corneal curvature.11 This fact can be used to detect very early subclinical keratoconus.12–14 In fact, shifts in the epithelial thickness distribution might entirely mask early ectatic corneal changes.9
Contact lens–related warpage has long been known to mimic early ectasia changes on topography.5 We hypothesize that these topographic changes are the result of contact lens–induced epithelial remodeling, with epithelial thickening in the areas of topographic steepening. This is opposite the findings of early keratoconus, where epithelial thinning occurs in the areas of topographic steepening.12
In this study, we examined the relationship between epithelial thickness and corneal topography maps in patients with keratoconus or contact lens warpage to determine whether there is focal epithelial thickening associated with the areas of corneal steepening in contact lens warpage and contrasted this with the focal epithelial thinning associated with the areas of corneal steepening in keratoconus.
PATIENTS AND METHODS
The Institutional Review Board, Oregon Health Sciences University, reviewed and approved this study. This work complied with the U.S. Health Insurance Portability and Accountability Act of 1996 and adhered to the tenets of the Declaration of Helsinki.
Forme fruste keratoconus cases were the better eyes of patients with asymmetric keratoconus in which the keratoconus percentage index (KISA%) was normal (KISA% <60). Keratoconus cases were enrolled prospectively if they had a KISA% index greater than 100 and were excluded if they had late keratoconic changes such as hydrops or corneal scarring or had previous corneal surgery.15 Keratoconus and forme fruste keratoconus cases were included only if they had not worn contact lenses for 1 month before scan acquisition and had not had previous corneal surgery. Cases of contact lens warpage were identified retrospectively from patients presenting for refractive surgery evaluation based on characteristic inferior steepening on topography that resolved with contact lens discontinuation. Abnormality criteria included inferior–superior asymmetry greater than 0.80 diopter (D) or a 5.0 mm zone irregularity index greater than 1.00 D.
Imaging was performed with the RTVue OCT system (Optovue, Inc.). The “Pachymetry+Cpwr” scan pattern, which consists of 8 radial scans with a total scan area of 6.0 mm, was used. Epithelial thickness maps were generated by the OCT software.6 The scans were taken centered on the patient’s pupil. Corneal topography maps, including axial power and mean power, were obtained with Scheimpflug tomography (Pentacam HR, Oculus Optikgeräte GmbH) or scanning-slit topography (Orbscan II, Bausch & Lomb, Inc.).
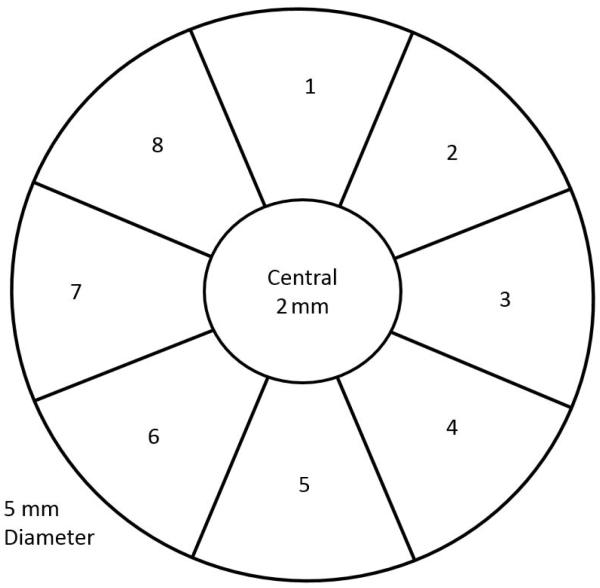
A 5.0 mm central sector map (Figure 1) that matched the sector map provided by the OCT software was applied to the axial power and mean power maps, and the location of the maximum axial power was recorded for all eyes based on sector averages. The location of the maximum mean power was identified when scanning-slit topography data were available. The location of the maximum epithelial thickness and minimum epithelial thickness were identified on the OCT epithelial thickness map based on sector averages. The outermost 5.0 mm to approximately 6.0 mm annular area was excluded because the readings there are less reliable.6 The central ring was considered adjacent to all sectors. The values of maximum epithelial thickness, minimum epithelial thickness, and average superior and inferior epithelial thickness were taken from the OCT report, and the central epithelial thickness was recorded as that within the central 2.0 mm area on the epithelial thickness map.
Figure 1.
Sector map used to determine the location of the maximum epithelial thickness and maximum corneal power.
Agreement between the maximum and minimum epithelial thickness and the maximum axial keratometry and maximum mean power was assessed in eyes with keratoconus, forme fruste keratoconus, and contact lens warpage. Agreement was defined as the extremums occurring in the same or adjacent sectors.
Because both eyes of most patients were included in this study, a generalized linear methods model to account for the interrelatedness between 2 eyes was used for continuous variables. For discreet variables, a logistic regression–based generalized estimating equation model was used. A P value less than 0.05 was considered statistically significant.
RESULTS
This study included 21 eyes of 13 patients with keratoconus, 6 eyes of 6 patients with forme fruste keratoconus, 15 eyes of 8 patients with contact lens warpage (8 eyes wearing rigid gas-permeable contact lenses, 7 eyes wearing soft toric contact lenses) and 18 normal eyes of 19 patients. No patient had previous corneal surgery. The mean manifest refractive error of the contact lens wearers was −7.2 ± 2.9 D (range −3.0 to −11.75 D) sphere and +0.9 ± 0.6 D (range 0.00 to +2.25 D) cylinder.
The OCT epithelial map showed a pattern of inferior thinning and superior thickening in the keratoconus group (Table 1). The keratoconus group and warpage group had wider ranges of epithelial thickness than the normal group, with significantly lower minimum and higher maximum values in the keratoconus group. There was no significant difference in the central values between the groups.
Table 1.
Epithelial thickness characteristics in contact lens–warpage and keratoconus groups.
| Mean (μm) ± SD | |||||
|---|---|---|---|---|---|
|
|
|||||
| Group | Minimum | Maximum | Superior* | Inferior† | Central |
| Warpage | 47 ± 7 | 57 ± 4 | 51 ± 4 | 52 ± 5 | 51 ± 6 |
| Keratoconus | 44 ± 5‡ | 63 ± 7‡ | 57 ± 4‡ | 51 ± 4‡ | 53 ± 5 |
| FFK | 50 ± 4 | 55 ± 5 | 53 ± 5 | 52 ± 5 | 53 ± 5 |
| Normal | 51 ± 3 | 57 ± 3 | 54 ± 3 | 55 ± 3 | 55 ± 3 |
FFK = forme fruste keratoconus
Superior values averaged from the 3 octants above the midline
Inferior values averaged from the 3 octants below the midline
Statistically different from normal (P < .01)
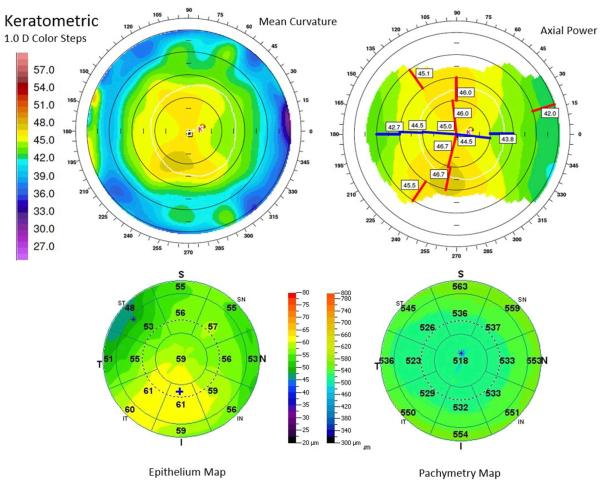
The characteristic topographic pattern associated with keratoconus is inferior or inferotemporal steepening (Figure 2). On the mean power map, this focal steepening is easier to appreciate as a simple small circular or elliptical region. On the axial power map, the pattern is more complex because of the interaction with the bowtie astigmatism pattern—it could appear as a skewed bowtie or claw shaped. The OCT epithelium map typically shows focal thinning in a distribution similar to the mean power map. In cases of forme fruste keratoconus with less obvious topographic abnormalities, this relationship also holds true (Figure 3).
Figure 2.
Keratoconus example. Top: Scanning-slit topography showing anterior topography. The mean curvature map shows focal inferotemporal steepening; the axial power map shows a complex claw pattern of steepening. Bottom: Optical coherence tomography maps show epithelial and pachymetric thinning over the area of increased mean curvature, confirming the inferotemporal location of cone apex. There is a ring of epithelial thickening at the base of the cone (I = inferior; IN = inferonasal; IT = inferotemporal; N = nasal; S = superior; SN = superonasal; ST = superotemporal; T = temporal).
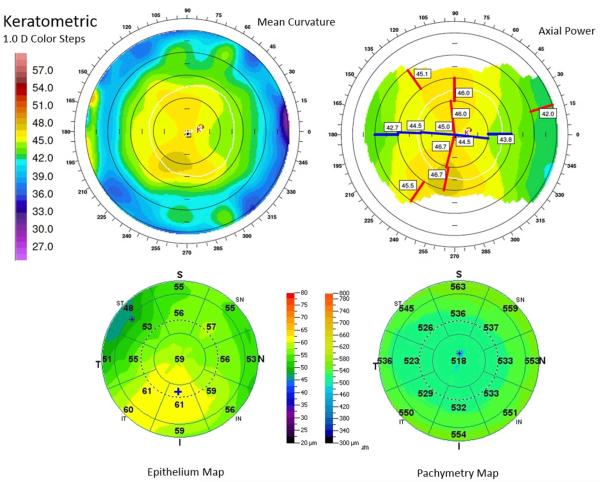
Figure 3.
Forme fruste keratoconus. Top: Scanning-slit topography showing anterior topography. The mean curvature map shows an inferotemporal area of increased curvature; the axial power map shows an asymmetric bowtie pattern of astigmatism. Bottom: Optical coherence tomography maps. There is epithelial and pachymetric thinning over the area of increased mean curvature (I = inferior; IN = inferonasal; IT = inferotemporal; N = nasal; S = superior; SN = superonasal; ST = superotemporal; T = temporal).
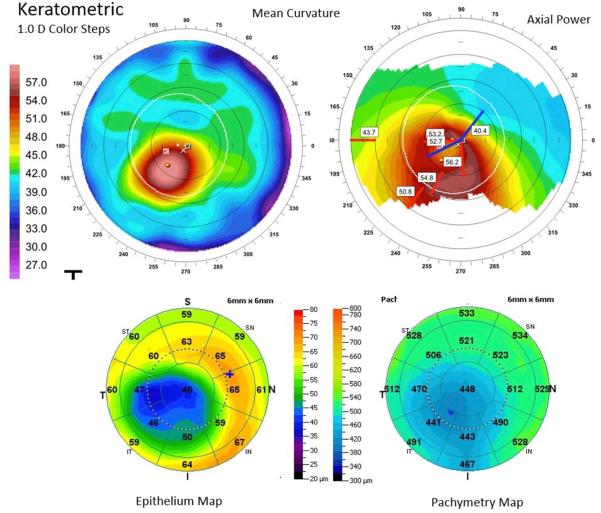
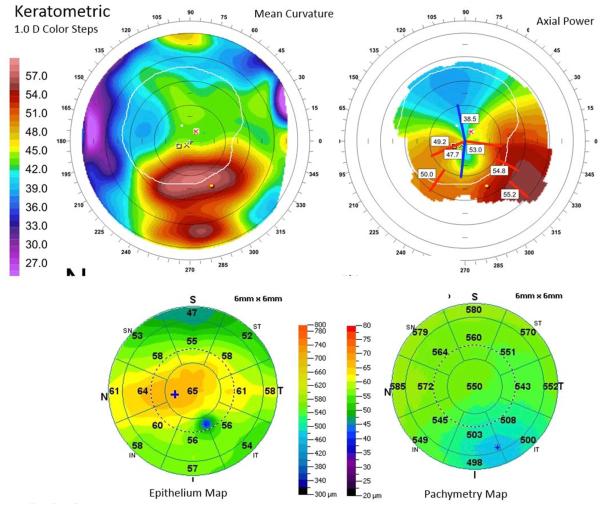
The characteristic pattern associated with contact lens-related corneal warpage (Figure 4) is focal topographic steepening associated with focal epithelial thickening. When the area of steepening is inferior (Figure 3) or inferotemporal, the topographic pattern can be indistinguishable from that of keratoconus. However, the focal epithelial thickening and lack of focal pachymetric thinning point to warpage rather than keratoconus.
Figure 4.
Example of contact lens warpage masquerading as topographic keratoconus. Top: Anterior topography from the 9.0 mm scanning-slit topographer. The mean curvature and axial curvature maps show inferior steepening; mild skewing of the steep axes is also shown on the axial map. Bottom: On the 6.0 mm OCT maps, the epithelial thickness map shows epithelial thickening in the area of steepening; the pachymetry map does not show inferior thinning (I = inferior; IN = inferonasal; IT = inferotemporal; N = nasal; S = superior; SN = superonasal; ST = superotemporal; T = temporal).
Sector mapping of corneal topography (Figure 1) and epithelial thickness maps in keratoconus and forme fruste keratoconus showed that focal epithelial thinning tended to occur in the same or adjacent sector as the location of maximum topographic steepening (Table 2). The agreement was almost perfect (95% for keratoconus and 83% for forme fruste keratoconus) when corneal steepening was defined by the location of the maximum mean power (also known as the mean curvature). The agreement was also good when corneal steepening was defined by the location of maximum axial power.
Table 2.
Agreement between the locations of epithelial thickness and topographic curvature extremums in keratoconus and contact lens warpage.*
| Number (%) | |||
|---|---|---|---|
|
|
|||
| Agreement | Keratoconus | FFK | CL Warpage |
| Max ET/Max MP | 4/21 (19) | 3/6 (50) | 11/11 (100) |
| Max ET/Max K | 4/21 (19) | 3/6 (50) | 14/15 (93) |
| Min ET/Max MP | 20/21 (95) | 5/6 (83) | 4/11 (36) |
| Min ET/Max K | 19/21 (90) | 5/6 (83) | 5/15 (33) |
CL = contact lens; FFK = forme fruste keratoconus; MaxET = maximum epithelial thickness; Max K = maximum axial keratometry; Max MP = maximum mean power; MinET = minimum epithelial thickness
Keratoconus and contact lens–warpage eyes showed widely different patterns, and these difference are statistically significant for all rows (P ≤ .005). The mean power map was not available in 4 eyes with warpage.
In 1 eye in the keratoconus group, the sector of minimum epithelial thickness did not coincide with maximum mean power (Figure 5). This exception, however, still partially conformed to the typical pattern. The epithelium showed focal thinning at the location of topographic steepening (cone apex). However, the area of apical epithelial thinning was small and fell between the inferior and inferotemporal sectors. The thinnest epithelium was in the superior sector; however, the superior epithelium was only 1 µ m thinner than the inferior and inferotemporal sectors.
Figure 5.
An exceptional case of partial disagreement between maximum curvature (upper left), maximum keratometry (upper right), and minimum epithelial thickness (lower left). Note that the epithelium thinned focally over the maximum mean power (cone apex) but that a separate area of epithelial thinning at the superior periphery defined the map’s sector minimum. The area of pachymetric thinning is more inferotemporally displaced than the spot of maximum mean power (I = inferior; IN = inferonasal; IT = inferotemporal; N = nasal; S = superior; SN = superonasal; ST = superotemporal; T = temporal).
Contact lens–related warpage showed the opposite association, with the location of focal epithelial thickening occurring in the same or adjacent sector as the location of maximum topographic steepening (Table 2). The agreement was perfect when corneal steepening was defined by the location of the maximum mean power. The agreement was also good when corneal steepening was defined by the location of the maximum axial power.
DISCUSSION
Many corneal conditions can present with abnormal topography. The abnormal corneal topography associated with forme fruste keratoconus, keratoconus, and post-refractive ectasia has been well described; however, other nonectatic conditions, such as contact lens warpage, mimic the topography seen in ectasia but are not progressive. Differentiating them in a clinical setting is essential to allow appropriate selection of corneal refractive surgery candidates and to select patients who might have a progressive condition and who could benefit from corneal collagen crosslinking.
Corneal epithelial thickness mapping is a relatively new diagnostic technique, and its usefulness in the diagnosis of keratoconus,6 subclinical keratoconus,12,13 and ectasia after myopic refractive surgery7,8 has been described. Previous studies6,12 have shown examples in which the thinnest epithelium coincided with the cone apex (location of maximum corneal curvature). Similarly, in ectasia after refractive surgery, the epithelium thins over the steepest portion of the cornea.8 However until now, there did not appear to have been a systematic study to show whether this association holds in keratoconus eyes. In the keratoconus eyes in this study, we found that this association holds when the cone apex is defined as the location of the maximum mean power.
The focal epithelial thinning seen at the apex of the cone is likely a direct response to curvature. A mathematical model of the epithelial response to local corneal curvature has been described in the context of corneal curvature change in response to keratorefractive surgery.10 Thus, the mean curvature map, in contrast to the axial power map, is best predictive of the overlying corneal epithelial thickness in an eye that does not wear a contact lens. The axial power map, which is the common map available on Placido disk topographers, measures the local slope relative to an optical axis and, unlike the mean power map, is very sensitive to astigmatism. This causes the axial power map in a keratoconic eye to usually appear as a complex pattern of focal steepening superimposed on bowtie astigmatism and is therefore not a reflection of the true curvature.16 Our results show that the location of the maximum axial power is not as reliably associated with focal epithelial thinning as the maximum mean curvature. The topographic mean power map, which is calculated from the mean curvature, might better define the location of the cone apex.
Chronic contact lens wear can induce topographic abnormalities that can mimic ectasia.17 Epithelial thickness maps in contact lens–induced warpage have not, to our knowledge, been previously described in the literature. We found here that in cases of contact lens warpage, there was epithelial thickening corresponding to the location of topographic steepening. This is in direct contrast to the epithelial thinning over the area of steepening that is seen with the ectatic conditions and can be used in a clinical setting, along with corneal pachymetry mapping, to differentiate warpage from an ectatic condition.
Coincident epithelial thinning and topographic flattening have been described in the orthokeratology literature.18,19 In this study, we describe the association between topographic steepening and epithelial thickening in contact lens–related warpage. Combined, these 2 observations suggest that topographic curvature is inversely related to epithelial thickness in contact lens warpage. It is possible that other diseases that modulate epithelial thickness without distorting the stroma, such as dry eye and epithelial basement membrane dystrophy, would also lead to similar topographic distortions. As in the case of keratoconus, we found that the correlation between the topography and epithelial maps is better when topography is represented by the mean power rather than the axial power.
Our criterion for location agreement is the minimum epithelial thickness (or maximum epithelial thickness) and the maximum mean power (or maximum keratometry) found in the same sector or adjacent sectors. This is a loose criterion because the sectors are relatively large. This was necessary because of the difference between the pupil centration of the OCT scans and the apex centration of the topography. In a separate recent publication,20 our group described the use of the epithelial and topographic pattern deviation maps to develop quantitative metrics to differentiate warpage from ectasia in which recentration of topography maps was performed. We did not attempt recentration of OCT or topography maps in this study because it required special computer programs to export and reanalyze the OCT and topographic data files. The purpose of this study was to develop an easy-to-use guideline for clinicians to differentiate warpage from ectasia. The proposed guideline requires only visual evaluation and side-by-side comparison of the topography and epithelial maps, which would be an advantage in a busy clinic. Eventually, the best solution might be to measure the topography using the same OCT machine so that computerized analysis of topographic and epithelial maps can be easily performed.
In conclusion, the epithelial map was useful in differentiating between ectasia and pseudo-ectasia caused by contact lens–related warpage identified on corneal topography. Topographic steepening was associated with focal epithelial thinning in keratoconus and other ectatic condition; however in warpage, the reverse was true and the steepening was associated with focal epithelial thickening. This information is complements the pachymetry map, which also helped identify ectasia by detecting focal thinning. Optical coherence tomography was found to be a reliable tool for detecting changes in the epithelial thickness maps in this study, although other technologies could also be used.9 Our results also showed that the mean power map might define topographic steepening more reliably than the axial power map and might deserve greater use clinically. Thus, corneal OCT and topography maps are powerful synergistic tools to help clinicians discern the true underlying condition in corneas with irregular surfaces.
WHAT WAS KNOWN.
Forme fruste keratoconus is the most important risk factor for ectasia after laser in situ keratomileusis and often presents a diagnostic challenge to contact lens wearers.
Optical coherence tomography epithelial mapping is a new technology that is more sensitive to subclinical keratoconus than conventional topography indices.
WHAT THIS PAPER ADDS
Topographic corneal steepening was associated with focal epithelial thinning in keratoconus but with epithelial thickening in warpage. By combining OCT and topography, a tripartite classification of normal, keratoconus, and warpage can be achieved.
Acknowledgments
Supported by U.S. National Institutes of Health, Bethesda, Maryland (grants R01 EY018184 and P30 EY010572(, a grant from Optovue, Inc., Freemont, California, and unrestricted departmental funding from Research to Prevent Blindness, New York, New York, USA.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures: Drs. Tang, Li, and Huang have significant financial interests in Optovue, Inc., a company that may have a commercial interest in the results of this research and technology. This potential individual conflict of interest has been reviewed and managed by the Oregon Health & Science University. No other author has a financial or proprietary interest in any material or method mentioned.
REFERENCES
- 1.Randleman JB, Russell B, Ward MA, Thompson KP, Stulting RD. Risk factors and prognosis for corneal ectasia after LASIK. Ophthalmology. 2003;110:267–275. doi: 10.1016/S0161-6420(02)01727-X. [DOI] [PubMed] [Google Scholar]
- 2.Li X, Rabinowitz YS, Rasheed K, Yang H. Longitudinal study of the normal eyes in unilateral keratoconus patients. Ophthalmology. 2004;111:440–446. doi: 10.1016/j.ophtha.2003.06.020. [DOI] [PubMed] [Google Scholar]
- 3.Rabinowitz YS. Videokeratographic indices to aid in screening for keratoconus. J Refract Surg. 1995;11:371–379. doi: 10.3928/1081-597X-19950901-14. [DOI] [PubMed] [Google Scholar]
- 4.Kanellopoulos AJ, Asimellis G. Forme fruste keratoconus imaging and validation via novel multi-spot reflection topography. Case Rep Ophthalmol. 2013;4:199–209. doi: 10.1159/000356123. Available at: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3843937/pdf/cop-0004-0199.pdf. Accessed October 30, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wilson SE, Lin DTC, Klyce SD, Reidy JJ, Insler MS. Topographic changes in contact lens-induced corneal warpage. Ophthalmology. 1990;97:734–744. doi: 10.1016/s0161-6420(90)32516-2. [DOI] [PubMed] [Google Scholar]
- 6.Li Y, Tan O, Brass R, Weiss JL, Huang D. Corneal epithelial thickness mapping by Fourier-domain optical coherence tomography in normal and keratoconic eyes. Ophthalmology. 2012;119:2425–2433. doi: 10.1016/j.ophtha.2012.06.023. Available at: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3514625/pdf/nihms389040.pdf. Accessed October 30, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kanellopoulos AJ, Aslanides IM, Asimellis G. Correlation between epithelial thickness in normal corneas, untreated ectatic corneas, and ectatic corneas previously treated with CXL; is overall epithelial thickness a very early ectasia prognostic factor? Clin Ophthalmol. 2012;6:789–800. doi: 10.2147/OPTH.S31524. Available at: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3373227/pdf/opth-6-789.pdf. Accessed October 30, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rocha KM, Perez-Straziota CE, Stulting RD, Randleman JB. SD-OCT analysis of regional epithelial thickness profiles in keratoconus, postoperative corneal ectasia, and normal eyes. J Refract Surg. 2013;29:173–179. doi: 10.3928/1081597X-20130129-08. errata, 234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Reinstein DZ, Archer TJ, Gobbe M. Corneal epithelial thickness profile in the diagnosis of keratoconus. J Refract Surg. 2009;25:604–610. doi: 10.3928/1081597X-20090610-06. [DOI] [PubMed] [Google Scholar]
- 10.Huang D, Tang M, Shekhar R. Mathematical model of corneal surface smoothing after laser refractive surgery. Am J Ophthalmol. 2003;135:267–278. doi: 10.1016/s0002-9394(02)01942-6. [DOI] [PubMed] [Google Scholar]
- 11.Dillon EC, Eagle RC, Jr, Laibson PR. Compensatory epithelial hyperplasia in human corneal disease. Ophthalmic surgery. 1992;23:729–732. [PubMed] [Google Scholar]
- 12.Li Y, Chamberlain WD, Tan O, Brass R, Weiss JL, Huang D. Subclinical keratoconus detection by pattern analysis of corneal and epithelial thickness maps with optical coherence tomography. J Cataract Refract Surg. 2016;42:284–295. doi: 10.1016/j.jcrs.2015.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kanellopoulos AJ, Asimellis G. OCT corneal epithelial topographic asymmetry as a sensitive diagnostic tool for early and advancing keratoconus. Clin Ophthalmol. 2014;8:2277–2287. doi: 10.2147/OPTH.S67902. Available at: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4242699/pdf/opth-8-2277.pdf. Accessed October 30, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kanellopoulos AJ, Asimellis G. OCT-derived comparison of corneal thickness distribution and asymmetry differences between normal and keratoconic eyes. Cornea. 2014;33:1274–1281. doi: 10.1097/ICO.0000000000000275. [DOI] [PubMed] [Google Scholar]
- 15.Rabinowitz YS, Rasheed K. KISA% index: a quantitative videokeratography algorithm embodying minimal topographic criteria for diagnosing keratoconus. J Cataract Refract Surg. 1999;25:1327–1335. doi: 10.1016/s0886-3350(99)00195-9. errata, 2000; 26:480. [DOI] [PubMed] [Google Scholar]
- 16.Tang M, Shekhar R, Miranda D, Huang D. Characteristics of keratoconus and pellucid marginal degeneration in mean curvature maps. Am J Ophthalmol. 2005;140:993–1001. doi: 10.1016/j.ajo.2005.06.026. [DOI] [PubMed] [Google Scholar]
- 17.Lebow KA, Grohe RM. Differentiating contact lens induced warpage from true keratoconus using corneal topography. CLAO J. 1999;25:114–122. [PubMed] [Google Scholar]
- 18.Reinstein DZ, Gobbe M, Archer TJ, Couch D, Bloom B. Epithelial, stromal, and corneal pachymetry changes during orthokeratology. Optom Vis Sci. 2009;86:E1006–E1014. doi: 10.1097/OPX.0b013e3181b18219. [DOI] [PubMed] [Google Scholar]
- 19.Lian Y, Shen M, Jiang J, Mao X, Lu P, Zhu D, Chen Q, Wang J, Lu F. Vertical and horizontal thickness profiles of the corneal epithelium and Bowman’s layer after orthokeratology. Invest Ophthalmol Vis Sci. 2013;54:691–696. doi: 10.1167/iovs.12-10263. Available at: http://iovs.arvojournals.org/article.aspx?articleid=2189438. Accessed October 30, 2016. [DOI] [PubMed] [Google Scholar]
- 20.Tang M, Li Y, Chamberlain W, Louie DJ, Schallhorn JM, Huang D. Differentiating keratoconus and corneal warpage by analyzing focal change patterns in corneal topography, pachymetry, and epithelial thickness maps. Invest Ophthalmol Vis Sci. 2016;57(9):OCT544–OCT549. doi: 10.1167/iovs.15-18938. Available at: http://iovs.arvojournals.org/article.aspx?articleid=2542546. Accessed October 30, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]