Abstract
Purpose
To report a case of bilateral cytomegalovirus (CMV) retinitis in an otherwise healthy infant.
Methods
A four-month-old, healthy, male infant was evaluated for visual inattention.
Results
This full-term infant with a normal birth weight and an uneventful gestational period was referred with symptoms of visual inattention, fever, and agitation one week prior to admission. Ocular involvements were detected in the form of bilateral pan uveitis with diffuse bilateral retinitis and vasculitis with hemorrhage in the peripheral retina and posterior pole. CMV DNA was detected in the patient's ocular sample and cerebrospinal fluid by polymerase chain reaction (PCR). He was treated with intravitreal and systemic ganciclovir. Unfortunately, the infant died because of CMV encephalitis. Therefore, bilateral CMV retinitis (CMVR), which was probably transmitted from the mother, was diagnosed in this immunocompetent infant.
Conclusions
The present case highlights the possibility of CMVR in immunocompetent infant associated with systemic CMV infection, even during the postnatal period. Therefore, a high index of clinical suspicion and prompt treatment may be life-saving in similar cases.
Keywords: Cytomegalovirus, Retinitis, Ganciclovir
Introduction
Cytomegalovirus (CMV) infection is the most common congenital infection around the world, affecting 1% of live births in the United States. The incidence of this infection is speculated to rise to 5% of seropositive newborns in developing countries.1 CMV retinitis (CMVR) is less common among children than adults.
CMV infection could be either a congenital or an acquired infection in the postnatal period. Postnatal CMV infection can be transmitted through vaginal secretions, contact with infected individuals, blood transfusion, or breast milk which is the most common route of transmission.2 This infection, in terms of neonates, is usually asymptomatic, whereas in premature or immunocompromised infants, can lead to a broad spectrum of symptoms, including life-threatening conditions.3
CMVR is mainly associated with acquired immunodeficiency syndrome (AIDS).4, 5, 6 Besides AIDS and human immunodeficiency virus (HIV), other immunosuppressive conditions such as severe combined immunodeficiency are associated with CMVR in children. Moreover, this infection has been reported in patients undergoing bone marrow transplants and chemotherapy.7, 8 Surprisingly, CMVR has been detected in individuals without any evidence of immunodeficiency.9, 10
Herein, we present the case of a healthy, full-term infant, who presented with CMVR and died due to the involvement of the central nervous system (CNS).
Case report
We present the case of a four-month-old, healthy, male infant, referring to us. The patient had symptoms such as visual inattention, fever, and agitation one week prior to admission. This full-term infant had a normal birth weight, with an uneventful gestational period; it should be noted that the patient was born via vaginal delivery.
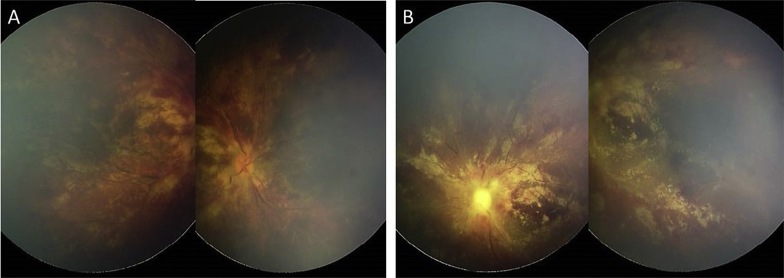
Ocular involvement was detected in form of bilateral pan uveitis with diffuse bilateral retinitis, vasculitis, and hemorrhage in the peripheral retina and posterior pole (Fig. 1, Fig. 2). Fundus images were captured, using a Ret Cam 120 wide-field digital fundus camera (Clarity Medical Systems Inc., Pleasanton, CA, USA).
Fig. 1.
RetCam fundus photography (composite) at first presentation shows retinitis, severe vasculitis, diffuse retinal hemorrhages, and optic disc paleness in the right (A) and the left eyes (B).
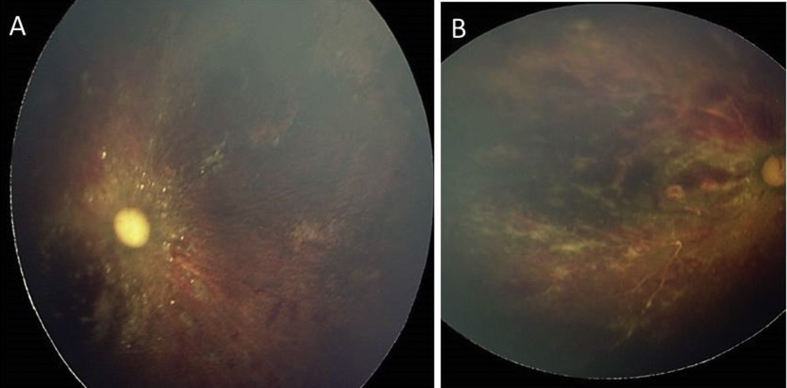
Fig. 2.
The last RetCam fundus photography discloses no significant change in the right (A) and the left eyes (B) after treatment.
The patient's history of medical and ocular conditions was unremarkable. Prenatal and 1st trimester screening tests were normal with negative CMV serology. However, the mother had a previous history of fever and malaise in the eighth month of pregnancy, which remained undiagnosed. The mother was presumed immunocompetent without any remarkable past medical history.
With a suspicion of infectious retinitis (especially CMVR), a sample of the anterior chamber was used for polymerase chain reaction (PCR) assay of herpes simplex virus (HSV), varicella-zoster virus (VZV), CMV, and toxoplasmosis. Intravitreal ganciclovir (1 mg/0.1 cc) was injected in the right eye at the same time.
The results of systemic workup and laboratory tests evaluating the immune system were normal, except for CMV infection. CMV DNA was detected in the patient's ocular sample and cerebrospinal fluid (CSF) (via PCR). Lab tests were performed to rule out immunodeficiency in the mother, the results of which were inconclusive except for the serologic tests which revealed positive immunoglobulin G (IgG) for CMV with negative IgM (seroconversion). The blood CMV antigen (e.g. antigen pp 65) was not evaluated for his mother. Therefore, bilateral CMVR, which was probably transmitted from the mother within the final days of pregnancy, was diagnosed in this healthy infant.
Accordingly, intravenous ganciclovir (10 mg/kg/day) was commenced. Intravitreal injection of ganciclovir (1 mg/0.1 cc) was performed twice a week in both eyes, three injection in each one (Fig. 2 A & B). The patient was admitted to the neonatal intensive care unit, and treatment, along with diagnostic workup for possible immunodeficiency, was continued.
The following laboratory test results were unremarkable in the patient: abdominal ultrasonography, liver function tests, chest X-ray, complete blood cell count, lymphocyte count (i.e., CD4 and CD8), HIV test, hepatitis B surface antigen (HBs Ag) test, hepatitis C virus antibody test, toxoplasma serology, and peripheral blood smear test.
Only CNS involvement was reported in the patient, which led to generalized paralysis, hypotonia, poor feeding, lethargy, and finally death. No intracranial calcification or microcephaly was reported in the patient. Despite proper treatment, the infant died due to CMV encephalitis.
The patient's father provided written consent for publication of personal information including medical record details and photographs.
Discussion
The present case is of considerable interest, owing to the diagnosis of CMVR in an otherwise healthy infant. The infant's infection, associated with CNS involvement, was most probably due to perinatal infection or transmission via breast feeding, which led to the patient's death.
The proposed patterns of CMVR are more diverse in infants, compared to adults. In this regard, Baumal et al. reported a series of nine immunocompromised children with CMVR below 16 years of age. Bilateral (89%) and posterior pole involvements were reported in all cases, with at least one affected eye11, 12; ophthalmoscopic findings in the present case were similar to the mentioned study.
Unlike the present case, low CD4 count (<50 cell/mL) has been introduced as a predictive index for the development of CMV infection.13 The pattern of congenital CMVR differs from the acquired adult type, and the fundus manifestations may vary from subtle white flecks to more florid presentations with white infiltrates (accompanied by hemorrhage). Overall, congenital CMV is typically less hemorrhagic and less progressive than the acquired type in immunocompromised children.7, 8 Surprisingly, the presentation of this hemorrhagic case was suggestive of a postnatally-acquired infection rather than a congenitally perinatal infection. Regardless of the clinical features, we believe this otherwise healthy infant was probably affected by perinatal maternal transmission during the eighth month of pregnancy, addressed by sero-conversion in his mother. The unique feature in our case is a late manifestation of perinatal infection with four months delay after birth. It seems that primary infection at the last month of pregnancy may put the infant at greater risk of developing a more severe disease, while sufficient time has not elapsed in mother for production and transference of protective antibodies via placenta.
As for other possible routes of infection in this scenario, we can name breast feeding, vaginal delivery, and contact with infected carrier. Assuming acquisition of the CMV postnatally, then inadequate re-stimulation of immune system and enhancement of antibody production or higher viral load of CMV, can be named as main reasons.
A higher incidence of CMV encephalitis has been reported in patients with CMVR, especially peri-papillary CMVR, as reported in the present case. Therefore, evaluation of high-risk children, requiring prompt CMVR treatment, is important for the prevention of long-term visual morbidities.9, 10
The majority of patients with congenital CMV infection are asymptomatic. A 10–15% mortality rate has been reported in symptomatic infants. The survivors often suffer from long-term sequelae such as cerebral palsy, developmental delays, hearing loss, epilepsy, ocular abnormalities, and microcephaly. Also, the clinical manifestations of intrauterine infection include hepatosplenomegaly, jaundice, thrombocytopenia, periventricular calcification, and chorioretinitis.3, 7, 8
In the present case, the infant was speculated to be perinatally affected by CMV infection in the third trimester of pregnancy. The unique features of the present case included the patient's negative history of immunosuppression and the time gap between birth and appearance of clinical manifestations. Unfortunately, the patient's poor response to systemic medications and delayed treatment resulted in the patient's death.
The present case highlights the possible mortality associated with CMV infection, even during the postnatal period. Therefore, a high index of clinical suspicion and prompt treatment may be life-saving in similar cases.
Footnotes
Source(s) of support: None.
Presentation at a meeting: None.
Conflicts of interest: The authors declare no conflicts of interest.
Peer review under responsibility of the Iranian Society of Ophthalmology.
References
- 1.Kadambari S., Williams E., Luck S., Griffiths P., Sharland M. Evidence based management guidelines for the detection and treatment of congenital CMV. Early Hum Dev. 2011;87(11):723–728. doi: 10.1016/j.earlhumdev.2011.08.021. [DOI] [PubMed] [Google Scholar]
- 2.Manicklal S., Emery V.C., Lazzarotto T., Boppana S.B., Gupta R.K. The “silent” global burden of congenital cytomegalovirus. Clin Microbiol Rev. 2013;26(1):86–102. doi: 10.1128/CMR.00062-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Whitley R.J. The use of antiviral drugs during the neonatal period. Clin Perinatol. 2012;39(1):69–81. doi: 10.1016/j.clp.2011.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tawse K.L., Baumal C.R. Intravitreal foscarnet for recurring CMV retinitis in a congenitally infected premature infant. J Am Assoc Pediatr Ophthalmol Strabismus. 2014;18(1):78–80. doi: 10.1016/j.jaapos.2013.09.015. [DOI] [PubMed] [Google Scholar]
- 5.Voigt S., Michel D., Kershaw O. Fatal reactivation of postnatal cytomegalovirus infection with rapid emergence of ganciclovir resistance in an infant after allogeneic stem cell transplantation. J Clin Microbiol. 2005;43(7):3551–3554. doi: 10.1128/JCM.43.7.3551-3554.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rahbarimanesh A., Ehsani M., Karahroudi M. Cytomegalovirus disease in children with acute lymphoblastic leukemia in the nontransplant setting: case series and review of the literature. J Pediatr Hematol/Oncol. 2015;37(6):429–432. doi: 10.1097/MPH.0000000000000298. [DOI] [PubMed] [Google Scholar]
- 7.Leung A.K., Sauve R.S., Davies H.D. Congenital cytomegalovirus infection. J Natl Med Assoc. 2003;95(3):213. [PMC free article] [PubMed] [Google Scholar]
- 8.Mota A., Breda J., Silva R., Magalhães A., Falcão-Reis F. Cytomegalovirus retinitis in an Immunocompromised Infant: a case report and review of the literature. Case Rep Ophthalmol. 2011;2(2):238–242. doi: 10.1159/000330550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ross S.A., Boppana S.B., editors. Congenital Cytomegalovirus Infection: Outcome and Diagnosis. Seminars in Pediatric Infectious Diseases. Elsevier; 2005. [DOI] [PubMed] [Google Scholar]
- 10.Vishnevskia-Dai V., Shapira Y., Rahav G., Shimoni A., Somech R., Moisseiev J. Cytomegalovirus retinitis in HIV-negative patients: a practical management approach. Ophthalmology. 2015;122(4):866. doi: 10.1016/j.ophtha.2014.11.010. [DOI] [PubMed] [Google Scholar]
- 11.Foster C.S., Vitale A.T. JP Medical Ltd; 2013. Diagnosis & Treatment of Uveitis. [Google Scholar]
- 12.Baumal C.R., Levin A.V., Read S.E. Cytomegalovirus retinitis in immunosuppressed children. Am J Ophthalmol. 1999;127(5):550–558. doi: 10.1016/s0002-9394(99)00031-8. [DOI] [PubMed] [Google Scholar]
- 13.Tuncer S., Oray M., Yildirim Y., Camcioglu Y., Tugal-Tutkun I. Bilateral intraocular calcification in necrotizing cytomegalovirus retinitis. Int Ophthalmol. 2014;34(5):1119–1122. doi: 10.1007/s10792-014-9917-9. [DOI] [PubMed] [Google Scholar]