Abstract
Purpose
To investigate the effect of omega-3 polyunsaturated fatty acid supplement on qualitative and quantitative subjective (ocular surface disease index [OSDI]) and objective (Schirmer's test, tear break up time [TBUT], and tear osmolarity) dry eye indices after cataract surgery.
Methods
In this randomized clinical study, 61 eyes of 48 patients complaining of new onset dry eye symptoms after phacoemulsification were enrolled. Subjects were randomly allocated into two groups using urn randomization. Controls received conventional treatment. The treatment group received omega-3 dietary supplement in addition to conventional therapy.
Results
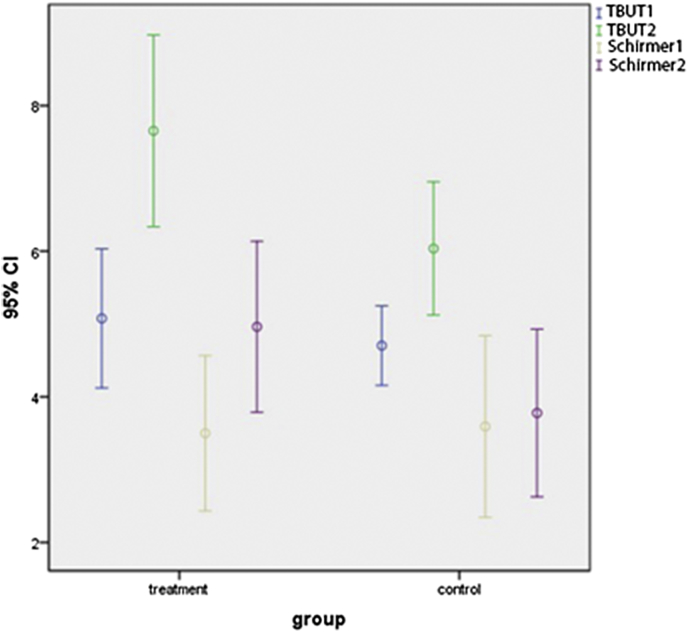
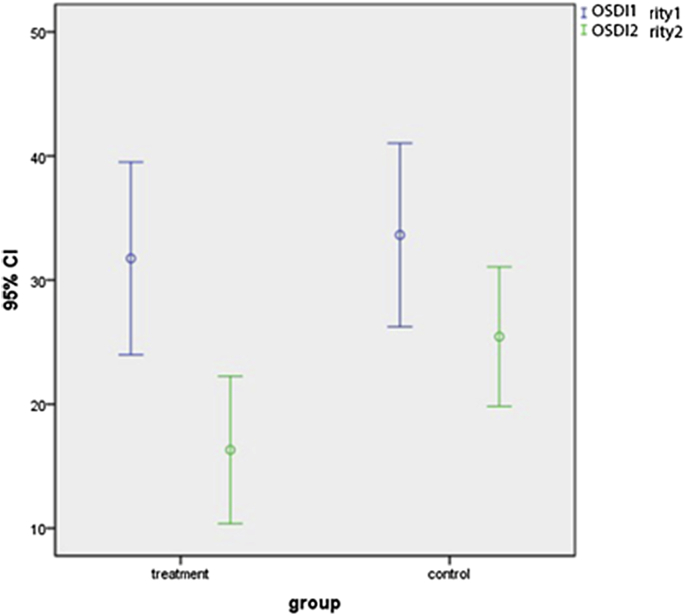
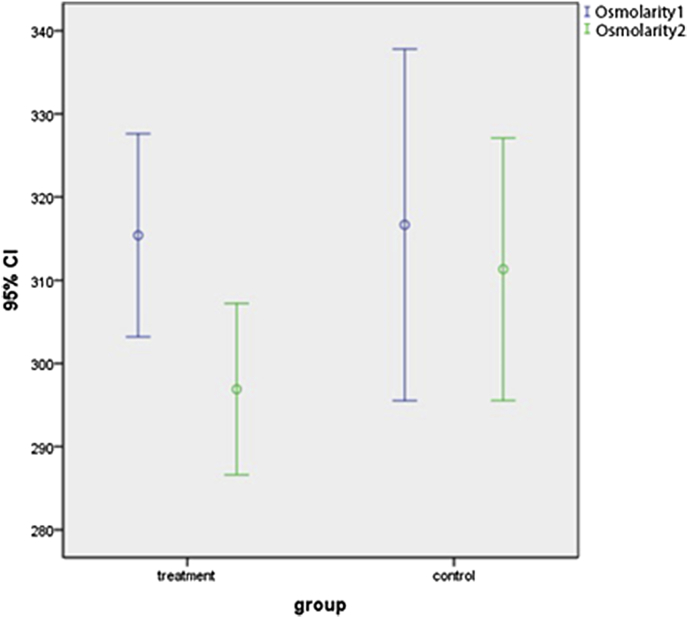
There was no significant difference between the control and treatment groups in pre-treatment indices of Schirmer (3.50 ± 3.13 and 2.96 ± 3.39, respectively, P = 0.582), TBUT (6.67 ± 1.36 and 4.87 ± 2.22, respectively, P = 0.687), osmolarity (316.66 ± 8.50 and 315.4 ± 17.06, respectively, P = 0.906), and OSDI (32.99 ± 19.03 and 35.32 ± 18.99, respectively, P = 0.635).
Mean pre-treatment OSDI in the control group was 32.99 ± 19.03, which improved significantly after treatment to 25.43 ± 14.49 (P = 0.003). The mean pre-treatment OSDI in the treatment group was 35.32 ± 18.99 (range: 7.5–77.77), which improved significantly after treatment to 16.31 ± 13.72 (range: 2.77–47.22) (P < 0.001). OSDI improvement was significantly higher in the treatment group than the control group (P = 0.026).
TBUT improved in both the control and treatment groups after treatment (P < 0.001). However, TBUT was affected significantly more in the treatment group compared with the control group (P = 0.038).
Mean tear film osmolarity in the control group was 316.67 ± 8.50 (range: 308–325), which improved insignificantly after treatment to 311.33 ± 6.35 (range: 304–315) (P = 0.157). Mean pre-treatment tear film osmolarity in the treatment group was 315.40 ± 17.06 (range: 279–340), which improved significantly after treatment to 296.90 ± 14.39 (range: 260–310) (P < 0.001). Also, post-treatment Schirmer results between the two groups were not statistically significant (P = 0.155).
Conclusion
Omega-3 dietary supplements have an additive effect on tear film indices of patients with dry eye syndrome after phacoemulsification.
Keywords: Polyunsaturated fatty acids, Omega-3, Dry eye, Cataract surgery
Introduction
Dry eye is a chronic multifactorial disorder, and is characterized by ocular surface inflammation and inadequate production of tears.1, 2, 3 It is the most common cause of ophthalmology visits in daily practice and has recently been noticed as a major problem in public health.4, 5, 6 Dry eye is an important complication of intraocular surgeries including cataract surgery (phacoemulsification).7, 8 This complication can lead to patient dissatisfaction even after a non-complicated cataract surgery.9, 10, 11, 12 Patients are more likely to complain from discomfort, burn, itching, red eye, photophobia, or even temporary blurring of vision.13, 14
The etiology of dry eye after cataract surgery is not clearly understood; however, various mechanisms have been proposed that might affect ocular surface environment after phacoemulsification and contribute to the development of dry eye. Eye drops and topical anesthesia containing preservatives such as benzalkonium chloride have been proven to negatively affect the corneal epithelium.15, 16 Exposure to the light emitted from the operating microscope might be another factor causing dry eye after surgery.15 The normal organization of the corneal innervation can also be disrupted during the procedure that might lead to pathologic changes of the cornea and, consequently, the discomforts associated with dry eye.17
As time passes after surgery, inflammation decreases, and patients' symptoms alleviate. We should notice this critical early postoperative period and manage the dry eye-related symptoms. In this period, topical artificial tears and low potent steroids are the most common drugs to control inflammation and dry eye symptoms. The problem with artificial tears is their incomplete and temporary effect. The problem with topical steroids is their long list of side effects in long-term use, so it would be desirable to control inflammation with an alternative steroid sparing drug like anti-inflammatory omega-3 supplements with evidence in their different systemic benefits in elderly patients.18, 19
Docosahexaenoic acid (DHA) is an essential omega-3 polyunsaturated fatty acid that is necessary for the development of cognitive functions, reducing the risk factor for cardiovascular diseases, decreasing acute and chronic inflammation, and inducing anti-microbial resistance.18, 19 Mounting evidence also has shown potential advantages of polyunsaturated fatty acid on the human eye.19, 20, 21, 22
Artificial tears are the mainstay of treatment in this condition, but only yield temporary and partial relief. Dietary intake of essential fatty acids is an alternative treatment in patients with dry eye. These fatty acids are the precursors for the synthesis of eicosanoids, i.e. prostaglandins, thromboxanes, and leukotrienes, which play important roles in inflammatory cascades. Arachidonic acid (AA) is converted into 2-series prostaglandins and 4-series leukotrienes via the cyclooxygenase and 5-lipoxygenase enzymes, respectively. The production of these AA-derived mediators can be decreased by the dietary intake of omega-3 fatty acid or eicosapentaenoic acid (EPA) through a process of competitive enzyme inhibition, shifting the balance towards a less inflammatory state.23 The effectiveness of anti-inflammatory omega-3 polyunsaturated fatty acids in the treatment of dry eye syndrome has been shown in multiple studies.24, 25, 26, 27, 28 However, few have simultaneously assessed the changes in tear film osmolarity, ocular surface disease index (OSDI), tear break up time (TBUT), and Schirmer's test in patients taking omega-3 fatty acids supplementation as an adjuvant treatment for dry eye syndrome following cataract surgery in a clinical trial. Accordingly, to do so, we aimed to conduct the present survey.
Methods
All patients with new onset dry eye symptoms (foreign body sensation, burning, itching, red eye, photophobia, or blurring of vision) with a history of recent cataract surgery via phacoemulsification were enrolled in this study. Patients were recruited between September 2013 and May 2014 during ophthalmologic appointments at the study center. Exclusion criteria of this study were history of ocular trauma, uveitis, other previous ocular surgeries, contact lens wearing in the previous 2 years, systemic diseases that are associated with dry eye syndrome including diabetes, rheumatoid arthritis and Sjogren's syndrome, existing dry eye symptoms prior to cataract surgery, and considerable change in lifestyle with an impact on ocular surface diseases (e.g., computer use) during the postoperation period.
This study was a parallel group randomized controlled trial and conducted based on principles of the Declaration of Helsinki. The study protocol was supervised and approved by the Ethical Committee of Tehran University of Medical Sciences. Iran Registry of Clinical Trials (IRCT) Number: 2013062413567.
Utilizing the above formula,29 α = 0.05, β = 0.2 (CI = 95% and power = 80%) and also considering previous studies, the expected difference of osmolarity of d = 13 between the two groups was σ = 8. The sample size was calculated with 20 patients in each group. However, in order to reduce the risk of loss to follow-up, we decided to recruit at least 30 patients in each group.
Patients were randomly allocated into two groups using urn randomization. In the control group, patients were treated with standard therapy of dry eye (Artelac artificial tears every 4 h – Dr. Gerhard Mann company, Germany – and Betamethasone 0.1% eye drops every 8 h) for one month. In the treatment group, omega-3 dietary supplement (1000 mg every 8 h, Advanced® Canada, each capsule containing 180 mg EPA and 120 mg DHA) was added to conventional therapy. Patients filled the standard questionnaire for OSDI, which is an instrument to quantify the severity of dry eye symptoms. OSDI questionnaire was scored from 0 to 100 (100 being the most severe disease). All measurements were done by a single person (M.M), and the physician in charge of collecting outcome data was kept blinded to the allocation.
TBUT was done after instillation of 5 μL of 2% sodium fluorescein without any irritation and manipulation of the patients' ocular surface. We measured the mean time between last blinking and the first appearance of a dark spot in tear film in slit-lamp examination. The mentioned test was repeated 3 times solely on the affected eye, and the mean value was recorded. Participants then waited for at least 45 min, and 5 min Schirmer's test without topical anesthesia was done. Tear osmolarity was measured obtaining 50 nL of patient's tear and using Tearlab™ osmometer. All examinations were done during morning hours, and the patients were prohibited from using any topical drugs for at least 3 h prior to visits. All statistical analyses were performed by SPSS (IBM Corp. Released 2013. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp.), using Student t-test, paired t-test and analysis of variance (ANOVA). A P-value of less than 0.05 was considered statistically significant.
Results
In total, sixty-three eyes of 48 patients met our inclusion criteria and were enrolled in this study. Among 63 eyes, 31 eyes were randomly allocated in the control group, and 32 eyes were placed in the treatment group; however, 2 eyes in the control group were excluded due to the missed follow-up, so, analysis was performed on 29 and 32 eyes. The difference between the mean postoperative time was 1.59 ± 1.58 years (range: 20 days to 7 years) in this study. There was not any statistically significant difference between the control and treatment groups with regard to the mean postoperative time (1.61 ± 1.60 and 1.57 ± 1.57 years, respectively, P = 0.930). Mean patient age in this study was 63.78 ± 11.74 years. Mean patient age in the control group was 67.81 ± 9.62 years (range: 39–81) and 59.75 ± 11.57 years (range: 37–82) in the treatment group, which was significantly different comparing the two groups (P = 0.003). Demographic data is presented in Table 1.
Table 1.
Demographic data.
| Characteristic | Control group | Treatment group | Overall |
|---|---|---|---|
| Age | 67.81 ± 9.62 years (range: 39–81) | 59.75 ± 11.57 years (range: 37–82) | 63.78 ± 11.74 years (range: 37–82) |
| P value: 0.003 | |||
| Sex | 17 (77%) females, 6 (23%) males | 21 (84%) females, 4 (16%) males | 38 (79.1%) females, 10 (20.9%) males |
| Eye | 13 (44.8%) OS, 16 (55.2%) OD | 16 (50%) OS, 16 (50%) OD | 29 (47.5%) OS, 32 (52.5%) OD |
| Mean post-operative time | 1.61 ± 1.60 years | 1.57 ± 1.57 years | 1.59 ± 1.58 years |
| P value: 0.930 | |||
As for baseline indices, there was no significant difference in TBUT, Schirmer's test, mean tear osmolarity, and mean OSDI between the two study groups (P = 0.687, P = 0.582, P = 0.906, and P = 0.635, respectively) (Table 2). These findings reflect the similarity between the two groups regarding dry eye severity.
Table 2.
Comparison of tear beak up time (TBUT), Schirmer, osmolarity and OSDI in treatment and control groups.
| Characteristic | Control/treatment | Control | Treatment | P |
|---|---|---|---|---|
| TBUT | Pre-treatment | 6.67 ± 1.36 s (3–8) | 4.87 ± 2.22 s (2–11) | 0.687 |
| Post-treatment | 6.03 ± 2.26 s (4–11) | 7.65 ± 3.26 s (2–15) | 0.038 | |
| Schirmer | Pre-treatment | 3.50 ± 3.13 mm (0–13) | 3.96 ± 3.39 mm (1–15) | 0.582 |
| Post-treatment | 3.85 ± 2.88 mm (1–15) | 4.96 ± 2.84 mm (1–11) | 0.155 | |
| Osmolarity | Pre-treatment | 316.66 ± 8.50 osmol/L (308–325) | 315.4 ± 17.06 osmol/L (279–340) | 0.906 |
| Post-treatment | 311.33 ± 6.35 osmol/L (304–315) | 296.9 ± 14.39 osmol/L (260–310) | 0.01 | |
| OSDI | Pre-treatment | 32.99 ± 19.03 (3.12–77.77) | 35.32 ± 18.99 (7.50–77.77) | 0.635 |
| Post-treatment | 25.43 ± 14.49 (0–58.33) | 16.31 ± 13.72 (2.77–47.22) | 0.026 |
TBUT: tear beak up time, OSDI: ocular surface disease index.
Mean pre-treatment TBUT in both the control and treatment groups improved significantly after treatment (P = 0.010 and P < 0.001, respectively). However, TBUT drift was significantly higher in the treatment group in comparison to the control (P = 0.038) (Table 3, Table 4).
Table 3.
Comparison of tear beak up time (TBUT), Schirmer, osmolarity and ocular surface disease index (OSDI) in control group.
| Characteristic | Mean ± SD (range) | Confidence interval 95% | P | |
|---|---|---|---|---|
| TBUT | Pre-treatment | 6.67 ± 1.36 s (3–8) | −2.32 to −3.39 | 0.010 |
| Post-treatment | 6.03 ± 2.26 s (4–11) | |||
| Schirmer | Pre-treatment | 3.50 ± 3.13 mm (0–13) | −0.81 to 0.44 | 0.551 |
| Post-treatment | 3.85 ± 2.88 mm (1–15) | |||
| Osmolarity | Pre-treatment | 316.66 ± 8.50 osmol/L (308–325) | −5 to 15.67 | 0.157 |
| Post-treatment | 311.33 ± 6.35 osmol/L (304–315) | |||
| OSDI | Pre-treatment | 32.99 ± 19.03 (3.12–77.77) | 3.14–13.24 | 0.003 |
| Post-treatment | 25.43 ± 14.49 (0–58.33) | |||
TBUT: tear beak up time, OSDI: ocular surface disease index.
Table 4.
Comparison of tear beak up time (TBUT), Schirmer, osmolarity and ocular surface disease index (OSDI) before and after treatment with omega-3.
| Characteristic | Mean ± SD (range) | Confidence interval 95% | P | |
|---|---|---|---|---|
| TBUT | Pre-treatment | 4.87 ± 2.22 s (2–11) | −3.63 to −1.51 | 0.0001 |
| Post-treatment | 7.65 ± 3.26 s (2–15) | |||
| Schirmer | Pre-treatment | 3.96 ± 3.39 mm (1–15) | −2.25 to 0.25 | 0.113 |
| Post-treatment | 4.96 ± 2.84 mm (1–11) | |||
| Osmolarity | Pre-treatment | 315.4 ± 17.06 osmol/L (279–340) | 11.74 to 25.25 | 0.0001 |
| Post-treatment | 296.9 ± 14.39 osmol/L (260–310) | |||
| OSDI | Pre-treatment | 35.32 ± 18.99 (7.50–77.77) | 9.64–21.19 | 0.0001 |
| Post-treatment | 16.31 ± 13.72 (2.77–47.22) | |||
TBUT: tear beak up time, OSDI: ocular surface disease index.
Mean pre-treatment Schirmer in the control group was 3.50 ± 3.13 mm (range: 0–13), which changed insignificantly after treatment to 3.85 ± 2.88 mm (range: 1–7) (P = 0.551, CI 95%: −0.81 to 0.44). Mean Schirmer in the treatment group changed insignificantly from 2.96 ± 3.39 mm (range: 1–15) at baseline to 4.96 ± 2.84 (range: 1–15) at final visit (P = 0.113, CI 95%: −2.25 to 0.25). There was no difference between the control and treatment groups regarding Schirmer's test at final visit (P = 0.155).
Mean tear film osmolarity did not change significantly in the control group (P = 0.157). However, the respective value improved significantly from 315.40 ± 17.06 osmol/L (range: 279–340) to 296.90 ± 14.39 osmol/L (range: 260–310) in the treatment group (P < 0.001).
Mean pre-treatment OSDI improved significantly at final visit in both the control and treatment groups (P = 0.003 and P < 0.001, respectively).
It is noteworthy to mention that the mean OSDI improvement was significantly higher in the treatment group in comparison to the control group (P = 0.026).
Discussion
This randomized clinical trial demonstrates the positive effect of omega-3 fatty acids in the treatment of dry eye syndrome in terms of qualitative objective and subjective dry eye indices after cataract surgery.
Dry eye is an important complication of ocular surgeries including cataract and refractive surgery. As patients who undergo cataract surgery are older than refractive surgery candidates and have more comorbidities, they may experience even more severe post-surgical dry eye.7, 8
This complication leads to patient complaints even after a non-complicated cataract surgery.9, 10, 11, 12 Dry eye after eye surgeries can negatively influence the quality of life by causing eye discomfort, burning, itching, red eye, photophobia, or even temporary blurring of vision.13, 14 Post-surgical dry eye can be triggered by different mechanisms, one of the most important of which is post-surgical inflammation.24, 25, 26, 27, 28
Long chain fatty acids modulate the AA pathway and reduce inflammatory response. Omega-3 is considered an essential fatty acid that should be supplemented in diet and cannot be produced in the body.18
Dry eye syndrome is a multifactorial disease, affecting tears and the ocular surface, accompanied by increased osmolarity of tear film, and inflammation of the ocular surface.30 DHA promotes synthesis of anti-inflammatory prostaglandins such as prostaglandin E3 and relieves dry eye symptoms.22
Several studies have investigated the role of oral supplement of omega-3 fatty acids in the treatment of dry eye syndrome as an anti-inflammatory agent. Adding omega-3 has shown to increase tear production.24, 25, 26, 27 Another suggested mechanism of omega-3 in the treatment of dry eye syndrome is changing the fatty acid composition of meibomian glands and therefore, the properties of their secretions.31, 32 By these two different mechanisms, omega-3 fatty acids have shown to be effective in the treatment of dry eye syndrome. In a large cross-sectional study, Miljanović et al. have observed a lower incidence of dry eye symptoms in women with a higher dietary intake of omega-3.33
In this study, OSDI and TBUT showed significant improvement in both the control and treatment groups, but this improvement was significantly higher in the treatment group in comparison to the control group for OSDI, TBUT, and tear osmolarity (which all cause improvement in tear film “quality”) (Fig. 1, Fig. 2, Fig. 3).
Fig. 1.
Comparison of pre-treatment (tear beak up time [TBUT] and Schirmer 1) and post-treatment (TBUT and Schirmer 2) in omega-3 (treatment) and conventional (control) groups.
Fig. 2.
Comparison of pre-treatment (ocular surface disease index [OSDI] 1) and post-treatment (OSDI 2) in omega-3 (treatment) and conventional (control) groups.
Fig. 3.
Comparison of pre-treatment (osmolarity 1) and post-treatment (osmolarity 2) in omega-3 (treatment) and conventional (control) groups.
These results illustrated that supplementing the diet with high amounts of omega-3 polyunsaturated fatty acids decreases dry eye symptoms after cataract surgery and increases tear film stability.
In our study, tear film osmolarity and consequently Schirmer's test results did not change significantly in the control group, but osmolarity showed significant improvement in the treatment group (P < 0.001). Despite clinically considerable improvement in mean Schirmer's test of the treatment group (from 3.96 ± 3.39 to 4.96 ± 2.84), these results were not significant statistically.
Kangari et al.25 showed that adding omega-3 supplements to standard treatment of non-surgically-induced dry eye syndrome would significantly improve OSDI, TBUT, and Schirmer's test results. We observed similar results in post-cataract surgery dry eye syndrome for OSDI and TBUT, but in our study, there was not any statistically significant higher improvement in the treatment group in Schirmer's test, which is a quantitative tear film index (P = 0.155). It seems that omega-3 supplementation has positive effects on tear film quality rather than its quantity in surgically-induced dry eye syndrome. It could be explained by the more important role of inflammation in surgically-induced dry eye. Although inflammation could lead to the decreased production of tears, studies demonstrated conflicting results of anti-inflammatory medication in improvement of Schirmer's test24, 25, 26, 30.
A possible explanation for this discrepancy could be in the homogenous studied population, with those with longer lasting inflammation and irreversible damage of lacrimal gland, showing the least improvement.
Although there are some studies investigating the effect of omega-3 on post-surgical dry eye,28, 34 to our knowledge, this is the first study exploring the impact of omega-3 oral supplementation on cataract surgery induced dry eye.
Ong et al.'s study on the effect of omega-3 fatty acids in the treatment of dry eye syndrome after photorefractive keratectomy concluded that adding omega-3 to standard treatment can lead to a significant higher improvement in epithelial healing, TBUT, and visual acuity. In their study, all patients in the treatment group reached visual acuity of 20/20, but only 4 patients in the control group reached this level of visual acuity.28 Our study also demonstrated significant improvement in tear osmolarity and alleviation of symptoms measured by OSDI, in addition to improve TBUT, with oral supplement of omega-3 combined with conventional therapy.
As for limitations to our study, lack of placebo could affect the observed response driven from oral medication which was missing in the control group. A long post-operative period in some cases might also have restricted our study due to possible confounding factors. We also excluded patients suffering from dry eye who underwent other type of cataract surgeries such as extracapsular cataract extraction (ECCE) or intracapsular cataract extraction (ICCE). Further randomized placebo-controlled clinical trials and subsequent systematic reviews can help in better illustration of the effects of supplementary omega-3 in the treatment of post-cataract surgery dry eye.
In conclusion, this randomized clinical trial shows the effectiveness of omega-3 supplements in the management of dry eye syndrome after cataract surgery in terms of both subjective and objective measurements. Therefore, it could be safely added to the postoperative protocols following cataract surgery to reduce the incidence of post-operative dry eye syndrome.
Footnotes
Peer review under responsibility of the Iranian Society of Ophthalmology.
The present study was performed at Farabi Eye Hospital, Tehran University of Medical Sciences, Tehran, Iran.
Conflicts of interest: None declared.
Financial disclosure: None of the authors has a financial or proprietary interest in any mentioned product, method, or material.
References
- 1.The definition and classification of dry eye disease: report of the Definition and Classification Subcommittee of the International Dry Eye WorkShop (2007) Ocul Surf. 2007;5:75–92. doi: 10.1016/s1542-0124(12)70081-2. [DOI] [PubMed] [Google Scholar]
- 2.Schein O.D., Munoz B., Tielsch J.M., Bandeen-Roche K., West S. Prevalence of dry eye among the elderly. Am J Ophthalmol. 1997;124:723–728. doi: 10.1016/s0002-9394(14)71688-5. [DOI] [PubMed] [Google Scholar]
- 3.Lemp M.A. Report of the National Eye Institute/industry workshop on clinical trials in dry eyes. CLAO J. 1995;21:221–232. [PubMed] [Google Scholar]
- 4.The epidemiology of dry eye disease: report of the Epidemiology Subcommittee of the International Dry Eye WorkShop (2007) Ocul Surf. 2007;5:93–107. doi: 10.1016/s1542-0124(12)70082-4. [DOI] [PubMed] [Google Scholar]
- 5.Brewitt H., Sistani F. Dry eye disease: the scale of the problem. Surv Ophthalmol. 2001;45:S199–S202. doi: 10.1016/s0039-6257(00)00202-2. [DOI] [PubMed] [Google Scholar]
- 6.Schaumberg D.A., Sullivan D.A., Dana M.R. Epidemiology of dry eye syndrome. Adv Exp Med Biol. 2002;506(Pt B):989–998. doi: 10.1007/978-1-4615-0717-8_140. [DOI] [PubMed] [Google Scholar]
- 7.Thylefors B., Negrel A.D., Pararajasegaram R., Dadzie K.Y. Global data on blindness. Bull World Health Organ. 1995;73:115–121. [PMC free article] [PubMed] [Google Scholar]
- 8.Liu X., Gu Y.S., Xu Y.S. Changes of tear film and tear secretion after phacoemulsification in diabetic patients. J Zhejiang Univ Sci B. 2008;9(4):324–328. doi: 10.1631/jzus.B0710359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li X.M., Hu L., Hu J., Wang W. Investigation of dry eye disease and analysis of the pathogenic factors in patients after cataract surgery. Cornea. 2007;26(9 Suppl 1):S16–S20. doi: 10.1097/ICO.0b013e31812f67ca. [DOI] [PubMed] [Google Scholar]
- 10.Begley C.G., Caffery B., Nichols K., Mitchell G.L., Chalmers R., group Ds. Results of a dry eye questionnaire from optometric practices in North America. Adv Exp Med Biol. 2002;506(Pt B):1009–1016. doi: 10.1007/978-1-4615-0717-8_142. [DOI] [PubMed] [Google Scholar]
- 11.Albietz J.M., Lenton L.M. Management of the ocular surface and tear film before, during, and after laser in situ keratomileusis. J Refract Surg. 2004;20:62–71. doi: 10.3928/1081-597X-20040101-11. [DOI] [PubMed] [Google Scholar]
- 12.Khanal S., Tomlinson A., Esakowitz L. Changes in corneal sensitivity and tear physiology after phacoemulsification. Ophthalmic Physiol Opt. 2008;28:127–134. doi: 10.1111/j.1475-1313.2008.00539.x. [DOI] [PubMed] [Google Scholar]
- 13.Jacobi C., Jacobi A., Kruse F.E., Cursiefen C. Tear film osmolarity measurements in dry eye disease using electrical impedance technology. Cornea. 2011;30:1289–1292. doi: 10.1097/ICO.0b013e31821de383. [DOI] [PubMed] [Google Scholar]
- 14.Mathers W.D., Stovall D., Lane J.A., Zimmerman M.B., Johnson S. Menopause and tear function: the influence of prolactin and sex hormones on human tear production. Cornea. 1998;17:353–358. doi: 10.1097/00003226-199807000-00002. [DOI] [PubMed] [Google Scholar]
- 15.Hiroko B. Cataract surgery in the presence of other ocular comorbidities. In: Steinert R.F., editor. Cataract surgery. Saunders; 2010. pp. 411–415. Chap. 34. [Google Scholar]
- 16.Walker T. Benzalkonium toxicity. Clin Experiment Ophthalmol. 2004;32:657. doi: 10.1111/j.1442-9071.2004.00922.x. [DOI] [PubMed] [Google Scholar]
- 17.Kohlhaas M. Corneal sensation after cataract and refractive surgery. J Cataract Refract Surg. 1998;24:1399–1409. doi: 10.1016/s0886-3350(98)80237-x. [DOI] [PubMed] [Google Scholar]
- 18.Swanson D., Block R., Mousa S.A. Omega-3 fatty acids EPA and DHA: health benefits throughout life. Adv Nutr. 2012;3:1–7. doi: 10.3945/an.111.000893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McMurray D.N., Bonilla D.L., Chapkin R.S. n-3 Fatty acids uniquely affect anti-microbial resistance and immune cell plasma membrane organization. Chem Phys Lipids. 2011;164:626–635. doi: 10.1016/j.chemphyslip.2011.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pinazo-Duran M.D., Galbis-Estrada C., Pons-Vazquez S., Cantu-Dibildox J., Marco-Ramirez C., Benitez-del-Castillo J. Effects of a nutraceutical formulation based on the combination of antioxidants and omega-3 essential fatty acids in the expression of inflammation and immune response mediators in tears from patients with dry eye disorders. Clin Interv Aging. 2013;8:139–148. doi: 10.2147/CIA.S40640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.SanGiovanni J.P., Chew E.Y., Clemons T.E. The relationship of dietary lipid intake and age-related macular degeneration in a case–control study: AREDS Report No. 20. Arch Ophthalmol. 2007;125:671–679. doi: 10.1001/archopht.125.5.671. [DOI] [PubMed] [Google Scholar]
- 22.Dawczynski J., Jentsch S., Schweitzer D., Hammer M., Lang G.E., Strobel J. Long term effects of lutein, zeaxanthin and omega-3-LCPUFAs supplementation on optical density of macular pigment in AMD patients: the LUTEGA study. Graefes Arch Clin Exp Ophthalmol. 2013;251:2711–2723. doi: 10.1007/s00417-013-2376-6. [DOI] [PubMed] [Google Scholar]
- 23.James M.J., Gibson R.A., Cleland L.G. Dietary polyunsaturated fatty acids and inflammatory mediator production. Am J Clin Nutr. 2000;71:343s–348s. doi: 10.1093/ajcn/71.1.343s. [DOI] [PubMed] [Google Scholar]
- 24.Wojtowicz J.C., Butovich I., Uchiyama E., Aronowicz J., Agee S., McCulley J.P. Pilot, prospective, randomized, double-masked, placebo-controlled clinical trial of an omega-3 supplement for dry eye. Cornea. 2011;30:308–314. doi: 10.1097/ICO.0b013e3181f22e03. [DOI] [PubMed] [Google Scholar]
- 25.Kangari H., Eftekhari M.H., Sardari S. Short-term consumption of oral omega-3 and dry eye syndrome. Ophthalmology. 2013;120:2191–2196. doi: 10.1016/j.ophtha.2013.04.006. [DOI] [PubMed] [Google Scholar]
- 26.Sheppard J.D., Jr., Singh R., McClellan A.J. Long-term supplementation with n-6 and n-3 PUFAs improves moderate-to-severe keratoconjunctivitis sicca: a randomized double-blind clinical trial. Cornea. 2013;32:1297–1304. doi: 10.1097/ICO.0b013e318299549c. [DOI] [PubMed] [Google Scholar]
- 27.Brignole-Baudouin F., Baudouin C., Aragona P. A multicentre, double-masked, randomized, controlled trial assessing the effect of oral supplementation of omega-3 and omega-6 fatty acids on a conjunctival inflammatory marker in dry eye patients. Acta Ophthalmol. 2011;89:e591–e597. doi: 10.1111/j.1755-3768.2011.02196.x. [DOI] [PubMed] [Google Scholar]
- 28.Ong N.H., Purcell T.L., Roch-Levecq A.-C. Epithelial healing and visual outcomes of patients using omega-3 oral nutritional supplements before and after photorefractive keratectomy: a pilot study. Cornea. 2013;32:761–765. doi: 10.1097/ICO.0b013e31826905b3. [DOI] [PubMed] [Google Scholar]
- 29.Sakpal T.V. Sample size estimation in clinical trial. Perspect Clin Res. 2010;1:67–69. [PMC free article] [PubMed] [Google Scholar]
- 30.Bhargava R., Kumar P., Kumar M., Mehra N., Mishra A. A randomized controlled trial of omega-3 fatty acids in dry eye syndrome. Int J Ophthalmol. 2013;6:811–816. doi: 10.3980/j.issn.2222-3959.2013.06.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tanaka H., Harauma A., Takimoto M., Moriguchi T. Association between very long chain fatty acids in the meibomian gland and dry eye resulting from n-3 fatty acid deficiency. Prostaglandins Leukot Essent Fatty Acids. 2015;97:1–6. doi: 10.1016/j.plefa.2015.02.004. [DOI] [PubMed] [Google Scholar]
- 32.Olenik A., Mahillo-Fernandez I., Alejandre-Alba N. Benefits of omega-3 fatty acid dietary supplementation on health-related quality of life in patients with meibomian gland dysfunction. Clin Ophthalmol. 2014;8:831–836. doi: 10.2147/OPTH.S62470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Miljanovic B., Trivedi K.A., Dana M.R., Gilbard J.P., Buring J.E., Schaumberg D.A. Relation between dietary n-3 and n-6 fatty acids and clinically diagnosed dry eye syndrome in women. Am J Clin Nutr. 2005;82:887–893. doi: 10.1093/ajcn/82.4.887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.He J., Bazan H.E.P. Omega-3 fatty acids in dry eye and corneal nerve regeneration after refractive surgery. Prostaglandins Leukot Essent Fatty Acids. 2010;82:319–325. doi: 10.1016/j.plefa.2010.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]