Abstract
Fucoidan, a sulfated polysaccharide extracted from brown algae, exhibits anti-cancer activity. However, the effects and mechanism of fucoidan-induced apoptosis via endoplasmic reticulum (ER) stress is unclear. In this study, we demonstrated that fucoidan prevents tumorigenesis and reduces tumor size in LLC1-xenograft male C57BL/6 mice. Fucoidan induces an ER stress response by activating the PERK-ATF4-CHOP pathway, resulting in apoptotic cell death in vitro and in vivo. Furthermore, ATF4 knockdown abolishes fucoidan-induced CHOP expression and rescues cell viability. Specifically, fucoidan increases intracellular reactive oxygen species (ROS), which increase ATF4 and CHOP in lung cancer cells. Using the ROS scavenger N-acetyl-l-cysteine (NAC), we found that ROS generation is involved in fucoidan-induced ER stress-mediated apoptosis. Moreover, via Toll-like receptor 4 (TLR4) knockdown, we demonstrated that fucoidan-induced ROS and CHOP expression were attenuated. Our study is the first to identify a novel mechanism for the antitumor activity of fucoidan. We showed that fucoidan inhibits tumor viability by activating the TLR4/ROS/ER stress axis and the downstream PERK-ATF4-CHOP pathway, leading to apoptosis and suppression of lung cancer cell progression. Together, these results indicate that fucoidan is a potential preventive and therapeutic agent for lung cancer that acts via activation of ROS-dependent ER stress pathways.
Fucoidan consists of fucose-based sulfated polysaccharides and is extracted from brown algae; it is a heparin-like molecule with a substantial percentage of L-fucose and sulfated ester groups as well as small proportions of D-xylose, D-galactose, D-mannose, and glucuronic acid1,2,3. Fucoidan has low toxicity4 and various beneficial biological properties, such as anti-tumor, anti-bacterial and anti-inflammatory activities5. We recently reported that fucoidan leads to Smurf2-dependent ubiquitin proteasome pathway-mediated TGFbeta receptor (TGFR) degradation and inhibition of breast6 and lung cancer7 cell growth and mobility in vitro and in vivo. The molecular mechanisms of fucoidan-mediated antitumor signaling pathways have also been examined and proposed. In general, fucoidan appears to affect cancer cells through various biological processes or responses. One biological response may be accomplished by several independent signalling pathways. For example, a variety of signal transduction pathways can independently cause cellular apoptosis. The cellular and molecular biology aspects of fucoidan’s antitumor function include fucoidan-induced apoptosis, cell cycle arrest, anti-angiogenesis, inhibition of metastasis, migration and invasion, and immunological reactions3,8. In our current research, we examine fucoidan-induced apoptosis in lung cancer.
Lung cancer is one of the most common cancers in the world and has a high mortality rate. There are two types of lung cancer: non-small cell lung cancer (NSCLC, approximately 80% of lung cancers) and small cell lung cancer (SCLC, approximately 20% of lung cancers). Additionally, there are three types of NSCLC, including adenocarcinoma (~40% of NSCLCs), squamous cell carcinoma (~25–30% of NSCLCs), and large cell lung cancer (~10–15% of NSCLCs)9. Multiple anti-cancer drugs have been developed and used to inhibit tumor angiogenesis or induce cancer cell death via various signaling pathways10; however, these clinical drugs can result in tumor cell resistance and have numerous detrimental side effects11.
The endoplasmic reticulum (ER) is an important intracellular organelle with many functions, such as protein folding, initially post-translational modification, lipid biogenesis, and maintenance of Ca2+ homeostasis in cells12. Physiological or pathological conditions, such as hypoxia, nutrient deprivation and ER calcium depletion, interfere with the normal functions of the ER, resulting in accumulation of abnormal proteins. Induction of ER stress from accumulation of unfolded protein aggregates activate a series of intracellular signaling pathways known as the unfolded protein response (UPR)13. The UPR is activated by the coordinated action of three separate ER stress sensors that are located on the ER membrane including protein kinase RNA-like ER kinase (PERK); inositol-requiring protein-1α (IRE1α) and activating transcription factor 6 (ATF6)14. In general, PERK, a type III ER resident protein kinase, phosphorylates serine 51 of eukaryotic initiation factor 2α (eIF2α), and followed by the selective translation of ATF4, when cells are under ER stress14. ATF4 induces UPR target genes that promote ER folding and adaptation to stress via induction of C/EBP homologous protein (CHOP/GADD153)15. CHOP is a major pro-apoptotic transcription factor that increases the rate of Bim transcription16. It is reported that aberrant stimulation of ER or ER stress may imbalance the redox reactions and activate reactive oxygen species (ROS) release; moreover, ER stress–induced apoptosis is implicated in various pathological conditions including cancer17.
Reactive oxygen species (ROS) are defined as oxygen-containing, reactive chemical species. There are two types of ROS: free radicals and non-free radicals18. Free radical ROS, such as superoxide (O2−) and the hydroxyl radical (OH•), contain an unpaired electron. Non-free radical ROS do not have unpaired electrons but can be converted to free radical ROS19. ROS are produced by or derived from the mitochondria respiratory chain. In some cancer cells, ROS are produced through a reaction catalyzed by NADPH oxidase complexes18. Previous reports demonstrated that ROS may deplete calcium stores in the ER via inhibition of Ca2+-ATPase, leading to (or triggering) ER stress and apoptosis20. Additionally, ROS may also exacerbate protein misfolding in the ER lumen by oxidizing amino acids in folding proteins and inducing the UPR21, which then promotes ER stress.
Fucoidan-induced apoptosis of human MDA-MB-231 breast cancer cells and HCT116 colon cancer cells by modulating the ER stress cascades has been reported22. In addition, evidence of the involvement of ROS in a variety of fucoidan and induced apoptosis has been accumulated; for example, fucoidan of the Mozuku seaweed (Cladosiphon novae-caledoniae Kylin) activates a caspase-independent apoptotic pathway in human MCF-7 breast cancer cells through ROS-dependent JNK activation and the mitochondria-mediated Bcl-2 family pathways23; fucoidan (Undaria pinnatifida sporophylls) induces apoptosis in human SMMC-7721 hepatocellular carcinoma via the ROS-mediated mitochondrial pathway and activation of caspases process24; and fucoidan (Fucus vesiculosus) inhibits proliferation of human myelodysplastic syndrome/acute myeloid leukemia cell line SKM-1 via the activation of apoptotic pathways and production of ROS25. However, the mechanism by which fucoidan-induced extracellular signaling induces ER stress and ROS remains unclear. Therefore, we investigated the effect of fucoidan-mediated ROS (redox modulation) on induction of ER stress and the consequent apoptotic reactions in lung cancer.
In our current study, we demonstrate that fucoidan (i) promotes apoptosis of lung cancer cells, (ii) reduces lung tumorigenesis, (iii) induces ATF4 and CHOP protein expression in an LLC1-xenograft mice model via continuous oral feeding of fucoidan, and (iv) induces ROS-mediated ER stress via TLR4. Our study elucidates the mechanism underlying fucoidan-induced ROS-mediated induction of ATF4 and CHOP protein expression via the TLR4/ROS/PERK/eIF2α axes. Moreover, our findings suggest that fucoidan is a potential therapeutic agent for preventing lung tumorigenesis.
Results
Fucoidan prevents tumorigenesis in LLC1 cell-xenograft male C57BL/6 mice in vivo
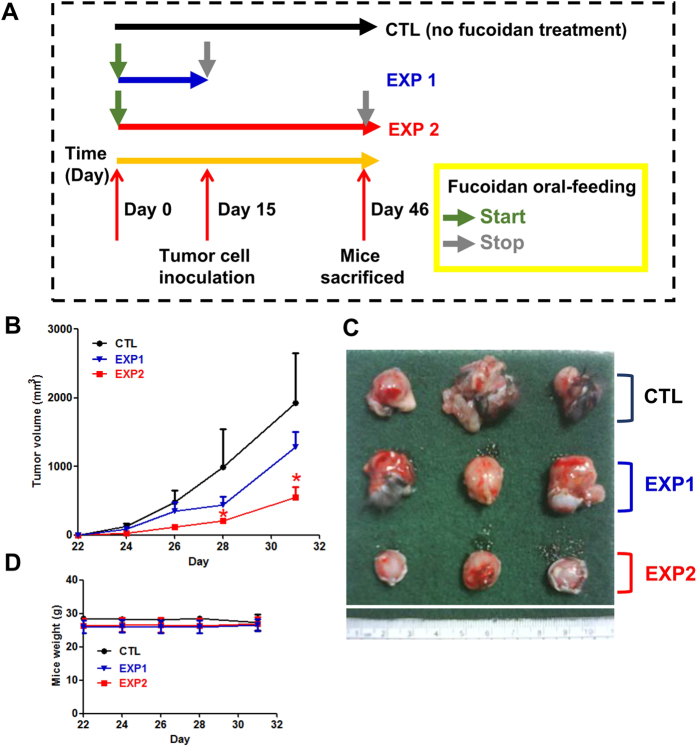
We previously demonstrated that continuous feeding with fucoidan effectively inhibits tumor growth in LLC1-bearing mice7. To further explore the cancer inhibitory activity of fucoidan, we examined the tumor volumes of mice that were exposed to oral feeding prior to hypodermic inoculation of cancer cells into the dorsum. Briefly, we divided the mice into three groups: group 1 was the ddH2O control (CTL); group 2 was fed only fucoidan prior to LLC1 inoculation, and oral feeding of fucoidan was stopped on the 15th day (EXP 1); and group 3 was fed fucoidan for the entire experimental period (EXP 2; Fig. 1A). At the indicated time, the mice in EXP 1 exhibited smaller tumor volumes than those of the mice in CTL (Fig. 1B and C). Additionally, tumor volumes of mice in EXP 2 were significantly reduced compared with those of the mice in EXP 1 (Fig. 1B and C). Thus, fucoidan treatment in EXP 1 (i.e., discontinuous oral feeding with fucoidan) exhibited reduced efficacy in inhibiting tumor growth compared with that of the EXP 2 continuous fucoidan treatment. Moreover, a smaller difference was observed in the mouse body weights between the fucoidan-fed mice (EXP 1 and EXP 2) and the ddH2O controls (CTL; Fig. 1D). Together, these results indicate that continuous oral feeding with fucoidan elicits the greatest efficacy in preventing and suppressing tumorigenesis.
Figure 1. Fucoidan prevents tumorigenesis in LLC1-bearing C57BL/6 mice in vivo.
Mice were pretreated with fucoidan (24 mg/kg) for 14 days before LLC1 cells (2 × 105) were hypodermically inoculated into the dorsum of male C57BL6 mice. On the 15th day, the mice were divided into three groups and processed in a “previous and continuous” fashion (A). In brief, the following groups were established: oral feeding with ddH2O (control), oral feeding with cessation of fucoidan feeding on the day of LLC1 cell inoculation, (EXP 1) and maintained fucoidan feeding for 26 days (EXP 2) at 7 oral feedings/week/mouse. (B) The tumor volumes and (C) tumor samples from the mice were collected at the end of the treatment. (D) The mouse weights were measured as indicated. Three of five individual experiments are presented (n = 5). Each bar represents the mean ± standard deviation (SD), and error bars indicate the SD. Statistically significant differences are shown (*P < 0.05) compared with the control group.
Fucoidan reduces lung tumor growth and induces endoplasmic reticulum (ER) stress-related proteins in LLC1-bearing mice in vivo and in vitro
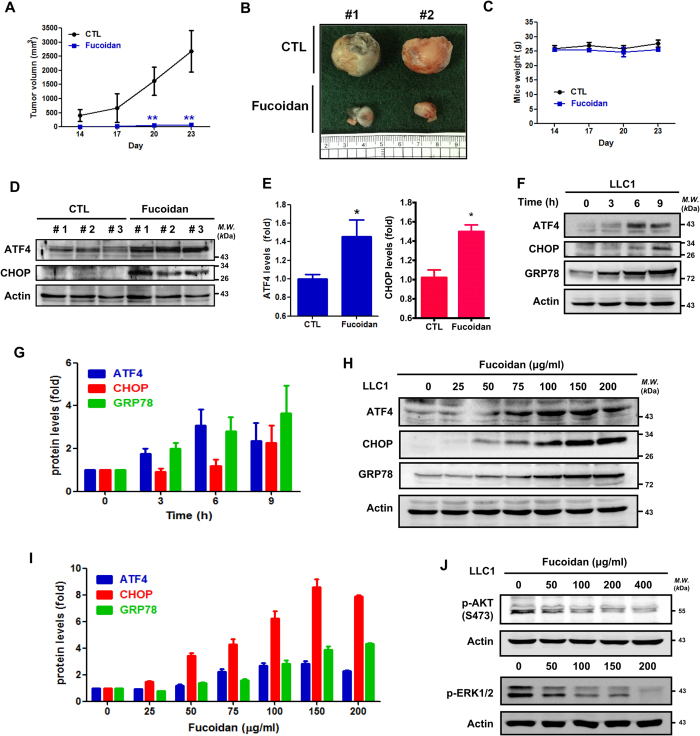
To investigate the effect of fucoidan feeding on LLC1-bearing mice in vivo, we fed the mice fucoidan (24 mg/kg/daily) for 14 days and subsequently hypodermically inoculated them with LLC1 cells in the dorsum on day 14. The treated mice were fed daily with fucoidan, and tumor growth rates were assessed over 23 days. The mice fed fucoidan exhibited significant reductions in tumor volumes (Fig. 2A,B). In contrast, a smaller difference was observed in body weights of the fucoidan-fed mice and the ddH2O control groups (Fig. 2C), which indicated this dose of fucoidan did not have a toxic effect in the C57BL/6 mice model. Next, the tumor lesions of the mice were collected to analyze ER stress-related protein expression. As shown in Fig. 2D and E, ATF4 and CHOP protein levels increased in the fucoidan-fed LLC1-bearing mice compared with those in the control group, indicating that fucoidan induced ER stress-related proteins in tumors in vivo (see the following section).
Figure 2. Fucoidan suppresses tumor growth and induces apoptosis-related proteins in vitro and in vivo.
(A) Continuous once daily feeding of C57BL/6 male mice with fucoidan (24 mg/kg) for 14 days prior to inoculation with LLC1 cells. After prior oral administration of fucoidan, LLC1 cells were subcutaneously inoculated into the abdomens of mice, and continuous once daily fucoidan feeding was performed (24 mg/kg) for 23 days. The tumor volumes were measured every 3 days for 23 days. (B) Tumor samples from the mice were collected at the end of the treatment. (C) The body weights of the mice were measured every 3 days for 23 days. (D) After fucoidan treatment, the tumors were collected. The tumor samples were homogenized, and Western blotting analyses of tumor samples were performed to detect ATF4 and CHOP expression. (E) Quantification of fucoidan-mediated up-regulation of the apoptotic protein levels in (D). (F) LLC1 cells were treated with fucoidan (100 μg/ml) for 3–9 h followed by Western blotting analyses of whole-cell lysates to detect the expressions of the following ER stress-related proteins: ATF4, CHOP, and GRP78. (G) Quantification of fucoidan-mediated up-regulation of ER stress-related protein levels in (F). (H) LLC1 cells were treated with various dosages of fucoidan (μg/ml) for 24 h followed by Western blotting analyses of whole-cell lysates to detect ATF4, CHOP and GRP78 expression. (I) Quantification of fucoidan-mediated up-regulation of the ER stress-related proteins levels in (H). (J) LLC1 cells were treated with fucoidan (0 to 400 μg/ml) for 24 h followed by Western blotting analyses of whole cell lysates to detect p-Akt (Ser 473) and p-ERK1/2 expression. Actin was used as an internal control.
Further supporting the effect of fucoidan on LLC1 cells in vitro, we previously showed that fucoidan (effective concentration about 224 μg/ml) inhibits the proliferation of LLC1 cells in dose- and time-dependent manners using an MTT assay7. Specifically, we found that fucoidan induces ER stress-related protein expression, including GRP78, ATF4 and CHOP, in both time- and dose-dependent manners (Fig. 2F–I). Additionally, we demonstrated that fucoidan inhibits AKT and ERK phosphorylations (Fig. 2J), which are related to the viability and proliferation of cancer cells26. Together, these results indicate that induction of ER stress and inhibition of AKT/ERK signaling are involved in fucoidan-mediated prevention and suppression of tumorigenesis in vitro and in vivo.
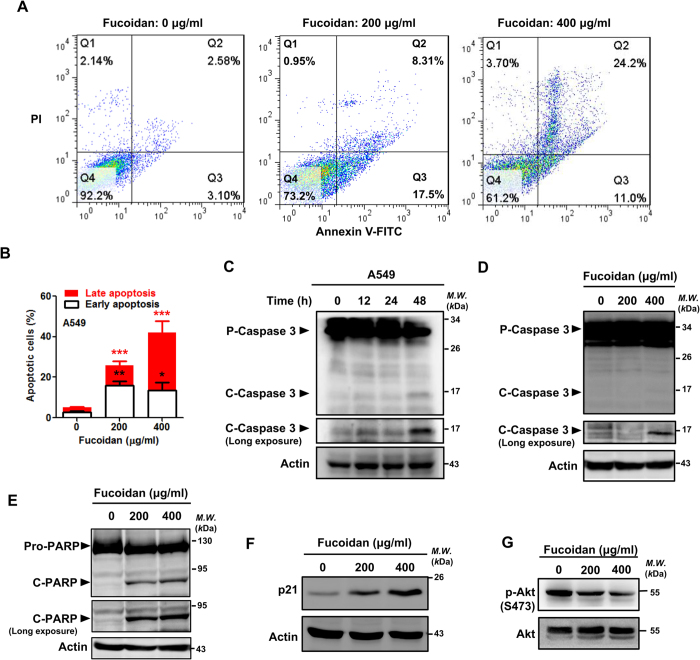
Fucoidan induces apoptosis-related reactions and p21 expression and inhibits AKT phosphorylation in human lung cancer in vitro
Using an MTT assay, we previously showed that fucoidan significantly inhibits the proliferation and viability of human lung cancer cells in dose- and time-dependent manners7. We found and applied that concentrations of fucoidan to A549 cells and CL1-5 cells are about 400–800 μg/ml and 100–200 μg/ml, respectively in our experiments. Next, using FACS analysis with propidium iodide (PI)/annexin V-FITC double staining, we investigated whether fucoidan induced apoptosis in A549 and CL1-5 lung cancer cells. As shown in Fig. 3A,B and Supplementary Fig. 1A,B, following 48 h of fucoidan treatment, apoptotic cells increased from 5% to 40–60% and from 3% to 18–50% in the A549 and CL1-5 cell lines, respectively. Furthermore, using Western blot analysis of the caspase activity, we demonstrated that fucoidan induced apoptosis in A549 and CL1-5 cells as indicated by the dose- and time-dependent expressions of the pro-apoptotic proteins caspase 3 and poly ADP ribose polymerase (PARP; Fig. 3C–E and Supplementary Fig. 1C). Moreover, using the Western blot assay and FACS analysis, we also found that fucoidan activated caspase 3 and PARP, leading to induction of apoptosis in LLC-1 cells (Supplementary Fig. 2).
Figure 3. Fucoidan inhibits proliferation and induces apoptosis in A549 cells.
(A) A549 cells were treated with fucoidan (200 and 400 μg/ml) for 48 h. The cells were stained with annexin V-FITC and PI and subsequently analyzed using flow cytometry. (B) Quantification of fucoidan-induced apoptotic cells by annexin/PI double-staining. Apoptosis was evaluated by determining the percentage of annexin V-positive cells. The data are representative of three independent experiments and are presented as the mean ± the SD, and error bars indicate the SD. Significant differences are shown (***P < 0.001, compared with the control group). (C) A549 cells were treated with fucoidan (200 μg/ml) for 12, 24 and 48 h. Then, Western blotting analysis of whole-cell lysates was performed to detect the expressions of pro (p)-caspase 3 and cleaved (c)-caspase 3. (D) A549 cells were treated with fucoidan (0–400 μg/ml) for 24 h, and Western blotting of whole-cell lysates was subsequently performed to detect Caspase 3 expression. (E) A549 cells were treated with fucoidan (0–400 μg/ml) for 48 h, and Western blotting of whole-cell lysates was subsequently performed to detect PARP expression. Actin was used as an internal control. (F) A549 cells were treated with fucoidan (200 and 400 μg/ml) for 24 h, and Western blotting analyses of whole-cell lysates were subsequently performed to detect p21 expression. (G) A549 cells were treated with fucoidan (0 to 400 μg/ml) for 24 h, and Western blotting analyses of whole-cell lysates were subsequently performed to detect p-Akt (Ser 473) expression. Total AKT was used as an internal control.
Additionally, we also analyzed the effect of fucoidan on cell cycle distribution in lung cancer cells. Compared to the control cells, fucoidan treatment (200 μg/ml, 48 h) increased the proportions of A549 cells in sub-G1 and G1 phases from 1% to 4% and from 63% to 85%, respectively (Supplementary Fig. 3), and these results are comparable to those of another report27 that assessed the biological activity of low-dose fucoidan. Moreover, we confirmed that fucoidan up-regulated the expressions of cell cycle-related proteins, including p21, in both A549 and CL1-5 cells (Fig. 3F and Supplementary Fig. 1D). In contrast, fucoidan inhibited AKT phosphorylation in the treated cells (Fig. 3G and Supplementary Fig. 1E).
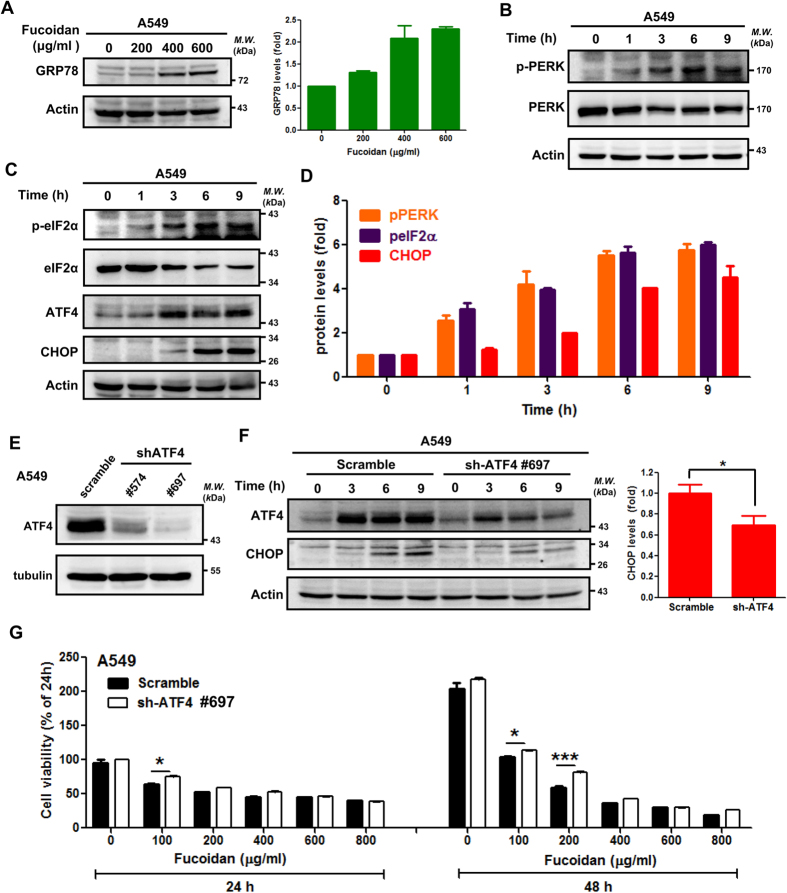
Fucoidan induces ER stress-related signaling molecules in lung cancer cells
Following treatment with fucoidan, GRP78 expression was increased in A549 and CL1-5 cells (Fig. 4A and Supplementary Fig. 4A), which suggests that GRP78 is a gatekeeper in fucoidan-mediated activation of ER stress as previously reported28. Fucoidan also induced phosphorylation of the ER membrane protein PERK in a time-dependent manner (Fig. 4B and Supplementary Fig. 4B). We systematically analyzed molecules downstream of PERK. As shown in Fig. 4C and D, fucoidan induced eIF2α phosphorylation, and ATF4 and CHOP (i.e., molecules downstream of eIF2α) expressions were increased in a time-dependent manner in these cells. CHOP expression increased in CL1-5 cells treated with fucoidan for 24 h (Supplementary Fig. 4C). These results indicate the following: (i) fucoidan induced ER stress via activation of the PERK/eIF2α/ATF4/CHOP axes, which is consistent with other reports on ER stress; and (ii) activations of these axes are related to apoptosis in some cancer cells and involved in inhibition of cell viability22.
Figure 4. Fucoidan induces ER stress, and ATF4-shRNA (sh-ATF4) interferes with fucoidan-induced CHOP expression in lung cancer cells.
(A) A549 cells were treated with fucoidan (0–600 μg/ml) for 48 h, and Western blotting analyses of whole cell lysates were subsequently performed to detect GRP78 expression. Right panel: Quantification of the intensities of GRP78 bands, which is representative of three separate determinations with ImageJ. (B,C) A549 cells were treated with fucoidan (400 μg/ml) for 1–9 h, and Western blotting analyses of whole-cell lysates were subsequently performed to detect the expressions of ER stress-related proteins. (D) Quantification of the band intensities of pPERK, peIF2α and CHOP (B-C) is representative of three separate determinations with ImageJ. (E) ATF4 expression in A549 cells was detected by Western blotting of whole-cell lysates following TG treatment for 24 h. (F) A549 cells (scramble and ATF4-knockdown) were incubated with fucoidan (200 μg/ml) for 0–9 h, and Western blotting of whole-cell lysates was subsequently performed to detect ATF4 and CHOP. Actin was used as an internal control. Right panel: The densitometric values of CHOP normalized to the relative actin value. Quantification of the intensities of CHOP bands was performed following fucoidan treatment for 9 h. The data are presented as the mean ± the SD, and error bars indicate the SD. Significant differences are noted (*P < 0.05 compared with the control group). (G) A549 cells (scramble and ATF4-knockdown cells) were treated with various doses of fucoidan (μg/ml) for 24 and 48 h. Cell viabilities were determined by crystal violet staining assays. Each group with fucoidan was normalized against each untreated control.
Effect of ATF4 shRNAs on CHOP induction in fucoidan-induced ER stress in lung cancer
To further confirm the role of ATF4 in ER stress-mediated cell death, we performed ATF4-knockdown experiments using ATF4 shRNAs #574 (sh-S1) and #697 (sh-S2) in A549 cells. Based on the Western blotting analysis, we found that ATF4 knockdown reduced ER stress-induced ATF4 expression (Fig. 4E). In addition, CHOP, a downstream target of ATF4, is a marker of ER stress that promotes apoptotic cell death15. By examining the ER stress-induced activation of the ATF4/CHOP axis, we found that ATF4 knockdown (by ATF4 shRNA#697) abolished fucoidan-induced ATF4-mediated CHOP expression (Fig. 4F), which suggests that ATF4 plays an important upstream role in ER stress-mediated CHOP in the presence of fucoidan. To further investigate the role of ATF4 in lung cancer cell viability following fucoidan treatment, we performed a crystal violet staining assay to examine cell viability and proliferation. As illustrated in Fig. 4G, fucoidan effectively inhibited cell viability and proliferation in dose- and time-dependent manners. In contrast, abolishing ATF4 expression via ATF4 shRNA (#697) partially rescued the viability of low-dosage fucoidan-treated A549 cells although we also observed a reduction in high-dose of fucoidan treatment. Together, these results indicate that ATF4 may play a fucoidan-mediated cell death molecule that is involved in ER stress in lung cancer.
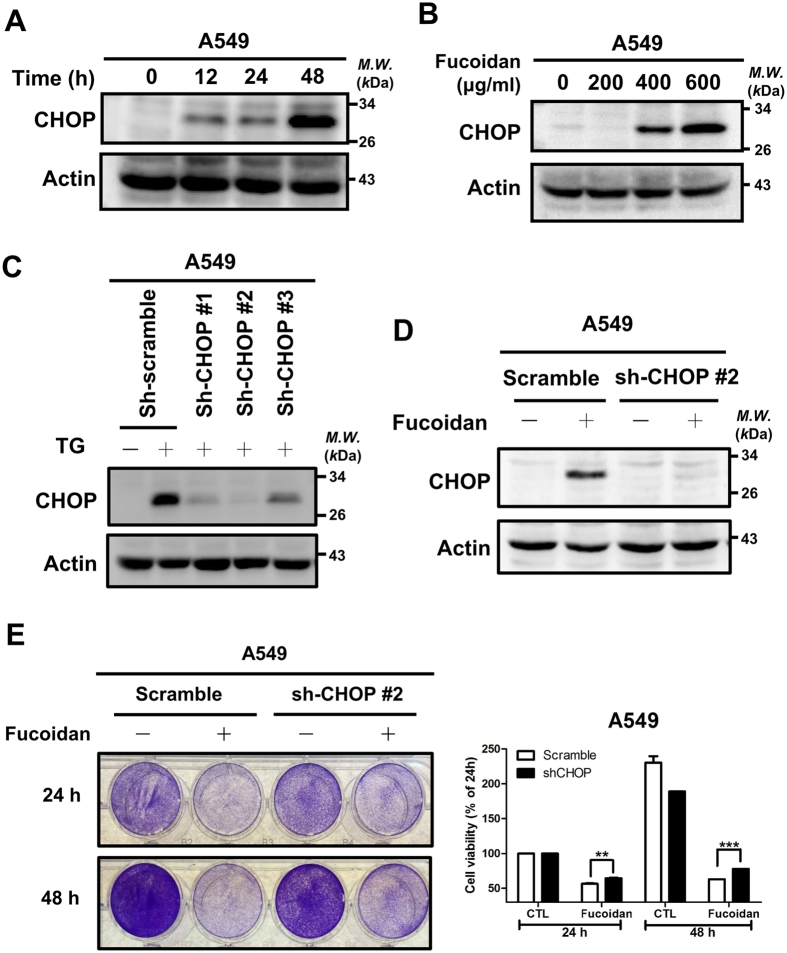
Effect of CHOP knockdown on fucoidan-mediated ER stress in A549 cells
CHOP expression is up-regulated upon ER stress, resulting in apoptosis16. To further explore and confirm the role of CHOP in fucoidan-induced apoptosis, we demonstrated that long-term treatment with fucoidan induces CHOP expression in time- and dose-dependent manners (Fig. 5A,B and Supplementary Fig. 5A,B). Using CHOP shRNAs, including #328 (sh-S1), #393(sh-S2) and #985 (sh-S3), we performed CHOP-knockdown experiments in A549 and CL1-5 cells. Based on Western blotting analyses, we used the ER stress inducer thapsigargin (TG) and found that CHOP knockdown led to a reduction in TG-induced ER stress-mediated CHOP expression (Fig. 5C and Supplementary Fig. 5C). Next, we demonstrated that CHOP knockdown (sh-S2) substantially inhibited fucoidan-mediated CHOP expression in A549 and CL1-5 cells (Fig. 5D and Supplementary Fig. 5D). Furthermore, CHOP knockdown rescued the fucoidan-inhibited cell viability in A549 cells (Fig. 5E). These results indicate that CHOP plays an essential role in fucoidan-induced ER stress-mediated apoptosis in lung cancer cells.
Figure 5. CHOP plays a role in fucoidan-inhibited cell viability.
(A) A549 cells were treated with fucoidan (400 μg/ml) for 0 to 48 h, and Western blotting analysis of whole-cell lysates was subsequently performed to detect CHOP expression. (B) A549 cells were treated with fucoidan (0 to 600 μg/ml) for 6 h, and Western blotting analysis of the CHOP expression in whole-cell lysates was subsequently performed. (C) HEK293T cells were transfected with three types of sh-CHOP plasmid (sh-#1, sh-#2 and sh-#3) to produce lentiviruses as described in the Materials and Methods section. After the media were harvested, viruses containing individual CHOP-shRNAs were used to infect A549 cells for 24 h followed by puromycin selection. CHOP expression was detected by Western blotting of whole cell lysates following TG (50 nM) treatment for 6 h. (D) A549 cells (scramble and CHOP-knockdown) were incubated with fucoidan (200 μg/ml) for 12 h, and Western blotting of whole-cell lysates was subsequently performed to detect CHOP expression. Actin was used as an internal control. (E) A549 cells (scramble and CHOP-knockdown cells) were treated with fucoidan (200 μg/ml) for 24 and 48 h. Cell viabilities were determined by crystal violet staining assays. Each group of fucoidan-treated samples was normalized against each untreated control. The data are representative of three separate experiments and are presented as the mean ± the SD. Error bars indicate the SD. Significant differences are noted (**P < 0.01 and ***P < 0.001, compared with the control group).
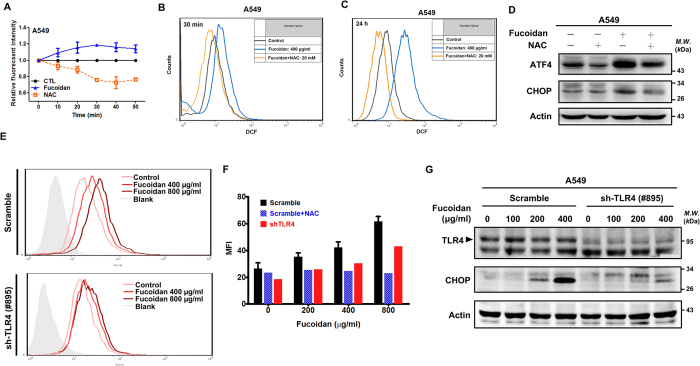
The putative roles of Toll-like receptor 4 (TLR4) in fucoidan-induced intracellular generation of ROS and ER stress-mediated CHOP expression in lung cancer
Induction of intracellular ROS generation can trigger cell apoptosis via the ER stress pathway29. We previously found that fucoidan induces ROS and ER stress in lung cancer cells. However, the effect of fucoidan-induced ROS on ER stress in lung cancer cells is not fully understood. Here, using H2DCFDA, we measured the generation of intracellular ROS in fucoidan-treated lung cancer cells. As illustrated in Fig. 6A, following treatment of the cells with fucoidan, we observed a time-dependent increase in DCF fluorescence, which indicated that fucoidan induced intracellular ROS generation in A549 cells. Additionally, using flow cytometric assays, we confirmed that ROS generation in A549 cells was detectable after short-term (30 min) and long-term (24 h) fucoidan treatment (Fig. 6B and C), which indicates that fucoidan effectively induced ROS generation over a broad range of times. Alternatively, using the ROS inhibitor N-acetyl-l-cysteine (NAC) to block intracellular ROS generation, we demonstrated that fucoidan-induced ROS generation is abolished by pretreatment of cells with NAC (Fig. 6B and C). To further determine whether ROS participates in fucoidan-induced ER stress and its relevant bio-functions, we examined ATF4 and CHOP expression during co-treatment with fucoidan and NAC. ATF4 and CHOP expressions in A549 cells decreased following co-treatment with fucoidan and NAC compared with those in cells that were treated with fucoidan alone (Fig. 6D). These results indicate that fucoidan-induced ROS generation is involved in ER stress and ROS-stimulated ER stress-related molecule (ATF4 and CHOP) expression.
Figure 6. Fucoidan induces intracellular ROS generation in A549 cells.
(A) A549 cells (5 × 104 cells per well in 96-well plates) were treated with fucoidan (400 μg/ml) or NAC (5 mM) for 0–60 min and then stained with fluorescent dye (H2DCFHDA, DCF) for 30 min. The fluorescence intensity of DCF was detected using Infinite 200 PRO multimode microplate readers (TECAN, Switzerland) at excitation and emission wavelengths of 485 and 535 nm, respectively. (B,C) A549 cells were pre-treated with NAC (20 mM) for 30 min, followed by additional incubation with fucoidan (400 μg/ml) for 30 min (B) and 24 h (C). The fluorescence intensity of DCF was detected by flow cytometry. (D) A549 cells were pre-treated with 5 mM of NAC for 1 h and were then treated with fucoidan (400 μg/ml) for 24 h, and Western blotting analyses of whole-cell lysates were subsequently performed to measure ATF4 and CHOP expressions. (E) A549 cells (scramble and sh-TLR4) were treated with fucoidan (400 to 1600 μg/ml) or NAC (20 mM) for 30 min. The fluorescence intensity of DCF was detected by flow cytometry. (F) Quantification of MFI in an experiment (E) is representative of three separate determinations by FlowJo. (G) A549 cells (scramble and TLR4-knockdown cells) were treated with fucoidan (0 to 400 μg/ml) for 24 h. Cell viabilities were determined with crystal violet staining assays. Western blot analysis was performed to determine the TLR4 and CHOP protein levels.
We previously demonstrated that lipopolysaccharide (LPS) binds to TLR and stimulates ROS, which results in expression of interleukin-130. Moreover, fucoidan was shown to interact with TLR4 and activate the transcription nuclear factor kappa B (NF-κB) in embryonic human kidney epithelial cells31. Based on our previous studies, we hypothesized that TLR4 is involved in fucoidan-induced ROS. TLR4 knockdown experiments were conducted. We found that knockdown of TLR4 expression (shTLR4) abolishes fucoidan-induced ROS compared with that of the “scrambled” TLR4 control group (Fig. 6E). Second, we found that knockdown of TLR4 expression abolishes fucoidan-induced ROS in a dose-dependent manner (Fig. 6E). Third, we analyzed the mean fluorescence intensity (MFI) of fluorescent dyes (H2DCFHDA and DCF) and observed a 40% reduction of ROS in TLR4 knockdown cells upon fucoidan treatment (Fig. 6F). NAC effectively inhibited fucoidan-induced intracellular ROS generation in the “scrambled” TLR4 control group at various concentrations of fucoidan treatment compared with that of the TLR4 knockdown group (Fig. 6F), suggesting that the TLR4-dependent pathway is involved in fucoidan-induced ROS generation. The putative role of TLR4 in fucoidan-induced ER stress-mediated CHOP expression was also examined. Fucoidan induced CHOP expression in the “scrambled” TLR4 A549 control group in a dose-dependent manner (Fig. 6G). In contrast, fucoidan-induced CHOP expression was significantly inhibited in the TLR4-knockdown (sh-TLR4#895) A549 group (Fig. 6G). Together, our results demonstrate that TLR4 plays a partial role in fucoidan-induced ROS, which then promote ER stress and stress-mediated apoptotic gene expression.
Discussion
Our previous findings show that orally administered fucoidan significantly reduces tumor volume/weight and TGFR protein levels in lung cancer LLC1-xenograft mice in vivo6,7; in our current study, we reported that pre-treatment of LLC1-xenograft mice with fucoidan could prevent and reduce tumor proliferation in mice (Fig. 1). In brief, we demonstrated that continuous oral feeding with fucoidan significantly reduces tumor volumes and induces ATF4 and CHOP protein expressions in LLC1-bearing mice in vivo. We found that fucoidan (i) effectively inhibits the proliferation of lung cancer cells via induction of G1 phase arrest and (ii) promotes cell death via apoptosis. One fucoidan-inducing apoptosis mechanism involves the induction of cell cycle arrest and enhancement of ROS levels via TLR4. We also found that fucoidan triggers ROS-mediated ER stress and activates UPR pathways to induce cell death (Supplementary Fig. 6). Taken together, our results demonstrate the pharmaceutical efficacy of fucoidan in a mouse lung cancer model. We also provide the first evidence of TLR4-mediated fucoidan induction of ROS that is dependent on the PERK/ATF4/CHOP axis and apoptosis as the underlying mechanisms.
The molecular mechanism of anticancer effects of fucoidan is summarized as the signaling pathways associated with the processes of apoptosis, cell cycle arrest, anti-angiogenesis, inhibiting metastasis (migration and invasion), etc. Our current finding proposed that fucoidan-induced apoptosis of lung cancer cell results from activation of the TLR4/ROS/ER stress axis and the mediation of downstream PERK-ATF4-CHOP signaling pathways. In addition, the fucoidan-mediated transducing signal pathways relevant to fucoidan-induced apoptosis have been reported as a pathway of the FAK-AKT axis32, activation of caspase-8 -9 and -3 pathways33, and suppression of the ASK1-p38 signaling pathway34. Our findings are that fucoidan induces apoptosis in lung cancer cells, as detected by expressions of the pro-apoptotic proteins caspase 3 and PARP, which is comparable to reports from other investigators35. On the other hand, fucoidan induces G1 arrest in cell cycle progression, leading to apoptosis in cancer cells3. In our study, we found that fucoidan treatment increases the proportions of lung cancer cells in G1 phases and the results are comparable to those of another reports36,37. Several transducing signal pathways involved in fucoidan-mediated cell cycle arrest have been proposed, such as fucoidan activation of the AKT signaling pathway36 and activation of p16INK4a-Rb and p14Arf-p53 pathways37.
Under ER stress, cells activate various signaling pathways to induce apoptosis and other reactions. ER stress–induced apoptosis is implicated in various pathological conditions, but the mechanisms linking ER stress–mediated signaling to downstream apoptotic pathways need to be studied17. CHOP is a marker of ER stress-mediated apoptosis; additionally, ATF4 has known pro-apoptotic functions that mediating the regulation of CHOP expression upon ER stress15. Here we found that fucoidan induces CHOP expression in lung cancer cells; and the PERK-eIF2α-ATF4-CHOP signaling pathway is one of major pathways in ER stress-mediated apoptosis17.
During tumor progression, elevated ROS promotes many tumor properties, including proliferation, transformation and metastasis18,38. Tumor cells also manipulate and increase multiple antioxidant proteins to reduce the toxicity of endogenous ROS. Thus, a delicate and complicated balance of “reduction” and “oxidation” (redox) modulation of intracellular ROS expression exists in cancer cells to maintain the malignant functions while eliminating ROS-induced toxicity. However, induction of excess ROS in cancer cells via therapeutic approaches, such as chemotherapy and radiotherapy, may trigger ROS-mediated cell death mechanisms39. ROS induce ER stress through modification of proteins and lipids29. Here, we examined effects of fucoidan on ROS-mediated ER stress and apoptosis, developing a potential therapeutic strategy for the treatment of lung cancer patients.
Under normal conditions, lung cancer cells keep a well-maintained redox balance. Following addition of fucoidan to testing cancer cells, there is a rapid increase in cellular ROS levels, disrupting the intracellular redox balance. The sudden fucoidan-induced redox dysfunction or ROS accumulation induces ER stress and activates apoptotic-related molecules. In addition, we found that fucoidan-induced ROS, as one of the upstream “initiating” signaling molecules, could be inhibited by the antioxidant NAC, followed by decreased ER stress and subsequent reduced activation of downstream apoptotic molecules and/or reactions in the cells. Importantly, we demonstrated that fucoidan induces ROS in a very short period (within 30 min). In contrast, fucoidan has been reported to promote mitochondrial-derived ROS generation after approximately 24–48 h25. Thus, the fucoidan-induced increase in ROS may occur at an early stage (receptor-mediated) or at a later stage (mitochondria-derived). Based on our current results from lung cancer cells, fucoidan can function as a redox modulation agent for treatment of lung cancer.
Recent findings indicate that the TLRs are expressed not only on immune cells, including macrophages30, but also on some cancer cells. In lung cancer cells, TLR4 facilitates tumor progression, metastasis and drug resistance40,41. Specifically, TLR4 activation triggers ROS generation42. It is unknown how fucoidan induces ROS generation in lung cancer cells. Thus, we hypothesized that TLR4 activation may be associated with fucoidan-induced ROS generation. Our results demonstrated that knockdown of TLR4 abolishes fucoidan-induced ROS levels and CHOP expression, indicating TLR4 involvement in fucoidan-induced ROS generation and ER stress in lung cancer. However, we could not exclude the possibility that the TLR4-shRNAs we used were inefficient at inhibiting endogenous TLR4 expression and function in our cells. It is also likely that other TLRs are involved in the interaction with fucoidan. Fucoidan increases ROS levels over a broad range of time, suggesting that fucoidan induces the activation of TLR4-mediated ROS generation. Alternatively, we could not exclude the possibility that the ROS-mediated mitochondrial pathway and apoptosis are involved in our system23,24.
We previously demonstrated that fucoidan effectively inhibits cell growth and migration via induction of Smurf2-dependent ubiquitin degradation of TGFβ (TGF) receptors (TGFR) in lung cancer cells7. Here we also found that fucoidan activation of TLR4 and TLR4-mediated ROS-induced ER stress (PERK-eIF2α-ATF4-CHOP pathway), which involved in fucoidan-induced apoptosis (activation of caspase 3 and PARP) of lung cancer cells. These findings suggest that there are multiple signaling pathways involved in fucoidan-mediated antitumor functions within lung cancer cells; however, the binding or targeting molecule or receptor of fucoidan on the surface of cancer cell membranes is still unclear. Interestingly, we previously reported that fucoidan may serve as a ligand to interact with TLR4 or scavenger receptor A on cellular surfaces of macrophages, resulting in induction of cytokine expression43,44,45. Alternatively, Tollip, a negative regulator of TLR4, cooperates with Smad7 to mediate ubiquitination-dependent degradation of TGFR46. More recently, we found that fucose-containing polysaccharides from Reishi enhances the cooperation of Tollip with the TGFR/Smurf2/Smad7 complex and further modulates the degradation of TGFR47. Thus, it would be an interesting topic of research for whether there is any association between degradation of TGFR and activation of TLR4 upon fucoidan treatment.
Recently, the interplay between TGF/TGFR and ROS-mediated oxidative stress has been discussed. Evidence indicates that TGF/TGFR is able to control ROS production directly or by modulating anti-oxidation systems. Several studies have shown that ligation of TGF to TGFR can induce ROS production in different cellular compartments, including that TGF-β induces ROS production in mitochondria39. By contrast, ROS can influence TGF/TGFR signaling and increase TGF expression as well as its activation from the latent complex. It is demonstrated that ROS mediates the TGF/TGFR-regulated expression of a group of genes, but little is known about how ROS may regulate the activation of TGF/TGFR-mediated intracellular signal transduction. It has been reported that Smad2-mediated signaling seems to be sensitive to ROS effects, due to studies which showed that TGF-stimulated Smad2 phosphorylation can be inhibited by N-acetyl cysteine39. Elucidating the complex interplay and roles of TGF/TGFR-mediated signalings and ROS-induced signal redox stress in cancer is important for the understanding of their participation in tumorigenesis. In the future, we will examine the possibility of TLR4 activation and induced ROS involved in fucoidan-induced degradation of TGFRs and the downstream signaling pathways.
It is reported that fucoidan, polysaccharides derived from various brown seaweeds, exert different anti-cancer effects. However, there are many “factors” of fucoidan involved in anti-cancer functions; for example, sources of fucoidan (species of brown seaweeds)23,24,25, effective concentration, structural characteristics, sulfate content, molecular weight, purity, isolation/extraction methods, etc., as well as importantly the kind of cancer cells to be tested. Here, using HiQ-fucoidan from Laminaria japonica, we found that fucoidan also prevents and inhibits lung tumor growth at higher concentrations (Supplementary Fig. 7) in vitro and in vivo, even though the species from which HiQ-fucoidan (Laminaria japonica) and fucoidan (Fucus vesiculosus) are derived from differ. Under the same experimental conditions, we found that both types of fucoidan exert similar biological functions in cellular apoptosis and anti-lung cancer activity. In our future work, we will further examine and compare the relationship between structural characteristics and anti-cancer activity within HiQ-fucoidan and fucoidan. Overall, our current results suggest that fucoidan exerts both preventive and therapeutic effects in a lung cancer mouse model. Therefore, we propose using fucoidan as a nutritional/dietary supplement to prevent and inhibit lung cancer progression.
Materials and Methods
Cell lines and cell culture
Human non-small cell lung adenocarcinoma cell lines A549 and CL1-5 were obtained from Dr. P.-C. Yang (NTU, Taiwan). The human embryonic kidney (HEK) 293 T cell line was obtained from Dr. I.-T. Chen (NYMU, Taiwan). The mouse Lewis lung carcinoma LLC1 was purchased from the Bioresource Collection and Research Center (BCRC, Hsinchu, Taiwan). Cells were cultured as previously described7,48.
Reagents and antibodies
Fucoidan from Fucus vesiculosus was obtained from Sigma-Aldrich Co. (St. Louis, MO, USA) as fucoidan. Fucoidan from Laminaria japonica was a gift from Hi-Q Marine Biotech International, Ltd. (Taiwan) as HiQ-fucoidan. PI, NAC, anti-actin (AC-74), anti-pERK1/2 (MAPK-YT) and anti-p21 (CP74) were purchased from Sigma-Aldrich Co. (St. Louis, MO, USA). Lipofectamine 2000 was purchased from Invitrogen (Grand Island, NY, USA). Anti-AKT, anti-p-AKT (S473) and anti-mouse IgG-HRP were purchased from Santa Cruz Biotechnology (CA, USA). Anti-CHOP, anti-GRP78, anti-eIF2α, and anti-rabbit IgG-HRP were purchased from GeneTex, Inc. (Hsinchu, Taiwan). Anti-caspase3 (8G10), anti-p-PERK (T980; 16F8), anti-PERK (D11A8), anti-p-eIF2α (Ser51, 119A11), anti-TLR4 (D8L5W) and anti-ATF4 (D4B8) were purchased from Cell Signaling (Beverly, MA, USA).
Western blot analysis
Cancer cells from each experimental condition were rinsed with cold phosphate-buffered saline (PBS) containing 1% Na3VO4 and harvested by scraping into lysis buffer (10 mM HEPES pH 7.9, 10 mM KCl, 0.1 mM EDTA, 0.1 mM EGTA, proteinase inhibitors). Whole-cell lysates were centrifuged at 13,000 × g for 10 min at 4 °C. Protein concentration of the supernatant was determined by Bradford assays (Bio-Rad, Hercules, CA, USA), and bovine serum albumin (BSA; Thermo Fisher Scientific, Rockwood, TN) was used as a standard. Cell extracts (40 μg) were subjected to Western blot analysis. Actin expression was used as an internal control. The detailed procedure has been described previously6. Quantification of the detected protein band intensities was determined using ImageJ (National Institute of Mental Health, Bethesda, MD, USA) and is representative of three separate experiments.
Cell viability assay via crystal violet staining
Cells (1 × 105 cells per well) were seeded in a 12-well plates and incubated overnight prior to treatment with fucoidan for 48 h. After incubation, each well was rinsed with PBS. The attached cells were fixed and stained with 1% crystal violet (Bioman, Taiwan) solution in 30% ethanol (PanReac AppliChem, USA) for 30 min followed by staining with 33% acetic acid (Bioman, Taiwan) to dissolve the crystal violet. Cell viability was determined by detecting absorbance wavelengths from 570 to 670 nm.
Apoptosis analysis
Cells (5 × 105 cells per plate) were seeded in a 6-cm plate and incubated overnight prior to treatment with fucoidan (100 to 400 μg/ml) for 48 h. These cells were harvested by trypsinization and washed with 1.0 ml cold PBS. Fucoidan-induced apoptosis was detected using an Alexa Fluor 488 Annexin V Apoptosis Kit (Life Technologies).
Detection of intracellular ROS
ROS was measured using 2′,7′-dichlorodihydrofluorescein diacetate (H2DCFDA, Life Technologies) as previously reported30. Cells (1 × 104 cells per well) were seeded in triplicate in a 96-well plate and incubated overnight prior to treatment with fucoidan (20 to 400 μg/ml) for 10 to 60 min. After the cells were washed with PBS, they were stained with 200 μM H2DCFDA and incubated at 37 °C for 30 min. After incubation, cells were washed with PBS. The medium was replaced with fresh cell medium, and the cells were incubated at 37 °C for 30 min. Fluorescence intensity of the DCF probe was detected using Infinite 200 PRO multimode microplate readers (TECAN, Switzerland) or FACScan flow cytometry (Becton Dickinson, Germany) at excitation and emission wavelengths of 485 and 535 nm, respectively.
In vivo lung cancer mouse model
Male C57BL/6 strains of mice (aged 6 to 8 weeks) were obtained from the National Laboratory Animal Center of Taiwan. Mice were raised under pathogen-free conditions in the Animal Center of National Yang-Ming University (NYMU). All experimental methods involving animals were carried out in accordance with guidelines and regulations of the Institutional Animal Care and Use Committee (IACUC) of NYMU, and all experimental protocols were approved by the IACUC of NYMU.
To examine the effect of fucoidan on tumor volume, the mice were randomly distributed into two groups and orally fed with either ddH2O (control group) or fucoidan at 24 mg/kg/day (experimental group). After oral feeding with fucoidan for 2 weeks, each mouse was inoculated with LLC1 cells (2 × 105 cells per mouse) into the hypodermic dorsum and orally fed with fucoidan for 3 weeks. The detailed procedure has been described previously7.
RNA interference with sh-ATF4, sh-CHOP or sh-TLR4
Specific shRNA oligonucleotides targeting ATF4, CHOP and TLR4 based on the human ATF4 (NM_001675.2), DDIT3 (NM_004083), and TLR4 genes (NM_138554.3), respectively, were obtained from the Taiwan National RNAi Core Facility Platform. The targeting sequences for ATF4, CHOP and TLR4 are listed in Supplementary Table S1, and the procedure has previously been described7.
Statistical analysis
All data are expressed as the mean ± standard error. Significant differences between two groups were determined by t-test analyses using statistical software, GraphPad Prism5. A P-value of <0.05 was considered statistically significant (*P < 0.05, **P < 0.01 and ***P < 0.005).
Additional Information
How to cite this article: Hsu, H.-Y. et al. Fucoidan induces Toll-like receptor 4-regulated reactive oxygen species and promotes endoplasmic reticulum stress-mediated apoptosis in lung cancer. Sci. Rep. 7, 44990; doi: 10.1038/srep44990 (2017).
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Material
Acknowledgments
This work was supported by the Ministry of Science and Technology of Taiwan (MOST-104-2320-B-010-024-MY2 and MOST-104-2320-B-010-029-MY2 to H.-Y.H.); The Ministry of Education, The Top University Project (104AC-P664 to H.-Y.H.); and National Yang-Ming University (Ministry of Education, Aim for the Top University Plan) Taiwan (to H.-Y.H.).
Footnotes
The authors declare no competing financial interests.
Author Contributions H.Y. Hsu, T.Y. Lin, M.K. Lu, S.M. Tsao, and Y.C. Wu designed the experiments; T.Y. Lin, P.J. Leng, and S.M. Tsao performed the experiments and analyzed data; H.Y. Hsu, T.Y. Lin and S.M. Tsao wrote the paper.
References
- Cumashi A. et al. A comparative study of the anti-inflammatory, anticoagulant, antiangiogenic, and antiadhesive activities of nine different fucoidans from brown seaweeds. Glycobiology 17, 541–552, doi: 10.1093/glycob/cwm014 (2007). [DOI] [PubMed] [Google Scholar]
- Ustyuzhanina N. E. et al. Fucoidans: pro- or antiangiogenic agents? Glycobiology 24, 1265–1274, doi: 10.1093/glycob/cwu063 (2014). [DOI] [PubMed] [Google Scholar]
- Atashrazm F., Lowenthal R. M., Woods G. M., Holloway A. F. & Dickinson J. L. Fucoidan and cancer: a multifunctional molecule with anti-tumor potential. Marine drugs 13, 2327–2346, doi: 10.3390/md13042327 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwak J. Y. Fucoidan as a marine anticancer agent in preclinical development. Mar Drugs 12, 851–870, doi: 10.3390/md12020851 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee H., Kim J. S. & Kim E. Fucoidan from seaweed Fucus vesiculosus inhibits migration and invasion of human lung cancer cell via PI3K-Akt-mTOR pathways. PLoS One 7, e50624, doi: 10.1371/journal.pone.0050624 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsu H. Y. et al. Fucoidan induces changes in the epithelial to mesenchymal transition and decreases metastasis by enhancing ubiquitin-dependent TGFbeta receptor degradation in breast cancer. Carcinogenesis 34, 874–884, doi: 10.1093/carcin/bgs396 (2013). [DOI] [PubMed] [Google Scholar]
- Hsu H. Y. et al. Fucoidan inhibition of lung cancer in vivo and in vitro: role of the Smurf2-dependent ubiquitin proteasome pathway in TGFbeta receptor degradation. Oncotarget 5, 7870–7885 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu G., Kuang S., Wu S., Jin W. & Sun C. A novel polysaccharide from Sargassum integerrimum induces apoptosis in A549 cells and prevents angiogensis in vitro and in vivo. Scientific Reports 6, 26722, doi: 10.1038/srep26722 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuribayashi K., Funaguchi N. & Nakano T. Chemotherapy for advanced non-small cell lung cancer with a focus on squamous cell carcinoma. Journal of cancer research and therapeutics 12, 528–534, doi: 10.4103/0973-1482.174185 (2016). [DOI] [PubMed] [Google Scholar]
- Zhang J. F., Li M., Miao J. Y. & Zhao B. X. Biological activities of novel pyrazolyl hydroxamic acid derivatives against human lung cancer cell line A549. Eur J Med Chem 83C, 516–525, doi: 10.1016/j.ejmech.2014.06.065 (2014). [DOI] [PubMed] [Google Scholar]
- Tan C.-S., Gilligan D. & Pacey S. Treatment approaches for EGFR-inhibitor-resistant patients with non-small-cell lung cancer. The Lancet Oncology 16, e447–e459, doi: 10.1016/S1470-2045(15)00246-6 (2015). [DOI] [PubMed] [Google Scholar]
- Berridge M. J. The endoplasmic reticulum: a multifunctional signaling organelle. Cell Calcium 32, 235–249 (2002). [DOI] [PubMed] [Google Scholar]
- Kim K. M. et al. Expression of ER stress and autophagy-related molecules in human non-small cell lung cancer and premalignant lesions. International Journal of Cancer 131, E362–E370, doi: 10.1002/ijc.26463 (2012). [DOI] [PubMed] [Google Scholar]
- Xu C., Bailly-Maitre B. & Reed J. C. Endoplasmic reticulum stress: cell life and death decisions. J Clin Invest 115, 2656–2664, doi: 10.1172/JCI26373 (2005). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oyadomari S. & Mori M. Roles of CHOP/GADD153 in endoplasmic reticulum stress. Cell Death Differ 11, 381–389, doi: 10.1038/sj.cdd.4401373 (2004). [DOI] [PubMed] [Google Scholar]
- Puthalakath H. et al. ER stress triggers apoptosis by activating BH3-only protein Bim. Cell 129, 1337–1349, doi: 10.1016/j.cell.2007.04.027 (2007). [DOI] [PubMed] [Google Scholar]
- Timmins J. M. et al. Calcium/calmodulin-dependent protein kinase II links ER stress with Fas and mitochondrial apoptosis pathways. The Journal of clinical investigation 119, 2925–2941, doi: 10.1172/JCI38857 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trachootham D., Alexandre J. & Huang P. Targeting cancer cells by ROS-mediated mechanisms: a radical therapeutic approach? Nat Rev Drug Discov 8, 579–591 (2009). [DOI] [PubMed] [Google Scholar]
- Liou G. Y. & Storz P. Reactive oxygen species in cancer. Free Radic Res 44, 479–496, doi: 10.3109/10715761003667554 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yokouchi M. et al. Involvement of selective reactive oxygen species upstream of proapoptotic branches of unfolded protein response. J Biol Chem 283, 4252–4260, doi: 10.1074/jbc.M705951200 (2008). [DOI] [PubMed] [Google Scholar]
- Malhotra J. D. et al. Antioxidants reduce endoplasmic reticulum stress and improve protein secretion. Proc Natl Acad Sci USA 105, 18525–18530, doi: 10.1073/pnas.0809677105 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen S., Zhao Y., Zhang Y. & Zhang D. Fucoidan induces cancer cell apoptosis by modulating the endoplasmic reticulum stress cascades. PloS one 9, e108157, doi: 10.1371/journal.pone.0108157 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Z., Teruya K., Eto H. & Shirahata S. Fucoidan extract induces apoptosis in MCF-7 cells via a mechanism involving the ROS-dependent JNK activation and mitochondria-mediated pathways. PloS one 6, e27441, doi: 10.1371/journal.pone.0027441 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang L. et al. Fucoidan derived from Undaria pinnatifida induces apoptosis in human hepatocellular carcinoma SMMC-7721 cells via the ROS-mediated mitochondrial pathway. Marine drugs 11, 1961–1976, doi: 10.3390/md11061961 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wei C. et al. Fucoidan inhibits proliferation of the SKM-1 acute myeloid leukaemia cell line via the activation of apoptotic pathways and production of reactive oxygen species. Molecular medicine reports 12, 6649–6655, doi: 10.3892/mmr.2015.4252 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y. et al. Perturbation of the heparin/heparin-sulfate interactome of human breast cancer cells modulates pro-tumourigenic effects associated with PI3K/Akt and MAPK/ERK signalling. Thrombosis and haemostasis 109, 1148–1157, doi: 10.1160/th12-12-0935 (2013). [DOI] [PubMed] [Google Scholar]
- Park H. Y. et al. Fucoidan inhibits the proliferation of human urinary bladder cancer T24 cells by blocking cell cycle progression and inducing apoptosis. Molecules 19, 5981–5998, doi: 10.3390/molecules19055981 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sano R. & Reed J. C. ER stress-induced cell death mechanisms. Biochim Biophys Acta 1833, 3460–3470, doi: 10.1016/j.bbamcr.2013.06.028 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zou P. et al. ROS generation mediates the anti-cancer effects of WZ35 via activating JNK and ER stress apoptotic pathways in gastric cancer. Oncotarget 6, 5860–5876 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsu H. Y. & Wen M. H. Lipopolysaccharide-mediated reactive oxygen species and signal transduction in the regulation of interleukin-1 gene expression. The Journal of biological chemistry 277, 22131–22139, doi: 10.1074/jbc.M111883200 (2002). [DOI] [PubMed] [Google Scholar]
- Makarenkova I. D. et al. [Sulfated polysaccharides of brown seaweeds--ligands of toll-like receptors]. Biomed Khim 58, 318–325 (2012). [DOI] [PubMed] [Google Scholar]
- Lee J. H., Lee S. H., Choi S. H., Asahara T. & Kwon S. M. The sulfated polysaccharide fucoidan rescues senescence of endothelial colony-forming cells for ischemic repair. Stem cells (Dayton, Ohio) 33, 1939–1951, doi: 10.1002/stem.1973 (2015). [DOI] [PubMed] [Google Scholar]
- Kasai A., Arafuka S., Koshiba N., Takahashi D. & Toshima K. Systematic synthesis of low-molecular weight fucoidan derivatives and their effect on cancer cells. Organic & biomolecular chemistry 13, 10556–10568, doi: 10.1039/c5ob01634g (2015). [DOI] [PubMed] [Google Scholar]
- Yoshimoto M., Higaki K., Nanba E. & Ikeguchi M. Anti-Proliferation Activity of Fucoidan in MKN45 Gastric Cancer Cells and Downregulation of Phosphorylated ASK1, a Cell Cycle-Regulated Kinase. Yonago acta medica 58, 1–7 (2015). [PMC free article] [PubMed] [Google Scholar]
- Yamasaki-Miyamoto Y., Yamasaki M., Tachibana H. & Yamada K. Fucoidan induces apoptosis through activation of caspase-8 on human breast cancer MCF-7 cells. Journal of agricultural and food chemistry 57, 8677–8682, doi: 10.1021/jf9010406 (2009). [DOI] [PubMed] [Google Scholar]
- Han Y. S., Lee J. H. & Lee S. H. Antitumor Effects of Fucoidan on Human Colon Cancer Cells via Activation of Akt Signaling. Biomolecules & therapeutics 23, 225–232, doi: 10.4062/biomolther.2014.136 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Min E. Y. et al. The effects of fucodian on senescence are controlled by the p16INK4a-pRb and p14Arf-p53 pathways in hepatocellular carcinoma and hepatic cell lines. International journal of oncology 45, 47–56, doi: 10.3892/ijo.2014.2426 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pelicano H., Carney D. & Huang P. ROS stress in cancer cells and therapeutic implications. Drug resistance updates: reviews and commentaries in antimicrobial and anticancer chemotherapy 7, 97–110, doi: 10.1016/j.drup.2004.01.004 (2004). [DOI] [PubMed] [Google Scholar]
- Krsti J., Trivanovi D., Mojsilovi S. & Santibanez J. F. Transforming Growth Factor-Beta and Oxidative Stress Interplay: Implications in Tumorigenesis and Cancer Progression. Oxidative Medicine and Cellular Longevity 2015, 15, doi: 10.1155/2015/654594 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu X. et al. NADPH oxidase 1-dependent ROS is crucial for TLR4 signaling to promote tumor metastasis of non-small cell lung cancer. Tumour Biol 36, 1493–1502, doi: 10.1007/s13277-014-2639-9 (2015). [DOI] [PubMed] [Google Scholar]
- Li D., Jin Y., Sun Y., Lei J. & Liu C. Knockdown of toll-like receptor 4 inhibits human NSCLC cancer cell growth and inflammatory cytokine secretion in vitro and in vivo. Int J Oncol 45, 813–821, doi: 10.3892/ijo.2014.2479 (2014). [DOI] [PubMed] [Google Scholar]
- Yuan X. et al. Activation of TLR4 signaling promotes gastric cancer progression by inducing mitochondrial ROS production. Cell Death Dis 4, e794, doi: 10.1038/cddis.2013.334 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsu H. Y., Hajjar D. P., Khan K. M. & Falcone D. J. Ligand binding to macrophage scavenger receptor-A induces urokinase-type plasminogen activator expression by a protein kinase-dependent signaling pathway. The Journal of biological chemistry 273, 1240–1246 (1998). [DOI] [PubMed] [Google Scholar]
- Hsu H. Y., Chiu S. L., Wen M. H., Chen K. Y. & Hua K. F. Ligands of macrophage scavenger receptor induce cytokine expression via differential modulation of protein kinase signaling pathways. The Journal of biological chemistry 276, 28719–28730, doi: 10.1074/jbc.M011117200 (2001). [DOI] [PubMed] [Google Scholar]
- Yu H. et al. Scavenger receptor A (SR-A) is required for LPS-induced TLR4 mediated NF-kappaB activation in macrophages. Biochimica et biophysica acta 1823, 1192–1198, doi: 10.1016/j.bbamcr.2012.05.004 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu L. et al. Tollip, an intracellular trafficking protein, is a novel modulator of the transforming growth factor-beta signaling pathway. The Journal of biological chemistry 287, 39653–39663, doi: 10.1074/jbc.M112.388009 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsao S.-M. & Hsu H.-Y. Fucose-containing fraction of Ling-Zhi enhances lipid rafts-dependent ubiquitination of TGFβ receptor degradation and attenuates breast cancer tumorigenesis. Scientific Reports 6, 36563, doi: 10.1038/srep36563 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu C. T. et al. Ling Zhi-8 mediates p53-dependent growth arrest of lung cancer cells proliferation via the ribosomal protein S7-MDM2-p53 pathway. Carcinogenesis 32, 1890–1896, doi: 10.1093/carcin/bgr221 (2011). [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.