Summary
Setting
Four regions in Kazakhstan where participants were recruited from June 2012 to May 2014.
Objective
To examine associations between incarceration history and tobacco, alcohol, and drug consumption, and human immunodeficiency virus (HIV) infection and diabetes mellitus (DM) with TB.
Design
This matched case-control study included 1600 participants who completed a survey on sociodemographics, history of incarceration, tobacco, alcohol and drug use, and HIV and DM diagnosis. Conditional logistic regression analysis was used to examine associations between a TB diagnosis and risk factors.
Results
Participants who had ever smoked tobacco (aOR 1.73, 95%CI 1.23–2.43, P ≤ 0.01), ever drank alcohol (aOR 1.41, 95%CI 1.03–1.93, P ≤ 0.05), were HIV-positive (aOR 36.37, 95%CI 2.05–646.13, P ≤ 0.05) or had DM (aOR 13.96, 95%CI 6.37–30.56, P ≤ 0.01) were more likely to have TB.
Conclusions
The association between TB and tobacco use, alcohol use, HIV and DM in Kazakhstan suggests a need for comprehensive intervention and prevention approaches that also address tobacco and alcohol use, DM and HIV.
Keywords: tobacco, alcohol, HIV, diabetes
Following The Collapse of the Soviet Union, Kazakhstan experienced a drastic increase in tuberculosis (TB).1 In 2014, the World Health Organization estimated the TB prevalence in Kazakhstan at 127 cases per 100 000 population.2 Individual risks, such as age, sex, smoking, diabetes mellitus (DM), human immunodeficiency virus (HIV) status, incarceration and migrant status have been found to be associated with TB.3–6 Broader socio-economic and environmental factors, such as financial insecurity and housing conditions, have also been found to be associated with TB.3,4 Using Kazakhstan national surveillance data for the period 2006–2010, Terlikbayeva et al. found that being a registered contact of a TB case, being incarcerated within the past 2 years and being unemployed were among the factors significantly associated with new TB cases.7 However, there is a paucity of research on TB in Kazakhstan, and risk factors associated with TB in the country have not been adequately studied. Studies have primarily focused on incarcerated populations and injecting drug users.8,9 Few studies have focused on TB among the general population in Kazakhstan, and little research has been conducted on other risk factors associated with TB in Kazakhstan, such as chronic diseases.
There is growing evidence to support associations between TB and concomitant diseases, such as between TB and DM10 and TB and HIV.11 In Kazakhstan, the Joint United Nations Programme on HIV and AIDS estimates HIV/AIDS (acquired immune-deficiency syndrome) prevalence at 0.2%,12 while the International Diabetes Federation estimates DM prevalence at 6.2%.13 Previous research indicates that these diseases may worsen the progression of TB and complicate effective anti-tuberculosis treatment.10,11 However, these diseases are not always screened for in TB clinics.
Tobacco use is widespread throughout Kazakhstan.14 Individuals who smoke have been found to have more severe clinical presentations of TB, a lower rate of treatment success and a higher rate of TB relapse.15 High rates of tobacco use may play a role in limiting the effectiveness of TB treatment and control efforts in Kazakhstan.16 The present study examines potential risk factors associated with TB in a matched sample of the general population in Kazakhstan.
Study Population and Methods
Sampling and recruitment
Data were collected from June 2012 to May 2014. Participants were recruited from four regions of Kazakhstan: Almaty City and the Almaty, Kyzylorda, and Kostanay oblasts. Sites were selected based on an analysis of countrywide surveillance data. Both high and low TB burden sites located in geographically diverse areas were selected. The sample consisted of 562 individuals, with TB identified by the national TB programme. One household and one community control were identified for each index case to differentially assess household- and environment-related risk factors for TB.
All participants had to be aged ≥18 years, have other adults living in their household, speak fluent Russian or Kazakh and be free of conditions that would impair their ability to provide informed consent. Individuals with TB had to have been diagnosed with new pulmonary TB by positive TB culture or on clinical and radiographic grounds within 3 months before study enrolment and respond to anti-tuberculosis treatment. Of all cases studied, 36% were culture-positive and the remainder were diagnosed based on clinical grounds. Household and community controls self-reported at baseline that they did not have TB. We confirmed with the local TB clinics at each site that controls were not registered and had not received treatment for TB.
In case more than one household control was eligible, the Kish method was used to randomly select a household control for the case. Community controls were sampled from the same building in urban settings or within a limited geographic radius in rural settings. In urban settings, all residences within the building were given a number and an apartment was randomly selected for inclusion in the study. In rural settings, the community control household was selected by choosing a random direction from the index case's residence and selecting the third dwelling from the index's household. If more than one adult was eligible after pre-screening all adults in the household, recruiters randomly selected one community control. Eligible individuals who refused to participate in the study were replaced by other index cases or other randomly sampled household and community controls.
Measures
Consenting participants completed a survey in Russian or Kazakh language using audio computer-assisted self-interviews. All questionnaires were administered in private rooms. Demographic variables, such as age, country of origin, marital status and education, were gathered. Data were also collected on criminal history, substance-related risk behaviours and chronic diseases. Participants were also asked whether they had ever been tested for HIV or diagnosed with DM by a physician. Measures used included the Living Standards Measurement Survey,17 the CAGE questionnaire18 and the Global Adult Tobacco Survey.19 Additional questions were taken from previous pilot studies conducted by the Columbia University Global Health Research Center of Central Asia, the Demographic Health Survey20 and the World Health Survey.21
Power considerations
We calculated that a sample size of 1600 participants (600 cases and 500 in each control group) would give us 80% power to detect an odds ratio (OR) of 1.6 for any risk factor with a prevalence between 10% and 85% in controls, and an OR of 1.4 for any factor with a prevalence between 20% and 70%. To account for possible loss to follow-up, we aimed to recruit a total of 1800 participants, i.e., 600 in each group.
Statistical analyses
We used descriptive statistics to characterise the sample. Estimates of risk factors were calculated overall and by TB status (individuals with TB vs. individuals without TB). For the bivariate analysis to determine which factors were associated with TB status, we conducted conditional logistic regression using three different models: one comparing TB cases to household controls, one comparing TB cases to community controls and one comparing TB cases to both control groups combined. For the multivariate model, all sociodemographic variables, lifetime occurrence behavioural variables, and HIV and DM comorbidities were simultaneously included in the conditional logistic regression for each of the three different models. Behavioural variables involving frequency and current behaviour were excluded from the multivariate model to avoid collinearity. In Model 1, because low numbers of household controls reported some variables (i.e., drug use behaviours, HIV diagnosis), these variables had to be removed for the model to converge. χ2 tests were used to calculate significant differences in risk factors between TB cases who were bacteriologically confirmed and those who were non-bacteriologically confirmed. A subgroup analysis was conducted examining risk factors associated with TB cases who were bacteriologically confirmed. All analyses were conducted using SPSS, version 23 (Statistical Package for the Social Sciences, Durham, NC, USA).
All protocols for the study were approved by the institutional review boards of the Kazakhstan School of Public Health, Almaty; Nazarbayev University, Astana, Kazakhstan; and Columbia University, New York, NY, USA (#IRB-AAAJ8510). All participants provided informed consent.
Results
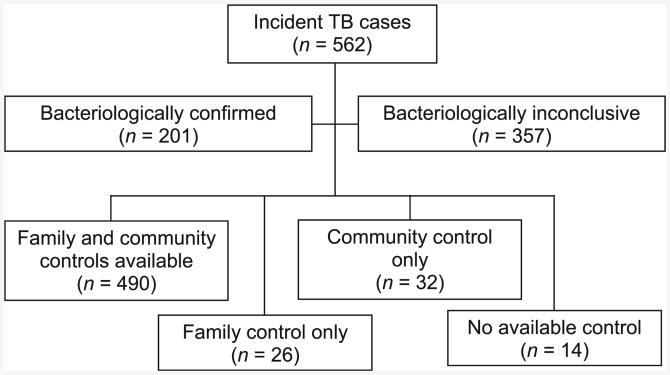
Of 1802 participants screened for the study, 1600 were enrolled (562/744 cases, 515/516 household controls, 523/543 community controls). Of the total TB cases, 201 were bacteriologically confirmed and 357 were non-bacteriologically confirmed. Four hundred and ninety cases had both family and community controls, 32 had only a community control, 26 had only a family control and 14 had no controls (Figure). Demographic characteristics are shown in Table 1.
Figure.
Recruitment groups. TB = tuberculosis.
Table 1. Sociodemographic characteristics by TB status (n = 1600, TB cases = 562, individuals without TB = 1038).
| Characteristics | Overall (n = 1600) n (%) | Individuals with TB (n = 562, 35.1%) n (%) | Individuals without T (n = 1038, 64.9%) n (%) |
|---|---|---|---|
| Sociodemographic | |||
| Age, years, mean ± SD | 38.89 ± 13.52 | 35.38 ± 13.1 | 40.77 ± 13.37 |
| Sex, n (%) | |||
| Male | 739 (46.2) | 308 (55.0) | 431 (41.4) |
| Female | 861 (53.8) | 252 (45.0) | 609 (58.6) |
| Country of birth | |||
| Kazakhstan | 1461 (91.3) | 510 (91.1) | 951 (91.4) |
| Other | 139 (8.7) | 50 (8.9) | 89 (8.6) |
| Ethnicity | |||
| Kazakh | 1209 (75.6) | 430 (76.8) | 779 (74.9) |
| Russian | 230 (14.4) | 78 (13.9) | 152 (14.6) |
| Other | 161 (10.1) | 52 (9.3) | 109 (10.5) |
| Education | |||
| High school or less | 569 (35.6) | 213 (38.0) | 356 (34.2) |
| Vocational education or higher | 1031 (64.4) | 349 (62.1) | 682 (65.7) |
| Marital status | |||
| Married | 1100 (68.8) | 347 (62.0) | 753 (72.4) |
| Divorced/separated | 204 (12.8) | 61 (10.9) | 143 (13.8) |
| Single, never married | 296 (18.5) | 152 (27.3) | 144 (13.8) |
| Behavioural | |||
| Ever incarcerated | |||
| Yes | 36 (2.3) | 21 (3.7) | 15 (1.4) |
| No | 1564 (97.8) | 541 (96.3) | 1023 (98.6) |
| Time incarcerated in the past 90 days, days, mean ± SD | 0.02 ± 0.78 | 0.07 ± 1.32 | 0 |
| Ever smoked tobacco | |||
| Yes | 569 (35.6) | 250 (44.5) | 319 (30.7) |
| No | 1031 (64.4) | 312 (55.5) | 719 (69.3) |
| Currently smoke tobacco | |||
| Yes | 231 (14.4) | 138 (13.3) | 93 (16.5) |
| No | 1369 (85.6) | 900 (86.7) | 469 (83.5) |
| Cigarettes smoked in a week, mean ± SD | 12.83 ± 38.34 | 13.97 ± 38.94 | 12.21 ± 38.02 |
| Ever used non-smoking tobacco | |||
| Yes | 91 (5.7) | 51 (9.1) | 40 (3.9) |
| No | 1509 (94.3) | 511 (90.9) | 998 (96.1) |
| Currently use non-smoking tobacco | |||
| Yes | 19 (1.2) | 12 (2.1) | 7 (0.7) |
| No | 1581 (98.8) | 550 (97.9) | 1031 (99.3) |
| Number of times used non-smoking tobacco in last week, mean ± SD | 0.31 ± 3.30 | 0.20 ± 2.74 | 0.51 ± 4.13 |
| Ever drank alcohol | |||
| Yes | 679 (42.4) | 279 (49.6) | 400 (38.5) |
| No | 921 (57.6) | 283 (50.4) | 638 (61.5) |
| Binge drank alcohol in past 90 days | |||
| Yes | 138 (8.6) | 43 (7.7) | 95 (9.2) |
| No | 1462 (91.4) | 519 (92.3) | 943 (90.8) |
| Frequency of alcohol consumption | |||
| Never drank alcohol | 921 (57.6) | 283 (50.4) | 638 (61.5) |
| Monthly or less | 324 (20.3) | 105 (18.7) | 219 (21.1) |
| 2–4 times a month | 108 (6.8) | 36 (6.4) | 72 (6.9) |
| 2–3 times a week | 13 (0.8) | 6 (1.1) | 7 (0.7) |
| ≥4 times a week | 9 (0.6) | 3 (0.5) | 6 (0.6) |
| Does not currently drink | 225 (14.1) | 129 (23.0) | 96 (9.2) |
| Alcohol abuse (CAGE scale)18 | |||
| Yes | 140 (8.8) | 56 (10.0) | 84 (8.1) |
| No | 1460 (91.3) | 506 (90.0) | 954 (91.9) |
| Ever used opium | |||
| Yes | 11 (0.7) | 7 (1.2) | 4 (0.4) |
| No | 1589 (99.4) | 555 (98.8) | 1034 (99.6) |
| Ever smoked heroin | |||
| Yes | 4 (0.3) | 1 (0.2) | 3 (0.3) |
| No | 1596 (99.8) | 561 (99.8) | 1035 (99.7) |
| Ever injected heroin | |||
| Yes | 10 (0.6) | 5 (0.9) | 5 (0.5) |
| No | 1590 (99.4) | 557 (99.1) | 1033 (99.5) |
| Ever used marijuana | |||
| Yes | 44 (2.8) | 26 (4.6) | 18 (1.7) |
| No | 1556 (97.3) | 536 (95.4) | 1020 (98.3) |
| Used marijuana in the past 90 days | |||
| Yes | 12 (0.8) | 8 (1.4) | 4 (0.4) |
| No | 1588 (99.3) | 554 (98.6) | 1034 (99.6) |
| Ever injected drugs | |||
| Yes | 19 (1.2) | 5 (0.9) | 14 (1.3) |
| No | 1581 (98.8) | 557 (99.1) | 1024 (98.7) |
| Concomitant disease | |||
| Diagnosed with diabetes | |||
| Yes | 49 (3.1) | 40 (7.1) | 9 (0.9) |
| No | 1551 (96.9) | 522 (92.9) | 1029 (99.1) |
| Ever tested for HIV | |||
| Yes | 1282 (80.1) | 531 (94.5) | 751 (72.4) |
| No | 318 (19.9) | 31 (5.5) | 287 (27.6) |
| Diagnosed with HIV | |||
| HIV-positive | 8 (0.5) | 7 (1.2) | 1 (0.1) |
| HIV-negative | 1166 (72.9) | 466 (82.9) | 700 (67.4) |
| Did not get test results back | 108 (6.8) | 58 (10.3) | 50 (4.8) |
| Was never tested for HIV | 318 (19.9) | 31 (5.5) | 287 (27.6) |
TB = tuberculosis; SD = standard deviation; HIV = human immunodeficiency virus.
Bivariable analysis comparing TB cases to the combined control group revealed that younger age (P ≤ 0.01), male sex (P ≤ 0.01), being single (P ≤ 0.01), previous incarceration (P ≤ 0.05), ever smoked or currently smokes tobacco (P ≤ 0.01), ever used non-smoking tobacco (P ≤ 0.01), currently uses non-smoking tobacco (P ≤ 0.05), ever drank alcohol (P ≤ 0.01), previously drank but does not currently drink (P ≤ 0.01), ever used marijuana (P ≤ 0.01), used marijuana in the past 90 days (P ≤ 0.05), being HIV-positive (P ≤ 0.01) or having DM (P ≤ 0.01) were associated with TB (Appendix Table A.1).*
Multivariable conditional logistic regression analysis revealed that individuals who were older and Russian were less likely to have TB in all three models (Table 2). Participants who were single were more likely to have TB in Model 1 (P ≤ 0.01) and Model 3 (P ≤ 0.01). Those who had ever smoked tobacco were significantly more likely to have TB in Model 2 (P ≤ 0.01) and in Model 3 (P ≤ 0.01). Participants who had ever drank alcohol were more likely to have TB in Model 1 (P ≤ 0.05) and in Model 3 (P ≤ 0.05). Participants who were HIV-positive were more likely to have TB in Model 3 (P ≤ 0.05). Participants who were ever diagnosed with DM were significantly more likely to have TB in all three models.
Table 2. Factors associated with TB case status in the Almaty Region, Kazakhstan (TB cases = 562, household controls = 515, community controls = 523)*.
| Variable | Model 1 | Model 2 | Model 3 | |||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| aOR (95%CI) | P value | aOR (95%CI) | P value | aOR (95%CI) | P value | |
| Sociodemographic | ||||||
| Age | 0.97 (0.95–0.98) | 0.000† | 0.97 (0.96–0.98) | 0.000† | 0.97 (0.96–0.98) | 0.000† |
| Sex | ||||||
| Male | 0.91 (0.64–1.28) | 0.573 | 0.77 (0.54–1.09) | 0.135 | 0.78 (0.59–1.05) | 0.104 |
| Female | Reference | Reference | Reference | |||
| Ethnicity | ||||||
| Kazakh | Reference | Reference | Reference | |||
| Russian | 0.34 (0.12–1.00) | 0.050† | 0.39 (0.19–0.79) | 0.009† | 0.40 (0.21–0.78) | 0.007† |
| Other | 0.65 (0.24–1.76) | 0.395 | 0.53 (0.29–0.98) | 0.043† | 0.62 (0.35–1.12) | 0.113 |
| Education | ||||||
| Vocational education or higher | Reference | Reference | Reference | |||
| High school or less | 1.42 (0.97–2.08) | 0.070 | 1.35 (0.96–1.90) | 0.088 | 1.26 (0.94–1.69) | 0.126 |
| Marital status | ||||||
| Married | Reference | Reference | Reference | |||
| Divorced/separated | 1.44 (0.82–2.51) | 0.203 | 1.04 (0.66–1.65) | 0.858 | 1.16 (0.77–1.74) | 0.478 |
| Single, never married | 2.81 (1.55–5.09) | 0.001† | 1.38 (0.95–2.02) | 0.095 | 1.80 (1.27–2.56) | 0.001† |
| Behavioural | ||||||
| Incarceration | ||||||
| Ever incarcerated | 1.74 (0.63–4.80) | 0.287 | 1.66 (0.57–4.88) | 0.357 | 1.72 (0.73–4.01) | 0.213 |
| Never incarcerated | Reference | Reference | Reference | |||
| Ever smoked tobacco | ||||||
| Yes | 1.45 (0.96–2.20) | 0.080 | 1.79 (1.20–2.68) | 0.004† | 1.73 (1.23–2.43) | 0.002† |
| No | Reference | Reference | Reference | |||
| Ever used non-smoking tobacco | ||||||
| Yes | 1.58 (0.80–3.12) | 0.187 | 1.47 (0.80–2.72) | 0.218 | 1.64 (0.96–2.79) | 0.068 |
| No | Reference | Reference | Reference | |||
| Ever drank alcohol | ||||||
| Yes | 1.50 (1.02–2.21) | 0.041† | 1.19 (0.82–1.71) | 0.357 | 1.41 (1.03–1.93) | 0.033† |
| No | Reference | Reference | Reference | |||
| Used opium | ||||||
| Yes | Removed from the model | 23.91 (0.75–761.05) | 0.072 | 30.98 (1.67–579.68) | 0.022† | |
| No | Reference | Reference | ||||
| Ever smoked heroin | ||||||
| Yes | Removed from the model | 0.04 (0.00–1.13) | 0.073 | 0.05 (0.00–1.25) | 0.068 | |
| No | Reference | Reference | ||||
| Ever used marijuana | ||||||
| Yes | 2.00 (0.72–5.58) | 0.184 | 1.25 (0.51–3.04) | 0.622 | 1.64 (0.76–3.54) | 0.210 |
| No | Reference | Reference | Reference | |||
| Ever injected drugs | ||||||
| Yes | Removed from the model | 0.10 (0.01–1.64) | 0.108 | 0.07 (0.01–0.86) | 0.038† | |
| No | Reference | Reference | ||||
| Comorbidity | ||||||
| HIV diagnosis‡ | ||||||
| Yes | Removed from the model | 18.83 (0.84–424.37) | 0.065 | 36.37 (2.05–646.13) | 0.014† | |
| No | Reference | Reference | ||||
| Diabetes diagnosis‡ | ||||||
| Yes | 19.72 (5.68–68.50) | 0.000† | 10.09 (3.98–25.58) | 0.000† | 13.96 (6.37–30.56) | 0.000† |
| No | Reference | Reference | Reference | |||
| χ2 = 142.96; P = 0.000 | χ2 = 97.63; P = 0.00 | 0 | χ2 = 188.79; P = 0.0 | 00 | ||
Model 1 compares TB cases to household controls; Model 2 compares TB cases to community controls; Model 3 compares TB cases to both household and community controls.
Statistically significant.
Ever diagnosed with disease.
TB = tuberculosis; aOR = adjusted odds ratio; CI = confidence interval; HIV = human immunodeficiency virus.
We compared differences between bacteriologically confirmed and non-bacteriologically confirmed TB cases. Bacteriologically confirmed cases were more likely to be younger, male, previously incarcerated, have ever smoked tobacco, have binge drunk in the past 90 days, have alcohol abuse problems, have ever used marijuana and have DM than non-bacteriologically confirmed cases (Appendix Table A.2).
We found few differences between overall analysis and subgroup analysis examining risk factors only among TB cases who were bacteriologically confirmed (Appendix Table A.3). In the subgroup analysis, in Model 1, having a high school education or less was significantly associated with TB. Marital status lost significance in the subgroup analysis. Incarceration was significantly associated with TB in Models 2 and 3. Ever smoked tobacco was significant across all three models in the subgroup analysis, and not just Models 2 and 3. Ever drank alcohol was non-significant in the subgroup analysis. HIV was also non-significant in Model 3.
Discussion
The findings of this study indicate that history of incarceration (in the subgroup analysis), tobacco use, alcohol use (in the original analysis), and having HIV or DM were associated with TB among a sample of the general population in Kazakhstan. Despite the implementation of DOTS in Kazakhstan, TB remains a significant public health problem in the country. To reduce the TB burden in the region, current factors that are driving the TB epidemic should be addressed. Our results lend support to the argument that smoking, alcohol use and DM are the new social determinants of TB, as opposed to past eras where crowded housing conditions and malnutrition were significant contributors.22,23
Few studies have examined DM and TB in Kazakhstan,7 but our study found that DM had a strong association with TB in this sample. Individuals with TB were 10–20 times as likely to have DM as individuals without TB. As DM continues to increase worldwide, particularly in developing countries with high rates of TB, the association between DM and TB should not be overlooked. Research has indicated that DM has an adverse effect on TB treatment outcomes.24 The treatment of TB in DM patients is often challenging. The pharmokinetics of TB medications are altered in DM patients, resulting in a slow response to anti-tuberculosis treatment.25 DM has a slow onset and may go unrecognised for years. Many TB patients in Kazakhstan may not be aware they have DM, as they are not regularly screened. Given the complications that can arise in treating TB among DM patients, it would be beneficial for TB clinics in Kazakhstan to screen newly diagnosed TB patients for DM.
Although there was a small number of HIV-positive individuals in this study, almost all were co-infected with TB. Integration of TB and HIV services in Kazakhstan is challenging due to difficulties in drug management, confidentiality issues and lack of trained staff. TB control programmes in the region should be aware of the particular challenges associated with HIV-TB coinfection and the need to help link patients to HIV care.
Our results also indicated significant associations between tobacco and alcohol use and TB. Reports in the literature indicate that tobacco use is a significant risk factor for TB,26,27 and the results of our study support those findings. However, smoking is not currently recognised as a risk factor for TB in Kazakhstan. Given the high rates of tobacco use in Kazakhstan,28,29 the integration of smoking cessation components into TB intervention and prevention programmes may be beneficial. Furthermore, the finding that higher frequencies of alcohol consumption were not significantly associated with TB, but that individuals who previously drank but did not currently drink were significantly more likely to have TB, is interesting. The reason for this association is unclear. It may be that some individuals did not report their current alcohol consumption truthfully, that some individuals stopped drinking while receiving TB treatment, or that individuals with previous drinking problems are at greater risk for TB. Further research is needed to examine links between previous alcohol users and TB infection.
Our study has several limitations. First, our findings are limited by the fact that the study was not designed to determine causal relationships between DM, HIV infection, incarceration history, substance use and TB. Second, the study was based on incident TB cases already detected and treated and was not a population-based study. Risk factors among detected TB cases may differ from those among undetected TB cases. Third, biological tests were not conducted among controls. We relied on self-reported diagnosis and TB clinic registries to classify individuals without TB; it is thus possible that some were misclassified. Fourth, because much of the data were self-reported, there may be some inaccuracies. For example, a large number (94.5% of cases and 72.4% of controls) reported receiving testing for HIV. Although TB cases are supposed to be tested for HIV according to the public health protocol in Kazakhstan, the reported HIV testing rate among controls is likely an overestimate. Over-reporting of HIV testing may be due to social desirability bias or a misunderstanding of the question. Finally, as our study had a small number of HIV-positive participants, HIV-related results should be interpreted with caution.
Conclusion
Our findings indicate that DM, HIV, tobacco use, alcohol use and history of incarceration were associated with TB. These findings have important implications for TB prevention and intervention programmes in Kazakhstan. TB treatment does not occur in a vacuum, and it can be significantly affected by patients' comorbidities. Screening and treatment for comorbidities such as DM and HIV are crucial for effective treatment of TB. TB clinics in Kazakhstan may need to integrate TB, HIV and DM testing and treatment services to reduce the TB epidemic. Furthermore, failing to properly diagnosis and treat TB among previously incarcerated individuals increases the risk of spreading TB among their families and community members. In addition, implementing smoking cessation or alcohol rehabilitation programmes into TB prevention and intervention programmes may provide some benefit to TB control in Kazakhstan. Achieving a successful reduction in TB in Kazakhstan will depend on the ability of TB control programmes to effectively address the new social determinants of TB.
Acknowledgments
The authors would like to thank the National TB Center, Almaty, and oblast TB dispensaries in Almaty City and in the Almaty, Kyzylorda, and Kostanay oblasts, the patients with TB and their families, as well as the other participants for their assistance with this study.
The study was funded by the Ministry of Education and Science, Astana, through the Center for Life Sciences, Nazarbayev University, Astana, Kazakhstan.
Table A.1. Factors associated with TB case status in the Almaty Region, Kazakhstan (TB cases = 562, household controls = 515, community controls = 523).
| Variable | Model 1* | Model 2* | Model 3* | |||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| OR (95%CI) | P value | OR (95%CI) | P value | OR (95%CI) | P value | |
| Sociodemographic | ||||||
| Age | 0.98 (0.97–0.99) | 0.000† | 0.99 (0.98–0.99) | 0.000† | 0.98 (0.97–0.98) | 0.000† |
| Sex | ||||||
| Male | 1.45 (1.22–1.73) | 0.000† | 1.26 (1.05–1.52) | 0.014† | 1.47 (1.23–1.74) | 0.000† |
| Female | Reference | Reference | Reference | |||
| Ethnicity | ||||||
| Kazakh | Reference | Reference | Reference | |||
| Russian | 1.01 (0.76–1.32) | 0.973 | 0.89 (0.68–1.16) | 0.388 | 0.93 (0.71–1.21) | 0.583 |
| Other | 0.98 (0.70–1.36) | 0.896 | 0.86 (0.63–1.17) | 0.332 | 0.89 (0.65–1.22) | 0.461 |
| Education | ||||||
| Vocational education or higher | Reference | Reference | Reference | |||
| High school or less | 1.06 (0.88–1.29) | 0.525 | 1.13 (0.94–1.37) | 0.200 | 1.13 (0.94–1.35) | 0.207 |
| Marital status | ||||||
| Married | Reference | Reference | Reference | |||
| Divorced/separated | 1.00 (0.74–1.35) | 0.977 | 0.91 (0.67–1.22) | 0.513 | 0.94 (0.71–1.25) | 0.673 |
| Single, never married | 1.89 (1.52–2.35) | 0.000† | 1.29 (1.05–1.59) | 0.018† | 1.78 (1.45–2.19) | 0.000† |
| Behavioural | ||||||
| Incarceration | ||||||
| Ever incarcerated | 1.66 (0.99–2.77) | 0.055 | 1.51 (0.91–2.50) | 0.110 | 1.87 (1.14–3.06) | 0.013† |
| Never incarcerated | Reference | Reference | Reference | |||
| Time incarcerated in the past 90 days | 1.15 (0.67–1.97) | 0.610 | 1.15 (0.67–1.97) | 0.610 | 1.19 (0.65–2.18) | 0.582 |
| Ever smoked tobacco | ||||||
| Yes | 1.45 (1.21–1.75) | 0.000† | 1.35 (1.12–1.63) | 0.002† | 1.54 (1.29–1.84) | 0.000† |
| No | Reference | Reference | Reference | |||
| Currently smoke tobacco | ||||||
| Yes | 12.33 (3.80–40.00) | 0.000† | 6.00 (2.53–14.24) | 0.000† | 8.17 (3.95–16.90) | 0.000† |
| No | Reference | Reference | Reference | |||
| Cigarettes smoked in the past week | 1.00 (1.00–1.01) | 0.355 | 1.00 (1.00–1.00) | 0.647 | 1.00 (1.00–1.00) | 0.706 |
| Ever used non-smoking tobacco | ||||||
| Yes | 1.62 (1.18–2.23) | 0.003† | 1.43 (1.04–1.97) | 0.028† | 1.78 (1.30–2.43) | 0.000† |
| No | Reference | Reference | Reference | |||
| Currently use non-smoking tobacco (sample too small, not significant) | ||||||
| Yes | 1.75 (0.91–3.35) | 0.093 | 1.60 (0.83–3.06) | 0.158 | 1.99 (1.05–3.75) | 0.034† |
| No | Reference | Reference | Reference | |||
| Number of times used non-smoking tobacco in the last week | 1.04 (1.00–1.09) | 0.087 | 1.03 (0.99–1.07) | 0.174 | 1.03 (1.00–1.06) | 0.085 |
| Ever drank alcohol | ||||||
| Yes | 1.41 (1.17–1.71) | 0.000† | 1.25 (1.03–1.51) | 0.025† | 1.44 (1.19–1.74) | 0.000† |
| No | Reference | Reference | Reference | |||
| Binge drank alcohol in the past 90 days | ||||||
| Yes | 1.15 (0.81–1.63) | 0.427 | 0.72 (0.52–1.01) | 0.057 | 0.87 (0.62–1.21) | 0.394 |
| No | Reference | Reference | Reference | |||
| Frequency of alcohol consumption | ||||||
| Never drank alcohol | Reference | Reference | Reference | |||
| Monthly or less | 1.28 (0.88–1.84) | 0.194 | 0.95 (0.66–1.38) | 0.801 | 1.12 (0.82–1.54) | 0.469 |
| 2–4 times a month | 2.07 (1.08–3.97) | 0.029† | 0.75 (0.45–1.25) | 0.264 | 1.17 (0.74–1.85) | 0.498 |
| 2–3 times a week | 3.01 (0.52–17.45) | 0.219 | 1.31 (0.34–5.03) | 0.699 | 1.92 (0.55–6.66) | 0.307 |
| ≥4 times a week | 0.61 (0.11–3.37) | 0.566 | 2.24 (0.34–14.65) | 0.399 | 1.27 (0.30–5.35) | 0.743 |
| Does not currently drink | 3.64 (2.43–5.47) | 0.000† | 2.93 (1.95–4.41) | 0.000† | 3.43 (2.45–4.80) | 0.000† |
| Alcohol abuse‡ | ||||||
| Yes | 1.21 (0.90–1.64) | 0.209 | 1.05 (0.78–1.41) | 0.769 | 1.16 (0.87–1.56) | 0.317 |
| No | Reference | Reference | Reference | |||
| Used opium | ||||||
| Yes | 1.66 (0.71–3.85) | 0.240 | 1.65 (0.70–3.88) | 0.252 | 2.04 (0.89–4.70) | 0.092 |
| No | Reference | Reference | Reference | |||
| Ever smoked heroin | ||||||
| Yes | 1.00 (0.12–8.34) | 1.000 | 0.63 (0.08–4.95) | 0.663 | 0.71 (0.09–5.44) | 0.745 |
| No | Reference | Reference | Reference | |||
| Ever injected heroin | ||||||
| Yes | 1.51 (0.56–4.04) | 0.415 | 1.23 (0.47–3.22) | 0.679 | 1.53 (0.59–3.99) | 0.383 |
| No | Reference | Reference | Reference | |||
| Ever used marijuana | ||||||
| Yes | 1.69 (1.08–2.65) | 0.021† | 1.45 (0.94–2.25) | 0.095 | 1.86 (1.21–2.85) | 0.005† |
| No | Reference | Reference | Reference | |||
| Used marijuana in the past 90 days | ||||||
| Yes | 1.54 (0.70–3.36) | 0.284 | 1.98 (0.88–4.43) | 0.097 | 2.18 (1.00–4.73) | 0.049† |
| No | Reference | Reference | Reference | |||
| Ever injected drugs | ||||||
| Yes | 0.66 (0.26–1.68) | 0.385 | 0.97 (0.37–2.54) | 0.944 | 0.75 (0.30–1.88) | 0.542 |
| No | Reference | Reference | Reference | |||
| Comorbidity | ||||||
| HIV diagnosis§ | ||||||
| Yes | 2.67 (1.03–6.91) | 0.043† | 2.07 (0.84–5.11) | 0.116 | 3.38 (1.37–8.32) | 0.008† |
| No | Reference | Reference | Reference | |||
| Diabetes diagnosis§ | ||||||
| Yes | 2.12 (1.46–3.07) | 0.000† | 1.94 (1.34–2.82) | 0.001 † | 2.81 (1.95–4.06) | 0.000† |
| No | Reference | Reference | Reference | |||
Model 1 compares TB cases to household controls; Model 2 compares TB cases to community controls; Model 3 compares TB cases to both household and community controls.
Statistically significant.
CAGE score ≥ 2.
Ever diagnosed with disease.
TB=tuberculosis; OR=odds ratio; CI=confidence interval; HIV=human immunodeficiency virus; CAGE=(Have you ever felt you needed to Cut down on your drinking? Have people Annoyed you by criticizing your drinking? Have you ever felt Guilty about drinking? Have you ever felt you needed a drink first thing in the morning [Eye-opener] to steady your nerves or to get rid of a hangover?).
Table A.2. Comparison of risk factors between individuals with bacteriologically confirmed TB and those with non-bacteriologically confirmed TB.
| Variable | Bacteriologically confirmed TB cases (n = 201) n (%) | Non-bacteriologically confirmed TB cases (n = 357) n (%) | P value |
|---|---|---|---|
| Sociodemographic | |||
| Age, years, mean ± SD | 36.33 ± 13.28 | 41.73 ± 13.43 | 0.000* |
| Sex | |||
| Male | 127 (63.2) | 179 (50.1) | 0.003* |
| Female | 74 (36.8) | 178 (49.9) | |
| Ethnicity | |||
| Kazakh | 143 (71.1) | 286 (80.1) | 0.040* |
| Russian | 33 (16.4) | 45 (12.6) | |
| Other | 25 (12.4) | 26 (7.3) | |
| Education | |||
| Vocational education or higher | 127 (63.2) | 219 (61.3) | 0.667 |
| High school or less | 74 (36.8) | 138 (38.7) | |
| Marital status | |||
| Married | 121 (60.2) | 223 (62.5) | 0.362 |
| Divorced/separated | 27 (13.4) | 34 (9.5) | |
| Single, never married | 53 (26.4) | 100 (28.0) | |
| Behavioural | |||
| Incarceration | |||
| Ever incarcerated | 12 (6.0) | 8 (2.2) | 0.023* |
| Never incarcerated | 189 (94.0) | 349 (97.8) | |
| Time incarcerated in the past 90 days, days, mean ± SD | 0.04 ± 0.64 | 0.00 ± 0.00 | 0.319 |
| Ever smoked tobacco | |||
| Yes | 111 (55.2) | 137 (38.4) | 0.000* |
| No | 90 (44.8) | 220 (61.6) | |
| Currently smoke tobacco | |||
| Yes | 40 (19.9) | 51 (14.3) | 0.085 |
| No | 161 (80.1) | 306 (85.7) | |
| Number of cigarettes smoked in the past week, mean ± SD | 17.48 ± 44.04 | 11.07 ± 35.30 | 0.066 |
| Ever used non-smoking tobacco | |||
| Yes | 23 (11.4) | 28 (7.8) | 0.157 |
| No | 178 (88.6) | 329 (92.2) | |
| Currently use non-smoking tobacco | |||
| Yes | 6 (3.0) | 6 (1.7) | 0.308 |
| No | 195 (97.0) | 351 (98.3) | |
| Number of times used non-smoking tobacco in the last week | 0.71 (4.77) | 0.16 (2.17) | 0.120 |
| Ever drank alcohol | |||
| Yes | 109 (54.2) | 168 (47.1) | 0.104 |
| No | 92 (45.8) | 189 (52.9) | |
| Binge drank in the past 90 days | |||
| Yes | 22 (10.9) | 20 (5.6) | 0.022* |
| No | 179 (89.1) | 337 (94.4) | |
| Frequency of alcohol consumption | 0.332 | ||
| Never drank alcohol | 92 (45.8) | 189 (52.9) | |
| Monthly or less | 42 (20.9) | 63 (17.6) | |
| 2–4 times a month | 17 (8.5) | 19 (5.3) | |
| 2–3 times a week | 3 (1.5) | 3 (0.8) | |
| ≥4 times a week | 2 (1.0) | 1 (0.3) | |
| Does not currently drink | 45 (22.4) | 82 (23.0) | |
| Alcohol abuse† | |||
| Yes | 31 (15.4) | 24 (6.7) | 0.001* |
| No | 170 (84.6) | 333 (93.3) | |
| Used opium | |||
| Yes | 2 (1.0) | 4 (1.1) | 0.890 |
| No | 199 (99.0) | 353 (98.9) | |
| Ever smoked heroin | |||
| Yes | 1 (0.5) | 0 (0.0) | 0.360 |
| No | 200 (99.5) | 357 (100.0) | |
| Ever injected heroin | |||
| Yes | 1 (0.5) | 3 (0.8) | 1.000 |
| No | 200 (99.5) | 354 (99.2) | |
| Ever used marijuana | |||
| Yes | 15 (7.5) | 10 (2.8) | 0.011* |
| No | 186 (92.5) | 347 (97.2) | |
| Used marijuana in the past 90 days | |||
| Yes | 3 (1.5) | 4 (1.1) | 0.707 |
| No | 198 (98.5) | 353 (98.9) | |
| Ever injected drugs | |||
| Yes | 1 (0.5) | 3 (0.8) | 1.000 |
| No | 200 (99.5) | 354 (99.2) | |
| Concomitant diseases | |||
| HIV diagnosis‡ | |||
| Yes | 4 (2.0) | 3 (0.8) | 0.259 |
| No | 197 (98.0) | 354 (99.2) | |
| Diabetes diagnosis‡ | |||
| Yes | 26 (12.9) | 14 (3.9) | 0.000* |
| No | 175 (87.1) | 343 (96.1) | |
Statistically significant.
CAGE score ≥ 2.
Ever diagnosed with disease.
TB = tuberculosis; SD = standard deviation; HIV = human immunodeficiency virus; CAGE = (Have you ever felt you needed to Cut down on your drinking? Have people Annoyed you by criticizing your drinking? Have you ever felt Guilty about drinking? Have you ever felt you needed a drink first thing in the morning [Eye-opener] to steady your nerves or to get rid of a hangover?).
Table A.3. Subgroup analysis: factors associated with bacteriologically confirmed tuberculosis case status in Almaty Region, Kazakhstan.
| Model 1* | Model 2* | Model 3* | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| aOR (95%CI) | P value | aOR (95%CI) | P value | aOR (95%CI) | P value | |
| Sociodemographic | ||||||
| Age | 0.95 (0.92–0.99) | 0.004† | 0.97 (0.94–0.99) | 0.012† | 0.96 (0.94–0.99) | 0.001† |
| Sex | ||||||
| Male | 1.30 (0.64–2.65) | 0.469 | 0.76 (0.41–1.39) | 0.368 | 0.90 (0.53–1.53) | 0.691 |
| Female | Reference | Reference | Reference | |||
| Ethnicity | ||||||
| Kazakh | Reference | Reference | Reference | |||
| Russian | 0.11 (0.10–1.23) | 0.073† | 0.12 (0.03–0.50) | 0.004† | 0.17 (0.05–0.61) | 0.006† |
| Other | 0.12 (0.01–1.60) | 0.109 | 0.83 (0.30–2.31) | 0.719 | 0.64 (0.24–1.73) | 0.376 |
| Education | ||||||
| Vocational education or higher | Reference | Reference | Reference | |||
| High school or less | 2.99 (1.39–6.42) | 0.005† | 1.26 (0.66–2.38) | 0.483 | 1.51 (0.88–2.59) | 0.135 |
| Marital status | ||||||
| Married | Reference | Reference | Reference | |||
| Divorced/separated | 2.21 (0.73-6.65) | 0.160 | 1.02 (0.43–2.41) | 0.972 | 1.47 (0.71–3.04) | 0.297 |
| Single, never married | 2.03 (0.74-5.62) | 0.172 | 0.95 (0.46–1.93) | 0.882 | 1.32 (0.71–2.44) | 0.377 |
| Behavioural | ||||||
| Incarceration | ||||||
| Ever incarcerated | 2.13 (0.41–11.13) | 0.373 | 6.96 (1.03–46.81) | 0.046† | 4.38 (1.07–17.98) | 0.041† |
| Never incarcerated | Reference | Reference | Reference | |||
| Ever smoked tobacco | ||||||
| Yes | 2.55 (1.06–6.12) | 0.036† | 3.22 (1.53–6.80) | 0.002† | 2.75 (1.49–5.09) | 0.001† |
| No | Reference | Reference | Reference | |||
| Ever used non-smoking tobacco | ||||||
| Yes | 1.69 (0.45–6.36) | 0.438 | 2.49 (0.74–8.43) | 0.141 | 1.96 (0.76–5.10) | 0.166 |
| No | Reference | Reference | Reference | |||
| Ever drank alcohol | ||||||
| Yes | 0.75 (0.34–1.62) | 0.457 | 0.70 (0.36–1.38) | 0.304 | 0.90 (0.52–1.57) | 0.709 |
| No | Reference | Reference | Reference | |||
| Used opium | ||||||
| Yes | Removed from the model | 2.04 (0.02–187.93) | 0.757 | 8.43 (0.26–278.74) | 0.232 | |
| No | Reference | Reference | ||||
| Ever smoked heroin | ||||||
| Yes | Removed from the model | 0.14 (0.00–12.80) | 0.398 | 0.11 (0.00–3.69) | 0.215 | |
| No | Reference | Reference | ||||
| Ever used marijuana | ||||||
| Yes | 2.82 (0.48–16.73) | 0.253 | 0.87 (0.24–3.13) | 0.830 | 1.60 (0.55–4.67) | 0.391 |
| No | Reference | Reference | Reference | |||
| Ever injected drugs | ||||||
| Yes | Removed from the model | 0.05 (0.00–92.29) | 0.437 | 0.06 (0.00–5.12) | 0.218 | |
| No | Reference | Reference | ||||
| Comorbidity | ||||||
| HIV diagnosis‡ | ||||||
| Yes | Removed from the model | 8.48 (0.44–162.05) | 0.156 | 13.23 (0.94–186.05) | 0.056 | |
| No | Reference | Reference | ||||
| Diabetes diagnosis‡ | ||||||
| Yes | 53.95 (6.13–474.81) | 0.000† | 27.60 (4.92–154.79) | 0.000† | 33.05 (8.26–132.14) | 0.000† |
| No | Reference | Reference | Reference | |||
| χ2 = 71.45; P = 0.000 | χ2 = 57.34; P = 0.000 | χ2 = 98.84; P = 0.000 | ||||
Model 1 compares TB cases to household controls; Model 2 compares TB cases to community controls; Model 3 compares TB cases to both household and community controls.
Statistically significant.
Ever diagnosed with disease.
aOR= adjusted odds ratio; CI = confidence interval; HIV = human immunodeficiency virus.
Footnotes
The appendix is available in the online version of this article, at http://www.ingentaconnect.com/content/iuatld/ijtld/2017/00000021/00000001/art00016
Conflicts of interest: none declared.
References
- 1.Rios M, Monleon-Getino T. A graphical study of tuberculosis incidence and trends in the WHO's European region (1980– 2006) Eur J Epidemiol. 2009;24:381–387. doi: 10.1007/s10654-009-9347-6. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization. Kazakhstan Tuberculosis Profile 2014. Geneva, Switzerland: WHO; 2014. [Accessed October 2016]. https://extranet.who.int/sree/Reports?op=Replet&name=%2FWHO_HQ_Reports%2FG2%2FPROD%2FEXT%2FTBCountryProfile&ISO2=KZ&LAN=EN&outtype=html. [Google Scholar]
- 3.Coker R, McKee M, Atun R, et al. Risk factors for pulmonary tuberculosis in Russia: case-control study. BMJ. 2006;332:85–87. doi: 10.1136/bmj.38684.687940.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.de Alencar Ximenes R, de Albuquerque M, Souza W, Montarroyos U, et al. Is it better to be rich in a poor area or poor in a rich area? A multilevel analysis of a case-control study of social determinants of tuberculosis. Int J Epidemiol. 2009;38:1285–1296. doi: 10.1093/ije/dyp224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dye C, Lönnroth K, Jaramillo E, Williams B, Raviglione M. Trends in tuberculosis incidence and their determinants in 134 countries. Bull World Health Organ. 2009;87:683–691. doi: 10.2471/BLT.08.058453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Goldhaber-Fiebert J, Jeon C, Cohen T, Murray M. Diabetes mellitus and tuberculosis in countries with high tuberculosis burdens: individual risks and social determinants. Int J Epidemiol. 2011;40:417–428. doi: 10.1093/ije/dyq238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Terlikbayeva A, Hermosilla S, Galea S, et al. Tuberculosis in Kazakhstan: analysis of risk determinants in national surveillance data. BMC Infect Dis. 2012;12:262. doi: 10.1186/1471-2334-12-262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hermosilla S, El-Bassel N, Aifah A, et al. Tuberculosis report among injection drug users and their partners in Kazakhstan. Public Health. 2015;129:569–575. doi: 10.1016/j.puhe.2015.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stuckler D, Basu S, McKee M, King L. Mass incarceration can explain population increases in TB and multidrug-resistant TB in European and central Asian countries. Proc Natl Acad Sci USA. 2008;105:13280–13285. doi: 10.1073/pnas.0801200105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dooley K, Chaisson R. Tuberculosis and diabetes mellitus: convergence of two epidemics. Lancet Infect Dis. 2009;9:737–746. doi: 10.1016/S1473-3099(09)70282-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lodi S, del Amo J, d'Arminio Monforte A, et al. Risk of tuberculosis following HIV seroconversion in high-income countries. Thorax. 2013;68:207–213. doi: 10.1136/thoraxjnl-2012-201740. [DOI] [PubMed] [Google Scholar]
- 12.Joint United Nations Programme on HIV and AIDS. Kazakhstan: HIV and AIDS estimates. Geneva, Switzerland: UNAIDS; 2014. [Google Scholar]
- 13.International Diabetes Federation. Diabetes in Kazakhstan: 2015. Brussels, Belgium: IDF; 2015. [Google Scholar]
- 14.Roberts B, Gilmore A, Stickley A, et al. Changes in smoking prevalence in 8 countries of the former Soviet Union between 2001 and 2010. Am J Public Health. 2012;102:1320–1328. doi: 10.2105/AJPH.2011.300547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Leung C, Yew W, Chan C, et al. Smoking adversely affects treatment response, outcome and relapse in tuberculosis. Eur Respir J. 2015;45:738–745. doi: 10.1183/09031936.00114214. [DOI] [PubMed] [Google Scholar]
- 16.Gegia M, Magee M, Kempker R, et al. Tobacco smoking and tuberculosis treatment outcomes: a prospective cohort study in Georgia. Bull World Health Organ. 2015;93:390–399. doi: 10.2471/BLT.14.147439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.World Bank. Model Living Standards Measurement Study survey questionnaire for the countries of the former Soviet Union. Washington DC, USA: World Bank; 1996. [Google Scholar]
- 18.Ewing J. Detecting alcoholism: the CAGE questionaire. JAMA. 1984;252:1905–1907. doi: 10.1001/jama.252.14.1905. [DOI] [PubMed] [Google Scholar]
- 19.World Health Organization. Global adult tobacco survey. Geneva, Switzerland: WHO; 2007. [Google Scholar]
- 20.United States Agency for International Development. Demographic health survey. Washington DC, USA: USAID; 2012. [Google Scholar]
- 21.World Health Organization. World Health Survey. Geneva, Switzerland: WHO; 2002. [Google Scholar]
- 22.Lönnroth K, Jaramillo E, Williams B, Dye C, Raviglione M. Drivers of tuberculosis epidemics: the role of risk factors and social determinants. Soc Sci Med. 2009;68:2240–2246. doi: 10.1016/j.socscimed.2009.03.041. [DOI] [PubMed] [Google Scholar]
- 23.Aparicio J, Capurro A, Castillo-Chavez C. Markers of disease evolution: the case of tuberculosis. J Theor Biol. 2002;215:227–237. doi: 10.1006/jtbi.2001.2489. [DOI] [PubMed] [Google Scholar]
- 24.Jimenez-Corona M, Cruz-Hervert L, Garcia-Garcia L, et al. Association of diabetes and tuberculosis: impact on treatment and post-treatment outcomes. Thorax. 2013;68:214–220. doi: 10.1136/thoraxjnl-2012-201756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Skowronski M, Zozulinska-Ziolkiewicz D, Barinow-Wojewodzki A. Tuberculosis and diabetes mellitus: an underappreciated association. Arch Med Sci. 2014;10:1019–1027. doi: 10.5114/aoms.2014.46220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pai M, Mohan A, Dheda K, et al. Lethal interaction: the colliding epidemics of tobacco and tuberculosis. Expert Rev Anti Infect Ther. 2007;5:385–391. doi: 10.1586/14787210.5.3.385. [DOI] [PubMed] [Google Scholar]
- 27.Chan E, Kinney W, Honda J, et al. Tobacco exposure and susceptibility to tuberculosis: Is there a smoking gun? Tuberculosis. 2014;94:544–550. doi: 10.1016/j.tube.2014.08.010. [DOI] [PubMed] [Google Scholar]
- 28.World Health Organization. WHO report on the global tobacco epidemic, 2011: warning about the dangers of tobacco. Geneva, Switzerland: WHO; 2011. [Google Scholar]
- 29.Ezzati M, Lopez A. Measuring the accumulated hazards of smoking: global and regional estimates for 2000. Tobacco Control. 2003;12:79–85. doi: 10.1136/tc.12.1.79. [DOI] [PMC free article] [PubMed] [Google Scholar]