Abstract
Background and Aims:
The objective of the study was to determine the incidence of failed extubations in our Intensive Care Unit (ICU) and identify associated clinical factors.
Materials and Methods:
A prospective observational study of mechanically ventilated patients who underwent extubation attempts in our (predominantly surgical) ICU was undertaken from July 2012 to August 2013. The primary endpoint was the need for nonelective reintubation within 72 h of extubation. Clinical data of the reintubated patients were compared with those who were successfully extubated to identify factors associated with reintubation.
Results:
Five hundred and eight extubation attempts were documented, 38 (7.5%) of which were unsuccessful. On multivariate analysis, the following clinical factors were found to be associated with an increased risk of failed extubation: unplanned extubations (adjusted odds ratio [OR] 5.8), the use of noninvasive ventilation (NIV) postextubation (adjusted OR 3.2), and sepsis (adjusted OR 2.9). Patient demographic factors, other premorbid and comorbid medical conditions, and differences of laboratory parameters did not appear to significantly influence reintubation rates in our study.
Conclusions:
Our study has demonstrated a relatively low reintubation rate, likely due to inclusion of elective admissions/intubations in our patient population. Unplanned extubations, the use of NIV postextubation, and sepsis were associated with increased reintubation risk, reinforcing the need for increased vigilance in this subgroup of patients after extubation.
Keywords: Extubation failure, mechanical ventilation, risk factors
INTRODUCTION
The use of mechanical ventilation in the critically ill patient has long been regarded as a double-edged sword; while essential and life sustaining, the complications associated with unnecessarily prolonged endotracheal intubation are legion and include airway injury, ventilator-induced lung injury, ventilator-associated pneumonia, and the general complications associated with immobility. However, the decision to extubate cannot be taken lightly, as premature liberation from mechanical ventilation in the unprepared patient will result in extubation failure and reintubation, an outcome known to be independently associated with prolonged Intensive Care Unit (ICU) stays, and increased rates of morbidity and mortality.
The reluctant acceptance of a certain degree of extubation failure in the ICU as not only inevitable but also desirable (as reflecting the optimal risk balance between the respective morbidities of extubation failure and prolonged ventilation) is a less than ideal state of affairs and is indicative of the inability of the intensivist to perfectly predict extubation failure. While numerous studies have been performed in an attempt to determine an optimal rate of reintubation failure rate and characterize risk factors associated with extubation failure, none of the predictive tests or models have proven ideal to date. Part of the reason for this likely lies with the inability of one or a few test parameters to sufficiently describe the patient's overall physiological state with regard to the need for continued airway and ventilatory support. Added to this are the challenges from the great heterogeneity of the critically ill population, with each individual center studied differing profoundly in patient profile, case mix, illness severity and extubation criteria, and practices, affecting the applicability of predictive strategies based on one subgroup of critically ill patients onto another.
Against this backdrop, our current study was performed with the aim of benchmarking our extubation failure rate against international norms, identifying associations with extubation failure in our own local ICU population, and contributing to the growing body of data available in the literature regarding this topic.[1]
MATERIALS AND METHODS
Our ICU serves as a general adult (>16 years old) surgical ICU while also functioning as an overflow unit for medical patients requiring intensive care when the medical ICU is at full occupancy. Coronary care, cardiac, thoracic, and vascular surgical patients are not included in our patient population.
Over the period of July 2012–August 2013, data were collected at the time of extubation by intensive care residents and respiratory therapists and supplemented by chart review for a total of 508 extubations. Patients who underwent a tracheostomy before any extubation attempts, who died before extubation, or who underwent a terminal extubation (with no plans for reintubation should this prove necessary) were not included in the data collection and analysis, as were patients who were reintubated electively (e.g., for procedures or surgery) within the 72 h period following extubation.
All patients were ventilated on the Puritan Bennett™ 840 Ventilator (Covidien, Dublin, Republic of Ireland). Sedation was titrated according to the Richmond Agitation-Sedation Scale aiming for a score of 0 (alert) to − 2 (light sedation), with continuous active reviews by staff for suitability to wean or cease sedation as indicated and tolerated. Apart from the patients who inadvertently self-extubated (whose extubations were also included in the data collection), all patients underwent spontaneous breathing trials (SBTs) on low levels of pressure support ventilation (pressure support levels ranging from +5 to +10 cm H2O, Positive end-expiratory pressure [PEEP] 4–5 cm H2O) before extubation, and following a successful trial were extubated.
Data collected included demographic factors (age, gender, ethnicity, weight, and admitting discipline), circumstances surrounding the intubation (location of intubation, whether any surgery had been performed on the patient preceding ICU admission, and indication for intubation), and extubation (duration of prior mechanical ventilation, planned vs. unplanned extubation, and use of noninvasive ventilation [NIV] after extubation). Data were also collected regarding selected premorbid conditions before intubation (ischemic heart disease, congestive cardiac failure, smoking status, asthma, and chronic obstructive pulmonary disease), as well as information on active conditions managed during the ICU stay (e.g., shock, myocardial infarction or troponin rise, sepsis, and pneumonia) and selected laboratory parameters at the time of extubation (hemoglobin and albumin).
The primary outcome was the result of the extubation (pass vs. fail). Failed extubation was defined as unplanned reintubation within 72 h of extubation. In the patients requiring reintubation, the reason for reintubation was recorded.
Data analysis was performed on SPSS software version 22 (IBM SPSS Statistics for Windows, Version 22.0. IBM Corp, Armonk, NY. Released 2013). All statistical tests were performed using two-sided tests. Univariate analysis of categorical variables was performed using Fisher's exact test and Pearson's Chi-squared test, while continuous variables were analyzed using Mann–Whitney U-test (for nonparametric data), with the level of statistical significance set at P < 0.05. Subsequently, all univariate variables with a P < 0.1 were evaluated using a bivariate correlation matrix for multicollinearity and then included in multivariable logistic regression analysis, with those having a P < 0.05 retained as factors associated with reintubation risk in our study. Local Ethics Board approval was obtained before commencement of the study.
RESULTS
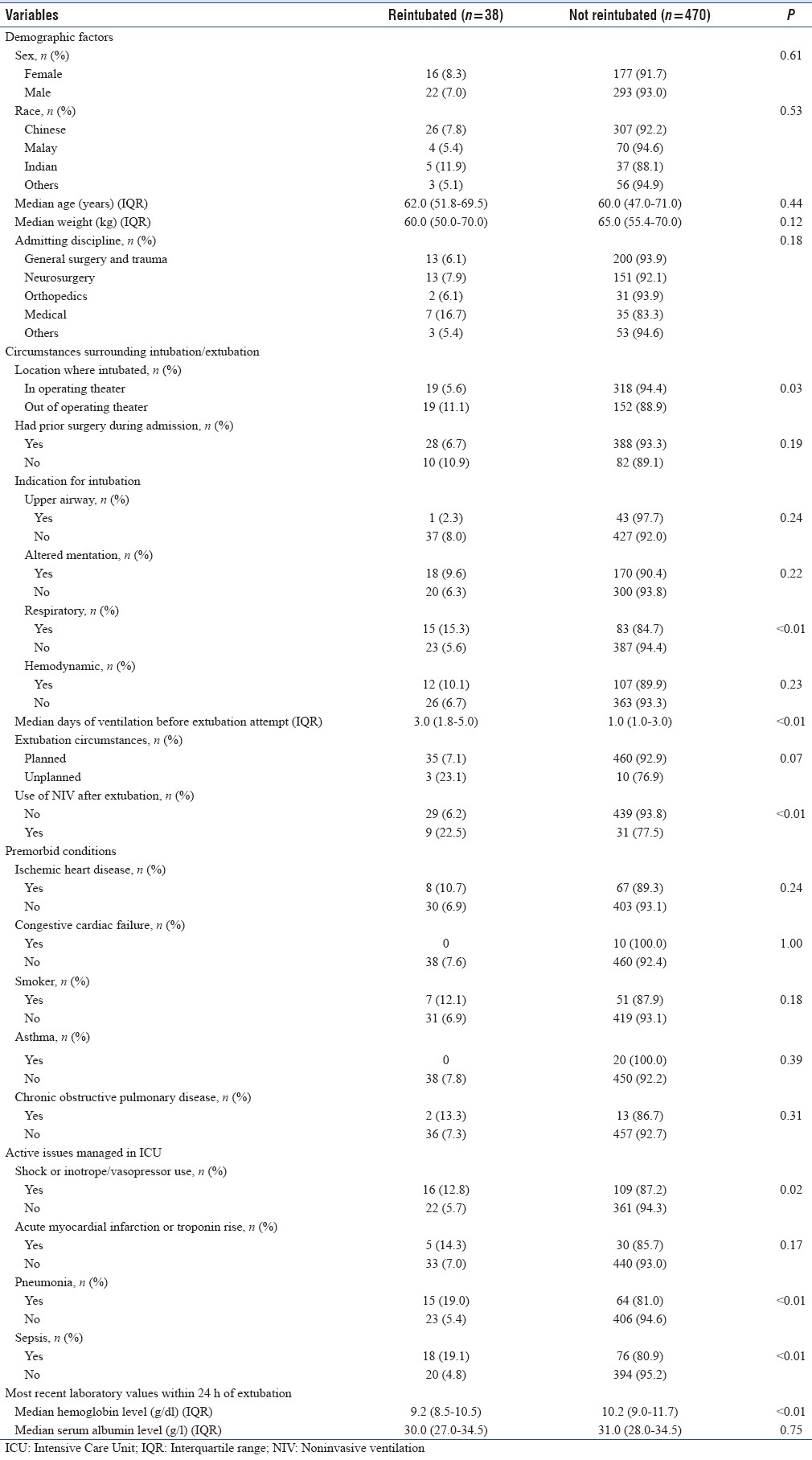
Five hundred and eight extubations were included under our study criteria, 13 of which were unplanned. The median age of the patients undergoing extubation was 60.0 (interquartile range [IQR] 47.0, 71.0) years old, and the median weight was 64.5 (IQR 55.0, 70.0) kg. The population was 62.0% male (n = 315) and had the following ethnic distribution: 65.6% (n = 333) Chinese, 14.6% (n = 74) Malay, 8.3% (n = 42) Indian, and 11.6% (n = 59) others. The majority of the patients were admitted under the general surgery and trauma service (41.9%, n = 213) and neurosurgical service (32.3%, n = 164) [Table 1 – Full breakdown by service]. The most common indications for initial intubation (or for not extubating patients at the end of the case in situations where the patient is intubated in the operating room for surgery and transferred to the unit intubated) were neurological reasons (37.0%, n = 188), hemodynamic reasons (23.4%, n = 119), and respiratory reasons (19.3%, n = 98).
Table 1.
Potential factors analyzed for association with reintubation
After extubation, 470 patients (92.5%) remained successfully extubated, whereas 38 patients (7.5%) required nonelective reintubation within 72 h.
Univariate analysis comparing the failed and successful extubation groups [Table 1] showed that the following factors were found to be associated with a higher risk of reintubation (P < 0.05): A longer duration of mechanical ventilation before extubation (3.0 vs. 1.0 days), initial intubation for respiratory reasons, initial intubation outside of the operating room setting, unplanned extubation, and the use of NIV after extubation. The patients who failed extubation were also more likely to have had shock/inotrope/vasopressor use, pneumonia, and/or sepsis during their ICU stay. Those who failed extubation also had lower hemoglobin levels (9.2 vs. 10.2 g/dl) at the time of extubation.
There were no statistically significant differences in demographic factors such as age, gender, or weight in the two groups. There was also no difference between both groups in the prevalence of the premorbid conditions studied.
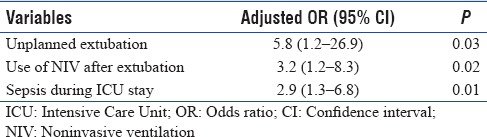
After multivariable logistic regression analysis, unplanned extubations, the use of NIV, and sepsis during the intensive care admission remained as factors which were associated with increased risk of failed extubation [Table 2].
Table 2.
Significant risk factors for extubation failure following multivariate analysis
DISCUSSION
The high costs of extubation failure (independently increased length of stay, morbidity and mortality among other things) have been well described, as has the price of delayed extubation in terms of increased ventilator-associated complications, along with the more insidious problems associated with prolonged recumbency and immobility.[2,3] Nonetheless, the search for accurate predictors of extubation success and failure has remained one of the more difficult areas in critical care medicine over the past few decades.
In a recent review article, Kulkarni and Agarwal suggested the categorization of predictors of extubation failure into demographic factors, parameters assessing respiratory mechanics, airway patency and protection, and cardiovascular reserve.[4] With regard to respiratory mechanics, many of the predictive tests used in isolation have demonstrated at best a moderate ability to accurately distinguish extubation failures from successes, owing to the limited information provided by assessing only a small aspect of the patient's overall physiological status at a single time point. For instance, one of the more extensively studied tests, the rapid shallow breathing index (taken as the respiratory rate/min divided by the tidal volume in L) when used as a predictor of success of weaning from mechanical ventilation was found in one meta-analysis to show sensitivities ranging from 65% to 96% and specificities ranging from 0% to 73% at a cutoff of 100–105 breaths/min/L, an accuracy regarded by the authors as modest.[5] Cognizant of the problems with the use of single indices at single time points, investigators have made attempts to improve on predictive power by trending multiple predictors over time; an approach that has yielded improved results but has yet to be validated prospectively.[6] While assessment of respiratory mechanics was found to correlate better with the outcomes of an SBT, they have fared less well with regard to predicting overall extubation failure, suggesting that a more holistic assessment of both respiratory and nonrespiratory factors integrated with analysis of clinical risk factors might better predict overall outcomes.[4,7]
To this end, Mokhlesi et al. were able to demonstrate the predictive value of endotracheal secretions, Glasgow coma scale, and pre-extubation hypercapnia in predicting extubation failure after a successful SBT, achieving an area under the curve of the receiver operator characteristic curve of 0.87.[8] A more recent attempt along those lines was a study by Miu et al., who were able to demonstrate 70% accuracy in predicting extubation failure using the combination of Simplified Acute Physiology Score II, suctioning frequency, number of prior SBTs, diastolic blood pressure, minute ventilation during SBT, and oxygen saturation as predictive factors.[9] Where generation of predictive models is concerned, a significant error rate still remains despite these efforts, and a key issues the retrospective nature of these and other studies and the general absence of prospective validation in both similar and materially different patient populations, precluding wider application in other critical care settings. The heterogeneous nature of the critical care population also adds a significant layer of difficulty to these efforts, with potentially differing relative importances of various factors in different patient subgroups, contributing to inconsistent results across clinical studies. For instance, authors of a systematic review of predictors of extubation failure in neurocritical care patients concluded that traditional weaning parameters including the rapid shallow breathing index and minute ventilation performed poorly in this specific patient subgroup.[10]
With these limitations in mind, our study was a prospective observational one of a single multidisciplinary (but predominantly general surgical and neurosurgical) ICU of adult patients which focused on delineating clinical and demographic associations with extubation failure in our own local ICU population to enable benchmarking and comparison with other published literature. The primary outcome measure was the overall reintubation rate, which was found to be 7.5% within 72 h.
This figure lay within the 5%–10% range somewhat arbitrarily and reluctantly proposed by Krinsley et al. as representing an optimal balance between the risks of unnecessarily prolonged intubation and extubation failure.[7] In the same article, a series of both interventional trials and observational cohort studies were reviewed and revealed a wide range of extubation failure rates from <5% to >30%, with a median of 14%, regarded by the authors as unacceptably high. We believe that our comparatively lower rate of reintubation reflected the preponderance of postoperative patients (a significant proportion of whom would have had elective surgery) included in our analysis, a hypothesis supported by the finding of a relatively short duration of mechanical ventilation of patients in our study compared to the other studies. Indeed, analysis of the subgroup of patients who underwent intubation outside of the operating room (likely for more emergent indications) revealed a reintubation rate of 11.1% which was closer to the median figure quoted in Krinsley's report. Along similar lines, the extubation failure rate was the highest among the medical overflow patients at 16.7% and patients with pneumonia compared to the other groups (although not eventually statistically significant), as well as in patients with sepsis, consistent with prior studies that showed higher rates of failed extubation among medical patients compared to surgical ones, and higher failure rates in patients with pneumonia.[11,12,13,14,15,16]
By way of comparison, a database review by Lee et al. of reintubations in the operating room and recovery unit following anesthetic cases in a noncritical care population demonstrated a reintubation rate of just 0.17% (191 reintubations in 107,317 general anesthetics).[17] While the figure obtained in this study might be less useful for comparison in a critical care context, it would not be unreasonable to consider that patients undergoing extubations as a whole lie on a continuous spectrum from low-risk elective surgical patient to high-risk emergency patient, with different risk/benefit profiles attached to each decision to extubate. In this regard, the development of a “sliding scale” of optimal reintubation rates as calibrated according to case mix and patient population of each unit and ideally individualized to the clinical parameters in the individual patient might be favorable over the blanket application of a single target rate across all units and patients, and perhaps an area worthy of further investigation.
Nearly 2.6% of our study patients experienced an unplanned extubation, with a reintubation rate of 23.1% in this group, with unplanned extubation being a statistically significant risk factor for reintubation in our study. This is consistent with findings from other studies which showed high reintubation rates in this group.[18,19,20,21,22] However, our figures were again found to be much lower than those from another local study (which found an unplanned extubation rate of 8.7% and a subsequent reintubation rate of 58.3% in a medical ICU) and reported rates in other literature of 3%–16% and 37%–76% for each of these variables, respectively, again likely reflecting differences in disease and patient population characteristics between medical and surgical patients.[23] It was interesting to note, however, that while the incidence of unplanned extubations has generally been found to be lower in surgical patients (2%–3.7%) than medical, none of the unplanned extubations in our study occurred in our 42 medical patients.[24]
The use of NIV in our study was found to be associated with increased extubation failure, even after adjustment with multivariable analysis. This is in contrast to literature which has shown NIV to improve reintubation rates and mortality, particularly in those with hypercapnic respiratory failure and chronic respiratory disease.[25,26] Our findings are likely due to the observational nature of our study, with incomplete adjustment for confounders such as severity of illness, and the fact that the patients on NIV in our study represented a subgroup already identified to be at high risk before extubation.
Anemia (defined either as serum hemoglobin levels <10 g/dl or hematocrit <34% in prior studies) has been found to correlate with reintubation risk, findings that were duplicated in our study, which showed lower hemoglobin levels in the group that failed extubation at approximately similar cutoff points to these studies.[11,27] The precise role of anemia in extubation failure, whether merely serving as an association or marker of disease severity, or alternatively as a causative factor perhaps through the pathophysiologic mechanism of decreased oxygen delivery reserves has been a subject of some debate, with the distinction being important in advising on the appropriateness of red cell transfusions as a means of reducing extubation failures. Our study showed a 1.0 g/dl difference in median hemoglobin levels between groups which did not remain associated with extubation failure after adjustment with multivariable analysis, which appears to support the former conclusion. Apart from physiological studies and a case series where blood transfusions (from a mean hemoglobin level of 8.7 g/dl to approximately 12 g/dl) were proposed to have aided successful extubation in difficult to wean COPD patients, evidence elsewhere in this area is indirect at best.[28,29] In the absence of dedicated prospective randomized studies specifically addressing this question, it is notable that the two significant bodies of randomized data regarding the issue of restrictive (7 g/dl) versus liberal (9 g/dl) transfusion thresholds (namely the TRICC and TRISS studies) reported increased rates of pulmonary edema and a trend toward significantly increased rates of acute respiratory distress syndrome in the group with a liberal transfusion threshold in the former study, and no difference in ventilator-free days between liberal and restrictive groups in the latter study, cautioning against overenthusiasm and suggesting the need for careful patient selection when considering this intervention as a mean to improve extubation prospects.[30,31]
In our study, the patients that failed extubation were found to have had a longer preceding duration of mechanical ventilation that those who did not an observation also made in other prior studies.[32,33] However, none of the premorbid conditions analyzed for, including underlying cardiac disease and chronic obstructive pulmonary disease (conditions found in other studies to add to reintubation risk), appeared to have any bearing on reintubation rates. These findings contrasted with those of Thille et al, Rady and Ryan, and Engoren et al, who demonstrated these premorbid conditions as associated with an reintubation risk. We were also unable to demonstrate any association between reintubation with advanced age or serum albumin levels, factors which have been found correlate with extubation failure in other studies.[11,34,35]
Limitations
The limitations of our study included the relatively small sample size (particularly in the extubation failure group) which would have limited statistical power for some of the clinical factors of lower prevalence. There was also a lack of data on illness severity scores which would have allowed for more precise adjustment of odds ratios and been of help in benchmarking our extubation failure rate against other units. The observational nature of the study also meant that there was no strictly standardized protocol for SBT and extubation; variations in which may possibly have contributed to differences in rates of extubation failure.
CONCLUSIONS
Reintubations occurred in 7.5% of our study patients. Factors associated with extubation failure identified in our study included the presence of sepsis during the ICU stay, unplanned extubation, and use of NIV after extubation, reinforcing the need for increased vigilance in this subgroup of patients after extubation.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Nichol A, Duff S, Pettila V, Cooper DJ. What is the optimal approach to weaning and liberation from mechanical ventilation? In: Deutschman CS, Neligan PJ, editors. Evidence-Based Practice of Critical Care. Philadelphia, PA: Elsevier; 2016. pp. 52–60. [Google Scholar]
- 2.Krinsley J, Reddy P, Iqbal A. Case-control study of failed extubation. Crit Care. 2012;16(Suppl 1):128. doi: 10.1186/cc11185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Beckmann U, Gillies DM. Factors associated with reintubation in intensive care: An analysis of causes and outcomes. Chest. 2001;120:538–42. doi: 10.1378/chest.120.2.538. [DOI] [PubMed] [Google Scholar]
- 4.Kulkarni AP, Agarwal V. Extubation failure in Intensive Care Unit: Predictors and management. Indian J Crit Care Med. 2008;12:1–9. doi: 10.4103/0972-5229.40942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Meade M, Guyatt G, Cook D, Griffith L, Sinuff T, Kergl C, et al. Predicting success in weaning from mechanical ventilation. Chest. 2001;120(6 Suppl):400S–24S. doi: 10.1378/chest.120.6_suppl.400s. [DOI] [PubMed] [Google Scholar]
- 6.Liu Y, Wei LQ, Li GQ, Lv FY, Wang H, Zhang YH, et al. A decision-tree model for predicting extubation outcome in elderly patients after a successful spontaneous breathing trial. Anesth Analg. 2010;111:1211–8. doi: 10.1213/ANE.0b013e3181f4e82e. [DOI] [PubMed] [Google Scholar]
- 7.Krinsley JS, Reddy PK, Iqbal A. What is the optimal rate of failed extubation? Crit Care. 2012;16:111. doi: 10.1186/cc11185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mokhlesi B, Tulaimat A, Gluckman TJ, Wang Y, Evans AT, Corbridge TC. Predicting extubation failure after successful completion of a spontaneous breathing trial. Respir Care. 2007;52:1710–7. [PubMed] [Google Scholar]
- 9.Miu T, Joffe AM, Yanez ND, Khandelwal N, Dagal AH, Deem S, et al. Predictors of reintubation in critically ill patients. Respir Care. 2014;59:178–85. doi: 10.4187/respcare.02527. [DOI] [PubMed] [Google Scholar]
- 10.Wang S, Zhang L, Huang K, Lin Z, Qiao W, Pan S. Predictors of extubation failure in neurocritical patients identified by a systematic review and meta-analysis. PLoS One. 2014;9:e112198. doi: 10.1371/journal.pone.0112198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rady MY, Ryan T. Perioperative predictors of extubation failure and the effect on clinical outcome after cardiac surgery. Crit Care Med. 1999;27:340–7. doi: 10.1097/00003246-199902000-00041. [DOI] [PubMed] [Google Scholar]
- 12.Demling RH, Read T, Lind LJ, Flanagan HL. Incidence and morbidity of extubation failure in surgical intensive care patients. Crit Care Med. 1988;16:573–7. doi: 10.1097/00003246-198806000-00001. [DOI] [PubMed] [Google Scholar]
- 13.Engoren M, Buderer NF, Zacharias A, Habib RH. Variables predicting reintubation after cardiac surgical procedures. Ann Thorac Surg. 1999;67:661–5. doi: 10.1016/s0003-4975(98)01321-6. [DOI] [PubMed] [Google Scholar]
- 14.Daley BJ, Garcia-Perez F, Ross SE. Reintubation as an outcome predictor in trauma patients. Chest. 1996;110:1577–80. doi: 10.1378/chest.110.6.1577. [DOI] [PubMed] [Google Scholar]
- 15.Frutos-Vivar F, Ferguson ND, Esteban A, Epstein SK, Arabi Y, Apezteguía C, et al. Risk factors for extubation failure in patients following a successful spontaneous breathing trial. Chest. 2006;130:1664–71. doi: 10.1378/chest.130.6.1664. [DOI] [PubMed] [Google Scholar]
- 16.Rothaar RC, Epstein SK. Extubation failure: Magnitude of the problem, impact on outcomes, and prevention. Curr Opin Crit Care. 2003;9:59–66. doi: 10.1097/00075198-200302000-00011. [DOI] [PubMed] [Google Scholar]
- 17.Lee PJ, MacLennan A, Naughton NN, O'Reilly M. An analysis of reintubations from a quality assurance database of 152,000 cases. J Clin Anesth. 2003;15:575–81. doi: 10.1016/j.jclinane.2003.03.006. [DOI] [PubMed] [Google Scholar]
- 18.Balon JA. Common factors of spontaneous self-extubation in a critical care setting. Int J Trauma Nurs. 2001;7:93–9. doi: 10.1067/mtn.2001.117769. [DOI] [PubMed] [Google Scholar]
- 19.Epstein SK, Nevins ML, Chung J. Effect of unplanned extubation on outcome of mechanical ventilation. Am J Respir Crit Care Med. 2000;161:1912–6. doi: 10.1164/ajrccm.161.6.9908068. [DOI] [PubMed] [Google Scholar]
- 20.Boulain T. Unplanned extubations in the adult Intensive Care Unit: A prospective multicenter study. Association des Réanimateurs du Centre-Ouest. Am J Respir Crit Care Med. 1998;157(4 Pt 1):1131–7. doi: 10.1164/ajrccm.157.4.9702083. [DOI] [PubMed] [Google Scholar]
- 21.Mort TC. Unplanned tracheal extubation outside the operating room: A quality improvement audit of hemodynamic and tracheal airway complications associated with emergency tracheal reintubation. Anesth Analg. 1998;86:1171–6. doi: 10.1097/00000539-199806000-00006. [DOI] [PubMed] [Google Scholar]
- 22.Betbesé AJ, Pérez M, Bak E, Rialp G, Mancebo J. A prospective study of unplanned endotracheal extubation in Intensive Care Unit patients. Crit Care Med. 1998;26:1180–6. doi: 10.1097/00003246-199807000-00016. [DOI] [PubMed] [Google Scholar]
- 23.Phoa LL, Pek WY, Syap W, Johan A. Unplanned extubation: A local experience. Singapore Med J. 2002;43:504–8. [PubMed] [Google Scholar]
- 24.Atkins PM, Mion LC, Mendelson W, Palmer RM, Slomka J, Franko T. Characteristics and outcomes of patients who self-extubate from ventilatory support: A case-control study. Chest. 1997;112:1317–23. doi: 10.1378/chest.112.5.1317. [DOI] [PubMed] [Google Scholar]
- 25.Ferrer M, Valencia M, Nicolas JM, Bernadich O, Badia JR, Torres A. Early noninvasive ventilation averts extubation failure in patients at risk: A randomized trial. Am J Respir Crit Care Med. 2006;173:164–70. doi: 10.1164/rccm.200505-718OC. [DOI] [PubMed] [Google Scholar]
- 26.Kee A, Phua J, Huang Y, Dela Pena E, Santiago E, Santos J, et al. A five-year series on the use of noninvasive ventilation as a weaning tool from invasive ventilation. Eur Respir J. 2011;38(Suppl 55):2065. [Google Scholar]
- 27.Khamiees M, Raju P, DeGirolamo A, Amoateng-Adjepong Y, Manthous CA. Predictors of extubation outcome in patients who have successfully completed a spontaneous breathing trial. Chest. 2001;120:1262–70. doi: 10.1378/chest.120.4.1262. [DOI] [PubMed] [Google Scholar]
- 28.Schönhofer B, Wenzel M, Geibel M, Köhler D. Blood transfusion and lung function in chronically anemic patients with severe chronic obstructive pulmonary disease. Crit Care Med. 1998;26:1824–8. doi: 10.1097/00003246-199811000-00022. [DOI] [PubMed] [Google Scholar]
- 29.Schönhofer B, Böhrer H, Köhler D. Blood transfusion facilitating difficult weaning from the ventilator. Anaesthesia. 1998;53:181–4. doi: 10.1046/j.1365-2044.1998.00275.x. [DOI] [PubMed] [Google Scholar]
- 30.Hébert PC, Wells G, Blajchman MA, Marshall J, Martin C, Pagliarello G, et al. A multicenter, randomized, controlled clinical trial of transfusion requirements in critical care. Transfusion Requirements in Critical Care Investigators, Canadian Critical Care Trials Group. N Engl J Med. 1999;340:409–17. doi: 10.1056/NEJM199902113400601. [DOI] [PubMed] [Google Scholar]
- 31.Holst LB, Haase N, Wetterslev J, Wernerman J, Guttormsen AB, Karlsson S, et al. Lower versus higher hemoglobin threshold for transfusion in septic shock. N Engl J Med. 2014;371:1381–91. doi: 10.1056/NEJMoa1406617. [DOI] [PubMed] [Google Scholar]
- 32.Lee KH, Hui KP, Chan TB, Tan WC, Lim TK. Rapid shallow breathing (frequency-tidal volume ratio) did not predict extubation outcome. Chest. 1994;105:540–3. doi: 10.1378/chest.105.2.540. [DOI] [PubMed] [Google Scholar]
- 33.Edmunds S, Weiss I, Harrison R. Extubation failure in a large pediatric ICU population. Chest. 2001;119:897–900. doi: 10.1378/chest.119.3.897. [DOI] [PubMed] [Google Scholar]
- 34.Thille AW, Harrois A, Schortgen F, Brun-Buisson C, Brochard L. Outcomes of extubation failure in medical Intensive Care Unit patients. Crit Care Med. 2011;39:2612–8. doi: 10.1097/CCM.0b013e3182282a5a. [DOI] [PubMed] [Google Scholar]
- 35.El Solh AA, Bhat A, Gunen H, Berbary E. Extubation failure in the elderly. Respir Med. 2004;98:661–8. doi: 10.1016/j.rmed.2003.12.010. [DOI] [PubMed] [Google Scholar]


