Abstract
INTRODUCTION:
There is a rise in prevalence of work-related musculoskeletal disorders in surgeons performing laparoscopic surgeries due to lack of ergonomic considerations to the minimal access surgical environment. The objective of this study was to assess the physical ergonomics in experienced and novice surgeons during a simulated laparoscopic cholecystectomy.
METHODOLOGY:
Thirty-two surgeons participated in this study and were distributed in two groups (experienced and novices) based on the inclusion criteria. Both groups were screened for the spinal and wrist movements on the orientation sensor-based, motion analysis device while performing a simulated laparoscopic cholecystectomy. Simultaneous video recording was used to estimate the other joint positions. The RULA (Rapid Upper Limb Assessment) ergonomic risk scores were estimated with the acquired data.
RESULTS:
We found that surgeons in both novice and experienced groups scored a high on the RULA. Limited awareness of the influence of monitor position on the postural risk caused surgeons to adopt non-neutral range cervical postures. The thoracolumbar spine is subjected to static postural demand. Awkward wrist postures were adopted during the surgery by both groups. There was no statistically significant difference in the RULA scores between the novice and experienced, but some differences in maximum joint excursions between them as detected on the motion analysis system.
CONCLUSION:
Both experienced and novice surgeons adopted poor spinal and wrist ergonomics during simulated cholecystectomy. We concluded that the physical ergonomic risk is medium as estimated by the RULA scoring method, during this minimally invasive surgical procedure, demanding implementation of change in the ergonomic practices.
Keywords: Ergonomic analysis, rapid upper limb assessment, simulated laparoscopic cholecystectomy, spinal and wrist motion analysis
INTRODUCTION
The impression of open surgery is characteristically that of prolonged painful recuperative periods with long scars. This has been transformed to more acceptable painless, cosmetically satisfying surgery with a short hospital stay due to the advent of operative laparoscopy.[1,2] This has been achieved at the expense of surgeons’ discomfort and fatigue. Work-related musculoskeletal disorders (WRMSDs) are being considered as an important health issue among surgeons performing minimally invasive surgeries (MISs), especially laparoscopic procedures.[3,4,5,6,7] Inadequate understanding of physical ergonomics, ergonomically deficient design of laparoscopic instruments and increased technological complexity have been cited as possible causes.[5,6,8]
Hence, ergonomic assessments to identify risk factors of WRMSDs are being increasingly researched. Laboratory research is prevalent in this field, frequently conducted in simulated environment using box trainers or other models. Suturing[9,10,11,12,13,14,15] and tying of knots[16,17,18,19,20] have been the most commonly tested laparoscopic manipulation tasks utilised for assessing muscle activity, fatigue, task accuracy, pattern of joint movements, etc. The above-mentioned tasks, although very important for the performance of a successful surgery, occupy only a small percentage of the total surgical time. There is a limitation to generalise the applicability of the results of aforementioned tasks in surgical ergonomics. Moreover, there is a dearth of ergonomic assessment studies analysing the important components such as dissection and exposure retraction. Hence, in this study, we selected a basic, simulated, surgical protocol which incorporated tasks such as tissue dissection, exposing, retraction, clipping and suction with a surgical flow mimicking a real case scenario.
The main purpose of this study was to conduct an ergonomic analysis of experienced and novice surgeons while performing a simulated laparoscopic cholecystectomy. We aimed to assess and report the cumulative ergonomic risk to the spine and the wrist during a procedure incorporating surgical flow as this may incorporate more natural movement patterns utilised by the surgeon. Furthermore, the movements that occurred during task transition would be included in the final risk analysis. Other purpose of this analysis was to analyse whether any difference exists in ergonomic between the experienced and novice surgeons.
METHODOLOGY
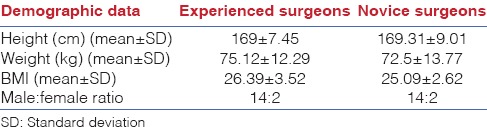
Thirty-six right-handed laparoscopic surgeons were included in the study after obtaining informed consent. Participants were divided into two groups according to the level of laparoscopic surgical experience: Experts (n = 16) and novices (n = 16). The expert group included the surgeons who were practising laparoscopic procedures for at least a minimum of 3 years and the novice group consisted of surgeons and residents who had no previous laparoscopic surgical experience else than observation of laparoscopic surgeries. The demographic characteristics of the participating surgeons are given in Table 1.
Table 1.
Demographic characteristics of the participating surgeons
The simulated cholecystectomy was performed on LapVR simulator (CAE care manufacturer). In this virtual reality surgical simulator, there are three input portals, i.e. two trocars and one camera and a screen to visualise the procedure [Figure 1]. Both right- and left-hand controls of the trocars were ring-handled. The procedure was selected at a basic level for aiding the completion by the novice surgeon. Training session for familiarising with the surgical simulator controls was provided for the surgeons participating in the study. The height of the monitor and the trocars was fixed during all procedures in this study. The working height and dimension of the simulator monitor and trocar were as follows:
Figure 1.

LapVR surgical simulator
Monitor screen height from the ground - 168.5 cm
Monitor screen width - 56 cm
Height of the trocars from the ground - 108 cm.
A common surgical procedure was performed by the surgeons in both groups which comprised the three main tasks mentioned below.
Task 1: Exposure of the gallbladder and dissection of adhesions
Task 2: Clipping and division of cystic structures
Task 3: Mobilisation and removal of the gallbladder.
At the end of the simulation task, the performance measures and dexterity were displayed on the simulator screen as a compiled report. The motion analysis data and rapid upper limb assessment (RULA) were used to estimate the surgeons’ ergonomics. Performance score was computed based on metric evaluation system report on the simulator. The details of the outcome measures are discussed below.
Metrics evaluation system available on the simulation equipment
(a) Time required to complete the procedure and whether the designated time was exceeded. (b) Proficiency was tested on analysis of items such as the total blood loss during the procedure, a number of clips dropped and used. There were 25 components on performance measures for which each surgeon was given a positive marking once the criteria were met. (c) Dexterity was analysed on the basis of total path length of the left and right hand during the procedure.
Objective record of wrist joint and spinal movements with the help of movement analysis system and software
Noraxon's three-dimensional (3D) Myomotion analysis system consists of a set of sensors using inertial sensor technology [Figure 2]. Based on fusion algorithms, the information from a 3D accelerometer, gyroscope and magnetometer is used to measure the 3D rotation angles of each sensor in absolute space. Noraxon's system software converts the quaternion data into anatomical angles using a rigid body model.
Figure 2.

Noraxon myomotion inertial measurement unit sensors and display screen
The motion sensors were attached to the following sites:
Forehead
Thoracic spine - T1 ( first thoracic) vertebra
Lumbar spine - S2 (second sacral) level
Mid-forearm - strapped on both left and right forearms
Hand - strapped around the dorsal aspect of the hand (both left and right side).
The data from the software, the movement of the cervical and thoracolumbar (TL) spine, are computed in all three dimensions, namely, sagittal, coronal and transverse planes and movement of the wrist in the sagittal and coronal planes. At the cervical and TL spine flexion, the right side rotation and lateral flexion are displayed as positive, and at extension, the left side rotation and lateral flexion are designated negative signs. Similarly, the wrist extension and radial deviation (RD) are designated positive and wrist flexion and ulnar deviation (UD) with negative signs. For example, −30° in the sagittal plane means 30° of extension and +30° means 30° of flexion. Accordingly, the joint movement values are assigned positive or negative signs [Tables 2 and 3]. The motion analysis data were measured through the entire simulated procedure. The maximum angles in each direction were computed and used for comparison between the groups.
Table 2.
Maximum excursion of the cervical and thoracolumbar spine
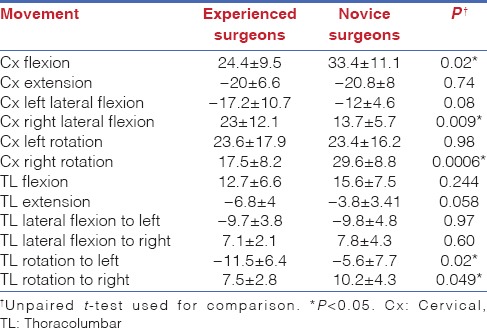
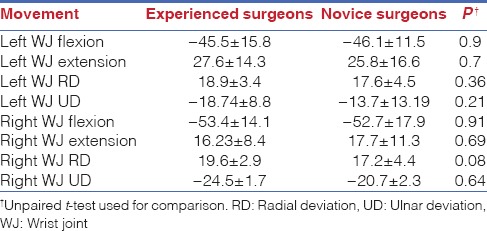
Table 3.
Maximum excursion of the wrist joint
Observational record of upper limb posture and risk assessment on rapid upper limb assessment scale
The RULA scale is a tool which helps draw conclusion on ergonomic risks related to an occupational task. The RULA is divided into components such as upper arm, lower arm, wrist, neck, trunk and leg. The positions of the upper arm, lower arm and wrist are grouped together which give out a score, that is, clubbed alongside the similar score formed by the neck, trunk and leg. The two scores are looked up in a table consisting values which indicate risk. Based on the outcomes of the score, further investigations and ergonomic changes can be decided.[21]
1 or 2 = Acceptable posture
3 or 4 = Further investigation, change may be needed
5 or 6 = Further investigation, change soon
7 = Investigate and implement change.
RESULTS
The data of the maximum cervical and TL movement excursion [Table 2], wrist movement excursion [Table 3], RULA scores [Table 4] and performance scores [Table 5] obtained during the simulated cholecystectomy was statistically compared between the novice and experienced surgeons. P < 0.05 was considered statistically significant.
Table 4.
Comparison of rapid upper limb assessment scores
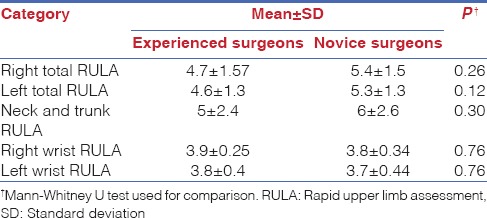
Table 5.
Comparison of performance and dexterity scores

Objective movement analysis data
During the simulated surgery, myomotion system-generated data of the cervical spine movements indicate that the maximum cervical flexion and the right side rotation were higher in novice whereas the right lateral flexion was higher in experienced surgeons.
The results of the TL spine indicate that the novice showed more right TL rotation and the experienced surgeons showed more left TL rotation when maximum angles were compared. The other movement values were not different between the groups.
The results of motion analysis indicate the high left wrist flexion angles adopted by the surgeons, i.e., maximum angles >45° with concomitant RD. At the right wrist joint (WJ) too, maximum angles of >50° flexion and concomitant RD or UD were recorded in the sagittal and coronal plane. On comparison, there were no differences in the maximum angles of both left and right WJs between the experienced and novice surgeons.
Rapid upper limb analysis scores
The result of the RULA score indicates that there is a high postural risk during this surgical procedure. Although the RULA scores were higher in the novice surgeons, the difference was not statistically significant.
Performance and dexterity measures
For comparing path length, unpaired t-test was used whereas Mann–Whitney U test statistic was used to compare performance measures. The performance score was higher in the experienced group; however, the difference was not statistically significant.
DISCUSSION
The primary objective of this study was to assess the ergonomics in the novice and experienced surgeons during a simulated laparoscopic cholecystectomy, and the secondary objective was to compare them for any differences in ergonomics. We studied the spinal and wrist postures during a simulated cholecystectomy using objective motion analysis.
Spinal ergonomic analysis
Our study findings confirm that the surgeons’ head posture depends on the orientation of the monitor at the operation theatre as has been reported in other studies.[22,23]
In our study, most of the surgeons adopted neck extension posture during the simulated surgery, which they attributed to either screen height or habitual neck postures. The novice had higher maximum excursions into flexion and rotation which may be both due to limited visual cueing (loss of 3D visual perspective and limited peripheral vision due to limited viewing spectrum) and insufficient laparoscopic surgical experience. However, the reason for the higher maximum lateral flexion in the experienced surgeons remains inexplicable.
Overall, there was ergonomically acceptable upright TL posture adopted by the surgeons during the simulated surgery. Our study results support the findings of Berguer et al. which state that although the posture of the surgeon is more upright during laparoscopy, it seems to be accompanied by substantially less body movement and weight shifting than during open surgery.[24] This situation could account for increased static postural fatigue as the operation lasts for minimum period of 60 min and can extend to a couple of hours. Sjøgaard et al.[25] have revealed that even relatively low levels (5% of maximum voluntary contraction [MVC]) of muscle contraction, if sustained for an hour, can lead to muscle fatigue. Jonsson et al.[26] have suggested that the static muscle contraction should not exceed 5% of MVC for tasks of prolonged duration. The probable reason for this as elucidated by Sjogaard[27] could be that during low-level contractions, the muscle can maintain homoeostasis with respect to energy turnover but not with respect to intracellular/extracellular potassium concentration. This potassium imbalance may well play a role in the muscle fatigue. The static trunk posture could be one of the reasons that increase the risk of musculoskeletal problems and pain in minimal access surgeons.
When compared, there were no statistically significant differences in the maximum ranges between the experienced and novice surgeons except in TL rotation. The reason for higher right side TL rotation in novice could be due to their incorrect starting position. Their entire body was rotated to the left due to the inappropriate feet placement, due to which there was a compensatory right side neck and trunk rotation.
Neck and trunk rapid upper limb assessment
In our study, no surgeon scored in an acceptable range of 1–2 on the neck and trunk RULA. Fifteen surgeons scored 3–4 on the RULA whereas 17 surgeons scored more than 5.
Although the TL spine was in near neutral postures, the positions adopted by the cervical spine scores increased the RULA scores during the simulated surgery. The surgeons who scored high on the RULA (>5) had adopted cervical extension along with rotation and lateral flexion. The surgeons who scored lower on the RULA (3 or 4) had adopted either near neutral postures of the cervical spine or lesser degrees of flexion during the surgery. Inappropriate monitor position, limited ergonomic awareness and habitual extension and lateral flexion postures adopted during the simulation surgery, culminated to the high neck and trunk RULA scores in both groups. Hence, there was no statistically significant difference between the groups on neck and trunk RULA.
These findings further strengthen the existing body of evidence which indicates that the monitor position can greatly influence the adoption of wrong postures of the neck. The static TL posture adds to the musculoskeletal risk at the spine in both novice and experienced surgeons.
Wrist and hand ergonomic analysis
The role of the left upper extremity is predominantly to hold and manoeuvre the tissue which had to be operated on. The typical trend observed in both experienced and novice surgeons at the left wrist was flexion >45° with radial angular deviation. The RD was a result of the handle design of the ring handle grasper. However, at higher wrist flexion angles, the wrist was positioned in either neutral or UD [Figure 3].
Figure 3.

The right and left wrist awkward position while using ring-handled instrument during the simulated surgery
The right upper extremity had to function to manoeuvre the different instruments (Maryland dissector, clip applicator, endoscopic shear, L-hook electrocautery and suction) for various tasks of the simulated surgery.
In our study, the maximum right wrist flexion was above 50° in both experienced and novice surgeons. The frequently adopted wrist position in the frontal plane was of UD [Figure 3], with intermittent RD. There were periodic changes in position of the right wrist in both sagittal and frontal plane while performing tasks such as dissection, clipping and cauterisation. The demand on the right wrist and hand was movement predominated.
No surgeon in both experienced and novice group adopted a neutral wrist posture. When we compared maximum right and left wrist excursions, there was no significant difference between the experienced and novice surgeons.
Adopting wrist flexion posture during surgery can be unfavourable for the surgeon. There is a reduction in grip strength as well as an increase in the carpal tunnel pressure with wrist in flexed posture. Keir et al. had revealed that the hydrostatic pressure in the carpal tunnel was found to be affected by both wrist posture and tendon load. Muscular loading elevated carpal tunnel pressure, particularly the loading of palmaris longus with the wrist in extension and the digital flexors with the wrist flexed. Correspondingly, the local contact forces by the digital flexors indicated the highest loads on the median nerve with the wrist flexed. Anteriorly positioned nerves were flattened in the anteroposterior plane between the tendon and flexor retinaculum; this was greatest with flexion and least with extension.[28] Furthermore, maximum grip efficiency has been reported in 20–35° of extension and relatively low angles (5–7°) of UD by other researchers.[29,30] Hence, in light of the aforementioned reasons, the high wrist flexion angles occurring during laparoscopic surgeries should be reduced by novel ergonomic handle designs.
Matern et al. have discussed earlier that a drawback of MIS handles is their deviation from the longitudinal axis of the forearm, which causes uncomfortable UD and RD of the wrist and requires large-scale arm movements for simple instrument rotation along the longitudinal axis.[31] Many previous studies have highlighted on sagittal plane angles (flexion and extension) at the wrist. However, a limited number of studies[32,33,34] have emphasised on frontal plane movements (wrist RD/UD) during laparoscopic procedures. Although UD has been more commonly reported, occurrence of RD during laparoscopic procedures has also been mentioned in previous research.[35,36] Nguyen et al. have reported that at the upper extremity, there are more wrist supination and wrist UD and RD during a laparoscopic procedure as compared to open surgery.[36]
Furthermore, the method utilised in previous research more commonly was video analysis.[35,36] During video analysis, if the camera is not aligned well or the participant under study changes his/her position with respect to the camera, some movements and the precise degree to which they occur can be overlooked. Since the accelerometer sensor used in this study is attached to the forearm and hand, even with a change in upper limb position, the angular movements are recorded with sufficient precision at the wrist.
Although higher flexion angles and UD predominate, the presence of RD cannot be ignored. Furthermore, RD can cause a reduction in the grip force and add to the mechanical inefficiency.[37]
In our study, the wrist RULA score was high, i.e., 4, for majority of the surgeons (25 on the left and 29 on the right side), with few surgeons (7 surgeons on the left and 3 on the right side) scoring 3. There was no difference in mean RULA scores between the experienced and novice groups. The results of our study support the findings of Sánchez-Margallo et al., which indicate that the previous laparoscopic experience has no favourable effect while using ring-handled instrument. The RULA score results of their study suggest that all study surgeons adopt an inadequate position of the wrist associated with a marked hyperflexion of this joint.[38] They computed the RULA scores for the risk based on sagittal plane deviations (i.e., flexion-extension). In our study, we included the WJ deflections in the both sagittal and frontal planes to compute wrist RULA.
The surgeons in our study performed the simulated surgical procedure with ring-handled instrument handles in both hands. In biomechanical terms, these elongated instruments increase the leverage of the load arm leading to greater angles of wrist deviations in the sagittal and coronal plane. This leads to an increased postural stress at the WJ and may contribute to wrist and hand pain. Previous research indicates that ring handled instruments are less preferred due to the awkward wrist position imposed by them, when compared to axial handled instruments.[39]
Berguer et al. compared the muscle tension (surface electromyography) caused by two different grasping modalities during the use of ring-handled laparoscopic scissors, showing that it is beneficial to use larger palm support instead of introducing the thumb through the rings of the handle.[40] In our study, we observed that all the surgeons placed their fingers through the rings in the scissors’ handle contrary to Berguer's recommendations, with the exception of one surgeon who used palmar grasp on the left hand to hold the ring-handled instrument. This reflects the fact that reported ergonomic guidelines are usually ignored by operating laparoscopic surgeons, similarly to evidence reported by Wauben et al. in their study.[41]
In comparison to previous research, we did not find any statistically significant difference in performance measures between the experienced and novice surgeons [Table 5]. The probable reason for this could be because basic level surgery was chosen for comparison; as well, to the goal-oriented task, nature of the surgical task could have led to greater motivation for task completion in the novice surgeons.
CONCLUSION
An objective analysis of the wrist shows that both expert and novice surgeons adopt disadvantageous postures of both right and left wrists while using axial-handled instruments on the simulator. Hence, there is an impeding need for revision in the handle design. The spinal analysis indicates that the monitor position greatly influences the neck posture, and predominantly static postures are adopted at the TL spine.
We conclude that ergonomic inadequacies can lead to the physical postural risk, during the minimally invasive surgical procedure in both experienced and novice surgeons.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Berggren U, Gordh T, Grama D, Haglund U, Rastad J, Arvidsson D. Laparoscopic versus open cholecystectomy: Hospitalization, sick leave, analgesia and trauma responses. Br J Surg. 1994;81:1362–5. doi: 10.1002/bjs.1800810936. [DOI] [PubMed] [Google Scholar]
- 2.Richards C, Edwards J, Culver D, Emori TG, Tolson J, Gaynes R National Nosocomial Infections Surveillance (NNIS) System. Does using a laparoscopic approach to cholecystectomy decrease the risk of surgical site infection? Ann Surg. 2003;237:358–62. doi: 10.1097/01.SLA.0000055221.50062.7A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wauben LS, van Veelen MA, Gossot D, Goossens RH. Application of ergonomic guidelines during minimally invasive surgery: A questionnaire survey of 284 surgeons. Surg Endosc Interv Tech. 2006;20:1268–74. doi: 10.1007/s00464-005-0647-y. [DOI] [PubMed] [Google Scholar]
- 4.Stomberg MW, Tronstad SE, Hedberg K, Bengtsson J, Jonsson P, Johansen L, et al. Work-related musculoskeletal disorders when performing laparoscopic surgery. Surg Laparosc Endosc Percutan Tech. 2010;20:49–53. doi: 10.1097/SLE.0b013e3181cded54. [DOI] [PubMed] [Google Scholar]
- 5.Sari V, Nieboer TE, Vierhout ME, Stegeman DF, Kluivers KB. The operation room as a hostile environment for surgeons: Physical complaints during and after laparoscopy. Minim Invasive Ther Allied Technol. 2010;19:105–9. doi: 10.3109/13645701003643972. [DOI] [PubMed] [Google Scholar]
- 6.Szeto GP, Ho P, Ting AC, Poon JT, Cheng SW, Tsang RC. Work-related musculoskeletal symptoms in surgeons. J Occup Rehabil. 2009;19:175–84. doi: 10.1007/s10926-009-9176-1. [DOI] [PubMed] [Google Scholar]
- 7.Dabholkar T, Yardi S, Dabholkar YG, Khanvilkar A. Work Related musculoskeletal disorders in surgeons performing minimal invasive procedures in Mumbai and Navi Mumbai India. Int J Health Sci Res. 2015;5:347–55. [Google Scholar]
- 8.Lucas-Hernández M, Pagador JB, Pérez-Duarte FJ, Castelló P, Sánchez-Margallo FM. Ergonomics problems due to the use and design of dissector and needle holder: A survey in minimally invasive surgery. Surg Laparosc Endosc Percutan Tech. 2014;24:e170–7. doi: 10.1097/SLE.0b013e3182937fe8. [DOI] [PubMed] [Google Scholar]
- 9.Moorthy K, Munz Y, Undre S, Darzi A. Objective evaluation of the effect of noise on the performance of a complex laparoscopic task. Surgery. 2004;136:25–30. doi: 10.1016/j.surg.2003.12.011. [DOI] [PubMed] [Google Scholar]
- 10.Uchal M, Brogger J, Rukas R, Karlsen B, Bergamaschi R. In-line versus pistol-grip handles in a laparoscopic simulators. A randomized controlled crossover trial. Surg Endosc. 2002;16:1771–3. doi: 10.1007/s00464-002-8816-8. [DOI] [PubMed] [Google Scholar]
- 11.Joice P, Hanna GB, Cuschieri A. Ergonomic evaluation of laparoscopic bowel suturing. Am J Surg. 1998;176:373–8. doi: 10.1016/s0002-9610(98)00202-5. [DOI] [PubMed] [Google Scholar]
- 12.Brown SI, Frank TG, El Shallaly G, Cuschieri A. Comparison of conventional and gaze-down imaging in laparoscopic task performance. Surg Endosc. 2003;17:586–90. doi: 10.1007/s00464-002-8525-3. [DOI] [PubMed] [Google Scholar]
- 13.Emam TA, Hanna G, Cuschieri A. Ergonomic principles of task alignment, visual display, and direction of execution of laparoscopic bowel suturing. Surg Endosc. 2002;16:267–71. doi: 10.1007/s00464-001-8152-4. [DOI] [PubMed] [Google Scholar]
- 14.Emam TA, Frank TG, Hanna GB, Cuschieri A. Influence of handle design on the surgeon's upper limb movements, muscle recruitment, and fatigue during endoscopic suturing. Surg Endosc. 2001;15:667–72. doi: 10.1007/s004640080141. [DOI] [PubMed] [Google Scholar]
- 15.Ahmed S, Hanna GB, Cuschieri A. Optimal angle between instrument shaft and handle for laparoscopic bowel suturing. Arch Surg. 2004;139:89–92. doi: 10.1001/archsurg.139.1.89. [DOI] [PubMed] [Google Scholar]
- 16.Emam TA, Hanna GB, Kimber C, Cuschieri A. Differences between experts and trainees in the motion pattern of the dominant upper limb during intracorporeal endoscopic knotting. Dig Surg. 2000;17:120–3. doi: 10.1159/000018813. [DOI] [PubMed] [Google Scholar]
- 17.Emam TA, Hanna GB, Kimber C, Dunkley P, Cuschieri A. Effect of intracorporeal-extracorporeal instrument length ratio on endoscopic task performance and surgeon movements. Arch Surg. 2000;135:62–5. doi: 10.1001/archsurg.135.1.62. [DOI] [PubMed] [Google Scholar]
- 18.Patil PV, Hanna GB, Frank TG, Cuschieri A. Effect of fixation of shoulder and elbow joint movement on the precision of laparoscopic instrument manipulations. Surg Endosc. 2005;19:366–8. doi: 10.1007/s00464-003-8284-9. [DOI] [PubMed] [Google Scholar]
- 19.Emam TA, Frank TG, Hanna GB, Stockham G, Cuschieri A. Rocker handle for endoscopic needle drivers. Surg Endosc. 1999;13:658–61. doi: 10.1007/s004649901068. [DOI] [PubMed] [Google Scholar]
- 20.Hanna GB, Shimi SM, Cuschieri A. Task performance in endoscopic surgery is influenced by location of the image display. Ann Surg. 1998;227:481–4. doi: 10.1097/00000658-199804000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McAtamney L, Nigel Corlett E. RULA: A survey method for the investigation of work-related upper limb disorders. Appl Ergon. 1993;24:91–9. doi: 10.1016/0003-6870(93)90080-s. [DOI] [PubMed] [Google Scholar]
- 22.Smith WD, Berguer R, Nguyen NT. Monitor height affects surgeons’ stress level and performance on minimally invasive surgery tasks. Stud Health Technol Inform. 2005;111:498–501. [PubMed] [Google Scholar]
- 23.Zehetner J, Kaltenbacher A, Wayand W, Shamiyeh A. Screen height as an ergonomic factor in laparoscopic surgery. Surg Endosc. 2006;20:139–41. doi: 10.1007/s00464-005-0251-1. [DOI] [PubMed] [Google Scholar]
- 24.Berguer R, Rab GT, Abu-Ghaida H, Alarcon A, Chung J. A comparison of surgeons’ posture during laparoscopic and open surgical procedures. Surg Endosc. 1997;11:139–42. doi: 10.1007/s004649900316. [DOI] [PubMed] [Google Scholar]
- 25.Sjøgaard G, Kiens B, Jørgensen K, Saltin B. Intramuscular pressure, EMG and blood flow during low-level prolonged static contraction in man. Acta Physiol Scand. 1986;128:475–84. doi: 10.1111/j.1748-1716.1986.tb08002.x. [DOI] [PubMed] [Google Scholar]
- 26.Jonsson B. The static load component in muscle work. Eur J Appl Physiol Occup Physiol. 1988;57:305–10. doi: 10.1007/BF00635988. [DOI] [PubMed] [Google Scholar]
- 27.Sjogaard G. Muscle energy metabolism and electrolyte shifts during low-level prolonged static contraction in man. Acta Physiol Scand. 1988;134:181–7. doi: 10.1111/j.1748-1716.1988.tb08478.x. [DOI] [PubMed] [Google Scholar]
- 28.Keir PJ, Wells RP, Ranney DA, Lavery W. The effects of tendon load and posture on carpal tunnel pressure. J Hand Surg Am. 1997;22:628–34. doi: 10.1016/S0363-5023(97)80119-0. [DOI] [PubMed] [Google Scholar]
- 29.Li ZM. The influence of wrist position on individual finger forces during forceful grip. J Hand Surg Am. 2002;27:886–96. doi: 10.1053/jhsu.2002.35078. [DOI] [PubMed] [Google Scholar]
- 30.O’Driscoll SW, Horii E, Ness R, Cahalan TD, Richards RR, An KN. The relationship between wrist position, grasp size, and grip strength. J Hand Surg Am. 1992;17:169–77. doi: 10.1016/0363-5023(92)90136-d. [DOI] [PubMed] [Google Scholar]
- 31.Matern U, Giebmeyer C, Bergmann R, Waller P, Faist M. Ergonomic aspects of different handles for minimally invasive surgery – An EMG based study. Proceedings of the Human Factors and Ergonomics Society Annual Meeting. 2001;2:1269. [Google Scholar]
- 32.van Veelen MA, Kazemier G, Koopman J, Goossens RH, Meijer DW. Assessment of the ergonomically optimal operating surface height for laparoscopic surgery. J Laparoendosc Adv Surg Tech A. 2002;12:47–52. doi: 10.1089/109264202753486920. [DOI] [PubMed] [Google Scholar]
- 33.Person JG, Hodgson AJ, Nagy AG. Automated high-frequency posture sampling for ergonomic assessment of laparoscopic surgery. Surg Endosc. 2001;15:997–1003. doi: 10.1007/s004640080155. [DOI] [PubMed] [Google Scholar]
- 34.Judkins TN, DiMartino A, Doné K, Hallbeck MS, Oleynikov D. Effect of handle design and target location on wrist posture during aiming with a laparoscopic tool. Proceedings of the Human Factors and Ergonomics Society Annual Meeting 2004 Sep 1. (Vol. 48, No. 12, pp. 1464-1468). SAGE Publications. [Google Scholar]
- 35.Gillette JC, Quick NE, Adrales GL, Shapiro R, Park AE. Changes in postural mechanics associated with different types of minimally invasive surgical training exercises. Surg Endosc. 2003;17:259–63. doi: 10.1007/s00464-002-8842-6. [DOI] [PubMed] [Google Scholar]
- 36.Nguyen NT, Ho HS, Smith WD, Philipps C, Lewis C, De Vera RM, et al. An ergonomic evaluation of surgeons’ axial skeletal and upper extremity movements during laparoscopic and open surgery. Am J Surg. 2001;182:720–4. doi: 10.1016/s0002-9610(01)00801-7. [DOI] [PubMed] [Google Scholar]
- 37.Lamoreaux L, Hoffer MM. The effect of wrist deviation on grip and pinch strength. Clin Orthop Relat Res. 1995:152–5. [PubMed] [Google Scholar]
- 38.Sánchez-Margallo FM, Pérez-Duarte FJ, Sánchez-Margallo JA, Lucas-Hernández M, Matos-Azevedo AM, Díaz-Güemes I. Application of a motion capture data glove for hand and wrist ergonomic analysis during laparoscopy. Minim Invasive Ther Allied Technol. 2014;23:350–6. doi: 10.3109/13645706.2014.925928. [DOI] [PubMed] [Google Scholar]
- 39.Matern U, Koneczny S, Tedeus M, Dietz K, Buess G. Ergonomic testing of two different types of handles via virtual reality simulation. Surg Endosc. 2005;19:1147–50. doi: 10.1007/s00464-004-2171-x. [DOI] [PubMed] [Google Scholar]
- 40.Berguer R, Gerber S, Kilpatrick G, Remler M, Beckley D. A comparison of forearm and thumb muscle electromyographic responses to the use of laparoscopic instruments with either a finger grasp or a palm grasp. Ergonomics. 1999;42:1634–45. doi: 10.1080/001401399184721. [DOI] [PubMed] [Google Scholar]
- 41.Wauben LS, van Veelen MA, Gossot D, Goossens RH. Application of ergonomic guidelines during minimally invasive surgery: A questionnaire survey of 284 surgeons. Surg Endosc. 2006;20:1268–74. doi: 10.1007/s00464-005-0647-y. [DOI] [PubMed] [Google Scholar]


