Abstract
Appendectomy is one of the most common emergency surgical procedures. Stump appendicitis is well-recognised entity has been described in the literature. Still, with recent advance in imaging technique, it remains as a clinical challenge for diagnosis and effective treatment. We present a case of 13-year-old boy who underwent laparoscopic appendectomy 3 months back and presented to us with acute abdomen associated with vomiting and fever. Imaging revealed the presence of a tubular residual inflamed tip of the appendix of size 4 cm laying in paracaecal position with approximately 50cc purulent collection around it. Subsequently, the patient underwent successful laparoscopic completion appendectomy with uneventful postoperative recovery. Histopathological examination confirmed that resected structure as an inflammatory residual appendix. For our knowledge, after an extensive search of English literature, no study had described about laparoscopic completion appendectomy for residual tip appendicitis. We authors hereby would like to emphasise the importance of complete removal of appendix not only stump part but also tip, especially in certain locations such as paracaecal, retrocaecal and subhepatic. Laparoscopy can be an option for the management of these patients, in selected cases, and with available expertise.
Keywords: Appendicular tip, completion appendectomy, laparoscopic surgery, stump appendicitis
INTRODUCTION
An emergency appendectomy is still one of the most common surgical procedures performed worldwide. The incidence of acute appendicitis in person over a lifetime is approximately 7%.[1] The post-operative development of stump appendicitis is a very rare clinical condition. Moreover, its diagnosis is delayed partly due to prior surgical history coupled with low index of suspicion; hence, the rate of perforation for stump appendicitis approaches 70%.[2] For our knowledge, no study in literature had described about laparoscopic completion appendectomy for residual tip appendicitis. Here, we present a case of residual tip appendicitis diagnosed 3 months after the index surgery and underwent successful completion appendectomy.
CASE REPORT
A 13-year-old boy who underwent laparoscopic surgery, probably appendectomy 3 months ago for acute appendicitis was referred for episodic pain in lower abdomen over last 1 month that had been treated with trial of antibiotics and analgesics. There were waxing and waning of these symptoms over the mentioned duration. This episode was sudden in onset, severe in intensity associated with two episodes of non-bilious vomiting and high-grade fever which brought this patient to us. On examination, signs of localised peritonitis were evident in the right upper quadrant. Inflammatory markers were elevated. A clinical diagnosis of residual appendicitis was made, and empirical broad spectrum antibiotics were started.
An ultrasound abdomen was performed, which revealed the presence of inflamed noncompressible, non-peristaltic, tubular structure about 2.5 cm in length and 1.2 cm in diameter located in paracaecal region with a collection of viscous fluid of around 50cc. Findings were confirmed by doing a contrast enhanced computed tomography (CECT) [Figure 1]. After optimising the patient clinically, he was taken to the operating room. Laparoscopy revealed intraperitoneal adhesions in right iliac fossa with purulent collection about 50cc. Following careful adhesiolysis, the inflamed residual tip of appendix of size 4 cm laying in paracaecal position was confirmed. We observed the presence of intact blood supply [Figure 2] to this portion from adjoining colonic wall, which probably has maintained the viability and thus persistent inflammation. The excised specimen was confirmed histologically as residual portion of the appendix. Post-operative recovery was uneventful; the patient was discharged on the 3rd post-operative day.
Figure 1.
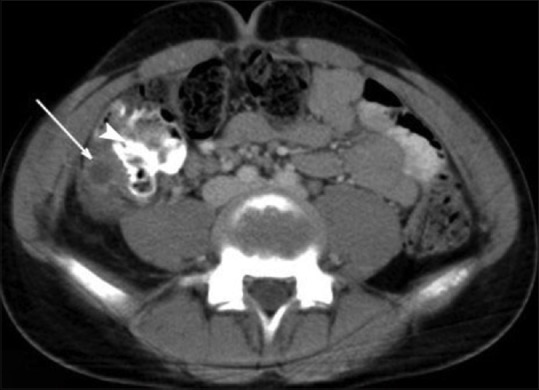
Axial section CT abdomen and pelvis: Arrow showing residual tip of appendix
Figure 2.

Black arrow: Residual appendix. Red arrow: Tip of appendix with blood supply. Violet arrow: Cecum
DISCUSSION
Stump appendicitis is an acute inflammation of the residual appendicular stump which is usually an under-reported, delayed complication of an appendectomy.[3] Rose in 1945 was the first to describe stump appendicitis.[4] There are 37 cases of residual stump appendicitis which had been reported in the published literature, but no study in English literature had mentioned about residual tip appendicitis. The reported interval between surgery and presentation of stump appendicitis varies between few weeks to many years. It many present as acute or subacute appendicitis.[1] This patient presented to us after 3 months of laparoscopic appendectomy. In the last two decades, with the introduction of laparoscopic appendectomy, the incidence of stump appendicitis had increased, which has been reported in many previous studies. The possible causes could be due to initial improper surgical technique or may be contributed by relative increase in number of laparoscopic appendectomies. However, the most recent review by Liang et al. revealed that incidence of stump appendicitis after standardised laparoscopic appendectomy is less than half as compared to open technique.[5] There is a high morbidity rate for stump appendicitis in comparison to the initial episode, due to a combination of delayed diagnosis and high rate of stump-related complications. The incidence of perforation of stump appendicitis is about 70%.[1]
Pre-operative diagnosis of stump appendicitis is difficult because of prior surgical history of appendectomy which usually leads to exclusion of appendicular pathology as differential diagnosis unless a high index of suspicion is exercised. Although ultrasound abdomen can be informatory, the confirmation is usually obtained by cross-sectional imaging studies.[2] CECT features of stump appendicitis can include distended appendiceal stump, pericaecal inflammatory changes, abscess formation, fluid in the right paracolic gutter, caecal wall thickening and sometimes an ileocaecal mass.[6] Diagnostic laparoscopy is useful in some doubtful cases with persistent abdominal symptoms after ruling out other pathologies by doing extensive imaging. It may allow safe completion appendectomy simultaneously if diagnosis of stump appendicitis is confirmed.[7] The completion appendectomy is the treatment of choice for stump appendicitis, most commonly done as an open operation but a successful laparoscopic approach also had been reported in literature.[1] It is recognised that long appendiceal stump and improper identification of stump during appendectomy is the main risk factor for residual appendix.[5] In our case, during previous surgery, stump removal was complete, but the terminal portion of tip of appendix was left behind. Usually, a residual tip will not manifest as it would get sloughed off in view of ischemia, but in certain cases like ours, it can acquire the blood supply from adjacent organs, especially in areas like retrocaecal, paracaecal or sub hepatic locations. If the residual tip is left intact incidentally in such location during an initial appendectomy, it can manifest itself as described above. Mangi and Berger have suggested that the incidence of stump appendicitis can be decreased by proper identification of the base of the appendix and by leaving an appendiceal stump of <3 mm long.[8]
CONCLUSION
Stump appendicitis should be included in differential diagnosis of right-sided abdominal pain, especially with prior history of appendectomy. Clinicians should exercise a high index of suspicion in such cases to avoid morbidity due to delayed diagnosis. Diagnostic laparoscopy can be an important evaluation tool in armamentarium of a surgeon which can contribute for precise diagnosis as well as a therapy. We authors hereby would like to emphasise the importance of complete removal of appendix not only stump part but also tip, especially in certain locations such as paracaecal, retrocaecal and subhepatic.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.O’Leary DP, Myers E, Coyle J, Wilson I. Case report of recurrent acute appendicitis in a residual tip. Cases J. 2010;3:14. doi: 10.1186/1757-1626-3-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Awe JA, Soliman AM, Gourdie RW. Stump appendicitis: An uncompleted surgery, a rare but important entity with potential problems. Case Rep Surg 2013. 2013 doi: 10.1155/2013/972596. 972596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bu-Ali O, Al-Bashir M, Samir HA, Abu-Zidan FM. Stump appendicitis after laparoscopic appendectomy: Case report. Ulus Travma Acil Cerrahi Derg. 2011;17:267–8. doi: 10.5505/tjtes.2011.47123. [DOI] [PubMed] [Google Scholar]
- 4.Sreeramulu PN, Shetty NS, Babu BM, Baig A, Supreeth CS. Stump appendicitis: A bane or boon of laparoscopic appendectomy. World J Laparosc Surg. 2011;4:5–6. [Google Scholar]
- 5.Liang MK, Lo HG, Marks JL. Stump appendicitis: A comprehensive review of literature. The American Surgeon. 2006;72(2):162–6. [PubMed] [Google Scholar]
- 6.Hirano Y, Shimizu J, Kinoshita S, Tatsuzawa Y, Kawaura Y. Stump appendicitis with lipohyperplasia of the ileocecal valve: Report of a case. Indian J Surg. 2004;66:367–9. [Google Scholar]
- 7.Botianu PV, Botianu AM, Boeriu C. Laparoscopic management of stump appendicitis after open appendectomy. J Surg. 2016;12:37–8. [Google Scholar]
- 8.Mangi AA, Berger DL. Stump appendicitis. The American Surgeon. 2000;66(8):739–41. [PubMed] [Google Scholar]


