Abstract
Background
Low socioeconomic and health care access realities of being American Indian/Alaskan Native (AI/AN) in the US combined with decades of data documenting poor cancer outcomes for this population provide a population nested within the US that is analogous to the cancer care landscape of low and middle income countries (LMICs)internationally.
Methods
We reviewed the medical literature with respect to cancer prevention, access to cancer treatment, and access to effective supportive and palliative care for AI/AN populations in the US.
Results
Research confirms poorer cancer outcomes, sub-optimal cancer screening, and high-risk cancer behaviors among AI/AN communities. AI/AN cancer patients are less likely to undergo recommended cancer surgeries and adjuvant chemotherapy and radiation therapy than their white counterparts. Studies including both rural and urban AI cancer survivors revealed barriers to receipt of optimal cancer symptom management and proportionally lower hospice utilization among AI/AN populations. Culturally-tailored programs in targeted communities have been shown to mitigate the observed cancer-related health disparities among AI/AN communities.
Conclusions
There is still much work to be done to improve cancer-related health outcomes in AI/AN communities, and the goals of the providers serving them corresponds with those propelling the growing interest in global oncology equity. Policy work and more funding are needed to continue to build upon the work that the Indian Health Service and established cancer-related health programs have begun in AI/AN communities.
Introduction
Recently, there has emerged growing interest in addressing global disparities in cancer outcomes. Senior colleagues and leaders in oncology have called for attention to remedying the difficulties of providing cancer care in low and middle income countries (LMIC),1 and the importance of radiation oncology. 2 The goal is to expand the focus of the developed world’s oncology community to include countries or societies where such cancer-specific expertise or resources are relatively lacking. Considerable organizational firepower has been mobilized to address this goal. The National Cancer Institute has moved to fund research-minded innovations to delivery of cancer care in LMICs. The American Society of Clinical Oncology (ASCO) recently launched a new journal, the Journal of Global Oncology, a companion publication to its high-impact, premier publications of the Journal Clinical Oncology and Journal of Oncology Practice. In addition, we published a special issue on global cancer disparities for the online Journal, Frontiers In Oncology, with a summary editorial by Petereit and Coleman.2
The movement toward balancing the scales between the “haves” and “have-nots” of cancer care is just and necessary in today’s ever more interconnected world, and commendable given possible headwinds generated by cultural differences and resource inequities. The scope and size of the shortfall is large but economic models for closing the gap for radiation therapy indicate it is not only good for people’s health but is also both cost-effective and economically feasible.3 A preview of possible challenges and models for progress can be obtained by considering the state of cancer care outcomes and care delivery for American Indian/Alaska Native (AI/AN) populations in the US. Furthermore, there is much to be gained by including indigenous and geographically isolated populations with the collective approach to global cancer care.
The 5.2 million AI/AN in the US who belong to among 566 federally-recognized tribes 4 are living the legacy of over 400 years of colonization, geographic displacement, resource appropriation, and varying degrees of cultural assimilation. American Indians/Alaska Natives as a group have the highest poverty rate, 29%, of any racial group in the US, and some of the poorest counties in the US are those that encompass reservation lands 4,5 Unemployment among AI/ANs is over 12% nationally and approaches 90% among some Northern Plains tribes. 6,7 Cancer is the second leading cause of death among AI/ANs nationwide, 8 and disproportionately presents at advanced stages for AI/ANs who are diagnosed with the disease. 9,10 However, per capita funding for the Indian Health Service, the primary system through which many AI/ANs access their health care, was $3099 in 2015 compared to $8097 for the US general population. This perennial underfunding of the US trust responsibility to provide health care to AI/ANs for all health-related needs sets up particular challenges and the need for innovative approaches for providing the highly-coordinated and multidisciplinary care necessary for affecting optimal cancer outcomes. Furthermore, approximately 60% of AI/ANs live in urban settings, many far away from an IHS provider, and 27% of AI/ANs lack health insurance coverage, almost double the national rate. 5,3 Essentially, the low socioeconomic and health care access realities of being AI/AN in the US combined with decades of data documenting poor cancer outcomes for this population provide a population nested within the US that is analogous to the cancer care landscape of LMICs internationally.
Health behaviors, cancer risk, and cancer prevention
Low- or no-income status combined with lack of employment opportunity, historical trauma, and decades of policies that explicitly sought to fracture AI/AN communities through relocation mandates or incentives as a means to facilitate land and resource appropriation together provide rich fuel for perpetuation of social stress which leads to unhealthful lifestyles and high-risk health behaviors. Investigators specifically studying behavioral risk factors in the Northern Plains American Indian populations, where cancer death rates are particularly high, 11,7 have confirmed high rates of diabetes, heart disease, obesity, heavy alcohol use, as well as low rates of cancer screening and physical activity. 12 Analyses of nation-wide samples have confirmed similar findings. 13 The cancer-related health outcome implications of these findings are not theoretical. Research confirms poorer cancer outcomes, suboptimal cancer screening, and high-risk cancer behaviors in areas of low health care access, especially in rural areas and areas that coincide with AI/AN reservations. 14
In addition to the data confirming a need for better primary cancer prevention efforts in AI/AN communities, studies have also examined cancer screening services use. AI/AN consistently show lower rates of cancer screening utilization regardless of the cancer screening test studied or the regional characteristics of cohort studied. 13,15,16 These lower screening rates among AI/AN populations persist even when adjustments are made for income, education, or state of residence. 15 Geographic remoteness from health care provision has been consistently demonstrated as a barrier to cancer screening for AI/AN populations, especially among reservation-based communities. 10,15 This barrier is particularly difficult to address with governmental or philanthropically funded health programs, because most benefactors do not envision their health improvement funds should be used for transportation projects. Consequently, even the best designed and implemented health improvement initiative will falter if the targeted population cannot physically arrive at the location of the intervention. However, some models exist such as Walking Forward, discussed below, that have reached out to these communities with “on site” navigators and telemedicine to mitigate these geographic barriers. 9
Other studies have suggested cultural barriers prevent early accession of cancer care and preventative services in AI/AN communities. Mistrust of health care providers and dissatisfaction with the health care system contribute to disparate cancer outcomes in AI/AN populations. 17,18 These barriers bare relevance to global oncology initiatives in international settings such as Africa or Latin America, where there may be economically marginalized, or geographically remote populations, or those whose experience of colonization engenders a similar wariness of developed-world medical interventions. No amount of “moonshot”-medicine, 19 targeted agents, or high-energy linear accelerators will meaningfully stem the tide of poor cancer outcomes without cultural engagement with these rapidly growing populations both in the US and abroad. It will require culturally-appropriate strategies and relationship-building within communities to improve primary and secondary cancer prevention behaviors. For many individuals in AI/AN and LMIC populations the daily worries include food security, a job that pays a meaningful wage, and physical safety in homes or on streets. The overarching question is: how do we put cancer-related health goals and care back into the context of the lives of the individuals in these populations?
Access to optimal cancer treatment
Once diagnosed with cancer, AI/ANs experience the worst cancer-specific survival rates of any racial/ethnic group in the US. 20,21 This is in part related to the fact that AI/ANs are more likely to have advanced-stage cancer at the time of their cancer diagnosis. 9,7, 22,23 However, there are also notable differences in cancer care processes for AI/AN populations when compared to non-AI/AN populations. Studies of national samples have shown that a relatively lower proportion of AI/ANs receive cancer-directed therapies after cancer diagnosis than non-Hispanic Whites, and, not surprisingly, this is likely related to socioeconomic indicators such as lower income and rural residence. 24 An analysis of the Nationwide Inpatient Sample (the largest all-payer data source for hospital admissions for the US and includes all states except Alaska) of patients admitted to the hospital with cancer diagnoses confirmed that American Indian patients were more likely to live in low income zip codes, more likely to have Medicaid as their payer, and more likely to have their cancer surgeries performed at a rural hospital. 25 American Indians admitted with a cancer diagnosis were also more likely to be admitted for a non-elective procedure. A study using the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) database also revealed that AI/AN patients undergoing cancer surgery were more likely to undergo emergent procedures. 26 This suggests a greater urgency of care for AI cancer patients, a clinical scenario which may preclude multidisciplinary oncologic care planning. The ACS NSQIP study also showed longer length of hospital stay for AI/AN patients undergoing cancer surgery compared to other racial/ethnic groups.26 Analyses of the Surveillance, Epidemiology, and End-Results Medicare linked database revealed that AI/AN patients were actually less likely to undergo cancer surgery at all when compared to other racial/ethnic groups.23 Furthermore, AI/AN patients were less likely to receive recommended adjuvant chemotherapy and radiation therapy for breast, colon, or prostate cancers and generally less likely to receive guideline concordant care overall than their white counterparts.
Access to effective supportive and palliative care
The disparities in cancer management continue beyond up-front and cancer-directed therapy. A qualitative study of both rural and urban American Indian cancer survivors revealed structural (health system-related), physical, and cultural barriers to receiving optimal cancer symptom management. 27 Barriers to symptom management included long wait-times between specialist appointments and transportation difficulties (both rural and urban respondents) and long travel distances to cancer care providers (rural respondents). The need for consultation with multiple specialists combined with transportation difficulties also created hardships with respect to paying for lodging costs and burdens on a patient’s social support network. Cultural barriers to optimal cancer symptom management also included issues with integrating illness beliefs, Native healing practices, and use of traditional healers. Difficulties in communicating with physicians and lack of cancer care knowledge were also cited as barriers.
In the palliative care setting overcoming the barriers to effective cancer symptom management acquires the urgency to provide patient comfort as the end-of-life approaches. American Indian Medicare beneficiaries dying of cancer have proportionally lower rates of hospice utilization than white patients.28 This, in part, reflects the relative lack of hospice programs on or near AI/AN reservations. 29,30 It may also reflect culturally-rooted barriers to effective end-of-life care for AI/AN populations in that such care must incorporate diverse cultural beliefs about death, families, rituals, and communities. 31 For some there will be culturally-informed negative perceptions of discussing death’s approach, 32 while for others a discussion of withdrawing aggressive therapies may be viewed through a lens of perceived discrimination.18 Palliative care cannot be an afterthought to provision of oncology care to diverse cultures, as it is essential to improving quality of life 33,34 and early palliative care can actually prolong survival for some patients with advanced cancer.35 Culturally-appropriate training and tools must be developed, can be effective, 36,37 and require community engagement with AI/AN communities—not unlike the efforts that will be required to provide effective palliative care in LMIC settings internationally.
Models for progress
Fortunately, there are successful models for addressing cancer-related health disparities in AI/AN communities. Petereit and colleagues are entering their second decade of a multi-faceted program, the Walking Forward Program, to reduce stage-at-presentation disparities and increase access to innovative treatments through clinical trials and patient navigation among AI/AN populations in South Dakota. 38,39 Burhannstipanov and colleagues from the Native Navigators and the Cancer Care Continuum (NNACC) have harnessed years of community-based participatory research to create effective cancer education tools for American Indian cancer patients and train patient navigators who provide a critical cultural bridge between these communities and the oncology care setting. 40,41 Marr and colleagues at the University of New Mexico have implemented a successful Palliative Care Consultation Service that uses culturally-tailored communication techniques and incorporates traditional healers in to their consultation workflow. This program has been effective at reducing disparities in hospice utilization among American Indians that are served by their hospital.36
The unifying tenet of successful programs in these communities is that: one-size does not fit all. Cultural issues specific to certain tribes, regional gradients of inequity, geography, and a multitude of other factors contribute to the fact that any program will need to be regionally tailored to serve its target population. Successful programs do have a few common characteristics that can be drawn upon to guide new efforts: 1) they are community-based, engaging individuals who live and work in the target community; and 2) include a period of program development that is dedicated to eliciting needs, barriers, cultural concerns, and explanatory models of illness regarding cancer. Another commonality of successful programs is that they often incorporate the use of patient navigators or community-based health workers. The concept and role of a patient navigator in general oncology practice remains somewhat ill-defined; and whether or not they are worthwhile adjuncts to health care provision continues to be academically debated. However, programs that serve AI/AN communities have been shown to improve screening rates and timely diagnostic follow up of abnormal tests, 42,43 decrease days of cancer treatment interruption, and improve satisfaction with health care. 44,45 Patient navigators in these settings must have agency both within the target population as well as within the health care system to coordinate care and services. They are ideally well-connected to the community they serve, have firm understanding of the barriers encountered by community, and understand the cultural issues well-enough to affect oncology care that fits into the context of the lives of the individuals in the target community.
Some of the key findings and lessons learned from the WF program over a 15 year period include enrolling over 4,000 AIs on various research studies, the establishment of trust within tribal communities, identification of barriers to cancer screening, creation of research infrastructure, higher completion rates and patient satisfaction for patients undergoing cancer treatment, enrollment of patients on trials with excellent clinical outcomes, and the establishment of new research partners which is critical for sustainability. Recent analysis suggests that AI cancer patients with screen-detectable cancers are now presenting with earlier stages of disease and higher cure rates (Peteret, personal communication). We recently completed a smoking cessation trial in which 256 AIs were randomized to various interventions including counseling, nicotine replacement and tailored text messages on cell phones, as the smoking rate is over 50% in this population. We are initiating a lung cancer project that will include education, lung cancer screening, and genomic profiling of non-small-cell-lung cancer (NSCLC) with the goal of developing targeted therapies as the death rate form NSCLs exceeds that of the non-AI population in our area.46
The AI/AN journey toward global oncology equity
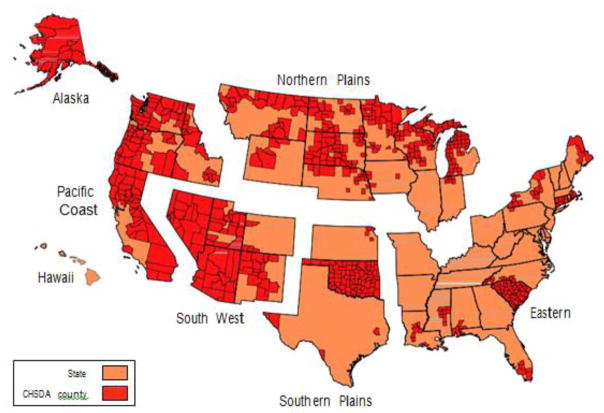
There is still much work to be done to improve cancer-related health outcomes in AI/AN communities, and the goals of the providers serving them corresponds with those propelling the growing interest in global oncology equity. For AI/AN populations, as for many LMIC populations, better data collection is needed,47 both nationally and through local qualitative investigations to target specific interventions and direct policies and funding. Health care system factors continue to present unique challenges for addressing cancer-related disparities for AI/AN populations. Health care for many AI/ANs in the US occurs through a separate system via the Indian Health Service (IHS), and it is charged with providing healthcare for a relatively sicker population than the rest of the US with 38% of the per capita funds. IHS is divided into 6 geographic regions as depicted in Figure 1. Despite these challenges, the quality of care within the IHS, especially as it pertains to preventative services, has steadily improved in recent years, 48 especially as tribal governments have become more involved in the delivery of health care to their people. However, perennial underfunding and continued suboptimal coordination between the IHS and the Medicare and Medicaid programs continue to hinder progress. 48,49,50 Policy work and more funding are needed to continue to build upon the work that IHS and established cancer-related health programs have begun in AI/AN communities. Practitioners doing this work must publish their findings and their experiences so that funders have data upon which to justify continued support. Finally, program leaders must recruit and train new providers to the effort. There are few quick fixes and a good program takes time and work of many dedicated individuals over the course of years.
Figure 1. Indian Health Services (IHS) Regions within the US.
States and Contract Health Service Delivery Area (CHSDA) Counties by Indian Health Service Region: Colorectal Cancer Mortality and Incidence in American Indian/ Alaska Native Persons, 1999–2009.
Common ground in global health
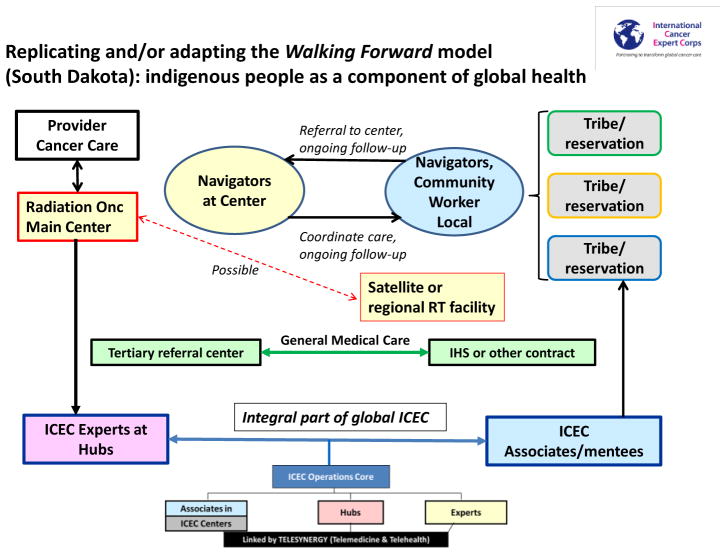
The similarities in the type of general medical health issues of AI/AN and those in LMICs are referred to collectively as the non-communicable diseases: diabetes, heart disease, respiratory diseases and cancer).51 The issues of limited access to cancer care are also similar although the extent of shortfall in radiation therapy is far worse in LMICs with some having almost no capacity. 3 Cultural differences, geographic isolation and need for qualified personnel to assist on-site are issues in common. Described in detail in this issue of Seminars in Radiation Oncology is an emerging program, the International Cancer Expert Corps (ICEC).1 The mission is to establish a mentorship program from resource-rich countries and cancer centers and practices to help educate, train, advise and partner with healthcare providers within LMICs to build sustainable on-site expertise. The Walking Forward (WF) program provided education, mentorship and support for healthcare workers and navigators on the reservation and helped create a cancer care enterprise. The WF program is fortunate to have achieved sustainability over the years, in part due to sheer persistence, dedicated staff who are AI or non-AI who are culturally sensitive, flexibility in partnering with private and public institutions, and trust with tribal communities as many of our staff live on the communities in which they serve. With the similarities in issues, and much to learn about how to implement necessary changes, the benefits from having a critical mass of people with whom to create and exchange ideas and the need for a career path that not only allows for, but also encourages altruistic outreach, ICEC has an indigenous populations group as an integral component of the global cancer care mission and will collaborate with members of the Union for International Cancer Control on programs involving indigenous and aboriginal populations.52
Figure 2 illustrates the similarity between the Walking Forward model and its interactions with the tribes and reservations and the ICEC mentorship model of Experts from a network of “Hubs” in resource-rich settings mentoring Associates in ICEC Centers in LMICs. An overarching concept is that of addressing the enormous need for cancer care to help transform the value systems in healthcare careers by bringing altruistic service as an integral component.53 Expanding cancer services also opens up opportunities for novel technology, telecommunications, better understanding of the impact of genetics and environment on cancer etiology, new means of cancer prevention such as vaccines and the development of a healthcare enterprise with all the supporting activities within the underserved communities. Over the years, the IHS facilities saw the value of WF patient navigators (PN), and as a result, created office space within their hospital for WF PNs to facilitate cancer screening, education, and cancer care coordination with the cancer center in Rapid City. In addition, the cancer center in Rapid City developed a dedicated breast navigator for all newly diagnosed breast cancer patients. In part due to the dedicated breast PN in Rapid City, the breast conservation rates now mirror those of the SEER database since the breast PN program was implemented 10 years ago (Petereit, South Dakota State Medical Journal - in press).
Figure 2. Replicating and/or adapting the model.
The Walking Forward model will be assessed and replicated or adapted for indigenous populations. 39,46. The radiation oncology center provided patient navigators at the center and also helped develop navigators and community health workers at the community level. This facilitated referrals to the center and follow-up care which utilized telemedicine between scheduled visits, which could occur either at the radiation oncology center or in the community. Becoming advocates for cancer care helped the community advocate for better health in general. While not utilized here, an option for geographically remote communities is for the main center to have a “satellite” treatment facility which could enhance access for the majority of treatments, using the main center for specialized technology or procedures. While ICEC is still in development, the main center would function as an ICEC Hub and the community facility would function as an ICEC Center thereby sharing experiences, expertise and models with global partners.
Conclusions
There is a role in the discussion of global oncology for what best addresses the oncology health needs of indigenous populations worldwide. The current experience of AI/AN cancer access and outcomes in the US informs that role. Each global health intervention locus will face its own challenges and require its own deep dive into the social determinants of health for the targeted community. The state of cancer care and outcomes for American Indians and Alaska Natives in the United States not only illuminates challenges this global oncology movement might encounter, but also provides examples of successful models for interventions that bridge cultural and socio-economic divides.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Coleman CN, Formenti SC, Williams TR, et al. The International Cancer Expert Corps: a unique approach for sustainable cancer care in low and lower-middle income countries. Frontiers in Oncology. 2014;4:1–11. doi: 10.3389/fonc.2014.00333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Petereit DG, Coleman CN. Editorial: “Global Challenges in Radiation Oncology”. Frontiers in Oncology. 2015;5:1–4. doi: 10.3389/fonc.2015.00103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Atun R, Jaffray DA, Barton MB, et al. Expanding global access to radiotherapy. The Lancet Oncology. 2015;16:1153–1186. doi: 10.1016/S1470-2045(15)00222-3. [DOI] [PubMed] [Google Scholar]
- 4.Bureau USC; Department of the Interior BoIA, editor. Federal Register. 2015. Indian Entities Recognized and Eligible To Receive Services From the United States Bureau of Indian Affairs; pp. 1942–48. [Google Scholar]
- 5.Bureau USC; Department of the Interior BoIA, editor. Facts for Features: American Indian and Alaska Native Heritage Month: November 2014. 2014. [Google Scholar]
- 6.Statistics USBoL. Labor Force Characteristics by Race and Ethnicity, 2012, BLS Reports (ed Report 1044) 2013. pp. 1–62. [Google Scholar]
- 7.Espey DK, Jim MA, Cobb N, et al. Leading Causes of Death and All-Cause Mortality in American Indians and Alaska Natives. American Journal of Public Health. 2014;104:S303–S311. doi: 10.2105/AJPH.2013.301798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.American Indian & Alaska Native Populations, American Indian & Alaska Native Populations, Centers for Disease Control and Prevention
- 9.Petereit DG, Rogers D, Govern F, et al. Increasing Access to Clinical Cancer Trials and Emerging Technologies for Minority Populations: The Native American Project. Journal of Clinical Oncology. 2004;22:4452–4455. doi: 10.1200/JCO.2004.01.119. [DOI] [PubMed] [Google Scholar]
- 10.Guadagnolo BA, Cina K, Helbig P, et al. Assessing Cancer Stage and Screening Disparities Among Native American Cancer Patients. When Free Primary Care is not Enough. Public Health Reports. 2009;124:79–89. doi: 10.1177/003335490912400111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Espey D, Paisano R, Cobb N. Regional patterns and trends in cancer mortality among American Indians and Alaska Natives, 1990–2001. Cancer. 2005;103:1045–1053. doi: 10.1002/cncr.20876. [DOI] [PubMed] [Google Scholar]
- 12.Holm JE, Vogeltanz-Holm N, Poltavski D, et al. Assessing Health Status, Behavioral Risks, and Health Disparities in American Indians Living on the Northern Plains of the U.S. Public Health Reports. 2010;125:68–78. doi: 10.1177/003335491012500110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Steele CB, Cardinez CJ, Richardson LC, et al. Surveillance for health behaviors of American Indians and Alaska Natives—Findings from the behavioral risk factor surveillance system, 2000–2006. Cancer. 2008;113:1131–1141. doi: 10.1002/cncr.23727. [DOI] [PubMed] [Google Scholar]
- 14.Belasco EJGG, Pence B, Wilkes E. The impact of rural health care accessibility on cancer-related behaviors and outcomes. Applied Health Economics and Health Policy. 2014;12:461–70. doi: 10.1007/s40258-014-0099-4. [DOI] [PubMed] [Google Scholar]
- 15.Towne SD, Smith ML, Ory MG. Geographic variations in access and utilization of cancer screening services: examining disparities among American Indian and Alaska Native Elders. International Journal of Health Geographics. 2014;13:18–18. doi: 10.1186/1476-072X-13-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Filippi MK, N-mF, Braiuca SL, Goodman T, Hammer T. Breast cancer screening perceptions among american indian women under age 40. Journal of Cancer Education. 2013;28:535–40. doi: 10.1007/s13187-013-0499-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Guadagnolo BA, Cina K, Helbig P, et al. Medical Mistrust and Less Satisfaction with Health Care among Native Americans Presenting for Cancer Treatment. J Health Care for Poor and Underserved. 2009;20:210–226. doi: 10.1353/hpu.0.0108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Call KT, McAlpine DD, Johnson PJ. Barriers to care among American Indians in public health care programs. Med Care. 2006;44:595–600. doi: 10.1097/01.mlr.0000215901.37144.94. [DOI] [PubMed] [Google Scholar]
- 19.Joyner M. “Moonshot” Medicine will Let Us Down. NY Times; 2015. [Google Scholar]
- 20.Jemal A, Clegg LX, Ward E, et al. Annual Report to the Nation on the Status of Cancer, 1975–2001, with a Special Feature Regarding Survival. Cancer. 2004;101:3–27. doi: 10.1002/cncr.20288. [DOI] [PubMed] [Google Scholar]
- 21.White MC, Espey DK, Swan J, et al. Disparities in Cancer Mortality and Incidence Among American Indians and Alaska Natives in the United States. American Journal of Public Health. 2014;104:S377–S387. doi: 10.2105/AJPH.2013.301673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Espey DK, Wu X, Swan J, et al. Annual Report to the Nation on the Status of Cancer, 1975–2004, Featuring Cancer in American Indians and Alaska Natives. Cancer. 2007;110:2119–2152. doi: 10.1002/cncr.23044. [DOI] [PubMed] [Google Scholar]
- 23.Javid SH, Varghese TK, Morris AM, et al. Guideline-concordant cancer care and survival among American Indian/Alaskan Native patients. Cancer. 2014;120:2183–2190. doi: 10.1002/cncr.28683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shiovitz S, Bansal A, Burnett-Hartman AN, et al. Cancer-Directed Therapy and Hospice Care for Metastatic Cancer in American Indians and Alaska Natives. Cancer Epidemiology Biomarkers & Prevention. 2015;24:1138–1143. doi: 10.1158/1055-9965.EPI-15-0251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Markin A, Habermann EB, Zhu Y, et al. CAncer surgery among american indians. JAMA Surgery. 2013;148:277–284. doi: 10.1001/jamasurg.2013.1423. [DOI] [PubMed] [Google Scholar]
- 26.Parsons HM, Habermann EB, Stain SC, et al. What Happens to Racial and Ethnic Minorities after Cancer Surgery at American College of Surgeons National Surgical Quality Improvement Program Hospitals? Journal of the American College of Surgeons. 2012;214:539–547. doi: 10.1016/j.jamcollsurg.2011.12.024. [DOI] [PubMed] [Google Scholar]
- 27.Itty TL, Hodge FS, Martinez F. Shared and Unshared Barriers to Cancer Symptom Management Among Urban and Rural American Indians. The Journal of Rural Health. 2014;30:206–213. doi: 10.1111/jrh.12045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Guadagnolo BA, Huo J, Buchholz TA, et al. Disparities in Hospice Utilization among American Indian Medicare Beneficiaries Dying of Cancer. Ethnicity and Disease. 2014;24:393–398. [PubMed] [Google Scholar]
- 29.Organization NHaPC. NHPCO Facts and Figures: Hospice Care in America. PRWeb Newswire; 2012. [Google Scholar]
- 30.Kitzes J, Berger L. End-of-Life Issues for American Indians/Alaska Natives: Insights from One Indian Health Service Area. Journal of Palliative Medicine. 2004;7:830–838. doi: 10.1089/jpm.2004.7.830. [DOI] [PubMed] [Google Scholar]
- 31.Duggleby WK, Samantha, Macleod Rod, Holyoke Paul, Scott Tracy, Holtslander Lorraine, Letendre Angeline, Moeke-Maxwell Tess, Burhansstipanov Linda, Chambers Thane. Indigenous people’s experiences at the end of life. Palliative and Supportive Care. 2015;13:1721–33. doi: 10.1017/S147895151500070X. [DOI] [PubMed] [Google Scholar]
- 32.Carrese JR, Lorna Western bioethics on the Navajo reservation. JAMA. 1995;274:826–829. [PubMed] [Google Scholar]
- 33.Teno JM, Clarridge BR, Casey V, et al. FAmily perspectives on end-of-life care at the last place of care. JAMA. 2004;291:88–93. doi: 10.1001/jama.291.1.88. [DOI] [PubMed] [Google Scholar]
- 34.El-Jawahri AG, Joseph A, Temel Jennifer S. Does Palliative Care Improve Outcomes for Patients with Incurable Illness? A Review of the Evidence. Journal of Supportive Oncology. 2011;9:87–94. doi: 10.1016/j.suponc.2011.03.003. [DOI] [PubMed] [Google Scholar]
- 35.Temel JSG, Joseph A, Muzikansky Alona, Gallagher Emily R, Admane Sonal, Jackson Vicki A, Dahlin Constance M, Blinderman Craig D, Jacobsen Juliet, Pirl William F, Billings J Andrew, Lynch Thomas J. Early Palliative Care for Patients with Metastatic Non–Small-Cell Lung Cancer. New England Journal of Medicine. 2010;363:733–742. doi: 10.1056/NEJMoa1000678. [DOI] [PubMed] [Google Scholar]
- 36.Marr L, Neale D, Wolfe V, et al. Confronting Myths: The Native American Experience in an Academic Inpatient Palliative Care Consultation Program. Journal of Palliative Medicine. 2012;15:71–76. doi: 10.1089/jpm.2011.0197. [DOI] [PubMed] [Google Scholar]
- 37.Arenella CF, Bruce, Domer Timothy, Kaur Judith S, Merriman Melanie P, Ousley Anita. Adaptation, dissemination, and evaluation of a cancer palliative care curriculum for the Indian health system. Journal of palliative care. 2010;26:15–21. [PubMed] [Google Scholar]
- 38.Rogers D, Petereit DG. Cancer Disparities Research Partnership in Lakota Country: Clinical Trials, Patient Services and Community Education for the Oglala, Rosebud and Cheyenne River Sioux Tribes. American Journal of Public Health. 2005;95:1–4. doi: 10.2105/AJPH.2004.053645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Petereit DG, Guadagnolo BA, Wong R, et al. Addressing Cancer Disparities Among American Indians Through Innovative Technologies and Patient Navigation: The Walking Forward Experience. Frontiers in Oncology. 2011;1:1–9. doi: 10.3389/fonc.2011.00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Burhansstipanov L, Krebs L, Dignan M, et al. Findings from the Native Navigators and The Cancer Continuum (NNACC) Study. Journal of Cancer Education. 2014;29:420–427. doi: 10.1007/s13187-014-0694-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Burhansstipanov L, Krebs LU, Harjo L, et al. Providing Community Education: Lessons Learned from Native Patient Navigators. Journal of Cancer Education. 2014;29:596–606. doi: 10.1007/s13187-014-0690-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dignan MB, Burhansstipanov L, Hariton J, et al. A Comparison of Two Native American Navigator Formats: Fact-to-Face and Telephone. Cancer Control. 2005:28–33. doi: 10.1177/1073274805012004S05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Burhansstipanov L, Dignan MB, Bad Wound D, et al. Native American Recruitment into Breast Cancer Screening: The NAWWA Projct. J Cancer Educ. 2000;15:29–33. doi: 10.1080/08858190009528649. [DOI] [PubMed] [Google Scholar]
- 44.Guadagnolo BA, Boylan A, Sargent M, et al. Patient navigation for American Indians undergoing cancer treatment: utilization and impact on care delivery in a regional health care center. Cancer. 2011;117:2754–2761. doi: 10.1002/cncr.25823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Guadagnolo BACK, Koop D, Brunette D, Petereit DG. A pre-post survey analysis of satisfaction with health care and medical mistrust after patient navigation for american indian cancer patients. Journal of Health Care for the Poor and Underserved. 2011;22:1331–43. doi: 10.1353/hpu.2011.0115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Petereit DG, Rogers D, Burhansstipanov L, et al. Walking Forward: The South Dakota Native American Project. Journal of Cancer Education. 2005;20:65–70. doi: 10.1207/s15430154jce2001s_14. [DOI] [PubMed] [Google Scholar]
- 47.Watanabe-Galloway S, Duran T, Stimpson JP, et al. Gaps in Survey Data on Cancer in American Indian and Alaska Native Populations: Examination of US Population Surveys, 1960–2010. Preventing Chronic Disease. 2013;10:E39. doi: 10.5888/pcd10.120258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sequist TD, Cullen T, Bernard K, et al. Trends in Quality of Care and Barriers to Improvement in the Indian Health Service. Journal of General Internal Medicine. 2011;26:480–486. doi: 10.1007/s11606-010-1594-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Warne D, Kaur J, Perdue D. American Indian/Alaska Native Cancer Policy: Systemic Approaches to Reducing Cancer Disparities. Journal of Cancer Education. 2012;27:18–23. doi: 10.1007/s13187-012-0315-6. [DOI] [PubMed] [Google Scholar]
- 50.Burnett-Hartman AN, Bensink ME, Berry K, et al. Access to the Indian Health Service Care System Is Not Associated with Early Enrollment in Medicaid for American Indian and Alaska Natives with Cancer. Cancer Epidemiology Biomarkers & Prevention. 2014;23:362–364. doi: 10.1158/1055-9965.EPI-13-1099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lucas S, Wolfe R. Draft Political Declaration of the High-level Meeting on the prevention and control of non-communicable diseases. United Nations General Assembly; 2011. [Google Scholar]
- 52.Moore SPAS, Colquhoun A, Healy B, Ellison-Loschmann L, Potter JD, Garvey G, Bray F. Cancer incidence in indigenous people in Australia, New Zealand, Canada, and the USA: a comparative population-based study. Lancet Oncology. 2015;16:1483–92. doi: 10.1016/S1470-2045(15)00232-6. [DOI] [PubMed] [Google Scholar]
- 53.Coleman CN, Love RR. Transforming Science, Service, and Society. Science Translational Medicine. 2014;6:1–3. doi: 10.1126/scitranslmed.3009640. [DOI] [PubMed] [Google Scholar]