Abstract
Background
The evidence for treatment decision‐making in emergency general surgery has not been summarized previously. The aim of this overview was to review the quantity and quality of systematic review evidence for the most common emergency surgical conditions.
Methods
Systematic reviews of the most common conditions requiring unplanned admission and treatment managed by general surgeons were eligible for inclusion. The Centre for Reviews and Dissemination databases were searched to April 2014. The number and type (randomized or non‐randomized) of included studies and patients were extracted and summarized. The total number of unique studies was recorded for each condition. The nature of the interventions (surgical, non‐surgical invasive or non‐invasive) was documented. The quality of reviews was assessed using the AMSTAR checklist.
Results
The 106 included reviews focused mainly on bowel conditions (42), appendicitis (40) and gallstone disease (17). Fifty‐one (48·1 per cent) included RCTs alone, 79 (74·5 per cent) included at least one RCT and 25 (23·6 per cent) summarized non‐randomized evidence alone. Reviews included 727 unique studies, of which 30·3 per cent were RCTs. Sixty‐five reviews compared different types of surgical intervention and 27 summarized trials of surgical versus non‐surgical interventions. Fifty‐seven reviews (53·8 per cent) were rated as low risk of bias.
Conclusion
This overview of reviews highlights the need for more and better research in this field.
Short abstract
Evidence still limited
Introduction
Unplanned, urgent and emergency surgery are terms used to describe the work undertaken by surgeons to manage a diverse and challenging group of pathologies linked by the need for unscheduled, non‐elective treatment. Attempts have been made to reach consensus regarding the primary conditions that represent emergency general surgical diagnoses, treated by general surgeons1. They may include upper and lower gastrointestinal tract pathology, hepatopancreatobiliary disease, appendicitis, anorectal soft tissue infections and abdominal wall hernias. These conditions comprise a substantial healthcare burden, accounting for 7 per cent of all US hospital admissions (equating to over 4 million inpatient encounters per year) and 50 per cent of a general surgeon's workload2, 3. In the UK, the most frequently performed emergency general surgical operations are incision and drainage of abscess, appendicectomy and cholecystectomy, whereas abdominal infections and bowel obstructions (with or without ischaemia) contribute the majority of operative workload3. A recent study from the USA4 found that the seven most frequent operations, which accounted for 80 per cent of emergency surgical procedures, were partial colectomy, small bowel resection, cholecystectomy, operative management of peptic ulcer disease, lysis of peritoneal adhesions, appendicectomy and laparotomy. Recent reports from the Royal College of Surgeons of England3, 5 found the delivery of unplanned and urgent general surgical care to be suboptimal with wide variations in outcomes, such as mortality, between hospitals6. Similarly, studies from the USA7, 8 have reported that outcomes of emergency and urgent abdominal surgery are variable and poorly measured. Reports highlighted the urgent need for well designed and conducted research to inform decision‐making, underpin national guidelines and influence health policy7.
The first step towards generating well designed research is to understand the current volume, quality and breadth of evidence. Evidence may take the form of primary research studies, ideally RCTs assessing effectiveness of treatments, health economic evaluations assessing cost‐effectiveness, or diagnostic studies comparing diagnostic procedures. Systematic reviews of evidence enable primary research studies investigating a common question to be summarized and assessed. Overviews of reviews are a recognized method of compiling and assessing the findings from multiple systematic reviews into one accessible and usable summary, which can then be used to identify evidence gaps and prioritize future research9, 10, 11, 12. The aim of this study, therefore, was to undertake an overview of systematic reviews in unplanned general surgery to obtain an understanding of the volume and quality of current evidence.
Methods
This study is the first part of a larger body of work which includes: an overview of reviews of intervention studies; an overview of reviews of diagnostic studies; and a review of economic evaluation and cost‐effectiveness studies in unplanned and urgent general surgery. The review protocol is published in the PROSPERO systematic review register (CRD42015014198)13. Methods relating to the search strategies and study selection (which were common to all 3 parts of this work), and other methods specific to the intervention reviews, are described below.
Inclusion criteria
Systematic reviews of interventions for patients with a condition of interest (see below), requiring unplanned and emergency treatment by general surgeons and published in English, were eligible. A systematic review was defined as one that made a documented attempt to identify studies addressing a research question of interest, with or without a statistical summary of included studies (meta‐analysis).
Participants, conditions and interventions of interest
Unplanned, urgent and emergency general surgery is a large clinical area. This overview therefore focused on the most common conditions managed by general surgeons in emergency settings, based on data from the Hospital Episode Statistics database in the UK14, and the Royal College of Surgeons report3. These are inflammatory, obstructive or ischaemic conditions affecting the small or large bowel; appendicitis; gallstone disease; peptic ulcer disease; anorectal soft tissue infections; and abdominal wall hernias. Reviews of acute trauma treated by general surgeons were excluded. All surgical, non‐surgical invasive (for example radiological and endoscopic) and non‐invasive (such as pharmacological) interventions were included as long as the condition was considered to be managed predominantly by general surgeons. For example, endoscopic or pharmacological interventions for bleeding peptic ulcer disease were excluded (being initially and primarily managed by gastroenterologists), whereas surgical interventions for the same condition were included. Care pathways and interventions for postoperative complications were excluded. Reviews reporting combined details of elective and urgent interventions were excluded unless the results could be extracted separately. Paediatric reviews (patients aged less than 16 years) were excluded. Also excluded were reviews where the sole purpose was to compare patients with different characteristics (such as different disease severity) all undergoing the same intervention.
Search methods for identification of reviews
The following databases were searched from inception to April 2014: DARE (Database of Abstracts of Reviews of Effects), NHS EED (NHS Economic Evaluation Database) and HTA (Health Technology Assessments). In addition, the PROSPERO systematic reviews register was searched within the same time frame. Full search strategies are shown in Appendix S1 (supporting information). No language restrictions were imposed at the search stage. Search hits were downloaded to a citation management program and duplicate records removed.
Data collection and analysis
Selection of reviews
Titles and abstracts of search hits were screened independently by two reviewers with clinical expertise in the conditions of interest. Records with discrepant decisions were rescreened by a senior reviewer whose decision was final. More complex clinical queries were referred to senior members of the research team. Full papers were obtained for all relevant records (including those deemed unclear at the abstract stage) and assessed for inclusion by two reviewers independently, based on prespecified criteria (Appendix S2, supporting information). Disagreements were discussed and, if unresolved, a senior reviewer cast a final decision. When several versions of Cochrane reviews were identified, only the most recent was included. If there was more than one publication of an identical review (for example a Cochrane review and a journal version including the same papers), only the most detailed was included.
Data extraction and management
Data were extracted on a prespecified form that was piloted by two authors (Appendix S3, supporting information). For approximately one‐third of papers, data extraction was completed independently by two reviewers. As agreement was good, for subsequent reviews one reviewer extracted the data and another checked the extraction. Disagreements were resolved as described above.
The following information was extracted: basic bibliographic details; key review methods; start and end dates of the searches; types and number of included studies (RCTs, non‐randomized studies) and patients; the nature of interventions and comparators; and all synthesized outcomes. Where meta‐analyses were available, these were documented. Data were entered and stored in a custom‐made electronic database.
Assessment of methodological quality of the systematic reviews
Before the review began, three tools for quality assessment of reviews were piloted: Overview Quality Assessment Questionnaire (OQAQ)15, AMSTAR (a measurement tool with 11 items, specifically used to assess systematic reviews)16, and one proposed by Li and colleagues12. AMSTAR was selected as it was developed and validated specifically for the assessment of methodological quality of systematic reviews, and was the easiest to apply (Part G; Appendix S3, supporting information). However, it does not provide guidance on how to integrate the 11 items into an overall risk‐of‐bias judgement. A previously described method was therefore used17 in which reviews were considered to be at low risk of bias, and thus of high methodological quality, if the following four items were satisfied: a comprehensive literature search; assessment of the scientific quality of the included studies; appropriate use of quality assessments in formulating review conclusions; and appropriate use of methods to combine findings. Reviews failing to meet one or more of these criteria were considered to be at high risk of bias. If insufficient details were provided to permit judgement on one or more items, a review was deemed to be at unclear risk17. The AMSTAR criteria were applied independently by two reviewers and disagreements resolved through discussion.
Data synthesis
Included reviews were summarized descriptively by each condition, including the number of reviews, and the number and type of included studies (RCTs or non‐randomized studies). Conditions of the small and large bowel are heterogeneous, but they were summarized together because in the emergency setting these conditions (such as bowel obstruction, colitis and diverticulitis) are frequently managed by general surgeons. The number of included patients was documented for each review. To examine the overall volume of evidence, the total number of unique primary studies and their design were recorded for each condition (thus avoiding double‐counting of the same studies cited in multiple reviews). The nature of the interventions (surgical, non‐surgical invasive (endoscopic or radiological) or non‐invasive) was documented and mapped by study design to identify evidence gaps. Details about outcomes of specific reviews are not reported here and will be the focus of subsequent disease‐specific publications.
Results
Searches identified 4362 hits; 607 were considered potentially relevant and, of these, 555 were obtained and read in full. The remaining 52 papers were not assessed; seven could not be obtained (withdrawn, superseded or could not be obtained via an interlibrary loan or from the authors/publishers) and 45 were not written in English. A total of 106 reviews were included (Fig. 1). A full list of excluded studies with reasons is available in Appendix S4 (supporting information).
Figure 1.
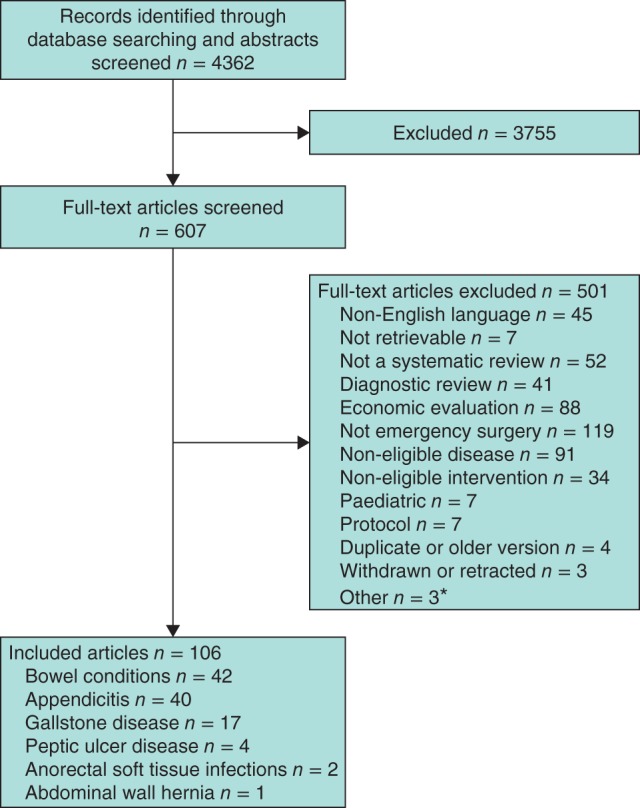
PRISMA flow chart for the overview. *Comparison of patients with different disease severity, all undergoing the same intervention (1) and review not focused on the main intervention for treating the eligible condition (2)
Characteristics of included reviews
The included 106 reviews focused on bowel conditions (42 reviews)18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, appendicitis (40)60, 61, 62, 63, 64, 65, 66, 67, 68, 69, 70, 71, 72, 73, 74, 75, 76, 77, 78, 79, 80, 81, 82, 83, 84, 85, 86, 87, 88, 89, 90, 91, 92, 93, 94, 95, 96, 97, 98, 99, gallstone disease (17)100, 101, 102, 103, 104, 105, 106, 107, 108, 109, 110, 111, 112, 113, 114, 115, 116, peptic ulcer disease (4)117, 118, 119, 120, anorectal soft tissue infections (2)121, 122 and abdominal wall hernias (1)123. The reviews of bowel conditions encompassed a diverse group of conditions that included bowel obstructions, colitis, ischaemia and diverticulitis. The 106 reviews included a median of 8 studies (i.q.r. 5–15), although two reviews33, 66 were empty (no eligible studies were identified). The 106 reviews summarized results from 727 unique papers, of which 220 were RCTs (30·3 per cent). Seventy‐nine reviews (74·5 per cent) included at least one RCT, 51 (48·1 per cent) included exclusively RCTs and 25 (23·6 per cent) summarized solely non‐randomized evidence. The highest number of included RCTs was in reviews of appendicitis (106 of 176 included studies in this category); there were just four unique RCTs in peptic ulcer disease, and none in abdominal wall hernia. The median number of patients included in the reviews varied between conditions, from eight for abdominal wall hernia to 1235 for appendicitis. The median number of patients in the RCTs included in the reviews also varied, from zero for abdominal wall hernia to 701 for appendicitis. Detailed descriptions of the systematic reviews by condition are provided in Table 1.
Table 1.
Descriptions of systematic reviews by condition of interest
| No. of reviews | No. of studies in reviews* | No. of RCTs in reviews | No. of patients in reviews | No. of patients in included RCTs | |
|---|---|---|---|---|---|
| Bowel conditions | 42 | 9 (5–16; 0–98) | 2 (0–4; 0–9) | 509 (233–878; 0–3975) | 78 (0–315; 0–1074) |
| Appendicitis | 40 | 10 (5–17; 0–57) | 5 (1–15; 0–56) | 1235 (744–2277; 0–57 851) | 701 (9–1381; 0–5896) |
| Gallstone disease | 17 | 5 (3–10; 1–53) | 3 (1–6; 0–28) | 488 (272–878; 51–3659) | 388 (63–595; 0–3659) |
| Peptic ulcer disease | 4 | 9 (3–15; 3–15) | 3 (2–4; 2–4) | 487 (296–999; 289–1113) | 252 (178–309; 166–315) |
| Anorectal soft tissue infection | 2 | 6 (5–6; 5–6) | 6 (5–6; 5–6) | 442 (405–479; 405–479) | 442 (405–479; 405–479) |
| Abdominal wall hernia | 1 | 8 | 0 | 8 | 0 |
Values are median (i.q.r.; range).
Includes all types of study design.
Interventions summarized in the reviews
Most reviews summarized studies comparing different types of surgical treatment (65 reviews, 165 unique RCTs) (Table 2). For some conditions (peptic ulcer disease, anorectal soft tissue infections and abdominal wall hernia) no other types of review were identified. Just seven reviews (including 21 unique RCTs) compared different types of non‐invasive treatment, all for bowel conditions managed by general surgeons. Reviews of non‐surgical invasive treatments (such as endoscopic or radiological interventions) were identified only for bowel and gallstone disease, and few reviews examined the evidence for surgical versus non‐surgical treatment (whether invasive or non‐invasive).
Table 2.
Characteristics of included reviews and numbers of RCTs by types of intervention
| Types of intervention compared | ||||||
|---|---|---|---|---|---|---|
| Surgical treatments | Surgery versus non‐surgical invasive treatments | Surgery versus non‐invasive treatments | Non‐surgical invasive versus non‐invasive treatments | Non‐surgical invasive treatments | Non‐invasive treatments | |
| Bowel conditions (42 reviews, 47 RCTs*) | 14 reviews | 14 reviews | 4 reviews | 1 review† | 2 reviews | 7 reviews |
| 8 RCTs | 12 RCTs | 0 RCTs | 0 RCTs | 8 RCTs | 21 RCTs | |
| Appendicitis (40 reviews, 106 RCTs) | 33 reviews | 0 | 7 reviews | 0 | 0 | 0 |
| 100 RCTs | 6 RCTs | |||||
| Gallstone disease (17 reviews, 57 RCTs) | 11 reviews | 2 reviews | 0 | 4 reviews | 0 | 0 |
| 47 RCTs | 3 RCTs‡ | 7 RCTs | ||||
| Peptic ulcer disease (4 reviews, 4 RCTs) | 4 reviews | 0 | 0 | 0 | 0 | 0 |
| 4 RCTs | ||||||
| Anorectal soft tissue infection (2 reviews, 6 RCTs) | 2 reviews | 0 | 0 | 0 | 0 | 0 |
| 6 RCTs | ||||||
| Abdominal wall hernia (1 review, 0 RCTs) | 1 review§ | 0 | 0 | 0 | 0 | 0 |
| 0 RCTs | ||||||
| Total (106 reviews, 220 RCTs) | 65 reviews | 16 reviews | 11 reviews | 5 reviews | 2 reviews | 7 reviews |
| 165 RCTs | 15 RCTs | 6 RCTs | 7 RCTs | 8 RCTs | 21 RCTs | |
Number of reviews and number of unique RCTs included in reviews are shown. Non‐surgical invasive treatments include all endoscopic or radiological procedures; non‐invasive treatments include all pharmacological interventions (such as antibiotics, intravenous fluid regimens).
Two RCTs were included in multiple reviews across two different intervention comparisons (surgical versus surgical treatments and surgical versus non‐surgical invasive treatments) and were therefore included in both intervention categories.
Review included 25 non‐randomized case series (no comparator) reporting outcomes from a total of 315 patients.
Surgery versus radiological treatments.
Review included 17 non‐randomized case series studies (no comparator) reporting outcomes from a total of 28 patients, of which only 8 single‐patient case reports were in emergency settings.
Methodological quality of reviews
The methodological quality of the reviews was variable, meeting between one and ten AMSTAR items (median 7, i.q.r. 5–9). Just over half (57, 53·8 per cent) met all four of the key AMSTAR items and were thus considered at low risk of bias. Common reasons for being assessed as high risk were failure to apply quality assessments of included studies to appropriately formulating review conclusions (31, 29·2 per cent), not assessing the quality of included studies (28, 26·4 per cent), not conducting a comprehensive literature search (16, 15·1 per cent), and using inappropriate methods to combine the studies statistically, or combining when it was not appropriate to do so (30, 28·3 per cent). The majority of reviews (85 of 106, 80·2 per cent) included one or more meta‐analyses. Most reviews (11 of 17) about gallstone disease were rated as low risk of bias, as were the two reviews of anorectal soft tissue infection; the sole hernia review was rated as high risk of bias. Detailed assessments of methodological quality are shown in Table 3.
Table 3.
Critical appraisal of systematic reviews by condition of interest
| AMSTAR criteria | No. of reviews that met specified AMSTAR criteria | |||||
|---|---|---|---|---|---|---|
| Bowel conditions (n = 42) | Appendicitis (n = 40) | Gallstone disease (n = 17) | Peptic ulcer disease (n = 4) | Anorectal soft tissue infection (n = 2) | Abdominal wall hernia (n = 1) | |
| A priori design | 28 | 29 | 15 | 2 | 2 | 0 |
| Duplicate study selection and data extraction | 32 | 32 | 14 | 3 | 2 | 0 |
| Adequate literature search† | 39 | 29 | 16 | 3 | 2 | 1 |
| Inclusion not restricted by publication status | 21 | 20 | 5 | 2 | 1 | 0 |
| Included and excluded studies listed | 15 | 12 | 10 | 1 | 0 | 0 |
| Details of included studies provided | 29 | 31 | 14 | 4 | 2 | 1 |
| Scientific quality of included studies assessed† | 31 | 29 | 14 | 2 | 2 | 0 |
| Conclusions appropriate based on study quality† | 30 | 27 | 14 | 2 | 2 | 0 |
| Appropriate methods to combine study results† | 26 | 35 | 9 | 4 | 2 | 0 |
| Publication bias assessed | 16 | 23 | 10 | 2 | 1 | 0 |
| Conflict of interest included | 8 | 10 | 1 | 4 | 0 | 0 |
| Overall risk of bias rated low‡ | 22 | 20 | 11 | 2 | 2 | 0 |
| No. of AMSTAR criteria met (of 11)* | 6 (1–10) | 7 (1–10) | 8 (2–10) | 6 (3–10) | 10 (10–10) | 2 |
Values are median (range).
Key AMSTAR criteria for assessment of overall risk of bias.
Low risk was assigned to reviews that fulfilled all four key criteria (comprehensive literature search was performed; the scientific quality of the included studies was assessed; these quality assessments were then used appropriately in formulating review conclusions; and the methods used to combine the findings were appropriate).
Discussion
This synthesis included 106 systematic reviews summarizing evidence for unplanned, urgent and emergency general surgery. Although good numbers of reviews were available for bowel conditions and appendicitis (42 and 40 respectively), the summarized evidence for the treatment of emergency hernias and anorectal soft tissue infections was sparse. Evidence from RCTs was most prevalent in reviews of gallstone disease and appendicitis, and least prevalent in bowel conditions. Similarly, gallstone disease and appendicitis had the highest number of large RCTs (over 500 participants). The quality of included reviews was variable, with just over half being rated as low risk of bias. There was a paucity of RCTs comparing surgery and non‐surgical interventions (whether these were invasive or non‐invasive). It is recommended that future research is prioritized in the areas where there are limited numbers of well designed and conducted RCTs and systematic reviews12, 124.
Understanding the state of current evidence and areas where it is lacking is a valuable exercise to map the evidence base, and inform commissioning of primary and secondary research. It also highlights the need to provide educational research opportunities for general surgeons themselves. The observed lack of evidence may be representative of an unfamiliarity with trials, collaborative working and the need for high‐quality evidence. Provision of facilities for research training and opportunities to participate in well designed studies is therefore recommended. Over the past decade this issue has partially been addressed by the Royal College of Surgeons surgical trials initiative125, 126. Several multicentre trainee‐led studies127, 128, 129, 130, 131 have been successfully designed, conducted and reported. Once these trainees complete their surgical training the opportunity for more research will escalate, and the collective experiences and knowledge will equip the surgical community to undertake more difficult trials in the emergency general surgical setting.
Overviews of evidence are an important tool for prioritization of any future research12, 124. Overviews of systematic reviews may provide opportunities for considerable cost savings if their findings are used to focus future research efforts and reduce research waste (for example by identifying that a question has already been answered and does not require further research). The quality of primary studies and their syntheses should be considered in this process. Historically, RCTs have not been undertaken readily in surgery because of methodological issues with blinding and intervention complexity. These are compounded in the emergency surgical setting, with particular challenges to recruitment and data collection132. Although little is known about how to optimize data collection in this setting, a recent study133 has examined the feasibility of collecting patient‐reported outcome data during unplanned hospital admissions. It found that, with specific research support during the working week, good baseline response rates to questionnaires could be achieved.
Another area for further work is to identify whether there are primary RCTs in the areas where no reviews were identified. It is possible that RCTs have been undertaken but not yet reviewed. In some areas the reason for a lack of reviews will be the lack of primary studies, and future work should focus on conducting good‐quality RCTs to provide answers to clinical questions.
Non‐English‐language studies were excluded for logistical reasons and this means that some reviews were likely missed. However, multiple reviews were identified for most topics, usually with overlapping trials. It is thus reasonable to assume that most topics for which reviews are conducted will have at least one review published in English. Some reviews had been published multiple times but the duplicate publications were not always identical. Duplicate publications were removed where possible, but when the two publications differed, both were included.
The evidence base for the care of some patients requiring emergency treatment by general surgeons is poor. Evidence for emergency hernia repair and treatment of anorectal abscess is currently particularly sparse. There is also a lack of comparative evidence to inform clinical decisions regarding invasive versus non‐invasive interventions in this setting, where patients may be high risk and may benefit from less invasive treatment options. Although these types of trial may be particularly difficult to undertake, they are key to influencing practice and should be encouraged. It is therefore recommended that focused and better multicentre studies are undertaken.
Collaborators
J. Savović (J.S.)*, †, N. Blencowe (N.S.B.)* and J. Blazeby (J.M.B.)*,‡, designed the study, wrote the protocol and together led the project, which was conceived by J.M.B.* J.S. and N.S.B. designed the screening and data extraction forms. N.S.B. developed systematic literature searches. J.S. oversaw the review process, resolved discrepancies, constructed tables and figures and wrote the main body of the manuscript. N.S.B., Sean Strong (S.S.)* and Noah Howes (N.H.)* screened abstracts and full papers, resolved discrepancies and checked data extractions. N.S.B. and S.S. made substantial contributions to the writing of the manuscript and tables. J.S., K. Chalmers (K.C.)* and K. Whale* designed the database for data collection and carried out full paper screening and data extraction. K.C. also completed data analyses, managed the database for the review and contributed to the manuscript. N.H., J. Crichton*, L. Gould*, S. Kariyawasam*, J. Mason*, V. Pegna*, S. Richards*, C. Rowlands* and D. Stevens* wrote sections of the study protocol and contributed to the study design, screened abstracts and full papers, extracted data, resolved discrepancies and checked data extractions. All authors read and approved the final manuscript.
*Centre for Surgical Research, School of Social and Community Medicine, University of Bristol, UK; †National Institute for Health Research Collaboration for Leadership in Applied Health Research and Care West, University Hospitals Bristol NHS Foundation Trust, Bristol, UK; ‡Division of Surgery, Head and Neck, University Hospitals Bristol NHS Foundation Trust, Bristol, UK.
Supporting information.
Additional supporting information may be found in the online version of this article:
Appendix S1 Search strategy (Word document)
Appendix S2 Study selection form (Word document)
Appendix S3 Data extraction form (Word document)
Appendix S4 List of excluded studies with reasons (Word document)
Supporting information
Appendix S1 Search strategy
Appendix S2 Study selection form
Appendix S3 Data extraction form
Appendix S4 List of excluded studies with reasons
Acknowledgements
The authors thank A. Jones for data entry work and A. Richards for literature searching. This study received infrastructure support from the Medical Research Council ConDuCT‐II Hub (Collaboration and innovation for Difficult and Complex randomized controlled Trials In Invasive procedures – MR/K025643/1) and the Bristol Royal College of Surgeons of England Surgical Trials Centre. J.S. was funded partly by a NIHR Collaboration for Leadership in Applied Health Research and Care West. N.S.B. is a NIHR Clinical Lecturer and J.M.B. a NIHR Senior Investigator. The views expressed are those of the authors and not necessarily those of the National Health Service, the NIHR or the Department of Health.
Disclosure: The authors declare no conflict of interest.
@csr_bris @BristolUni @CLAHRC_West @JelenaSavovic @blazebyj @natalieblencowe
References
- 1. Shafi S, Aboutanos MB, Agarwal S Jr, Brown CV, Crandall M, Feliciano DV et al Emergency general surgery: definition and estimated burden of disease. J Trauma Acute Care Surg 2013; 74: 1092–1097. [DOI] [PubMed] [Google Scholar]
- 2. Gale SC, Shafi S, Dombrovskiy VY, Arumugam D, Crystal JS. The public health burden of emergency general surgery in the United States: a 10‐year analysis of the Nationwide Inpatient Sample 2001 to 2010. J Trauma Acute Care Surg 2014; 77: 202–208. [DOI] [PubMed] [Google Scholar]
- 3. Royal College of Surgeons of England . Emergency Surgery: Standards for Unscheduled Surgical Care. RCSENG – Professional Standards and Regulation, 2011. https://www.rcseng.ac.uk/library-and-publications/college-publications/docs/emergency-surgery-standards-for-unscheduled-care/ [accessed 9 January 2017]. [Google Scholar]
- 4. Scott JW, Olufajo OA, Brat GA, Rose JA, Zogg CK, Haider AH et al Use of national burden to define operative emergency general surgery. JAMA Surg 2016; 151: e160480. [DOI] [PubMed] [Google Scholar]
- 5. Royal College of Surgeons of England, Department of Health . The Higher Risk Surgical Patient: Towards Improved Care for a Forgotten Group. RCSENG – Professional Standards and Regulation, 2011. https://www.rcseng.ac.uk/library-and-publications/college-publications/docs/the-higher-risk-general-surgical-patient/ [accessed 9 January 2017]. [Google Scholar]
- 6. Saunders DI, Murray D, Pichel AC, Varley S, Peden CJ; UK Emergency Laparotomy Network . Variations in mortality after emergency laparotomy: the first report of the UK Emergency Laparotomy Network. Br J Anaesth 2012; 109: 368–375. [DOI] [PubMed] [Google Scholar]
- 7. Becher RD, Hoth JJ, Miller PR, Mowery NT, Chang MC, Meredith JW. A critical assessment of outcomes in emergency versus nonemergency general surgery using the American College of Surgeons National Surgical Quality Improvement Program database. Am Surg 2011; 77: 951–959. [PubMed] [Google Scholar]
- 8. Becher RD, Meredith JW, Chang MC, Hoth JJ, Beard HR, Miller PR. Creation and implementation of an emergency general surgery registry modeled after the National Trauma Data Bank. J Am Coll Surg 2012; 214: 156–163. [DOI] [PubMed] [Google Scholar]
- 9. Singh JA, Christensen R, Wells GA, Suarez‐Almazor ME, Buchbinder R, Lopez‐Olivo MA et al Biologics for rheumatoid arthritis: an overview of Cochrane reviews. Cochrane Database Syst Rev 2009; (4)CD007848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Cochrane Collaboration . Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0; 2011. http://handbook.cochrane.org/ [accessed 9 January 2017].
- 11. Keus F, Gooszen HG, van Laarhoven CJ. Open, small‐incision, or laparoscopic cholecystectomy for patients with symptomatic cholecystolithiasis. An overview of Cochrane Hepato‐Biliary Group reviews. Cochrane Database Syst Rev 2010; (1)CD008318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Li T, Vedula SS, Scherer R, Dickersin K. What comparative effectiveness research is needed? A framework for using guidelines and systematic reviews to identify evidence gaps and research priorities. Ann Intern Med 2012; 156: 367–377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. University of York Centre for Reviews and Dissemination . Evidence in Emergency Non‐Trauma Gastrointestinal Surgery: Synthesis of Systematic Reviews; 2015. http://www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42015014198 [accessed 9 January 2017].
- 14. Health and Social Care Information Centre . Hospital Episode Statistics, Admitted Patient Care, England – 2012–13; 2013. http://content.digital.nhs.uk/catalogue/PUB12566 [accessed 9 January 2017].
- 15. Oxman AD, Guyatt GH, Singer J, Goldsmith CH, Hutchison BG, Milner RA et al Agreement among reviewers of review articles. J Clin Epidemiol 1991; 44: 91–98. [DOI] [PubMed] [Google Scholar]
- 16. Shea BJ, Hamel C, Wells GA, Bouter LM, Kristjansson E, Grimshaw J et al AMSTAR is a reliable and valid measurement tool to assess the methodological quality of systematic reviews. J Clin Epidemiol 2009; 62: 1013–1020. [DOI] [PubMed] [Google Scholar]
- 17. Potter S, Browning D, Savović J, Holcombe C, Blazeby JM. Systematic review and critical appraisal of the impact of acellular dermal matrix use on the outcomes of implant‐based breast reconstruction. Br J Surg 2015; 102: 1010–1025. [DOI] [PubMed] [Google Scholar]
- 18. Abbas SM, Bissett IP, Parry BR. Meta‐analysis of oral water‐soluble contrast agent in the management of adhesive small bowel obstruction. Br J Surg 2007; 94: 404–411. [DOI] [PubMed] [Google Scholar]
- 19. Watt A, Faragher I, Griffin T, Rieger N, Maddern G. Self‐expanding metallic stents for relieving malignant colorectal obstruction: a systematic review. Ann Surg 2007; 246: 24–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Khanna A, Ognibene SJ, Koniaris LG. Embolization as first‐line therapy for diverticulosis‐related massive lower gastrointestinal bleeding: evidence from a meta‐analysis. J Gastrointest Surg 2005; 9: 343–352. [DOI] [PubMed] [Google Scholar]
- 21. Salem L, Flum DR. Primary anastomosis or Hartmann's procedure for patients with diverticular peritonitis: a systematic review. Dis Colon Rectum 2004; 47: 1953–1964. [DOI] [PubMed] [Google Scholar]
- 22. Kam MH, Tang CL, Chan E, Lim JF, Eu KW. Systematic review of intraoperative colonic irrigation vs. manual decompression in obstructed left‐sided colorectal emergencies. Int J Colorectal Dis 2009; 24: 1031–1037. [DOI] [PubMed] [Google Scholar]
- 23. Sagar J. Colorectal stents for the management of malignant colonic obstructions. Cochrane Database Syst Rev 2011; (11)CD007378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kucukmetin A, Naik R, Galaal K, Bryant A, Dickinson HO. Palliative surgery versus medical management for bowel obstruction in ovarian cancer. Cochrane Database Syst Rev 2010; (7)CD007792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Abbas S, Bissett IP, Parry BR. Oral water soluble contrast for the management of adhesive small bowel obstruction. Cochrane Database Syst Rev 2007; (3)CD004651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Suo T, Gu X, Andersson R, Ma H, Zhang W, Deng W et al Oral traditional Chinese medication for adhesive small bowel obstruction. Cochrane Database Syst Rev 2012; (5)CD008836. [DOI] [PubMed] [Google Scholar]
- 27. Constantinides VA, Tekkis PP, Athanasiou T, Aziz O, Purkayastha S, Remzi FH et al Primary resection with anastomosis vs. Hartmann's procedure in nonelective surgery for acute colonic diverticulitis: a systematic review. Dis Colon Rectum 2006; 49: 966–981. [DOI] [PubMed] [Google Scholar]
- 28. de Korte N, Unlü C, Boermeester MA, Cuesta MA, Vrouenreats BC, Stockmann HB. Use of antibiotics in uncomplicated diverticulitis. Br J Surg 2011; 98: 761–767. [DOI] [PubMed] [Google Scholar]
- 29. Tan CJ, Dasari BV, Gardiner K. Systematic review and meta‐analysis of randomized clinical trials of self‐expanding metallic stents as a bridge to surgery versus emergency surgery for malignant left‐sided large bowel obstruction. Br J Surg 2012; 99: 469–476. [DOI] [PubMed] [Google Scholar]
- 30. Feuer DJ, Broadley KE. Surgery for the resolution of symptoms in malignant bowel obstruction in advanced gynaecological and gastrointestinal cancer. Cochrane Database Syst Rev 2000; (3)CD002764. [DOI] [PubMed] [Google Scholar]
- 31. Abbas S. Resection and primary anastomosis in acute complicated diverticulitis, a systematic review of the literature. Int J Colorectal Dis 2007; 22: 351–357. [DOI] [PubMed] [Google Scholar]
- 32. Khot UP, Lang AW, Murali K, Parker MC. Systematic review of the efficacy and safety of colorectal stents. Br J Surg 2002; 89: 1096–1102. [DOI] [PubMed] [Google Scholar]
- 33. Cirocchi R, Abraha I, Farinella E, Montedori A, Sciannameo F. Laparoscopic versus open surgery in small bowel obstruction. Cochrane Database Syst Rev 2010; (2)CD007511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Branco BC, Barmparas G, Schnüriger B, Inaba K, Chan LS, Demetriades D. Systematic review and meta‐analysis of the diagnostic and therapeutic role of water‐soluble contrast agent in adhesive small bowel obstruction. Br J Surg 2010; 97: 470–478. [DOI] [PubMed] [Google Scholar]
- 35. Feuer DJ, Broadley KE, Shepherd JH, Barton DP. Systematic review of surgery in malignant bowel obstruction in advanced gynecological and gastrointestinal cancer. Gynecol Oncol 1999; 75: 313–322. [DOI] [PubMed] [Google Scholar]
- 36. Ghosheh B, Salameh JR. Laparoscopic approach to acute small bowel obstruction: review of 1061 cases. Surg Endosc 2007; 21: 1945–1949. [DOI] [PubMed] [Google Scholar]
- 37. Feuer DJ, Broadley KE. Systematic review and meta‐analysis of corticosteroids for the resolution of malignant bowel obstruction in advanced gynaecological and gastrointestinal cancers. Ann Oncol 1999; 10: 1035–1041. [DOI] [PubMed] [Google Scholar]
- 38. Tilney HS, Lovegrove RE, Purkayastha S, Sains PS, Weston‐Petrides GK, Darzi AW et al Comparison of colonic stenting and open surgery for malignant large bowel obstruction. Surg Endosc 2007; 21: 225–233. [DOI] [PubMed] [Google Scholar]
- 39. Zhang Y, Shi J, Shi B, Song CY, Xie WF, Chen YX. Self‐expanding metallic stent as a bridge to surgery versus emergency surgery for obstructive colorectal cancer: a meta‐analysis. Surg Endosc 2012; 26: 110–119. [DOI] [PubMed] [Google Scholar]
- 40. Zhang Y, Shi J, Shi B, Song CY, Xie WF, Chen YX. Comparison of efficacy between uncovered and covered self‐expanding metallic stents in malignant large bowel obstruction: a systematic review and meta‐analysis. Colorectal Dis 2012; 14: e367–e374. [DOI] [PubMed] [Google Scholar]
- 41. Breitenstein S, Rickenbacher A, Berdajs D, Puhan M, Clavien PA, Demartines N. Systematic evaluation of surgical strategies for acute malignant left‐sided colonic obstruction. Br J Surg 2007; 94: 1451–1460. [DOI] [PubMed] [Google Scholar]
- 42. Toorenvliet BR, Swank H, Schoones JW, Hamming JF, Bemelman WA. Laparoscopic peritoneal lavage for perforated colonic diverticulitis: a systematic review. Colorectal Dis 2010; 12: 862–867. [DOI] [PubMed] [Google Scholar]
- 43. Bartels SA, Gardenbroek TJ, Ubbink DT, Buskens CJ, Tanis PJ, Bemelman WA. Systematic review and meta‐analysis of laparoscopic versus open colectomy with end ileostomy for non‐toxic colitis. Br J Surg 2013; 100: 726–733. [DOI] [PubMed] [Google Scholar]
- 44. Bhangu A, Nepogodiev D, Gupta A, Torrance A, Singh P; West Midlands Research Collaborative . Systematic review and meta‐analysis of outcomes following emergency surgery for Clostridium difficile colitis. Br J Surg 2012; 99: 1501–1513. [DOI] [PubMed] [Google Scholar]
- 45. Cennamo V, Luigiano C, Coccolini F, Fabbri C, Bassi M, De Caro G et al Meta‐analysis of randomized trials comparing endoscopic stenting and surgical decompression for colorectal cancer obstruction. Int J Colorectal Dis 2013; 28: 855–863. [DOI] [PubMed] [Google Scholar]
- 46. Cirocchi R, Farinella E, Trastulli S, Desiderio J, Listorti C, Boselli C et al Safety and efficacy of endoscopic colonic stenting as a bridge to surgery in the management of intestinal obstruction due to left colon and rectal cancer: a systematic review and meta‐analysis. Surg Oncol 2013; 22: 14–21. [DOI] [PubMed] [Google Scholar]
- 47. Cirocchi R, Trastulli S, Desiderio J, Listorti C, Boselli C, Parisi A et al Treatment of Hinchey stage III–IV diverticulitis: a systematic review and meta‐analysis. Int J Colorectal Dis 2013; 28: 447–457. [DOI] [PubMed] [Google Scholar]
- 48. Currie A, Christmas C, Aldean H, Mobasheri M, Bloom IT. Systematic review of self‐expanding stents in the management of benign colorectal obstruction. Colorectal Dis 2014; 16: 239–245. [DOI] [PubMed] [Google Scholar]
- 49. De Ceglie A, Filiberti R, Baron TH, Ceppi M, Conio M. A meta‐analysis of endoscopic stenting as bridge to surgery versus emergency surgery for left‐sided colorectal cancer obstruction. Crit Rev Oncol Hematol 2013; 88: 387–403. [DOI] [PubMed] [Google Scholar]
- 50. Huang X, Lv B, Zhang S, Meng L. Preoperative colonic stents versus emergency surgery for acute left‐sided malignant colonic obstruction: a meta‐analysis. J Gastrointest Surg 2014; 18: 584–591. [DOI] [PubMed] [Google Scholar]
- 51. Li MZ, Lian L, Xiao LB, Wu WH, He YL, Song XM. Laparoscopic versus open adhesiolysis in patients with adhesive small bowel obstruction: a systematic review and meta‐analysis. Am J Surg 2012; 204: 779–786. [DOI] [PubMed] [Google Scholar]
- 52. Liang TW, Sun Y, Wei YC, Yang DX. Palliative treatment of malignant colorectal obstruction caused by advanced malignancy: a self‐expanding metallic stent or surgery? A system review and meta‐analysis. Surg Today 2014; 44: 22–33. [DOI] [PubMed] [Google Scholar]
- 53. Liu Z, Kang L, Li C, Huang M, Zhang X, Wang J. Meta‐analysis of complications of colonic stenting versus emergency surgery for acute left‐sided malignant colonic obstruction. Surg Laparosc Endosc Percutan Tech 2014; 24: 73–79. [DOI] [PubMed] [Google Scholar]
- 54. Shabanzadeh DM, Wille‐Jørgensen P. Antibiotics for uncomplicated diverticulitis. Cochrane Database Syst Rev 2012; (11)CD009092. [DOI] [PubMed] [Google Scholar]
- 55. Stewart DB, Hollenbeak CS, Wilson MZ. Is colectomy for fulminant Clostridium difficile colitis life saving? A systematic review. Colorectal Dis 2013; 15: 798–804. [DOI] [PubMed] [Google Scholar]
- 56. Toro A, Mannino M, Reale G, Cappello G, Di Carlo I. Primary anastomosis vs Hartmann procedure in acute complicated diverticulitis. Evolution over the last twenty years. Chirurgia (Bucur) 2012; 107: 598–604. [PubMed] [Google Scholar]
- 57. Yang Z, Wu Q, Wang F, Ye X, Qi X, Fan D. A systematic review and meta‐analysis of randomized trials and prospective studies comparing covered and bare self‐expandable metal stents for the treatment of malignant obstruction in the digestive tract. Int J Med Sci 2013; 10: 825–835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Ye GY, Cui Z, Chen L, Zhong M. Colonic stenting vs emergent surgery for acute left‐sided malignant colonic obstruction: a systematic review and meta‐analysis. World J Gastroenterol 2012; 18: 5608–5615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Zhao XD, Cai BB, Cao RS, Shi RH. Palliative treatment for incurable malignant colorectal obstructions: a meta‐analysis. World J Gastroenterol 2013; 19: 5565–5574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Ansaloni L, Catena F, Coccolini F, Ercolani G, Gazzotti F, Pasqualini E et al Surgery versus conservative antibiotic treatment in acute appendicitis: a systematic review and meta‐analysis of randomized controlled trials. Dig Surg 2011; 28: 210–221. [DOI] [PubMed] [Google Scholar]
- 61. Sajid MS, Khan MA, Cheek E, Baig MK. Needlescopic versus laparoscopic appendectomy: a systematic review. Can J Surg 2009; 52: 129–134. [PMC free article] [PubMed] [Google Scholar]
- 62. Chung RS, Rowland DY, Li P, Diaz J. A meta analysis of randomized controlled trials of laparoscopic versus conventional appendectomy. Am J Surg 1999; 177: 250–256. [DOI] [PubMed] [Google Scholar]
- 63. Varadhan KK, Neal KR, Lobo DN. Safety and efficacy of antibiotics compared with appendicectomy for treatment of uncomplicated acute appendicitis: meta‐analysis of randomised controlled trials. BMJ 2012; 344: e2156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Gorenoi V, Dintsios CM, Schoenermark MP, Hagen A. Laparoscopic Versus Open Appendectomy – A Systematic Review of Medical Efficacy and Health Economic Analysis. German Agency for Health Technology Assessment at the German Institute for Medical Documentation and Information: Cologne, 2006. [Google Scholar]
- 65. Bennett J, Boddy A, Rhodes M. Choice of approach for appendicectomy: a meta‐analysis of open versus laparoscopic appendicectomy. Surg Laparosc Endosc Percutan Tech 2007; 17: 245–255. [DOI] [PubMed] [Google Scholar]
- 66. Rehman H, Rao AM, Ahmed I. Single incision versus conventional multi‐incision appendicectomy for suspected appendicitis. Cochrane Database Syst Rev 2011; (7)CD009022. [DOI] [PubMed] [Google Scholar]
- 67. Southgate E, Vousden N, Karthikesalingam A, Markar SR, Black S, Zaidi A. Laparoscopic vs open appendectomy in older patients. Arch Surg 2012; 147: 557–562. [DOI] [PubMed] [Google Scholar]
- 68. McCall JL, Sharples K, Jadallah F. Systematic review of randomized controlled trials comparing laparoscopic with open appendicectomy. Br J Surg 1997; 84: 1045–1050. [PubMed] [Google Scholar]
- 69. Sajid MS, Rimple J, Cheek E, Baig MK. Use of endo‐GIA versus endo‐loop for securing the appendicular stump in laparoscopic appendicectomy: a systematic review. Surg Laparosc Endosc Percutan Tech 2009; 19: 11–15. [DOI] [PubMed] [Google Scholar]
- 70. Golub R, Siddiqui F, Pohl D. Laparoscopic versus open appendectomy: a metaanalysis. J Am Coll Surg 1998; 186: 545–553. [DOI] [PubMed] [Google Scholar]
- 71. Markides G, Subar D, Riyad K. Laparoscopic versus open appendectomy in adults with complicated appendicitis: systematic review and meta‐analysis. World J Surg 2010; 34: 2026–2040. [DOI] [PubMed] [Google Scholar]
- 72. Wei B, Qi CL, Chen TF, Zheng ZH, Huang JL, Hu BG et al Laparoscopic versus open appendectomy for acute appendicitis: a metaanalysis. Surg Endosc 2011; 25: 1199–1208. [DOI] [PubMed] [Google Scholar]
- 73. Varadhan KK, Humes DJ, Neal KR, Lobo DN. Antibiotic therapy versus appendectomy for acute appendicitis: a meta‐analysis. World J Surg 2010; 34: 199–209. [DOI] [PubMed] [Google Scholar]
- 74. Sauerland S, Lefering R, Holthausen U, Neugebauer E. A meta‐analysis of studies comparing laparoscopic with conventional appendectomy In Progress in Surgery. Acute Appendicitis: Standard Treatment or Laparoscopic Surgery, Krähenbühl L, Frei E, Klaiber C, Büchler MW. (eds). Kluwer Publishers: Dordrecht, 1997: 109–114. [Google Scholar]
- 75. Sauerland S, Jaschinski T, Neugebauer EAM. Laparoscopic versus open surgery for suspected appendicitis. Cochrane Database Syst Rev 2010; (10)CD001546. [DOI] [PubMed] [Google Scholar]
- 76. Mason RJ, Moazzez A, Sohn H, Katkhouda N. Meta‐analysis of randomized trials comparing antibiotic therapy with appendectomy for acute uncomplicated (no abscess or phlegmon) appendicitis. Surg Infect (Larchmt) 2012; 13: 74–84. [DOI] [PubMed] [Google Scholar]
- 77. Henry MC, Moss RL. Primary versus delayed wound closure in complicated appendicitis: an international systematic review and meta‐analysis. Pediatr Surg Int 2005; 21: 625–630. [DOI] [PubMed] [Google Scholar]
- 78. Simillis C, Symeonides P, Shorthouse AJ, Tekkis PP. A meta‐analysis comparing conservative treatment versus acute appendectomy for complicated appendicitis (abscess or phlegmon). Surgery 2010; 147: 818–829. [DOI] [PubMed] [Google Scholar]
- 79. Sauerland S, Lefering R, Holthausen U, Neugebauer EA. Laparoscopic vs conventional appendectomy: a meta‐analysis of randomised controlled trials. Langenbeck Arch Chir 1998; 383: 289–295. [DOI] [PubMed] [Google Scholar]
- 80. Temple LK, Litwin DE, McLeod RS. A meta‐analysis of laparoscopic versus open appendectomy in patients suspected of having acute appendicitis. Can J Surg 1999; 42: 377–383. [PMC free article] [PubMed] [Google Scholar]
- 81. Wilms IM, de Hoog DE, de Visser DC, Janzing HM. Appendectomy versus antibiotic treatment for acute appendicitis. Cochrane Database Syst Rev 2011; (11)CD008359. [DOI] [PubMed] [Google Scholar]
- 82. Kim CB, Kim MS, Hong J, Lee HY, Yu SH. Is laparoscopic appendectomy useful for the treatment of acute appendicitis in Korea: a meta‐analysis. Yonsei Med J 2004; 45: 7–16. [DOI] [PubMed] [Google Scholar]
- 83. Li X, Zhang J, Sang L, Zhang W, Chu Z, Li X et al Laparoscopic versus conventional appendectomy: a meta‐analysis of randomized controlled trials. BMC Gastroenterol 2010; 10: 129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Kazemier G, in't Hof KH, Saad S, Bonjer HJ, Sauerland S. Securing the appendiceal stump in laparoscopic appendectomy: evidence for routine stapling? Surg Endosc 2006; 20: 1473–1476. [DOI] [PubMed] [Google Scholar]
- 85. Garbutt JM, Soper NJ, Shannon WD, Botero A, Littenberg B. Meta‐analysis of randomized controlled trials comparing laparoscopic and open appendectomy. Surg Laparosc Endosc 1999; 9: 17–26. [PubMed] [Google Scholar]
- 86. Markar SR, Venkat‐Raman V, Ho A, Karthikesalingam A, Kinross J, Evans J et al Laparoscopic versus open appendicectomy in obese patients. Int J Surg 2011; 9: 451–455. [DOI] [PubMed] [Google Scholar]
- 87. Antoniou SA, Koch OO, Antoniou GA, Lasithiotakis K, Chalkiadakis GE, Pointner R et al Meta‐analysis of randomized trials on single‐incision laparoscopic versus conventional laparoscopic appendectomy. Am J Surg 2014; 207: 613–622. [DOI] [PubMed] [Google Scholar]
- 88. Cai YL, Xiong XZ, Wu SJ, Cheng Y, Lu J, Zhang J et al Single‐incision laparoscopic appendectomy vs conventional laparoscopic appendectomy: systematic review and meta‐analysis. World J Gastroenterol 2013; 19: 5165–5173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Ciarrocchi A, Amicucci G. Laparoscopic versus open appendectomy in obese patients: a meta‐analysis of prospective and retrospective studies. J Minim Access Surg 2014; 10: 4–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Ding J, Xia Y, Zhang ZM, Liao GQ, Pan Y, Liu S et al Single‐incision versus conventional three‐incision laparoscopic appendicectomy for appendicitis: a systematic review and meta‐analysis. J Pediatr Surg 2013; 48: 1088–1098. [DOI] [PubMed] [Google Scholar]
- 91. Gao J, Li P, Li Q, Tang D, Wang DR. Comparison between single‐incision and conventional three‐port laparoscopic appendectomy: a meta‐analysis from eight RCTs. Int J Colorectal Dis 2013; 28: 1319–1327. [DOI] [PubMed] [Google Scholar]
- 92. Gill RS, Shi X, Al‐Adra DP, Birch DW, Karmali S. Single‐incision appendectomy is comparable to conventional laparoscopic appendectomy: a systematic review and pooled analysis. Surg Laparosc Endosc Percutan Tech 2012; 22: 319–327. [DOI] [PubMed] [Google Scholar]
- 93. Hua J, Gong J, Xu B, Yang T, Song Z. Single‐incision versus conventional laparoscopic appendectomy: a meta‐analysis of randomized controlled trials. J Gastrointest Surg 2014; 18: 426–436. [DOI] [PubMed] [Google Scholar]
- 94. Li P, Chen ZH, Li QG, Qiao T, Tian YY, Wang DR. Safety and efficacy of single‐incision laparoscopic surgery for appendectomies: a meta‐analysis. World J Gastroenterol 2013; 19: 4072–4082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Markar SR, Karthikesalingam A, Di Franco F, Harris AM. Systematic review and meta‐analysis of single‐incision versus conventional multiport appendicectomy. Br J Surg 2013; 100: 1709–1718. [DOI] [PubMed] [Google Scholar]
- 96. Ohtani H, Tamamori Y, Arimoto Y, Nishiguchi Y, Maeda K, Hirakawa K. Meta‐analysis of the results of randomized controlled trials that compared laparoscopic and open surgery for acute appendicitis. J Gastrointest Surg 2012; 16: 1929–1939. [DOI] [PubMed] [Google Scholar]
- 97. Pisanu A, Porceddu G, Reccia I, Saba A, Uccheddu A. Meta‐analysis of studies comparing single‐incision laparoscopic appendectomy and conventional multiport laparoscopic appendectomy. J Surg Res 2013; 183: e49–e59. [DOI] [PubMed] [Google Scholar]
- 98. Qiu J, Yuan H, Chen S, He Z, Wu H. Single‐port laparoscopic appendectomy versus conventional laparoscopic appendectomy: evidence from randomized controlled trials and nonrandomized comparative studies. Surg Laparosc Endosc Percutan Tech 2014; 24: 12–21. [DOI] [PubMed] [Google Scholar]
- 99. Wilasrusmee C, Sukrat B, McEvoy M, Attia J, Thakkinstian A. Systematic review and meta‐analysis of safety of laparoscopic versus open appendicectomy for suspected appendicitis in pregnancy. Br J Surg 2012; 99: 1470–1478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Antoniou SA, Antoniou GA, Makridis C. Laparoscopic treatment of Mirizzi syndrome: a systematic review. Surg Endosc 2010; 24: 33–39. [DOI] [PubMed] [Google Scholar]
- 101. Papi C, Catarci M, D'Ambrosio L, Gili L, Koch M, Grassi GB et al Timing of cholecystectomy for acute calculous cholecystitis: a meta‐analysis. Am J Gastroenterol 2004; 99: 147–155. [DOI] [PubMed] [Google Scholar]
- 102. Uy MC, Daez ML, Sy PP, Banez VP, Espinosa WZ, Talingdan‐Te MC. Early ERCP in acute gallstone pancreatitis without cholangitis: a meta‐analysis. JOP 2009; 10: 299–305. [PubMed] [Google Scholar]
- 103. Gurusamy K, Samraj K, Gluud C, Wilson E, Davidson BR. Meta‐analysis of randomized controlled trials on the safety and effectiveness of early versus delayed laparoscopic cholecystectomy for acute cholecystitis. Br J Surg 2010; 97: 141–150. [DOI] [PubMed] [Google Scholar]
- 104. Petrov MS, van Santvoort HC, Besselink MG, van der Heijden GJ, van Erpecum KJ, Gooszen HG. Early endoscopic retrograde cholangiopancreatography versus conservative management in acute biliary pancreatitis without cholangitis: a meta‐analysis of randomized trials. Ann Surg 2008; 247: 250–257. [DOI] [PubMed] [Google Scholar]
- 105. Tse F, Yuan Y. Early routine endoscopic retrograde cholangiopancreatography strategy versus early conservative management strategy in acute gallstone pancreatitis. Cochrane Database Syst Rev 2012; (5)CD009779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Moretti A, Papi C, Aratari A, Festa V, Tanga M, Koch M et al Is early endoscopic retrograde cholangiopancreatography useful in the management of acute biliary pancreatitis? A meta‐analysis of randomized controlled trials. Dig Liver Dis 2008; 40: 379–385. [DOI] [PubMed] [Google Scholar]
- 107. Gurusamy KS, Samraj K. Routine abdominal drainage for uncomplicated open cholecystectomy. Cochrane Database Syst Rev 2007; (2)CD006003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Gurusamy KS, Samraj K, Fusai G, Davidson BR. Early versus delayed laparoscopic cholecystectomy for biliary colic. Cochrane Database Syst Rev 2008; (4)CD007196. [DOI] [PubMed] [Google Scholar]
- 109. Siddiqui T, MacDonald A, Chong PS, Jenkins JT. Early versus delayed laparoscopic cholecystectomy for acute cholecystitis: a meta‐analysis of randomized clinical trials. Am J Surg 2008; 195: 40–47. [DOI] [PubMed] [Google Scholar]
- 110. Winbladh A, Gullstrand P, Svanvik J, Sandström P. Systematic review of cholecystostomy as a treatment option in acute cholecystitis. HPB (Oxford) 2009; 11: 183–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Lau H, Lo CY, Patil NG, Yuen WK. Early versus delayed‐interval laparoscopic cholecystectomy for acute cholecystitis: a metaanalysis. Surg Endosc 2006; 20: 82–87. [DOI] [PubMed] [Google Scholar]
- 112. Gurusamy KS, Davidson C, Gluud C, Davidson BR. Early versus delayed laparoscopic cholecystectomy for people with acute cholecystitis. Cochrane Database Syst Rev 2013; (6)CD005440. [DOI] [PubMed] [Google Scholar]
- 113. Gurusamy KS, Nagendran M, Davidson BR. Early versus delayed laparoscopic cholecystectomy for acute gallstone pancreatitis. Cochrane Database Syst Rev 2013; (9)CD010326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Gurusamy KS, Rossi M, Davidson BR. Percutaneous cholecystostomy for high‐risk surgical patients with acute calculous cholecystitis. Cochrane Database Syst Rev 2013; (8)CD007088. [DOI] [PubMed] [Google Scholar]
- 115. Randial Pérez LJ, Fernando Parra J, Aldana Dimas G. The safety of early laparoscopic cholecystectomy (< 48 hours) for patients with mild gallstone pancreatitis: a systematic review of the literature and meta‐analysis. Cir Esp 2014; 92: 107–113. [DOI] [PubMed] [Google Scholar]
- 116. van Baal MC, Besselink MG, Bakker OJ, van Santvoort HC, Schaapherder AF, Nieuwenhuijs VB et al Timing of cholecystectomy after mild biliary pancreatitis: a systematic review. Ann Surg 2012; 255: 860–866. [DOI] [PubMed] [Google Scholar]
- 117. Lunevicius R, Morkevicius M. Systematic review comparing laparoscopic and open repair for perforated peptic ulcer. Br J Surg 2005; 92: 1195–1207. [DOI] [PubMed] [Google Scholar]
- 118. Lau H. Laparoscopic repair of perforated peptic ulcer: a meta‐analysis. Surg Endosc 2004; 18: 1013–1021. [DOI] [PubMed] [Google Scholar]
- 119. Antoniou SA, Antoniou GA, Koch OO, Pointner R, Granderath FA. Meta‐analysis of laparoscopic versus open repair of perforated peptic ulcer. JSLS 2013; 17: 15–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Sanabria A, Villegas MI, Morales Uribe CH. Laparoscopic repair for perforated peptic ulcer disease. Cochrane Database Syst Rev 2013; (2)CD004778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121. Quah HM, Tang CL, Eu KW, Chan SY, Samuel M. Meta‐analysis of randomized clinical trials comparing drainage alone vs primary sphincter‐cutting procedures for anorectal abscess‐fistula. Int J Colorectal Dis 2006; 21: 602–609. [DOI] [PubMed] [Google Scholar]
- 122. Malik AI, Nelson RL, Tou S. Incision and drainage of perianal abscess with or without treatment of anal fistula. Cochrane Database Syst Rev 2010; (7)CD006827. [DOI] [PubMed] [Google Scholar]
- 123. Deeba S, Purkayastha S, Darzi A, Zacharakis E. Obturator hernias: a review of the laparoscopic approach. J Minim Access Surg 2011; 7: 201–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Moher D, Glasziou P, Chalmers I, Nasser M, Bossuyt PM, Korevaar DA et al Increasing value and reducing waste in biomedical research: who's listening? Lancet 2016; 387: 1573–1586. [DOI] [PubMed] [Google Scholar]
- 125. Royal College of Surgeons . The Rosetrees and the RCS Surgical Trials Initiative https://www.rcseng.ac.uk/standards-and-research/research/surgical-trials-initiative/ [accessed 9 January 2017].
- 126. Bhangu A, Kolias AG, Pinkney T, Hall NJ, Fitzgerald JE. Surgical research collaboratives in the UK. Lancet 2013; 382: 1091–1092. [DOI] [PubMed] [Google Scholar]
- 127. Pinkney TD, Calvert M, Bartlett DC, Gheorghe A, Redman V, Dowswell G et al; West Midlands Research Collaborative; ROSSINI Trial Investigators. Impact of wound edge protection devices on surgical site infection after laparotomy: multicentre randomised controlled trial (ROSSINI Trial). BMJ 2013; 347: f4305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Strong S, Blencowe N, Bhangu A; National Surgical Research Collaborative . How good are surgeons at identifying appendicitis? Results from a multi‐centre cohort study. Int J Surg 2015; 15: 107–112. [DOI] [PubMed] [Google Scholar]
- 129. United Kingdom National Surgical Research Collaborative , Bhangu A. Safety of short, in‐hospital delays before surgery for acute appendicitis: multicentre cohort study, systematic review, and meta‐analysis. Ann Surg 2014; 259: 894–903. [DOI] [PubMed] [Google Scholar]
- 130. National Surgical Research Collaborative . Multicentre observational study of performance variation in provision and outcome of emergency appendicectomy. Br J Surg 2013; 100: 1240–1252. [DOI] [PubMed] [Google Scholar]
- 131. Rowlands C, Griffiths SN, Blencowe NS, Brown A, Hollowood A, Hornby ST et al Surgical ward rounds in England: a trainee‐led multi‐centre study of current practice. Patient Saf Surg 2014; 8: 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132. Stevens DJ, Blencowe NS, McElnay PJ, Macefield RC, Savović J, Avery KN et al A systematic review of patient‐reported outcomes in randomized controlled trials of unplanned general surgery. World J Surg 2016; 40: 267–276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133. Mason J, Blencowe NS, McNair AGK, Stevens DJ, Avery KN, Pullyblank AM et al Investigating the collection and assessment of patient‐reported outcome data amongst unplanned surgical hospital admissions: a feasibility study. Pilot Feasibility Stud 2015; 1: 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1 Search strategy
Appendix S2 Study selection form
Appendix S3 Data extraction form
Appendix S4 List of excluded studies with reasons


