Abstract
Aim
Guidance on reducing the risk of sudden infant death syndrome (SIDS) was successfully introduced to a number of countries in the early 1990s. The most important recommendations were supine sleeping for infants and non‐smoking for mothers. This 2012–2014 study examined adherence to the national Swedish SIDS advice.
Methods
We asked 1000 parents with infants registered at child healthcare centres in western Sweden to complete a questionnaire on infant care from birth to 12 months of age.
Results
We analysed 710 responses and found that, in the first three months, 1.3% of the infants were placed in the prone sleeping position and 14.3% were placed on their side. By three to five months, this had risen to 5.6% and 23.6%. In the first three months, 83.1% were breastfed, 84.1% used a pacifier and 44.2% shared their parents' bed, while 5.8% slept in another room. Bed sharing was more likely if infants were breastfed and less likely if they used pacifiers. During pregnancy, 2.8% of the mothers smoked and the mothers who had smoked during pregnancy were less likely to bed share.
Conclusion
Overall adherence to the SIDS advice was good, but both prone and side sleeping practices should be targeted.
Keywords: Bed sharing, Prone sleeping position, Side sleeping position, Smoking, Sudden infant death syndrome
Key notes.
National guidance has lowered sudden infant death syndrome (SIDS) rates in Sweden, but information on adherence was lacking.
Our 2012–2014 study of 710 infants showed that, in the first three months, 1.3% of the infants were placed in the prone sleeping position, 14.3% were placed on their side and 44.2% slept in their parents' bed.
Adherence to SIDS advice was good, but both prone and side sleeping practices should be targeted.
Introduction
During the 1980s, it was common for infants in the Western world to be placed in a prone sleeping position. However, when pivotal case–control studies demonstrated that prone sleeping increased the risk of sudden infant death syndrome (SIDS), parents were advised to change to a supine sleeping position 1, 2, 3. This change in sleep position was followed by a dramatic decline in the worldwide incidence of SIDS 4.
One of the organisations that advised against prone sleeping was the National Board of Health and Welfare in Sweden, and its guidance, issued in 1992 5, resulted in a rapid reduction in the incidence of SIDS in the country 6. That recommendation was soon followed by advice on not smoking. Furthermore, parents were advised that overheating should be avoided, the infant's ability to move should not be impeded and mothers should breastfeed if possible. As time passed, the advice was updated and the current Swedish advice to reduce the risk of SIDS, which was last updated in December 2013 7, 8, is that:
The infant should sleep on its back.
Smoking and nicotine should be avoided.
The infant's face should be kept free, overheating should be avoided and the infant's movement should not be impeded.
The safest place for an infant under three months of age to sleep is in its own cot.
Mothers should breastfeed if possible.
A pacifier (dummy) can be used when the infant is going to sleep.
The national guidance, and the changes that took place partway through the 2012–2014 study period in December 2013, are discussed in more detail in the Methods section.
Providing Swedish parents with advice on how to reduce the risk of SIDS has been so successful that the incidence declined from 1.12 per 1000 births in 1991 to an average of 0.2 per 1000 births during the last decade 6, 9. This preventive advice has been provided by maternal and child healthcare services, and we know that more than 99% of the targeted population use these services when they have a child. However, we had no information about to what extent parents followed the advice they were given to reduce the risk of SIDS, because official data on the prevalence of important SIDS risk factors, such as sleeping arrangements, were lacking in Sweden. Therefore, the aim of this study was to examine to what extent the recommendations were followed by parents and to see if there was room for improvement.
Methods
Setting
Between April 2012 and October 2014, child healthcare (CHC) nurses asked 1000 families with infants of up to 12 months of age to fill in a questionnaire on infant care practices. The infants were registered at 28 CHC centres, which were located in the counties of Halland, Bohuslän, Dalsland and Västergötland in western Sweden and situated in both urban and rural areas. They were chosen to reflect a variety of socioeconomic areas. The only inclusion criteria were that the infant should be aged from birth to 12 months of age and that the parents could read and write Swedish. Children were not selected based on the presence or absence of any specific health issues or disabilities. The CHC nurses were asked to give the questionnaires to families with infants of varying ages, in order to provide a good distribution of ages during the first year of life. Otherwise, there was no specific randomised selection procedure.
National advice
During the first two years of the study period, the national advice given to parents to reduce the risk of SIDS were: use the supine sleep position, avoid nicotine, breastfeed if possible and make sure that the baby can move and does not become overheated. In addition, the risks of bed sharing and the possible beneficial effects of a pacifier were discussed in the text of the SIDS brochure issued by the National Board of Health and Welfare and distributed to parents by CHC centres. In order to reduce the risk of positional skull deformity, parents were advised to use a pillow until the baby was able to start to turn around. In December 2013, the information regarding bed sharing and pacifier use was given a higher profile, when it was moved from the general text to the main bulleted advice 7. Parents were advised that infants who were younger than three months of age were safest if they slept in their own bed and that a pacifier could be used when the baby was going to sleep. Furthermore, the recommendation to use a pillow was removed due to the lack of convincing evidence that this prevented skull deformities. The advice was amended before the end of our study, which finished in October 2014. By the time that the revised advice was issued in December 2013, 43% of our study subjects had already completed the questionnaire. It would also have taken time for the revised advice to filter down to parents.
Questionnaire
During a routine visit to their local CHC centre, the families were invited to fill in the questionnaire and, if they agreed, they were asked to take it away and return it by postal mail to the team of investigators. The questions focused on infant care practices regarding sleeping, breastfeeding, use of a pacifier and the maternal use of nicotine. The questionnaire is presented in Table S1, and the main questions are summarised below.
The questionnaire was returned by 753 (75.3%) of the 1,000 families. Two infants with an obviously erroneous age and 41 infants over the age of 395 days – 13 months – were excluded. The upper age limit of 395 days was chosen so that we could include a number of late answers, mainly from questionnaires distributed at the 12‐month visits to the CHC centres. This means that the final calculations were based on 710 infants.
Sleeping position
Parents were asked what position they last placed their baby in when they put them down to sleep: supine, prone or side. The questionnaire referred to babies being placed on their back, stomach or side, to ensure that the parents easily understood the question. Some parents answered that they alternately used the side or supine positions or alternately used the side or prone positions. The side or supine answers were counted as side and the side or prone answers were counted as prone, to take into account the position associated with the greatest risk of SIDS. We found it difficult to interpret 10 answers and they were excluded from the analysis.
Bed sharing
We also asked parents where the baby last slept. The infants were put in the bed sharing category if they were placed to sleep in their parents' bed and were not moved from that bed during the night. The bed sharing category also included infants who initially slept in their parents' bed before being moved to their own bed and infants who were initially placed to sleep in a bed of their own and later moved to the parents' bed. They were categorised as not bed sharing if they were put down to sleep in their own bed and not moved from that bed.
Breastfeeding
The questionnaire asked whether the baby was breastfed and, if the answer was yes, whether it was partly or completely breastfed.
Pacifier use
We asked if the baby used a pacifier in general and also asked about its use when the baby was last put down to sleep. The question included sleeping at night as well as sleeping during the day.
Smoking or any other use of nicotine
The four questions we asked were whether the mother smoked or used any other form of nicotine during pregnancy or whether they were smoking or using any other form of nicotine when they completed the questionnaire.
Statistical analysis
The statistical analysis used the Chi‐square test, and a p value of <0.05 was considered significant.
The population attributable risk (PAR) was calculated according to Coughlin 10, where PAR was equal to (pe (OR−1)/(1 + pe (OR−1))*100% and pe was the proportion of the population exposed. As the current study was not designed as a case–control study, we were unable to measure the effects of risk factors. These were estimated by using by the odds ratios found in the Nordic SIDS study in 1991–1995 11, 12 (Table S2). Due to the fact that the calculation of the confidence interval was based on approximate figures, we restricted the upper limit to 100%.
The SPSS version 22 statistical package (IBM Corp, Armonk, NY, USA) was used for the statistical calculations.
Ethics
The study was approved by the Regional Ethics Board in Gothenburg, and written informed consent was obtained from the participants.
Results
There were slightly more responses for younger infants (Fig. 1), and the median age of the 710 infants included in the study sample was five months. Of these, 50.5% were girls. There were 227 (30.1%) infants under three months, 186 (24.7%) aged three to five months, 155 (20.6%) aged six to eight months and 91 (12.1%) aged nine to 12 months (Table 1). The age distribution for each month ranged from about 3% to 12% of the total cohort, with a mean of 7.3%. There were small peaks at the ages of one, five and 12 months, which coincided with the regular CHC centre visits (Fig. 1).
Figure 1.
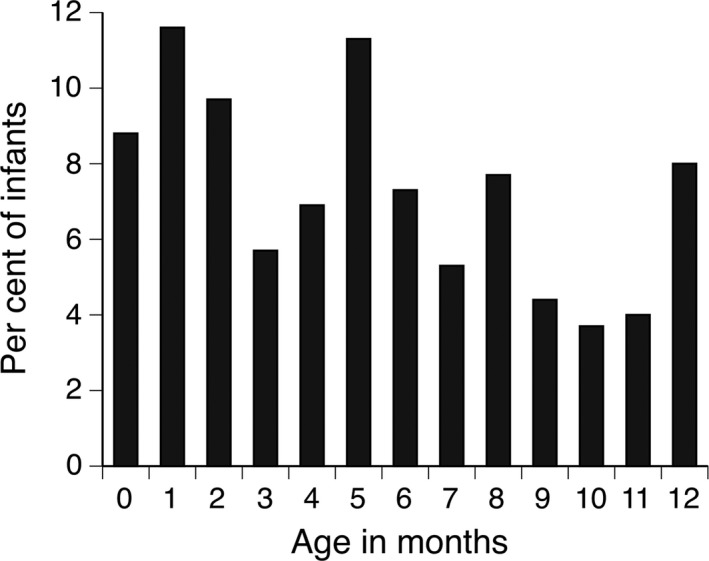
Percentage of children in each of the months covered by the study (n = 710).
Table 1.
Prevalence of sleeping position, breastfeeding, bed sharing, use of pacifier and sleeping in the parents' bedroom at various infant ages
| Age | ||||||||
|---|---|---|---|---|---|---|---|---|
| Under three months (n = 227)a | Three to five months (n = 186)a | Six to eight months (n = 155)a | Nine to 12 months (n = 91)a | |||||
| % | n | % | n | % | n | % | n | |
| Sleeping position | ||||||||
| Supine | 84.4 | 189/224 | 70.8 | 126/178 | 63.6 | 96/151 | 57.3 | 51/89 |
| Side | 14.3 | 32/224 | 23.6 | 42/178 | 31.1 | 47/151 | 31.5 | 28/89 |
| Prone | 1.3 | 3/224 | 5.6 | 10/178 | 5.3 | 8/151 | 11.2 | 10/89 |
| Breastfeeding | ||||||||
| Breastfed (partly or completely) | 83.1 | 187/225 | 67.6 | 121/179 | 54.7 | 81/148 | 35.2 | 31/88 |
| Bed sharing | ||||||||
| Slept in own bed only | 50.9 | 115/226 | 57.9 | 103/178 | 59.5 | 91/153 | 47.8 | 43/90 |
| Went to sleep in own bed, moved to parents' bed | 10.2 | 23/226 | 17.4 | 31/178 | 15.7 | 24/153 | 30 | 27/90 |
| Went to sleep in parents' bed, moved to own bed | 8.8 | 20/226 | 5.6 | 10/178 | 9.2 | 14/153 | 8.9 | 8/90 |
| Slept in parents' bed only | 25.2 | 57/226 | 16.3 | 29/178 | 11.8 | 18/153 | 11.1 | 10/90 |
| Other sleep habits | 4.9 | 11/226 | 2.8 | 5/178 | 3.9 | 6/153 | 2.2 | 2/90 |
| Use of pacifier | ||||||||
| Any general use of pacifier | 84.1 | 190/226 | 80.6 | 145/180 | 77.5 | 117/151 | 73.3 | 66/90 |
| Pacifier used during last sleep | 50.0 | 113/226 | 65.0 | 117/180 | 71.1 | 108/152 | 73.6 | 67/91 |
| Sleeping in the parents' bedroom | ||||||||
| Slept in the parents' bedroom last sleep | 94.2 | 212/225 | 86.1 | 155/180 | 74.8 | 113/151 | 71.1 | 64/90 |
Based on a maximum of 710 responses.
These numbers relate to the total number of infants in each age band. Please note that there were some missing responses in the questionnaires.
The results regarding the prevalence of sleeping position, breastfeeding, bed sharing, use of a pacifier and sleeping in the parents' bedroom at various ages are presented in Table 1.
Sleeping position
During the first three months after birth, 1.3% of the infants slept in the prone position and the figures were 5.6% at the age of three to five months and 5.3% at the age of six to eight months. At nine to 12 months, 11.2% of the infants were placed in the prone position when they went to bed, but their age meant that they moved around their cot much more by this age.
The side sleeping position was used for 14.3% of the infants during the first three months, and this figure increased to 23.6% at three to five months and to 31.1% at six to eight months. At six months the side sleeping position was used for 27.3% of the infants.
Bed sharing
Bed sharing was practiced by 44.2% of the families in the first three months, when we added together the infants who slept in their parents' beds all the time to the infants who slept part‐time in their parents' bed. This figure was 39.3% at the age three to five months, 36.7% at six to eight months and 50% by the age of nine to 12 months. The figure at six months was 34.6%, compared with the 19.8% found in an earlier study that is referenced in Discussion section.
In the first three months, 50.9% slept in a separate bed in their parents' bedroom, and at six months 54% slept in a separate bed in the parental bedroom (data not shown). Almost 6% slept in another room than the parental bedroom in the first three months, and this percentage rose to 13.9% at the age three to five months.
Breastfeeding
Breastfeeding was practiced by 83.1% of the mothers when the children were up to three months of age, and by 10–12 months of age this figure had steadily fallen to 35.2%.
Pacifier use
Up to three months of age, 84.1% of the infants routinely used a pacifier and 50% had used a pacifier during their last sleep. By 10–12 months routine pacifier use had fallen to 73.3%, but pacifier use at the time of the last sleep had risen to 73.6%.
Tobacco smoking
During pregnancy 2.8% of mothers smoked: 2.3% smoked 1–9 cigarettes a day and 0.5% smoked 10 or more cigarettes a day. We also found that 1.1% of the cigarette smokers also used another nicotine product and that 0.7% just used another nicotine product.
At the time of completing the questionnaire, 3.6% of the mothers who answered that question said that they smoked: 2.4% smoked 1–9 cigarettes a day and 1.2% smoked 10 or more cigarettes a day. Some of the mothers used other forms of nicotine than cigarettes: 2.4% used another nicotine product as well as cigarettes and 2.1% just used another nicotine product.
Other factors and associations
In the first three months, 7.1% of the infants slept under their parents' duvet and 1.3% woke up with their head covered by duvet. In contrast, 92.4% of the infants had their own pillow in the first three months of life and 3.8% of these children were placed in the prone position at their last sleep (data not shown). The number of infants that used a pillow did not go down in 2014, which was after the recommendation to use a pillow was removed from the official advice in December 2013.
Factors affecting the use of prone sleeping and bed sharing during the first six months are presented in Table 2. Prone sleeping was more likely to occur if the mother had smoked during pregnancy or was currently smoking. Bed sharing during the first six months was more likely if the infants were breastfed and less likely if they used a pacifier. Furthermore, mothers who had smoked during pregnancy were less likely to bed share. No smoking mothers bed shared with their infant at the time that they answered the questionnaire and consequently it was not possible to calculate an odds ratio for smoking and bed sharing. However, the 13 (6%) mothers that smoked at the time that they answered the questionnaire did not bed share.
Table 2.
Factors affecting the use of prone sleeping, side sleeping and bed sharing during the first six months
| Prone sleeping during the first six months | |||
|---|---|---|---|
| Prone n (%) | Supine n (%) | OR (95% CI) | |
| Any breastfeeding | |||
| Yes | 9 (69.2) | 237 (75.7) | 0.72, (0.22, 2.41) |
| No | 4 (30.8) | 76 (37.4) | Ref |
| Any use of pacifier | |||
| Yes | 9 (69.2) | 263 (83.5) | 0.44 (0.13, 1.50) |
| No | 4 (30.8) | 52 (16.5) | Ref |
| Pacifier last sleep | |||
| Yes | 8 (61.5) | 174 (55.2) | 1.30 (0.42, 4.05) |
| No | 5 (38.5) | 141 (44.8) | Ref |
| Tobacco smoking during pregnancy | |||
| Yes | 2 (15.4) | 9 (2.9) | 6.14 (1.18, 31.9) |
| No | 11 (84.6) | 304 (97.1) | Ref |
| Tobacco smoking when answering the questionnaire | |||
| Yes | 2 (15.4) | 9 (2.9) | 6.16 (1.19, 32.0) |
| No | 11 (84.6) | 305 (97.1) | Ref |
| Side sleeping during the first six months | |||
| Side n (%) | Supine n (%) | OR (95% CI) | |
|---|---|---|---|
| Any breastfeeding | |||
| Yes | 59 (79.7) | 237 (75.7) | 1.26 (0.68, 2.35) |
| No | 15 (20.3) | 76 (24.3) | Ref |
| Any use of pacifier | |||
| Yes | 61 (82.4) | 263 (83.5) | 0.93 (0.48, 1.81) |
| No | 13 (17.6) | 52 (16.5) | Ref |
| Pacifier last sleep | |||
| Yes | 46 (62.2) | 174 (55.2) | 1.33 (0.79, 2.24) |
| No | 28 (37.8) | 141 (44.8) | Ref |
| Tobacco smoking during pregnancy | |||
| Yes | 1 (1.4) | 9 (2.9) | 0.46 (0.06, 3.71) |
| No | 73 (98.6) | 304 (97.1) | Ref |
| Tobacco smoking when answering the questionnaire | |||
| Yes | 2 (2.7) | 9 (2.9) | 0.94 (0.20, 4.45) |
| No | 72 (97.3) | 305 (97.1) | Ref |
| Any bed sharing during the first six months | |||
|
Any bed sharing n (%) |
Own bed n (%) |
OR (95% CI) | |
|---|---|---|---|
| Any breastfeeding | |||
| Yes | 148 (87.1) | 147 (68.1) | 3.16 (1.86, 5.37) |
| No | 22 (12.9) | 69 (31.9) | Ref |
| Any use of pacifier | |||
| Yes | 124 (72.9) | 196 (89.9) | 0.30 (0.17, 0.53) |
| No | 46 (27.1) | 22 (10.1) | Ref |
| Pacifier last sleep | |||
| Yes | 75 (44.1) | 143 (65.6) | 0.41 (0.27, 0.63) |
| No | 95 (55.9) | 75 (34.4) | Ref |
| Tobacco smoking during pregnancy | |||
| Yes | 1 (0.6) | 11 (5.1) | 0.11 (0.01, 0.87) |
| No | 168 (99.4) | 206 (94.9) | Ref |
| Tobacco smoking when answering the questionnaire | |||
| Yes | 0 (0.0) | 13 (6.0) | 0 |
| No | 170 (100.0) | 204 (94.0) | Ref |
Based on a maximum of 710 responses. Bold odds ratios, ORs, and confidence intervals, CIs, denote statistical significance.
Population attributable risk (PAR)
The PAR for prone sleeping, side sleeping and smoking was 65% (95% confidence interval 35%–100%), 60% (14%–100%) and 15% (8%–24%), respectively.
Discussion
The main finding of this study was that, overall, parents followed the national advice to reduce the risk of SIDS. Only 2.8% of mothers smoked during pregnancy, and only 1.3% of infants slept prone during the first three months. However, at the age of three to five months, 5.6% slept prone. Furthermore, 14.3% of the infants were placed to sleep on their side during the first three months and this increased to 23.6% by three to five months. This means that not all families followed the national advice to reduce the risk of SIDS.
The incidence of SIDS varies with age, with the peak incidence during the first months of life. In 1975–1991, before the campaign to reduce the risk of SIDS started, the median age at death from SIDS in Sweden was 80 days 13. In the period after the campaign, 1992–2005, the median age at death fell to 64 days 13. During the period 2005–2011, Möllborg et al. reported the same median age of 64 days at death in SIDS cases 9. In the present study only 1% reported using the prone sleeping position during the first three months, which means that the parents' adherence to advice regarding the prone position during the most vulnerable age period was very good.
In infants aged from three to five months, the prevalence of prone sleeping rose to 5.6% and there may be several explanations for this. It is possible that the parents were less rigorous when it came to complying with the advice when their infants got older. The parents' fear of SIDS may also have diminished when the infants were a few months old. Furthermore, it is commonly accepted that many infants are comforted by sleeping in the prone position 14 and parents may have used this position and a pacifier as two ways of comforting the infant. In addition to these explanations, infants start to turn around by themselves around five to six months of age.
The side sleeping position was used for almost 15% of the infants below three months of age despite the fact that the side position is unstable 15 and therefore involves a higher risk of SIDS than sleeping supine 16. The prevalence of side sleeping increased with age, and by six months it was 27.3%. This included babies who were alternatively put down to sleep in side and supine positions. This can be compared with a study we performed in western Sweden some 10 years ago, where parents put 43.8% of babies aged six months in the side sleeping position or alternatively used the side and supine positions 14. We conclude that although the use of the side sleeping position seems to have decreased, it is still common.
Smoking during pregnancy has decreased steadily in Sweden, but in this study we found that the figure of 2.8% was even lower than the official statistics. These showed that, on average, 6.6% of pregnant women in the county of Halland, which was one of our study areas, smoked in early pregnancy in 2014 and 5.4% smoked in late pregnancy. The figures for Västra Götaland, the region that included our study site counties of Bohuslän, Dalsland and Västergötland, were 6.0% and 4.4%, respectively 17. Our low figure was probably due to some selection bias, but nevertheless it was largely in agreement with official Swedish statistics. As smoking is a dose‐dependent risk factor, it is also important to inform mothers that even reducing smoking during pregnancy lowers the risk of SIDS 12.
We found that smoking, both during pregnancy and at the time of completing the questionnaire, was associated with a higher odds ratio for placing infants in the prone sleeping position (Table 2). This was consistent with an earlier finding from our west Sweden cohort study, which found that heavy smoking during the first trimester was a risk factor for prone sleeping 14. However, very few mothers smoked during pregnancy or around the time they answered the questionnaire. This is probably the reason for the wide confidence intervals and the fact that the effect of current smoking did not reach statistical significance.
Mothers who had smoked during pregnancy were less likely to bed share. Furthermore, the 13 mothers that smoked at the time that they answered the questionnaire did not bed share. Taken together, this suggests that smoking mothers actively chose not to share bed with their infants.
In our previous study in 2010, we found that 19.8% of infants bed shared at the age of six months 18, compared to 44.2% in the present study. In view of the current discussions concerning the possible hazards associated with bed sharing 19, 20, 21, 22, 23, 24, we need to obtain more detailed knowledge on how families bed share and to what extent methods for the so‐called safe bed sharing, or safer bed sharing 24, 25, are used.
As expected, bed sharing was significantly associated with breastfeeding, which has been found in several other studies 13, 19. Bed sharing facilitates breastfeeding, which makes it an attractive option for women who want to breastfeed.
The finding that smoking during pregnancy was associated with a lower prevalence of bed sharing might be caused by greater awareness of the knowledge that smoking increases the risk of SIDS when bed sharing 20.
Several studies have reported that pacifier use reduces the risk of SIDS 26 and this is now stated in the national Swedish advice 7. In this study we found a negative correlation between bed sharing and pacifier use. Both bed sharing and pacifier use can calm the infant, which could explain the inverse relationship between the practices. It could also be speculated that mothers who bed shared and breastfed were more negative about pacifiers use.
In December 2013 when the advice to reduce the risk of SIDS was revised, the number of subjects that had already been included in the study (43%) was approaching the halfway mark. The guidance emphasised that the safest place for infants up to three months of age to sleep was in a separate bed and that a pacifier could be used when the infant was going to sleep. The updated advice did not affect the results on prone sleeping, smoking or breastfeeding, and the use of a pillow during the first three months was not reduced. Obviously, there was a time lag before the revised recommendations had an impact.
In an attempt to measure the effects on the population level of the risk factors of side sleeping, prone sleeping and maternal smoking during pregnancy, we calculated the PAR. The effects were estimated based on the odds ratios found in the Nordic SIDS study, and the exposed fraction of the population was taken from the current study. This revealed that a reduction of side sleeping (PAR 60%), due to the high exposure in the population, would be of similar importance as a reduction of prone sleeping (PAR 65%), despite the higher risk of that practice. Due to the reduction of smoking during pregnancy in Sweden, this habit now is associated with a smaller PAR (15%).
Strengths and limitations
The strengths of this study were the large number of infants in the study cohort (n = 710) and the fact that we asked detailed questions about the infants' sleeping habits.
A limitation was that there probably was some selection bias, which led us to underestimate smoking and possibly overestimate compliance with the national advice to reduce the risk of SIDS. Furthermore, there was a risk that providing socially acceptable responses may have affected the replies to the questions. To reduce that effect, the questionnaires were not returned to the CHC nurses but mailed by post to another address. Another limitation was that the SIDS advice was updated in 2013, in the middle of our 2012–2014 study period. However, the important elements of the advice were unchanged and the results did not seem to be affected.
Conclusion
In conclusion, this study showed that the adherence to national advice given in Sweden to reduce the risk of SIDS was generally good. However, due to high attributable risks, both prone and side sleeping positions should be targeted.
Funding
The study was supported by the Swedish Government under the ALF agreement between the Government and the County Councils concerning economic support of medical research.
Conflicts of interest
The authors declare that they have no conflict of interests.
Supporting information
Table S1 Questionnaire regarding infant environment and sleeping habits.
Table S2 Odds ratios (from the Nordic SIDS Study 1991–1995) and proportions of the currently studied population exposed to prone sleeping, side sleeping and maternal smoking during pregnancy, used in the calculation of population attributable risks.
Acknowledgements
The authors want to thank Annette Whibley for excellent editing of the manuscript and valuable suggestions and Henrik Källberg, PhD, for valuable statistical advice.
References
- 1. Fleming PJ, Gilbert R, Azaz Y, Berry PJ, Rudd PT, Stewart A, et al. Interaction between bedding and sleeping position in the sudden infant death syndrome: a population based case control study. BMJ 1990; 301: 85–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Mitchell EA, Scragg R, Stewart AW, Becroft DM, Taylor BJ, Ford RP, et al. Results from the first year of the New Zealand cot death study. N Z Med J 1991; 104: 71–6. [PubMed] [Google Scholar]
- 3. Dwyer T, Ponsonby AL, Newman NM, Gibbons LE. Prospective cohort study of prone sleeping position and sudden infant death syndrome. Lancet 1991; 337: 1244–7. [DOI] [PubMed] [Google Scholar]
- 4. Mitchell EA, Hutchison L, Stewart AW. The continuing decline in SIDS mortality. Arch Dis Child 2007; 92: 625–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Socialstyrelsen (National Board of Health and Welfare) . Skall spädbarn ligga på mage eller rygg? Finns det ett samband mellan magläge och plötslig spädbarnsdöd? (Should infants be placed prone or supine? Is there a connection between prone position and cot death?). Stockholm: Socialstyrelsens meddelandeblad, 1992. [Google Scholar]
- 6. Wennergren G, Alm B, Øyen N, Helweg‐Larsen K, Milerad J, Skjærven R, et al., on behalf of the Nordic Epidemiological SIDS Study , The decline in the incidence of SIDS in Scandinavia and its relation to risk‐intervention campaigns. Acta Paediatr 1997; 86: 963–8. [DOI] [PubMed] [Google Scholar]
- 7. Socialstyrelsen (National Board of Health and Welfare) . Minska risken för plötslig spädbarnsdöd (Reduce the risk of cot death). 11 Dec 2013. Available at: http://www.socialstyrelsen.se/Lists/Artikelkatalog/Attachments/19486/2014-8-2.pdf (accessed on October 30, 2016).
- 8. Wennergren G, Nordstrand K, Alm B, Möllborg P, Öhman A, Berlin A, et al. Updated Swedish advice on reducing the risk of sudden infant death syndrome. Acta Paediatr 2015; 104: 444–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Möllborg P, Wennergren G, Almqvist P, Alm B. Bed sharing is more common in sudden infant death syndrome than in explained sudden unexpected deaths in infancy. Acta Paediatr 2015; 104: 777–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Coughlin SS, Benichou J, Weed DL. Attributable risk estimation in case‐control studies. Epidemiol Rev 1994; 16: 51–64. [DOI] [PubMed] [Google Scholar]
- 11. Øyen N, Markestad T, Skjærven R, Irgens LM, Helweg‐Larsen K, Alm B, et al. Combined effects of sleeping position and prenatal risk factors in Sudden Infant Death Syndrome. The Nordic Epidemiological SIDS Study. Pediatrics 1997; 100: 613–21. [DOI] [PubMed] [Google Scholar]
- 12. Alm B, Milerad J, Wennergren G, Skjærven R, Øyen N, Norvenius G, et al., on behalf of the Nordic Epidemiological SIDS Study . A case‐control study of smoking and sudden infant death syndrome in the Scandinavian countries, 1992 to 1995. Arch Dis Child 1998; 78: 329–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Möllborg P, Alm B. Sudden infant death syndrome during low incidence in Sweden 1997–2005. Acta Paediatr 2010; 99: 94–8. [DOI] [PubMed] [Google Scholar]
- 14. Alm B, Möllborg P, Erdes L, Pettersson R, Åberg N, Norvenius G, et al. SIDS risk factors and factors associated with prone sleeping in Sweden. Arch Dis Child 2006; 91: 915–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Skadberg BT, Morild I, Markestad T. Abandoning prone sleeping: effect on the risk of sudden infant death syndrome. J Pediatr 1998; 132: 340–3. [DOI] [PubMed] [Google Scholar]
- 16. Carpenter RG, Irgens LM, Blair PS, England PD, Fleming P, Huber J, et al. Sudden unexplained infant death in 20 regions in Europe: case control study. Lancet 2004; 363: 185–91. [DOI] [PubMed] [Google Scholar]
- 17. Sveriges officiella statistik, Statistik – Hälso‐ och Sjukvård (Official statistics of Sweden, Statistics – Health and Medical Care) . Graviditeter, förlossningar och nyfödda barn, Medicinska födelseregistret 1973–2014, Assisterad befruktning, 1991‐2013 (Pregnancies, deliveries and newborn infants, The Swedish Medical Birth Register 1973–2014, Assisted Reproduction, treatment 1991–2013). Socialstyrelsen (National Board of Health and Welfare). 27 Dec 2015. Available at: http://www.socialstyrelsen.se/Lists/Artikelkatalog/Attachments/20009/2015-12-27.pdf (accessed on October 30, 2016).
- 18. Möllborg P, Wennergren G, Norvenius G, Alm B. Bed sharing among six‐month‐old infants in western Sweden. Acta Paediatr 2011; 100: 226–30. [DOI] [PubMed] [Google Scholar]
- 19. Ball HL, Howel D, Bryant A, Best E, Russell C, Ward‐Platt M. Bed‐sharing by breastfeeding mothers: who bed‐shares and what is the relationship with breastfeeding duration? Acta Paediatr 2016; 105: 628–34. [DOI] [PubMed] [Google Scholar]
- 20. Carpenter R, McGarvey C, Mitchell EA, Tappin DM, Vennemann MM, Smuk M, et al. Bed sharing when parents do not smoke: Is there a risk of SIDS? An individual level analysis of five major case‐control studies. BMJ Open 2013; 3: e002299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Blair PS, Sidebotham P, Pease A, Fleming PJ. Bed‐sharing in the absence of hazardous circumstances: is there a risk of sudden infant death syndrome? An analysis from two case‐control studies conducted in the UK. PLoS ONE 2014; 9: e107799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. McKenna JJ, Gettler LT. There is no such thing as infant sleep, there is no such thing as breastfeeding, there is only breastsleeping. Acta Paediatr 2016; 105: 17–21. [DOI] [PubMed] [Google Scholar]
- 23. Wennergren G. Why it is important to present all the available facts about bed sharing and breastfeeding. Acta Paediatr 2016; 105: 22. [DOI] [PubMed] [Google Scholar]
- 24. Mitchell EA, Cowan S, Tipene‐Leach D. The recent fall in post‐perinatal mortality in New Zealand and the Safe Sleep Programme. Acta Paediatr 2016; 105: 1312–20. [DOI] [PubMed] [Google Scholar]
- 25. Wennergren G. No bed sharing or safer bed sharing? Acta Paediatr 2016; 105: 1321. [DOI] [PubMed] [Google Scholar]
- 26. Alm B, Wennergren G, Möllborg P, Lagercrantz H. Breastfeeding and dummy use have a protective effect on sudden infant death syndrome. Acta Paediatr 2016; 105: 31–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1 Questionnaire regarding infant environment and sleeping habits.
Table S2 Odds ratios (from the Nordic SIDS Study 1991–1995) and proportions of the currently studied population exposed to prone sleeping, side sleeping and maternal smoking during pregnancy, used in the calculation of population attributable risks.


