Abstract
Feelings can shape how people respond to persuasive messages. In health communication, adaptive affective responses to potentially threating messages constitute one key to intervention success. The current study tested dispositional mindfulness, characterized by awareness of the present moment, as a predictor of adaptive affective responses to potentially threatening health messages and desirable subsequent health outcomes. Both general and discrete negative affective states (i.e., shame) were examined in relation to mindfulness and intervention success. Individuals (n=67) who reported less than 195 weekly minutes of exercise were recruited. At baseline, participants’ dispositional mindfulness and exercise outcomes were assessed, including self-reported exercise motivation and physical activity. A week later, all participants were presented with potentially threatening and self-relevant health messages encouraging physical activity and discouraging sedentary lifestyle, and their subsequent affective response and exercise motivation were assessed. Approximately one month later, changes in exercise motivation and physical activity were assessed again. In addition, participants’ level of daily physical activity was monitored by a wrist worn accelerometer throughout the entire duration of the study. Higher dispositional mindfulness predicted greater increases in exercise motivation one month after the intervention. Importantly, this effect was fully mediated by lower negative affect and shame specifically, in response to potentially threatening health messages among highly mindful individuals. Baseline mindfulness was also associated with increased self-reported vigorous activity, but not with daily physical activity as assessed by accelerometers. These findings suggest potential benefits of considering mindfulness as an active individual difference variable in theories of affective processing and health communication.
Keywords: health communication, mindfulness, affect, physical activity, shame
Introduction
Exercise is associated a wide range of health benefits including lower risk of several cancers (Holmes, Chen, Feskanich, Kroenke, & Colditz, 2005; Slattery et al., 2003), coronary heart disease (Manson et al., 1999; Tanasescu et al., 2002), and stroke (Do Lee, Folsom, & Blair, 2003), as well as lower overall morbidity and mortality (Gregg et al., 2003; Lee, Hsieh, & Paffenbarger, 1995; Moore et al., 2012). Increases in even light activity (vs. sedentary behavior) have both short and longer-term mental and physical health benefits (Owen, Healy, Matthews, & Dunstan, 2010; Seguin et al., 2012). However, one classic challenge intrinsic to designing health messages to promote exercise is that those at the highest health risk for disease tend to be the most defensive. That is, feelings can impact how people respond to persuasive health messages. In the domain of health communication, personally relevant messages can be threatening to individuals’ sense of self-competence, which can have counterproductive effects on receptivity to messages and subsequent health outcomes. In the context of physical activity behavior, sedentary individuals may show negative affective reactivity when presented with messages encouraging exercise because such messages can threaten self-worth. Negative responses to health messages, in turn, can lead to decreased risk perception, motivation, and decreased likelihood of altering risk behaviors (Resnicow & McMaster, 2012). Therefore, identifying predictors of adaptive affective responses to potentially threatening health messages is critical among at-risk individuals.
Mindfulness, characterized by attention to and awareness of the present experience (Brown, Ryan, & Creswell, 2007a), has been associated with various positive health outcomes (Langer, 1989). For example, dispositional mindfulness predicted healthy dietary habits (Jordan, Wang, Donatoni, & Meier, 2014; Murphy, Mermelstein, Edwards, & Gidycz, 2012), and better quality of sleep and self-reported general physical health (Murphy et al., 2012). Although some studies have examined mindfulness in the context of existing health behavior theories (e.g., Black, Sussman, Johnson, & Milam, 2012; Chatzisarantis & Hagger, 2007), few attempts have been made to incorporate mindfulness within established health behavior models (Black, 2010), or within the context of health communication specifically.
High dispositional mindfulness may dampen negative affective reactivity in the face of potentially threatening health messages. In response to health messages, having mindful awareness may help people disengage from patterns of automatized thought processing. This may in turn allow individuals to make more considered decisions, instead of reacting habitually to incoming stimuli (e.g., Brown, Ryan, & Creswell, 2007b; Langer, 1989; Kang, Gruber, & Grey, 2013). In support of this view, greater dispositional mindfulness was associated with lower daily negative affect (Brown & Ryan, 2003; Miners, 2007) and less negative affect during experimentally induced interpersonal conflict (Barnes, Brown, Krusemark, Campbell, & Rogge, 2007). Furthermore, dispositional mindfulness was associated with attenuated activity within limbic regions implicated in affective reactivity. Specifically, high mindfulness was associated with less amygdala activation both at rest (Way, Creswell, Eisenberger, & Lieberman, 2010) and during psychological threat (Desbordes et al., 2012), and more efficient prefrontal cortex inhibition of amygdala during psychological threat (Creswell, Way, Eisenberger, & Lieberman, 2007). In addition, dispositional mindfulness predicted decreased late positive potential, a marker of high arousal affective reactivity, to unpleasant and threatening stimuli (Brown, Goodman, & Inzlicht, 2013). These findings suggest that individuals higher in mindfulness may be both less reactive to potential threat and better at regulating negative affect. Therefore, when presented with potentially threatening health information, highly mindful individuals may report low negative affect, which may then predict increased exercise outcomes over time.
Negative affect in response to perceived threat is a central construct predicting the likelihood of change in a number of major theories of behavior change, including the widely-used Health Belief Model (Becker, 1974). Indeed, threat-induced fear appeals are common in public health interventions to induce motivation and behavior change. When accompanied by perceived efficacy (Peters et al., 2013), negative affect can increase the persuasiveness of health messages (Witte & Allen, 2000) under some circumstances (c.f., Earl & Albarracín, 2007). However, negative affect may also trigger or accompany defensive tendencies, resulting in counterproductive outcomes. For example, when people are confronted with potentially threatening health information of high personal relevance, they may react defensively by avoiding (Mendolia, 1999) and/or refuting (Chaiken, 1992) the beneficial information. Therefore, lowering negative affective responses to potentially threatening health messages can promote receptivity to important and beneficial health information.
In particular, shame, a negative affective response that may result from failing to meet personal or social expectations (e.g., Dickerson, Gruenewald, & Kemeny, 2004), can result from facing personally relevant and potentially threatening health messages. Shame is a maladaptive response to health information, and may trigger defensive tendencies and avoidance (Tangney & Dearing, 2004). For example, individuals primed with shame were more likely to resist shame-inducing anti-drinking messages and report increased intention to binge drink (Agrawal & Duhachek, 2010). Furthermore, among newly recovering alcoholics, nonverbal displays of shame about past addiction predicted the likelihood and severity of relapse (Randles & Tracy, 2013), suggesting that shame may perpetuate or exacerbate problematic health behaviors. In the context of physical activity, prior experiences with shame-inducing weight stigma were associated with increased desire to avoid exercise, which in turn related to less frequent strenuous and moderate exercise (Vartanian & Shaprow, 2008). Therefore, negative affect, felt in response to health messages, may be associated with decreased exercise outcomes driven by shame.
Exercise outcomes can be assessed at various stages using diverse methods. In several theories of health behavior change (e.g., Health Action Process Approach; Schwarzer & Luszczynska, 2008), the motivation phase often precedes the subsequent action or volition phase by providing an initial impetus necessary for the change. In particular, increases in motivation to exercise after exposure to health messages may reflect a positive initial step. In addition to this proximal outcome (exercise motivation), more distal changes in physical activity behavior can be assessed, using self-reported physical activity and daily physical activity monitored by a wrist worn accelerometer.
In the current study, we tested dispositional mindfulness as a predictor of adaptive affective responses to health messages as well as increased exercise outcomes. Specifically, we tested a) the association between dispositional mindfulness and attenuated negative affective responses to health messages that encourage physical activity, b) dispositional mindfulness as a predictor of increased exercise outcomes following a health message intervention, and c) the mediating role of negative affect, both general (i.e., averaged across multiple negative affect items) and specifically with regard to shame, in the association between dispositional mindfulness and exercise motivation. Motivated by previous findings that linked mindfulness and attenuated affective reactivity, we show that a) those with higher dispositional mindfulness reported lower negative affect, both generally and shame specifically, after a potentially threatening health message intervention. Given the detrimental impact negative affect may have in processing health messages, we further show that b) attenuation in negative affect predicted increased positive exercise-relevant outcomes. Finally, we show that c) negative affect mediates the effect of dispositional mindfulness on exercise motivation.
Method
Participants
Participants (n=67; 41 females; mean age=33.42 years, SD=13.04; 44 White, 12 Black, 3 Asian, 1 Hispanic, 7 Other; Table 1) were recruited through convenience sampling for a longitudinal study that involved three visits to the laboratory (T1, T2, T3) across five weeks, with compensation up to $100. Participants who self-reported having engaged in less than 195 minutes of exercise, consisting of walking, moderate, and vigorous physical activity, throughout the last seven days from the time of participation were recruited (see Table 1 for baseline characteristics). Participants also met the standard functional magnetic resonance imaging (fMRI) safety criteria (no metal in body, not claustrophobic, not pregnant) and were right handed. Individuals who self-reported a history of major physical or mental health disorders were excluded. Participants responded to online advertisement and flyers describing a study about “daily activities” (to avoid selection bias related to physical activity), posted in Ann Arbor and surrounding communities. Across three visiting time points, seven participants did not complete the study, and the final samples consisted of 67 at T1, 61 at T2, and 60 participants at T3.
Table 1.
Demographic and Baseline Characteristics
| Demographic | |
|---|---|
| Age (Yrs) | 33.43 (13.04) |
| Female (%) | 61.2% |
| Caucasian (%) | 65.7% |
| Education (Yrs) | 16.62 (3.44) |
| Baseline Characteristics | |
|---|---|
| Weekly Exercise Minutes (IPAQ) | 123.5 (49.52) |
| BMI | 27.99 (6.84) |
| Mindfulness (MAAS) | 4.07 (0.90) |
| Exercise Motivation (BREQ-2) | 5.94 (6.34) |
| Depression (BDI) | 1.35 (0.39) |
Note: BDI = Beck Depression Inventory; BMI = Body Mass Index; BREQ-2 = Behavioral Regulation in Exercise Questionnaire-version 2; IPAQ = International Physical Activity Questionnaire (short-form, self-reported during the pre-study screening); MAAS = Mindful Attention Awareness Scale. Mean values are displayed with standard deviations in parentheses where applicable. N=67 unless otherwise noted.
Procedure
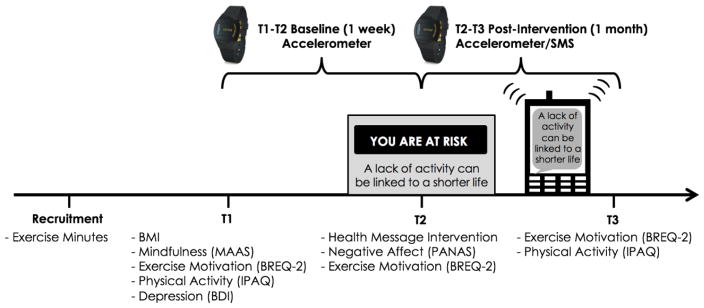
Participants visited the laboratory at three time points (i.e., T1, T2, T3; Figure 1). All experimenters who worked with the participants and participants themselves were blind to the present hypotheses throughout the study. During their initial visit (T1), participants reported their weight and height from which the Body Mass Index (BMI) scores were derived, and completed self-report measures of mindfulness, exercise motivation, physical activity, and depression (a potential covariate, see Measures below for more detail). For T1 accelerometer calibration, participants completed a range of activities including walking at their usual pace along a hallway, climbing stairs, and sitting for at least 30 minutes while wearing an accelerometer device on their wrist. Participants continued to wear the accelerometers for the week between T1 and T2, which served as their baseline activity period, and for a month between T2 and T3, which served as their post-intervention activity period.
Figure 1.
Overall study protocol. BDI = Beck Depression Inventory; BREQ-2 = Behavioral Regulation in Exercise Questionnaire-version 2; IPAQ = International Physical Activity Questionnaire; MAAS = Mindful Attention Awareness Scale; PANAS = Positive and Negative Affect Scale; SMS = Short Message Service.
Approximately a week after T1 (M=9.35 days, SD=6.16) participants visited the laboratory for the second time (T2) to complete the health message intervention, followed by reporting current positive and negative affect and exercise motivation. Participants continued to wear their accelerometers for an additional month leading up to the last visit (T3). As a part of the health message intervention, participants continued to receive daily health text messages on their phone for a month between T2 and T3.
During the final T3 visit that took place approximately one month (M=35.92, SD=7.19) after T2, participants completed self-report measures of exercise motivation and physical activity. Upon completion, participants returned their accelerometers, were debriefed, paid, and thanked for their participation.
Health message intervention
Participants were oriented to the health message intervention verbally by the experimenter, and were self-guided through the intervention while in an fMRI scanner using computerized software (Presentation; NeuroBehavioral Systems Inc.). The health messages were developed in consultation with senior investigators and staff from Center for Health Communications Research at University of Michigan, and were designed to be an intervention that parallels what would be seen in everyday health communication contexts (e.g., from a doctor, media, friends, etc.).
Specifically, messages were designed to promote physical activity by highlighting increased risk for chronic disease due to sedentary behavior and elevated BMI (risk messages), benefits of becoming more active (active why) and less sedentary (sedentary why), as well as behavioral strategies to become more active (active how) and less sedentary (sedentary how). All messages were pilot tested to elicit varying degrees of threat responses. All participants were presented with the same distribution of 50 health messages in a randomized order, with 10 active why, 10 sedentary why, 10 active how, and 10 sedentary how messages, and a random selection of 10 risk messages from a list of 16 (See Supplemental Material 1 for a complete list of messages). At the end of each block of messages, participants were given a brief reflection period in which they were asked to think of how they would apply the message in their own life. The task also included advice regarding other daily behaviors not related to physical activity, which are not the focus of the current investigation.
Health messages were reinforced via short message service (SMS) throughout the month following the health intervention (T2) up until the third visit (T3). Participants received one message per day drawn from the same health messages shown during the primary message intervention.
Measures
Mindfulness
Dispositional mindfulness was measured by the 15-item Mindful Attention Awareness Scale (MAAS; Brown & Ryan, 2003) at T1. The MAAS assesses an individual’s tendency to attend and be aware of the present moment’s experience, rated on a 1 (almost always) to 5 (almost never) scale. All scores were reverse coded for higher values to reflect higher dispositional mindfulness. An example item is, “I could be experiencing some emotion and not be conscious of it until some time later.” The scale’s internal consistency in the current study (α=.92) was high.
Negative affect
Self-reported negative affect following the health message intervention was assessed at T2 using the positive and negative affect scale (PANAS; Watson, Clark, & Tellegen, 1988) consisting of fifteen negative affect terms (frustrated, upset, distressed, guilty, miserable, scared, hostile, irritable, disappointed, ashamed, nervous, troubled, jittery, unhappy, afraid) rated on a 1 (not at all) to 5 (extremely) scale. In addition, positive affect was measured, by using the PANAS’s fifteen individual positive affect terms (interested, excited, strong, happy, relieved, enthusiastic, pleased, proud, alert, content, inspired, joyful, determined, attentive, active). From this, general negative and positive affect mean scores were created. Internal consistency scores in the current study for negative (α=.88) and positive (α=.93) affect items were high.
Exercise motivation
Motivation to exercise was measured at T1, T2, and T3 with the 19-item Behavioral Regulation in Exercise Questionnaire-version 2 (BREQ-2; Markland & Tobin, 2004). The BREQ-2 includes five subscales assessing different types of exercise motivation (i.e., intrinsic, identified, introjected, and external), as well as amotivation, rated on a 0 (not true for me) to 4 (very true for me) scale. A global composite score that represents the degree to which individuals are self-determined to exercise was derived by multiplying each subscale score by its weighting and summing these weighted scores (See Markland, 2011, for scoring instruction). Internal consistency scores within subscales across T1, T2, and T3 in the current study (αmean=.84, αrange=.74–.93) were high.
Self-reported physical activity
Self-reported physical activity was obtained using the long version of the International Physical Activity Questionnaire (IPAQ; Craig et al., 2003) at T1 and T3 (though not at T2 due to time constraints). The IPAQ assesses minutes of moderate and vigorous-intensity physical activity and walking over the past seven days across four domains, including occupation, transportation, house/yard work, and recreation/leisure.
Daily physical activity
Daily physical activity was monitored using accelerometers. We collected accelerometer data throughout the entire five-week duration of the study using a triaxial GENEA accelerometer (Esliger et al., 2011) worn on the left wrist (all participants were right-handed). Subjects were encouraged to continue wearing the waterproof accelerometers at all times.
In order to calculate levels of non-sedentary physical activity, we defined baseline physical activity cut points according to measurements taken during the T1 laboratory baseline calibration in which participants performed a number of activities including at least 30 minutes of sedentary activities such as completing surveys while seated at a computer terminal. The peak acceleration during this 30-minute sedentary period was used to determine appropriate cut points for each participant such that activity above that threshold was tagged as “physical activity.” Using the physical activity threshold, we computed the minutes of physical activity each day throughout the T1–T2 (one week) baseline and the T2–T3 (one month) post-intervention periods (Figure 1). Changes in daily physical activity represent the difference scores between physical activity during the T1–T2 and T2–T3 periods, with positive scores representing increases in physical activity.
Covariates
Baseline exercise minutes and BMI scores were assessed as potential covariates. Baseline exercise minutes were assessed at the time of recruitment during the prescreening process, and represent the sum of self-reported minutes spent walking and doing moderate and vigorous physical activity in the prior seven days. BMI was calculated by dividing body weight (kg) by body height squared (m2), self-reported at T1. Participants’ baseline level of depression was assessed as a potential covariate given its association to both mindfulness (Argus & Thompson, 2008; Christopher & Gilbert, 2010; Paul, Stanton, Greeson, Smoski, & Wang, 2013) and negative affectivity (Bylsma, Morris, & Rottenberg, 2008). Depression was measured by the 21-item Beck Depression Inventory (BDI; Beck, Ward, Mendelson, Mock, & Erbaugh, 1961). Scores were summed to reflect current depressive symptoms, ranging from 0 to 63. The measure’s internal consistency in the current study (α=.92) was high (For a complete list of survey measures administered in this study, see Supplemental Material 2).
Data Analyses
All regression analyses were conducted with dispositional mindfulness as a predictor variable for each of the outcome measures, with reported covariates when appropriate. Formal bootstrapping procedures with 1000 bootstraps were used for mediation analyses (Preacher & Hayes, 2008). In addition, evidence of moderate heteroscedasticity was present in the equation for mindfulness predicting shame. To address this issue, we normalized the mindfulness and shame variables by applying square root transformations and obtained parallel results (raw scores are reported for the ease of interpretation). Assumptions of homoscedasticity were met in all other analyses. The coefficient of determination (R2, R2adjusted), standardized beta coefficients (β), and 95% confidence intervals are reported for all focal results. All reported p values are two-tailed. All analyses were performed in R (v3.0.1, www.r-project.org) using the R-studio interface (v0.98.1103) and the Statistical Package for Social Science software (IBM SPSS Statistics 21).
Results
Effect of Mindfulness on Negative Affect
Participants’ dispositional mindfulness did not significantly differ with respect to age, gender, ethnicity, or education (ps>.50). We first tested whether dispositional mindfulness measured at baseline (T1) predicted negative affect generally and shame specifically, following exposure to health messages. Two regression analyses with mindfulness as a predictor and negative affect and shame, separately, as an outcome variable revealed a significant effect of mindfulness on decreased general negative affect and shame, such that those with greater dispositional mindfulness reported lower general negative affect, R2step2=.175, R2adjusted=.161, β=−.419, t(58)=−3.512, p<.001, 95% CI [−0.343, −0.094], and shame R2step2=.143, R2adjusted=.128, β=−.378, t(57)=−3.083, p=.003, 95% CI [−0.498, −0.106], after the health message intervention. Mindfulness was not associated with positive affect following the health message intervention, R2=.006, R2adjusted=.−.011, β=.076, t(58)=.580, p=.565, 95% CI [−0.165, 0.300].
Effect of Mindfulness on Exercise Outcomes
We next examined the impact of dispositional mindfulness on our primary, proximal outcome: changes in exercise motivation. Exercise motivation scores at T1, T2, and T3 were significantly correlated (rmean=.847, ps<.001; See Table 2). Two hierarchical regression analyses tested our hypothesis that those with higher dispositional mindfulness would report a greater increase in exercise motivation. In each regression model, T1 exercise motivation was entered as a covariate at Step 1, and mindfulness as a predictor at Step 2; exercise motivation at T2 and T3, separately, were entered as an outcome variable (Table 3). Greater dispositional mindfulness was associated with a non-significant (marginal) increase in exercise motivation at T2, R2step2=.845, R2adjusted=.839, ΔR2=.010, β=.099, t(57)=1.875, p=.066, 95% CI [−0.046, 1.389], and a significant increase in exercise motivation at T3 with modest effect size, R2step2=.698, R2adjusted=.687, ΔR2=.047, β=.219, t(56)=2.952, p=.005, 95% CI [0.479, 2.500].
Table 2.
Zero-order Correlations of Predictor Variables and Main Outcome Measures
| Mindfulness (MAAS; n=66) | Negative Affect (PANAS; n=61) | Shame (PANAS; n=60) | T1 Exercise Motivation (BREQ-2; n=67) | T2 Exercise Motivation (BREQ-2; n=61) | T3 Exercise Motivation (BREQ-2; n=60) | |
|---|---|---|---|---|---|---|
| Mindfulness | - | −.42** | −.38** | .14 | .25 | .33* |
| Negative Affect | - | .79** | −.33* | −.37** | −.53* | |
| Shame | - | −.35** | −.35** | −.55** | ||
| T1 Exercise Motivation | - | .91** | .81** | |||
| T2 Exercise Motivation | - | .82** | ||||
| T3 Exercise Motivation | - |
Note: BREQ-2 = Behavioral Regulation in Exercise Questionnaire-version 2; MAAS = Mindful Attention Awareness Scale; PANAS = Positive and Negative Affect Scale. Pearson product-moment correlation coefficients are displayed.
p < .05,
p < .01.
Table 3.
Hierarchical multiple regression analyses assessing mindfulness as a predictor of exercise motivation at T2 and T3
| β | t | p | R2 | ΔR2 | |
|---|---|---|---|---|---|
| T2 Exercise Motivation | |||||
| Step 1 | .835 | ||||
| T1 Exercise Motivation | .914 | 17.150 | .000 | ||
| Step 2 | .845 | .010 | |||
| T1 Exercise Motivation | .897 | 16.953 | .000 | ||
| Mindfulness | .099 | 1.875 | .066 | ||
|
| |||||
| T3 Exercise Motivation | |||||
| Step 1 | .651 | ||||
| T1 Exercise Motivation | .807 | 10.313 | .000 | ||
| Step 2 | .698 | .047 | |||
| T1 Exercise Motivation | .775 | 10.437 | .000 | ||
| Mindfulness | .219 | 2.952 | .005 | ||
Note: Exercise motivation was measured by the Behavioral Regulation in Exercise Questionnaire-version 2 (BREQ- 2); Mindfulness was measured by the Mindful Attention Awareness Scale (MAAS). Standardized beta coefficients are reported.
Next, we examined the impact of dispositional mindfulness on more distal changes in self-reported weekly minutes of vigorous and moderate physical activity and walking. In three hierarchical regression models, self-reported vigorous activity, moderate activity, and walking at T1 were separately entered as a covariate at Step 1, and mindfulness was entered as a predictor at Step 2. Self-reported vigorous activity, moderate activity, and walking at T3 was entered as an outcome. Mindfulness predicted increases in self-reported vigorous activity, R2step2=.118, R2adjusted = .083, ΔR2=.095, β=.314, t(50)=2.322, p=.024, 95% CI [29.620, 409.566]. However, additional regression analyses revealed a non-significant effect of mindfulness on changes in self-reported moderate activity (p=.680) and walking minutes (p=.777). In addition, changes in exercise motivation were positively correlated with self-reported vigorous physical activity (r=.337, p=.013), suggesting that motivation was relevant to at least one important behavioral outcome. Our measure of exercise motivation, however, was not associated with moderate activity or walking (ps>.40). None of the subdomains of self-reported physical activity were associated with feelings of shame following exposure to the health messages (ps>.10).
Lastly, we examined the impact of dispositional mindfulness on changes in daily physical activity as measured by accelerometers. A hierarchical regression analysis with T1–T2 baseline activity entered as a covariate at Step 1, mindfulness as a predictor at Step 2, and T2–T3 activity as outcome variable revealed no significant association between mindfulness and changes in daily physical activity, R2step2=.572, R2adjusted=.552, ΔR2=.004, β=.064, t(42)=0.631, p=.531, 95% CI [−24.108, 46.039]. In addition, changes in daily physical activity was not associated with exercise motivation (p=.584), subcategories of self-reported physical activity (ps>.20), or feelings of shame after exposure to the health messages (p=.436).
Mediation Tests: Mindfulness, Negative Affect and Shame, and Exercise Motivation
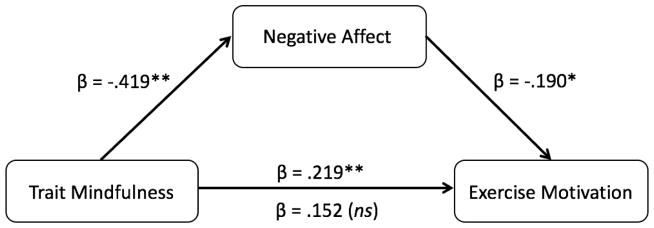
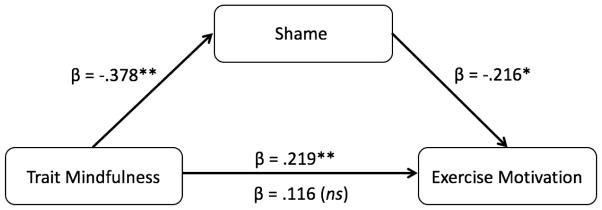
Given our theoretical framework and positive results linking mindfulness, negative affect and exercise motivation, we followed the analyses above with formal tests of mediation. Two hierarchical regression models included T1 exercise motivation at Step 1, mindfulness at Step 2, and negative affect and shame, separately for each model, at Step 3, with T3 exercise motivation as an outcome variable. Supportive of mediation, mindfulness no longer significantly predicted increased exercise motivation when accounting for negative affect recorded after the health message, β=.152, t(54)=1.920, p=.060, 95% CI [−0.046, 2.138] while negative affect did, β=−.190, t(54)=−2.203, p=.032, 95% CI [−4.842, −0.228], with lower negative affect predicting greater increases in motivation, R2step3=.724, R2adjusted=.709, ΔR2Step 2–3=.025. Results from a formal bootstrap test of mediation (Figure 2a) supported our prediction: The indirect effect from greater mindfulness to lower negative affect to increased exercise motivation was significant (bias corrected confidence intervals: 0.0196 to 1.1628, which does not contain 0).
Figure 2.
Heuristic models of the predicted relationships between dispositional mindfulness and (a) general negative affect and (b) shame on exercise motivation at T3. Formal tests of mediation (bootstrapping; Preacher & Hayes, 2008) provided evidence that both general negative affect and shame mediated the effect of mindfulness on increased motivation to exercise one month after the health message presentation (bias corrected confidence intervals=0.0196 to 1.1628 and 0.0049 to 1.4982 for negative affect and shame, respectively).
Note: *p<.05, **p<.01.
a. Mediation by negative affect
b. Mediation by shame
Specifically, among the negative affect items, the mediating effect was driven by lower feelings of shame among highly mindful people (Figure 2b). The effect of mindfulness on exercise motivation at T3 disappeared, β=.116, t(53)=1.528, p=.133, 95% CI [−0.253, 1.868] when shame, mindfulness, and exercise motivation at T1 were considered as predictor variables, while effect of shame on exercise motivation at T3 remained significant, β=−.216, t(53)=−2.652, p=.011, 95% CI [−3.322, −0.461], with lower shame predicting increased motivation, R2step3=.740, R2adjusted=.725, ΔR2Step 2–3=.035. Results from a bootstrap test of mediation revealed that decreased feelings of shame fully mediated the effect of mindfulness on increased motivation to exercise (bias corrected confidence intervals: 0.0049 to 1.4982, which does not contain 0). No other positive or negative discrete affect items mediated the indirect effect of mindfulness on exercise motivation.
Covariates: Baseline exercise minutes, BMI, and Depression
Next, we examined baseline exercise minutes, BMI, and depression as covariates, and obtained parallel results when controlling for each one of them. Baseline exercise minutes and BMI, respectively, were not associated with mindfulness (p=.667, p=.136), negative affect (p=.743, p=.676), shame (p=.675, 693), or changes in exercise motivation (p=.743, .815), and did not interact with mindfulness in predicting exercise motivation (p=.358, .726).
Replicating previous findings (Argus & Thompson, 2008; Christopher & Gilbert, 2010; Paul et al., 2013), depression was negatively correlated to mindfulness (r=−.480, p<.001) and positively correlated with negative affect (r=.525, p<.001) and shame (r=.404, p=.001) post message intervention. However, depression was not associated with the changes in exercise motivation (p=.256) and did not interact with mindfulness in predicting exercise motivation (p=.663), suggesting that effects of negative affect and shame on exercise motivation are not merely an effect of more negative affect at baseline.
Discussion
Adaptive affective responses to health messages may contribute to successful health communication. The current study tests the effect of dispositional mindfulness on affective responses to health messages and subsequent health-relevant outcomes. Dispositional mindfulness predicted greater increases in self-reported motivation to exercise a month after the exposure to potentially threatening health messages, as well as increased self-reports of vigorous physical activity a month after the health message intervention with modest effect size. Furthermore, the effect of mindfulness on exercise motivation was fully mediated by decreased self-reported general negative affect and shame in response to health messages among those with higher vs. lower dispositional mindfulness. These effects were not explained by baseline exercise or BMI, suggesting that mindfulness may be important across groups.
The present findings suggest that shame-inducing messages can elicit defensive reactivity and negative health outcomes. Furthermore, no other specific negative affect items mediated the effect of mindfulness, suggesting the specificity of shame as a detrimental affective state, associated with decreased exercise motivation in response to health communication.
In considering the mechanisms through which mindfulness might reduce deleterious affective reactivity that hinders positive health outcomes, at least two conceptually distinct paths may exist and relate to negative affective responses: affect induced by messages, or general affective states after the message intervention that are incidental to the message. That is, individuals with greater dispositional mindfulness might experience less negative affect in response to potentially threatening health messages, and/or highly mindful individuals might experience lower negative affect regardless of the message intervention. The current data suggest greater support for the former given that depression scores at baseline did not predict changes in exercise motivation on their own or in interaction with mindfulness, and all reported results held when controlling for baseline depression. We thus suggest that negative affect was likely induced by the messages and that mindfulness may buffer the tendency to experience negative affect, and shame specifically, in response to such messages. State affect was not collected prior to health messages to avoid bias in processing. However, additional research that collects state affect at multiple time points would add to our understanding of the temporal relationships among these variables.
Another possible mechanism through which mindful awareness can reduce the detrimental effects of self-defensiveness is by reconfiguring the sense of self that no longer needs to be defended. Mindfulness in several forms has previously been associated with decreased attachment to the idea of a stable and unchanging sense of self (e.g., Hölzel et al., 2011; Langer, 1989). Therefore, mindfulness may augment the effects of other interventions designed to shape the sense of self in a desirable way. Future studies may further examine mechanisms through which mindfulness predicts adaptive health message processing by transforming self-concepts. For example, lovingkindness meditation and compassion meditation explicitly aim to cultivate self-transcending compassionate attitudes toward all beings (e.g., Kang, Gray, Dovidio, 2014), and thus may relate to lower perceived need to defend oneself (Kang et al., 2013).
Given the mounting evidence on the benefits of mindfulness and mindfulness practice, it is worth noting that mindfulness was not associated with positive affect in this study. In the domain of affect, this result is consistent with previous findings in which mindfulness was associated with decreased overall affective reactivity to all positive, negative, and neutral stimuli, indexed by generalized decreases in activity within the right amygdala (Desbordes et al., 2012). Mindfulness may be associated with measures of more eudaimonic wellbeing that relate to self-transcendent flourishing, rather than self-enhancing hedonic pleasure (Taylor et al., 2014). We encourage future studies to test this potential divergence. Experiments that manipulate mindfulness beyond assessing dispositional mindfulness would be particularly informative.
Another conceptualization of mindfulness refers to openness to new information and awareness of multiple perspectives by creating new categories (Langer, 1989). This conceptualization of mindfulness has been implicated in a wide range of positive health outcomes, such that simple manipulations to induce open and flexible attitudes to incoming information have been associated with decreased mortality (Rodin & Langer, 1977) and other indices related to health such as BMI (Crum & Langer, 2007). Although this conceptualization of mindfulness has overlapping qualities with the form of mindful attention that is the focus of the current investigation, major differences between two conceptualizations are proposed (Kang, Gruber, & Grey, 2014), which may lead to distinctive downstream consequences. Future work may explicitly compare these two types of mindfulness in order to test potentially unique and/or shared mechanisms through which they may promote openness to health messages and subsequent positive health effects. In addition, future studies may also utilize multiple mindfulness scales that capture multidimensional qualities of distinctive conceptualizations of mindfulness to test convergence or divergence of the current findings.
Findings from the present study should be interpreted in the context of the study’s strengths and limitations, which suggest opportunities for future research. Taken together, our data demonstrate novel predictors of health communication effects on exercise motivation. However, several potential boundary conditions would be of interest to address. First, dispositional mindfulness may be qualitatively different from meditation-oriented mindfulness, a quality developed through meditation practice (Desbordes & Negi, 2013). Future studies that use meditation intervention programs to directly test the potentially divergent effects of dispositional vs. learned mindfulness in the context of health communications are warranted. Second, although numerous previous studies report that dispositional mindfulness (e.g., MAAS) has strong and lasting influence on various outcomes (e.g., Barnes et al., 2007; Brown & Ryan, 2003; Jordan et al., 2014; Murphy et al, 2012; Way et al., 2010), the present longitudinal data may only suggest predictive validity of the current findings. Therefore, experimental studies are needed to test whether increasing mindfulness through meditation practice can prospectively reduce the harmful effect of negative affect and shame. Third, although the current analyses included and controlled for three potential covariates (baseline exercise minutes, BMI, and depression were examined based on their potential associations to mindfulness, affective reactivity, and/or exercise motivations), other potential covariates that have both been associated with mindfulness and health outcomes such as trait anxiety (Miller, Fletcher, & Kabat-Zinn, 1995) or stress (Grossman, Niemann, Schmidt, & Walach, 2004) should be assessed and controlled for in future studies. In addition, future studies may use objectively measured (vs. self-reported) BMI scores. Fourth, several types of messages were presented, including those highlighting the risk of sedentary behavior, benefits of an active lifestyle, and strategies to become more active and less sedentary. To reduce the possibility that the reported effect is conditional on having multiple types of messages from the same source, future studies may concentrate on a focal construct in presenting threat messages. Fifth, daily health messages were delivered to participants via SMS, but responses were not required. Future studies may elicit SMS feedback from participants to confirm their receipt and track the changes in exercise outcomes. In addition, self-reported physical activity was assessed only at T1 and T3, but not T2. Future studies may obtain self-reported physical activity data more continuously and potentially integrate them with the accelerometer data. Finally, perceived threat in response to the health messages was not assessed. Measures of threat perception can be included in future studies to strengthen our understanding and interpretation of the shown effect.
Future research using multiple methods for assessing physical activity may also help reconcile selective effects of mindfulness on self-reports of vigorous physical activity. Dispositional mindfulness did not significantly predict changes in self-reported moderate activity or daily physical activity as measured by accelerometer. It is possible that the wrist-worn accelerometers employed in this study may not have been sensitive enough to capture certain vigorous activities such as bicycling. Indeed, self-reported vigorous recreational activity which included bicycling was significantly associated with mindfulness (p=.024), but this may have not been reflected in the accelerometer data. It is also possible that mindfulness was associated with participants’ perceptions of their physical activity, but less to measurable, physical changes. Another possibility is that our primary, proximal theoretical outcome (exercise motivation) may relate to behavior change beyond the one-month timescale that we measured. In addition, given the modest effect size of mindfulness predicting exercise outcomes, future studies may use longer-term longitudinal designs and incorporate more comprehensive measures of physical activity to further examine the magnitude and duration of effects. Nevertheless, the current research offers evidence that dispositional mindfulness should be carefully considered in future health intervention strategies, with different approaches potentially exerting more powerful effects for those beginning at different levels of mindfulness.
Supplementary Material
A complete list of health messages used in the health message intervention
A complete list of survey measures used in the current study
Acknowledgments
Funding: This research was funded by The Michigan Center of Excellence in Cancer Communication Research/NIH Grant P50 CA101451 [principal investigator (PI), V.J. S.], NIH New Innovator Award 1DP2DA03515601 (PI, E.B.F), and NIH/National Cancer Institute Grant 1R01CA180015-01 (PI, E.B.F). We also thank HopeLab for generous support.
This study was a part of a larger investigation on neural predictors of health behavior change (reported in Cascio et al., 2016; Falk et al., 2015). Although health related outcomes are included in those previous reports, no reports using this data have focused on individual differences in mindfulness and subsequent motivation changes. We thank Chris Cascio, Kristin Shumaker, and Frank Tinney for research assistance, Larry An, Ken Resnicow, Thad Polk, and Angie Fagerlin for helpful discussions and input, Holly Derry, Ian Moore, and Michele Demers for assistance in developing intervention materials, and the staff of the University of Michigan fMRI Center for support and assistance.
Footnotes
Compliance with Ethical Standards
Conflict of Interest: The authors declare that they have no conflict of interest.
Contributor Information
Yoona Kang, Annenberg School for Communication, University of Pennsylvania, 3620 Walnut street Philadelphia, PA 19104.
Matthew Brook O’Donnell, Annenberg School for Communication, University of Pennsylvania.
Victor J. Strecher, School of Public Health, University of Michigan
Emily B. Falk, Annenberg School for Communication, University of Pennsylvania
References
- Agrawal N, Duhachek A. Emotional compatibility and the effectiveness of antidrinking messages: A defensive processing perspective on shame and guilt. Journal of Marketing Research. 2010;47(2):263–273. [Google Scholar]
- Argus G, Thompson M. Perceived social problem solving, perfectionism, and mindful awareness in clinical depression: An exploratory study. Cognitive Therapy and research. 2008;32(6):745–757. [Google Scholar]
- Barnes S, Brown KW, Krusemark E, Campbell WK, Rogge RD. The role of mindfulness in romantic relationship satisfaction and responses to relationship stress. Journal of marital and family therapy. 2007;33(4):482–500. doi: 10.1111/j.1752-0606.2007.00033.x. [DOI] [PubMed] [Google Scholar]
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Archives of general psychiatry. 1961;4(6):561. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- Becker MH. The health belief model and personal health behavior 1974 [Google Scholar]
- Black DS. Incorporating mindfulness within established theories of health behavior. Complementary Health Practice Review. 2010;15(2):108–109. [Google Scholar]
- Black DS, Sussman S, Johnson C, Milam J. Trait mindfulness helps shield decision-making from translating into health-risk behavior. Journal of Adolescent Health. 2012;51(6):588–92. doi: 10.1016/j.jadohealth.2012.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown KW, Goodman RJ, Inzlicht M. Dispositional mindfulness and the attenuation of neural responses to emotional stimuli. Social cognitive and affective neuroscience. 2013;8(1):93–99. doi: 10.1093/scan/nss004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown KW, Ryan RM. The benefits of being present: mindfulness and its role in psychological wellbeing. Journal of personality and social psychology. 2003;84(4):822. doi: 10.1037/0022-3514.84.4.822. [DOI] [PubMed] [Google Scholar]
- Brown KW, Ryan RM, Creswell JD. Addressing fundamental questions about mindfulness. Psychological Inquiry. 2007a;18(4):272–281. [Google Scholar]
- Brown KW, Ryan RM, Creswell JD. Mindfulness: Theoretical foundations and evidence for its salutary effects. Psychological Inquiry. 2007b;18(4):211–237. [Google Scholar]
- Bylsma LM, Morris BH, Rottenberg J. A meta-analysis of emotional reactivity in major depressive disorder. Clinical psychology review. 2008;28(4):676–691. doi: 10.1016/j.cpr.2007.10.001. [DOI] [PubMed] [Google Scholar]
- Cascio C, O’Donnell MB, Tinney F, Lieberman M, Taylor S, Stretcher V, Falk EB. Self-affirmation activates brain systems associated with self-related processing and reward and is reinforced by future orientation. Social Cognitive and Affective Neuroscience. 2016;11(4):621–629. doi: 10.1093/scan/nsv136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaiken S. Defensive processing of personally relevant health messages. Personality and Social Psychology Bulletin. 1992;18(6):669–679. [Google Scholar]
- Chatzisarantis NL, Hagger MS. Mindfulness and the intention-behavior relationship within the theory of planned behavior. Personality and Social Psychology Bulletin. 2007;33(5):663–76. doi: 10.1177/0146167206297401. [DOI] [PubMed] [Google Scholar]
- Christopher MS, Gilbert BD. Incremental validity of components of mindfulness in the prediction of satisfaction with life and depression. Current Psychology. 2010;29(1):10–23. [Google Scholar]
- Craig CL, Marshall AL, Sjostrom M, Bauman AE, Booth ML, Ainsworth BE, et al. International physical activity questionnaire: 12-country reliability and validity. Medicine & Science in Sports & Exercise. 2003;195(9131/03):3508–1381. doi: 10.1249/01.MSS.0000078924.61453.FB. http://www.ipaq.ki.se/scoring.pdf. [DOI] [PubMed] [Google Scholar]
- Creswell JD, Way BM, Eisenberger NI, Lieberman MD. Neural correlates of dispositional mindfulness during affect labeling. Psychosomatic Medicine. 2007;69(6):560–565. doi: 10.1097/PSY.0b013e3180f6171f. [DOI] [PubMed] [Google Scholar]
- Crum AJ, Langer EJ. Mind-Set Matters Exercise and the Placebo Effect. Psychological Science. 2007;18(2):165–171. doi: 10.1111/j.1467-9280.2007.01867.x. [DOI] [PubMed] [Google Scholar]
- Desbordes G, Negi LT. A new era for mind studies: training investigators in both scientific and contemplative methods of inquiry. Frontiers in human neuroscience. 2013:7. doi: 10.3389/fnhum.2013.00741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Desbordes G, Negi LT, Pace TW, Wallace BA, Raison CL, Schwartz EL. Effects of mindful-attention and compassion meditation training on amygdala response to emotional stimuli in an ordinary, non-meditative state. Frontiers in human neuroscience. 2012;6 doi: 10.3389/fnhum.2012.00292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickerson SS, Gruenewald TL, Kemeny ME. When the social self is threatened: Shame, physiology, and health. Journal of personality. 2004;72(6):1191–1216. doi: 10.1111/j.1467-6494.2004.00295.x. [DOI] [PubMed] [Google Scholar]
- Do Lee C, Folsom AR, Blair SN. Physical activity and stroke risk a meta-analysis. Stroke. 2003;34(10):2475–2481. doi: 10.1161/01.STR.0000091843.02517.9D. [DOI] [PubMed] [Google Scholar]
- Earl A, Albarracín D. Nature, decay, and spiraling of the effects of fear-inducing arguments and HIV counseling and testing: a meta-analysis of the short-and long-term outcomes of HIV-prevention interventions. Health Psychology. 2007;26(4):496. doi: 10.1037/0278-6133.26.4.496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esliger DW, Rowlands AV, Hurst TL, Catt M, Murray P, Eston RG. Validation of the GENEA Accelerometer. Medicine and science in sports and exercise. 2011;43(6):1085–1093. doi: 10.1249/MSS.0b013e31820513be. [DOI] [PubMed] [Google Scholar]
- Falk EB, O’Donnell MB, Cascio CN, Tinney F, Kang Y, Lieberman MD, … Strecher VJ. Self-affirmation alters the brain’s response to health messages and subsequent behavior change. Proceedings of the National Academy of Sciences. 2015;112(7):1977–1982. doi: 10.1073/pnas.1500247112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gregg EW, Cauley JA, Stone K, Thompson TJ, Bauer DC, Cummings SR … Group, S. o. O. F. R. Relationship of changes in physical activity and mortality among older women. Journal of the American Medical Association. 2003;289(18):2379–2386. doi: 10.1001/jama.289.18.2379. [DOI] [PubMed] [Google Scholar]
- Grossman P, Niemann L, Schmidt S, Walach H. Mindfulness-based stress reduction and health benefits: A meta-analysis. Journal of psychosomatic research. 2004;57(1):35–43. doi: 10.1016/S0022-3999(03)00573-7. [DOI] [PubMed] [Google Scholar]
- Holmes MD, Chen WY, Feskanich D, Kroenke CH, Colditz GA. Physical activity and survival after breast cancer diagnosis. Journal of the American Medical Association. 2005;293(20):2479–2486. doi: 10.1001/jama.293.20.2479. [DOI] [PubMed] [Google Scholar]
- Hölzel BK, Lazar SW, Gard T, Schuman-Olivier Z, Vago DR, Ott U. How does mindfulness meditation work? Proposing mechanisms of action from a conceptual and neural perspective. Perspectives on Psychological Science. 2011;6(6):537–559. doi: 10.1177/1745691611419671. [DOI] [PubMed] [Google Scholar]
- Jordan CH, Wang W, Donatoni L, Meier BP. Mindful eating: Trait and state mindfulness predict healthier eating behavior. Personality and Individual Differences. 2014;68:107–111. [Google Scholar]
- Kang Y, Gray JR, Dovidio JF. The nondiscriminating heart: Lovingkindness meditation training decreases implicit intergroup bias. Journal of Experimental Psychology: General. 2014;143(3):1306. doi: 10.1037/a0034150. [DOI] [PubMed] [Google Scholar]
- Kang Y, Gruber J, Gray JR. Mindfulness and De-Automatization. Emotion Review. 2013;5(2):192–201. [Google Scholar]
- Kang Y, Gruber J, Gray JR. Mindfulness: Deautomatization of Cognitive and Emotional Life. The Wiley Blackwell Handbook of Mindfulness. 2014:168–185. [Google Scholar]
- Langer EJ. Mindfulness. Addison-Wesley/Addison Wesley Longman; 1989. [Google Scholar]
- Lee IM, Hsieh C-c, Paffenbarger RS. Exercise intensity and longevity in men: the Harvard Alumni Health Study. Journal of the American Medical Association. 1995;273(15):1179–1184. [PubMed] [Google Scholar]
- Manson JE, Hu FB, Rich-Edwards JW, Colditz GA, Stampfer MJ, Willett WC, … Hennekens CH. A prospective study of walking as compared with vigorous exercise in the prevention of coronary heart disease in women. New England Journal of Medicine. 1999;341(9):650–658. doi: 10.1056/NEJM199908263410904. [DOI] [PubMed] [Google Scholar]
- Markland DA. Exercise motivation measurement-BREQ and BREQ-2 scoring. 2011 Mar 3; http://pages.bangor.ac.uk/~pes004/exercise_motivation/breq/breq.htm.
- Markland D, Tobin V. A modification to the Behavioural Regulation in Exercise Questionnaire to include an assessment of amotivation. Journal of sport & exercise psychology. 2004;26(2) [Google Scholar]
- Mendolia M. Repressors’ appraisals of emotional stimuli in threatening and nonthreatening positive emotional contexts. Journal of Research in Personality. 1999;33(1):1–26. [Google Scholar]
- Miller JJ, Fletcher K, Kabat-Zinn J. Three-year follow-up and clinical implications of a mindfulness meditation-based stress reduction intervention in the treatment of anxiety disorders. General hospital psychiatry. 1995;17(3):192–200. doi: 10.1016/0163-8343(95)00025-m. [DOI] [PubMed] [Google Scholar]
- Miners R. Collected and connected: mindfulness and the early adolescent. Concordia University; 2007. [Google Scholar]
- Moore SC, Patel AV, Matthews CE, de Gonzalez AB, Park Y, Katki HA, … Helzlsouer KJ. Leisure time physical activity of moderate to vigorous intensity and mortality: a large pooled cohort analysis. PLoS medicine. 2012;9(11):e1001335. doi: 10.1371/journal.pmed.1001335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy MJ, Mermelstein LC, Edwards KM, Gidycz CA. The benefits of dispositional mindfulness in physical health: a longitudinal study of female college students. Journal of American College Health. 2012;60(5):341–348. doi: 10.1080/07448481.2011.629260. [DOI] [PubMed] [Google Scholar]
- Owen N, Healy GN, Matthews CE, Dunstan DW. Too much sitting: the population-health science of sedentary behavior. Exercise and sport sciences reviews. 2010;38(3):105. doi: 10.1097/JES.0b013e3181e373a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paul NA, Stanton SJ, Greeson JM, Smoski MJ, Wang L. Psychological and neural mechanisms of trait mindfulness in reducing depression vulnerability. Social cognitive and affective neuroscience. 2013;8(1):56–64. doi: 10.1093/scan/nss070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters GJY, Ruiter RA, Kok G. Threatening communication: a critical re-analysis and a revised meta-analytic test of fear appeal theory. Health psychology review. 2013;7(sup1):S8–S31. doi: 10.1080/17437199.2012.703527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior research methods. 2008;40(3):879–891. doi: 10.3758/brm.40.3.879. http://www.afhayes.com/spss-sas-and-mplus-macros-and-code.html. [DOI] [PubMed] [Google Scholar]
- Randles D, Tracy JL. Nonverbal displays of shame predict relapse and declining health in recovering alcoholics. Clinical Psychological Science. 2013;1(2):149–155. [Google Scholar]
- Resnicow K, McMaster F. Motivational interviewing: Moving from why to how with autonomy support. International Journal of Behavioral Nutrition and Physical Activity. 2012;9(1):1–9. doi: 10.1186/1479-5868-9-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodin J, Langer EJ. Long-term effects of a control-relevant intervention with the institutionalized aged. Journal of personality and social psychology. 1977;35(12):897. doi: 10.1037//0022-3514.35.12.897. [DOI] [PubMed] [Google Scholar]
- Schwarzer R, Luszczynska A. How to overcome health-compromising behaviors: The health action process approach. European Psychologist. 2008;13(2):141. [Google Scholar]
- Seguin R, LaMonte M, Tinker L, Liu J, Woods N, Michael YL, … LaCroix AZ. Sedentary behavior and physical function decline in older women: findings from the Women’s Health Initiative. Journal of aging research. 2012 doi: 10.1155/2012/271589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slattery M, Edwards S, Curtin K, Ma K, Edwards R, Holubkov R, Schaffer D. Physical activity and colorectal cancer. American journal of epidemiology. 2003;158(3):214–224. doi: 10.1093/aje/kwg134. [DOI] [PubMed] [Google Scholar]
- Tanasescu M, Leitzmann MF, Rimm EB, Willett WC, Stampfer MJ, Hu FB. Exercise type and intensity in relation to coronary heart disease in men. Journal of the American Medical Association. 2002;288(16):1994–2000. doi: 10.1001/jama.288.16.1994. [DOI] [PubMed] [Google Scholar]
- Tangney JP, Dearing RL. Shame and guilt. Guilford Press; 2004. [Google Scholar]
- Taylor SA, Black HG, Donovan LAN, Ishida C, Judson K. The relationship between eudaimonic well-being and social well-being with millennials. Journal of Consumer Satisfaction, Dissatisfaction & Complaining Behavior. 2014;27 [Google Scholar]
- Vartanian LR, Shaprow JG. Effects of Weight Stigma on Exercise Motivation and Behavior A Preliminary Investigation among College-aged Females. Journal of Health Psychology. 2008;13(1):131–138. doi: 10.1177/1359105307084318. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. Journal of personality and social psychology. 1988;54(6):1063. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Way BM, Creswell JD, Eisenberger NI, Lieberman MD. Dispositional mindfulness and depressive symptomatology: correlations with limbic and self-referential neural activity during rest. Emotion. 2010;10(1):12. doi: 10.1037/a0018312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witte K, Allen M. A meta-analysis of fear appeals: Implications for effective public health campaigns. Health Education & Behavior. 2000;27(5):591–615. doi: 10.1177/109019810002700506. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A complete list of health messages used in the health message intervention
A complete list of survey measures used in the current study