Abstract
Objective
This study examined the prevalence of and changes in loss of control over eating (LOC) among pregnant women with overweight/obesity, along with associations between LOC and depressive symptoms and stress.
Method
Community women (N=200; BMI≥25; 12–20 weeks gestation) reported LOC before and during early pregnancy using the Eating Disorder Examination, which was adapted for administration in pregnancy. Women self-reported depressive symptoms and stress during early pregnancy.
Results
Twenty-eight percent (n=56) of women reported LOC before or during early pregnancy: 14.5% (n=29) reported LOC incidence during early pregnancy, 9.5% (n=19) reported LOC persistence from pre-pregnancy to early pregnancy, and 4.0% (n=8) reported LOC pre-pregnancy only. Women with LOC reported more depressive symptoms and stress than did those without. Women with LOC persistence reported clinically-significant depressive symptoms and elevated stress. Levels of depressive symptoms and stress differed between women with LOC persistence and those without LOC (ps<.05).
Discussion
LOC during pregnancy was prevalent and associated with distress, particularly when present before and during pregnancy. Among women with LOC, few reported remission, but one-half reported onset during early pregnancy. Longitudinal studies are needed among mothers with overweight/obesity to identify patterns of LOC throughout pregnancy and how LOC affects perinatal outcomes.
Keywords: Loss of control, pregnancy, obesity, overweight, community sample
Women who begin pregnancy with overweight or obesity often have greater gestational weight gain (GWG) than is recommended and retain more weight postpartum (1). One eating behavior that may impact GWG is loss of control over eating (LOC), the feeling that one cannot stop eating or control what or how much one is eating (2). LOC is associated with higher body mass index (BMI) (3), weight gain (4), and psychological distress among non-pregnant individuals (2, 4–8).
In a community-based study, LOC was reported by one-third of pregnant women with obesity who did not have an eating disorder, using a single-item (9). In a study of women with eating disorders, LOC episodes decreased for nearly half and persisted for the remainder of women during pregnancy (10). There are scant data on how LOC rates change from pre-pregnancy to pregnancy, and studies of prenatal LOC have utilized varied samples (e.g., community cohorts, women with eating disorders), assessment methods (e.g., interviews, questionnaires, single-items), and measurement periods (e.g., pre-pregnancy and pregnancy, pregnancy only) (9–11). Women with obesity may experience LOC incidence as they gain weight and their eating changes during pregnancy, and may experience increased distress. However, to date, there have been no interview-based data evaluating LOC before and during early pregnancy or in relation to distress among community women with overweight/obesity.
Accordingly, we assessed LOC via interview to describe the prevalence of and changes in LOC across the period before and during early pregnancy in a community sample of women with overweight/obesity. We evaluated when LOC was endorsed (pre-pregnancy, during pregnancy), and associations between LOC and demographic and weight-related variables, depressive symptoms, and stress. We hypothesized that LOC, and particularly LOC persistence from pre-pregnancy to early pregnancy, would relate to higher prenatal BMI, weight gain, depressive symptoms, and stress.
Methods
Participants
Two hundred pregnant women completed assessments between 12–20 weeks gestation (Table 1).
Table 1.
Demographic and weight-related characteristics of the sample.
| Variable | All Participants (N = 200) Mean (SD) or n (%) |
No LOC (n = 144) Mean (SD) or n (%) |
LOC Incidence (n = 29) Mean (SD) or n (%) |
LOC Persistence (n = 19) Mean (SD) or n (%) |
|---|---|---|---|---|
| Age (years) | 27.675 (5.525) | 27.43 (5.33) | 28.69 (6.04) | 28.53 (6.60) |
| BMI prior to pregnancy (kg/m2) | 32.885 (6.782) | 33.11 (6.83) | 30.96 (5.23) | 34.43 (8.59) |
| BMI during early pregnancy (kg/m2) | 34.135 (7.228) | 34.32 (7.38) | 32.44 (6.13) | 35.65 (8.30) |
| Gestational age to date (weeks) | 15.321 (2.403) | 15.36 (2.37) | 15.13 (2.56) | 15.58 (2.50) |
| Weight gain during early pregnancy (kg) | 3.440 (6.950) | 3.36 (7.19) | 4.15 (5.96) | 3.11 (7.37) |
| Gravidity (number of pregnancies) | 2.910 (2.324) | 2.81 (2.28) | 3.55 (2.49) | 2.89 (2.64) |
| Parity (number of births) | 1.180 (1.377) | 1.09 (1.3) | 1.59 (1.52) | 1.42 (1.80) |
| Intentional pregnancy | ||||
| Yes | 92 (46.0%) | 72 (50.0%) | 17 (58.6%) | 14 (73.7%) |
| No | 108 (54.0%) | 72 (50.0%) | 12 (41.4%) | 5 (26.3%) |
| Education | ||||
| Grade school or some high school | 23 (11.6%) | 14 (9.7%) | 6 (20.7%) | 3 (15.8%) |
| High school graduate/GED | 46 (23.1%) | 34 (23.6%) | 5 (17.2%) | 4 (21.1%) |
| Some college/technical school | 78 (39.2%) | 54 (37.5%) | 13 (44.8%) | 9 (47.4%) |
| 4-year college graduate | 22 (11.1%) | 18 (12.5%) | 2 (6.9%) | 2 (10.5%) |
| Post-graduate degree | 30 (15.1%) | 23 (16.0%) | 3 (10.3%) | 1 (5.3%) |
| Race | ||||
| White or Caucasian | 89 (44.5%) | 70 (48.6%) | 8 (27.6%) | 9 (47.4%) |
| Black or African American | 88 (44.0%) | 61 (42.4%) | 16 (55.2%) | 7 (36.8%) |
| Mixed race | 19 (9.5%) | 10 (6.9%) | 4 (13.8%) | 3 (15.8%) |
| American Indian/Alaska Native | 1 (0.5%) | 1 (0.7%) | 1 (3.4%) | 0 (0.0%) |
| Ethnicity (Hispanic/Latina) | ||||
| Yes | 7 (3.5%) | 4 (2.8%) | 2 (6.9%) | 1 (5.3%) |
| No | 193 (96.5%) | 140 (97.2%) | 27 (93.1%) | 18 (94.7%) |
| Income | ||||
| ≤$30,000 | 135 (67.8%) | 94 (65.3%) | 23 (79.3%) | 13 (68.4%) |
| >$30,000 | 65 (32.5%) | 49 (34.0%) | 6 (20.7%) | 6 (31.6%) |
| Pre-pregnancy LOC episode frequency (range) | 0–132 | 0 | 0 | 1–132 |
| Early pregnancy LOC episode frequency (range) | 0–158 | 0 | 1–158 | 1–74 |
| LOC episode frequency (pre- and early pregnancy) | 5.77 (22.39) | 0.00 (0.00) | 11.45 (30.27) | 34.79 (51.33) |
| OBE frequency (pre- and early pregnancy) | 2.22 (12.84) | 0.00 (0.00) | 1.45 (2.95) | 16.89 (34.46) |
| SBE frequency (pre- and early pregnancy) | 3.54 (15.96) | 0.00 (0.00) | 10.00 (28.17) | 17.89 (32.05) |
Abbreviation: BMI (body mass index); GED (General Educational Development certificate); LOC (loss of control over eating); OBE (objective bulimic episode); SBE (subjective bulimic episode).
Procedure
Women were recruited from obstetric clinics for a longitudinal perinatal eating behavior study. Women were eligible if they were ≥14 years old, had a pre-pregnancy BMI≥25 kg/m2, and a singleton pregnancy. Exclusion criteria were use of weight-affecting medications, participation in weight-management programming, or psychiatric disorders requiring immediate treatment.
Women completed interviews, questionnaires, and weight and height measurements using a digital scale and calibrated stadiometer. Participants provided written informed consent and were compensated. The study site’s Institutional Review Board approved this research.
Measures
Demographic and weight information
Women self-reported demographic and pregnancy-related information, and pre-pregnancy weight, which has been shown to be valid among pregnant women (12). Weight gain during early pregnancy (current minus pre-pregnancy weight), pre-pregnancy BMI (kg/m2), and current BMI (kg/m2) were calculated.
LOC
We administered the Eating Disorder Examination-Pregnancy Version (EDE-PV), a structured interview that assesses eating disorder psychopathology and has been found to be reliable among pregnant women (13, 14). We obtained LOC data from the Overeating Section (objective bulimic episodes [OBEs] and subjective bulimic episodes [SBEs]) in the past three months during pregnancy and the three months prior to conception (i.e., pre-pregnancy), yielding two measurement periods, similar to previous research (13). We analyzed LOC presence (≥1 episode) or absence (5) during either period to understand the influence of when LOC occurred, along with LOC episode frequency across pre-pregnancy and early pregnancy. Interrater reliability for LOC episodes was high (intraclass correlation coefficient = .89).
Distress
Women reported depressive symptoms on the Center for Epidemiological Studies-Depression Scale (CES-D) (15) and stress on the Perceived Stress Scale (PSS) (16), which have demonstrated adequate reliability and validity in pregnant women (17, 18).
Data Analytic Plan
We analyzed LOC rates pre-pregnancy versus during early pregnancy using Pearson χ2 analyses. There were four groups: no LOC (n = 144; 72.0%), LOC incidence (absent pre-pregnancy but present during pregnancy; n = 29; 14.5%), LOC remission (present pre-pregnancy but absent during pregnancy; n = 8; 4.0%), and LOC persistence (present pre-pregnancy and during pregnancy, n = 19; 9.5%). A small percentage of women reported LOC remission, which was not large enough for sub-group analysis (exclusion of this group did not alter the pattern of findings; data not shown). Thus, we conducted two sets of analyses: LOC presence versus absence (n = 200; collapsing across women who endorsed LOC in either period), and LOC as a function of the perinatal phase (n = 192; LOC incidence, LOC persistence, no LOC). Pearson χ2 and t-test analyses were used to evaluate demographic and weight-related variables in association with LOC presence/absence. Pearson χ2 analyses and ANOVA were used to evaluate associations with LOC persistence, incidence, or no LOC. We applied a Bonferroni correction and included pairwise comparisons for depressive symptoms and stress. We conducted correlational analyses to assess LOC episode frequency (across pre-pregnancy and early pregnancy) in relation to depressive symptoms and stress. Statistical significance was determined by an alpha of .05. Standardized mean differences (d) are provided. Analyses were performed in IBM SPSS Statistics for Windows, Version 23.0 [IBM Corp., Armonk, NY].
Results
LOC presence versus absence
More than one-quarter of the women (n = 56; 28.0%) reported LOC before or during pregnancy. No demographic or weight-related variables were significantly associated with LOC presence (ps > .07).
On average, women reported a CES-D score of 12.02 (±9.68) and a PSS score of 20.60 (±8.78). Depressive symptoms and stress were associated (r = .71, p < .001). Women with LOC reported more depressive symptoms (t(198) = −3.14, p < .002, d = 0.48) and stress (t(198) = −3.11, p < .003, d = 0.49) than those without LOC.
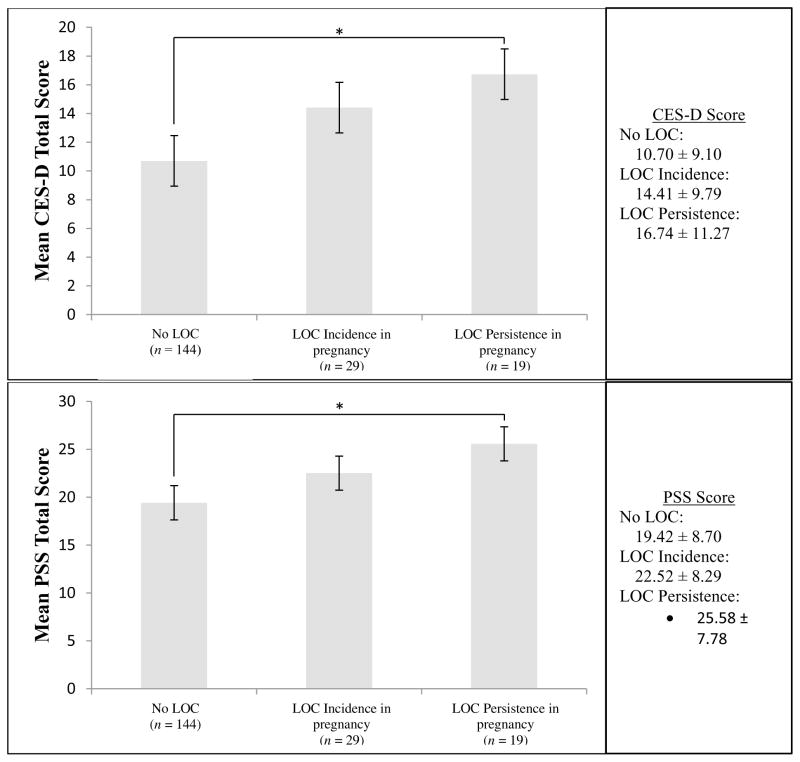
LOC pre-pregnancy to early pregnancy
More women reported LOC during early pregnancy than pre-pregnancy (χ2 = 36.80, p < .001). In sub-analyses (no LOC, incidence, persistence), no demographic or weight-related variables were associated (ps > .17). However, differences emerged in depressive symptoms (F(2, 189) = 4.69, p < .02, d = 0.64) and stress (F(2, 189) = 5.31, p < .006, d = 0.68): women with LOC persistence evidenced the most symptoms, followed by women with incidence, and those without LOC (Figure 1). In pairwise comparisons, depressive symptoms (p < .03) and stress (p < .02) differed between women with LOC persistence and those without LOC. Symptoms among women with LOC incidence did not differ from the other two groups (ps > .17). Higher LOC episode frequency was associated with higher depressive symptoms (r = .31, p < .001) and stress (r = .22, p < .002).
Figure 1.
Differences in depressive symptoms and perceived stress by LOC presentation in early pregnancy (n = 192).
Abbreviations: LOC (loss of control over eating), CES-D (Center for Epidemiological Studies-Depression Scale), PSS (Perceived Stress Scale). *p < .05. The CES-D ranges from 0–60 and the PSS from 0–56, with higher scores indicating greater symptom severity.
Discussion
This study provides the first data on LOC rates among community women with overweight/obesity before and during early pregnancy using a structured interview. We documented that LOC was evident in more than one-quarter of the women before and during pregnancy (28% overall), and distress was most apparent among women in whom LOC was present before and during pregnancy (LOC persistence). Moreover, we found incident LOC during early pregnancy in this population at risk for excessive weight gain.
The current findings provide initial evidence that LOC rates in pregnant community women with overweight/obesity are similar to rates reported in previous studies of pregnancy and by non-pregnant women. Furthermore, these data indicate the emergence of LOC during pregnancy and underscore the importance of further study of LOC during the transition from pre- to early pregnancy in women with overweight/obesity.
Demographic variables were unrelated to prenatal LOC in the present study. Some, but not all, previous studies have suggested that LOC and OBEs are more common among racial/ethnic minorities (19). Against hypotheses, LOC was not associated with weight-related variables, possibly because all women had BMIs in the overweight/obese range, limiting our ability to detect associations. Future research is warranted with broader BMI ranges.
Across the sample, women’s CES-D scores were below the clinical cutoff (≥16), and PSS scores were comparable to adult norms (16). However, women with LOC persistence reported clinically-significant depressive symptoms and elevated stress, consistent with LOC data in non-pregnant individuals with obesity (5–7). Distress levels among women with prenatal LOC incidence were not significantly higher than women without LOC and did not differ from women with LOC persistence. The severity of distress associated with LOC incidence may increase with ongoing LOC throughout pregnancy, and longer time intervals are needed to evaluate the impact of LOC incidence on distress.
Study strengths include assessment of a large, diverse sample of pregnant women and detailed LOC evaluation using the EDE-PV interview. Limitations include cross-sectional design and retrospective recall, although this is common for eating measures (13). Moreover, assessments addressed early pregnancy (not pregnancy in its entirety), and the three-months immediately pre-pregnancy (not lifetime history). In the sub-analyses, we did not include the eight women with LOC remission; data from larger samples will help clarify associations between LOC remission and distress across pregnancy.
Longitudinal research is needed to assess LOC throughout pregnancy and in relation to GWG, health behaviors, perinatal outcomes, and distress. If LOC predicts excessive GWG or poorer outcomes, developing and evaluating interventions that target perinatal LOC (20) may improve women’s health and psychosocial functioning.
Acknowledgments
This work was supported by NICHD (R01 HD068802) and NIMH (T32 MH018269).
Footnotes
Author Disclosure Statement: No competing financial interests reported for RPK, RLE, or MDL. MDM is on the Scientific Advisory Board of Weight Watchers International, Inc.
References
- 1.Vesco KK, Dietz PM, Rizzo J, Stevens VJ, Perrin NA, Bachman DJ, et al. Excessive gestational weight gain and postpartum weight retention among obese women. Obstet Gynecol. 2009;114(5):1069–75. doi: 10.1097/AOG.0b013e3181baeacf. [DOI] [PubMed] [Google Scholar]
- 2.Striegel-Moore RH, Rosselli F, Perrin N, DeBar L, Wilson GT, May A, et al. Gender difference in the prevalence of eating disorder symptoms. Int J Eat Disord. 2009;42(5):471–4. doi: 10.1002/eat.20625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Telch CF, Agras SW, Rossiter EM. Binge eating increases with increasing adiposity. Int J Eat Disord. 1988;7(1):115–9. [Google Scholar]
- 4.Sonneville KR, Horton NJ, Micali N, Crosby RD, Swanson SA, Solmi F, et al. Longitudinal associations between binge eating and overeating and adverse outcomes among adolescents and young adults: does loss of control matter? JAMA Pediatr. 2013;167(2):149–55. doi: 10.1001/2013.jamapediatrics.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Colles SL, Dixon JB, O’Brien PE. Loss of control is central to psychological disturbance associated with binge eating disorder. Obesity (Silver Spring) 2008;16(3):608–14. doi: 10.1038/oby.2007.99. [DOI] [PubMed] [Google Scholar]
- 6.Goldschmidt AB, Engel SG, Wonderlich SA, Crosby RD, Peterson CB, Le Grange D, et al. Momentary affect surrounding loss of control and overeating in obese adults with and without binge eating disorder. Obesity (Silver Spring) 2012;20(6):1206–11. doi: 10.1038/oby.2011.286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Marcus MD, Wing RR, Hopkins J. Obese binge eaters: affect, cognitions, and response to behavioural weight control. J Consult Clin Psychol. 1988;56(3):433–9. doi: 10.1037//0022-006x.56.3.433. [DOI] [PubMed] [Google Scholar]
- 8.Tanofsky-Kraff M, Yanovski SZ. Eating disorder or disordered eating? Non-normative eating patterns in obese individuals. Obes Res. 2004;12(9):1361–6. doi: 10.1038/oby.2004.171. [DOI] [PubMed] [Google Scholar]
- 9.Micali N, Treasure J, Simonoff E. Eating disorders symptoms in pregnancy: A longitudinal study of women with recent and past eating disorders and obesity. J Psychosom Res. 2007;63(3):297–303. doi: 10.1016/j.jpsychores.2007.05.003. [DOI] [PubMed] [Google Scholar]
- 10.Crow SJ, Agras WS, Crosby R, Halmi K, Mitchell JE. Eating disorder symptoms in pregnancy: a prospective study. Int J Eat Disord. 2008;41(3):277–9. doi: 10.1002/eat.20496. [DOI] [PubMed] [Google Scholar]
- 11.Bulik CM, Von Holle A, Hamer R, Knoph Berg C, Torgersen L, Magnus P, et al. Patterns of remission, continuation and incidence of broadly defined eating disorders during early pregnancy in the Norwegian Mother and Child Cohort Study (MoBa) Psychol Med. 2007;37(8):1109–18. doi: 10.1017/S0033291707000724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shin D, Chung H, Weatherspoon L, Song WO. Validity of prepregnancy weight status estimated from self-reported height and weight. Matern Child Health J. 2014;18(7):1667–74. doi: 10.1007/s10995-013-1407-6. [DOI] [PubMed] [Google Scholar]
- 13.Fairburn CG, Stein A, Jones R. Eating habits and eating disorders during pregnancy. Psychosom Med. 1992;54(6):665–72. doi: 10.1097/00006842-199211000-00006. [DOI] [PubMed] [Google Scholar]
- 14.Emery RL, Grace J, Kolko RP, Levine MD. Adapting the Eating Disorder Examination for use during pregnancy: Preliminary results from a community sample of overweight and obese women. doi: 10.1002/eat.22646. Under review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Radloff L. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- 16.Cohen S, Williamson G. Perceived stress in a probability sample of the U.S. In: Oskamp SSS, editor. The social psychology of health: Claremont Symposium on Applied Social Psychology. Newbury Park, CA: Sage; 1988. [Google Scholar]
- 17.Maloni JA, Park S, Anthony MK, Musil CM. Measurement of antepartum depressive symptoms during high-risk pregnancy. Res Nurs Health. 2005;28(1):16–26. doi: 10.1002/nur.20051. [DOI] [PubMed] [Google Scholar]
- 18.Solivan AE, Xiong X, Harville EW, Buekens P. Measurement of Perceived Stress Among Pregnant Women: A Comparison of Two Different Instruments. Matern Child Health J. 2015;19(9):1910–5. doi: 10.1007/s10995-015-1710-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jennings KM, Kelly-Weeder S, Wolfe BE. Binge eating among racial minority groups in the United States: an integrative review. J Am Psychiatr Nurses Assoc. 2015;21(2):117–25. doi: 10.1177/1078390315581923. [DOI] [PubMed] [Google Scholar]
- 20.Wilfley DE, Welch RR, Stein RI, Spurrell EB, Cohen LR, Saelens BE, et al. A randomized comparison of group cognitive-behavioral therapy and group interpersonal psychotherapy for the treatment of overweight individuals with binge-eating disorder. Arch Gen Psychiatry. 2002;59(8):713–21. doi: 10.1001/archpsyc.59.8.713. [DOI] [PubMed] [Google Scholar]