Abstract
Background
In the United States intertrochanteric and pertrochanteric fractures occur at a rate of more than 150,000 cases annually. Current standard of care for these fractures includes fixation with either a cephalomedullary nail (CMN) or a sliding hip screw (SHS). The purpose of this study was to compare failure and medical complications of intertrochanteric femoral fractures repaired by CMN or SHS.
Methods
This study is a retrospective cohort study that included 249 patients with AO/OTA 31 A1.1–3, 31 A2.1–3 nonpathological fractures of the femur, of which 137 received CMN and 112 received SHS. Analysis was stratified by fracture type as stable (AO 31A1.1–2.1) or unstable (AO 31A2.2–3).
Results
The tip-apex distance in stable fractures fixed with CMN was 17.3 ± 5.9 compared to 26.2 ± 7.9 in the stable SHS group (p<0.001) while it was 19.0 ± 5.3 in the unstable CMN group compared to 24.0 ± 6.7 in the unstable SHS patients (P = 0.004). Among patients with stable fracture patterns there was no difference in collapse, complications, failure, or mortality (all P > 0.05). Among patients with unstable fractures CMN had significantly less collapse (P < 0.001) and failure (P = 0.046) but no difference in complications (P = 0.126) or mortality (P = 0.586).
Conclusions
There were no significant differences in failure or complication rates when comparing the CMN to the SHS in stable intertrochanteric fractures. CMN demonstrated significantly reduced failure and collapse rates in unstable intertrochanteric fractures when compared to SHS; however, this study had a relatively small sample size of unstable fractures and all results must be interpreted within this context.
Keywords: Femur, comparison, treatment, stable fracture, unstable fracture
INTRODUCTION
Intertrochanteric and pertrochanteric hip fractures are common injuries in the elderly, with an annual incidence of more than 150,000 reported in the United States.1–3 Both cephalomedullary nails (CMN), and sliding hip screws (SHS) are utilized as the standard of care for fixation of these fractures. Operative management with either fixation device allows for early rehabilitation and decreased morbidity and mortality.4–6 However, which modality is superior is up for debate. While CMN has been shown to have biomechanical advantages over the SHS,7,8 clinical reports of complications and mortality have been conflicting. Some studies have reported that CMN has a higher rate of morbidity,1,3,9 while others report that CMN has a lower rate,9–13 and a number of other studies show no difference between CMN and SHS.14–18 Regardless of fixation type, reoperation and failure rates are variable across studies, ranging from 0 to 32% and mortality rates are as high as 33% depending on fracture stability.14,19–28 Thus, the optimal treatment for intertrochanteric hip fracture is currently uncertain.
Because of the ever-increasing average age of the population and rising number of hip fractures in the elderly, it is essential to optimize treatment and reduce complications from such fractures. The aim of this study was to compare failure and complication rates between CMN and SHS fixation for intertrochanteric femur fractures. This comparison of failure rates and complications is meant to provide an up-to-date analysis of the short- and long-term morbidity and mortality that occurs with these types of fractures at an academic level I trauma center.
MATERIALS AND METHODS
All protocols were reviewed and approved by the institutional review board (IRB) prior to data collection. Hospital and office records were used to identify all patients older than 18 years of age who underwent operation for fractures of the intertrochanteric region between 2000 and 2012. We identified 535 patients with the International Classification of Diseases, 9th Revision (ICD-9) code 820.21 or 829.22 listed as the primary diagnosis. The Current Procedural Terminology (CPT) codes of 27244 and 27245 were then used to separate patients into two groups, those with intramedullary implants, and those with extramedullary implants. Patient diagnosis and fracture patterns were confirmed by chart review and by examining the initial injury radiographs. Fractures were then classified according to the AO/OTA classification system.29 AO 31A1.1–3 and 31A2.1–3 fracture patterns were included, while reverse oblique patterns were excluded (AO 31A3.1–3) to provide comparable groupings, as SHS are not used in these patients. Patients with pathologic fractures, previous hip fractures, subtrochanteric extension, or concurrent, nonintertrochanteric ipsilateral lower extremity fractures were excluded.
Demographic characteristics collected included age, sex, and date of service. Data obtained to determine preoperative state of health included past medical history, past surgical history, body mass index (BMI), and chronic conditions. Control for differences in comorbidities was accomplished by utilizing the Iezzoni chronic condition index.30 Operative notes were searched to identify the type of implant, operative time, and any intraoperative complication. We classified postoperative complications into one of 14 categories: cardiovascular, stroke, urinary tract infection (UTI), pulmonary embolus (PE) or deep vein thrombosis (DVT), non-PE, pulmonary, gastrointestinal, renal, hematoma, infection, heterotopic ossification requiring surgical removal, periprosthetic fracture, pain or irritation necessitating removal of implant, fixation failure, and mortality within 30 days. Cardiovascular complications included any arrhythmia requiring medical intervention, myocardial infarction, or acute exacerbation of congestive hear failure occurring in the immediate post-operative state. Pulmonary complications included pneumonia, severe atelectasis, and respiratory failure. Gastrointestinal complications recorded included GI bleeds and obstruction occurring during hospital admission. The Social Security Death Index (SSDI) was also used to assess mortality in all patients at the time of the study. Fixation failure was defined as cutout, fracture, collapse of more than 2 cm on follow-up radiographs, or revision surgery, not including removal of symptomatic implant.
Immediate postoperative radiographs were used to measure the tip-apex distance (TAD) following the method described by Baumgaertner et al.31 The tip-apex distance was defined as the sum of the distance from the tip of the lag screw to the apex of the femoral head in both the anteroposterior and lateral views. The apex of the femoral head was defined as the point of intersection between the subchondral bone and a line in the center of and parallel to the femoral neck. The immediate postoperative images were then assessed for varus or valgus angulation on anteroposterior radiograph and apex anterior or posterior angulation on the lateral radiograph. We then further classified the reduction as good, acceptable, or poor using the criteria similar to those of Baumgaertner et al.31 For a reduction to be classified as good, there had to be normal or slight valgus alignment (< 3 degrees) on the anteroposterior radiograph, less than 10 degrees of angulation on the lateral radiograph, and no more than 4 mm of displacement of any fragment. To be deemed acceptable, a reduction had to meet one criterion of a good reduction with respect to either alignment or displacement, but not both. A poor reduction met neither criterion.
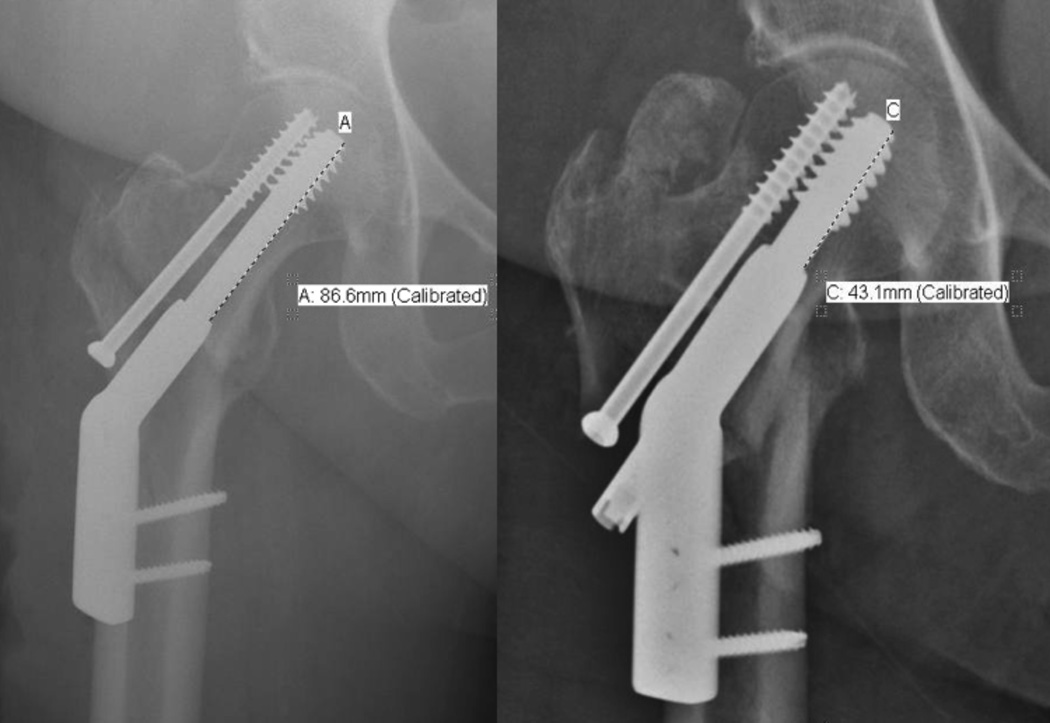
Intraoperative and follow-up radiographs were used to determine if collapse of the fracture region had occurred. Collapse was determined by measuring the shortening of the lag screw on comparable anteroposterior radiographs, with optimal technique and rotation, taken immediately postoperatively and at final follow-up. All images were calibrated, based on the diameter of the lag screw, prior to taking measurements (Figure 1). A collapse distance greater than 2 cm was considered a failure using the definition of mechanical failure proposed by Streubel et al.32
Figure 1.
Measurement of collapse of a sliding hip screw.
Due to the large catchment area of our institution, we attempted to contact every patient by phone to complete a phone questionnaire regarding any care they may have received from an outside provider. Any patient who received postoperative care at another facility or who did not complete a minimum of 12 months follow-up at our institution was asked to complete a telephone questionnaire. The questionnaire included patient information on length and timing of follow-up visits made to physicians outside our system, complications experienced and any further operations performed elsewhere. All patients with a completed questionnaire and outside follow-up of more than 6 months or attendance at our outpatient clinic for at least 6 months were included.
STATISTICAL METHODS
Patients were stratified into stable (AO 31A1.1–2.1) or unstable fracture pattern (AO 31A2.2–2.3) for all analyses. A chi-squared test was used to analyze differences in CMN versus SHS fixation by sex, AO classification, varus/valgus reduction, failure rate, and total complication rate. Fisher’s exact test was used for the analysis of Iezzoni comorbidities30 and reduction quality. A Wilcoxon rank sum test was used to compare TAD, collapse, age of patient population, and date of service. The p-values for failure and total complications were adjusted using multiple logistic regression with sex, age, Iezzoni comorbidities, TAD, and days since surgery as predictors. Mortality was compared between CMN and SHS using a log-rank test, and a Cox proportional hazard model was used to adjust for sex, age, Iezzoni comorbidities, TAD, and days since surgery. Collapse was also compared adjusting for sex, age, Iezzoni comorbidities, TAD, and days since surgery using an analysis of covariance model. Given that CMN became more prevalent over time, all multiple regression models were repeated without days since surgery as a predictor. Kaplan-Meier plots were used to visualize cumulative mortality curves between CMN and SHS fixation types.
RESULTS
Five hundred and thirty five patients treated with intertrochanteric femoral fractures were identified. Patients with a reverse oblique fracture pattern (AO 31A3.1–3, n=197) and those with less than 6 months follow-up (n=89) were excluded. The final analysis included 249 patients; 137 received a CMN and 112 received a SHS. Of the 137 patients that received a CMN, 84 were stable fracture patterns and 52 were unstable fractures. Of the 112 SHS patients, 97 were stable fractures and only 15 were unstable. Any patient that was unable to complete the phone questionnaire and had not completed the required 6-months follow up was excluded from the analysis. In total there were 21 CMN patients and 17 SHS patients who met follow-up inclusion criteria by completing the phone questionnaire; all others had adequate clinical follow-up regardless of their ability to participate in the phone questionnaire.
In the stable fracture group (AO 31A1.1–2.1), the mean CMN patient age was 71 years (range, 26 – 95 years) and 60.7% were women, while the mean age of those undergoing a SHS was 69 years (range, 25–97 hears) and 44.3% were women. The mean follow-up was 21.8 months (range, 0.1–140.8 months) for CMN patients and 26.0 months (range, 0.1–130.0 months) for SHS patients. All living patients were contacted by phone to complete a phone questionnaire. The average time to mortality for the deceased was 41.6 months (range, 0.1–142.8 months) and 54.2 months (range, 0.2–148.5 months) for patients receiving CMN and SHS, respectively (P = 0.016). There was no difference in age or comorbidities between patient groups (both P > 0.05). Women were more likely to receive a CMN and men a SHS (P = 0.028) (Table 1).
Table 1.
Descriptive summary of patients with AO 1.1–2.1 fractures
| AO class 1.1–2.1 | CMN (N=84) | SHS (N=97) | P | Test | |
|---|---|---|---|---|---|
| Age | Mean (SD) | 71.4 (17.9) | 68.6 (17.5) | 0.215 | Wilcoxon |
| Range | (26, 95) | (25, 97) | |||
| Median (IQR) | 77.5 (59, 85.5) | 70 (56, 83) | |||
| Sex | F | 51(60.7%) | 43(44.3%) | 0.028 | Chi-square |
| M | 33(39.3%) | 54(55.7%) | |||
| Year of service | Mean (SD) | 2008 (4) | 2007 (3) | 0.095 | Wilcoxon |
| Range | (2000, 2012) | (2000, 2012) | |||
| Median (IQR) | 2008 (2004, 2011) | 2007.5 (2005, 2009) | |||
| Follow-up (months) | Mean (SD) | 21.8 (31.3) | 26.0 (31.9) | 0.436 | Wilcoxon |
| Range | (0.1, 140.8) | (0.1, 130.0) | |||
| Median (IQR) | 8.5 (3.0, 28.0) | 10.2 (3.1, 42.8) | |||
| Time of service to mortality (months) |
Mean (SD) | 41.6 (38.5) | 54.2 (39.1) | 0.016 | Wilcoxon |
| Range | (0.1, 142.8) | (0.2, 148.5) | |||
| Median (IQR) | 28.7 (13.6, 64.2) | 50.1 (21.6, 83.7) | |||
| Iezzoni comorbidities | 0 | 44(52.4%) | 47(48.5%) | 0.900 | Fisher |
| 1 | 21(25%) | 25(25.8%) | |||
| 2 | 8(9.5%) | 13(13.4%) | |||
| 3 | 7(8.3%) | 9(9.3%) | |||
| 4 | 4(4.8%) | 3(3.1%) | |||
CMN, cephalomedullary nailing; IQR, interquartile range; SD, standard deviation; SHS, sliding hip screw
In the unstable fracture group (AO 31A2.2–2.3), the average CMN patient age was 71 years (range, 27–101 years) and 55.8% were women, while the average of those undergoing a SHS was 75 years (range, 55–91 years) and 53.3% were women. The mean follow-up was 26.4 months (range, 0.1–142.0 months) for CMN patients and 16.3 months (range, 0.4–81.9 months) for SHS patients. The average time to mortality among the deceased was 53.7 months (range, 0.1–155.7 months) and 43.8 months (range, 0.6–134.9 months) for patients receiving CMN and SHS patients, respectively. There was no difference in comorbidities (P = 1.000) (Table 2).
Table 2.
Descriptive summary of patients with unstable fractures (AO 2.2–2.3)
| AO class 2.2–2.3 (N=67) | CMN (N=52) | SHS (N=15) | P | Test | |
|---|---|---|---|---|---|
| Age | Mean (SD) | 71 (18) | 75 (9) | 0.904 | Wilcoxon |
| Range | (27, 101) | (55, 91) | |||
| Median (IQR) | 76 (57, 85) | 75 (73, 80) | |||
| Sex | F | 29 (55.8%) | 8 (53.3%) | 0.870 | Chi-square |
| M | 23 (44.2%) | 7 (46.7%) | |||
| Year of service | Mean (SD) | 2006 (3) | 2005 (3) | 0.139 | Wilcoxon |
| Range | (2000, 2012) | (2001, 2012) | |||
| Median (IQR) | 2007 (2004, 2010) | 2005 (2002, 2007) | |||
| Follow up months | Mean (SD) | 26.4 (37.2) | 16.3 (25.5) | 0.269 | Wilcoxon |
| Range | (0.1, 142.0) | (0.4, 81.9) | |||
| Median (IQR) | 7.7 (3.1, 33.7) | 4.7 (0.9, 21.0) | |||
| Time of service to mortality (months) |
Mean (SD) | 53.7 (43.8) | 43.8 (43.6) | 0.347 | Wilcoxon |
| Range | (0.1, 155.7) | (0.6, 134.9) | |||
| Median (IQR) | 43.6 (19.6, 81.5) | 23.0 (1.7, 75.4) | |||
| Iezzoni comorbidities | 0 | 26(51.0%) | 8(53.3%) | 1.000 | Fisher |
| 1 | 17(33.3%) | 5(33.3%) | |||
| 2 | 5(9.8%) | 2(13.3%) | |||
| 3 | 3(5.9%) | 0(0%) | |||
# Missing: Iezzoni_comorbidities=1; CMN, cephalomedullary nail; IQR, interquartile range; SD, standard deviation; SHS, sliding hip screw
In the stable fracture pattern group, TAD was lower in the CMN group, averaging 17.3 ± 5.9 compared to 26.2 ± 7.9 in the SHS group (P < 0.001). There was no statistical difference in reduction quality (P = 0.302). Six percent of CMN patients had valgus alignment and 2.4% had a varus alignment, while 3.1% of SHS patients had a valgus alignment and 3.1% had a varus alignment, with no significant difference between fixation types (P = 0.671). Unstable fracture patterns showed a significant difference in TAD, with a TAD of 19 ± 5 in the CMN group, and 24 ± 7 in the SHS group (P = 0.004). There was no difference in reduction quality between CMN and SHS (P = 0.317). There was a significant difference in alignment; 1.9% of CMN patient had a valgus alignment and 15.4% had a varus alignment, while 20.0% of SHS patients had a valgus alignment and 13.3% had a varus alignment (P = 0.043) (Table 3).
Table 3.
Descriptive summary of fracture pattern and reduction pattern
| Stable | CMN (N=84) | SHS (N=97) | P | Test | |
| AO class | 1.1 | 20(23.8%) | 23(23.7%) | 0.003 | Fisher |
| 1.2 | 19(22.6%) | 44(45.4%) | |||
| 1.3 | 4(4.8%) | 5(5.2%) | |||
| 2.1 | 41(48.8%) | 25(25.8%) | |||
| Reduction quality |
A | 21(25.0%) | 31(32.0%) | 0.302 | Chi square |
| E | 63(75.0%) | 66(68.0%) | |||
| Varus/Valgus | None | 77(91.7%) | 91(93.8%) | 0.671 | Fisher |
| Val | 5(6.0%) | 3(3.1%) | |||
| Var | 2(2.4%) | 3(3.1%) | |||
| Total TAD | Mean (SD) | 17.3 (5.9) | 26.2 (7.9) | <0.001 | Wilcoxon |
| Range | (7.5, 40.5) | (11.8, 52.0) | |||
| Median (IQR) | 16.8 (13.1, 20.0) | 23.9 (20.9, 30.5) | |||
| Unstable | CMN (N=52) | SHS (N=15) | P | Test | |
| AO class | 2.2 | 30(57.7%) | 13(86.7%) | 0.065 | Fisher |
| 2.3 | 22(42.3%) | 2(13.3%) | |||
| Reduction quality |
A | 29(55.8%) | 11(73.3%) | 0.317 | Fisher |
| E | 21(40.4%) | 3(20.0%) | |||
| P | 2(3.8%) | 1(6.7%) | |||
| Varus/Valgus | Non | 43(82.7%) | 10(66.7%) | 0.043 | Fisher |
| Val | 1(1.9%) | 3(20.0%) | |||
| Var | 8(15.4%) | 2(13.3%) | |||
| Total TAD | Mean (SD) | 19.0 (5.3) | 24.0 (6.7) | 0.004 | Wilcoxon |
| Range | (7.4, 32.6) | (10.9, 35.0) | |||
| Median (IQR) | 19.7 (16.0, 21.5) | 25.8 (20.1, 28.0) | |||
CMN, cephalomedullary nailing; IQR, interquartile range; SD, standard deviation; SHS, sliding hip screw
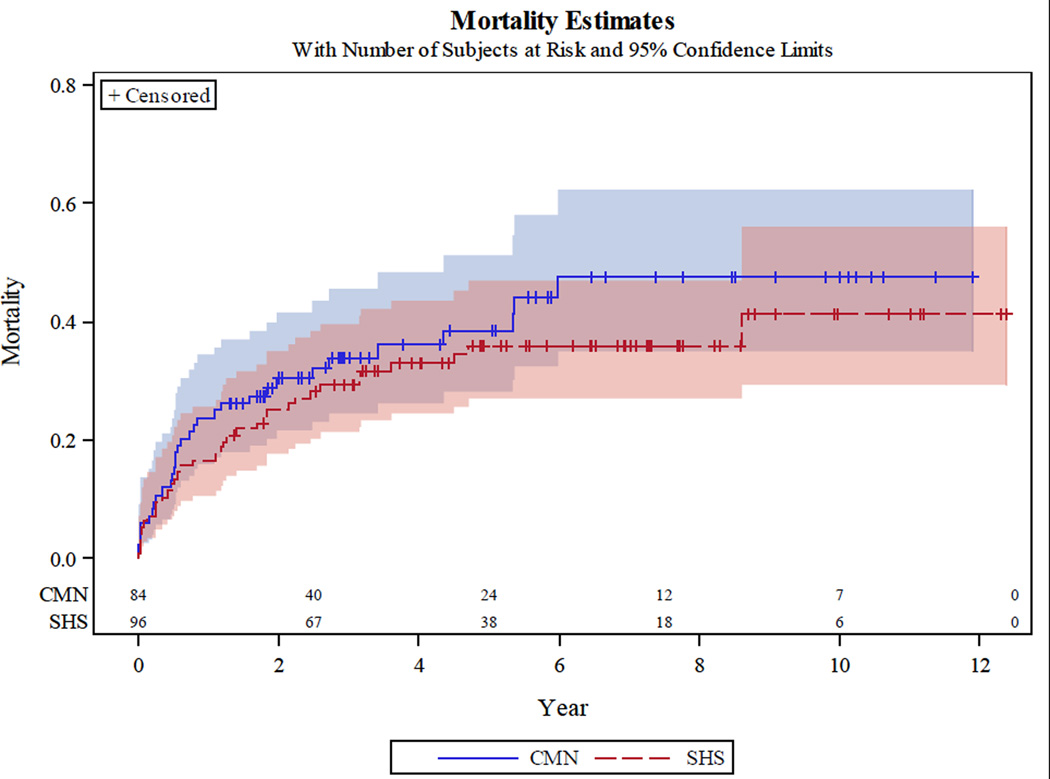
In the stable fracture pattern group, the patients receiving CMN had a mean collapse of 4.7 ± 5.2 mm, SHS patients had a mean collapse of 7.6 ± 9.3 mm, which was not significantly different (P = 0.223). Complications were found in 23.8% in the CMN group and 29.9% in the SHS group (P = 0.881). CMN group patients failed at a rate of 4.8% compared to 14.4% in the SHS group, which was not statistically significant (P = 0.364). Failure in the CMN group was due to three cases of cut-out and one case of collapse. Failure in the SHS group was due to one case of cut-out, 12 cases of collapse and one case of nonunion. Total mortality during the study period was 38.1% in patients receiving a CMN and 36.1% in patients receiving a SHS (P = 0.738) (Table 4). Mortality rate in the CMN group at 30 days, 1 year and 2 years was 6.0% (2.5 – 13.7%), 23.8% (16.1 – 34.4%), 30.4% (21.6 – 41.7%), respectively. Mortality rate in the SHS group at 30 days, 1 year and 2 years was 6.3% (2.9 – 13.4%), 16.7% (10.6 – 25.8%), and 25.1% (17.6 – 35.1%), respectively (Table 5). Mortality rates for the follow-up period (2 years) were graphed for each group, with no statistically significant difference between groups (Figure 2).
Table 4.
Outcomes of stable fractures treated with either CMN or SHS
| Outcome | CMN | SHS | P | Padj | Odds/Hazard ratio (95% CI) (CMN vs. SHS) |
|---|---|---|---|---|---|
| Collapse (mm) | 4.7(5.2)1 | 7.6(9.3)1 | 0.007 | 0.2237 | −1.7(−4.4–1.0) |
| Complication | 20(23.8%) | 29(29.9%) | 0.358 3 |
0.8815 | 1.06(0.47–2.40) |
| Failure | 4(4.8%) | 14(14.4%) | 0.030 3 |
0.2335 | 0.44(0.11–1.70) |
| - Cut-out | 3 | 1 | |||
| -Non-Union | 0 | 1 | |||
| -Collapse | 1 | 12 | |||
| Mortality | 32(38.1%) | 35(36.1%) | 0.376 4 |
0.7386 | 1.11(0.61–2.00) |
adjAdjusting for sex, age, Iezzoni comorbidities, total-tad, days since surgery. Results were consistent with and without days since surgery.
Mean (SD),
Wilcoxon rank sum test
Chi-square test,
Log-rank test comparing survivor functions,
Logistic regression,
Cox proportional hazard model comparing survivor functions,
Analysis of covariance covariates.
CMN, cephalomedullary nailing; SHS, sliding hip screw
Table 5.
Mortality rate with 95% confidence intervals in stable fractures at 30 days, 1 year, and 2 years
| Mortality | CMN | SHS |
|---|---|---|
| 30 day | 0.060 (0.025 – 0.137) | 0.063 (0.029 – 0.134) |
| 1 year | 0.238 (0.161 – 0.344) | 0.167 (0.106 – 0.258) |
| 2 year | 0.304 (0.216 – 0.417) | 0.251 (0.176 – 0.351) |
CMN, cephalomedullary nailing; SHS, sliding hip screw
Figure 2.
Cumulative mortality curve for stable fracture patterns treated with cephalomedullary nailing or sliding hip screw.
Patients with unstable AO 31A 2.2–3 fracture patterns who received a CMN had an average collapse of 5.3 ± 4.6 mm, while those who received a SHS had an average collapse of 16.8 ± 13.8 mm (P < 0.001). Failure was also significantly different between the two groups with CMNs having a failure rate of 7.7%, while SHS patients had a failure rate of 40.0% (P = 0.046). Failure in the unstable CMN group was due to three cases of cut-out and one case of collapse. Failure in the unstable SHS group was due to six cases of collapse. In total there were 14 (26.9%) patients who experienced a complication in the unstable CMN group and eight (53.3%) that experienced a complication in the unstable SHS group, which failed to reach statistical significance (P = 0.126). The total number of deaths was 20 (38.5%) and eight (53.3%) in the CMN and SHS groups, respectively, which was not significantly different (P = 0.586) (Table 6). The 30-day, 1-year, and 2- year mortality rate among unstable CMN patients was 0.058 (0.019 – 0.168), 0.173 (0.094 – 0.306) and 0.273 (0.171 – 0.417), respectively. The 30-day, 1-year, and 2-year mortality rate among unstable SHS patients was 0.067 (0.01 – 0.387), 0.333 (0.154 – 0.625), and 0.467 (0.256 – 0.737), respectively (Table 7). There was no statistically significant difference in mortality rates across the groups (Figure 3).
Table 6.
Outcomes of unstable fractures treated with either CMN or SHS
| Outcome | CMN | SHS | P | Padj | Odds/Hazard ratio (95% CI) (CMN vs. SHS) |
|---|---|---|---|---|---|
| Collapse (mm) | 5.3(4.6)1 | 16.8(13.8)1 | 0.0062 | <0.0017 | −10.7(−16.0~–5.5) |
| Complication | 14(26.9%) | 8(53.3%) | 0.0553 | 0.1265 | 0.34(0.08–1.36) |
| Failure | 4(7.7%) | 6(40.0%) | 0.0023 | 0.0465 | 0.20(0.04–0.97) |
| -Cut-Out | 3 | 0 | |||
| -Non-Union | 0 | 0 | |||
| -Collapse | 1 | 6 | |||
| Mortality | 20(38.5%) | 8(53.3%) | 0.2624 | 0.5866 | 0.78(0.31–1.94) |
adjAdjusting for sex, age, Iezzoni comorbidities, total-tad, days since surgery. Results were consistent with and without days since surgery.
Mean (SD),
Wilcoxon rank sum test,
Chi-square test,
Log-rank test comparing survivor functions,
Logistic regression,
Cox proportional hazard model comparing survivor functions
Analysis of covariance.
CMN, cephalomedullary nailing; SHS, sliding hip screw
Table 7.
Mortality rate with 95% confidence intervals in unstable fractures (AO 2.2–2.3) at 30 days, 1 year, and 2 years
| Mortality | CMN | SHS |
|---|---|---|
| 30 day | 0.058 (0.019 – 0.168) | 0.067 (0.010 – 0.387) |
| 1 year | 0.173 (0.094 – 0.306) | 0.333 (0.154 – 0.625) |
| 2 year | 0.273 (0.171 – 0.417) | 0.467 (0.256 – 0.737) |
CMN, cephalomedullary nailing; SHS, sliding hip screw
Figure 3.
Cumulative mortality curve for unstable fracture patterns treated with cephalomedullary nailing or sliding hip screw.
There were no periprosthetic fractures. Removal of painful implants occurred in six (4.4%) patients with a CMN, five in the stable fracture group and one in the unstable group. Removal of painful implants occurred in five (4.5%) patients with a SHS, all five were in stable fracture patterns. The mean time from surgery to removal for painful implants was 14 months (range, 4–33 months) for the CMN group and 16 months (range, 11–18 months) for SHS. Medical complications were similar in both groups with a slight increase in pulmonary complication in patients receiving CMN. In total, we recorded 102 medical complications with some patients experiencing more than one complication (Table 8).
Table 8.
Descriptive summary of complications in stable and unstable fractures
| Nail 1.1–2.1 | Nail 2.2–2.3 | Plate 1.1–2.1 | Plate 2.2–2.3 | |
|---|---|---|---|---|
| Cardiac | 4 | 3 | 5 | 1 |
| Stroke | 0 | 1 | 1 | 0 |
| UTI | 0 | 0 | 1 | 0 |
| DVT/PE | 2 | 1 | 2 | 0 |
| Pulmonary | 6 | 3 | 1 | 1 |
| GI | 0 | 0 | 1 | 1 |
| Hematoma | 0 | 1 | 0 | 0 |
| Infection | 2 | 2 | 2 | 0 |
| Heterotopic ossification |
0 | 0 | 1 | 0 |
| Renal | 0 | 0 | 0 | 0 |
| Removal for pain/irritation |
5 | 1 | 5 | 0 |
| Periprosthetic fracture | 0 | 0 | 0 | 0 |
| Cut out | 3 | 3 | 1 | 0 |
| Collapse | 1 | 1 | 12 | 6 |
| Nonunion | 0 | 0 | 1 | 0 |
| Mortality <30 days | 5 | 4 | 8 | 4 |
| Total | 28 | 20 | 41 | 13 |
CMN, cephalomedullary nailing; DVT, deep vein thrombosis; GI, gastrointestinal; PE, pulmonary embolism; SHS, sliding hip screw; UTI, urinary tract infection
DISCUSSION
The results of this study present failure rates and surgical and medical complications pertaining to the fixation of intertrochanteric femoral fractures in standard obliquity (AO 31A1.1–2.3), by either cephalomedullary nail (CMN) or sliding hip screw (SHS) over a 12-year period. This study provides a comprehensive overview and comparison of all recorded medical and surgical complications that have occurred in the postoperative period at an academic level I trauma center.
The total complication rate reported in this work is higher than the rate reported by many other authors. Our total complication rate was 28.5% with 102 total complications occurring in 71 patients. The high rate of complications reported may be due to our broad definition of a complication and the long follow-up period. While most complications were experienced in the immediate postoperative period, some events such as removal of painful implants occurred up to 33 months after the date of surgery. Such events would not be captured with a 1-year follow-up period. Although complications, such as fixation failure and cutout, are commonly reported in orthopaedic literature, other complications such as GI bleed occurring during the hospital stay, or new onset postoperative atrial fibrillation are rarely provided. Many of the medical complications found in this study may not be attributable to the implant but are more likely due to the exposure to general anesthesia and the physiological stress of surgery regardless of implant.
This study demonstrated that significantly better positioning of lag screws in the femoral head may be possible with CMN compared to SHS. The measurement of TAD has been previously shown to correlate with screw cutout and fixation failure.31,33 However, strength of the association between TAD and cutout has recently been challenged by newer biomechanical studies and may not be as significant as once thought.34 The TAD may in fact be an indirect measure of the reduction quality as positioning in a center-center or a low center seem to have comparable biomechanical stiffness regardless of TAD.31,33,34 In this study, CMN was found to have a decreased rate of fixation failure; in stable fracture patterns it did not reach statistical significance after adjusting for covariates. It was significant in unstable patterns. However, it should be noted that this group had only 15 SHS patients.
CMN in stable fractures were found to have fewer collapsed constructs, but this finding did not reach statistical significance (P = 0.223). In unstable patterns, collapse was significantly less in CMN patients (P < 0.001). SHS employ the principle of dynamic compression to modify physiologic force into compressive force of the fracture site by sliding of the lag screw in the barrel. This results in compression of the fracture surface, closing of the fracture gap, and a stable load-sharing construct. The collapse in this design occurs until either bone-on-bone contact occurs or the screw slides completely within the barrel, unlike the CMN in which the intramedullary shaft implant prevents further collapse once the calcar has collapsed to make contact. While this quality is desired to promote fracture healing, it can predispose the SHS to a higher rate of collapse without loss of fixation.35,36 Our study showed that even though the rate of failure was not significantly different between CMN and SHS failure of CMN was most often caused by cutout and SHS by collapse. Of the patients who received SHS, 18 had collapse greater than 2 cm, 12 in the stable (12.4%) group and six (40.0%) in the unstable group. For patients who received a CMN, only two patients had collapse greater than 2 cm, one in the stable group and one in the unstable group. Collapse and femoral neck shortening has been shown by Zielinski et al.37 to alter gait patterns, decrease gait velocity, and decrease abductor strength, leading to permanent physical limitations with increasing severity with severe femoral neck shortening defined as greater than 2 cm.37
This study has several limitations, including its retrospective design. Given that hospital records are error prone, we attempted to contact each patient by phone to verify the hospital record data and achieve longer follow-up times. Although this method was fruitful in obtaining information on most of our patients, it was limited by the patients’ ability to recall events and their current cognitive status. Despite these limitations, we successfully contacted most of the patients. Radiographic interpretation of reduction, TAD, and collapse were limited by the quality and alignment of imaging. A difference in alignment between immediate postoperative films and follow-up films could cause over or under interpretation of the degree of collapse and the TAD. Rotation of the films could also confound the interpretation of varus and valgus reduction. Results and conclusions were limited by the small sample, which becomes further limited when divided into fracture pattern, particularly in the unstable SHS group with only 15 patients. Analysis was limited to a quantitative comparison of failure, mortality, or total complication. While this approach is useful for providing a broad comparison of adverse events associated with different fixation devices, it does not display the difference in complication profile and it could be argued that postoperative myocardial infarction is not an equivalent complication to postoperative catheter-associated UTI. Finally, this study was limited in its ability to comment on functional outcomes such as ambulatory status. Although we collected data such as collapse that may reflect poor functional outcomes, direct measures of these outcomes were not available.
The institution in which this study took place is the only academic medical center in the region. As such, we receive patients from five states and because of the large geographic region that we cover, many of our patients choose to receive extended postoperative care at an outside facility that is closer to their residence. This presented a challenge for collecting complete follow-up data for several of our patients. We contacted the patients by phone and conducted a phone survey to assess any unknown adverse outcomes that may have occurred postoperatively and to inquire concerning any recent events. The phone survey provided an interesting insight into the behavior of patients as it was discovered that only two who experienced an adverse outcome received care for that event at an outside facility. One had the implant removed because of pain and the other suffered a pulmonary embolus. Despite the large geographic region and inconvenience of travel, all patients, except for the two previously mentioned patients, returned to the original operating physician for follow-up of any significant complication.
The strengths of this study include the long time period covered and the number of surgeons contributing to the data. Cases included in this study came from 18 orthopaedic surgeons with different fixation preferences. The time period from which data was collected for this paper was an era in which CMN gained acceptance in common orthopaedic practice with CMN use increased from 3% in 1999 to 67% in 2006.22 We covered a period from 2000, when CMN was less utilized to 2012 when it had been widely adopted. The large group and long time period of capture creates a heterogeneous cohort group with a variety of surgical techniques and implants increasing its external validity.
There were no significant differences in failure or complication rates when comparing the CMN to the SHS in stable intertrochanteric hip fractures (AO 31A1.1–2.1). CMN demonstrated significantly reduced failure and collapse rates in unstable intertrochanteric hip fractures (AO 31A2.2–2.3) when compared to SHS; however, this study had a relatively small sample size of unstable fractures and all results must be interpreted within this context.
Acknowledgments
This study was funded by the University of Utah Biostatistics Center with funding in part from the National Center for Research Resources, National Center for Advancing Translational Science and the National Institutes of Health through a grant.
Footnotes
Financial disclosure: Dr. Stuart discloses a financial relationship with CoNexations and Dr. Kubiak disclosed financial relationships with the DJO, DePuy Synthes, CoNexations, and Medical and OrthoGrid.
REFERENCES
- 1.Aros B, Tosteson AN, Gottlieb DJ, Koval KJ. Is a sliding hip screw or im nail the preferred implant for intertrochanteric fracture fixation? Clin Orthop Relat. Res. 2008;466(11):2827–2832. doi: 10.1007/s11999-008-0285-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Burge R, Dawson-Hughes B, Solomon DH, et al. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005–2025. J Bone Miner. Res. 2007;22(3):465–475. doi: 10.1359/jbmr.061113. [DOI] [PubMed] [Google Scholar]
- 3.Crawford CH, Malkani AL, Cordray S, Roberts CS, Sligar W. The trochanteric nail versus the sliding hip screw for intertrochanteric hip fractures: a review of 93 cases. J Trauma. 2006;60(2):325–328. doi: 10.1097/01.ta.0000197872.87439.f9. discussion 328–329. [DOI] [PubMed] [Google Scholar]
- 4.Novack V, Jotkowitz A, Etzion O, Porath A. Does delay in surgery after hip fracture lead to worse outcomes? A multicenter survey. Int J Qual Health Care. 2007;19(3):170–176. doi: 10.1093/intqhc/mzm003. [DOI] [PubMed] [Google Scholar]
- 5.Rogers FB, Shackford SR, Keller MS. Early fixation reduces morbidity and mortality in elderly patients with hip fractures from low-impact falls. J Trauma. 1995;39(2):261–265. doi: 10.1097/00005373-199508000-00012. [DOI] [PubMed] [Google Scholar]
- 6.Zuckerman JD, Skovron ML, Koval KJ, Aharonoff G, Frankel VH. Postoperative complications and mortality associated with operative delay in older patients who have a fracture of the hip. J Bone Joint Surg. Am. 1995;77(10):1551–1556. doi: 10.2106/00004623-199510000-00010. [DOI] [PubMed] [Google Scholar]
- 7.Curtis MJ, Jinnah RH, Wilson V, Cunningham BW. Proximal femoral fractures: a biomechanical study to compare intramedullary and extramedullary fixation. Injury. 1994;25(2):99–104. doi: 10.1016/0020-1383(94)90111-2. [DOI] [PubMed] [Google Scholar]
- 8.Haynes RC, Poll RG, Miles AW, Weston RB. An experimental study of the failure modes of the Gamma Locking Nail and AO Dynamic Hip Screw under static loading: a cadaveric study. Med Eng Phys. 1997;19:446–453. doi: 10.1016/s1350-4533(97)00003-9. England. [DOI] [PubMed] [Google Scholar]
- 9.Parker Martyn J, Handoll Helen HG. Gamma and other cephalocondylic intramedullary nails versus extramedullary implants for extracapsular hip fractures in adults. Cochrane Database of Systematic Reviews. 2010;(9) doi: 10.1002/14651858.CD000093.pub5. http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD000093.pub5/abstract. [DOI] [PubMed] [Google Scholar]
- 10.Little NJ, Verma V, Fernando C, Elliott DS, Khaleel A. A prospective trial comparing the Holland nail with the dynamic hip screw in the treatment of intertrochanteric fractures of the hip. J Bone Joint Surg. Br. 2008;90(8):1073–1078. doi: 10.1302/0301-620X.90B8.20825. [DOI] [PubMed] [Google Scholar]
- 11.Zou J, Xu Y, Yang H. A comparison of proximal femoral nail antirotation and dynamic hip screw devices in trochanteric fractures. J Int. Med Res. 2009;37(4):1057–1064. doi: 10.1177/147323000903700410. [DOI] [PubMed] [Google Scholar]
- 12.Pajarinen J, Lindahl J, Michelsson O, Savolainen V, Hirvensalo E. Pertrochanteric femoral fractures treated with a dynamic hip screw or a proximal femoral nail. A randomised study comparing post-operative rehabilitation. J Bone Joint Surg. Br. 2005;87(1):76–81. [PubMed] [Google Scholar]
- 13.Park SR, Kang JS, Kim HS, Lee WH, Kim YH. Treatment of intertrochanteric fracture with the Gamma AP locking nail or by a compression hip screw--a randomised prospective trial. Int Orthop. 1998;22(3):157–160. doi: 10.1007/s002640050231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bridle SH, Patel AD, Bircher M, Calvert PT. Fixation of intertrochanteric fractures of the femur. A randomised prospective comparison of the gamma nail and the dynamic hip screw. J Bone Joint Surg. Br. 1991;73(2):330–334. doi: 10.1302/0301-620X.73B2.2005167. [DOI] [PubMed] [Google Scholar]
- 15.Saudan M, Lubbeke A, Sadowski C, et al. Pertrochanteric fractures: is there an advantage to an intramedullary nail?: a randomized, prospective study of 206 patients comparing the dynamic hip screw and proximal femoral nail. J Orthop Trauma. 2002;16(6):386–393. doi: 10.1097/00005131-200207000-00004. [DOI] [PubMed] [Google Scholar]
- 16.Barton TM, Gleeson R, Topliss C, Greenwood R, Harries WJ, Chesser TJ. A comparison of the long gamma nail with the sliding hip screw for the treatment of AO/OTA 31-A2 fractures of the proximal part of the femur: a prospective randomized trial. J Bone Joint Surg. Am. 2010;92(4):792–798. doi: 10.2106/JBJS.I.00508. [DOI] [PubMed] [Google Scholar]
- 17.Adams CI, Robinson CM, Court-Brown CM, McQueen MM. Prospective randomized controlled trial of an intramedullary nail versus dynamic screw and plate for intertrochanteric fractures of the femur. J Orthop Trauma. 2001;15(6):394–400. doi: 10.1097/00005131-200108000-00003. [DOI] [PubMed] [Google Scholar]
- 18.Verettas DA, Ifantidis P, Chatzipapas CN, et al. Systematic effects of surgical treatment of hip fractures: gliding screw-plating vs intramedullary nailing. Injury. 2010;41(3):279–284. doi: 10.1016/j.injury.2009.09.012. [DOI] [PubMed] [Google Scholar]
- 19.Roche JJ, Wenn RT, Sahota O, Moran CG. Effect of comorbidities and postoperative complications on mortality after hip fracture in elderly people: prospective observational cohort study. BMJ. 2005;331(7529):1374. doi: 10.1136/bmj.38643.663843.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Keene GS, Parker MJ, Pryor GA. Mortality and morbidity after hip fractures. Bmj. 1993;307(6914):1248–1250. doi: 10.1136/bmj.307.6914.1248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Todd CJ, Freeman CJ, Camilleri-Ferrante C, et al. Differences in mortality after fracture of hip: the east Anglian audit. BMJ. 1995;310(6984):904–908. doi: 10.1136/bmj.310.6984.904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Anglen JO, Weinstein JN. Nail or plate fixation of intertrochanteric hip fractures: changing pattern of practice. A review of the American Board of Orthopaedic Surgery Database. J Bone Joint Surg. Am. 2008;90(4):700–707. doi: 10.2106/JBJS.G.00517. [DOI] [PubMed] [Google Scholar]
- 23.Hou Z, Bowen TR, Irgit KS, et al. Treatment of pertrochanteric fractures (OTA 31-A1 and A2): long versus short cephalomedullary nailing. J Orthop Trauma. 2013;27(6):318–324. doi: 10.1097/BOT.0b013e31826fc11f. [DOI] [PubMed] [Google Scholar]
- 24.Dujardin FH, Benez C, Polle G, et al. Prospective randomized comparison between a dynamic hip screw and a mini-invasive static nail in fractures of the trochanteric area: preliminary results. J Orthop Trauma. 2001;15(6):401–406. doi: 10.1097/00005131-200108000-00004. [DOI] [PubMed] [Google Scholar]
- 25.Bjorgul K, Reikeras O. Outcome after treatment of complications of Gamma nailing: a prospective study of 554 trochanteric fractures. Acta Orthop. 2007;78(2):231–235. doi: 10.1080/17453670710013735. [DOI] [PubMed] [Google Scholar]
- 26.Haidukewych GJ, Israel TA, Berry DJ. Reverse obliquity fractures of the intertrochanteric region of the femur. J Bone Joint Surg. Am. 2001;83-a(5):643–650. doi: 10.2106/00004623-200105000-00001. [DOI] [PubMed] [Google Scholar]
- 27.Min WK, Kim SY, Kim TK, et al. Proximal femoral nail for the treatment of reverse obliquity intertrochanteric fractures compared with Gamma nail. J Trauma. 2007;63(5):1054–1060. doi: 10.1097/01.ta.0000240455.06842.a0. [DOI] [PubMed] [Google Scholar]
- 28.Buecking B, Bliemel C, Struewer J, et al. Use of the Gamma 3 nail in a teaching hospital for trochanteric fractures: mechanical complications, functional outcomes, and quality of life. BMC Res Notes. 2012;5:651. doi: 10.1186/1756-0500-5-651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Marsh JL, Slongo TF, Agel J, et al. Fracture and dislocation classification compendium-- 2007: Orthopaedic Trauma Association classification, database and outcomes committee. J Orthop Trauma. 2007;21(10 Suppl):S1–S133. doi: 10.1097/00005131-200711101-00001. [DOI] [PubMed] [Google Scholar]
- 30.Iezzoni LI, Daley J, Heeren T, et al. Identifying complications of care using administrative data. Med Care. 1994;32(7):700–715. doi: 10.1097/00005650-199407000-00004. [DOI] [PubMed] [Google Scholar]
- 31.Baumgaertner MR, Curtin SL, Lindskog DM, Keggi JM. The value of the tip-apex distance in predicting failure of fixation of peritrochanteric fractures of the hip. J Bone Joint Surg. Am. 1995;77(7):1058–1064. doi: 10.2106/00004623-199507000-00012. [DOI] [PubMed] [Google Scholar]
- 32.Streubel PN, Moustoukas MJ, Obremskey WT. Mechanical failure after locking plate fixation of unstable intertrochanteric femur fractures. J Orthop Trauma. 2013;27(1):22–28. doi: 10.1097/BOT.0b013e318251930d. [DOI] [PubMed] [Google Scholar]
- 33.Baumgaertner MR, Solberg BD. Awareness of tip-apex distance reduces failure of fixation of trochanteric fractures of the hip. J Bone Joint Surg. Br. 1997;79(6):969–971. doi: 10.1302/0301-620x.79b6.7949. [DOI] [PubMed] [Google Scholar]
- 34.Kane P, Vopat B, Heard W, et al. Is tip apex distance as important as we think? A biomechanical study examining optimal lag screw placement. Clin Orthop Relat. Res. 2014;472(8):2492–2498. doi: 10.1007/s11999-014-3594-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Olson SA, Schemitsch G, Morwood M, et al. Hot topics in biomechanics: hip fracture fixation. J Orthop Trauma. 2015;29(Suppl 12):S1–S5. doi: 10.1097/BOT.0000000000000471. [DOI] [PubMed] [Google Scholar]
- 36.Skedros JG, Hunt KJ, Bloebaum RD. Relationships of loading history and structural and material characteristics of bone: development of the mule deer calcaneus. J Morphol. 2004;259(3):281–307. doi: 10.1002/jmor.10167. [DOI] [PubMed] [Google Scholar]
- 37.Zielinski SM, Keijsers NL, Praet SF, et al. Femoral neck shortening after internal fixation of a femoral neck fracture. Orthopedics. 2013;36(7):e849–e858. doi: 10.3928/01477447-20130624-13. [DOI] [PubMed] [Google Scholar]