Abstract
The aim of this review is to show the historical aspects of hands washing for healthy life and explains how can reduce the transmission of community-acquired infectious agents by healthcare workers and patients. This review article is prepared based on available database. The key words used were hands washing, risk assessment, hands hygiene, bacterial flora, contamination, infection, nosocomial, tap water, sanitizer, bacterial resistance, hands bacterial flora, washing methods, antiseptics, healthcare workers, healthcare personnel, from PubMed, ScienceDirect, Embase, Scopus, Web of Sciences, and Google Scholar. Data were descriptively analyzed. The insistence on hand washing has a history of 1400 years. The research results indicate that the bacteria released from the female washed hands in wet and dry condition was lower than from the male's hands with a significance level (3 CFU vs. 8 CFU; confidence interval 95%, P ≤ 0.001). The valuable results of the study indicated that released amount of bacterial flora from wet hands is more than 10 times in compared to dry hands. In addition, established monitoring systems for washing hands before and after patient's manipulation as well as after toilet were dominant indices to prevent the transfer of infectious agents to the patients. Increasing awareness and belief of the healthcare workers have shown an important role by about 30% reduction in the transfection. Hand washing could reduce the episodes of transmission of infectious agents in both community and healthcare settings. However, hand washing is an important key factor to prevent transmission of infectious agents to patients. There is no standard method for measuring compliance. Thus, permanent monitoring of hand washing to reduce the transmission of infections is crucial. Finally, the personnel must believe that hand washing is an inevitable approach to infection control.
Keywords: Bacterial flora, hand washing, healthcare worker, infection control
INTRODUCTION
According to available scientific data, since the mid of 18th century, hand washing is considered essential before any standard medical procedure.[1] In the first decade of the nineteenth-century hands, washing was accepted as a global standard. Currently, hands washing are a crucial measure for controlling infectious diseases.[2]
Hand washing is so important that some religions have also emphasized it. For example, the Prophet of Islam mentioned it as a necessary measure for public health and recommended it in different situations daily of life. Figure 1 summarized the comparative historical aspects of the important theories’ effect on human health.
Figure 1.
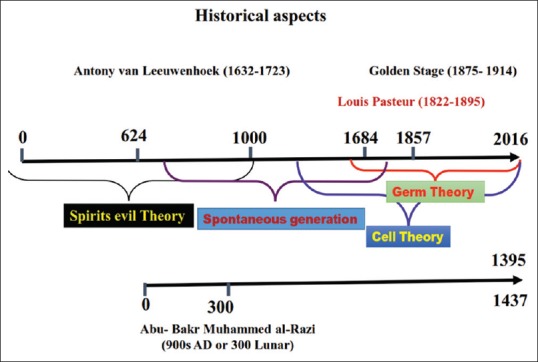
Graphically, comparison presented the synchronization with the Lunar and Gregorian calendar. In the mid-17th century AD, Anthonie Van Leeuwenhoek reported the presence of microorganisms. Then, Louis Pasteur (1822–1895), Joseph Lister (1827–1912), Ignaz Semmelweis (mid-18th century), and Robert Koch (1843–1910) explained the Germ Theory. After that, (in early 19th century) the importances of the hands washing were shown. Furthermore, after the Germ Theory, the pasteurization and sterilization were introduced
As shown in Figure 1, based on experimentally data obtained by the authors, the origin of the solar Lunar Islamic calendar was about in year 622 AD. Nearly, one thousand years (10 centuries) before Antonie Van Leeuwenhoek discovery (September 17 1683) the major health guidelines for human life; in term of the purity and cleanliness, hands, face and mouth washing, teeth brushing, baptism, and ablution are introduced by Islamic Prophet Muhammad (Medicine Prophet Page 21 and Baharolanvar Vol. 59 Page 291).
In addition, the Prophet Mohammad (Islamic Prophet) has said - the Allah has right upon on every Muslim is that once a week to wash his body (Makarem al akhlaq, Page 41). Elsewhere, he said when human beings wake up every morning; they should wash their mouth and nose for the purpose of elimination primary infection of the noses (Jamea al Saghir Vol. 1, Page 69).
Prophet Muhammad laid so much emphasis on the hand washing. As he said when human beings wake up in the morning, they should not touch a container before washing their hands three times (Jamea al Saghir Vol. 1, Page 69).
In addition, Imam Sadiq (as) said that whoever washes the hands before and after eating, he will live in happiness and health (Al Kafi; Vol. 6 Page 290).
Furthermore, there are many Islamic teachings and recommendations regarding handwashing before and after eating and washing the whole body after contact with the human cadaver.
As seen in Figure 1, in period of the documented and written history of the world, the sovereignty of the four major theories: spirits evil theory, spontaneous generation theory, cell theory, and germ theory have presented. In fact, when the world was dominated by spirits evil theory and good and bad events of human lives were attributed to evil spirit, the Prophet of Islam presented a set of guidelines and recommendations for human health, and the words such as teeth brushing, hands washing; purity, baptism, and ablution emerged after that.
However, based on the current knowledge, the importance of the hand washing is reported to have started about 200 years ago. While in the religion of Islam and in Islamic culture, it dates back to more than 1400 years ago. The effect of these two periods of time on the health condition and welfare of human well not understood. Thus, to clarify the health condition in these periods of times further researches are required. Because of, the health condition effects of these two periods may provide a model for prosperity and well-being of the people worldwide.
The reason for a lot of health guidelines within Islamic recommend is not clear to us. We do not know, why in Islamic culture so insisted the ablutions and recommended hands washing. Why the Islam recommends that should not dry the washed hands and we have to let the washed hand dry slowly in the open air? The reason may have been found in the bacterial flora of the skin.
Nowadays (early 21st century), the skin bacterial population is termed the normal bacterial flora, microbiota, and recently, microbiome.
The experimental studies results showed the important role of normal bacterial flora in human health and divided it into two groups: transient and intransient and their benefits have been demonstrated.[3] In addition, based on available data in the ninth century (11 centuries ago), a famous Islamic doctor named Abu-Bakr Mohammad Zakariae al-Razi practically has demonstrated the environment natural bacterial flora in Baghdad.[4] Recently, the role of health provided and importance of protective barrier of intransient bacterial flora has discussed, and the research results showed the impossibility removing them.[5] While the variety, removable and changeable of transient of bacterial flora in medical personnel enhance transmission of pathogenic bacteria in the hospital environment.
However, hands washing as one of the effective measures adopted to prevent infectious agents, it is not clear which method is more effective in preventing the transmission of the pathogenic bacteria. The efficacy of different hands washing methods on surgeons and nurses hands bacterial flora indicated the impact of bacterial transmission.[6]
Several research results indicated that the releasing bacterial flora populations of female unwashed hands were 8 to more than 200 colonies by frequency 3 to 7 types of bacteria. While sitting down with the male's hands from 36 to more than 200 colonies with a frequency of 5 to 13 types with a significance level P ≤ 0.001 have obtained. The released bacteria from the female washed hands in wet condition was 7 to more than 200 colonies with a frequency of 0–7 types and washed their hands in the dry state 7–58 colonies with a frequency of 2–4 types of colonies. While for the males in the same condition as well as in the dry state, it was 1–172 with a frequency of 1–5 type, colonies with a significance level P ≤ 0.001 was obtained.[7,8] However, further research is needed, based on the above results, bacterial population isolated from the hands of males were more than females. Perhaps, more exposure to ambient conditions can cause this phenomenon. It seems that females transfer fewer bacteria between environment and patients. One of the valuable results of that study indicated that the release of amount of bacterial flora from wet hands is more than 10 times with compared to the dry hands. Perhaps, this finding could be interpreted that based on the Islamic rules as to why we should not dry the washed hands in some cases. In fact, when we naturally allow spread of the nonpathogenic bacteria in the environment the competition between them, pathogenic is established, and finally, the pathogenic bacterial number is limited. In this way, a natural mechanism for controlling of pathogenic bacteria in the community may be provided. It may be due to noncompliance with this principal, the prevalence of resistance bacteria in hospital operating rooms.[9]
HANDS WASHING A PREREQUISITE FOR INFECTION CONTROL
The Center for Disease Control and World Health Organization (WHO) have revealed that the maintenance of the hand hygiene by medical staff[10] are prerequisite for nosocomial infection control.[11] In addition, understanding the principal of hand hygiene is essential.[12] Sometimes, the gel dispensers and paper towels at the bedside can assist the patients to prevent nosocomial infection.[13] In any way, under any circumstances, the health workers have to eliminate possible contamination of hands before and after patient's contact.[14] This is possible just with hand washing.[15] The essential point is that the medical personnel believed the effects of hand washing in such time and places.[10] In fact, monitor the level of professional beliefs and principals of hand washing method by health worker as an outcome is inevitable. Results of a study in Nepal teaching hospital showed that about 99% health workers agreed to have washing their hands after contact surfaces contaminated with blood and or other body fluids of patients.[16] However, in many parts of the world, awareness to the importance of and practice to it is far from there.[17] The results of the studies suggest that to succeed in nosocomial infection control; it should be increased the knowledge, beliefs, and behavioral of hand washing importance for nursing students.[18] This providing will be possible just through education and monitoring the level of nurses’ knowledge.[19] The health authority should also remove barriers; provide the necessary of facilities, including new technology.[20] In general, patients in intensive care unit often have been immunocompromised, and thus, they are susceptible to infection. Therefore, health workers[21] should consider hand hygiene. In this regards, the results of a study revealed that unavailability to proper detergents for hand washing is the main barrier for the Intensive Care Unit (ICU) staff listed.[22] In another study, personnel, as well as patients, should access to appropriate detergents and automatic valves as important factors for encouraging individuals wash their hand has been reported.[23] The lack of facilities for personnel hands washing will decrease their interest has shown.[24] Daily reports of infection associated with, could increase quantity and quality of hand washing.[25] In other words, while in a hospital center, hit the number of nosocomial resistant infection has reported routinely for inform the health workers; they have urged to wash their hands. One study has evaluated the knowledge of the nursing students hand washing and was shown in a population of 303 participated which about 25% of them stated enough five times wash hands daily. While 63% of participants believed of nonessential, wash their hands.[26] In this case, the necessity for health personnel's implementation of education programs is inevitable. Investigation on hand washing understanding of importance among nurses showed that 40 min face-to-face education significantly effect on increasing the quality and quantity of hand washing.[27] The implementation of a 6-month educational program of hand washing was associated with reduction of diarrhea rate by 41%.[28] However, the source of the enteric bacterial contamination of hands through oral-fecal route. Therefore, the soap or other detergents in toilets will reduce the hand contamination.[29] However, the public health experts suggest that hand washing will remove pathogenic viruses and bacteria from hands. Some methods are ineffective. For example, several research studies suggested that the use of ethanol solution is not able to remove the skin rhinoviruses completely in comparative to washing hands with soap and water. Thus, the purpose of this review is to show the historical importance of hands washing for healthy life and reduce the transmission of infectious agents by medical employees.
HAND WASHING IN THE OPERATING ROOM: PAST, PRESENT, AND THE FUTURE
The surveillance research revealed that the repeated of surgeon hand washing in operating room can causes dermatitis and skin inflammation;[30,31] in this case, the willingness of hand washing is reduced. Therefore, use of moisture antiseptic has more considered.[32] Recently, new antiseptic has introduced to surgeons washing hands without need to brushing. New antiseptic which composed of 61% ethanol and 1% chlorhexidine gluconate has entered market and the advantages are decreased skin sensitivity, lower water consumption, and cost-effectiveness. The results of a study revealed that hands washing with antiseptic without need brushes in comparison with traditional method in term of satisfaction level, washing time, and convenience, cost-effectiveness, and water consumption were significantly difference (P ≤ 0.004). Moreover, washing time in two groups (9.3 vs. 2 min) showed significant results. The traditional hand washing groups used more water, and therefore, cost has increased association. Nevertheless, the outcome of bacteriological results from washed hands did not reveal significant differences (25% vs. 12.5%; P ≤ 0.152) was observed.[33]
HANDS WASHING IN PUBLIC SERVICE, HOUSEHOLD, KINDERGARTENS, SCHOOLS, AND HOSPITALS
In recent years, the emergence and reemergence of infectious disease epidemic have been of great concern. For example, the global incidence of diarrheal diseases with 8.1 million deaths annually has associated. One of the most effective ways to prevent diarrheal disease in public, kindergartens, school, and hospitals is hand washing with antiseptic and tap water.[34] Immigrants are the main factor for entry and spread of microbial disease in different part of world, especially in cases of emergency. Thus, putting the hand wash system mobile (portable) has shown the significant effects on the prevention and control of infectious disease such as diarrhea.[35] However, the management of infectious disease without using the appropriate methods of hand washing is not possible.[36]
HAND WASHING METHODS
To prevent the transmission of infectious agents to patients, several hand washing methods have been introduced.[37,38,39] The WHO has recommended washing hands over six stages[40] as below.
Drying hands are mandatory when washing taken place in the operating room by each of the mentioned methods. Thus, in the operating room, ICU and Critical Care Unit, hands drying should be done by sterilized gauze or towels. Reused of the towels are usually causes of contamination. However, in all the above methods, drying hands are necessary. Use of hair dryer is time-consuming. While it is an effective means of drying the hands. Therefore, the hot air in place of hands washing in operating room, nursing stations, exam rooms, and toilets is affordable and essential health services. In the following, various methods of hand washing have been used.[41,42]
Wash hands with warm water alone: This method may be remove the blotches and infections while it could not eliminate or reduce of bacteria pathogen population
Wash hands with soap and water: This method will be clearance of the bacteria from skin and may be reduced the bacterial flora population. More repeat of this method may stimulate the skin and allergic reaction taken place. Therefore, nonirritating soap or detergent solution is recommended
Wash hands with water and an antimicrobial detergent: Despite, this method have enough efficacy of and be better by killing and eliminating skin bacterial flora and also viral population, but it is associated with severe skin irritation. In these cases, use of emollients may be helpful
Hands washing with alcohol-based new disinfectants: This method will able to remove or destroy transient's bacterial flora and may be still a part of intransient bacterial flora. While some viruses and spore of bacteria have no effects, this category of new disinfectant can be mentioned antiseptic spray and gels. However, the remaining the carcass of bacteria may causing the further problems. Therefore, rinsing and drying hands after using spray or antiseptic gels are necessary
Hands washing with traditional methods in operating room: This method involves using water and soap or an antimicrobial detergent such as 7.5% povidone-iodine and brushing. This hands washing method will take at least 1–3 min. In addition, being sure to scrub brushes should be used and concern with numerous skin lesions
New method for hand washing and disinfectant in operating room: In this method, by using cleaning solutions with fast action such as deconex which applied by surgery. In this way, there is no need to scrub brushes. However, rinsing and drying hands is needed.
GENERAL CARE REMARK 1
Choosing a long time of any above hand washing methods can cause some problems.[43,44] Therefore, the best way is that the combination hand washing methods have used. Diversification in the hands washing methods will reduce the skin damages and may be effects to the development of resistant organisms against used disinfectants.
GENERAL CARE REMARK 2
It should be more consider that the purpose of hands washing is removed the transient's micro flora. In fact, the action did not have causes destroy the intransient skin microflora completely [Figure 2]. On the other hand, complete elimination of skin bacterial flora is a futile attempt. Because of tried to destroyed bacteria, after a short time (1–3 h), they are going installation.[45]
Figure 2.
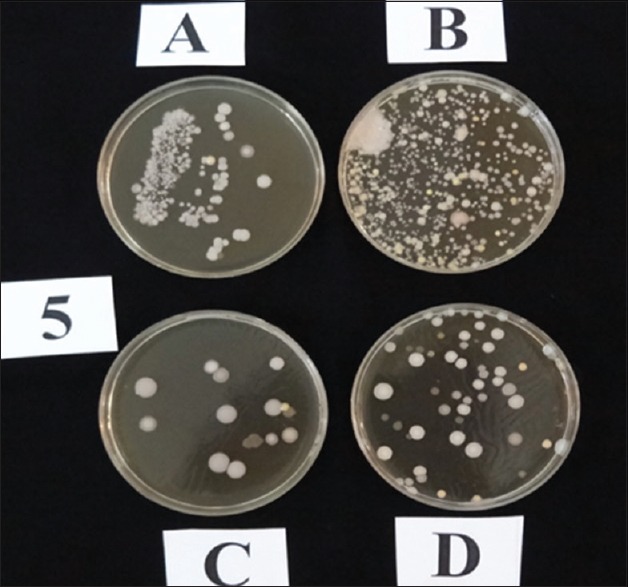
The results of bacteriological assay of subject five fingers sampling in the operating room is shown. Plate A: Culture of fingerprint before hand washing. Plate B: The bacterial culture results of the brain heart infusion broth extract of hand washing before hands scrubs. Plate D: The bacterial culture results of the brain heart infusion broth extract of hand washing after hands scrubs. Plate C: The results of fingerprinting after hand scrub. The differences of the colonies number on plate A, B, D, and C should have considered
GENERAL CARE REMARK 3
Hand washing is requiring enough carefully. It is necessary that during the hands washing, should be concentrated the minded on washing hands. Care must be taken out of all points are uniformly be washed. Carelessness and lack of concentration can cause detergent solution did not come in contact in all areas of the hands [Figure 3]. In this case, may be some area of the hands [Figure 3] remains without removing the contamination.
Figure 3.

How to rubbing the hands with detergent solution have shown. The blue flashes have shown the areas of hands that randomly have not affected with detergent. However, it must be careful that the detergent solution accuracy and uniformly distribute during hand washing. As the infection has left in the area showed and after the hands washing the remained contamination will quickly spread to another hands area
As shown in Figure 4, several areas of hands clearly not affected during washing as often as missed areas should be considered. The research results indicated that hands washing with carelessness and impatience to carry out in these areas would increase the level.
Figure 4.
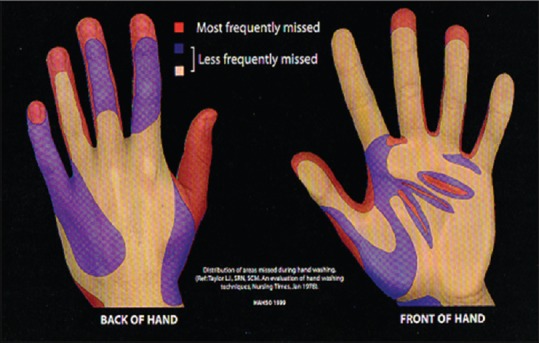
The hands areas of less scrubs and impact of the detergent solution has shown. The red areas are points of the hands that often left out of the affected of eluting (this picture was taken out from Google image search by fraise; hand washing methods and most frequently missed which is available on: http://image.slidesharecdn.com/slidesforhandhygienecoordinator-111120194340-phpapp02/95/hand-hygiene-practices-35-728.jpg?cb = 1321819019)
WHEN HANDS SHOULD BE WASHED
The common question on every physician and nurse's minds is that when they should wash their hands. Is there specific time to wash their hands? In general, daily washing of the hands causing the skin freshness, skin health and is the major tools for infection transmission obstacle. In the following cases, a hand washing is essential and unavoidable:
Viewing dirt on the hands
After contact with contaminated objects
Before and after patient's contact
Before putting on gloves and after removing it
After the toilet, especially after feces out (defecation)
After smoking
After sneezing
After dragging the hands on the scalp
After entering the hands on the mouth and nose
After scratching the skin, especially moist areas of the body.
Washing hands before and after contact with patients and after using the toilet is one of the most important measures to prevent and reduce the spread of infectious agents.[45,46]
GENERAL CARE REMARK 4
Contact with the saliva causing severe contamination of hands, which could transfer it to objects or patients. Oral microflora (microbiome) has containing more than 450 bacterial species some of which are potentially pathogen. The most common bacteria living in the mouth are Staphylococcus aureus, Staphylococcus epidermidis, and Streptococcus pneumoniae. Furthermore, different streptococcal species including Streptococcus pyogenes and viridans Streptococci are included in the study. Other bacteria such as Corynebacterium Spp, Actinomycet Spp, aerobic, and anaerobic Gram-negative bacteria are included of the mouth microflora. Patients with oral cavity or dental inflammation or infection [Figure 5] had increased the number of their mouth bacteria and therefore, hand-mouth contacts can cause to spread of contaminations.[47,48]
Figure 5.

Inflammation and infection of the gum, as well as anterior teeth decay, are seen. Most people with mouth infection, pharyngitis, and tonsillitis are the sources of trans-infections. In addition, low level of oral cavity health condition is the important sources of hands contamination and transfer the infectious agent to others. Traditionally, some people are habiting to use toothpicks, in this way possibility of hands contamination taken place (this picture was taken out from Google image search by “mouth disease and teeth decay which available on: https://www.google.com/search?q and hl = en and tbm = isch and tbs = rimg%3ACdN32FuZwAF2IjiBcZWlXdNoTOpM2wI0CisvF9Co5oESlB2jz8eT1G8ahdWdv)
Hands washing needs three agents including clean water, soap or an antiseptic, and a clean towel for dry the hands.
The results of several studies have shown that usually healthcare staffs do not know really what time and what extent of bacterial are arriving on their hands. Usually, in the cases that hands of employee became contaminant are as follows [Figure 6]:
Figure 6.
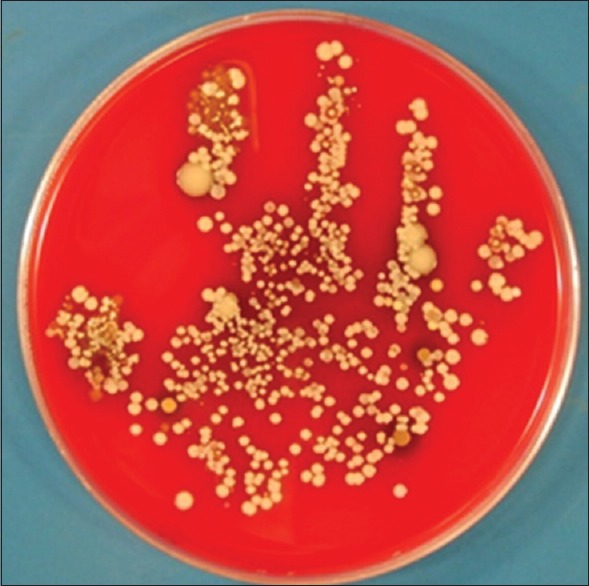
Place the palm of the hand on blood agar medium and incubated for 24 h in 37°C is shown. As can be seen, many bacteria have released on to the surface of bacterial culture media. It should have noted that few of the bacteria cause blood α or β hemolysis may be pathogenmeet
Patients transfer from stretcher to the bed
Taking blood pressure
Taking the pulse of the patients
Relocation of the patients on the bed
Contact with the patient's inanimate objects
Intramuscular injection.
It is estimated that during each of above actions, the healthcare provider (nurses and physicians) may could make an entry 100–1000 CFU of bacteria to their hands.[49,50]
GENERAL CARE REMARK 5
Medical health workers should have sufficient knowledge of the transient microbial flora inside and outside the hospital environments as well as they have to be aware of infectious disease changes periodically. Knowledge of the hands bacterial flora, diversity of the environmental bacterial microbiota can have reduced the prevalence of the infectious bacterial and is essential for selection the appropriate used detergents.
NORMAL BACTERIAL FLORA OF THE HANDS SKIN
The term of bacterial flora or microbiota is referring to the population of bacteria on the body surfaces of the healthy persons have been deployed. Bacterial flora is divided into two groups: the first group, named resident or intransient bacterial population, which formed, from the birth to end of the life. However, depending on the diet, lifestyle, environmental factors, age, and gender could change it. The second group is transient bacterial flora, which may include pathogenic potential bacteria. This group of bacteria may hourly, daily, or weekly changed. The main source of the bacteria is environment. Therefore, each environment has its own specific bacterial population. It is possible that a wide range of the potential pathogenic bacteria is occupying skin of hands. Bacteriological research results indicate that hand's bacterial flora may be including, Acinetobacter, Aerococcus, Bacillus, Clostridium, Corynebacterium, Micrococcus, Staphylococcus and Streptococcus Spp, and Candida and Malassezia Spp. The most of these bacteria are hand transfer from fecal-oral origin. Therefore, healthcare workers should believe to wash their hands to prevent the establishment this organism.[51,52,53,54]
GENERAL CARE REMARK 6
Sometimes, an important question has arising, what is the origin of the community-acquired bacterial infections (CABI)? Many researchers have tried to answer this question. The origin of the CABI may have related to unsanitary waters, lack of proper condition for collection of waste and sewages have been mentioned. The healthy carriers may be the main sources of the CABI. Other researchers have mentioned that domestic or wild type of birds and animals are as CABI sources.[55,56,57,58] Our previous study result has shown that the CABI may be related to jobs and community setting [Figure 7]. In this case, all the money gives to the customer has been contaminated with several microorganisms [Table 1], resultant contaminant the purses, and the pockets of individuals. The durability of the contaminations has been reported up to a week. Therefore, if the customer has been a nurse or physician which does not immediately washing and disinfectant their hands, they will associate with the risk of contamination spread in the hospital environment. In addition, if the customer has going to meet a hospitalized patients or even meet one of the health worker with hands and kissing will causes of the transferring the bacterial contaminations. All the hands touch money of this seller have been contaminated with fecal bacteria.[59] Due to the facing of the organism with different physicochemical agents; then, they may have acquired resistance and the cross-resistance in the face of antibiotic is released. Moreover, these entire organisms can transfer into the nurse's hands or even the patients and different objects. However, the bacteria can entrance into the hospital environment, by in causes of transient bacterial flora of different areas and has been spread and or colonization in different instrument surfaces of the hospitals. One of the most important hospital areas is ICUs which may be settle down by immunocompromised patient's hospitalized for a long time and are exposed to the potential virulence factors.
Figure 7.

After refund, extra money all would be contaminants. Due to the fact, the products are from the farms that have been feed by animal manure. Therefore, varieties of fecal bacteria are as infecting agents. The manner in which these contaminations are transferred to community health centers
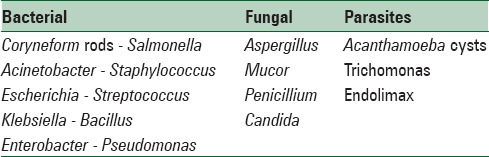
Table 1.
Aerobic and facultative anaerobic organisms isolated from vegetable seller from 100 banknotes are shown. These organisms have identified in the level of genus. The diagnostic of parasites of the banknotes were carried out directly by microscopic study of wash solution of the bill notes separately
GENERAL CARE REMARK 7
Use of the wedding ring on the culture of many countries, including Islamic Republic of Iran is common. The research results have shown[60,61,62] that the medical personnel should careful as follows:
During the hands washing, they should to bring out the ring to decrease contamination survival
The ring may be causes of the latex gloves rupture and increased the spread contamination level
The results research showed that the sub-ring area due to humidity would enhance the replication of the bacteria
The inside of the ring is as a site for bacterial colonization. In the conditions, these bacteria are gradually being acquired resistance to heavy metals.[60,61,62]
DISCUSSION AND CONCLUSIONS
Few exceptions, no part of the human body is free from the bacterial flora; bacterial are everywhere. The transient bacterial flora is constantly on the changes.
It should be considering that the load of transient bacterial flora in the hospital environment is more than the outside area. The entry of pathogenic microflora occurs from outside to the hospital wards, then transferred to the patients by healthcare worker and has increased great concern. The increasing of antibiotic resistance has extremely enhanced healthcare costs and occasionally failure the cure of the patients. Therefore, hand washing as one of the most important health priority throughout the word is very important.
Hence, washing hands before and after contact with patients and after toilet are one of the indicators to prevent or reduce the transfer of infectious agents to the patients. In the UK, annually 5000 deaths report due to health transmitted infectious agents by personnel's hand.[37] The reasons of nosocomial infectious prevalence are results the lack of observance with washing hand techniques by healthcare workers. In addition, absolute confidential use of one form of the alcohol-based antiseptic may lead to increase the incidence of infections related to hands contaminations.
One-study results showed that lack impact of alcohol-based antiseptic rate was decreasing from efficacy 10.4% in 2004 to 3.34% in 2005.[63] The results of this study indicated that use of this antiseptic for 1 year has reduced its antimicrobial activity to two-thirds. Another study results showed that based on coliform count after contact with animals had increased. Comparison of the results of hands washed with soap and water and alcohol-based antiseptic indicated no significant differences.[64] However, because of the importance of hand washing in preventing of the transmission of resistant infectious agents is inevitable. The results of investigation showed, the stress on hand washing with modified methods is necessary.[65] In this regards, the application of new methods for hand washing and preventing the antibiotic-resistant infections in the ICU by personnel is felted more.[66] Therefore, the negligence of hand washing in different hospital wards by personnel, particularly organ transplantation wards are associated with serious consequences.[67] According to the current research results, the healthcare systems have expected that the elite physicians and hard-worker nurses based on data presented in the manuscript have to extract the protocols and practical guideline for hospital wards and exposed to all healthcare workers.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The authors would like to thank the Deputy of Clinical Development Medical Center for their help and cooperation.
REFERENCES
- 1.Stewardson A, Allegranzi B, Sax H, Kilpatrick C, Pittet D. Back to the future: Rising to the Semmelweis challenge in hand hygiene. Future Microbiol. 2011;6:855–76. doi: 10.2217/fmb.11.66. [DOI] [PubMed] [Google Scholar]
- 2.Hand washing: A powerful antidote to illness. J Okla State Med Assoc. 2011;104:326. [PubMed] [Google Scholar]
- 3.Price PB. The bacteriology of normal skin: A new quantitative test applied to a study of the bacterial flora and the disinfectant action of mechanical cleansing. J Infect Dis. 1938;63:301–18. [Google Scholar]
- 4.Edward AI. Fundamental of Microbiology. 3rd ed. California: The Benjamin Cummings Publishing Company; 1991. p. 29. [Google Scholar]
- 5.Montes LF, Wilborn WH. Location of bacterial skin flora. Br J Dermatol. 1969;81(Suppl 1):23. doi: 10.1111/j.1365-2133.1969.tb12829.x. [DOI] [PubMed] [Google Scholar]
- 6.Ataee RA, Mehrabi Tavana A, Khatami SM, Ahmadi Baghmaleki F, Miry LS. The study effects of the hand washing on hands bacterial flora in operating room. J Health Policy Sustain Health. 2014;1:1–5. [Google Scholar]
- 7.Ataee RA, Moslemi M, Mehrabi Tavana A, Araghizadeh H. An assay on different hands washing on nursing hands bacterial flora. The 23rd Iranian Congress on Infectious Disease and Tropical Medicine. Tehran Iran: 2015. Jan 12-16, [Google Scholar]
- 8.Ahmadi B, Ataee AR, Miry L, Khatemi S. Evaluation of the Disinfectant Solution Effects on Hands Bacterial Flora Used in Operating Room. 4th Festival of Student and Research; 5-6 March, 2013. Tehran, Islamic Republic of Iran: Baqiyatallah University of Medical Sciences; 2013. [Google Scholar]
- 9.Ataee RA, Irannejad L, Esmaeili D, Mehrabi Tavana A, Salesi M. Antibiotic Resistance Profiles Determine of Bacteria Isolated from the Operating Room in a Hospital in 2013 Sumer. The 23rd Iranian Congress on Infectious Disease and Tropical Medicine. Tehran Iran: 2015. Jan 12-16, [Google Scholar]
- 10.Squires JE, Linklater S, Grimshaw JM, Graham ID, Sullivan K, Bruce N, et al. Understanding practice: Factors that influence physician hand hygiene compliance. Infect Control Hosp Epidemiol. 2014;35:1511–20. doi: 10.1086/678597. [DOI] [PubMed] [Google Scholar]
- 11.Garus-Pakowska A, Sobala W, Szatko F. Observance of hand washing procedures performed by the medical personnel after the patient contact. Part II. Int J Occup Med Environ Health. 2013;26:257–64. doi: 10.2478/s13382-013-0094-2. [DOI] [PubMed] [Google Scholar]
- 12.Busby SR, Kennedy B, Davis SC, Thompson HA, Jones JW. Assessing patient awareness of proper hand hygiene. Nursing. 2015;45:27–30. doi: 10.1097/01.NURSE.0000463667.76100.06. [DOI] [PubMed] [Google Scholar]
- 13.Di Muzio M, Cammilletti V, Petrelli E, Di Simone E. Hand hygiene in preventing nosocomial infections: A nursing research. Ann Ig. 2015;27:485–91. doi: 10.7416/ai.2015.2035. [DOI] [PubMed] [Google Scholar]
- 14.Cure L, Van Enk R. Effect of hand sanitizer location on hand hygiene compliance. Am J Infect Control. 2015;43:917–21. doi: 10.1016/j.ajic.2015.05.013. [DOI] [PubMed] [Google Scholar]
- 15.Garus-Pakowska A, Sobala W, Szatko F. Observance of hand washing procedures performed by the medical personnel before patient contact. Part I. Int J Occup Med Environ Health. 2013;26:113–21. doi: 10.2478/s13382-013-0092-4. [DOI] [PubMed] [Google Scholar]
- 16.Joshi S, Joshi A, Park BJ, Aryal UR. Hand washing practice among health care workers in a teaching hospital. J Nepal Health Res Counc. 2013;11:1–5. [PubMed] [Google Scholar]
- 17.Rabbi SE, Dey NC. Exploring the gap between hand washing knowledge and practices in Bangladesh: A cross-sectional comparative study. BMC Public Health. 2013;13:89. doi: 10.1186/1471-2458-13-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jeong SY, Kim KM. Influencing factors on hand hygiene behavior of nursing students based on theory of planned behavior: A descriptive survey study. Nurse Educ Today. 2016;36:159–64. doi: 10.1016/j.nedt.2015.09.014. [DOI] [PubMed] [Google Scholar]
- 19.Willmott M, Nicholson A, Busse H, MacArthur GJ, Brookes S, Campbell R. Effectiveness of hand hygiene interventions in reducing illness absence among children in educational settings: A systematic review and meta-analysis. Arch Dis Child. 2016;101:42–50. doi: 10.1136/archdischild-2015-308875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Al Salman JM, Hani S, de Marcellis-Warin N, Isa SF. Effectiveness of an electronic hand hygiene monitoring system on healthcare workers’ compliance to guidelines. J Infect Public Health. 2015;8:117–26. doi: 10.1016/j.jiph.2014.07.019. [DOI] [PubMed] [Google Scholar]
- 21.Birnbach DJ, Rosen LF, Fitzpatrick M, Arheart KL, Munoz-Price LS. An evaluation of hand hygiene in an Intensive Care Unit: Are visitors a potential vector for pathogens? J Infect Public Health. 2015;8:570–4. doi: 10.1016/j.jiph.2015.04.027. [DOI] [PubMed] [Google Scholar]
- 22.Sharma R, Sharma M, Koushal V. P134: Hand washing: A critical measure in prevention and infection control. Antimicrob Resist Infect Control. 2013;2(Suppl 1):134–2. [Google Scholar]
- 23.Devnani M, Kumar R, Sharma RK, Gupta AK. A survey of hand-washing facilities in the outpatient department of a tertiary care teaching hospital in India. J Infect Dev Ctries. 2011;5:114–8. doi: 10.3855/jidc.1003. [DOI] [PubMed] [Google Scholar]
- 24.Savolainen-Kopra C, Haapakoski J, Peltola PA, Ziegler T, Korpela T, Anttila P, et al. Hand washing with soap and water together with behavioural recommendations prevents infections in common work environment: An open cluster-randomized trial. Trials. 2012;13:10. doi: 10.1186/1745-6215-13-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ergin A, Bostanci M, Onal O, Bozkurt AI, Ergin N. Evaluation of students’ social hand washing knowledge, practices, and skills in a university setting. Cent Eur J Public Health. 2011;19:222–6. doi: 10.21101/cejph.a3664. [DOI] [PubMed] [Google Scholar]
- 26.Ergin A, Hascelik G. Antimicrobial Activity of Copper Alloys Against Invasive Multidrug-Resistant Nosocomial Pathogens. Curr Microbiol. 2015;71:291–5. doi: 10.1007/s00284-015-0840-8. [DOI] [PubMed] [Google Scholar]
- 27.Erkan T, Findik UY, Tokuc B. Hand-washing behaviour and nurses’ knowledge after a training programme. Int J Nurs Pract. 2011;17:464–9. doi: 10.1111/j.1440-172X.2011.01957.x. [DOI] [PubMed] [Google Scholar]
- 28.Langford R, Lunn P, Panter-Brick C. Hand-washing, subclinical infections, and growth: A longitudinal evaluation of an intervention in Nepali slums. Am J Hum Biol. 2011;23:621–9. doi: 10.1002/ajhb.21189. [DOI] [PubMed] [Google Scholar]
- 29.Ray SK, Amarchand R, Srikanth J, Majumdar KK. A study on prevalence of bacteria in the hands of children and their perception on hand washing in two schools of Bangalore and Kolkata. Indian J Public Health. 2011;55:293–7. doi: 10.4103/0019-557X.92408. [DOI] [PubMed] [Google Scholar]
- 30.Visscher MO, Randall Wickett R. Hand hygiene compliance and irritant dermatitis: A juxtaposition of healthcare issues. Int J Cosmet Sci. 2012;34:402–15. doi: 10.1111/j.1468-2494.2012.00733.x. [DOI] [PubMed] [Google Scholar]
- 31.Batalla A, García-Doval I, de la Torre C. Products for hand hygiene and antisepsis: Use by health professionals and relationship with hand eczema. Actas Dermosifiliogr. 2012;103:192–7. doi: 10.1016/j.ad.2011.06.005. [DOI] [PubMed] [Google Scholar]
- 32.Williams C, Wilkinson SM, McShane P, Lewis J, Pennington D, Pierce S, et al. A double-blind, randomized study to assess the effectiveness of different moisturizers in preventing dermatitis induced by hand washing to simulate healthcare use. Br J Dermatol. 2010;162:1088–92. doi: 10.1111/j.1365-2133.2010.09643.x. [DOI] [PubMed] [Google Scholar]
- 33.Vergara-Fernández O, Morales-Olivera JM, Ponce-de-León-Rosales S, Vega-Batista R, Mejía-Ovalle R, Huertas-Jiménez M, et al. Surgical team satisfaction levels between two preoperative hand-washing methods. Rev Invest Clin. 2010;62:532–7. [PubMed] [Google Scholar]
- 34.Ejemot-Nwadiaro R, Ehiri JE, Arikpo D, Meremikwu MM, Critchley JA. Hand washing promotion for preventing diarrhoea. The Cochrane database of systematic reviews. Cochrane Database Syst Rev. 2015;9:CD004265. doi: 10.1002/14651858.CD004265.pub3. doi: 10.1002/14651858.CD004265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Husain F, Hardy C, Zekele L, Clatworthy D, Blanton C, Handzel T. A pilot study of a portable hand washing station for recently displaced refugees during an acute emergency in Benishangul-Gumuz Regional State, Ethiopia. Confl Health. 2015;9:26. doi: 10.1186/s13031-015-0053-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Smith SM. A review of hand-washing techniques in primary care and community settings. J Clin Nurs. 2009;18:786–90. doi: 10.1111/j.1365-2702.2008.02546.x. [DOI] [PubMed] [Google Scholar]
- 37.Nabavi M, Alavi-Moghaddam M, Gachkar L, Moeinian M. Knowledge, attitudes, and practices study on hand hygiene among Imam Hossein Hospital's residents in 2013. Iran Red Crescent Med J. 2015;17:e19606. doi: 10.5812/ircmj.19606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Boyce JM, Kelliher S, Vallande N. Skin irritation and dryness associated with two hand-hygiene regimens: Soap-and-water hand washing versus hand antisepsis with an alcoholic hand gel. Infect Control Hosp Epidemiol. 2000;21:442–8. doi: 10.1086/501785. [DOI] [PubMed] [Google Scholar]
- 39.Best EL, Redway K. Comparison of different hand-drying methods: The potential for airborne microbe dispersal and contamination. J Hosp Infect. 2015;89:215–7. doi: 10.1016/j.jhin.2014.11.007. [DOI] [PubMed] [Google Scholar]
- 40.Arias AV, Garcell HG, Ochoa YR, Arias KF, Miranda FR. Assessment of hand hygiene techniques using the World Health Organization's six steps. J Infect Public Health. 2016;9:366–9. doi: 10.1016/j.jiph.2015.11.006. [DOI] [PubMed] [Google Scholar]
- 41.Gustafson DR, Vetter EA, Larson DR, Ilstrup DM, Maker MD, Thompson RL, et al. Effects of 4 hand-drying methods for removing bacteria from washed hands: A randomized trial. Mayo Clin Proc. 2000;75:705–8. doi: 10.4065/75.7.705. [DOI] [PubMed] [Google Scholar]
- 42.Ansari SA, Springthorpe VS, Sattar SA, Tostowaryk W, Wells GA. Comparison of cloth, paper, and warm air drying in eliminating viruses and bacteria from washed hands. Am J Infect Control. 1991;19:243–9. doi: 10.1016/s0196-6553(05)80256-1. [DOI] [PubMed] [Google Scholar]
- 43.Larson E, McGinley KJ, Grove GL, Leyden JJ, Talbot GH. Physiologic, microbiologic, and seasonal effects of handwashing on the skin of health care personnel. Am J Infect Control. 1986;14:51–9. doi: 10.1016/0196-6553(86)90055-6. [DOI] [PubMed] [Google Scholar]
- 44.Larson E, Leyden JJ, McGinley KJ, Grove GL, Talbot GH. Physiologic and microbiologic changes in skin related to frequent handwashing. Infect Control. 1986;7:59–63. doi: 10.1017/s019594170006389x. [DOI] [PubMed] [Google Scholar]
- 45.Rotter ML, Kampf G, Suchomel M, Kundi M. Population kinetics of the skin flora on gloved hands following surgical hand disinfection with 3 propanol-based hand rubs: A prospective, randomized, double-blind trial. Infect Control Hosp Epidemiol. 2007;28:346–50. doi: 10.1086/510865. [DOI] [PubMed] [Google Scholar]
- 46.Rotter ML, Kampf G, Suchomel M, Kundi M. Long-term effect of a 1.5 minute surgical hand rub with a propanol-based product on the resident hand flora. J Hosp Infect. 2007;66:84–5. doi: 10.1016/j.jhin.2007.02.012. [DOI] [PubMed] [Google Scholar]
- 47.Poole K. Bacterial resistance: Acquired resistance. In: Fraise AP, Lambert PA, Maillard JY, editors. Russell, Hugo & Ayliffe's Principles and Practice of Disinfection, Preservation, and Sterilization. 4th ed. Oxford: Blackwell Publishing Ltd; 2004. pp. 170–83. [Google Scholar]
- 48.Smith K, Gemmell CG, Hunter IS. The association between biocide tolerance and the presence or absence of qac genes among hospital-acquired and community-acquired MRSA isolates. J Antimicrob Chemother. 2008;61:78–84. doi: 10.1093/jac/dkm395. [DOI] [PubMed] [Google Scholar]
- 49.Messager S, Hann AC, Goddard PA, Dettmar PW, Maillard JY. Use of the ‘ex vivo’ test to study long-term bacterial survival on human skin and their sensitivity to antisepsis. J Appl Microbiol. 2004;97:1149–60. doi: 10.1111/j.1365-2672.2004.02403.x. [DOI] [PubMed] [Google Scholar]
- 50.Archibald LK, Manning ML, Bell LM, Banerjee S, Jarvis WR. Patient density, nurse-to-patient ratio and nosocomial infection risk in a pediatric cardiac Intensive Care Unit. Pediatr Infect Dis J. 1997;16:1045–8. doi: 10.1097/00006454-199711000-00008. [DOI] [PubMed] [Google Scholar]
- 51.Adams BG, Marrie TJ. Hand carriage of aerobic gram-negative rods may not be transient. J Hyg (Lond) 1982;89:33–46. doi: 10.1017/s0022172400070510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Patrick DR, Findon G, Miller TE. Residual moisture determines the level of touch-contact-associated bacterial transfer following hand washing. Epidemiol Infect. 1997;119:319–25. doi: 10.1017/s0950268897008261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Marples RR, Towers AG. A laboratory model for the investigation of contact transfer of micro-organisms. J Hyg (Lond) 1979;82:237–48. doi: 10.1017/s0022172400025651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Pittet D, Dharan S, Touveneau S, Sauvan V, Perneger TV. Bacterial contamination of the hands of hospital staff during routine patient care. Arch Intern Med. 1999;159:821–6. doi: 10.1001/archinte.159.8.821. [DOI] [PubMed] [Google Scholar]
- 55.Anaissie EJ, Penzak SR, Dignani MC. The hospital water supply as a source of nosocomial infections: A plea for action. Arch Intern Med. 2002;162:1483–92. doi: 10.1001/archinte.162.13.1483. [DOI] [PubMed] [Google Scholar]
- 56.LeChevallier M. The case for maintaining a disinfectant residual. J Am Water Works Assoc. 1999;91:86–94. [Google Scholar]
- 57.Chang HJ, Miller HL, Watkins N, Arduino MJ, Ashford DA, Midgley G, et al. An epidemic of Malassezia pachydermatis in an intensive care nursery associated with colonization of health care workers’ pet dogs. N Engl J Med. 1998;338:706–11. doi: 10.1056/NEJM199803123381102. [DOI] [PubMed] [Google Scholar]
- 58.Kohan C, Ligi C, Dumigan DG, Boyce JM. The importance of evaluating product dispensers when selecting alcohol-based handrubs. Am J Infect Control. 2002;30:373–5. doi: 10.1067/mic.2002.125586. [DOI] [PubMed] [Google Scholar]
- 59.Moslemi M, Ataee RA, Mahmodi R, Daneshmandi M. Effect of disinfectant solutions on the bacterial flora of nurse hands and its effects on infection transmission. S3 Proceedings of the 5th Annual Research Congress of the Baqiyatallah University of Medical Sciences – March 2014. Tehran Islamic Republic of Iran: 2014. [Google Scholar]
- 60.Hoffman PN, Cooke EM, McCarville MR, Emmerson AM. Micro-organisms isolated from skin under wedding rings worn by hospital staff. Br Med J (Clin Res Ed) 1985;290:206–7. doi: 10.1136/bmj.290.6463.206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Jacobson G, Thiele JE, McCune JH, Farrell LD. Handwashing: Ring-wearing and number of microorganisms. Nurs Res. 1985;34:186–8. [PubMed] [Google Scholar]
- 62.Wongworawat MD, Jones SG. Influence of rings on the efficacy of hand sanitization and residual bacterial contamination. Infect Control Hosp Epidemiol. 2007;28:351–3. doi: 10.1086/510790. [DOI] [PubMed] [Google Scholar]
- 63.Ogawa M, Takada S, Takahashi M, Yasuda E, Watase M, Taniguchi H. Survival of Gram-positive spore-forming bacteria including Bacillus cereus after hand washing using alcohol-based handrub. J UOEH. 2006;28:401–10. doi: 10.7888/juoeh.28.401. [DOI] [PubMed] [Google Scholar]
- 64.Davis MA, Sheng H, Newman J, Hancock DD, Hovde CJ. Comparison of a waterless hand-hygiene preparation and soap-and-water hand washing to reduce coliforms on hands in animal exhibit settings. Epidemiol Infect. 2006;134:1024–8. doi: 10.1017/S095026880600598X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Collins F, Hampton S. Hand-washing and methicillin-resistant Staphylococcus aureus. Br J Nurs. 2005;14:703–7. doi: 10.12968/bjon.2005.14.13.18451. [DOI] [PubMed] [Google Scholar]
- 66.Diomidous M, Ponirou P, Mpizopoulou Z, Tzalera V, Mechili A. Infection control and quality assurance of health services provided in ICU: Development of an ICU website. Stud Health Technol Inform. 2013;190:249–51. [PubMed] [Google Scholar]
- 67.Graf K, Ott E, Wolny M, Tramp N, Vonberg RP, Haverich A, et al. Hand hygiene compliance in transplant and other special patient groups: An observational study. Am J Infect Control. 2013;41:503–8. doi: 10.1016/j.ajic.2012.09.009. [DOI] [PubMed] [Google Scholar]


