Abstract
Introduction:
Ventilator-associated pneumonia (VAP) is the most common infection in the intensive care unit, and has many side effects such as increased mortality, increased length of hospital stay, and increased health costs. This study aimed to evaluate the compliance with the standards for prevention of VAP by nurses in the intensive care units.
Materials and Methods:
In this descriptive cross-sectional study, 120 nurses in 11 intensive care units of hospitals affiliated to Isfahan university of Medical Sciences, Iran, were assessed for 4 months from July to October 2014. The implementation of all measures for the prevention of VAP was investigated through observation and using a checklist.
Results:
The mean compliance with the standards for the prevention of VAP in the intensive care unit by the nurses was 56.32%; analysis of variance test showed significant difference between the hospitals (P < 0.001). Disposable ventilator circuit was performed for all patients; however, reviewing the patient readiness for separation from the ventilator was not conducted on a daily basis.
Conclusions:
Compliance with the standards for the prevention of VAP in the intensive care units was relatively acceptable; however, it still requires serious attention by the officials with training and sensitization of nurses in implementing preventive measures, especially through the provision of clinical guidelines and related protocols.
Keywords: Intensive care unit, Iran, ventilator-associated pneumonia
Introduction
Nosocomial infections are an important issue in healthcare centers and are a common cause of increase in length of hospitalization, hospital costs, and patient mortality rate.[1] The prevalence of nosocomial infections in intensive care units (ICUs) is 5 to 10 times higher than that in public units.[2] The most common types of hospital infections are urinary tract infections and pneumonia.[3] Ventilator-associated pneumonia (VAP) is one of the deadliest infections, and is the cause of more than 36000 deaths each year in the United States.[4] There is no specific VAP statistics in Iran, however, Afkhamzadeh reported this number as 32.2% in Sanandaj, Iran, and Ebrahimi reported it as 80%.[5,6] The results of the study by Safdari in Isfahan, Iran, showed a high rate of pneumonia in both the intervention and control groups.[7] The incidence of pneumonia in the control group was 47.4%, and in the intervention group, despite the use of closed suction and intermittent subglottic secretion drainage, it was 26.3%.[7]
VAP has consequences such as increased duration of hospitalization and length of stay in the ICU, increased cost of more than $ 40000 per patient, increased duration of mechanical ventilation, and therefore, further increase in morbidity and mortality rates.[3,8,9,10,11] ICU patients are usually in critical condition, and several risk factors predispose them to a range of infections. The primary risk factor for pneumonia is receiving mechanical ventilation.[12] Its other risk factors include the duration of mechanical ventilation, receiving parenteral nutrition, invasive devices, re-intubation, mental status changes, mouth colonization, contact with other patients and hospital caregivers, significant sedation, and malnutrition.[9,12,13]
VAP is preventable.[14] Reduction of VAP prevalence implies significant reduction in treatment costs and impact on mortality in the ICU.[15] Prevention of VAP is a team effort, and it is vital to encourage the care team to maintain patient safety.[12] Many studies have shown that simple and cost-effective measures can significantly reduce the incidence of VAP in developed countries.[16] Nurses make up the vast majority of health care providers.[9]
Based on the abovementioned facts, conducting research on compliance with VAP prevention measures in ICU patients can be beneficial in identifying shortcomings and resolving them, improving the level of care, and reducing medical and treatment costs. Research studies indicate that, despite the recognition of the need to implement preventive interventions, information about the status of care measures and their implementation in ICUs in Iran and Isfahan Province are not available. Therefore, it is unclear which of these interventions is implemented and to what extent. The aim of this study was to investigate the implementation of VAP preventive measures by nurses in ICUs.
Materials and Methods
This was a descriptive study on 120 nurses in 11 ICUs at 4 hospitals affiliated to the Isfahan University of Medical Sciences, Isfahan. The duration of the study was 4 months (July to October 2014). The inclusion criteria included nurses who were working in ICUs, permanent employees, willing to participate in the study, and providing care for patients under mechanical ventilation for more than 48 hours. Any nurse unwilling to participate in the study was excluded. In this study, the implementation of all measures for the prevention of VAP was assessed through observation of nurses and using a checklist. The researcher assessed compliance with these standards based on the designed checklist. The checklist contained two parts. The first part evaluated the performance of nurses and the second part assessed the physical structures of the ICU. In the first part, part A was related to demographic information and part B included 19-item questions regarding the assessment of performance. The researcher obtained the “Verification Form of VAP Preventive Measures” by referring to the Centers for Disease Control and Prevention (CDC). To ensure the validity of the checklist, content validity was used. Then, the checklist was distributed among 10 professors and faculty members of the School of Nursing and Midwifery, Isfahan University of Medical Sciences, specialist in intensive care, and ICU personnel. After implementing the proposed amendments, the finalized checklist was developed and confirmed by the experts.
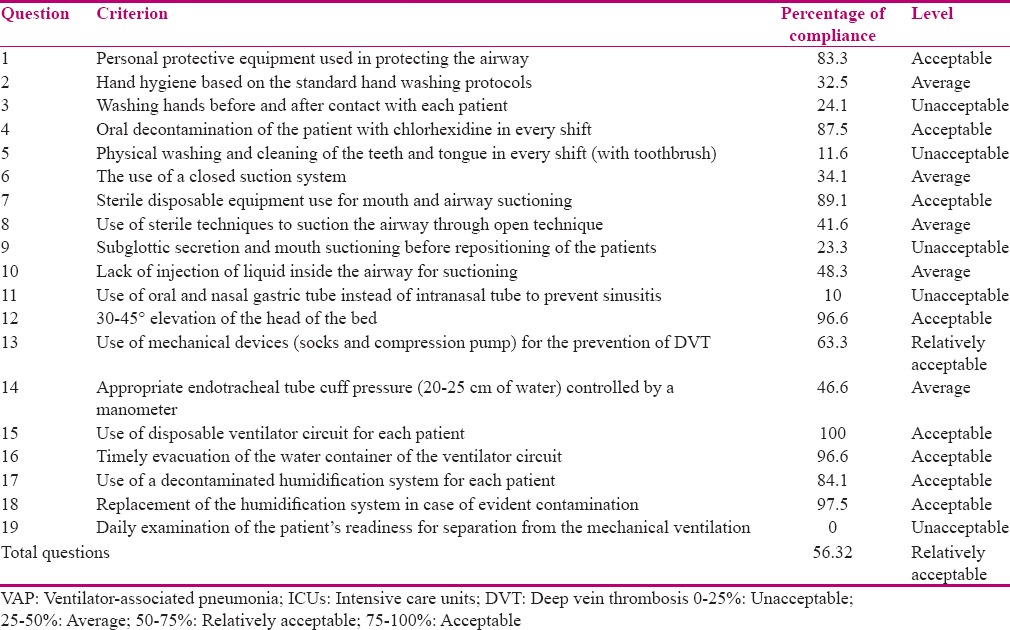
To determine the reliability of the tool, 10 ICU personnel were studied using the checklist in a pilot study. By observing their performance using this tools, the results were analyzed using Cronbach's alpha coefficient (α = 0.698). The reliability of the tool was assessed by evaluators using Wilcoxon test, and the result was P = 0.194. Therefore, evaluation using two evaluators showed no statistically significant difference. In this study, data was collected in a single step in the two morning and evening shifts. The information was collected on two shifts, morning and evening. The obtained data were studied using the Statistical Package for the Social Sciences software (version 20, SPSS Inc., Chicago, IL, USA) and were analyzed using Fisher's exact, Chi-square, and Kruskal–Wallis tests. After calculating compliance with each criterion, the percentages of implementation of measures were classified into 4 groups; 0–25% implementation was considered unacceptable, 25–50% was average, 50–75% was relatively acceptable, and 75–100% was considered acceptable [Table 1].
Table 1.
Frequency distribution of compliance with the preventive criteria for VAP by nurses in ICUs
Ethical considerations
Ethical principles of this study have been approved by Isfahan University of Medical Sciences.
Results
In this study, the performances of 120 nurses in the ICU were observed. The results of the investigation of demographic characteristics showed that contractual employees constituted the largest population of ICU nurses and official employees formed the smallest population. In addition, 85.8% of the nurses were women and 14.2% were men. Regarding work experience, 85.8% of the ICU nurses had less than 10 years of experience. In this study, 98.3% of nurses had a bachelor's degree and 1.7% had a master's degree. The mean (standard deviation) age of the participants was 30.63 (4.75) years.
The results showed that 56.32% of the criteria for the prevention of VAP in the ICU were met; according to analysis of variance results, there was a significant difference between the studied hospitals (P < 0.001). The items that did not have statistically significant differences were compliance with personal protective equipment use in protecting the airway, hand hygiene based on standard protocols, the use of disposable and sterile equipment for airway, and mouth suction (P = 0.168), use of sterile techniques for airway suctioning through open method (P = 0.175), oral and nasal gastric tube use instead of intranasal tube to prevent sinusitis (P = 0.09), 30–45° elevation of the head of the bed (P = 0.524), timely evacuation of the water container of the ventilator circuit (P = 0.332), and humidification system replacement in case of evident contamination (P = 0.181). Items with statistically significant differences included criteria for hand washing or hand sanitizer use before and after contacting each patient (P = 0.001), oral decontamination of the patient with chlorhexidine in every shift (P = 0.002), physical washing and cleaning of the teeth and tongue in every shift (P < 0.001), the use of closed suction system (P < 0.001), subglottic secretion and mouth suctioning before repositioning the patient (P < 0.001), lack of injection of liquid inside the airway for suctioning (P = 0.010), the use of mechanical devices to prevent deep vein thrombosis (DVT) (P < 0.001), appropriate control of the endotracheal tube cuff pressure by a manometer (P < 0.001), and use of a disinfected humidification system for each patient (P < 0.001).
Based on the study findings, compliance with the criteria of hand hygiene before and after contacting each patient, physical washing and cleaning the teeth and tongue in every shift, subglottic secretion and mouth suctioning before repositioning the patients, using oral and nasal gastric tube instead of intranasal tube to prevent sinusitis, and daily examination of the patient's readiness for separation from mechanical ventilation by means of separation was unacceptable.
Compliance with the criteria of personal protective equipment use in protecting the airway, oral decontamination of the patient with chlorhexidine in every shift, disposable and sterile equipment use for airway and mouth suction, 30–45° elevation of the head of the bed, disposable ventilator circuit used for each patient, timely evacuation of the water container of the ventilator circuit, use of a decontaminated humidification system for each patient, and humidification system replacement in case of evident contamination was acceptable.
Based on the findings, the highest and lowest rate of compliance with VAP prevention measures was observed in hospital C and hospital B, respectively. The percentage of compliance in hospital A was 55.70%, hospital B was 49.31%, hospital C was 65%, and hospital D was 63.81%. With regard to the structural measures for the prevention of VAP, the availability of disinfectant solutions for nurses, suitable washing rooms for hands washing, and the availability of an infection control nurse in the unit were implemented in all hospitals. Written protocols and clinical guidelines related to the prevention of VAP were only available in hospital B; VAP monitoring, evaluation, and reporting system did not exist in any of the surveyed hospitals.
Discussion[11,17,18,19,20,21,22,23,24]
The findings of the present study showed that the prevalence of use of personal equipment in protecting the airway was 80.3%. The results of the study by Kandeel et al. showed that wearing gloves was observed in 45.5% of the cases. The results of the current study indicated an acceptable level of compliance with this criterion and a higher prevalence of compliance compared with the study by Kandeel et al. In the present study, the criterion of oral decontamination of the patient with chlorhexidine in each shift was met in 87.5% of cases, its compliance rate was 43.26%, 0%, 6.1%, 45.6%, and 18.87% in the studies by Shaaban Ali, Kandeel et al., Gatell et al., Eom et al., and Behesht Aeen et al., respectively. The comparison of the results of this study and the abovementioned studies showed that the use of mouthwash for patients in the studied units was acceptable.
The findings of this study showed 89.1% compliance with the use of disposable and sterile equipment for mouth and airway suction. Behesht Aeen reported 53.78% compliance with this criteria, and Gatell et al. reported 99% compliance with the use of sterile catheter for suction. The results of the present study were similar to the study by Gatell et al. demonstrating an acceptable compliance with the above criterion.
The compliance with the criterion of 30–45° elevation of the head of the bed was observed in 96.6% of cases in the present study. This rate was 98%, 29.7%, 65.9%, more than 80%, and 40.58% in the studies by Bird et al., Korhan et al., Eom et al., Kiyoshi et al., and Ali, respectively. The results of the present study like that of the study by Bird et al. showed an acceptable level of compliance with this criterion. In the study by Eom et al., despite the intervention, the reported rate of implementation of this criterion was lower than the present study.
The criterion of disposable ventilator circuit use for each patient in all cases was observed and was consistent with the results of the study by Kandeel et al. The findings of this study indicated that the criterion of timely evacuation of the water container of the ventilator circuit was applied in 96.6% of cases. In the study by Kandeel et al., compliance with this criterion was observed in 82.78% of cases and the results of these two studies were consistent.
The findings of the present study showed that the frequency of compliance with the criteria of disinfected humidification system use for each patient and its replacement in case of evident contamination was 84.1% and 97.5%, respectively. In the study by Behesht Aeen et al., the prevention of respiratory equipment contamination was reported at a rate of 37.92%. The results of the present study demonstrated acceptable compliance with this criterion, which had a better status compared to the mentioned study. Regarding compliance with physically washing and cleaning teeth and tongue in every shift, the obtained result showed that this criterion was met in 11.6% of cases. This criterion was not demonstrated in other studies.
The results of the present study showed that compliance with subglottic secretion and mouth suctioning before repositioning of the patient was observed in 23.3% of cases. In the study by Gatell et al. and Eom et al., the rate of compliance with the criterion of subglottic secretion suctioning was reported as 88.6% and 0%, respectively. However, suctioning before repositioning the patient was not assessed in any of the previous studies. The results of the present study showed unacceptable compliance with this criterion in the studied units.
The use of oral and nasal gastric tube instead of intranasal tube to prevent sinusitis was observed in 10% of cases and no study was found in this regard. The results also showed unacceptable compliance with this criterion, and it seemed that this amount of compliance was related to the patients’ conditions. The rate of compliance to the daily examination of the patient's readiness for separation from the ventilator based on the separation tools was zero in all hospitals. In the study by Ali, this amount was also 0%. In the study by Bird et al., examination of the patient's readiness for extubation was at a rate of 96.5%. All nursing interventions related to separating the patients are based on anesthesiologists’ instructions. Thus, not only are nurses not involved in this matter but they also do not have any means to implement it. Therefore, in addition to introducing and training standard separation means, empowering nurses and planning for patients’ separation with the help of an anesthesiologist should be considered as one of the duties of ICU nurses. The findings of this study showed that the rate of compliance with the criterion of hand washing before and after contact with each patient was 24.1%. In the study by Behesht Aeen et al., hand hygiene compliance rate was 72%; the results of this study had a significant difference with that of the present study. Finally, the percentage of compliance with all 19 criteria in all the hospitals was 56.32%, which was relatively acceptable.
Bird et al. reported 86% compliance with VAP prevention criteria, which was obtained from the assessment of 4 criteria. In the study by Micik et al., the rate of compliance with 11 sensitive nursing interventions in the prevention of VAP was over 70%. Kiyoshi et al. evaluated 3 VAP prevention criteria using a questionnaire that was completed by the nurses. The results showed that more than 77% of the nurses complied with these 3 criteria in providing care for ICU patients. Kandeel et al. found 43.70% compliance with the preventive criteria by observing the nurses.
The comparison of the results of the present study with that of the studies by Bird et al., Micik et al., and Kiyoshi et al. showed that the rate of compliance with the preventive criteria of VAP in the ICU was low like that in the study by Kandeel et al. Moreover, there is a need for appropriate planning for nurses to implement VAP prevention measures. Nevertheless, it should also be noted that, in the present study, 19 preventive interventions were studied; however, the overall dimensions of VAP prevention were not taken into consideration in any of the previous studies. The strength of the present study was the method used for data collection, which was conducted by direct observation of the nurses’ performances, without causing reaction or change in their behavior, and therefore, the results show the real performance of the nurses. However, in the study by Kiyoshi et al., data were collected using a questionnaire that was completed by the nurses. In the study by Micik et al., although more criteria were reviewed, the review was carried out after the implementation of an intervention. Nevertheless, in the present study, no intervention was conducted before gathering the information, and the results indicated the common performance of the nurses. In the study by Kandeel et al., which was conducted, like the present study, through direct observation of the nurses and assessment of 12 criteria, the rate of compliance was low.
Overall, the results of this study showed an acceptable performance of the nurses, however, consideration of the prevalence of VAP and existence of risk factors, and its various complications is necessary. It seems that lack of time, personnel, and nurses’ knowledge in this field is effective. Therefore, it is recommended that a preventive clinical guide for VAP be prepared in all wards. Nursing managers should provide training courses and the necessary facilities for providing high quality services in hospitals.
Conclusion
The results showed that compliance with the requirements of VAP prevention by nurses in ICUs was relatively acceptable. Based on these findings, aspects such as personnel training in all VAP prevention measures, hand washing by the nurses, subglottic secretion suctioning specially before repositioning of the patients, daily examination of the patient's readiness for separation from the ventilator, and nurses training in using the standard equipment of separation in all ICUs should be considered. With regards to the structural criteria, the existence of a monitoring system and a written protocol for the prevention of VAP in ICUs requires the serious attention of hospital authorities.
Financial support and sponsorship
Isfahan University of Medical Sciences, Isfahan, Iran. Grant No: 393391.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The above article was the result of the thesis of Ms. Saiedeh Masoumeh Tabaeian, graduate student of the critical care nursing of Isfahan University of Medical Sciences. Our sincere appreciation goes to all the professors of the university, administrators, and nurses working in Alzahra, Amin, Kashani, Noor and Ali Asghar hospitals, who helped in conducting this research.
References
- 1.Sabery M, Shiri H, Moradiance V, Taghadosi M, Gilasi HR, Khamechian M. The frequency and risk factors for early-onset ventilator-associated pneumonia in intensive care units of Kashan Shahid-Beheshti. J Kashan Univ Med Sci. 2013;6:560–9. [Google Scholar]
- 2.Khorvash F, Abbasi A, Meidani M, Dehdashti F, Ataei B. The comparison between proton pump inhibitors and sucralfate in incidence of ventilator associated pneumonia in critically ill patients. Adv Biomed Res. 2014;3:52. doi: 10.4103/2277-9175.125789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rello J, Chastre J, Cornaglia G, Masterton R. A European care bundle for management of ventilator-associated pneumonia. J Crit Care. 2011;26:3–10. doi: 10.1016/j.jcrc.2010.04.001. [DOI] [PubMed] [Google Scholar]
- 4.El Azab SR, El Sayed AE, Abdelkarim M, Al Mutairi KB, Al Saqabi A, El Demerdash S. Combination of ventilator care bundle and regular oral care with chlorhexidine was associated with reduction in ventilator associated pneumonia. Egyptian J Anaesth. 2013;29:273–7. [Google Scholar]
- 5.Afkhamzadeh A, Lahoorpour F, Delpisheh A, Janmardi R. Incidence of ventilator- associated pneumonia (VAP) and Bacterial resistance pattern in adult patients hospitalised at the intensive care unit of Besat Hospital in Sanandaj. SJKU. 2011;16:20–6. [Google Scholar]
- 6.Ebrahimi Fakhar H, Rezaie K, kohestani H. Effect of closed endotracheal suction on incidence of ventilator-associated Pneumonia. SJKU. 2010;15:79–87. [Google Scholar]
- 7.Safdari R, Yazdannik A, Abbasi S. Effect of intermittent subglottic secretion drainage on ventilator-associated pneumonia: A clinical trial. Iran J Nurse Midwifery Res. 2014;19:376–80. [PMC free article] [PubMed] [Google Scholar]
- 8.Chow MC, Kwok SM, Luk HW, Law JW, Leung BP. Effect of continuous oral suctioning on the development of ventilator-associated pneumonia: A pilot randomized controlled trial. Int J Nurs Stud. 2012;49:1333–41. doi: 10.1016/j.ijnurstu.2012.06.003. [DOI] [PubMed] [Google Scholar]
- 9.Gallagher JA. Implementation of Ventilator-Associated Pneumonia Clinical Guideline (Bundle) J Nurse Pract. 2012;8:377–82. [Google Scholar]
- 10.Craven DE, Lei Y, Ruthazer R, Sarwar A, Hudcova J. Incidence and Outcomes of Ventilator-associated Tracheobronchitis and Pneumonia. Am J Med. 2013;126:542–9. doi: 10.1016/j.amjmed.2012.12.012. [DOI] [PubMed] [Google Scholar]
- 11.Micik S, Besic N, Johnson N, Han M, Hamlyn S, Ball H. Reducing risk for ventilator associated pneumonia through nursing sensitive interventions. Intensive Crit Care Nurs. 2013;29:261–5. doi: 10.1016/j.iccn.2013.04.005. [DOI] [PubMed] [Google Scholar]
- 12.Rebmann T, Greene LR. Preventing ventilator-associated pneumonia: An executive summary of the Association for Professionals in Infection Control and Epidemiology, Inc, Elimination Guide. Am J Infect Control. 2010;38:647–9. doi: 10.1016/j.ajic.2010.08.004. [DOI] [PubMed] [Google Scholar]
- 13.Giard M, Lepape A, Allaouchiche B, Guerin C, Lehot JJ, Robert MO, et al. Early- and late-onset ventilator-associated pneumonia acquired in the intensive care unit: Comparison of risk factors. J Crit Care. 2008;23:27–33. doi: 10.1016/j.jcrc.2007.08.005. [DOI] [PubMed] [Google Scholar]
- 14.Muscedere J, Dodek P, Keenan S, Fowler R, Cook D, Heyland D, et al. Comprehensive evidence-based clinical practice guidelines for ventilator-associated pneumonia. J Crit Care. 2008;23:126–37. doi: 10.1016/j.jcrc.2007.11.014. [DOI] [PubMed] [Google Scholar]
- 15.Sundar KM, Nielsen D, Sperry P. Comparison of ventilator-associated pneumonia (VAP) rates between different ICUs. J Crit Care. 2012;27:26–32. doi: 10.1016/j.jcrc.2011.05.019. [DOI] [PubMed] [Google Scholar]
- 16.Arabi Y, Al-Shirawi N, Memish Z, Anzueto A. Ventilator-associated pneumonia in adults in developing countries: A systematic review. Int J Infect Dis. 2008;12:505–12. doi: 10.1016/j.ijid.2008.02.010. [DOI] [PubMed] [Google Scholar]
- 17.Kandeel N, Tantawy N. Current Nursing Practice for Prevention of Ventilator Associated Pneumonia in ICUs. Life Sci J. 2012:9. [Google Scholar]
- 18.Jam Gatell MR, Santé Roig M, Hernández Vian Ó, Carrillo Santín E, Turégano Duaso C, Fernández Moreno I, et al. Assessment of a training program for the prevention of ventilator-associated pneumonia. Nurs Crit Care. 2012;17:285–92. doi: 10.1111/j.1478-5153.2012.00526.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shaaban Ali N. Critical Care Nurses’ Knowledge and Compliance with Ventilator Associated Pneumonia Bundle at Cairo University Hospitals. J Edu Pract. 2013 [Google Scholar]
- 20.Eom JS, Lee MS, Chun H, Choi H, Jung SY, Kim YS, et al. The impact of a ventilator bundle on preventing ventilator-associated pneumonia: A multicenter study. Am J Infect Control. 2014;42:34–7. doi: 10.1016/j.ajic.2013.06.023. [DOI] [PubMed] [Google Scholar]
- 21.Bird D, Zambuto A, O’Donnell C, Silva J, Korn C, Burke R, et al. Adherence to Ventilator-Associated Pneumonia Bundle and Incidence of Ventilator-Associated Pneumonia in the Surgical Intensive Care Unit. Arch Surg. 2010;145:465–70. doi: 10.1001/archsurg.2010.69. [DOI] [PubMed] [Google Scholar]
- 22.Akın Korhan E, Hakverdioğlu Yönt G, Parlar Kılıç S, Uzelli D. Knowledge levels of intensive care nurses on prevention of ventilator-associated pneumonia. Nurs Crit Care. 2014;19:26–33. doi: 10.1111/nicc.12038. [DOI] [PubMed] [Google Scholar]
- 23.Kiyoshi-Teo H, Cabana MD, Froelicher ES, Blegen MA. Prevention Guidelines Adherence to Institution-Specific Ventilator-Associated Pneumonia. Am J Crit Care. 2014;23:201–144. doi: 10.4037/ajcc2014837. [DOI] [PubMed] [Google Scholar]
- 24.Behesht Aeen F, Zolfaghari M, Asadi Noghabi AA, Mehran A. Nurses’ Performance in Prevention of Ventilator associated Pneumonia. Hayat J. 2013;19:17–27. [Google Scholar]


