Abstract
Aim:
This cross sectional study assessed knowledge, attitudes and practices regarding complementary feeding among mothers with children between 6-24 months at the national level.
Methods:
The sample of 492 mothers with children between 6-24 months, with a confidence level of 95%, the acceptable margin of 5%, the expected prevalence of 50% knowledge and effect of 1.3, were interviewed from all regions, in all Kosovo. Data were analyzed using SPSS version 17.0 and presented using descriptive and inferential statistics such as Chi-square with significance level set at 5%.
Results:
Overall, 88.4% of respondents had good knowledge of complementary feeding, while only 38.4% of mothers had good practices regarding time for starting complementary feeding. We found association between maternal knowledge and level of education for complementary feeding.
Conclusion:
There is a need to further explore the factors responsible to improving practices for complementary feeding.
Keywords: Complementary feeding, Knowledge and Practice, Kosova
1. INTRODUCTION
Complementary feeding refers to the process of starting giving foods and liquids other than breast milk to the infants for their nutritional needs due to the insufficiency of the breast milk (1). According to the World Health Organization (WHO), the complementary feeding must possess the following three main characteristics: Timely: Giving foods to all infants should be started from 6 months onwards; Adequate: The complementary foods should be of a nutritional value that can satisfy the growth needs of the child; Appropriate: The foods selected for complementary foods must have variety, be of appropriate texture and in sufficient quantity (2). Inappropriate complementary feeding practices cause to some problems such as stunting, delay in the motor and mental development, neurological and mental fatigue, frequent diarrhea, lack of micro-nutrients, and macro-nutrients or malnutrition (3). Data from the World Bank report shows that the health situation around birth and the first year of life is poor in Kosovo, as well as among the worst in Europe and the region (4). WHO recommends that infants start receiving complementary foods at 6 months of age in addition to breast milk, initially 2-3 times a day between 6-8 months, increasing to 3-4 times daily between 9-11 months and 12-24 months with additional nutritious snacks offered 1-2 times per day, as desired (5). It has been suggested that in addition to disease prevention strategies, complementary feeding interventions targeting this “critical window” are most efficient in reducing malnutrition and promoting adequate growth and development (6). Good nutrition is essential for healthy development. Malnutrition, as a result of bad practice of nutrition and lack of micro-nutrients such as vitamin A, iron, iodine and zinc, will contribute to increased morbidity and mortality among young children (7). A twenty-five children (four per cent) under the age of 5 have stagnated medium or heavy growth or are too short for their age, reflecting malnutrition chronic as a result of not receiving the nutrition adequate for a long period and frequent or chronic diseases. This low percentage shows no apparent problems regarding stagnation in growth or underweight (8). In most developing countries has proven link between practice breastfeeding in the first month of life and neonatal mortality (in the first month of life) and the fact that breast-feeding plays an important role in reducing neonatal mortality (9). Adequate nutrition during infancy and early childhood is essential to ensure the growth, health, and development of children to their full potential. Poor nutrition increases the risk of illness, and is responsible, directly or indirectly, for one third of the estimated 9.5 million deaths that occurred in 2006 in children less than 5 years of age. Inappropriate nutrition can also lead to childhood obesity which is an increasing public health problem in many countries. There is evidence that adults who were malnourished in early childhood have impaired intellectual performance. The first two years of life provide a critical window of opportunity for ensuring children’s appropriate growth and development through optimal feeding. Feeding practice has a lot of implication for the nutritional status of the child. Mothers’ knowledge about nutritious meals for the children influences how the child is fed. In many developing countries infants and young children are most vulnerable to malnutrition because of lack of knowledge on how to feed a child (10). Several observational studies show that maternal knowledge of optimal child feeding practices like exclusive breastfeeding for six months, continued breastfeeding and the timely transition to adequate complementary food is basic to keep health of a child (WHO, 2010) (11). A study by Hellen Keller International (2010) (12) in Baitadi District, Nepal showed that 28% and 42.1% of mothers had the perception that children of 6-12 months should not be fed on eggs and flesh meats, this translated to only 2.1% and 4.4% of their children being fed on eggs and flesh meats respectively. Scientific knowledge demonstrates that maternal knowledge on complementary feeding may positively influence practice or may lead to no change in feeding practices. Sethi et al., 2003 in their study in India, where nutritional education was given to mothers to improve awareness about infant feeding in the variety, quantity, quality and consistency of complementary feeding showed that, 86% complementary feeding practices were inadequate in quality, quantity, frequency and consistency (13). In a similar study in South India, mothers were counseled about the choice of appropriate complementary foods and feeding frequency. The intervention group had improved feeding practices such as avoiding feeding bottles and improved on dietary diversity and the types of complementary foods (14). Knowledge may not translate to practice, a study by Subedi et al (15) on infant and young child feeding practices in Chepang communities in Nepal showed that, only 35% had knowledge about breastfeeding initiation within one hour, 62% had known about exact time for exclusive breastfeeding and 81% mothers had knowledge about appropriate time for introduction of complementary feeding and total time for 11 breastfeeding. Findings from study (16, 17) revealed that a high proportion of the respondents were knowledgeable on the introduction of complementary feeding at 6 months.
Even it is recommended that infants start solid foods at 6 months, about one third of infants 6-8 months old, globally, are not yet eating solid foods. The situation is different among Regions, from about half of infants in South Asia to more than 80 per cent in Latin America and the Caribbean, but the indicator does not reflect how many infants started their first foods before the recommended age of 6 months (34).
2. AIM
The objective of the study is: Assessment of Knowledge, Attitudes, Practices (KAP) of mothers in Kosovo for supplementary food among infant and children 6-24 months.
3. MATERIAL AND METHODS
Study design: This descriptive, cross-sectional study was conducted during May-July 2013, and it assessed the mother’s knowledge and practice of complementary feeding from 28 locations cities, towns and villages across Kosovo. The sample of 492 mothers with infant between 6-24 months, with a confidence level of 95%, acceptable margin of 5%, the expected prevalence of knowledge 50% and effect of 1.3, were interviewed from all regions.
Instrument for data collection: Study is based on interviews using the questionnaire as the instrument for data collection to elicit information from the study participants. The sections of the questionnaire were divided into: sociodemographic characteristics, knowledge on complementary feeding, attitudes and complementary feeding practice of mothers with infant between 6-24 months.
Data analysis: The data collected was analyzed using SPSS version 17.0 and presented using descriptive and inferential statistics such as Chi-square test with the level of significance set at 5%.
Ethics: The study was conducted from the National Institute of Public Health of Kosova and approved from the Board of the National Institute of Public Health of Kosova.
4. RESULTS
4.1. Knowledge
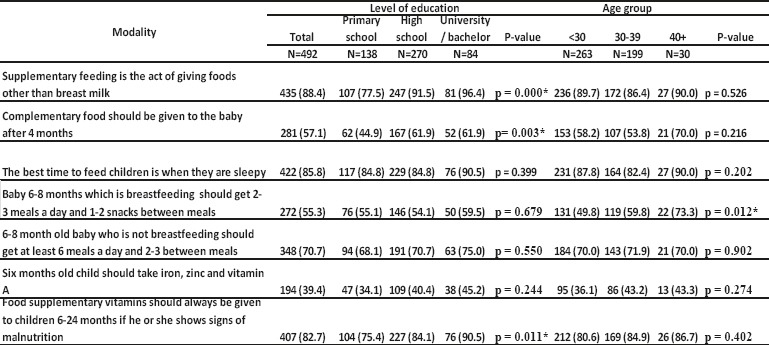
Mother’s knowledge shows significant distinction according to higher level of education regarding perceptions that complementary feeding is the act of giving foods and liquids other than breast milk to the infants (96%), complementary food should be given to the infants after 6 months (61.9% both high school and university) and food supplementary vitamins should always be given to children 6-24 months if he or she shows signs of malnutrition (90.5%). For other modalities: best to feed the children when they are sleepy, baby 6-8 months which is in the breast should get 2-3 meals a day and 1-2 between meals, 6-8 month old baby who is not breastfeeding should get at least 6 meals a day and 2-3 between meals, according to the level of education we didn’t find significant differences.
According to age group, significant level is shown by mothers aged 40+ for: baby 6-8 months which is breastfeeding should get 2-3 meals a day and 1-2 snacks between meals (73.3%) (Table 1).
Table 1.
Level of knowledge regarding supplementary feeding due to level of education and age group
4.2. Attitudes
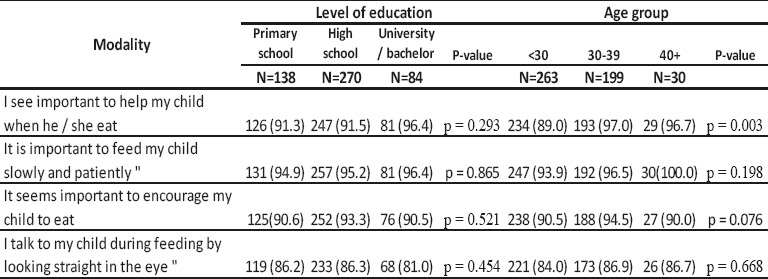
Mother’s attitudes regarding supplementary feeding due to the level of education do not show significant differences whereas according to age group for older mothers (97.0%) there is significant difference for modality: “I see important to help my child when he/she eat” (Table 2).
Table 2.
Mother’s attitudes regarding complementary food due to level of education and age group
4.3. Practices
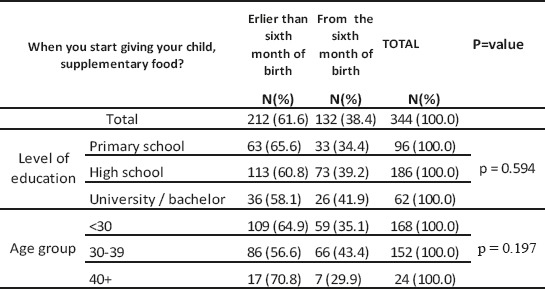
Despite the fact that 57.1% of all mothers know that complementary food should be given after 6 months, in practice 61.6% of them have started feeding their babies with complementary food before 6 months. There are no significant differences in mothers practices according to the level of education and age group, although there is higher percentage of incorrect practices among older mothers (70.8%) (Table 3).
Table 3.
Mother’s practices regarding complementary food due to level of education and age group
4.4. Information
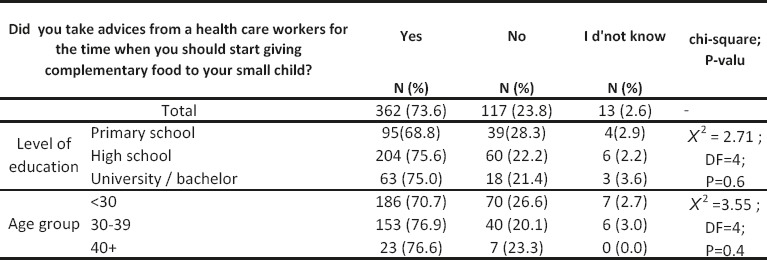
High percentage of mothers (73.6%) are informed by healthcare workers regarding the time when they should start feeding their children with complementary food. According to the level of education and age group there are no significant differences (Table 4).
Table 4.
Information of mother by healthcare workers regarding complementaryy food
5. DISCUSSION
According to this study, the correct knowledge of Mother’s show significant distinction according to higher level of education regarding perceptions that complementary feeding is the act of giving foods and liquids other than breast milk to the infants (96%), complementary food should be given to the infants after 6 months (61.9% both high school and university) and food supplementary vitamins should always be given to children 6-24 months if he or she shows signs of malnutrition (90.5%). Another study showed the correct knowledge of initiation of complementary feeding at 6 months was reported by 53.5% of mothers but it was found to be practiced by only 42.8% (18). The time of introduction and type of complementary food given to an infant are very important for the child’s nutritional status. According to current recommendations (WHO, 2007), complementary feeding should be introduced into the child’s diet at the age of 6 months (5, 19). The study done by Greer and Zutavern (20, 21) shows that delayed introduction of complementary foods until six months of age is thought to decrease a child’s risk of food sensitivity, allergies, eczema and asthma. MICS findings shows that the majority (90 %) of the children in Kosovo were fed with at least the minimum number of meals, only two-thirds (63%) were fed with the minimum number of foods or diversity minimal food, so less than half (49 %) of children aged 6-23 months and only a third (35%) from the poorest economies family feed acceptable minimum nutrition (22). The study done by B. Sasi Kumar et al., majority of mother’s complementary feeding initiated below 6 months (52%) (23).
In children between 6 and 23 months of age, in low and middle-income countries, evidences show that an inadequate diet increases the risk of stunting and micro-nutrient deficiencies (24-25). An analysis of 14 countries found that stunting and underweight is lower in children 6–8 months old who eat solid foods (26).
In our study only 38.4 % of mothers reported that they started with first foods in recommended time which is lower compared to other regions globally (34).
Many parents introduce their children to solid foods before the recommended age of 6 months (28-31) however, there is no added benefit to this practice (32) furthermore this may increase infants’ exposure to alimentary infections (27) and may increase the risk of becoming overweight in childhood (33).
We didn’t find statistical significance according to the level of education and group age of mothers for information they get from health workers since high percentage of mothers (73.6%) are informed by healthcare workers about complementary feeding and starting time of it.
6. CONCLUSION
This study reported significant association between knowledge’s of mothers for complementary feeding according to the level of education as well as for older mothers. There are not significant differences according to the level of education and age except for older mothers for the modality to help their children when they eat. Regarding practices for proper time of starting complementary feeding, we didn’t find significant differences as well as for the information got from health workers for this issue. As we found high percentage of bad practices among women for starting complementary feeding before proper timing there is a need to explore further socio-cultural factors and their impact toward ensuring proper timing for starting complementary feeding.
Footnotes
• Conflict of interest: The authors declare that they have no conflict of interest.
• Authorship: Authors of this manuscript made substantial contribution to: conception and design by Merita Berisha, Naser Ramadani, Drita Zajmi, Ilir Begolli; analysis and interpretation of data by Merita Berisha, Rina Hoxha, Sanije Gashi, Valbona Zhjeqi; drafting the manuscript or revising it critically by Merita Berisha, Naser Ramadani, Rina Hoxha, Drita Zajmi; given final approval of the version to be published by Merita Berisha, Naser Ramadani, Rina Hoxha, Sanije Gashi, Valbona Zhjeqi, Drita Zajmi and Ilir Begolli.
REFERENCES
- 1.Dewey K. Introduction. In: Lutter C, editor. Guiding Principles for Complementary Feeding of the Breastfed Child. Washington, DC: Pan American Health Organization; 2001. p. 8. [Google Scholar]
- 2.Imdad A, Yakoob MY, Bhutta ZA. Impact of maternal education about complementary feeding and provision of complementary foods on child growth in developing countries. BMC Public Health. 2011;11(Suppl 3):S25. doi: 10.1186/1471-2458-11-S3-S25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Salarkia N, Amini M, Eslami Amirabadi M, Dadkhah M, Zowghi T, Heidari H, et al. Mother’s views and beliefs about the role of complementary feeding in children under the age of two in Damavand: A qualitative study. Arak Med Univ J. 2010;13:63–74. [Google Scholar]
- 4.Report of Worl Bank. Kosovo Poverty Assessment, Promoting Opportunity, Security, and Participation for All. p. 28. Available from: http://siteresources.worldbank.org/Kosovo_PA_report_final-16 June 2005.pdf .
- 5.PAHO/WHO. Guiding principles for complementary feeding of the breastfed child. Washington DC, USA: 2003. Available from: http://www.who.int/nutrition/topics/complementary_feeding/en . [Google Scholar]
- 6.Martorell R, Khan LK, Schroeder DG. Reversibility of stunting: epidemiological findings in children from developing countries. Eur J Clin Nutr. 1994;48(Suppl 1):S45–57. [PubMed] [Google Scholar]
- 7.Strategy of Mother Child, Adolescent and Reproductive Health with Action Plan 2011-2015 Kosovo. 2011 [Google Scholar]
- 8.Multiple Indicator Cluster Survey in the Republic of Kosovo 2013-2014. Kosovo Agency of Statistics. 2015 [Google Scholar]
- 9.Huffman SL, Zehner ER, Victora C. Can improvements in breast-feeding practices reduce neonatal mortality in developing countries? Midwifery. 2001;17:80–92. doi: 10.1054/midw.2001.0253. [DOI] [PubMed] [Google Scholar]
- 10.WHO. Global Strategy for Infant and Young Child Feeding. Geneva, Switzerland: 2003. [Google Scholar]
- 11.WHO/UNICEF. Global strategy for infant and young child feeding. Geneva: World Health Organization 2003; 2010. [Google Scholar]
- 12.Hellen keller international, Nepal. Breastfeeding and complementary feeding practices are less than adequate among mothers of children 12-23 months in the Baitadi District of Nepal. Nepal nutrition and food security bulletin. 2010;(3rd issue) [Google Scholar]
- 13.Sethi V, Kashyap S, Seth V. Effect of nutrition education of mothers on infant feeding practices. Indian Journal of Pediatrics. 2003;70:463–6. doi: 10.1007/BF02723133. [DOI] [PubMed] [Google Scholar]
- 14.Hague MFM, Hussain A, Sarkar MM, Hogue A. Breastfeeding Counseling and its effects on the prevalence of exclusive breastfeeding. Journal of Health Population Nutrition. 2004;20(4):312–6. [PubMed] [Google Scholar]
- 15.Subedi N, Paudel S, Rana T, Poudyal AK. Infant and young child feeding practices in Chepang communities. Journal of Nepal Health resource council. 2012;10(21):141–6. [PubMed] [Google Scholar]
- 16.Sanusi RA, Leshi OO, Agada UN. Mother’s knowledge and practice of breastfeeding and complementary feeding in Enugu State, Nigeria. Journal of Research in Nursing and Midwifery (JRNM) 2016 Jan;5(1):29. Available from: http://www.interesjournals.org . [Google Scholar]
- 17.Chapagain RH. Knowledge and Practices of Mothers of Infant and Young Child on Complementary Feeding in Kathmandu, Nepal. PhD Thesis. 2012 [Google Scholar]
- 18.Anit Kujur, Vidyasagar, Shamim Haider, Vivek Kashyap. Knowledge Attitude and Practice of Complimentary Feeding Among Mothers Attending Immunization Centre, RIMS, Ranchi, Jharkhand. International Journal of Interdisciplinary and Multidisciplinary Studies (IJIMS) 2016;3(2):70–6. [Google Scholar]
- 19.WHO. Indicators for assessing infant and young child feeding practices, part 1 definitions. Conclusions of a consensus meeting held on 6-8, November, 2007 in Washington D.C., USA. 2007 [Google Scholar]
- 20.Greer Frank R, Scott H, Sicherer A. Wesley Burks, and the Committee on Nutrition, Section on Allergy, and Immunology. Effects of Early Nutritional Interventions on the Development of Atopic Disease in Infants and Children: The Role of Maternal Dietary Restriction, Breastfeeding, Timing of Introduction of Complementary Foods, and Hydrolyzed Formulas. Pediatrics. 2008;121(1):183–91. doi: 10.1542/peds.2007-3022. [DOI] [PubMed] [Google Scholar]
- 21.Zutavern A, Inken B, Beate S, von Berg A, Ulrike D, Borte M, Kraemer U, Herbarth O, Behrendt H, Wichmann H, Heinrich J LISA Study Group. Timing of Solid Food Introduction in Relation to Eczema, Asthma, Allergic Rhinitis, and Food and Inhalant Sensitization at the Age of 6 Years: Results From the Prospective Birth Cohort Study LISA. Pediatrics. 2008;121(1):e44–52. doi: 10.1542/peds.2006-3553. [DOI] [PubMed] [Google Scholar]
- 22.Multiple Indicator Cluster Survey in the Republic of Kosovo 2013-2014. Kosovo Agency of Statistics. 2015 [Google Scholar]
- 23.Sasi Kumar B, Sudha Priya P, Manohar B, Sekar MN, Siva Ramudu K, Reddy Dudala S, Naveen Kumar C. Knowledge Attitude and Practices regarding complimentary Feeding in mothers of children between 6- 24 months in and around Tirupati. International Journal of Advances in Health Sciences (IJHS) 2015;2(2):226–33. Available from: http://www.ijhsonline.com . [Google Scholar]
- 24.Victora CG, et al. Worldwide timing of growth faltering: revisiting implications for interventions. Pediatrics. 2010;125(3):e473–80. doi: 10.1542/peds.2009-1519. [DOI] [PubMed] [Google Scholar]
- 25.Bhutta ZA, et al. Evidence-based interventions for improvement of maternal and child nutrition: what can be done and at what cost? Lancet. 2013;382(9890):452–77. doi: 10.1016/S0140-6736(13)60996-4. [DOI] [PubMed] [Google Scholar]
- 26.Marriott BP, et al. World Health Organization (WHO) infant and young child feeding indicators: associations with growth measures in 14 lowincome countries. Matern Child Nutr. 2012;8(3):354–70. doi: 10.1111/j.1740-8709.2011.00380.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.WHO Programme of Nutrition: “Complementary feeding of young children in developing countries: a review of current scientific knowledge”. Geneva: 1988. [Google Scholar]
- 28.Alder EM, et al. What influences the timing of the introduction of solid food to infants? Br J Nutr. 2004;92(3):527–31. doi: 10.1079/bjn20041212. [DOI] [PubMed] [Google Scholar]
- 29.Brown A, Rowan H. Maternal and infant factors associated with reasons for introducing solid foods. Matern Child Nutr. 2016;12(3):500–15. doi: 10.1111/mcn.12166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Doub AE, Moding KJ, Stifter CA. Infant and maternal predictors of early life feeding decisions. The timing of solid food introduction. Appetite. 2015;92:261–8. doi: 10.1016/j.appet.2015.05.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kimani-Murage EW, et al. Patterns and determinants of breastfeeding and complementary feeding practices in urban informal settlements, Nairobi Kenya. BMC Public Health. 2011 doi: 10.1186/1471-2458-11-396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dewey KG. Nutrition, growth, and complementary feeding of the breastfed infant. Pediatr Clin North Am. 2001;48(1):87–104. doi: 10.1016/s0031-3955(05)70287-x. [DOI] [PubMed] [Google Scholar]
- 33.Pearce J, Taylor MA, Langley-Evans SC. Timing of the introduction of complementary feeding and risk of childhood obesity: a systematic review. Int J Obes (Lond) 2013;37(10):1295–306. doi: 10.1038/ijo.2013.99. [DOI] [PubMed] [Google Scholar]
- 34.UNICEFs Report. From the First Hour of Life, Making the case for improved infant and young child feeding everywhere. 2016. Available from: https://data.unicef.org/resources/first-hour-life-new-report-breastfeeding-practices/


