Abstract
Objective
The need to understand potential precipitants of smoking relapse is exemplified by relapse rates as high as 95%. The Self-Control Strength model, which proposes that self-control is dependent upon limited resources and susceptible to fatigue, may offer insight into relapse processes. The current study tested the hypothesis that self-control depletion (SCD), produced from engagement in emotional suppression, would serve as a novel antecedent for cessation failure, as indexed by a validated laboratory analogue of smoking lapse and relapse. We also examined whether SCD effects interacted with those of a well-established relapse precipitant (i.e., nicotine deprivation). Craving and behavioral economic indices (delay discounting and demand) were tested as hypothesized mechanisms for increased cessation failure. Ultimately, a moderated mediation model was used to test nicotine deprivation as a hypothesized moderator of SCD effects.
Method
We used a 2 ×2 (12-hour deprivation vs. no deprivation; SCD vs. no SCD) factorial between-subjects design (N = 128 smokers).
Results
The primary hypothesis of the study was supported, as SCD increased lapse behavior (p = .04). Nicotine deprivation significantly increased craving, cigarette demand, delay discounting, and lapse behavior. No main effects were found for SCD on putative mediators (i.e., craving, demand, discounting), but the SCD and deprivation manipulations interacted upon craving (p = .04). The moderated mediation model was significant. SCD was found to increase craving among nicotine deprived smokers, which mediated effects on lapse behavior.
Conclusions
SCD appears to play an important role in smoking relapse and may be a viable target for intervention.
Keywords: self-control, smoking, behavioral economics, withdrawal, relapse
Tobacco use is the leading preventable cause of mortality worldwide, accounting for over 5 million deaths per year (WHO, 2011). In the United States alone, smoking has caused approximately 20 million deaths over the past 50 years, and incurs at least $289 billion in annual medical and other economic costs (USDHHS, 2014). Fortunately, years of life lost can be reduced 90% if cessation occurs by age 40, and those who quit by age 60 can still mitigate this loss by 40% (USDHHS, 2014). Nevertheless, 17% of adults in the United States continue to smoke (CDCP, 2015), and 95% of those who make a cessation attempt without formal treatment relapse within 1 year (CDCP, 2011). Thus, a clear need exists to better understand the antecedents and mechanisms of cessation failure as a guide to intervention development. Shiffman and colleagues (2006) outlined cessation failure milestones that can be targeted, including the amount of time between initial abstinence and an act of smoking again (i.e., lapse) and progression from a lapse to regular smoking (i.e., relapse).
Nicotine Withdrawal, Craving, and Cessation Failure
The majority of smokers relapse within a week of initial cessation (Partos, Borland, Yong, Hyland, & Cummings, 2013), which corresponds with nicotine withdrawal trajectories (Piasecki, Fiore, & Baker, 1998). Nicotine withdrawal is characterized by an array of aversive behavioral, affective, cognitive, and physiological symptoms that emerge as nicotine levels decrease (Hughes, 2007), detectable within 30 minutes of abstinence (Hendricks, Ditre, Drobes, & Brandon, 2006). The most robust effects of acute abstinence (e.g., 12 hours) appear to occur on negative affect (i.e., dysphoria, anxiety, irritability) and craving (Leventhal, Waters, Moolchan, Heishman, & Pickworth, 2010). Symptom severity, volatility, and trajectory predict cessation failure (McCarthy, Piasecki, Fiore, & Baker, 2006; Piasecki, Jorenby, Smith, Fiore, & Baker, 2003, 2003; Piasecki et al., 2000). Multi-predictor models of all symptoms suggest that negative affect and craving contribute independently to cessation failure (Piper et al., 2011), but craving typically has the strongest predictive validity (McCarthy et al., 2006; Piper et al., 2008). That reactivity to acute nicotine deprivation has predictive utility suggests a timeframe (e.g., initial quit day) that may facilitate the detection of those at risk for relapse.
Behavioral withdrawal, in addition to pharmacologic withdrawal, may also contribute to cessation failure (Baker, Japuntich, Hogle, McCarthy, & Curtin, 2006; Piper, 2016). The inability to engage in the well-learned behavior of smoking, and efforts to resist conditioned responses to smoke, likely produces behavioral withdrawal (i.e., the act of smoking is no longer available as a strategy to cope with withdrawal). Theoretically, the newfound coping demands experienced by former smokers require the use of controlled cognitive resources to override automatic motivational processes and maintain abstinence. This suggests long-term abstinence may be determined, in part, by the amount of self-control resources a former smoker has and whether these resources are immutable.
Self-Control Depletion as a Novel Precipitant to Cessation Failure
The Self-Control Strength Model (Baumeister, Bratslavsky, Muraven, & Tice, 1998) defines self-control as the conscious, deliberate, and effortful ability to manipulate one’s own responses (Baumeister, Vohs, & Tice, 2007). This theory posits that self-control resources are limited and susceptible to fatigue, a supposition that has received empirical support as described in a meta-analysis of 198 experimental studies (Hagger, Wood, Stiff, & Chatzisarantis, 2010). These studies demonstrate that engaging in an effortful task (e.g., emotional suppression, resisting temptations), relative to a comparable but benign task (e.g., acting naturally), results in performance decrements on a subsequent task that requires effort/self-control (d =.62; typically indexed by persistence on a frustrating behavioral task). This sequential-task paradigm has employed a variety of initial and secondary tasks, which supports the notion of self-control as domain independent. Given the relevance of self-control depletion (SCD) across a multitude of behaviors not surprisingly this theoretical account has been met with empirical scrutiny. Carter and colleagues (2013, 2014, 2015) conducted an elegant set of secondary meta-analyses to examine publication bias and small study bias observed in the literature. These findings question the robustness and reliability of the SCD effect size estimates observed by Hagger and colleagues (2010). Experimental studies with null SCD effects are also beginning to emerge in the literature (Lurquin et al., 2016; Xu et al., 2014), including a large-scale, multi-lab, study (Hagger et al., in press). Others have called into question the underlying mechanisms of SCD effects on behavioral outcomes, and suggest SCD and its aftereffects are best explained through motivational and attentional processes rather than a finite resource (Inzlicht, Schmeichel, & Macrae, 2014; Kurzban, Duckworth, Kable, & Myers, 2013).
Despite controversy regarding tenets of the Self-Control Strength theory, evidence has accumulated from other areas of research to support the hypothesis that a short bout of self-control has acute consequences. Specifically, the emotion regulation literature has relied heavily on emotional suppression manipulations for over two decades (e.g., Gross & Levenson, 1993), which are nearly identical to procedures used in the SCD literature (Muraven, Tice, & Baumeister, 1998; Vohs & Heatherton, 2000). Inhibiting ongoing emotion-expressive behavior is commonly applied in everyday life (Gross et al., 2006), and is particularly relevant to modern models of addiction (Baker et al., 2004). A meta-analysis by Webb and colleagues (2012) found suppression manipulations had a negligible impact on subjective experience (d = .03; k = 92), small detrimental impact on physiological responses (d = −.19; k = 34), and large effects on behavior (i.e., emotional expression; d = .90; k = 43). Thus, while emotional suppression strategies may be effective at hiding emotional states, it provides no relief from subjective effects of the emotion, and comes with cognitive and physiological costs.
SCD may be integral to both maintenance and cessation of addictive behaviors (Baumeister & Vonasch, 2015). We previously proposed that state-dependent self-control resources may be central to the maintenance of nicotine dependence (Heckman, Ditre, & Brandon, 2012). This suggestion was supported by experimental studies that found dependent smokers to be more likely to smoke a cigarette during a “study break” after resisting the consumption of delectable foods (Shmueli & Prochaska, 2009, 2012), presumably due to the depletion of self-control resources needed to resist cravings to smoking (Hagger et al., 2013). Additionally, we found evidence that smoking can restore depleted self-control resources (Heckman et al., 2012), suggesting a negative reinforcement pathway that may maintain nicotine dependence. Thus, SCD may serve as a mechanism for relapse; however, the effects of SCD have never been tested on smoking in a context similar to a quit attempt (i.e., current withdrawal, competing motivation not to smoke). The current study was designed to fill this gap and examines SCD effects when abstinence is incentivized (i.e., a simulated quit attempt), among both satiated and nicotine deprived smokers.
Translational Paradigms to Detect Cessation Failure
Identification of lapse precipitants has been a critical first step for understanding cessation failure, given that approximately 90% of those who have an initial lapse progress to continued smoking (Brandon, Tiffany, Obremski, & Baker, 1990). Substantial time, effort, and expense is required to identify important precipitants (e.g., craving), as this traditionally has occurred in the context of large-scale clinical trials. Antecedents have also been identified via retrospective self-report in cross-sectional designs (Shiffman, 1982, 1986), prospectively within studies that used ecological momentary assessment (Shiffman, 2009), and more recently, in studies leveraging GPS-enabled smartphones (Kirchner et al., 2013). Although these designs have strong external validity in that they examine long-term behavioral outcomes, inferring causality oftentimes is difficult given that antecedents are not experimentally manipulated directly. Thus, a vast evidence base must accumulate before a robust pattern can be observed conclusively.
To address this, laboratory paradigms of cessation failure have been developed to examine mechanistic processes and screen potential cessation pharmacotherapies in an internally valid, timely, and cost-efficient manner (McKee, 2009; Perkins & Lerman, 2014). As such, these paradigms optimize the clinical utility of human laboratory research by facilitating the translation of basic behavioral science to applied clinical research. These paradigms also offer methods for reverse translational research that tests treatment outcome findings within the laboratory setting (Roche et al., 2014). McKee and colleagues (2009) have developed a cessation failure paradigm that captures lapse and relapse behaviors within a single experimental session, through the provision of financial incentives for abstinence. The lapse analogue for this paradigm is the number of minutes smoking is resisted during a 50 minute time period (i.e., latency to initial use), and relapse is captured by the number of cigarettes smoked during a 60 minute time period (i.e., continued or regular use). This paradigm has verified relapse antecedents commonly found in treatment outcome research, as increased lapse behavior has been observed following experimental manipulations of acute nicotine deprivation (1, 6, and 18 hours), stress/negative affect, and alcohol consumption (Leeman, O’Malley, White, & McKee, 2010; McKee, Krishnan-Sarin, Shi, Mase, & O’Malley, 2006; McKee et al., 2010; McKee, Weinberger, Shi, Tetrault, & Coppola, 2012). That known predictors of relapse are detected by the task suggests that it may also have utility for identifying novel relapse precipitants. Furthermore, the controlled setting in which the task is employed allows for the examination of mechanisms that may underlie the transition from abstinence to smoking (e.g., craving). Thus, this laboratory analogue task can be utilized to test the antecedents and mechanisms of cessation failure.
Behavioral Economic Indices as Novel Mechanisms for Cessation Failure
There is great opportunity for behavioral scientists to delineate mechanisms of SCD, which remain poorly understood. SCD has been proposed to cause performance deficits because individuals shift priorities away from long term goals towards short term goals (Tice, Bratslavsky, & Baumeister, 2001); however, this has yet to be demonstrated.
Delayed Reward Discounting
Variation in intertemporal reward preferences is an integral construct within behavioral economic theory, termed delayed reward discounting (Bickel, Koffarnus, Moody, & Wilson, 2014). Discounting tasks have participants choose between a series of smaller immediate monetary rewards versus larger delayed monetary rewards, and responses are used to objectively quantify impulsive decision-making (Madden & Bickel, 2009). As preferences for immediate rewards increase, the discounting rate becomes steeper (i.e., greater discounting), indicating higher levels of impulsivity. Discounting is often conceptualized as a stable individual difference variable (Anokhin, Golosheykin, & Mulligan, 2015), but this may be moderated by situational factors (Kirby, 2009). Indeed, empirical evidence supports discounting is susceptible to state fluctuations through variety of experimental manipulations (Koffarnus, Jarmolowicz, Mueller, & Bickel, 2013). Therefore, discounting tasks may provide a method to test the assumption that SCD causes greater impulsive decision-making, as suggested by the Self-Control Strength Model.
The clinical relevance of delay discounting is because it functions as a behavioral marker of addiction (Bickel et al., 2014). Excessive discounting is readily apparent among smokers, who often choose the short-lived, immediate, rewards of drug use (e.g., pleasurable effects and/or withdrawal reversal) over larger delayed rewards of abstinence (e.g., health, social, and economic benefits). Indeed, a meta-analysis of 17 studies indicated that smokers have higher discounting rates than nonsmokers (d = .57), across both clinical and subclinical samples (MacKillop et al., 2011). Within smokers, greater discounting is associated with nicotine dependence and predicts days to lapse (e.g., MacKillop & Kahler, 2009; Sheffer et al., 2012). Furthermore, experimental manipulations of acute nicotine deprivation have been found to increase discounting (Ashare & Hawk, 2012; Field, Santarcangelo, Sumnall, Goudie, & Cole, 2006; Mitchell, 2004), suggesting that discounting may serve as a novel mechanism for cessation failure.
Demand
Behavioral economists have also developed objective behavioral tasks that assess the relative reinforcement value of commodities, termed demand (Bickel, Johnson, Koffarnus, MacKillop, & Murphy, 2014). Specific to smoking, purchase tasks quantify participants’ cigarette consumption across varying levels of cost (Jacobs & Bickel, 1999; MacKillop et al., 2008). Responses generate multiple indices of consumption, expenditure, and price sensitivity (Bidwell, MacKillop, Murphy, Tidey, & Colby, 2012). Elevated cigarette demand is associated with higher levels of nicotine dependence (MacKillop & Tidey, 2011; Murphy, MacKillop, Tidey, Brazil, & Colby, 2011), lower motivation to quit (O’Connor et al., 2016, and greater cessation failure (Mackillop et al., 2015). Additionally, cigarette demand is increased through experimental manipulation of acute nicotine deprivation (MacKillop et al., 2012). Thus, demand may serve as a novel motivational process that underlies cessation failure.
Conceptually, there appears to be overlap between the constructs of demand and craving, in that they index motivation to use a substance. However, correlations between measures of demand and craving often are low in magnitude (Acker & MacKillop, 2013), perhaps because demand indices reflect motivational processes that occur outside subjective awareness, whereas self-reported craving is an entirely subjective experience. For example, participants are unlikely to calculate expenditure for each price and infer their aggregate demand curve slope. Thus, these constructs may serves as complementary assessment tools, and indeed, each provide unique predictive validity (Acker & MacKillop, 2013; MacKillop et al., 2012; MacKillop et al., 2010). Purchase tasks may be particularly helpful for the detection of SCD effects, which tend to influence behavioral, but not self-report, indices (Hagger et al., 2010). No relationship has been observed between SCD and craving across three studies of non-deprived smokers (Heckman et al., 2012; Shmueli & Prochaska, 2009, 2012). The current study is the first to examine the influence of SCD on motivation to smoke as measured via demand indices, and to examine SCD effects on craving among smokers in acute nicotine withdrawal (in addition to satiated smokers). Through the application of novel assessment tools and unique samples we anticipated our study design would be well-suited to delineate SCD effects.
Current Study
In summary, evidence suggests that: 1) acute nicotine deprivation is a well-established context that contributes to cessation failure, as indexed by real world treatment outcomes and analogue tasks; 2) deprivation manipulations cause increases in craving, demand, and discounting; 3) craving, demand, and discounting predict cessation failure, and 4) SCD may promote cessation failure. Therefore, behavioral economic constructs and craving offer clinically relevant pathways through which experimental manipulations may influence smoking behavior. These constructs also offer avenues to test theory-driven pathways (i.e., impulsive decision-making, motivation) that may be influenced by SCD.
A factorial experimental design that tests an established (i.e., deprivation), and a novel (i.e., SCD), relapse precipitant on a cessation failure task provides an internally valid method to identify novel contextual factors that may precede relapse in the real world. An additional strength of this design is that the magnitude of the main effects for the relapse precipitants can be compared, and their interaction examined. The current study is the first to apply this laboratory model to examine SCD as a novel contributor to cessation failure. Primary hypotheses tested were that SCD and nicotine deprivation manipulations would produce greater smoking lapse/relapse behavior (i.e., decreased latency to smoke/increased cigarette consumption), compared to the control conditions. Additionally, we tested the hypotheses that SCD and nicotine deprivation manipulations would produce elevated craving, demand, and discounting, compared to the control conditions. We also hypothesized these experimental manipulations would interact, such that those deprived and depleted would evince the greatest effects, relative to the remaining three conditions. This is based on the assumption that deprivation itself leads to a state of SCD, as suggested by theory regarding coping demands associated with nicotine withdrawal (Baker et al., 2006; Piper, 2016), and experimental findings to support nicotine deprivation can produce performance decrements on persistence tasks that require self-control (Bernstein, Trafton, Ilgen, & Zvolensky, 2008). Finally, we planned to test an integrated moderated mediation model for primary outcomes found to be influenced by SCD, with nicotine deprivation as the moderator and craving, demand, and discounting as candidate mediators. We planned to test putative mediators only if initial screening indicated they were significantly influenced by the SCD manipulation, and hypothesized that craving, demand, and discounting would mediate smoking lapse/relapse.
Method
Experimental Design Overview
We employed a 2 × 2, crossed-factorial, between-subjects design to evaluate the hypothesized interaction between SCD and nicotine deprivation conditions. Participants were randomly assigned to one of four conditions (No SCD + No Deprivation, SCD + No Deprivation, No SCD + Deprivation, and SCD + Deprivation), stratified by gender.
Participants
Participants were recruited from the Tampa, Florida area, via newspaper and electronic advertisements. Advertisements stated: “Smokers needed for research study. If you are a smoker between the ages of 18 and 65 you may qualify.” Prospective participants were screened via telephone for the following inclusion criteria: English-speaking, 18-65 years of age, smoked at least 15 cigarettes per day, and smoked at this rate for at least one year. Prospective participants were also screened for the following exclusion criteria: concurrent use of other nicotine or tobacco products, actively attempting to quit smoking (i.e., taking action to quit, such as enrollment in a cessation program or using cessation medications), pregnant, and hearing or visual impairment that would interfere with study procedures. Of the 164 participants who met telephone screening criteria, one per condition (i.e., four) were excluded at the experimental session due to other tobacco/nicotine use or active cessation attempt. Twenty eight participants randomized to the deprivation conditions and four participants assigned to the non-deprived conditions were excluded due to failure to meet pre-session expired carbon monoxide (CO) concentration levels (see below), yielding a final sample size of 128 participants (32 per group).
Measures
Participant Characteristics
Demographic and smoking history information was collected at baseline. This included the Fagerström Test for Nicotine Dependence (Heatherton, Kozlowski, Frecker, & Fagerstrom, 1991), an 11-point single item scale of cessation motivation (Contemplation Ladder; Biener & Abrams, 1991), and an index of cessation self-efficacy that aggregated confidence in the ability to quit smoking for a week, month, and year (α = .79). We also administered an assessment of impression management (Paulhus, 1991). Correlational analyses indicated impression management was not associated with any of the mediators/dependent variables from the current study (ps > .10).
Nicotine Deprivation Manipulation Check
Compliance with the 12 hour deprivation manipulation instructions was verified via self-reported nicotine abstinence and pre-session expired CO concentration levels. Participants randomized to the deprivation conditions were required to have a CO of ≤ 11ppm (Leventhal et al., 2010), and those non-deprived were required to have a CO level greater than 11ppm. Additionally, participants completed the 9-item version of the Minnesota Nicotine Withdrawal Scale (Hughes & Hatsukami, 1986), which yielded a reliable total withdrawal score (α = .82).
SCD Manipulation Check
The degree to which participants followed the assigned SCD instruction set was assessed with a 3-item (α = .82) emotional suppression index (Gross, 1998; Heckman et al., 2012). Subjective cognitive depletion was assessed with a 3-item (α = .76) composite index of how effortful, difficult, and fatiguing it was to follow the instruction set (Baumeister et al., 1998; Heckman et al., 2012). Emotional suppression and cognitive depletion scores were on a 7-point Likert scale, with possible scores of 0-6. We also assessed positive and negative affect via the Mood Form (Diener & Emmons, 1984) before and after the manipulation (α’s > .86). Finally, we examined glucose utilization, defined as the change in glucose levels from baseline to post-depletion task, as a biological proxy for self-control strength (Gailliot et al., 2007). Greater decreases in glucose have been considered to indicate greater SCD as found in a meta-analysis of five prior studies (d = −.87; Hagger et al., 2010), although more recent studies call into question whether glucose levels are a viable proxy for SCD (see Beedie & Lane, 2012; Inzlicht & Schmeichel, 2012; Kurzban, 2010; Molden et al., 2012). A digitized Aviva glucose meter, disposable lancing device, and a disposable test strip were used to test glucose levels (mg/dL). To allow pre-session glucose levels to stabilize (i.e., reduce error variance), all participants were asked to abstain from eating for 2 hours before their appointment time (Gailliot et al., 2007).
Craving
We used a composite craving score that was not subject to ceiling effects commonly observed in heavy smokers following nicotine deprivation, and that took into account expected baseline differences between deprivation conditions (Sayers & Sayette, 2013; Sayette, Martin, Hull, Wertz, & Perrott, 2003; Sayette, Martin, Wertz, Shiffman, & Perrott, 2001). Composite craving was calculated by multiplying baseline craving ratings on the Tobacco Craving Questionnaire-Short Form (Heishman, Singleton, & Pickworth, 2008) with proportion of change as measured by a Magnitude Estimation of Urge score completed after the SCD manipulation (Sayette et al., 2001). The magnitude estimate measure asked participants to compare their current urge to smoke, relative to their baseline urge (arbitrarily assigned a value of 10). Thus, the composite craving index accounts for 1) initial craving and 2) increases in craving from the SCD. Sayette and colleagues (2001) have used composite scores to examine acute responses to smoking-specific cues among deprived, and non-deprived, smokers.
Delayed Reward Discounting
The Monetary Choice Questionnaire is a validated assessment of discounting (Kirby, Petry, & Bickel, 1999). Participants made 27 choices between smaller rewards available immediately and larger rewards available after a delayed period of time. These reward choices are preconfigured at various levels of hyperbolic discounting, and participants’ choices yield temporal discounting estimates (k) of reward at three levels of reward magnitude (small: $25–$35; medium: $50–$60; large: $75–$85). Although all reward choices were hypothetical, this task has convergent validity with choices that are actualized (Bickel, Pitcock, Yi, & Angtuaco, 2009; Lagorio & Madden, 2005; Madden, Begotka, Raiff, & Kastern, 2003; Madden et al., 2004). Prior to analyses reported below, principal component analysis (PCA), with direct oblimin rotation, was conducted on the three k values to derive a single magnitude-independent discounting index. Similar to prior studies that employed this method (VanderBroek, Acker, Palmer, de Wit, & MacKillop, 2016), the PCA derived discounting index accounted for a high proportion of variance (85.01%) and was strongly correlated with each of the three k values (rs>.90). The PCA derived discounting index was used for subsequent analyses, thereby reducing risk for Type I error.
Demand
Demand was assessed with a state version of the Cigarette Purchase Task (MacKillop et al., 2008; Murphy et al., 2011), which asked participants to indicate how many cigarettes they would consume if given the immediate opportunity. Responses across 21 price intervals ($0-$5) were used to generate demand curves for each participant (i.e., consumption at each price). Oftentimes, researchers have examined five indices derived from demand curves (Hursh & Silberberg, 2008; Murphy & MacKillop, 2006), including: intensity (cigarette consumption at the lowest price), breakpoint (first price at which cigarette consumption is zero), Pmax (price at which expenditure is maximized), Omax (maximum financial expenditure on cigarettes), and elasticity of demand (sensitivity of cigarette consumption to increases in cost). Another approach for estimating demand is to quantify the area under the demand curve (Amlung, Yurasek, McCarty, MacKillop, & Murphy, 2015). The single demand metric produced from this method takes into account all aspects of the demand curve, and has been found to be strongly correlated with the five traditional demand indices (rs>.40). We opted for the area under the curve approach to reduce the likelihood of Type I error in the current study. Across the entire sample the maximum consumption values for each of the prices were used to define the total area (174 in the current sample). Each participant’s area under the curve was divided by the total area to provide proportionate values (0.0-1.0) such that larger values reflect higher demand. We administered a practice purchase task (on pizza) at baseline to familiarize participants with the task.
Prior to area under the curve analyses, cigarette purchase task data were screened for low effort responding, defined as more than two contradictions at escalating prices or invariant responses (Acker & MacKillop, 2013) and based on trend and bounce criteria recommended to identify nonsystematic responding (Stein, Koffarnus, Snider, Quisenberry, & Bickel, 2015). Low effort responding was observed for five participants. Similar results were observed when demand analyses were conducted with these participants excluded, and when their data were mean imputed, and we report the latter below. Data were examined for distribution abnormalities and outliers, defined as z > 3.29 (i.e., p < .001, two-tailed test), and those identified were recoded as one unit above the next highest non-outlier at the second decimal (Tabachnick & Fidell, 2013).
Lapse/Relapse Behavior
The lapse/relapse laboratory analogue task was comprised of 1) delay and 2) self-administration periods (McKee, 2009). At the beginning of the delay period, a tray containing eight preferred brand cigarettes, an ashtray, and a lighter were presented to participants, with instructions that they could begin smoking at any point over the next 50 minutes. They were also informed that they could earn $1 for every 5 minutes they delayed smoking, with a maximum payment of $10 over the 50 minute period. The 60 minute smoking self-administration period was initiated when a decision to smoke was made, or after the 50 minute delay period had expired. During this ad libitum smoking period, participants were instructed to “smoke as little or as much as you wish.” The primary dependent variables were latency to smoke (i.e., lapse) and the number of cigarettes smoked (i.e., relapse).
Participants were informed the duration of the experimental session would be the maximum potential time to complete the task (i.e., 110 minutes), regardless of performance on the delay period. However, five participants chose to forego the task to leave the experimental session early and were excluded from the latency to smoke analyses (four were in the no SCD + no deprivation condition and one from SCD + no deprivation condition). Three additional participants chose to terminate the experimental session during the ad lib portion and were excluded from cigarette consumption analyses (two were in the SCD + deprivation condition and one from SCD + no deprivation condition). Thus, the final sample for all lapse and relapse behavior analyses consisted of 123 and 120 participants, respectively.
Procedure
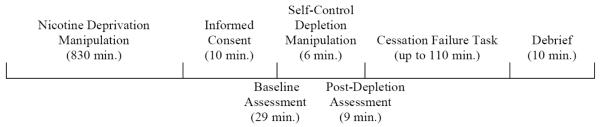
The experimental session involved obtaining informed consent and HIPAA authorization, collection of baseline measures, the SCD manipulation, collection of post-depletion measures (e.g., craving, discounting, and demand), and the cessation failure task. The average duration of each component is depicted in Figure 1. Participants were compensated $45, with the potential to earn up to $10 more based on smoking behavior during the lapse/relapse task. All procedures were approved by the Institutional Review Board at the University of South Florida.
Figure 1.
Schematic timeline of study procedures (and average duration).
Nicotine Deprivation Manipulation
Those randomized to the deprivation conditions were instructed to abstain from using any nicotine products for 12 hours prior to their laboratory session. Non-deprived participants were instructed to smoke one cigarette exactly 5 minutes prior to their appointment to standardize pre-session smoking.
SCD Manipulation
All participants watched the same six minute emotionally evocative video clip depicting mutations and death of sea life (Baumeister et al., 1998; Heckman et al., 2012), and were informed they would be video-recorded while viewing the clip. Those in the SCD conditions were instructed to: “Remain completely neutral on the inside and out. Please try your best not to let any feelings or responses you may have show on your face, and to the best of your ability, try to keep all of your internal reactions suppressed.” Participants in the no SCD conditions were instructed: “Be as natural as possible, both on the inside and out. If you have any feelings or reactions to the movie, let them flow naturally.”
Data Analyses
Preliminary
Analyses of variances (ANOVAs) and Chi-square analyses were used to test that randomization led to equivalent group characteristics, and zero-order correlations examined relationships between baseline, potential mediator, and outcome variables. Variables were included as covariates in subsequent analyses when baseline differences were detected, and when baseline variables were correlated with putative mediators and primary outcomes. ANCOVAs were used for manipulation checks.
Putative Mediator Screening
Prior to formal tests of mediation, we screened proposed mediators by examining how they were influenced by the experimental manipulations.
ANCOVAs were used for craving, demand, and delay discounting. Putative mediators that were significantly impacted by the SCD manipulation were included in moderated mediation analyses.
Primary
ANCOVAs were used to examine lapse/relapse task performance. This study was powered at .80 to detect ‘medium’ sized main and interaction effects, with a two-tailed alpha level of .05 (Cohen, 1988).
We planned to test for moderated mediation via conditional process analyses (PROCESS; Hayes, 2013) to follow-up on ANCOVA analyses that suggested significant SCD effects on the lapse/relapse task. We anticipated craving, discounting, and demand would be included as mediators, and that direct and indirect effects of the SCD manipulation would be moderated by nicotine deprivation (i.e., model 8). Ultimately, the moderated mediation model tested was based on initial screening analyses described above such that mediators/moderators were included only if significant, thereby improving model parsimony. As recommended by Hayes (2013), data were resampled 10,000 times (with replacement) and 95% confidence intervals (bias corrected) were calculated. The direct effect of the SCD manipulation, specific indirect effects of putative mediators, and the overall index of moderated mediation were considered statistically significant if their confidence intervals did not include zero (Hayes, 2015). The study was adequately powered (>.80) to detect moderated mediation (Preacher, Rucker, & Hayes, 2007). All analyses were conducted with SPSS v23, with traditional significance levels set at p < .05 (two-tailed).
Results
Preliminary Analyses
Participant Characteristics
As depicted in Table 1, the final sample (N = 128) consisted of equal proportions male/female. Of the final sample, 75% identified as Caucasian, 20% as African American, 2% American Indian or Alaskan Native, 2% Native Hawaiian or other Pacific Islander, and 1% Asian. The majority of participants had not obtained a college degree and reported an annual household income less than $20,000. On average, participants were 37 years of age, smoked 20 cigarettes per day, and were moderately to highly nicotine dependent (6 on 0-10 scale). Participants indicated moderate interest in quitting smoking (~5 on 0-10 scale), but minimal self-efficacy to do so (~1 on 0-4 scale).
Table 1.
Participant characteristics, with means (and SDs) or percentages
| No Self-Control Depletion + No Nicotine Deprivation (n = 32) |
Self-Control Depletion + No Nicotine Deprivation (n = 32) |
No Self-Control Depletion + Nicotine Deprivation (n = 32) |
Self-Control Depletion + Nicotine Deprivation (n = 32) |
Total (N = 128) |
|
|---|---|---|---|---|---|
|
|
|||||
| Demographics | |||||
| Age | 38.94 (12.39) | 38.16 (12.56) | 33.72 (11.90) | 35.09 (11.05) | 36.48 (12.04) |
| Gender (% Female) |
50% | 50% | 50% | 53% | 51% |
| Race (% Caucasian) |
78% | 84% | 78% | 59% | 75% |
| Ethnicity (% Hispanic) |
9% | 9% | 16% | 9% | 11% |
| Education (% College degree) |
13% | 0% | 6% | 3% | 6% |
| Income (% > $20,000) |
38% | 38% | 34% | 41% | 38% |
| Smoking History | |||||
| Cigarettes per day | 20.33 (5.05) | 21.41 (6.29) | 19.91 (5.88) | 19.97 (9.58) | 20.40 (6.86) |
| FTND* | 5.78 (1.81) | 6.25 (1.87) | 5.50 (1.88) | 5.22 (1.84) | 5.69 (1.87) |
| Motivation to Quit | 5.34 (2.56) | 4.44 (2.33) | 4.66 (2.89) | 4.22 (2.52) | 4.66 (2.89) |
| Self-efficacy* | .58 (.81) | .74 (.65) | .98 (1.20) | 1.28 (1.20) | .90 (1.02) |
Note: indicates significant difference between the nicotine deprivation and no nicotine deprivation conditions, p < .05.
FTND = Fagerström Test for Nicotine Dependence.
As expected, no significant differences were found across the experimental conditions for most baseline characteristics. However, those in the deprivation condition were less nicotine dependent [(M = 5.36; SD = 1.85) vs. (M = 6.02; SD = 1.84), F(1, 124) = 4.02, p =.047, η2p = .03], and reported greater self-efficacy [(M = 1.13; SD = 1.20) vs. (M = .66; SD = .74), F(1, 124) = 7.10, p = .01, η2p = .05)]. As presented in Table 2, significant correlations were observed between several of the outcomes assessed after both experimental manipulations, and baseline scores of nicotine dependence and motivation to quit. All three baseline covariates were included in subsequent analyses. Gender was also tested as a potential covariate, but it was dropped from final models for parsimony because it was not a significant predictor and did not influence experimental effects.
Table 2.
Correlations between covariates, putative mediators, and primary outcomes.
| Baseline Assessments | Post Experimental Manipulations Assessments | |||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Sample | (1) | (2) | (3) | (4) | (5) | (6) | (7) | |
|
|
||||||||
| Full Sample | (1) FTND | - | ||||||
| (2) Motivation to Quit | −.20 * | - | ||||||
| (3) Self-efficacy | −.24 ** | .15 | - | |||||
| (4) Craving | .33 ** | −.23 ** | −.15 | - | ||||
| (5) Discounting | .13 | .05 | −.04 | .06 | - | |||
| (6) Demand | .20 * | −.22 * | −.13 | .33 * | −.01 | - | ||
| (7) Latency to Smoke | .07 | .01 | .11 | −.25 ** | −.02 | −.03 | - | |
| (8) # Cigarettes Smoked | .04 | −.25 ** | −.14 | .14 | .01 | .24 * | .05 | |
|
| ||||||||
|
No SCD &
No Deprivation |
(1) FTND | - | ||||||
| (2) Motivation to Quit | −.13 | - | ||||||
| (3) Self-efficacy | −.47 ** | −.16 | - | |||||
| (4) Craving | .44 * | −.35 * | −.19 | - | ||||
| (5) Discounting | .22 | .02 | −.21 | .09 | - | |||
| (6) Demand | .08 | −.02 | .16 | −.07 | −.26 | - | ||
| (7) Latency to Smoke | −.07 | −.11 | −.16 | −.36 | .16 | .07 | - | |
| (8) # Cigarettes Smoked | −.13 | −.27 | .18 | .05 | .28 | −.01 | .07 | |
|
| ||||||||
|
SCD &
No Deprivation |
(1) FTND | - | ||||||
| (2) Motivation to Quit | −.23 | - | ||||||
| (3) Self-efficacy | .10 | .09 | - | |||||
| (4) Craving | .29 | −.17 | .01 | - | ||||
| (5) Discounting | −.11 | .18 | .30 | −.14 | - | |||
| (6) Demand | −.13 | −.37 * | −.11 | .33 | .14 | - | ||
| (7) Latency to Smoke | .05 | .11 | .08 | −.23 | .28 | −.06 | - | |
| (8) # Cigarettes Smoked | .05 | −.10 | −.26 | .44 * | −.26 | .39 * | −.05 | |
|
| ||||||||
|
No SCD &
Deprivation |
(1) FTND | - | ||||||
| (2) Motivation to Quit | −.14 | - | ||||||
| (3) Self-efficacy | −.25 | .17 | - | |||||
| (4) Craving | .49 ** | −.18 | −.11 | - | ||||
| (5) Discounting | −.06 | .24 | −.07 | −.05 | - | |||
| (6) Demand | .50 ** | −.29 | −.31 | .39 * | −.14 | - | ||
| (7) Latency to Smoke | −.04 | −.18 | .20 | −.24 | −.21 | −.05 | - | |
| (8) # Cigarettes Smoked | .09 | −.25 | −.22 | .07 | −.04 | .15 | .12 | |
|
| ||||||||
|
SCD &
Deprivation |
(1) FTND | - | ||||||
| (2) Motivation to Quit | −.36 * | - | ||||||
| (3) Self-efficacy | −.18 | .51 ** | - | |||||
| (4) Craving | .40 * | −.18 | −.47 ** | - | ||||
| (5) Discounting | .52 ** | −.16 | −.14 | .19 | - | |||
| (6) Demand | .32 | −.24 | −.20 | .45 ** | .09 | - | ||
| (7) Latency to Smoke | .19 | .03 | .36 * | −.22 | −.04 | .00 | - | |
| (8) # Cigarettes Smoked | .113 | −.41 * | −.14 | −.03 | .12 | .35 | .15 | |
Notes: p <.05,
p < .01; FTND = Fagerström Test for Nicotine Dependence; SCD = self-control depletion
Full Sample: n = 123 for all latency to smoke analyses, n = 120 for all # cigarettes smoked analyses, and N = 128 for all other correlations.
No SCD & No Deprivation: n = 28 for all latency to smoke analyses, n = 28 for all # cigarettes smoked analyses, and n = 32 for all others.
SCD & No Deprivation: n = 31 for all latency to smoke analyses, n = 30 for all # cigarettes smoked analyses, and n = 32 for all others.
No SCD & Deprivation: n = 32 for all analyses.
SCD & Deprivation: n = 31 for all latency to smoke analyses, n = 30 for all # cigarettes smoked analyses, and n = 32 for all others.
Nicotine Deprivation Manipulation Check
On average, those in the deprivation condition reported 830 minutes (SD = 93.50) of abstinence prior to completing baseline measures, and approximately nine minutes (SD = 6.93) had passed since those in the non-deprived condition had smoked. As expected, those in the nicotine deprivation conditions had lower CO levels (M = 5.25; SE = 1.88), relative to the satiated groups (M = 39.07; SE = 1.88), F(1, 121) = 154.18, p < .001, η2p = .56. Nicotine deprived participants also had higher self-reported nicotine withdrawal (M = 2.37; SE = .11), compared to those non-deprived (M = 1.83; SE = .11), F(1, 121) = 12.19, p = .001, η2p = .09.
SCD Manipulation Check
Those randomized to SCD conditions reported engaging in higher levels of emotional suppression (M = 4.43; SE = .15), compared to those in the no SCD conditions (M = 1.14; SE = .15), F(1, 121) = 224.84, p < .001, η2p = .65. Participants in the SCD conditions (M = 1.78; SE = .16) also reported that following the assigned instruction set led to more cognitive depletion compared to those asked to act naturally (M = .61; SE = .16), F(1, 121) = 27.22, p < .001, η2p = .18. No differences were observed for negative affect (p = .34) or positive affect (p = .62). Glucose levels were equivalent at baseline (SCD: M = 108.47; SD = 28.81; no SCD: M = 104.90; SD = 15.45; p = .48) and post-depletion (SCD: M = 105.86; SD = 28.04; no SCD: M = 103.41; SD = 13.11; p = .66). With respect to glucose utilization (i.e., change in glucose), only 59% complied with the pre-session dietary restriction instructions, which may have precluded the ability to detect depletion effects within the full sample (SCD: M = −2.78; SE = 1.09; no SCD: M = −1.86; SE = 1.08; p = .56). The subsample that complied with the two hour dietary restriction showed the expected pattern of greater glucose utilization (i.e., decreased blood glucose levels after the SCD manipulation) in the SCD condition (M = −2.54; SE = 1.25), relative to no SCD participants (M = .85; SE = 1.39), which approached traditional levels of statistical significance despite reduced power, F(1, 70) = 3.22, p = .08, η2p = .04.
Putative Mediator Screening
Craving (N = 128)
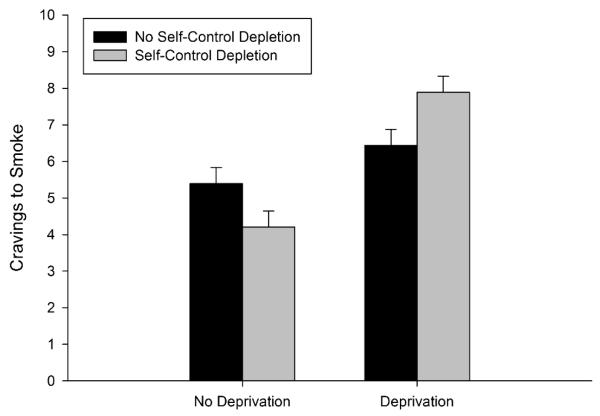
A main effect was observed for the deprivation manipulation [F(1, 121) = 13.71, p < .001, η2p = .10], but not for the SCD manipulation (p = .84). As depicted in Figure 2, these manipulations interacted significantly, F(1, 121) = 4.64, p = .03, η2p = .04. This suggested that SCD depletion only increased self-reported craving when participants were in a state of nicotine deprivation. Although follow up comparisons were not significant, differential effect sizes were observed for SCD when participants were deprived [F(1, 59) = 39.12, p = .06, η2p = .06, d = .46], relative to satiated [F(1, 59) = 27.67, p = .15, η2p = .04, d = −.35]. Furthermore, when tested against the complete control condition (no SCD + no deprivation), there was no effect of SCD (SCD + no deprivation, p = .18) or deprivation (no SCD + deprivation, p = .23) alone. Instead, these manipulations appeared to affect craving only when combined (SCD + deprivation, p = .007).
Figure 2.
Mean composite craving ratings (and standard errors), as a function of the Self-Control Depletion manipulation × Nicotine Deprivation manipulation interaction (p = .03).
Delayed Reward Discounting (N = 128)
A significant main effect was due to the deprivation manipulation, F(1, 121) = 4.00, p = .048, η2p = .03. No significant effects were observed for the SCD manipulation (p = .77) or interaction between experimental manipulations (p = .50). A medium effect size was observed for the PCA derived discounting index (d = .36) such that those deprived of nicotine discounted rewards to a greater degree than satiated participants (M = .03; SE = .13 vs. M = −.03; SE = .13).
Demand (N = 128)
The only significant main effect was again a function of the deprivation manipulation, F(1, 121) = 4.21, p = .04, η2p = .03. No significant effects were observed for the SCD manipulation (p = .94), or the interaction between SCD and nicotine deprivation manipulations (p = .12). Those deprived of nicotine had greater demand for cigarettes (M = .09; SE = .01), compared to those not deprived (M = .06; SE = .01). This was a medium effect size (d = .35).
Primary Analyses
Lapse (n = 123)/Relapse (n = 120) Behavior
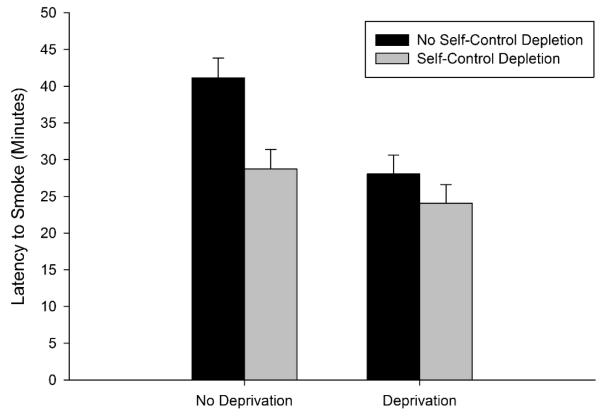
As depicted in Figure 3, main effects were observed for both the SCD [F(1, 116) = 5.03, p = .03, η2p = .04] and deprivation manipulations [F(1, 116) = 5.42, p = .03, η2p = .04] on latency to smoke. Medium effect sizes were observed for both experimental manipulations (d = .41), and the interaction was not significant (p = .24). Neither manipulation influenced cigarette consumption (p’s > .45). That is, SCD and nicotine deprivation increased lapse behavior (i.e., decreased latency to smoke), but had negligible effects on relapse behavior (i.e., number of cigarettes smoked), within this laboratory analogue task.
Figure 3.
Latency to smoke (and standard errors), as a function of the Self-Control Depletion (p = .03) × Nicotine Deprivation manipulations (p = .03).
Moderated Mediation Analyses for Lapse Behavior (n = 123)
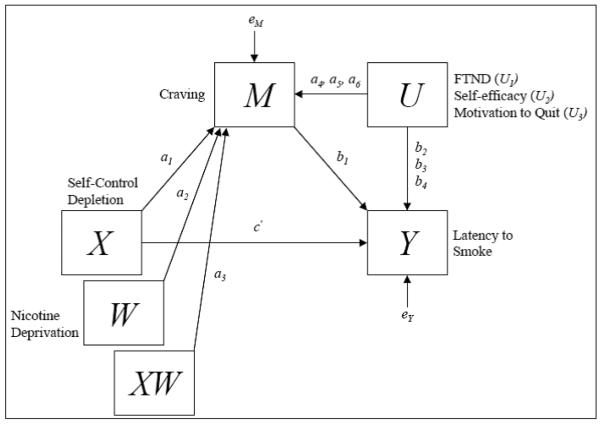
Craving was the only putative mediator found significant at the univariate level for the SCD manipulation, and this was moderated by the nicotine deprivation manipulation. The SCD manipulation also influenced latency to smoke, but this was not moderated by nicotine deprivation. These initial results suggested PROCESS model 7 was the most appropriate moderated mediation model of SCD on latency to smoke. Craving was specified as the sole mediator and deprivation status was included as a moderator for the effects of SCD on craving (a path). Figure 4 depicts the statistical model based on PROCESS model 7, with results shown in Table 3. Consistent with ANCOVA results described above, there was a direct effect of the SCD manipulation on latency to smoke (point estimate = −7.35; 95% CI = −14.41 to −.28). Conditional effects indicate mediation was observed among deprived participants (indirect point estimate = −2.37; 95% CI = −6.01 to −.12), but not in those non-deprived (indirect point estimate = 2.22; 95% CI = −.49 to 6.12). The test for moderated mediation was statistically significant (index of moderated mediation = −4.59; 95% CI = −10.36 to −.74). Additional moderated mediation analyses were conducted to explore the robustness of these effects. The moderated mediation index for craving remained statistically significant (index of moderated mediation = −4.77; 95% CI = −10.72 to −.89) when delayed reward discounting and demand were also included as mediators. Neither discounting (index of moderated mediation = −.07; 95% CI = −1.10 to 2.43) nor demand (index of moderated mediation = .52; 95% CI = −1.04 to 4.08) acted as mediators. A similar pattern of results was observed when moderated mediation analyses were run with PROCESS models 8 (moderation of a and c’ paths) and 59 (moderation of a, b, and c’ paths). In summary, the moderated mediation index for craving was statistically significant across all models, regardless of the number of mediators included or number of paths influenced by the moderator (i.e., deprivation). That is, increases in craving due to the SCD manipulation led to decreased latency to smoke, but only among participants in acute nicotine withdrawal.
Figure 4.
Moderated mediation statistical model.
Note: FTND = Fagerström Test for Nicotine Dependence.
Table 3.
Moderated mediation results via PROCESS (model 7)
| Unstandardized OLS Regression Coefficients With Confidence Intervals (Standard Errors in Parentheses) Estimating Craving and Latency to Smoke | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Craving (M) |
Latency to Smoke (Y) |
|||||||||
| Coeff. | 95% CI | Coeff. | 95% CI | |||||||
| Self-Control Depletion (X) | a1 → | −1.36 | (.92) | −3.18 | .45 | c′ → | −7.35* | (3.57) | −14.41 | −.28 |
| Craving (M) | b1 → | −1.63** | (.49) | −2.60 | −.67 | |||||
| Nicotine Deprivation (W) | a2 → | .73 | (.92) | −1.10 | 2.56 | |||||
| Interaction (X × W) | a3 → | 2.82* | (1.25) | .34 | 5.29 | |||||
| FTND (U1) | a4 → | .70*** | (.18) | .35 | 1.06 | b2 → | 1.93 | (1.02) | −.86 | 3.94 |
| Self-efficacy (U2) | a5 → | −.53 | (.34) | −1.21 | .15 | b3 → | 2.95 | (1.86) | −.73 | 6.62 |
| Motivation to Quit (U3) | a6 → | −.19 | (.13) | −.45 | .07 | b4 → | −.74 | (.72) | −2.17 | .69 |
| Constant | iM → | 3.07* | (1.55) | .01 | 6.13 | iY → | 33.75*** | (8.05) | 17.81 | 49.68 |
| R2 = .25 | R2 = .13 | |||||||||
| F(6,116) = 6.26, p < .001 | F(5,117) = 3.62, p = .004 | |||||||||
Note: p <.05,
p < .01,
p < .001
FTND = Fagerström Test for Nicotine Dependence.
Discussion
This is the first study, to our knowledge, to reveal that SCD may increase cravings to smoke, but these effects were only observed among smokers deprived of nicotine. Furthermore, this effect mediated the observed increase in lapse behavior resultant from SCD during acute nicotine withdrawal. Importantly, results provide causal evidence to suggest that SCD may increase motivation to smoke, as measured by self-reported craving and latency to smoke in a validated lapse analogue task. The medium effect sizes observed indicate SCD warrants consideration as a novel precipitant for cessation failure, particularly through its effects on the cessation milestone of time to lapse. However, SCD did not influence the proposed behavioral economic mediators of delayed reward discounting and demand.
The validity of this conclusion is bolstered by the high degree of replication observed for nicotine deprivation effects across the various laboratory models of nicotine dependence tested here. Consistent with past research, we found acute abstinence to increase discounting, demand, craving, and cessation failure as indexed by latency to smoke (i.e., lapse). The inclusion of deprivation in the experimental design also improved external validity. Whereas prior studies only included non-deprived smokers, the current study was the first to test SCD effects on smoking in the context of a simulated quit attempt when motives to smoke are pitted against motives for abstinence.
Theoretical Implications
Interestingly, craving was not influenced by the SCD manipulation among satiated smokers, yet lapse behavior was. Thus, fluctuations of self-control resources may drive smoking behavior, but this may occur outside of awareness when free of nicotine withdrawal. In light of evidence that smoking can restore depleted self-control (Heckman et al., 2012), smoking may be viewed as an automatic form of self-regulation that does not require deliberate control (Tiffany, 1990). Frequent smoking may prevent SCD, thereby alleviating any subjective awareness for the need to smoke, which parallels negative reinforcement models of addiction that posit consistent smoking may prevent negative affect from reaching consciousness (Baker, Piper, McCarthy, Majeskie, & Fiore, 2004). However, when self-control resources are progressively taxed through competing demands, the need for self-control restoration may manifest through goal-directed conscious processes such as craving. Resources are likely to be greatly compromised during a quit attempt when smokers must cope with nicotine withdrawal (Baker et al., 2006; Bernstein et al., 2008). Thus, self-control strength may influence the act of smoking, but the extent to which SCD influences subjective motivational processes may depend on the magnitude of SCD, based on factors such as nicotine deprivation or negative affect (Heckman et al., 2015; Heckman et al., 2013).
Although both experimental manipulations increased lapse behavior, they differentially impacted behavioral economic indices (i.e., discounting and demand). Results indicate impulsivity may very well be a valid symptom of nicotine withdrawal (Hughes, Dash, & Callas, 2015). That SCD did not affect impulsive decision making suggests that these two specific measures of self-control and impulsivity may not serve as antipodes on a self-control/impulsivity continuum (Bickel, Jarmolowicz, Mueller, Gatchalian, & McClure, 2012), as suggested by proponents of the Self-Control Strength Model (Tice et al., 2001). Findings are, in part, consistent with Inzlicht and colleagues (2012) motivational control account of SCD effects. Namely, our sample was more likely to act on impulse (i.e., give in to cravings/smoke) following the SCD task. Future studies could include measures to examine other processes proposed to explain SCD effects, including: a) decreased motivation to engage in self-control (e.g., avoidance motivation for smoking), b) reduced attention to cues supporting self-control, and c) increased attention to rewarding cues. Assessments of perception (e.g., time or level of SCD), as well as other cognitive biases, previously found to be influenced by SCD and craving may also help understand mechanisms (Clarkson, Hirt, Jia, & Alexander, 2010; Sayette, 2016; Vohs & Schmeichel, 2003). Future studies may also consider assessing delayed reward discounting for other commodities, such as cigarettes. Additionally, characterization of biological mechanisms through which SCD acts would address a major shortcoming of the Self-Control Strength Model (Inzlicht et al., 2014; Robinson, Schmeichel, & Inzlicht, 2010), as neurobiological correlates have yet to be identified.
Considerations & Future Directions
Several limitations are worth noting. The current study may be susceptible to Type I error given no formal correction of statistical significance. However, detection of novel cessation failure precipitants/processes is of high importance to guide future research and treatment development so we considered it prudent not to diminish capacity to detect potential signals due to formal correction of statistical significance (i.e., increase Type II error). Furthermore, we used an informed moderated mediation modeling building strategy in which candidate mediators were first screened in a modest number of preliminary analyses that included tests of replication for nicotine deprivation effects. The moderated mediation model tested was different than we had anticipated, and future research should replicate our findings. Second, given that those deprived were required to sustain 12 hours of abstinence, then those more dependent or unable to quit for 12 hours may have been underrepresented in the deprivation conditions. This may be reflected by the larger number of participants in the deprivation, compared to non-deprived, conditions unable to meet CO requirements (28 vs. 4). Prior studies have found craving, demand, and relapse are positively associated with nicotine dependence, which suggests that our findings may underestimate effect sizes observed across deprivation analyses. This was controlled for statistically in the current study, but future studies may mitigate this concern through within-subject designs. Our sample of 15+ CPD smokers reflect the majority of current smokers (CDCP, 2015), but future studies could explore whether the pattern of findings extend to those who smoke less frequently. Population trends indicate shifts towards less frequent smoking, for whom nicotine dependence/cessation failure may be qualitatively different. Finally, interpretation of study findings should, of course, be tempered by the extent to which the laboratory tasks model naturalistic cessation failure. Although we selected assessments that have previously been found to predict cessation failure and detect relapse precipitants found in treatment outcome studies, our sample consisted of smokers not attempting to quit. Thus, our approach traded off external validity to provide the most stringent and internally valid test of whether, and through what mechanisms, SCD may serve as an antecedent to cessation failure. Future studies should examine the extent to which our findings generalize to treatment seeking smokers and those actively quitting. Inclusion of highly motivated samples enhances the validity of brief medication screening studies (Perkins et al., 2008), and would likely to the same for relapse risk detection studies. We would expect SCD to promote lapse/relapse among those trying to quit, and motivation to quit may help counteract SCD effects. An important need remains to determine the predictive validity of the smoking lapse/relapse analogue task on relapse rates. Yet several areas of research suggest our findings are nonetheless relevant to cessation processes: quit attempts often occur in non-treatment seeking smokers reporting low motivation to quit (Burris, Heckman, Mathew, & Carpenter, 2014; Carpenter, Alberg, Gray, & Saladin, 2010), motivation to quit and quitting are dynamic processes that change rapidly (Hughes et al., 2014), and as indicated by a systematic review of population-based samples (N = 29,916) demographic factors do not reliably differentiate those whom make a quit attempt (Vangeli, Stapleton, Smit, Borland, & West, 2011).
A logical next step would be to test SCD effects in the real world among individuals engaged in quit attempts, which could be accomplished using ecological momentary assessment (Hofmann, Baumeister, Forster, & Vohs, 2012). Using this methodology, self-control demands have been found to predict alcohol consumption (Muraven, Collins, Shiffman, & Paty, 2005). Although studies have tested the effects of resisting temptations to smoke on cessation failure (O’Connell, Schwartz, & Shiffman, 2008), the role of self-control demands non-specific to substance use have yet to be tested. This approach may be particularly informative to emerging literatures on cessation fatigue and treatment fatigue, described as the processes with which those attempting to quit become tired due to coping demands associated with quitting and treatment engagement (Liu, Li, Lanza, Vasilenko, & Piper, 2013; Piasecki, Fiore, McCarthy, & Baker, 2002; Piper, 2015; Heckman, Mathew, & Carpenter, 2015).
Treatment Implications
Although resisting cravings has been found to deplete self-control resources (Hagger et al., 2013; Muraven & Shmueli, 2006), SCD effects are also observed across affective and cognitive manipulations devoid of drug cues/craving (Hagger et al., 2010). That is, self-control strength is theorized to be a domain-independent process, and subject to fatigue from a variety of sources (Baumeister et al., 2007). Even among those who consider performance decrements on repeated tasks of self-control as reflecting motivational and attentional processes rather than limited resources (Inzlicht & Schmeichel, 2012), it is still recognized that self-control failure is more likely to occur following self-control exertion. In light of the current study findings that suggest SCD may undermine smoking cessation, treatment approaches may benefit from a broader conceptualization of relapse risk. For example, a wide range of demands that draw upon self-control could potentially accumulate and impede successful cessation if left unaddressed. Fortunately, the self-control strength literature has identified several strategies that can counteract state dependent fluctuations of self-control strength (or motivation to exert self-control) and, therefore, may serve as viable alternatives to smoking.
Many preventive techniques can be taught pre-cessation and mirror traditional cognitive approaches, including implementation intentions (Webb & Sheeran, 2002), self-awareness (Alberts, Martijn, & de Vries, 2011), mindfulness meditation (Friese, Messner, & Schaffner, 2012), and self-affirmation (Schmeichel & Vohs, 2009). Behavioral methods can also be employed directly after SCD tasks, and they parallel contingency management interventions in that they provide rewards, such as positive mood induction (Tice, Baumeister, Shmueli, & Muraven, 2007), relaxation (Tyler & Burns, 2008), glucose administration, and monetary and social contingencies (Muraven & Slessareva, 2003). What remains unclear is whether these strategies directly restore self-control resources, enhance motivation to use remaining self-control reserves, or act through other mechanisms (Inzlicht et al., 2014; Kurzban et al., 2013), but all have been found to nullify SCD effects within non-smokers. That these strategies are similar to cognitive-behavioral smoking cessation interventions (Perkins, Conklin, & Levine, 2008) suggests strong potential for dissemination and implementation, should they be found effective within samples of smokers (Shmueli & Prochaska, 2012). An important distinction, however, is that the specific target of these strategies would be SCD, rather than smoking per se. Thus, this line of research could inform the literature on mechanisms of effective treatment approaches, as well as mechanisms of treatment failure (Heckman, Mathew, & Carpenter, 2015).
The number and potential reach of self-control strength interventions is promising, yet only one study has applied self-control theory with respect to smoking cessation (Muraven, 2010). Rather than focusing on strategies to “restore” self-control, the intervention focused on pre-cessation self-control ‘strength training.’ Smokers were instructed to engage in repeated acts of posture checking over two weeks, which led to increased abstinence duration. No study has tested the utility of combining trait and state self-control interventions, or more than one state intervention simultaneously. The laboratory paradigm employed here could be used to screen self-control interventions prior to full scale clinical trials, just as it has been used for pharmacotherapy screening (McKee et al., 2010). Identification of pragmatic and effective self-control interventions may provide benefits beyond smoking cessation, as numerous behavioral and impulse-control problems have been linked to self-control failure, including: overeating, alcohol and drug abuse, crime and violence, overspending, sexually impulsive behavior, and gambling (Baumeister, Heatherton, & Tice, 1994).
Conclusion
This experimental study reveals that SCD interacts with nicotine deprivation to impact motivation to smoke, and may serve as a novel antecedent to smoking lapse in a laboratory model. We also found that this effect may occur outside of awareness among minimally deprived smokers, serving as an automatic form of self-regulation. Among nicotine-deprived smokers (simulating a quit attempt) craving mediates the relationship between SCD and cessation failure. Thus, the current study suggests that SCD is involved in the maintenance of nicotine dependence, and provides a theoretical framework for its influence.
Acknowledgments
Funding for this research was provided by National Institute on Drug Abuse grant F31 DA033058 (BWH) and K12 DA031794 (BWH). James MacKillop is the holder of the Peter Boris Chair in Addictions Research, which partially support his role. Preparation of this report was supported in part by R01 DA034755 (WKB).
Footnotes
Public Health Significance: This study suggests self-control depletion precipitates smoking relapse. Interventions targeting this novel risk factor may help reduce relapse rates.
References
- Acker J, MacKillop J. Behavioral economic analysis of cue-elicited craving for tobacco: a virtual reality study. Nicotine & Tobacco Research. 2013;15:1409–1416. doi: 10.1093/ntr/nts341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alberts HJEM, Martijn C, de Vries NK. Fighting self-control failure: Overcoming ego depletion by increasing self-awareness. Journal of Experimental Social Psychology. 2011;47:58–62. [Google Scholar]
- Amlung M, Yurasek A, McCarty KN, MacKillop J, Murphy JG. Area under the curve as a novel metric of behavioral economic demand for alcohol. Exp Clin Psychopharmacol. 2015;23:168–175. doi: 10.1037/pha0000014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anokhin AP, Golosheykin S, Mulligan RC. Long-term test-retest reliability of delayed reward discounting in adolescents. Behav Processes. 2015;111:55–59. doi: 10.1016/j.beproc.2014.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashare RL, Falcone M, Lerman C. Cognitive function during nicotine withdrawal: Implications for nicotine dependence treatment. Neuropharmacology. 2014;76:581–591. doi: 10.1016/j.neuropharm.2013.04.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashare RL, Hawk LW., Jr. Effects of smoking abstinence on impulsive behavior among smokers high and low in ADHD-like symptoms. Psychopharmacology (Berl) 2012;219:537–547. doi: 10.1007/s00213-011-2324-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker TB, Japuntich SJ, Hogle JM, McCarthy DE, Curtin JJ. Pharmacologic and behavioral withdrawal from addictive drugs. Current Directions in Psychological Science. 2006;15:232–236. [Google Scholar]
- Baker TB, Piper ME, McCarthy DE, Majeskie MR, Fiore MC. Addiction motivation reformulated: an affective processing model of negative reinforcement. Psychol Rev. 2004;111:33–51. doi: 10.1037/0033-295X.111.1.33. [DOI] [PubMed] [Google Scholar]
- Baumeister RF, Bratslavsky E, Muraven M, Tice DM. Ego depletion: Is the active self a limited resource? Journal of Personality and Social Psychology. 1998;74:1252–1265. doi: 10.1037//0022-3514.74.5.1252. [DOI] [PubMed] [Google Scholar]
- Baumeister RF, Heatherton TF, Tice DM. Losing control: How and why people fail at self-regulation. Academic Press; San Diego, CA US: 1994. [Google Scholar]
- Baumeister RF, Vohs KD, Tice DM. The strength model of self-control. Current Directions in Psychological Science. 2007;16:351–355. [Google Scholar]
- Baumeister RF, Vonasch AJ. Uses of self-regulation to facilitate and restrain addictive behavior. Addict Behav. 2015;44:3–8. doi: 10.1016/j.addbeh.2014.09.011. [DOI] [PubMed] [Google Scholar]
- Beedie CJ, Lane AM. The role of glucose in self-control: another look at the evidence and an alternative conceptualization. Personality and Social Psychology Review. 2012;16:143–153. doi: 10.1177/1088868311419817. [DOI] [PubMed] [Google Scholar]
- Bernstein A, Trafton J, Ilgen M, Zvolensky MJ. An evaluation of the role of smoking context on a biobehavioral index of distress tolerance. Addict Behav. 2008;33:1409–1415. doi: 10.1016/j.addbeh.2008.06.003. [DOI] [PubMed] [Google Scholar]
- Bickel WK, Jarmolowicz DP, Mueller ET, Gatchalian KM, McClure SM. Are executive function and impulsivity antipodes? A conceptual reconstruction with special reference to addiction. Psychopharmacology (Berl) 2012;221:361–387. doi: 10.1007/s00213-012-2689-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bickel WK, Johnson MW, Koffarnus MN, MacKillop J, Murphy JG. The Behavioral Economics of Substance Use Disorders: Reinforcement Pathologies and Their Repair. Annu Rev Clin Psychol. 2014;10:641–677. doi: 10.1146/annurev-clinpsy-032813-153724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bickel WK, Koffarnus MN, Moody L, Wilson AG. The behavioral- and neuro-economic process of temporal discounting: A candidate behavioral marker of addiction. Neuropharmacology. 2014;76(Pt B):518–527. doi: 10.1016/j.neuropharm.2013.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bickel WK, Pitcock JA, Yi R, Angtuaco EJ. Congruence of BOLD response across intertemporal choice conditions: fictive and real money gains and losses. The Journal of Neuroscience. 2009;29:8839–8846. doi: 10.1523/JNEUROSCI.5319-08.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bidwell LC, MacKillop J, Murphy JG, Tidey JW, Colby SM. Latent factor structure of a behavioral economic cigarette demand curve in adolescent smokers. Addict Behav. 2012;37:1257–1263. doi: 10.1016/j.addbeh.2012.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biener L, Abrams DB. The Contemplation Ladder: Validation of a measure of readiness to consider smoking cessation. Health Psychology. 1991;10:360–365. doi: 10.1037//0278-6133.10.5.360. [DOI] [PubMed] [Google Scholar]
- Brandon TH, Tiffany ST, Obremski KM, Baker TB. Postcessation cigarette use: the process of relapse. Addictive Behaviors. 1990;15:105–114. doi: 10.1016/0306-4603(90)90013-n. [DOI] [PubMed] [Google Scholar]
- Burris JL, Heckman BW, Mathew AR, Carpenter MJ. A mechanistic test of nicotine replacement therapy sampling for smoking cessation induction. Psychol Addict Behav. 2014 doi: 10.1037/adb0000035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carpenter MJ, Alberg AJ, Gray KM, Saladin ME. Motivating the unmotivated for health behavior change: a randomized trial of cessation induction for smokers. Clin Trials. 2010;7:157–166. doi: 10.1177/1740774510361533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter EC, Kofler LM, Forster DE, McCullough ME. A series of meta-analytic tests of the depletion effect: Self-control does not seem to rely on a limited resource. J Exp Psychol Gen. 2015;144:796–815. doi: 10.1037/xge0000083. [DOI] [PubMed] [Google Scholar]
- Carter EC, McCullough ME. Is ego depletion too incredible? Evidence for the overestimation of the depletion effect. Behav Brain Sci. 2013;36:683–684. doi: 10.1017/S0140525X13000952. discussion 707-626. [DOI] [PubMed] [Google Scholar]
- Carter EC, McCullough ME. Publication bias and the limited strength model of self-control: has the evidence for ego depletion been overestimated? Front Psychol. 2014;5:823. doi: 10.3389/fpsyg.2014.00823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarkson JJ, Hirt ER, Jia L, Alexander MB. When perception is more than reality: the effects of perceived versus actual resource depletion on self-regulatory behavior. J Pers Soc Psychol. 2010;98:29–46. doi: 10.1037/a0017539. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention Quitting smoking among adults--United States, 2001-2010. Morbidity and Mortality Weekly Report. 2011;60:1513–1519. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention Current Cigarette Smoking Among Adults--United States, 2005-2014. Morbidity and Mortality Weekly Report. 2015;64:1233–1240. doi: 10.15585/mmwr.mm6444a2. [DOI] [PubMed] [Google Scholar]
- Diener E, Emmons RA. The independence of positive and negative affect. J Pers Soc Psychol. 1984;47:1105–1117. doi: 10.1037//0022-3514.47.5.1105. [DOI] [PubMed] [Google Scholar]
- Field M, Santarcangelo M, Sumnall H, Goudie A, Cole J. Delay discounting and the behavioural economics of cigarette purchases in smokers: the effects of nicotine deprivation. Psychopharmacology. 2006;186:255–263. doi: 10.1007/s00213-006-0385-4. [DOI] [PubMed] [Google Scholar]
- Friese M, Messner C, Schaffner Y. Mindfulness meditation counteracts self-control depletion. Conscious Cogn. 2012;21:1016–1022. doi: 10.1016/j.concog.2012.01.008. [DOI] [PubMed] [Google Scholar]
- Gailliot MT, Baumeister RF, DeWall CN, Maner JK, Plant EA, Tice DM, Schmeichel BJ. Self-control relies on glucose as a limited energy source: Willpower is more than a metaphor. Journal of Personality and Social Psychology. 2007;92:325–336. doi: 10.1037/0022-3514.92.2.325. [DOI] [PubMed] [Google Scholar]
- Gross JJ. Antecedent- and response-focused emotion regulation: divergent consequences for experience, expression, and physiology. J Pers Soc Psychol. 1998;74:224–237. doi: 10.1037//0022-3514.74.1.224. [DOI] [PubMed] [Google Scholar]
- Gross JJ, Levenson RW. Emotional suppression: Physiology, self-report, and expressive behavior. Journal of Personality and Social Psychology. 1993;64:970–986. doi: 10.1037//0022-3514.64.6.970. [DOI] [PubMed] [Google Scholar]
- Gross JJ, Richards JM, John OP, Snyder DK, Simpson J, Hughes JN. Emotion regulation in couples and families: Pathways to dysfunction and health. American Psychological Association; Washington, DC US: 2006. Emotion Regulation in Everyday Life; pp. 13–35. [Google Scholar]
- Hagger MS, Chatzisarantis NLD, Alberts H, Anggono CO, Batailler C, Birt A, Zwienenberg M. A multi-lab pre-registered replication of the ego depletion effect. Perspectives on Psychological Science. doi: 10.1177/1745691616652873. (in press) [DOI] [PubMed] [Google Scholar]
- Hagger MS, Leaver E, Esser K, Leung CM, Te Pas N, Keatley DA, Chatzisarantis NL. Cue-induced smoking urges deplete cigarette smokers’ self-control resources. Annals of Behavioral Medicine. 2013;46:394–400. doi: 10.1007/s12160-013-9520-8. [DOI] [PubMed] [Google Scholar]
- Hagger MS, Wood C, Stiff C, Chatzisarantis NL. Ego depletion and the strength model of self-control: a meta-analysis. Psychol Bull. 2010;136:495–525. doi: 10.1037/a0019486. [DOI] [PubMed] [Google Scholar]
- Hayes AF. An index and test of linear moderated mediation. Multivariate Behavioral Research. 2015;50:1–22. doi: 10.1080/00273171.2014.962683. [DOI] [PubMed] [Google Scholar]
- Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. Guilford Press; New York, NY: 2013. [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC, Fagerstrom KO. The Fagerstrom test for nicotine dependence: A revision of the Fagerstrom tolerance questionnaire. Br J Addict. 1991;86:1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- Heckman BW, Carpenter MJ, Correa JB, Wray JM, Saladin ME, Froeliger B, Brandon TH. Effects of experimental negative affect manipulations on ad libitum smoking: a meta-analysis. Addiction. 2015;110:751–760. doi: 10.1111/add.12866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heckman BW, Ditre JW, Brandon TH. The restorative effects of smoking upon self-control resources: A negative reinforcement pathway. J Abnorm Psychol. 2012;121:244–249. doi: 10.1037/a0023032. [DOI] [PubMed] [Google Scholar]
- Heckman BW, Kovacs MA, Marquinez NS, Meltzer LR, Tsambarlis ME, Drobes DJ, Brandon TH. Influence of affective manipulations on cigarette craving: A meta-analysis. Addiction. 2013;108:2068–2078. doi: 10.1111/add.12284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heckman BW, Mathew AR, Carpenter MJ. Treatment Burden and Treatment Fatigue as Barriers to Health. Current Opinions in Psychology. 2015;5:31–36. doi: 10.1016/j.copsyc.2015.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heishman SJ, Singleton EG, Pickworth WB. Reliability and validity of a Short Form of the Tobacco Craving Questionnaire. Nicotine Tob Res. 2008;10:643–651. doi: 10.1080/14622200801908174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendricks PS, Ditre JW, Drobes DJ, Brandon TH. The early time course of smoking withdrawal effects. Psychopharmacology. 2006;187:385–396. doi: 10.1007/s00213-006-0429-9. [DOI] [PubMed] [Google Scholar]
- Hofmann W, Baumeister RF, Forster G, Vohs KD. Everyday temptations: an experience sampling study of desire, conflict, and self-control. Journal of Personality and Social Psychology. 2012;102:1318–1335. doi: 10.1037/a0026545. [DOI] [PubMed] [Google Scholar]
- Hughes JR. Effects of abstinence from tobacco: Valid symptoms and time course. Nicotine & Tobacco Research. 2007;9:315–327. doi: 10.1080/14622200701188919. [DOI] [PubMed] [Google Scholar]
- Hughes JR, Dash M, Callas PW. Is impulsivity a symptom of initial tobacco withdrawal? A meta-analysis and qualitative systematic review. Nicotine Tob Res. 2015;17:503–509. doi: 10.1093/ntr/ntu220. [DOI] [PubMed] [Google Scholar]
- Hughes JR, Hatsukami D. Signs and symptoms of tobacco withdrawal. Archives of General Psychiatry. 1986;43:289–294. doi: 10.1001/archpsyc.1986.01800030107013. [DOI] [PubMed] [Google Scholar]
- Hughes JR, Solomon LJ, Naud S, Fingar JR, Helzer JE, Callas PW. Natural history of attempts to stop smoking. Nicotine Tob Res. 2014;16:1190–1198. doi: 10.1093/ntr/ntu052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hursh SR, Silberberg A. Economic demand and essential value. Psychological Review. 2008;115:186–198. doi: 10.1037/0033-295X.115.1.186. [DOI] [PubMed] [Google Scholar]
- Inzlicht M, Schmeichel BJ. What Is Ego Depletion? Toward a Mechanistic Revision of the Resource Model of Self-Control. Perspect Psychol Sci. 2012;7:450–463. doi: 10.1177/1745691612454134. [DOI] [PubMed] [Google Scholar]
- Inzlicht M, Schmeichel BJ, Macrae CN. Why self-control seems (but may not be) limited. Trends in Cognitive Sciences. 2014 doi: 10.1016/j.tics.2013.12.009. [DOI] [PubMed] [Google Scholar]
- Jacobs EA, Bickel WK. Modeling drug consumption in the clinic using simulation procedures: demand for heroin and cigarettes in opioid-dependent outpatients. Exp Clin Psychopharmacol. 1999;7:412–426. doi: 10.1037//1064-1297.7.4.412. [DOI] [PubMed] [Google Scholar]
- Kirby KN. One-year temporal stability of delay-discount rates. Psychon Bull Rev. 2009;16:457–462. doi: 10.3758/PBR.16.3.457. [DOI] [PubMed] [Google Scholar]
- Kirby KN, Petry NM, Bickel WK. Heroin addicts discount delayed rewards at higher rates than non-drug using controls. Journal of Experimental Psychology: General. 1999;128:78–87. doi: 10.1037//0096-3445.128.1.78. [DOI] [PubMed] [Google Scholar]
- Kirchner TR, Cantrell J, Anesetti-Rothermel A, Ganz O, Vallone DM, Abrams DB. Geospatial exposure to point-of-sale tobacco: real-time craving and smoking-cessation outcomes. American Journal of Preventive Medicine. 2013;45:379–385. doi: 10.1016/j.amepre.2013.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koffarnus MN, Jarmolowicz DP, Mueller ET, Bickel WK. Changing delay discounting in the light of the competing neurobehavioral decision systems theory: A review. J Exp Anal Behav. 2013;99:32–57. doi: 10.1002/jeab.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurzban R. Does the brain consume additional glucose during self-control tasks? Evol Psychol. 2010;8:244–259. [PubMed] [Google Scholar]
- Kurzban R, Duckworth A, Kable JW, Myers J. An opportunity cost model of subjective effort and task performance. Behavioral and Brain Sciences. 2013;36:661–679. doi: 10.1017/S0140525X12003196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lagorio CH, Madden GJ. Delay discounting of real and hypothetical rewards III: steady-state assessments, forced-choice trials, and all real rewards. Behavioural Processes. 2005;69:173–187. doi: 10.1016/j.beproc.2005.02.003. [DOI] [PubMed] [Google Scholar]
- Leeman RF, O’Malley SS, White MA, McKee SA. Nicotine and food deprivation decrease the ability to resist smoking. Psychopharmacology. 2010;212:25–32. doi: 10.1007/s00213-010-1902-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leventhal AM, Waters AJ, Moolchan ET, Heishman SJ, Pickworth WB. A quantitative analysis of subjective, cognitive, and physiological manifestations of the acute tobacco abstinence syndrome. Addict Behav. 2010;35:1120–1130. doi: 10.1016/j.addbeh.2010.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu X, Li R, Lanza ST, Vasilenko SA, Piper M. Understanding the role of cessation fatigue in the smoking cessation process. Drug Alcohol Depend. 2013;133:548–555. doi: 10.1016/j.drugalcdep.2013.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lurquin JH, Michaelson LE, Barker JE, Gustavson DE, von Bastian CC, Carruth NP, Miyake A. No Evidence of the Ego-Depletion Effect across Task Characteristics and Individual Differences: A Pre-Registered Study. PLoS One. 2016;11:e0147770. doi: 10.1371/journal.pone.0147770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKillop J, Amlung MT, Few LR, Ray LA, Sweet LH, Munafo MR. Delayed reward discounting and addictive behavior: a meta-analysis. Psychopharmacology (Berl) 2011;216:305–321. doi: 10.1007/s00213-011-2229-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKillop J, Brown CL, Stojek MK, Murphy CM, Sweet L, Niaura RS. Behavioral economic analysis of withdrawal- and cue-elicited craving for tobacco: an initial investigation. Nicotine & Tobacco Research. 2012;14:1426–1434. doi: 10.1093/ntr/nts006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKillop J, Kahler CW. Delayed reward discounting predicts treatment response for heavy drinkers receiving smoking cessation treatment. Drug Alcohol Depend. 2009;104:197–203. doi: 10.1016/j.drugalcdep.2009.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKillop J, Miranda R, Jr., Monti PM, Ray LA, Murphy JG, Rohsenow DJ, Gwaltney CJ. Alcohol demand, delayed reward discounting, and craving in relation to drinking and alcohol use disorders. J Abnorm Psychol. 2010;119:106–114. doi: 10.1037/a0017513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackillop J, Murphy CM, Martin RA, Stojek M, Tidey JW, Colby SM, Rohsenow DJ. Predictive Validity of a Cigarette Purchase Task in a Randomized Controlled Trial of Contingent Vouchers for Smoking in Individuals With Substance Use Disorders. Nicotine Tob Res. 2015 doi: 10.1093/ntr/ntv233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKillop J, Murphy JG, Ray LA, Eisenberg DTA, Lisman SA, Lum JK, Wilson DS. Further validation of a cigarette purchase task for assessing the relative reinforcing efficacy of nicotine in college smokers. Experimental and Clinical Psychopharmacology. 2008;16:57–65. doi: 10.1037/1064-1297.16.1.57. [DOI] [PubMed] [Google Scholar]
- MacKillop J, Tidey JW. Cigarette demand and delayed reward discounting in nicotine-dependent individuals with schizophrenia and controls: an initial study. Psychopharmacology. 2011;216:91–99. doi: 10.1007/s00213-011-2185-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madden GJ, Begotka AM, Raiff BR, Kastern LL. Delay discounting of real and hypothetical rewards. Exp Clin Psychopharmacol. 2003;11:139–145. doi: 10.1037/1064-1297.11.2.139. [DOI] [PubMed] [Google Scholar]
- Madden GJ, Bickel WK. Impulsivity: The Behavioral and Neurological Science of Discounting. 1st ed American Psychological Association; 2009. [Google Scholar]
- Madden GJ, Raiff BR, Lagorio CH, Begotka AM, Mueller AM, Hehli DJ, Wegener AA. Delay Discounting of Potentially Real and Hypothetical Rewards: II. Between- and Within-Subject Comparisons. Experimental and Clinical Psychopharmacology. 2004;12:251–261. doi: 10.1037/1064-1297.12.4.251. [DOI] [PubMed] [Google Scholar]
- McCarthy DE, Piasecki TM, Fiore MC, Baker TB. Life before and after quitting smoking: an electronic diary study. Journal of Abnormal Psychology. 2006;115:454–466. doi: 10.1037/0021-843X.115.3.454. [DOI] [PubMed] [Google Scholar]
- McKee SA. Developing human laboratory models of smoking lapse behavior for medication screening. Addiction Biology. 2009;14:99–107. doi: 10.1111/j.1369-1600.2008.00135.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKee SA, Krishnan-Sarin S, Shi J, Mase T, O’Malley SS. Modeling the effect of alcohol on smoking lapse behavior. Psychopharmacology. 2006;189:201–210. doi: 10.1007/s00213-006-0551-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKee SA, Sinha R, Weinberger AH, Sofuoglu M, Harrison EL, Lavery M, Wanzer J. Stress decreases the ability to resist smoking and potentiates smoking intensity and reward. Journal of Psychopharmacology. 2010;25:490–502. doi: 10.1177/0269881110376694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKee SA, Weinberger AH, Shi J, Tetrault J, Coppola S. Developing and validating a human laboratory model to screen medications for smoking cessation. Nicotine & Tobacco Research. 2012;14:1362–1371. doi: 10.1093/ntr/nts090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell SH. Effects of short-term nicotine deprivation on decision-making: Delay, uncertainty, and effort discounting. Nicotine & Tobacco Research. 2004;6:819–828. doi: 10.1080/14622200412331296002. [DOI] [PubMed] [Google Scholar]
- Molden DC, Hui CM, Scholer AA, Meier BP, Noreen EE, D’Agostino PR, Martin V. Motivational versus metabolic effects of carbohydrates on self-control. Psychol Sci. 2012;23:1137–1144. doi: 10.1177/0956797612439069. [DOI] [PubMed] [Google Scholar]
- Muraven M. Practicing self-control lowers the risk of smoking lapse. Psycholology of Addictive Behaviors. 2010;24:446–452. doi: 10.1037/a0018545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muraven M, Collins RL, Shiffman S, Paty JA. Daily Fluctuations in Self-Control Demands and Alcohol Intake. Psychology of Addictive Behaviors. 2005;19:140–147. doi: 10.1037/0893-164X.19.2.140. [DOI] [PubMed] [Google Scholar]
- Muraven M, Shmueli D. The self-control costs of fighting the temptation to drink. Psychology of Addictive Behaviors. 2006;20:154–160. doi: 10.1037/0893-164X.20.2.154. [DOI] [PubMed] [Google Scholar]
- Muraven M, Slessareva E. Mechanisms of self-control failure: motivation and limited resources. Pers Soc Psychol Bull. 2003;29:894–906. doi: 10.1177/0146167203029007008. [DOI] [PubMed] [Google Scholar]
- Muraven M, Tice DM, Baumeister RF. Self-control as a limited resource: Regulatory depletion patterns. Journal of Personality and Social Psychology. 1998;74:774–789. doi: 10.1037//0022-3514.74.3.774. [DOI] [PubMed] [Google Scholar]
- Murphy JG, MacKillop J. Relative reinforcing efficacy of alcohol among college student drinkers. Exp Clin Psychopharmacol. 2006;14:219–227. doi: 10.1037/1064-1297.14.2.219. [DOI] [PubMed] [Google Scholar]
- Murphy JG, MacKillop J, Tidey JW, Brazil LA, Colby SM. Validity of a demand curve measure of nicotine reinforcement with adolescent smokers. Drug Alcohol Depend. 2011;113:207–214. doi: 10.1016/j.drugalcdep.2010.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Connell KA, Schwartz JE, Shiffman S. Do resisted temptations during smoking cessation deplete or augment self-control resources? Psychology of Addictive Behaviors. 2008;22:486–495. doi: 10.1037/0893-164X.22.4.486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Connor RJ, Heckman BW, Adkison SE, Rees VW, Hatsukami DK, Bickel WK, Cummings KM. Persistence and amplitude of cigarette demand in relation to quit intentions and attempts. Psychopharmacology. 2016 doi: 10.1007/s00213-016-4286-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Partos TR, Borland R, Yong HH, Hyland A, Cummings KM. The quitting rollercoaster: how recent quitting history affects future cessation outcomes (data from the International Tobacco Control 4-country cohort study) Nicotine Tob Res. 2013;15:1578–1587. doi: 10.1093/ntr/ntt025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paulhus DL. Measurement and control of response bias. In: Robinson JP, Shaver PR, Wrightsman LS, editors. Measures of personality and social psychological attitudes. Academic Press; San Diego, CA, US: 1991. pp. 17–59. [Google Scholar]
- Perkins KA, Conklin CA, Levine MD. Cognitive-behavioral therapy for smoking cessation: a practical guidebook to the most effective treatments. Taylor & Francis; New York, NY: 2008. [Google Scholar]
- Perkins KA, Lerman C. An efficient early phase 2 procedure to screen medications for efficacy in smoking cessation. Psychopharmacology (Berl) 2014;231:1–11. doi: 10.1007/s00213-013-3364-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perkins KA, Lerman C, Stitzer ML, Fonte CA, Briski JL, Scott JA, Chengappa KNR. Development of procedures for early screening of smoking cessation medications in humans. Clinical Pharmacology & Therapeutics. 2008;84:216–221. doi: 10.1038/clpt.2008.30. [DOI] [PubMed] [Google Scholar]
- Piasecki TM, Fiore MC, Baker TB. Profiles in discouragement: two studies of variability in the time course of smoking withdrawal symptoms. J Abnorm Psychol. 1998;107:238–251. doi: 10.1037//0021-843x.107.2.238. [DOI] [PubMed] [Google Scholar]
- Piasecki TM, Fiore MC, McCarthy DE, Baker TB. Have we lost our way? The need for dynamic formulations of smoking relapse proneness. Addiction. 2002;97:1093–1108. doi: 10.1046/j.1360-0443.2002.00216.x. [DOI] [PubMed] [Google Scholar]
- Piasecki TM, Jorenby DE, Smith SS, Fiore MC, Baker TB. Smoking withdrawal dynamics: I. Abstinence distress in lapsers and abstainers. J Abnorm Psychol. 2003a;112:3–13. [PubMed] [Google Scholar]
- Piasecki TM, Jorenby DE, Smith SS, Fiore MC, Baker TB. Smoking withdrawal dynamics: II. Improved tests of withdrawal-relapse relations. J Abnorm Psychol. 2003b;112:14–27. [PubMed] [Google Scholar]
- Piasecki TM, Niaura R, Shadel WG, Abrams D, Goldstein M, Fiore MC, Baker TB. Smoking withdrawal dynamics in unaided quitters. J Abnorm Psychol. 2000;109:74–86. doi: 10.1037//0021-843x.109.1.74. [DOI] [PubMed] [Google Scholar]
- Piper ME. Withdrawal: Expanding a Key Addiction Construct. Nicotine Tob Res. 2015;17:1405–1415. doi: 10.1093/ntr/ntv048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piper ME, Federmen EB, McCarthy DE, Bolt DM, Smith SS, Fiore MC, Baker TB. Using mediational models to explore the nature of tobacco motivation and tobacco treatment effects. Journal of Abnormal Psychology. 2008;117:94–105. doi: 10.1037/0021-843X.117.1.94. [DOI] [PubMed] [Google Scholar]
- Piper ME, Schlam TR, Cook JW, Sheffer MA, Smith SS, Loh WY, Baker TB. Tobacco withdrawal components and their relations with cessation success. Psychopharmacology (Berl) 2011;216:569–578. doi: 10.1007/s00213-011-2250-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher KJ, Rucker DD, Hayes AF. Addressing Moderated Mediation Hypotheses: Theory, Methods, and Prescriptions. Multivariate Behav Res. 2007;42:185–227. doi: 10.1080/00273170701341316. [DOI] [PubMed] [Google Scholar]
- Robinson MD, Schmeichel BJ, Inzlicht M. A cognitive control perspective of self-control strength and its depletion. Social and Personality Psychology Compass. 2010;4:189–200. [Google Scholar]
- Roche DJ, Bujarski S, Moallem NR, Guzman I, Shapiro JR, Ray LA. Predictors of smoking lapse in a human laboratory paradigm. Psychopharmacology (Berl) 2014 doi: 10.1007/s00213-014-3465-x. [DOI] [PubMed] [Google Scholar]
- Sayers WM, Sayette MA. Suppression on your own terms: internally generated displays of craving suppression predict rebound effects. Psychol Sci. 2013;24:1740–1746. doi: 10.1177/0956797613479977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sayette MA. The Role of Craving in Substance Use Disorders: Theoretical and Methodological Issues. Annu Rev Clin Psychol. 2016;12:407–433. doi: 10.1146/annurev-clinpsy-021815-093351. [DOI] [PubMed] [Google Scholar]
- Sayette MA, Martin CS, Hull JG, Wertz JM, Perrott MA. Effects of nicotine deprivation on craving response covariation in smokers. J Abnorm Psychol. 2003;112:110–118. [PMC free article] [PubMed] [Google Scholar]
- Sayette MA, Martin CS, Wertz JM, Shiffman S, Perrott MA. A multidimensional analysis of cue-elicited craving in heavy smokers and tobacco chippers. Addiction. 2001;96:1419–1432. doi: 10.1080/09652140120075152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmeichel BJ, Vohs K. Self-affirmation and self-control: Affirming core values counteracts ego depletion. Journal of Personality and Social Psychology. 2009;96:770–782. doi: 10.1037/a0014635. [DOI] [PubMed] [Google Scholar]
- Sheffer C, Mackillop J, McGeary J, Landes R, Carter L, Yi R, Bickel W. Delay discounting, locus of control, and cognitive impulsiveness independently predict tobacco dependence treatment outcomes in a highly dependent, lower socioeconomic group of smokers. American Journal on Addictions. 2012;21:221–232. doi: 10.1111/j.1521-0391.2012.00224.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiffman S. Relapse following smoking cessation: A situational analysis. Journal of Consulting and Clinical Psychology. 1982;50:71–86. doi: 10.1037//0022-006x.50.1.71. [DOI] [PubMed] [Google Scholar]
- Shiffman S. A cluster-analytic classification of smoking relapse episodes. Addict Behav. 1986;11:295–307. doi: 10.1016/0306-4603(86)90057-2. [DOI] [PubMed] [Google Scholar]
- Shiffman S. Ecological momentary assessment (EMA) in studies of substance use. Psychological Assessment. 2009;21:486–497. doi: 10.1037/a0017074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiffman S, Scharf DM, Shadel WG, Gwaltney CJ, Dang Q, Paton SM, Clark DB. Analyzing milestones in smoking cessation: illustration in a nicotine patch trial in adult smokers. J Consult Clin Psychol. 2006;74:276–285. doi: 10.1037/0022-006X.74.2.276. [DOI] [PubMed] [Google Scholar]
- Shmueli D, Prochaska JJ. Resisting tempting foods and smoking behavior: implications from a self-control theory perspective. Health Psychology. 2009;28:300–306. doi: 10.1037/a0013826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shmueli D, Prochaska JJ. A test of positive affect induction for countering self-control depletion in cigarette smokers. Psychology of Addictive Behaviors. 2012;26:157–161. doi: 10.1037/a0023706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein JS, Koffarnus MN, Snider SE, Quisenberry AJ, Bickel WK. Identification and management of nonsystematic purchase task data: Toward best practice. Exp Clin Psychopharmacol. 2015;23:377–386. doi: 10.1037/pha0000020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tabachnick BG, Fidell LS. Using multivariate statistics. 6th ed Pearson Education; Boston: 2013. [Google Scholar]
- Tice DM, Baumeister RF, Shmueli D, Muraven M. Restoring the self: Positive affect helps improve self-regulation following ego depletion. Journal of Experimental Social Psychology. 2007;43:379–384. [Google Scholar]
- Tice DM, Bratslavsky E, Baumeister RF. Emotional distress regulation takes precedence over impulse control: if you feel bad, do it! Journal of Personality and Social Psychology. 2001;80:53–67. [PubMed] [Google Scholar]
- Tiffany ST. A cognitive model of drug urges and drug-use behavior: role of automatic and nonautomatic processes. Psychological Review. 1990;97:147–168. doi: 10.1037/0033-295x.97.2.147. [DOI] [PubMed] [Google Scholar]
- Tyler JM, Burns KC. After depletion: The replenishment of the self’s regulatory resources. Self and Identity. 2008;7:305–321. [Google Scholar]
- U.S. Department of Health and Human Services . The Health Consequences of Smoking-50 Years of Progress: A Report of the Surgeon General. Centers for Disease Control and Prevention (US); Atlanta (GA): 2014. Reports of the Surgeon General. [Google Scholar]
- VanderBroek L, Acker J, Palmer AA, de Wit H, MacKillop J. Interrelationships among parental family history of substance misuse, delay discounting, and personal substance use. Psychopharmacology. 2016;233:39–48. doi: 10.1007/s00213-015-4074-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vangeli E, Stapleton J, Smit ES, Borland R, West R. Predictors of attempts to stop smoking and their success in adult general population samples: A systematic review. Addiction. 2011;106:2110–2121. doi: 10.1111/j.1360-0443.2011.03565.x. [DOI] [PubMed] [Google Scholar]
- Vohs KD, Heatherton TF. Self-regulatory failure: A resource-depletion approach. Psychol Sci. 2000;11:249–254. doi: 10.1111/1467-9280.00250. [DOI] [PubMed] [Google Scholar]
- Vohs KD, Schmeichel BJ. Self-regulation and the extended now: Controlling the self alters the subjective experience of time. Journal of Personality and Social Psychology. 2003;85:217–230. doi: 10.1037/0022-3514.85.2.217. [DOI] [PubMed] [Google Scholar]
- Webb TL, Sheeran P. Can implementation intentions help to overcome egodepletion? Journal of Experimental Social Psychology. 2002;39:279–286. [Google Scholar]
- World Health Organization . WHO report on the global tobacco epidemic, 2011: warning about the dangers of tobacco. World Health Organization; Geneva: 2011. [Google Scholar]