Abstract
Objective
Behavioral couples therapy (BCT) is more efficacious than individually-based therapy (IBT) for substance and relationship outcomes among patients with substance use disorder (SUD). This study compared BCT with IBT for drug-abusing women.
Method
Sixty-one women, mostly White, late thirties, with primary SUD other than alcohol (74% opioid diagnosis), and male partners were randomized to 26 sessions over 13-weeks of BCT plus 12-step-oriented IBT (i.e. BCT+IBT) or IBT. Substance-related outcomes: percentage days abstinent (PDA), percentage days drug use (PDDU), Inventory of Drug Use Consequences. Relationship outcomes: Dyadic Adjustment Scale (DAS) and days separated. Data were collected at baseline, post-treatment, and quarterly for 1-yr follow-up.
Results
On PDA, PDDU, and substance-related problems, both BCT+IBT and IBT patients showed significant (p < .01) large effect size improvements throughout the 1-yr follow-up (d > .8 for most time periods). BCT+IBT showed a significant (p < .001) large effect size (d = −.85) advantage versus IBT on fewer substance-related problems, while BCT+IBT and IBT did not differ on PDA or PDDU (p’s > .47). On relationship outcomes, compared to IBT, BCT+IBT had significantly higher male-reported DAS (p < .001, d = .57) and fewer days separated (p = .01, d = −.47) throughout the 1-yr follow-up.
Conclusion
BCT+IBT for drug-abusing women was more efficacious than IBT in improving relationship satisfaction and preventing relationship break-up. On substance use and substance-related problems, women receiving both treatments substantially improved, and women receiving BCT+IBT had fewer substance-related problems than IBT.
Keywords: female drug abuse, couples therapy, treatment outcomes
Behavioral couples therapy (BCT) is a couple-based therapy for adults with substance use disorder (SUD) that aims to help the SUD patient and their partner build support for the patient’s abstinence and improve relationship functioning. BCT has a strong research base establishing its efficacy, and it has been shown to be more effective than more typical individual-based treatment (IBT) for married or cohabiting SUD patients. Specifically, BCT produces better outcomes than IBT, consisting of greater abstinence, fewer substance-related problems, and better relationship functioning (for reviews see Powers, Vedel and Emmelkamp, 2008; and Meis et al., 2013). Notably, the vast majority of the studies examining BCT have been conducted using couples where the male partner had an SUD and the female partner did not have any substance use disorder. However, 4 recent studies have examined BCT for female SUD patients.
With female AUD patients, 3 randomized controlled trials (RCT) have compared BCT to IBT (Fals-Stewart, Birchler & Kelly, 2006; McCrady, Epstein, Cook, Jensen & Hildebrant, 2009; Schumm, O’Farrell, Kahler, Murphy & Muchowski, 2014). Each of these studies showed greater days abstinent over 12-months follow-up for BCT than IBT. Further, women receiving BCT had fewer substance-related problems and greater relationship satisfaction than IBT in the 2 studies that examined these outcomes (i.e., Fals-Stewart et al., 2006; Schumm et al., 2014).
With female drug abuse patients, only 1 RCT has evaluated the efficacy of BCT (Winters, Fals-Stewart, O’Farrell, Birchler & Kelly, 2002). This study showed that BCT had greater days abstinent, fewer substance-related problems, and greater relationship satisfaction than IBT. However, superior outcomes for BCT only lasted through 6-months follow-up, thus showing less durable improvements for drug abusing women than in the 3 studies of alcoholic women which found BCT had better outcomes throughout the entire 12-month follow-up period. Winters et al., (2002) did not examine relationship stability even though relationships of drug-abusing women are known to be unstable and prone to break-up (Greenfield et al., 2007).
A major limitation of the Winters et al., (2002) study was that it excluded 70% of otherwise eligible study participants because the male partner had a current SUD. When treating women drug or alcohol patients, 40–70% of them may have a male partner with an alcohol or drug problem (Greenfield et al., 2007). These dual problem couples in which both the male and female have a current alcohol or drug problem have typically been excluded from studies of BCT which relies heavily on support for abstinence from the partner. This is an important limitation to the generalizability of BCT results, due to the size of the dual problem subgroup and the research showing that a substance abusing male partner may have a negative impact on a women’s SUD treatment outcome (e.g. Tuten & Jones, 2003).
Recent literature reviews (Meis et al. 2013; O’Farrell & Clements, 2012) have called for expanding the BCT model to include such couples, and initial efforts in that direction have appeared. First, in the McCrady et al. (2009) study of BCT with women AUD patients, 13% had male partners with a current AUD. However, given the small numbers, the impact of dual problem status on outcome was not examined. Second, a naturalistic study of BCT for couples in which both partners had AUD (Schumm, O’Farrell, & Burdzovic Andreas, 2012), found similar positive outcomes in terms of days abstinent for dual problem couples in which both members wanted to change as for couples with only one AUD member. Finally, Jones, Tuten and O’Grady (2011) used an eclectic couple counseling (not BCT) as part of an intervention for male partners of opioid-dependent pregnant patients. They found the intervention was feasible and efficacious in the short term after 4-weeks but not at 28-week follow-up when compared to usual care. Therefore, the present study of BCT with drug abusing women attempted to extend the Winters et al., (2002) study and the overall literature on BCT by including dual problem couples and examining their impact on substance and relationship outcomes.
This study compared BCT with IBT for drug-abusing women. In this study, married or cohabiting female drug-abusing patients and their male relationship partners were recruited from a substance abuse treatment program. They were randomly assigned to equally intensive treatments consisting of either (a) BCT plus 12-step oriented IBT (i.e. BCT+IBT) or (b) IBT only (i.e. IBT). Data on primary substance-related outcomes and secondary relationship outcomes were collected at baseline, post-treatment, and at 3-, 6-, 9- and 12-month follow-up.
First, we predicted that, after treatment and during the 1-year follow-up period, female drug-abusing patients receiving BCT+IBT would have more days abstinent from alcohol and drugs, fewer days of using illicit drugs, and fewer substance-related problems than patients receiving IBT only. Second, we predicted that couples receiving BCT+IBT would have higher relationship satisfaction and greater relationship stability than couples receiving IBT only. Third, we examined whether patients in each treatment condition showed significant improvement on substance and relationship outcomes from baseline to post, and whether outcomes continued to show significant improvement from baseline at each follow-up. Finally, we explored whether dual problem couple status was associated with response to treatment overall or with differential response to BCT+IBT versus IBT only.
Method
Institutional review boards at Harvard Medical School and VA Boston approved this study.
Participants
Study criteria
Participants were 61 drug-abusing women patients and their male partners. They were recruited from women patients seeking treatment at either of 2 SUD treatment centers in Massachusetts from May 2010 to January 2014. Eligibility criteria were: (1) both woman patient and male partner over 18 years old; (2) couple married or living together for at least 1 year, lived apart for no more than 4 of past 12 months, and had no immediate plans to separate or divorce; (3) woman met Structured Clinical Interview for DSM-IV (SCID; First, Spitzer, Gibbons & Williams, 1996) criteria for a current (past 12 months) SUD, and had a substance other than alcohol or nicotine as the primary substance according to a diagnostic algorithm; (4) woman used primary drug in 60 days prior to study; (5) during study-based treatment program, woman agreed to goal of abstinence from drugs and alcohol, and was willing to forgo other non-study SUD counseling (other than self-help meetings or treatment required for an emergency or clinical deterioration); (6) woman could not be in a methadone maintenance program (which typically involved non-study counseling that was excluded by the present study), but they could take prescribed buprenorphine maintenance medication or naltrexone (so long as non-study counseling was not included); (7) neither woman patient or male partner had current SUD that required inpatient treatment or medical detoxification (after treatment they may be eligible for study); (8) neither patient or partner met SCID criteria for current schizophrenia, bipolar disorder with mania, or other psychotic disorder; (9) neither patient or partner had drug overdose or suicide attempt in past 30 days, or were at immediate risk for suicide or homicide; (10) couple denied severe intimate partner violence (IPV) in past 3 years and neither reported fear that couples therapy might increase IPV risk.
Male partners had 3 additional criteria. First, they had to agree that, if randomized to BCT, they would work together in BCT to help the female patient stay abstinent from drugs and alcohol. Second, two subgroups of male partners were included, one without and one with a current substance problem. The latter 28 couples were designated dual problem couples1 (Schumm et al., 2012) because both male and female partners had a current substance problem. To be in the study, the male partner in a dual problem couple had to agree that, if randomized to BCT, he would be asked to seriously consider staying abstinent from alcohol and drugs to help the female patient. He would be the one to choose whether or not to abstain from or reduce his alcohol or drug intake. However, he had to agree to have this choice discussed in initial BCT sessions. Third, if the male partner had a current substance problem, he was permitted to take part in whatever non-study counseling, self-help, or prescribed recovery medications he chose.
Characteristics of sample
As shown in Table 1, participants were, on average, in their late thirties, with about 13 years of education. They had been married or cohabitating for around 10 years, most were White, and about 40% had children ages 6 to 16. Median annual income was $15,000 for women and $42,000 for men. Nearly 30% of women were employed full- (14.8%) or part-time (13.1%). Women averaged about 14 years of problematic substance use. Women’s total scores on the Inventory of Drug Use Consequences - Lifetime were similar to those previously found among women in SUD treatment (e.g., Tonigan & Miller, 2002). Women’s current substance dependence diagnoses were opioids for 45 (74%), cocaine for 22 (36%), sedatives for 18 (30%), alcohol for 13 (21%), cannabis for 12 (20%), stimulants for 5 (8%), and other substances for 3 (5%). Women’s primary substance of abuse was opioids for 34 (56%), cocaine for 13 (21%), sedatives for 7 (12%), cannabis for 5 (8%), and stimulants for 2 (3%). About one-third (33%) of male partners had a current substance dependence diagnosis based on SCID criteria. On the broader “current substance problem” criteria defined in footnote-1 above, nearly half (45%) the women had a male partner with a current substance problem, and thus were part of a dual problem couple. Finally, participants in BCT did not differ from those in IBT on the variables just described (ps ≥ .12; see Table 1), except for a trend for women in the IBT condition to be more likely to have a stimulant dependence diagnosis (p=0.053).
Table 1.
Pretreatment Characteristics for Participants by Treatment Condition
| Characteristic | IBT (n = 31) M(SD) or No (%) | BCT (n = 30) M(SD) or No (%) | t or χ2 | p |
|---|---|---|---|---|
|
| ||||
| Female age | 38.9 (10.0) | 38.5 (10.4) | 0.15 | 0.878 |
| Female education | 13.7 (2.6) | 13.3 (1.9) | 0.64 | 0.522 |
| Male age | 43.2 (10.6) | 42.3 (10.4) | 0.36 | 0.722 |
| Male education | 12.9 (1.6) | 13.2 (3.7) | 0.41 | 0.684 |
| Years married or cohabiting | 11.4 (11.1) | 8.0 (7.6) | 1.40 | 0.166 |
| Child age 6-16 living in home | 14 (45) | 12 (40) | 0.17 | 0.684 |
| Annual female median income | $20,000 | $15,000 | —a | 0.789 |
| Annual male median income | $42,500 | $42,000 | —a | 0.898 |
| Female ethnicity: | 2.00 | 0.367 | ||
| White | 27 (87) | 26 (87) | ||
| African-American | 3 (10) | 1 (3) | ||
| Hispanic | 1 (3) | 3 (10) | ||
| American Indian | 0 | 0 | ||
|
| ||||
| Male ethnicity: | 2.36 | 0.501 | ||
| White | 27 (87) | 24 (80) | ||
| African-American | 1 (3) | 3 (10) | ||
| Hispanic | 2 (7) | 3 (10) | ||
| American Indian | 1 (3) | 0 | ||
| Female employment: | 3.41 | 0.491 | ||
| Not employed | 16(52) | 15 (50) | ||
| Employed full-time | 4 (13) | 5 (17) | ||
| Employed part-time | 6 (19) | 2 (7) | ||
| Homemaker | 2 (7) | 5 (17) | ||
| Other | 3 (10) | 3 (10) | ||
|
| ||||
| Years female problematic substance use | 14.3 (10.9) | 13.8 (11.3) | 0.16 | 0.872 |
| Female InDUC-Lifetime total score Female current substance dependence dx | 35.19 (7.92) | 35.97 (5.16) | 0.45 | 0.654 |
| Alcohol | 4 (13) | 9 (30) | —b | 0.127 |
| Cannabis | 5 (16) | 7 (23) | 0.50 | 0.479 |
| Cocaine | 10 (32) | 12 (40) | 0.40 | 0.529 |
| Opioid | 22 (71) | 23 (77) | 0.26 | 0.613 |
| Sedatives | 9 (29) | 9 (30) | 0.01 | 0.934 |
| Stimulants | 5 (16) | 0 | —b | 0.053 |
| Other | 3 (10) | 0 | —b | 0.238 |
|
| ||||
| Female primary substance of abuse | ||||
| Alcohol | 0 | 0 | — | — |
| Cannabis | 2 (7) | 3 (10) | —b | 0.671 |
| Cocaine | 7 (23) | 6 (20) | 0.06 | 0.806 |
| Opioid | 17(55) | 17 (57) | 0.02 | 0.886 |
| Sedatives | 3 (10) | 4 (13) | —b | 0.707 |
| Stimulants | 2 (7) | 0 | —b | 0.492 |
| Other | 0 | 0 | — | — |
|
| ||||
| Male current substance dependence dx | ||||
| None | 20 (65) | 21 (70) | 0.21 | 0.648 |
| Alcohol | 1 (3) | 3 (10) | —b | 0.354 |
| Cannabis | 2 (7) | 2 (7) | —b | 1.00 |
| Cocaine | 4 (13) | 0 | —b | 0.113 |
| Opioid | 7 (23) | 6 (20) | 0.06 | 0.806 |
| Sedatives | 3 (10) | 1 (3) | —b | 0.612 |
| Stimulants | 1 (3) | 0 | —b | 1.00 |
| Other | 1 (3) | 0 | —b | 1.00 |
|
| ||||
| Dual problem couple | 14 (45) | 14 (47) | 0.01 | 0.906 |
Note. IBT = individual-based treatment. BCT = behavioral couples therapy plus IBT. Dx = DSM-IV diagnosis.
The p-value for this variable comes from a non-parametric independent samples median test.
The p-value for this variable comes from Fisher’s Exact Test because the data did not meet assumptions for chi-square.
Measures
Unless otherwise specified, measures were administered to both partners at pre- and post-treatment and then again at 3-, 6-, 9-, and 12-months following treatment.
Timeline Followback Interview (TLFB; Sobell & Sobell, 1996)
The TLFB uses a calendar and other memory aids to gather information about substance use over a specified period of time. TLFB has shown test-retest and patient-collateral correlations of ≥ .80 for alcohol and illicit drugs (Sobell & Sobell, 1996). TLFB variables analyzed were percent days of any illicit drug use (PDDU), and percent days abstinent (PDA) from using illicit drugs or drinking while not in jail or hospital for substance-related reasons. PDA was used in the 4 prior studies of BCT with women SUD patients. Patient and partner completed the TLFB about the female patient. To reduce underreporting, the TLFB scores used were the worst case score (indicating fewer PDA and more PDDU) of patient and partner reports at each time period; if only one person’s score was available, that score was used. There were large correlations between patient- and partner-reported PDA (r > .76) and PDDU (r > .75) at all time periods.
Urine drug samples (Vereby and Turner, 1991)
These were analyzed for presence or absence of: cannabis, cocaine, opiates, oxycodone, barbiturates, amphetamines, benzodiazepines, methamphetamines, phencyclidine, and propoxyphene. Samples were tested with the Rapid Detect iCup Drug Screen, a self-contained collection and testing device that provides results in a few minutes and is approved by the FDA. During the 13-week treatment period, patients were scheduled to give a urine sample once a week at an individual counseling session. During the 1-year follow-up, patients were planned to give a urine sample at each quarterly follow-up interview. A missing urine sample was coded as a positive result indicating drug use.
Inventory of Drug Use Consequences (InDUC; Tonigan & Miler, 2002)
The InDUC is a 45-item self-report measure of adverse consequences of drug and alcohol use. The InDUC has excellent test-retest reliability, good to excellent internal reliability, acceptable convergent validity, and good sensitivity to change in response to treatment (Tonigan & Miller, 2002). Internal reliabilities in this study were excellent at all time periods (α > .94). Both partners answered the InDUC about consequences of the woman’s drug and alcohol use. At baseline, the current (past 3 months) and lifetime versions of the InDUC were both administered. At post-treatment, the InDUC referenced the time during treatment, and the InDUC referenced the prior 3 months during the other follow-up assessments. To reduce possible underreporting, we used the higher report when both partners provided responses to an InDUC item. When data was available from only one partner on an InDUC item, we used the available partner’s report. For the lifetime version of the InDUC, response options are 0 = no or 1= yes, and possible scores range from 0–45 (see Table 1). For the current version of the InDUC, response options range from 0 = never to 3 = daily or almost daily, and possible scores range from 0–135 (see Table 2).
Table 2.
Substance Use Outcomes Observed M (SD), Sample Size, and Effect Size Change from Baseline by Treatment Condition
| Percentage days abstinent (PDA) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||
| Treatment | Baseline M (SD) | Post M (SD) | Post d | 3-month M (SD) | 3-month d | 6-month M (SD) | 6-month d | 9-month M (SD) | 9-month d | 12-month M (SD) | 12-month d |
| BCT + IBT | 24.20 (25.24) n = 30 |
76.23a (34.29) n = 30 |
1.56 | 70.54a (40.58) n = 30 |
1.06 | 66.85a (42.11) n = 30 |
.92 | 66.63a (41.76) n = 30 |
.94 | 70.34a (44.31) n = 29 |
.93 |
| IBT | 23.33 (29.89) n = 31 |
68.84a (41.12) n = 31 |
.94 | 68.02a (42.50) n = 31 |
.91 | 65.15a (44.55) n = 31 |
.90 | 58.28a (45.33) n = 29 |
.71 | 64.14a (43.97) n = 29 |
.75 |
|
| |||||||||||
| Percentage days drug use (PDDU) | |||||||||||
|
| |||||||||||
| Treatment | Baseline M (SD) | Post M (SD) | Post d | 3-month M (SD) | 3-month d | 6-month M (SD) | 6-month d | 9-month M (SD) | 9-month d | 12-month M (SD) | 12-month d |
|
| |||||||||||
| BCT + IBT | 70.86 (25.73) n = 30 |
18.63a (32.42) n = 30 |
1.54 | 26.28a (40.67) n = 30 |
.96 | 24.67a (39.43) n = 30 |
.97 | 24.18a (38.74) n = 30 |
1.04 | 27.10a (42.94) n = 29 |
.90 |
| IBT | 71.69 (33.47) n = 31 |
26.08a (37.97) n = 31 |
.92 | 26.88a (40.64) n = 31 |
.85 | 30.58a (43.77) n = 31 |
.80 | 34.48a (44.05) n = 29 |
.74 | 26.91a (41.27) n = 29 |
.84 |
|
| |||||||||||
| Inventory of Drug Use Consequences – Current (InDUC-C) | |||||||||||
|
| |||||||||||
| Treatment | Baseline M (SD) | Post M (SD) | Post d | 3-month M (SD) | 3-month d | 6-month M (SD) | 6-month d | 9-month M (SD) | 9-month d | 12-month M (SD) | 12-month d |
|
| |||||||||||
| BCT + IBT | 66.40 (23.83) n = 30 |
25.35a (30.32) n = 30 |
1.18 | 21.26a (29.29) n = 29 |
1.39 | 18.07a (27.14) n = 30 |
1.41 | 18.64a (28.56) n = 30 |
1.49 | 15.86a (27.58) n = 29 |
1.59 |
| IBT | 63.84 (27.05) n = 31 |
41.52a (41.79) n = 31 |
.51 | 23.60a (28.27) n = 30 |
1.02 | 23.23a (30.00) n = 30 |
1.00 | 29.68a (36.58) n = 29 |
.82 | 24.15a (31.91) n = 29 |
1.06 |
Note. IBT = individually-based therapy. BCT + IBT = behavioral couples therapy plus IBT. Post = post-treatment.
This score shows a significant (p < .01, Bonferonni corrected) improvement vs. baseline. Cohen’s d effect sizes guidelines are small = 0.2, medium = 0.5, large = 0.8.
Dyadic Adjustment Scale (DAS; Spanier, 2001)
The DAS is a widely used 32-item self-report measure of overall relationship adjustment, with possible total scores ranging from 0 to 146. The DAS exhibits excellent internal and test-retest reliability as well as strong concurrent and criterion-related validity in differentiating distressed from non-distressed couples (Spanier, 2001). Internal reliabilities in this study were very good at all time periods (α > .89).
Percent Days Separated (PSEP) Measure of Relationship Stability
Information about percent of days separated (i.e., living apart due to relationship discord or substance use) was gathered with the TLFB calendar interview method. PSEP is sensitive to changes in response to BCT (e.g., O’Farrell, Cutter, Choquette, Floyd & Bayog, 1992). There were large correlations between patient- and partner-reported PSEP at all time periods (r > .76).
Client Satisfaction Questionnaire-8 (CSQ-8; Attkinsson & Greenfield, 2004)
The CSQ-8 is an 8-item measure that was used to assess satisfaction with study-based treatment. Since some male partners were not directly involved with study-treatment, the CSQ-8 was given only to women at post-treatment. Possible total scores range from 8 to 32. The CSQ-8 performs consistently across a range of treatment settings, and has demonstrated construct validity (Attkinsson & Greenfield, 2004). In this study, internal reliability was excellent (α = .90).
Non-study-based treatment
Women were interviewed about substance-related treatment that they received during the 60 days prior to joining the study. Non-study-based treatment was defined as the total number of days of hospitalization for detoxification, residential substance-related treatment, and day treatment/intensive outpatient treatment. Also, we examined the number of patients who took prescribed buprenorphine maintenance medication or naltrexone during the study treatment period and during the 1-year follow-up period.
Procedure
Married and cohabiting women seeking treatment for a drug use disorder (N = 672) completed a screening questionnaire for possible study eligibility.2 Based on the screening, 264 were ineligible and 408 were deemed potentially eligible. Research staff attempted to contact women identified as potentially eligible but were not able to reach 101 women. Staff were able to speak with 307 potentially eligible women. Of the potentially eligible women that spoke with staff, 140 reported that they were not interested in the study.3 Another 78 reported initial interest in the study, but staff were unable to reconnect with them to confirm final interest and eligibility. For those who were potentially eligible, reported interest in the study, and responded to staff, interviews were privately and separately completed with the female patient and her male partner to further assess eligibility. Of the couples who completed these interviews, 15 couples were determined to be ineligible. Participant flow into the trial is shown in Figure 1.
Figure 1.
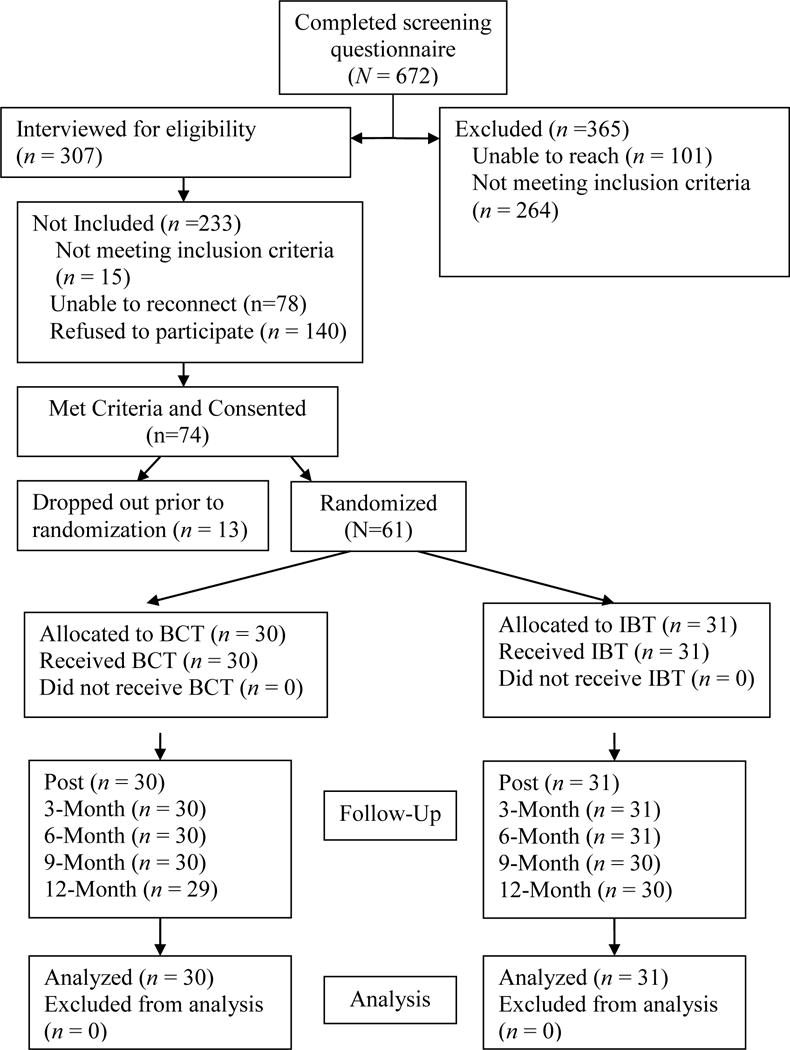
CONSORT (Consolidated Standards of Reporting Trials) flowchart. IBT = individual-based treatment. BCT = behavioral couples therapy plus IBT. Post = post-treatment.
A total of 74 couples met study criteria, signed informed consent, and were scheduled for baseline assessments with a research assistant. Following baseline assessments, the couple was scheduled to attend the first treatment session together. Randomization was conducted after couples had completed their baseline assessments and had scheduled their first treatment session. Of the 74 consented couples, 13 couples were not randomized because they dropped out prior to completing their baseline assessment (n = 10) or prior to scheduling their first treatment session (n = 3). The remaining 61 couples were put into an urn randomization computer program (Stout, Wirtz, Carbonari, & Del Boca, 1994) designed to balance the treatment groups in terms of age (34 or younger vs. 35 or older), married vs. cohabitation, primary drug of choice (opiate vs. other), dual problem couple status, and whether or not the couple had a child between the age of 6 and 16 living at home. Treatment assignment was concealed from couples until they arrived for their first treatment session. All couples who attended 1 or more treatment sessions became part of the intent-to-treat sample; they were randomized, followed and included in the analyses as long as at least one member of the couple provided some follow-up data (N = 61; see Figure 1).
Treatment Conditions
Women in either treatment condition were assigned to receive a total of 26, 60-minute therapy sessions over the course of 13 weeks. The BCT+IBT condition had 13 BCT sessions plus 13 individual counseling sessions, and the IBT condition had 26 individual sessions only.
BCT+IBT condition
Women in the BCT+IBT condition were planned to receive 13 BCT couple sessions – an initial couple-based clinical interview session followed by 12 sessions from the O’Farrell and Fals-Stewart (2006) BCT manual. BCT aimed to build support for abstinence by performing a daily “trust discussion” in which the patient states an intent to stay abstinent that day and the spouse expresses support for the patient’s efforts, and by other recovery activities. BCT also aimed to increase positive activities and communication.
BCT was modified for dual problem couples. In session 2 the couple decided if the male partner would be a “cheerleader” who focused on the female patient’s substance use only, or a “teammate” who used BCT to address his own substance use. Of 14 dual couples assigned to BCT, 8 (58%) chose teammate, 3 (21%) cheerleader, and 3 (21%) dropped out before choosing.
Women in the BCT+IBT condition also were planned to receive 13 individual, twelve-step oriented counseling sessions for treatment of SUD. For details see next paragraph.
IBT condition
Women in the IBT condition were planned to attend 26 individual sessions drawn from the individual drug counseling manual (Mercer & Woody, 1999), which was also the basis for individual sessions received in the BCT condition. This approach posits that SUD is a disease, and that recovery is achieved by staying abstinent from drugs and alcohol and attending NA or AA self-help groups. It had better outcomes than professional psychotherapy in NIDA’s Collaborative Cocaine Treatment Study (Crits-Christoph, et al., 1999). It also served as an IBT comparison group in 2 prior studies of BCT for women with AUD (Fals-Stewart et al., 2006; Schumm et al., 2014).
Study therapists
Five masters-level, licensed addiction counselors provided treatment in both BCT and IBT conditions. All 5 therapists were experienced in conducting 12-step oriented IBT, and 3 therapists had experience conducting BCT in a prior study of BCT. Patients were randomly assigned to either the BCT or IBT condition, and then one of the 5 therapists delivered the full course of the assigned treatment condition. Weekly supervision included review of audiotaped sessions and feedback about delivery of BCT and IBT.
Treatment fidelity
Sessions were audio-taped and rated to assess therapist adherence in delivering the manualized treatments. Items were rated on a 5-point scale (1 [not at all], 2 [a little], 3 [somewhat], 4 [considerably], 5 [extensively]). Adherence rating scales assessing fidelity to the individual drug counseling protocol were taken from the Appendix of Mercer and Woody (1999). They consisted of 6 items evaluating the degree to which the therapist focused upon abstinence from substance use and incorporated strategies for promoting abstinence which are consistent with a 12-step orientation. Adherence rating scales assessing fidelity to the BCT protocol consisted of 10 items (O’Farrell, 2013) evaluating key aspects of the BCT manual including review of promises, trust discussion, and recovery contract as well as other activities scheduled to be completed per the BCT manual.
Sessions were randomly selected to be rated, and ratings were performed by 2 independent raters trained in delivering the treatments. Thirty-two individual counseling and 30 BCT sessions were rated, and 22 individual drug counseling and 23 BCT sessions were independently coded by both raters. For sessions coded independently by both raters, level of agreement between raters was moderately high, and the percentage of items that were rated within 1 point difference between raters were 94.0% individual counseling, and 76.1% BCT.
Adherence ratings were acceptable for both session types. Mean adherence ratings for each session type were individual counseling (M=4.00, SD= 0.40), and BCT (M=3.85, SD=0.55). These scores are at or near the scale rating of 4=”considerably” for individual counseling and for BCT sessions. IBT and BCT+IBT conditions did not differ significantly on aggregate mean adherence ratings, F(1,45) = 3.13, p = .08. However, there was a significant difference between therapists on BCT adherence, F(2, 29) = 10.33, p < .001, with therapist A (who did not have experience with BCT prior to the present study) showing significantly less adherence versus the other therapists (p’s < .01 for post hoc pairwise comparisons).
Analyses
Comparison of treatment conditions on substance-related and relationship outcomes
We used generalized estimating equations (GEE) to test hypotheses involving primary substance-related and secondary relationship outcomes. PDA, PDDU, DAS, and PSEP were treated as continuous outcomes. GEE has several advantages, including the ability to include participants with missing data on the repeated measures outcome, the ability to model and account for variable non-independence, and the capacity to directly test the effects of time within the regression equations (Hall et al., 2001). Participants with data on at least one follow-up time period were included in the GEE models. For the outcome variable PSEP, we used an inverse transformation to improve normality. Continuous variables were z score-transformed to allow ready calculation of effect size estimates and to reduce multicollinearity between main effects and interaction terms. The effect of time corresponded to each assessment following treatment (i.e., post = 0, 3-month = 1, 6-month = 2, 9-month = 3, 12-month = 4). Treatment condition, study therapist, and dual problem couple status were treated as categorical variables. For treatment condition, IBT was coded as the reference group. Because study therapist A had significantly less adherence in delivering BCT, we covaried for the effect of therapist and treated therapist A as the categorical reference group. For dual problem couple status, couples in which only the female partner was drug-abusing were treated as the reference group. Finally, because a notable proportion of the sample received buprenorphine during and following treatment, we included percentage days of buprenorphine at post-treatment and at each follow-up as a time-varying covariate.
GEE analyses were conducted in several steps. Initial models were constructed that included time and the baseline outcome of interest as predictors. We then compared relative model fits for exchangeable, unstructured, and autoregressive dependent variable correlation structures and selected the structure with the lowest Quasi Likelihood under Independence Model Criterion (QIC) value.4 Once the best-fitting correlational structure was determined, we added treatment condition, percentage days of buprenorphine at post-treatment and each follow-up, therapist, and dual problem couple status to the model. We then entered the interaction between treatment condition and time to determine if treatment effects were diminished or enhanced over the course of follow-up. Finally, in an exploratory analysis, we tested the interaction between treatment condition and dual problem couple status to determine if women in dual problem relationships had a differential response to the study treatment conditions.
Changes in outcomes from baseline
To examine improvement for women who received IBT versus BCT+IBT, we computed paired sample t-tests to compare the baseline score with each outcome score (post, 3-, 6-, 9-and 12-month follow-up) for each measure to determine whether women in each condition showed significant improvement from baseline to that follow-up period. To control type 1 error, we used a Bonferonni-corrected significance level of p < .01 for each comparison. Cohen’s d effect sizes were calculated for the paired sample comparisons; we used Cohen’s (1988) guidelines of d = .2 as small, d = .5 as medium, and d = .8 as large.
Power analysis
Based upon findings in Winters et al. (2002), a Cohen’s f effect sizes of .25 and .26 were anticipated for differences between the BCT+IBT and IBT conditions on PDA and DAS. To achieve statistical power of .80 with α = .05, the study would require N = 84–104.
Results
Female Non-Study-Based Treatment
Treatment conditions did not differ on the amount of female non-study-based treatment during the 60 days prior to joining the study, t(59) = −0.72, p = .48. Women received an average of over 10 total days of detoxification, residential rehabilitation, and intensive outpatient treatment during the 60 days prior to the study, IBT M = 9.94, SD = 8.70; BCT+IBT M = 11.80, SD = 11.48. Also, treatment conditions did not differ on the number of patients who used adjunctive prescribed buprenorphine maintenance during the study treatment period (IBT = 29% vs. BCT+IBT = 27%; χ2(N = 61, 1) = 0.04, p=.837), or during the 1-year follow-up period (IBT = 29% vs. BCT+IBT = 33% ; χ2(N = 61, 1) = .13, p=.717). No patients used naltrexone.
Treatment Attendance, Patient Satisfaction, and Urine Drug Samples
Treatment attendance
Treatment conditions did not differ on number of female study-based psychotherapy sessions that were attended, t(59) = −0.83, p =.412. Women in both conditions attended an average of over 14 of 26 planned study therapy sessions: BCT+IBT M = 15.07, SD = 7.85; IBT M = 13.35, SD = 8.30. In addition, the conditions did not differ with regard to the number of women completing at least 50% (i.e., 13 or more) of the prescribed study psychotherapy sessions, χ2(N = 61, 1) = 1.43, p =.232. In BCT+IBT, 66.7% completed at least 50% of the study sessions, and in IBT, 51.6% completed at least 50% of the study sessions. Finally, women in the BCT+IBT condition attended an average of 7.43 BCT sessions (SD = 4.07) and 7.63 IBT sessions (SD = 4.32).
Patient satisfaction
On the CSQ-8, women, on average, were very satisfied with their study-based treatment. Total CSQ-8 scores in IBT, M = 28.0, SD = 3.36, and BCT+IBT, M = 29.19, SD = 4.22, did not differ significantly, t(53) = −1.16, p = .253. These scores were similar to large-scale samples of individuals seeking mental health care (Attkisson & Greenfield, 2004).
Urine drug specimens
During treatment, 60% of all planned weekly urine specimens were collected.5 Assuming any missing urine screen data represented a positive result, over the course of treatment, the mean number of urine samples that tested positive for female patients in the BCT+IBT condition (M = 7.7, SD = 4.8) and for female patients in the IBT condition (M = 7.6, SD = 4.9) did not differ significantly, t(59) = 0.07, p =.944. Across both treatment conditions, the correlation between self-reported percent days of drug use (PDDU) on the TLFB collected for the 13-week treatment period at post, and the number of positive urine screens collected weekly during the same period, showed a significant positive correlation (r = .56, p < .001) between self-report and urine screen data on drug use.
During the 1-year follow-up period, 82% of all planned quarterly urine specimens were collected.6 Over this period, the mean number of urine samples that tested positive for female patients in the BCT+IBT condition (M = 1.97, SD = 1.7) and for female patients in the IBT condition (M = 2.4, SD = 1.6) did not differ significantly, t(59) = 1.12, p =.267. Across both treatment conditions, the correlation between PDDU for the entire follow-up period, and the number of positive urine screens collected quarterly during the same period, showed a significant positive correlation (r = .58, p < .001) between self-report and urine screen data on drug use.
Primary Outcomes of Substance Use and Related Problems
For PDA, GEE models showed a better fit for an exchangeable (QIC = 300.51) versus unstructured (QIC = 307.31) or autoregressive (QIC = 301.04) correlation model. GEE analyses using an exchangeable correlation model showed that while controlling for baseline PDA and therapist, there were not significant main effects for treatment condition, dual problem couple status, or time. Also, there were not significant interactions with treatment condition in predicting PDA. Higher percentage days of buprenorphine use were associated with higher PDA (see Table 3). Turning to paired-sample t-tests for baseline PDA versus PDA during time points following treatment, results showed that both treatment conditions exhibited significant, large effect size improvements in PDA. Also, both treatment conditions maintained these significant improvements in PDA throughout the 12-month follow-up period (see Table 2).
Table 3.
Generalized Estimating Equation (GEE) Results for Substance Use Outcomes During Follow-up
| Percentage days abstinent (PDA) (N = 61) | ||||
|---|---|---|---|---|
|
| ||||
| Predictor | d | 95% CI | χ2 | p |
| Treatment condition | .166 | −.284, .617 | 0.522 | .470 |
| % days buprenorphine use | .335 | .227,, 442 | 37.233 | <.001 |
| Therapist A vs. Therapist B | −.377 | −1.171, .417 | 0.866 | .352 |
| vs. Therapist C | −.546 | −1.133, .041 | 3.324 | .068 |
| vs. Therapist D | −.601 | −1.418, .216 | 2.078 | .149 |
| vs. Therapist E | −.157 | −1.469, 1.175 | 0.047 | .828 |
| Baseline PDA | .140 | −.097, .377 | 1.342 | .247 |
| Dual problem couple | −.368 | −.860, .124 | 2.149 | .143 |
| Time | −.035 | −.073, .004 | 3.064 | .080 |
|
| ||||
| Treatment × time | −.006 | −.085, .072 | 0.026 | .872 |
| Treatment condition × dual problem couple | .427 | −.545, 1.399 | 0.741 | .389 |
|
| ||||
| Percentage days drug use (PDDU) (N = 61) | ||||
|
| ||||
| Predictor | d | 95% CI | χ2 | p |
|
| ||||
| Treatment condition | −.130 | −.563, .304 | 0.344 | .557 |
| % days buprenorphine use | −.240 | −.356, −.124 | 16.503 | <.001 |
| Therapist A vs. Therapist B | .137 | −.628, .903 | 0.124 | .725 |
| vs. Therapist C | .383 | −.181, .948 | 1.771 | .183 |
| vs. Therapist D | .195 | −.593, .983 | 0.235 | .628 |
| vs. Therapist E | .152 | −1.120, 1.425 | 0.055 | .814 |
| Baseline PDDU | .099 | −.134, .333 | 0.694 | .405 |
| Dual problem couple | .302 | −.177, .780 | 1.528 | .216 |
| Time | .014 | −.050, .078 | 0.183 | .669 |
|
| ||||
| Treatment × time | .036 | −.091, .163 | 0.308 | .579 |
| Treatment condition × dual problem couple | −.406 | −1.305, .537 | 0.713 | .399 |
|
| ||||
| Inventory of Drug Use Consequences (InDUC) (N = 61) | ||||
|
| ||||
| Predictor | d | 95% CI | χ2 | p |
|
| ||||
| Treatment condition | −.850 | −1.294, −.406 | 14.106 | <.001 |
| % days buprenorphine use | −.238 | −.314, −.162 | 37.483 | <.001 |
| Therapist A vs. Therapist B | 1.489 | .679, 2.300 | 12.972 | <.001 |
| vs. Therapist C | .437 | −.180, 1.054 | 1.930 | .165 |
| vs. Therapist D | 1.413 | .536, 2.291 | 9.963 | .002 |
| vs. Therapist E | −1.061 | −2.872, −.331 | 6.105 | .013 |
| Baseline InDUC | .490 | .246, .733 | 15.511 | <.001 |
| Dual problem couple | .370 | −.127, .867 | 2.130 | .144 |
| Time | −.077 | −.115, −.038 | 15.265 | <.001 |
|
| ||||
| Treatment × time | .095 | .021, .168 | 6.412 | .011 |
| Treatment condition × dual problem couple | −.801 | −1.748, .146 | 2.751 | .097 |
Note. Coding for treatment condition: 0 = individual-based treatment, 1 = behavioral couples therapy. Coding for dual problem couple: 0 = female but not male partner had substance use disorder, 1 = both partners had substance use disorder. Findings for main effects are displayed prior to entering interaction terms into the model. Cohen’s d effect sizes guidelines are small = 0.2, medium = 0.5, large = 0.8.
For PDDU, GEE models showed a better fit for an autoregressive (QIC = 313.44) versus unstructured (QIC = 328.46) or exchangeable (QIC = 314.29) correlation model. GEE analyses using an autoregressive correlation model showed that while controlling for baseline PDDU, there were not significant main effects for treatment condition, therapist, dual problem couple status, or time. Also, there were not significant interactions with treatment condition in predicting PDDU. Higher percentage days of buprenorphine use were associated with lower PDDU (see Table 3). Turning to paired-sample t-tests for baseline PDDU versus PDDU during time points following treatment, results showed that both treatment conditions had significant, large effect size improvements in PDDU. Also, both treatment conditions maintained these significant improvements in PDDU through the 12-month follow-up period (see Table 2).
For the InDUC-C measure of substance-related problems, an unstructured GEE correlational structure (QIC = 305.09) fit better than exchangeable (QIC = 305.33) or autoregressive (QIC = 305.82) structures. GEE analyses using an unstructured correlation matrix showed (see Table 3) that after controlling for other covariates, there was a significant, large effect size for treatment condition, which favored BCT+IBT over IBT. There was also a significant effect for time which showed that women had fewer substance-related problems as the follow-up period progressed. Higher percentage days of buprenorphine use was associated with lower InDUC-C. Finally, a small but significant treatment by time interaction was explained by a more rapid reduction of substance-related problems at post-treatment for women receiving BCT+IBT. Turning to paired-sample t-tests, findings showed (see Table 2) that women who received BCT+IBT had significant, large effect size reduction of substance-related problems starting at post-treatment and at all time periods during the 12-month follow-up. Women who received IBT showed significant, medium effect size reduction of substance-related problems at post-treatment and significant, large effect size reduction of substance-related problems starting at 3-month and at each subsequent time point through the 12-month follow-up.
Secondary Outcomes of Relationship Satisfaction and Relationship Stability
Female Relationship Satisfaction
For female-reported DAS, an autoregressive (QIC = 202.89) produced better fit versus an unstructured GEE model (QIC = 203.48) or exchangeable (QIC = 203.79) model. After controlling for other covariates, GEE analyses using an autoregressive correlation model showed there were not significant main effects of treatment condition or dual problem status. Interaction effects involving treatment condition were also non-significant. Turning to paired-sample t-tests, neither treatment condition showed significant changes in female baseline DAS versus DAS at time points following treatment (see Table 4).
Table 4.
Relationship Outcomes Observed M (SD) or %, Sample Size, and Effect Size Change from Baseline by Treatment Condition
| Female-reported Dyadic Adjustment Scale (DAS) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||
| Treatment | Baseline M (SD) | Post M (SD) | Post d | 3-month M (SD) | 3-month d | 6-month M (SD) | 6-month d | 9-month M (SD) | 9-month d | 12-month M (SD) | 12-month d |
| BCT + IBT | 106.27 (19.35) n = 30 |
108.52 (26.58) n = 28 |
.06 | 112.84 (25.29) n = 28 |
.23 | 111.48 (25.18) n = 29 |
.25 | 111.76 (25.85) n = 28 |
.15 | 108.56 (31.59) n = 26 |
.00 |
| IBT | 104.57 (22.16) n = 31 |
105.93 (25.74) n = 28 |
.02 | 107.45 (18.89) n = 25 |
.17 | 108.68 (23.09) n = 27 |
.04 | 105.84 (20.99) n = 22 |
.10 | 101.04 (22.85) n = 23 |
.31 |
|
| |||||||||||
| Male-reported Dyadic Adjustment Scale (DAS) | |||||||||||
|
| |||||||||||
| Treatment | Baseline M (SD) | Post M (SD) | Post d | 3-month M (SD) | 3-month d | 6-month M (SD) | 6-month d | 9-month M (SD) | 9-month d | 12-month M (SD) | 12-month d |
|
| |||||||||||
| BCT + IBT | 103.16 (15.69) n = 29 |
114.38a (21.14) n = 25 |
.62 | 114.49a (20.50) n = 27 |
.66 | 115.04a (25.64) n = 28 |
.64 | 114.60a (21.45) n = 27 |
.60 | 111.71b (14.78) n = 26 |
.50 |
| IBT | 101.65 (17.07) n = 31 |
106.14 (25.51) n = 29 |
.16 | 106.66 (18.47) n = 25 |
.26 | 101.50 (20.49) n = 26 |
.00 | 102.37 (23.56) n = 24 |
.10 | 102.70 (26.99) n = 23 |
.09 |
|
| |||||||||||
| Percentage Days Separated (PSEP) | |||||||||||
|
| |||||||||||
| Treatment | Baseline M (SD) | Post M (SD) | Post d | 3-month M (SD) | 3-month d | 6-month M (SD) | 6-month d | 9-month M (SD) | 9-month d | 12-month M (SD) | 12-month d |
|
| |||||||||||
| BCT + IBT | 2.81 (6.68) n = 30 |
2.63 (13.64) n = 30 |
.44 | 4.95 (16.12) n = 30 |
.22 | 3.95 (15.26) n = 30 |
.35 | 3.37 (18.25) n = 30 |
.44 | 9.52 (26.93) n = 30 |
.15 |
| IBT | 2.02 (6.41) n = 31 |
3.90 (17.21) n = 31 |
.06 | 18.68 (37.80) n = 31 |
.12 | 24.82 (43.10) n = 31 |
.19 | 26.70 (44.96) n = 30 |
.32 | 30.98 (45.33) n = 30 |
.40 |
Note. IBT = individually-based therapy. BCT + IBT = behavioral couples therapy plus IBT. Post = post-treatment.
This score shows a significant (p < .01, Bonferonni corrected) improvement vs. baseline.
p = .019 for comparison of this score vs. baseline. Cohen’s d effect sizes guidelines are small = 0.2, medium = 0.5, large = 0.8
Male Relationship Satisfaction
For the male-reported DAS, an autoregressive (QIC = 223.33) model produced better fit versus an unstructured (QIC = 223.85) and exchangeable (QIC = 223.85) GEE model. After controlling for other covariates, there was a significant, medium-to-large effect size difference across treatments, with male partners having higher DAS scores following treatment in BCT+IBT versus IBT. Higher percentage days of buprenorphine use was associated with higher male DAS scores (see Table 5). Paired sample t-tests showed that male partners in the BCT+IBT condition had significant, medium-to-large effect size improvements on baseline DAS versus DAS afte treatment, whereas male partners in the IBT condition did not demonstrate significant changes in DAS from baseline to following treatment (see Table 4).
Table 5.
Generalized Estimating Equation (GEE) Results for Relationship Outcomes During Follow-up
| Female-reported Dyadic Adjustment Scale (DAS) (N = 59) | ||||
|---|---|---|---|---|
|
| ||||
| Predictor | d | 95% CI | χ2 | p |
| Treatment condition | .283 | −.027, .593 | 3.204 | .073 |
| % days buprenorphine use | .076 | −.051, .203 | 1.387 | .239 |
| Therapist A vs. Therapist B | .071 | −.460, .602 | 0.068 | .794 |
| vs. Therapist C | −.221 | −.637, .196 | 1.076 | .299 |
| vs. Therapist D | .169 | −.398, .736 | 0.342 | .559 |
| vs. Therapist E | −.746 | −1.686, .193 | 2.423 | .120 |
| Dual problem couple | −.110 | −.451, .232 | 0.396 | .529 |
| Baseline female DAS | .587 | .406, .769 | 40.145 | <.001 |
| Time | −.030 | −.105, .045 | 0.605 | .437 |
|
| ||||
| Treatment × time | .051 | −.100, .203 | 0.443 | .506 |
| Treatment condition × dual problem couple | .096 | −.628, .821 | 0.068 | .794 |
|
| ||||
| Male-reported Dyadic Adjustment Scale (DAS) (N = 59) | ||||
|
| ||||
| Predictor | d | 95% CI | χ2 | p |
|
| ||||
| Treatment condition | .569 | .257, .880 | 12.800 | <.001 |
| % days buprenorphine use | .134 | .004, .264 | 4.103 | .043 |
| Therapist A vs. Therapist B | −.026 | −.563, .511 | 0.009 | .925 |
| vs. Therapist C | −.677 | −1.083, −.271 | 10.673 | .001 |
| vs. Therapist D | −.609 | −1.164, −.054 | 4.629 | .031 |
| vs. Therapist E | −.814 | −1.682, .055 | 3.371 | .066 |
| Baseline male DAS | .444 | .277, .612 | 27.021 | <.001 |
| Dual problem couple | −.293 | −.653, .068 | 2.563 | .111 |
| Time | −.045 | −.118, .028 | 1.443 | .230 |
|
| ||||
| Treatment × time | .021 | −.126, .167 | 0.076 | .782 |
| Treatment condition × dual problem couple | .142 | −.551, .835 | 0.162 | .688 |
|
| ||||
| Percentage Days Separated (PSEP) (N = 61) | ||||
|
| ||||
| Predictor | d | 95% CI | χ2 | p |
|
| ||||
| Treatment condition | −.470 | −.114, −.826 | 6.689 | .010 |
| % days buprenorphine use | −.040 | −.154, .074 | 0.483 | .487 |
| Therapist A vs. Therapist B | −.050 | −.614, .513 | 0.030 | .861 |
| vs. Therapist C | .481 | −.075, 1.037 | 2.876 | .090 |
| vs. Therapist D | .140 | −.437, .718 | 0.227 | .634 |
| vs. Therapist E | −.179 | −.812, .454 | 0.308 | .579 |
| Baseline % days separated | .214 | −.007, .435 | 3.615 | .057 |
| Dual problem couple | .194 | −.241, .629 | 0.763 | .382 |
| Time | .070 | .014, .125 | 6.058 | .014 |
|
| ||||
| Treatment × time | −.066 | −.176, .045 | 1.361 | .243 |
| Treatment condition × dual problem couple | −.402 | −1.229, .425 | 0.907 | .341 |
Note. Coding for treatment condition: 0 = individual-based treatment, 1 = behavioral couples therapy. Coding for dual problem couple: 0 = female but not male partner had substance use disorder, 1 = both partners had substance use disorder. Findings for main effects are displayed prior to entering interaction terms into the model. Cohen’s d effect sizes guidelines are small = 0.2, medium = 0.5, large = 0.8. To aid interpretation, the direction of the effects for PSEP is reversed, since PSEP is inversely transformed.
Percent Days Separated (PSEP) Measure of Relationship Stability
For PSEP, GEE showed the exchangeable model (QIC = 302.97) was superior to the autoregressive (QIC = 303.74) and unstructured (QIC = 306.78) models. Using an exchangeable correlation matrix, the GEE model showed a significant, small-to-medium effect size for treatment condition, along with a significant effect of time (see Table 5). Consistent with observed means (see Table 4), GEE models showed that couples in the BCT+IBT condition had significantly lower PSEP during follow-up versus those in the IBT condition. Although BCT+IBT was superior to IBT in the GEE models that accounted for the other covariates, paired sample t-tests did not reveal any significant differences for either treatment condition between baseline and follow-up PSEP.
Discussion
Extent of Support for Study Predictions
Primary substance-related outcomes provided partial support for predictions. Contrary to predictions, BCT+IBT was not superior to IBT in improving abstinence and reducing illicit drug use. Instead, we found that both BCT+IBT and IBT patients had significant (p < .01) large effect size improvements from baseline on each substance outcome examined, at post and at all follow-ups throughout 12-month follow-up (d > .8 for most time periods). Consistent with predictions, BCT+IBT showed a significant, large effect size (d = .85) advantage over IBT on fewer substance-related problems, and a significant time by treatment interaction showed that BCT+IBT produced more rapid declines of substance-related problems at post-treatment. Thus, BCT+IBT was not superior at improving abstinence and reducing illicit drug use but it did lead to less substance-related problems versus IBT.
Secondary outcomes of relationship satisfaction and relationship stability also provided partial support for study predictions that BCT+IBT would do better than IBT on these outcomes. First, relationship satisfaction of male partners on the DAS followed study predictions. During the 12-months following treatment, men who received BCT had significantly greater relationship satisfaction on the DAS than those whose female drug abusing partners received IBT only (p<.001, d=.57). Further, male partners in BCT+IBT had significant medium-to-large effect size improvements in DAS from baseline, at post and at all follow-ups throughout the 12-month follow-up period, whereas male partners in IBT did not improve significantly. Second, in contrast on female relationship satisfaction, there was a small effect size trend favoring BCT+IBT for female DAS, but this was not statistically significant (p = .07) and neither condition showed improvement versus baseline. Third, relationship stability followed study predictions. Couples in the BCT+IBT condition had significantly lower days separated during the 12-month follow-up than did couples in the IBT condition (p=.01, d=−.47).
The impact of dual problem couple status (which characterized nearly half of study patients) was examined in exploratory analyses. Dual problem couple status was not significantly associated with response to treatment overall or with differential response to BCT+IBT versus IBT. The present results are similar to Schumm et al. (2012) who found improvements in substance use outcomes following BCT, regardless of whether one or both partners exhibited SUD. These findings suggest it may be beneficial to involve in BCT a substance-abusing male partner who is willing to discuss his own substance use and support the female partner’s recovery efforts. However, more research with larger samples is needed.
The impact of buprenorphine use also was examined. Higher buprenorphine use was significantly associated (small effect size) with higher PDA, lower PDDU and InDUC, and higher male-reported DAS. Thus buprenorphine improved primary substance related outcomes and male relationship satisfaction. Future research should examine whether adding BCT as the counseling component of buprenorphine treatment leads to better outcomes for opioid patients.
Present Study Findings in Relation to Prior Studies
The present study did not show less substance use (PDA, PDDU) for BCT+IBT than IBT, which has been consistently found in the 4 prior studies of BCT with female patients (Fals-Stewart et al., 2006; McCrady et al., 2009; Schumm et al., 2014; Winters et al., 2002). Possible explanations for this discrepant finding should be noted. First, the only prior study of BCT with female drug-abusing patients (Winters et al., 2002) did not include women who used buprenorphine. In the present study, 27–33% of the women used buprenorphine, and buprenorphine use was significantly associated with less substance use. Buprenorphine use could have reduced the amount of variance in PDA and PDDU that would otherwise be accounted for by differences in the psychotherapy conditions. Second, lower dose of treatment also may have impacted substance use outcomes. Women in the present study had lower session attendance when compared to the earlier Schumm et al. 2014 study of BCT with alcoholic women (which had similar design, study team, setting, and 26 planned sessions). Women in the BCT+IBT conditions in the present vs the earlier study averaged 15 vs 21 sessions attended, and 67% vs 83% completed at least half of planned sessions. Further, in the Winters et al. (2002) study of BCT with drug-abusing women, those in the BCT+IBT condition averaged 39 sessions attended out of 56 planned sessions. Thus patients in the present study got a lower dose of treatment than in prior studies of BCT, and this may have contributed to lack of difference on substance use outcomes. Third, the Winters study, compared to the present study, had (a) more patients coerced to treatment by social service or criminal justice systems (35% vs < 10%), (b) fewer patients with current opioid dependence (40% vs 74%), (c) more patients taking naltrexone or disulfiram (25% vs 0%), and (d) longer duration of planned treatment (24 vs 13 weeks). Arguably, these factors may have contributed to less substance use for BCT in the Winters study.
Substance-related problems outcomes for BCT+IBT in the present study were consistent with prior studies showing fewer substance-related problems in BCT than in IBT (Fals-Stewart et al., 2006; Schumm et al., 2014; Winters et al., 2002). The findings showing superiority of BCT+IBT versus IBT on reducing substance-related problems may be explained by skills that couples learn in BCT to address relapses, improve communication, and improve problem-solving. These skills may help couples more effectively manage relapses, when they do occur, and improve couples’ abilities to work together to address substance-related problems.
Relationship outcomes in the present study were broadly consistent with prior research on BCT with female patients. First, relationship satisfaction outcomes for male partners in the present study showed more durable improvements than found in Winters et al. (2002), the only other study of BCT with female drug-abusing patients. Whereas superior outcomes for BCT only lasted through 6-months follow-up in Winters et al. (2002), we found that BCT+IBT had significant improvements and better outcomes than IBT throughout the entire 12-month follow-up period. The present study also showed similarly durable improvements through 12-month follow-up as were observed in 2 studies of BCT with female alcoholic patients (Fals-Stewart et al., 2006; Schumm et al., 2014). Second, the present finding that male partners had lower relationship satisfaction than female patients is consistent with other studies of drug-abusing women (Fals-Stewart, Birchler & O’Farrell, 1999; Winters et al. (2002). However, they differ from the larger literature for distressed couples without SUD, in which a typical pattern is for female partners to be more distressed when entering couple therapy. Fals-Stewart et al. (1999) specifically compared relationships of drug abusing women with those of distressed non-SUD couples and found that these opposite gender patterns did significantly differentiate these 2 types of couples. The present study findings may reflect that the male partner is typically the one in the couple that is more affected by the substance-related problems and the strains of being in a relationship with a woman with SUD (Schumm et al., 2014). Third, BCT+IBT had greater relationship stability than IBT, which is consistent with prior BCT research (O’Farrell et al., 1992). This points to a clinical need for BCT with women, because men are less willing to stay with a female drug abusing partner than vice versa (Greenfield et al., 2007).
Study Strengths and Limitations
Strengths included treatment fidelity ratings, high therapy satisfaction ratings, and reasonably high session attendance rates in both BCT+IBT and IBT suggesting they were equally credible and satisfying treatments, use of accepted outcome measures and collateral reports to reduce under-reporting, use of an intent-to-treat sample, accepted statistical analyses including an exploratory analysis of buprenorphine, low degree of missing data, and low attrition rates. Further, BCT+IBT was compared with a 12-step oriented individual counseling that has been shown to be efficacious in its own right (Crits-Christoph et al., 1999). Finally, nearly half the sample were dual problem couples, making this the first RCT of drug-abusing women to compare BCT vs. IBT and include such couples.
Limitations of the study also should be noted. First, the relatively modest sample size was the most important limitation. It lowered statistical power to detect significant effects and may have contributed to the lack of BCT+IBT superiority on substance use and on female relationship satisfaction. It resulted from the low recruitment rate (15% of potentially eligible patients in the present study vs 25–56% in the 4 other BCT studies with female patients – i.e. Fals-Stewart et al. 2006, McCrady et al. 2009, Schumm et al. 2014, Winters et al. 2002). Differences across studies in study site locations and initial screening methods (i.e., telephone, interview, questionnaire) make direct comparisons of enrollment rates difficult. However, because the site and initial screening method were the same for Schumm et al. 2014 study of alcoholic women and the present study, that provides a good way of investigating whether enrollment is lower for drug-abusing women and why. Comparison of these 2 studies showed that while the studies had similar percentages of women who were ineligible or who refused participation, the current study exhibited a lower percentage of potentially eligible women enrolled in the present study of drug-abusing women (15% vs 25%). The inability to reach patients after they completed the study screening questionnaire was the most prominent reason in explaining the lower enrollment rate for the present study. This was due most likely to the very high dropout rate in which patients filled out a study screening questionnaire at clinic intake, but then failed to return for treatment or reply to phone calls. Consistent with this explanation, we observed that many couples targeted for recruitment in the present study were clinically unstable dyads, with most drug abuse patients addicted to opioids. Many of these patients dropped out quickly and went back to using, before they could be engaged in study-based (or other) treatment. This was especially true when both members of the couple used drugs. These observations have implications for implementation of BCT with drug abusing women in SUD treatment settings. This suggests that additional interventions may be needed to improve treatment engagement among drug-abusing women. For example, it may be easier to engage opioid patients in BCT who, like many of those enrolled in the present study, have had recent intensive treatment and used buprenorphine.
Second, differences were found between therapists on adherence to the BCT protocol, and this may have impacted the findings, even though we controlled for therapist effects within the GEE models. Third, patients averaged over 10 days of non-study intensive SUD treatment in the 60 days prior to study treatment, so the present results may not generalize to samples that receive less intensive pre-study SUD treatment. Fourth, the present results may not generalize to more ethnically diverse samples, same sex couples, and couples in which both partners have SUD and only one partner is willing to do BCT – all of which were not included in the present study sample. Fifth, we did not include data on women’s mental health diagnoses, so we were unable to replicate McCrady et al. (2009) finding that superiority of BCT over IBT on drinking outcomes was stronger among women with AUD who had co-occurring mental health disorders.
Finally, our results also may not generalize beyond women who are agreeable to try either BCT or IBT. McCrady and colleagues (2011) found that when given a choice, women may be more prone to choose a treatment protocol that includes IBT due to a variety of factors, such as perceived lack of partner support and logistical issues. A recent RCT found that BCT plus IBT was equal to or slightly better than standalone BCT for women with AUD (McCrady et al., 2016). Hence, blending IBT with BCT, such as the format used in the present study, may be a way of addressing women’s preferences for IBT being a part of their treatment.
Conclusions
This study showed that BCT+IBT may have greater benefit than IBT in reducing drug-abusing women’s substance-related problems and in improving some aspects of relationship outcomes in terms of less days of separation and better male partner relationship satisfaction. This is only the second study to test BCT among drug-abusing women (Winters et al., 2002 was the other), and both studies showed that BCT+IBT produced less substance-related problems and better relationship outcomes than IBT. However, the current study did not show less substance use for BCT +IBT than IBT as was shown in the Winters et al. study and in most prior studies of BCT, possibly due to the relatively modest sample size and high levels of non-study opiate substitution therapy used by women in the present study. Further research is needed to examine the potential benefits and limitations of BCT for drug-abusing women.
Public Health Significance.
Couples therapy was compared with individual therapy for drug-abusing women. Couples therapy produced greater relationship satisfaction and stability and fewer substance-related problems. Both treatments had substantial substance use reductions. This suggests that either treatment is effective for reducing substance use, but couple therapy may be a more appropriate choice when also addressing substance-related problems and relationship issues.
Acknowledgments
This research was supported by grant R01DA025618 awarded to the first author by the National Institute on Drug Abuse and by the Department of Veterans Affairs. We gratefully acknowledge assistance from Keith Klostermann, Fay Larkin, Anne Gribauskas, and Leslie Reid.
Footnotes
Definition of dual problem couples was based on specific criteria for characterizing the male partner as having a current substance problem. Criteria from the baseline assessment were that the male partner met SCID criteria for current substance abuse or dependence (other than caffeine or nicotine) or that he reported heavy use of cannabis, cocaine, opioids, or alcohol on the Drug Use Frequency measure (DUF; O’Farrell, Fals-Stewart & Murphy, 2003). Determination of dual problem couple status was also based on clinician judgment in the intake interview and the initial therapy session. Of the 28 dual problem couples identified, 20 were classified based on the SCID and 5 were based on the DUF where they each reported daily cannabis use. For the remaining 3 couples, dual problem couple status was based mainly on clinician judgment. This typically involved males who reported more frequent and problematic substance use during the intake interview and initial couple session than on the SCID in the baseline assessment.
In accordance with the recruitment procedures approved by the study sites and the IRBs, female patients completed a self-report screening questionnaire at the time of intake at one study site (n=653), while those at the second smaller site completed the screening questionnaire with a study therapist at the time of referral to the research program (n=19).
About one-sixth (16%, n=22) of the 140 prospective participants who refused to participate simply stated that they were not interested with no further details offered. The remaining participants who refused provided a variety of reasons for their lack of interest. The most common reason (31%, n=43/140) concerned the male partners’ inability to participate either because he was not interested (n=31) or he was too busy/his schedule did not allow (n=12). One- quarter (25%, n=35) of the female patients were not interested in the treatment because they were either planning on attending other treatment (n=22) or they were not planning on attending any further treatment (n=13). The other reasons mentioned in descending frequency of occurrence are as follows: female patient was too busy or felt time commitment was too great (n=22), female patient did not want her partner in treatment (n=9), female patient only wanted couples treatment (n=3), female patient wanted to receive treatment at a different agency (n=2), female patient lived too far away (n=2), medical concern prevented attendance (n=1), and an impending jail sentence (n=1).
We also explored the effect of adding a quadratic time function to the GEE models. However, the quadratic effect of time was non-significant for all models, and the addition of a quadratic effect of time did not improve model fit in any model.
The mean number of missing urine specimens during the treatment perioddid not differ by treatment condition (BCT+IBT, M = 5.4, SD = 4.4; IBT, M = 5.5, SD = 4.5; t(59) = 0.16, p =.987).
The mean number of missing urine specimens during the follow-up period did not differ by treatment condition (BCT+IBT, M = 0.5, SD = 1.0; IBT, M = 0.9, SD = 1.2; t(59) = 1.4, p =.166).
Contributor Information
Timothy J. O’Farrell, Families and Addiction Program, VA Boston Healthcare System and Harvard Medical School, Dept. of Psychiatry
Jeremiah A. Schumm, School of Professional Psychology, Wright State University
Marie M. Murphy, Families and Addiction Program, VA Boston Healthcare System and Harvard Medical School, Dept. of Psychiatry
Patrice M. Muchowski, AdCare Hospital of Worcester, Inc
References
- Attkisson CC, Greenfield TK. The UCSF client satisfaction scales: I. The client satisfaction questionnaire-8. In: Maruish ME, editor. The use of psychological testing for treatment planning and outcomes assessment. Mahwah, NJ: Lawrence Erlbaum Associates Publishers; 2004. pp. 1333–1346. [Google Scholar]
- Cohen J. Statistical power analysis for the social sciences. 2nd. Hillsdale, NJ: Lawrence Erlbaum; 1988. [Google Scholar]
- Crits-Christoph P, Siqueland L, Blaine J, Frank A, Luborsky L, Onken L, Beck A. Psychosocial treatment for cocaine dependence: National Institute on Drug Abuse collaborative cocaine treatment study. Archives of General Psychiatry. 1999;56:493–502. doi: 10.1001/archpsyc.56.6.493. [DOI] [PubMed] [Google Scholar]
- Fals-Stewart W, Birchler GR, Kelley ML. Learning sobriety together: A randomized clinical trial examining behavioral couples therapy with alcoholic female patients. Journal of Consulting and Clinical Psychology. 2006;74:579–591. doi: 10.1037/0022-006X.74.3.579. [DOI] [PubMed] [Google Scholar]
- Fals-Stewart W, Birchler GR, O’Farrell TJ. Drug abusing patients and their partners: Dyadic adjustment, relationship stability, and substance use. Journal of Abnormal Psychology. 1999;108:11–23. doi: 10.1037//0021-843x.108.1.11. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders. Washington, DC: American Psychiatric Press; 1996. [Google Scholar]
- Greenfield SF, Brooks AJ, Gordon SM, Green CA, Kropp F, McHugh RK, Miele GM. Substance abuse treatment entry, retention, and outcome in women: A review of the literature. Drug and Alcohol Dependence. 2007;86:1–21. doi: 10.1016/j.drugalcdep.2006.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall SM, Delucchi K, Velicer W, Kahler C, Ranger-Moore J, Hedeker D, Niaura R. Statistical analysis of randomized trials in tobacco treatment: Longitudinal designs with dichotomous outcome. Nicotine & Tobacco Research. 2001;3:193–202. doi: 10.1080/14622200110050411. [DOI] [PubMed] [Google Scholar]
- Jones HE, Tuten M, O’Grady KE. Treating the partners of opiate-dependent pregnant patients: Feasibility and efficacy. The American Journal of Drug and Alcohol Abuse. 2011;37:170–178. doi: 10.3109/00952990.2011.563336. [DOI] [PubMed] [Google Scholar]
- McCrady BS, Epstein EE, Cook S, Jensen NK, Hildebrant T. A randomized trial of individual and couple behavioral alcohol treatment for women. Journal of Consulting and Clinical Psychology. 2009;77:243–56. doi: 10.1037/a0014686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCrady BS, Epstein EE, Cook S, Jensen NK, Ladd BO. What do women want? Alcohol treatment choices, treatment entry, and retention. Psychology of Addictive Behaviors. 2011;25:521–529. doi: 10.1037/adb0024037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCrady BS, Epstein EE, Hallgren KA, Cook S, Jensen NK. Women and alcohol dependence: A randomized trial of couple versus individual plus couple therapy. Psychology of Addictive Behaviors. 2016;30:287–299. doi: 10.1037/adb0000158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meis LA, Griffin JM, Greer N, Jensen AC, MacDonald R, Carlyle M, Wilt TJ. Couple and family involvement in adult mental health treatment: A systematic review. Clinical Psychology Review. 2013;33:275–286. doi: 10.1016/j.cpr.2012.12.003. [DOI] [PubMed] [Google Scholar]
- Mercer D, Woody GE. An Individual Drug Counseling Approach to Treating Cocaine Addiction: The Collaborative Cocaine Treatment Study Model. Rockville, MD: National Institute on Drug Abuse; 1999. (Manual 3: Therapy Manuals for Drug Addiction). [Google Scholar]
- O’Farrell TJ, Clements K. Review of outcome research on marital and family therapy in treatment of alcoholism. Journal of Marital and Family Therapy. 2012;38:122–144. doi: 10.1111/j.1752-0606.2011.00242.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Farrell TJ, Cutter HSG, Choquette KA, Floyd FJ, Bayog RD. Behavioral marital therapy for male alcoholics: Marital and drinking adjustment during the two years after treatment. Behavior Therapy. 1992;23:529–549. [Google Scholar]
- O’Farrell TJ, Fals-Stewart W. Behavioral couples therapy for alcoholism and drug abuse. New York: Guilford Press; 2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powers MB, Vedel E, Emmelkamp PMG. Behavioral couples therapy (BCT) for alcohol and drug use disorders: A meta-analysis. Clinical Psychology Review. 2008;28:952–962. doi: 10.1016/j.cpr.2008.02.002. [DOI] [PubMed] [Google Scholar]
- Schumm JA, O’Farrell TJ, Burdzovic Andreas J. Drinking outcomes following behavioral couples therapy for couples in which both partners have a current alcohol use disorder. Alcoholism Treatment Quarterly. 2012;30:407–421. doi: 10.1080/07347324.2012.718963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schumm J, O’Farrell TJ, Kahler C, Murphy M, Muchowski PM. A randomized clinical trial of behavioral couples therapy versus individually-based treatment for women with alcohol dependence. Journal of Consulting and Clinical Psychology. 2014;82:993–1004. doi: 10.1037/a0037497. http://dx.doi.org/10.1037/a0037497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Timeline followback user’s guide: a calendar method for assessing alcohol and drug use. Toronto, Canada: Addiction Research Foundation; 1996. [Google Scholar]
- Spanier GB. Dyadic adjustment scale: User’s manual. Toronto: Multi-Health Systems; 2001. [Google Scholar]
- Tonigan JS, Miller WR. The inventory of drug use consequences (InDUC): Test retest stability and sensitivity to detect change. Psychology of Addictive Behaviors. 2002;16:165–168. doi: 10.1037//0893-164X.16.2. [DOI] [PubMed] [Google Scholar]
- Tuten M, Jones HE. A partner’s drug-using status impacts women’s drug treatment outcome. Drug and Alcohol Dependence. 2003;70:327–330. doi: 10.1016/s0376-8716(03)00030-9. [DOI] [PubMed] [Google Scholar]
- Winters J, Fals-Stewart W, O’Farrell TJ, Birchler GR, Kelley ML. Behavioral couples therapy for female substance-abusing patients: Effects on substance use and relationship adjustment. Journal of Consulting and Clinical Psychology. 2002;70:344–355. doi: 10.1037//0022-006x.70.2.344. [DOI] [PubMed] [Google Scholar]


