Abstract
Introduction
Triage is the process of sorting patients based on the level of acuity to ensure the most severely injured and ill patients receive timely care before their condition worsens. The South African Triage Scale (SATS) was developed out of a need for an accurate and objective measure of urgency based on physiological parameters and clinical discriminators that is easily implemented in low resource settings. SATS was introduced in the emergency center (EC) of Komfo Anokye Teaching Hospital (KATH) in January 2010. This study seeks to evaluate the accurate use of the SATS by nurses at KATH.
Methods
This cross-sectional study was conducted in the EC at KATH in Kumasi, Ghana. Patients 12 years and over with complete triage information were included in this study. Each component of SATS was calculated (i.e. for heart rate of 41–50, a score of 1 was given) and summed. This score was compared to the original triage score. When scores did not equate, the entire triage record was reviewed by an emergency physician and an advanced practice emergency nurse separately to determine if the triage was appropriate. These reviews were compared and consensus reached.
Results
52 of 903 adult patients (5.8%) were judged to have been mis-triaged by expert review; 49 under-triaged (sent to a zone that corresponded to a lower acuity level than they should have been, based on their vital signs) and 3 over-triaged. Of the 49 patients who were under-triaged, 34 were under-triaged by one category and 7 by two categories.
Conclusion
Under-triage is a concern to patient care and safety, and while the under-triage rate of 5.7% in this sample falls within the 5–10% range considered unavoidable by the American College of Surgeons Committee on Trauma, concentrated efforts to regularly train triage nurses to ensure no patients are under-triaged have been undertaken. Overall though, SATS has been implemented successfully in the EC at KATH by triage nurses.
Abstract
Introduction
Le triage est le processus consistant à classer les patients selon le degré de gravité afin de s’assurer que les patients les plus gravement blessés et malades sont rapidement pris en charge avant que leur état ne s’aggrave. L’échelle de triage sud-africaine (SATS) été développée en raison de la nécessité de disposer d’une mesure précise et objective du degré d’urgence à l’aide de paramètres physiologiques et de discriminants cliniques, mesure aisément mise en oeuvre dans des environnements caractérisés par un manque de ressources. Le SATS a été introduit dans le service d’urgences de l’hôpital universitaire Komfo Anokye (KATH) en janvier 2010. L’objectif de cette étude est d’évaluer l’usage précis du SATS par les infirmières du KATH.
Méthodes
Cette étude transversale a été menée au service d’urgences du KATH à Kumasi, au Ghana. Des patients âgés de plus de 12 ans, pour lesquels les informations de triage étaient complètes, ont étéintégrés à cette étude. Chaque composante du SATS a été calculée (par ex., pour une fréquence cardiaque comprise entre 41 et 50, une note de 1 a été attribuée) et additionnée. Cette note a été comparée à la note de triage d’origine. Quand les notes n’ étaient pas les mêmes, l’intégralité du dossier de triage était étudiée séparément par un urgentiste et une infirmiére urgentiste de pratique avancée afin de déterminer si le triage était approprié. Ces révisions ont été comparées en vue de parvenir à un consensus.
Résultats
52 Patients adultes sur 903 (5.8%) ont été considérés comme ayant fait l’objet d’une erreur de triage par l’ étude menée par les professionnels; 49 ont été considérés «sous-triés» (envoyés vers une catégorie de prise en charge correspondant à un degré de gravité inférieur à ce qui aurait dû être choisi, d’aprés les signes vitaux), et trois ont été sur-triés. Sur les 49 patients «sous-triés», 34 ont été «sous-triés» d’une catégorie, et sept de deux catégories.
Conclusion
Le «sous-triage» pose problème en termes de prise en charge et de sécurité des patients, et si le taux de «sous-triage» de 5.7% enregistré dans cet échantillon est considéré comme inévitable par le Comité de traumatologie de l’American College of Surgeons, des efforts intensifs ont été réalisés afin de former régulièrement les infirmières chargées du triage pour s’assurer qu’aucun patient n’était «sous-trié». Cependant, d’un point de vue général, les infirmiéres de triage sont parvenues à mettre le SATS en oeuvre avec succès au service d’urgences du KATH.
Introduction
Triage is the process of sorting patients according to acuity. In the emergency centers (EC), the purpose of triage is to effectively sort patients based on their immediate presentation in order to ensure the most severely injured and ill patients receive timely care before their condition worsens.1 Triage tools developed and widely used in the developed world are not applicable to developing country settings.2,3 The South African Triage Scale (SATS) was developed out of a need for an accurate measure of urgency based on physiological parameters and clinical discriminators that is easily adopted in low resource settings.4 The SATS was designed to be used by a range of healthcare providers due to the low number of nurses and doctors and nurses in South Africa. Nurse-led triage has been shown to have high levels of sensitivity and specificity in Brazil5 and Malawi.6 Further, nurse-led triage has been shown to reduce waiting times for emergency patients in South Africa.7
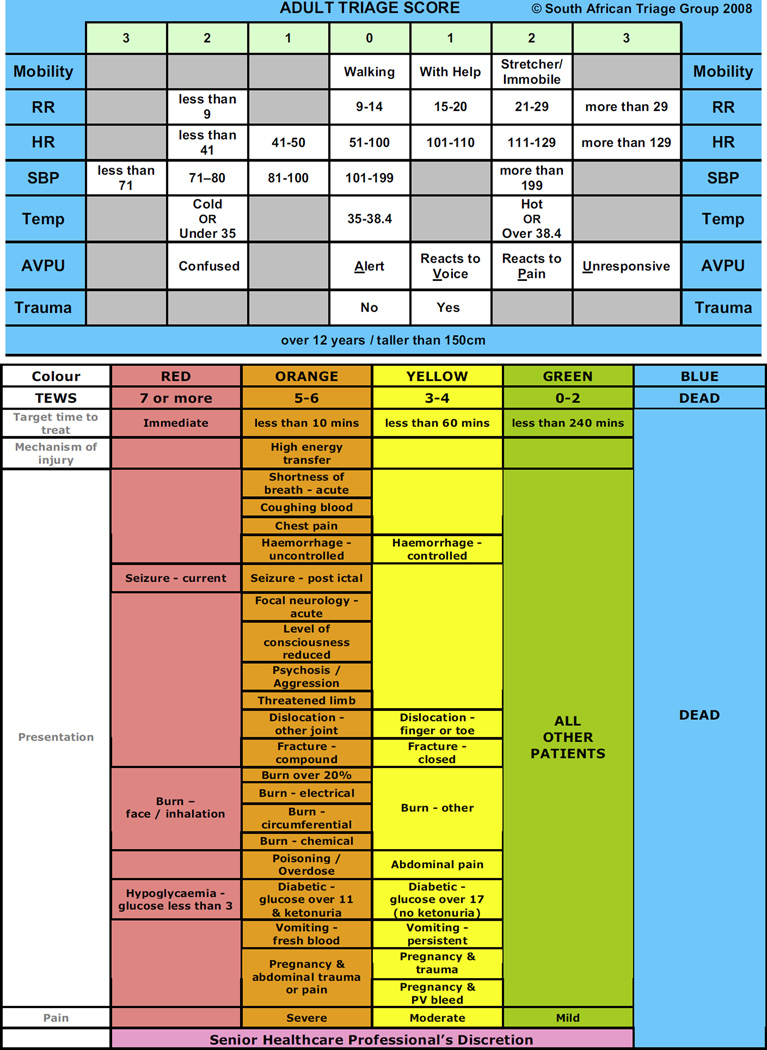
Versions of SATS exist for adults, children and infants. This current study focuses on the adult version, meant for those over 12 years of age or 150 cm in height.8 Physiologic aspects of triage are measured via the Triage Early Warning Score (TEWS). Patient presentation variables are scored on a scale of 0–3 based on established parameters for vital signs (temperature, heart rate, respiration and systolic blood pressure) in addition to level of consciousness, mobility and exposure to trauma (Fig. 1). The TEWS is a good fit with an emergency setting as it allows for accurate and uniform assessment of both medical and trauma patients,7 it is fairly low resource, requiring only a blood pressure cuff and a thermometer, and its scoring system facilitates communication between the healthcare team.8
Figure 1.
The South African Triage Scale; RR, respiration rate; HR, heart rate; SBP, systolic blood pressure; AVPU, awake verbal pain unresponsive; TEWS, triage early warning score.
The emergency center at Komfo Anokye Teaching Hospital (KATH) in Kumasi, Ghana, represents the first formalized emergency center in West Africa. Opened in 2009, the EC serves as the regional training and referral center for injury and trauma management. A formal system of post-graduate emergency medical education was established at the EC in October 2009. A specialization in emergency nursing was subsequently implemented in 2012.
Prior to the introduction of emergency medicine, the EC was split into three separate areas; the medical emergency unit, staffed by internal medicine clinicians, the trauma unit, staffed by traumatologists, and a general surgical area. Upon arrival, patients were judged by a nurse to be either medical, surgical or orthopedic. There was no objective triage occurring at this time. This process caused delays in patients receiving definitive interventions. After studying a variety of triage methods in place in other settings, the South African Triage Scale (SATS)3 was implemented in July 2009, beginning with emergency center training seminars for physicians and nurses, followed by a guided implementation process. Currently, nurses are trained in SATS during their initial EC orientation and then provided with periodic refresher trainings. International EM physicians trained emergency medicine residents to conduct the initial training of nurse leaders.9 At the end of training, nurses took a paper-based exam to assess comfort with and ability to implement the material. However, practical applicability had not been assessed prior to this study.
In February 2010, the patient flow through the EC was restructured to align the location of patients with the available resources. For example, the highest acuity patients are now seen in the red zone, where necessary equipment and supplies to treat these patients are located.
With the conversion of the EC to nurse-led triage, with the SATS as the guiding instrument, there was a need to ensure that the triage system was being correctly implemented. Therefore, the purpose of this paper is to objectively evaluate the accurate use of the SATS by emergency center nurses at Komfo Anokye Teaching Hospital in Ghana using secondary data analysis of an existing dataset.
Methods
The cross-sectional study, from which the presently analyzed data were drawn, was conducted in the EC at KATH. This tertiary care facility provides injury and medical emergency care to the 1.4 million residents of Kumasi and the 4.4 million who live in the surrounding Ashanti region. The emergency center at KATH treats 27,000 patients/year.
When patients arrive to the EC, they are interviewed by a triage nurse to assess presenting complaint, mobility and AVPU score (A = alert, V= responds to voice, P= responds to pain, U = unresponsive). Pulse rate, blood pressure, respiratory rate and temperature are measured and recorded. The Triage Early Warning Scale (TEWS) score7 is then matched to a SATS discriminator list, and an appropriate triage color is assigned. This information is routinely noted by the triage nurse in the chart and is part of regular patient care.
Data for this analysis come from an existing dataset that was collected between 13 July 2011 and 12 August 2011. All patients who present to the KATH EC for treatment were surveyed as to their medical and personal characteristics. Information regarding their vital signs at the time they were triaged was extracted from the patient chart and forms the basis on which the present analysis is conducted.
The TEWS for each patient was calculated by a series of algorithms in Excel. For example, for heart rate of 100–110, a score of 1 was given; while a heart rate of 111–120 was given a score of 2 (Fig. 1). These individual scores were then summed by Excel. This series of algorithms sought to replicate the process undertaken by a triage nurse. The calculated TEWS was compared to the score recorded by the triage nurse. For those scores that did not match, three authors, one an emergency nurse, the director of nursing services at KATH, and one emergency physician, (SAB, PA, RAO) reviewed the information separately and determined whether the patient had been triaged correctly or not. The reason for the discrepancy documented by the nurse, if available, was reviewed. For example, there are some patients who, based only on vital signs would have been triaged to Green, but since all suturing is done in the EC, the patient was sent to the Yellow area of the center. If this reasoning was not recorded then the recorded chief complaint was reviewed to evaluate whether the difference could be explained. These separate reviews were then compared together and discrepancies were discussed until agreement was reached.
Study procedures were approved and conducted in compliance with the Committee on Human Research Publication and Ethics, School of Medical Sciences, Kwame Nkrumah University of Science and Technology and the University of Michigan Institutional Review Board for Human Subjects guidelines.
Results
The total sample size was 909 adults. Five hundred and forty-six (546) of them i.e. 60% were males, and 331 were females. During the study period, 63 (7.1%) were triaged to Red, 260 (29.4%) were triaged to Orange, 539 (61%) to Yellow and 3 (.3%) to Green. The most common chief complaint was abdominal pain (n = 126, 14.3%), followed by pain (n = 120, 13.6%). The mean age of our adult sub-sample was 43.99 years (s.d. 19.7). 355 (40.1%) of the patients included were presenting for the treatment of an injury.
Of all the patients, 173 (19%) were determined by the Excel® program to have been incorrectly triaged. After expert review, 52 (5.7%) patients were judged to have been wrongly-triaged by the triage nurse; 49 under-triaged (sent to a zone that corresponded to a lower acuity level than they should have been, based on their vital signs) and 3 over-triaged. Many of those who had been deemed by Excel to have been mis-triaged contained missing information, which is why they were identified as being incorrectly triaged.
Of the 49 patients who were identified to have been under-triaged, 28 (53.8%) had been triaged to Yellow when they should have been sent to Orange, 14 (26.9%) were triaged to Orange when they should have been seen in Red, 6 (11.5%) were triaged to Yellow when they should have been triaged to Red and one (1.9%) was determined to be Green when they should have been sent to Orange.
Discussion
Triage is an important way to systematically sort patients so those who are the most acutely ill or injured receive timely care before their condition worsens.1 Accurate, objective triage has the potential to reduce patient waiting times, and decrease time to physician intervention. In a setting such as Ghana where there are low physician-to-population ratios (.9 per 10,000 population10), it is important to utilize the available health care professionals in a manner most appropriate to providing timely and specialized treatment. At Komfo Anokye, while there was immediate resistance to the idea of not involving the physicians in the triage process, the implementation of nurse-led triage appears successful.
While under-triage is a concern to patient care and safety, the under-triage rate of 5.7% in this sample falls within the 5–10% range considered unavoidable by the American College of Surgeons Committee on Trauma.11 Conversely, over-triage, while not posing threats to patients, will stretch already limited healthcare resources. It has been suggested that an over-triage rate of up to 50% may be required to keep under-triage at an acceptable rate11(ACSCOT, 1999). In this sample, less than 1% of patients were over-triaged.
The result of 5.7% of patients being under-triaged is higher than the 4.4% under-triage rate reported in a rural emergency center in South Africa,12 and the over-triage rate of less than 1% in our study is lower than the 4.3% reported.
The low rate of over-triage in our sample is worrisome given the emphasis during training of the importance of erring on the side of over-triage. The finding of 17 times as many patients being under-triaged as opposed to over-triaged is troublesome, especially given the way the KATH EC is positioned in the larger hospital where only patients triaged to Yellow, Orange and Red are seen in the EC. Patients triaged to Green are sent to the outpatient general clinic (Polyclinic) where they will certainly encounter long waiting times and may not be evaluated that day. The outpatient department is also staffed by the family physicians, and not by trained emergency physicians. Similar triage training has been conducted with staff in the outpatient area. Although the rate of triage is low, they do have the ability to re-asses the patients they receive and send them back to the EC to be evaluated by emergency physicians, if they feel this is necessary. In this analysis there was only one out of the 909 patients in our sample who was incorrectly triaged to Green when they should have, according to their recorded vital signs, been seen in the emergency center. However, even with one patient, this should never happen and could lead to significant delays in the appropriated delivery of care. The construction of the EC brought with it some restructuring of resources and departments. The outpatient general clinics at KATH are now staffed by the departments of Family Medicine and Internal Medicine, and thus any patient with a potential surgical issue is to be up-triaged to stay and receive management in the EC. However, given the lack of patients found in this study to be up-triaged, this issue may need to be stressed in future nurse trainings. To address this issue, nursing leadership at KATH has initiated plans to provide refresher trainings to all nurses in appropriate triage quarterly.
As this is a secondary data analysis of an existing dataset, only information collected for the original study could be used. There were some patients for whom it was not possible to ascertain whether or not they had been correctly triaged due to missing information, and it is not possible to assess whether data is missing because SATS is too complicated for this setting. Further, there were no data collected on the individuals conducting the triage at any particular time. Thus, it is not possible to determine whether it is one triage nurse who is mis-triaging multiple patients or a general low level of mis-triage evenly spread out among all triage nurses.
Although SATS is an algorithm, there is an important aspect of nursing judgment. The level of nursing documentation concerning their reasons for adjusting the calculated triage score was often missing, which is not necessarily indicative of a lack of judgment being undertaken. As triage was not a focal point of the initial study, we often could not ascertain the reasons why nurses made the judgments they did.
There is a need to objectively evaluate and validate the effectiveness of SATS to appropriately triage patients presenting to the EC at KATH. The predictive validity of SATS at KATH has not been established by this study and is an important area for further research.
Conclusion
Nurses at the emergency center at Komfo Anokye have correctly implemented objective and systematic triage using the South African Triage Scale. This important achievement provides a strong basis in the advancement of a functional emergency center. Before this system was put in place, there was no objective triage being undertaken. With an objective measure of acuity, the center is now able to provide each patient with appropriately timed interventions and management. The result of this study point toward the possibility of training nurses and physicians working in emergency centers in regional, district and teaching hospitals throughout Ghana, has the potential to reduce mortality and morbidity and improve efficiency and the delivery of emergency medical services.6
The results of this study have also led an effort to increase triage refresher training provided to nurses at the entry points of KATH. There is also the recognized need for further study examining patient outcomes following appropriate triage.
Although there are many systems of triage implemented in the developed world, there are few that have been systematically implemented and evaluated in developing countries. This study is a first step to assess the applicability and validity of the South African Triage Scale in Ghana, a country that is leading sub-Saharan Africa in the development of emergency medicine.
African relevance.
Triage scales used in more developed areas may not be relevant to Africa.
This low-cost quality assurance study was able to identify needs for further training.
Implementing objective triage is an important part of the development of emergency medicine.
Acknowledgments
This work was supported by the Award Number R24TW008899 from the Fogarty International Centre, National Institutes of Health, and USA. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Fogarty International Centre or the National Institutes of Health.
Footnotes
Conflict of interest
The authors state they have no conflicts of interest.
References
- 1.Twomey M, Wallis LA, Myers JE. Limitations in validating emergency department triage scales. Emerg Med J. 2007;24:477–479. doi: 10.1136/emj.2007.046383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gottschalk SB, Wood D, DeVries S, Wallis LA, Bruijins S. The cape triage score: a new triage system. Emerg Med J. 2006;23:149–153. doi: 10.1136/emj.2005.028332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gove S, Tamburlini G, Molyneux E, Whitesell P, Campbell H. Development and technical basis of simplified guidelines for emergency triage assessment and treatment in developing countries. Arch Dis Child. 1999;81:473–477. doi: 10.1136/adc.81.6.473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.South African Triage Group. A division of the Emergency Medicine Society of South Africa. South African Triage Score (SATS) 2008 < www.triagesa.co.za>. [Google Scholar]
- 5.Tamburlini G, Di Mario S, Maggi RS, Vilarim JN, Gove S. Evaluation of guidelines for emergency triage assessment and treatment in developing countries. Arch Dis Child. 1999;81:478–482. doi: 10.1136/adc.81.6.478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Robertson MA, Molyneux EM. Triage in the developing world – can it be done? Arch Dis Child. 2001;85:208–213. doi: 10.1136/adc.85.3.208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bruijns SR, Wallis LA, Burch VC. Effect of introduction of nurse triage on waiting times in a South African emergency department. Emerg Med J. 2008;25:395–397. doi: 10.1136/emj.2007.049411. [DOI] [PubMed] [Google Scholar]
- 8.Wallis LA, Gottschalk SB, Wood D, Bruijns SDe, Vries S Balfour CCape Triage Group. The Cape Triage Score: a triage system for South Africa. S Afr Med J. 2006;96:53–56. [PubMed] [Google Scholar]
- 9.Rominski SD, Bell SA, Yeboah D, Sarna K, Hartney H, Oteng RA. Skills and educational needs of accident and emergency nurses in Ghana: an initial needs analysis. Afr J Emerg Med. 2011;1:119–125. doi: 10.1016/j.afjem.2011.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kaiser Family Foundation. [accessed May 14, 2013]; at < http://www.kff.org/global-indicator/physicians/>. [Google Scholar]
- 11.American College of Surgeons Committee on Trauma. Resources for optimal care of the injured patient. Chicago: American College of Surgeons; 1999. p. 98. [Google Scholar]
- 12.Rosedale K, Smith ZA, Wood DD. The effectiveness of the South African Triage Score (SATS) in a rural emergency department. S Afr Med J. 2011;101(8):537–540. [PubMed] [Google Scholar]