Abstract
The present study aimed to detect early changes in the concentration of matrix metalloproteinase-9 (MMP-9), matrix metalloproteinase-2 (MMP-2) and tissue inhibitor of metalloproteinase-1 (TIMP-1) in a rat model of brain injury combined with traumatic heterotopic ossification (HO). A total of 132 male Sprague-Dawley rats were used to establish the experimental and control groups. Anatomy and sample collection were conducted on postoperative days 1, 2, 3, 4, 5, 6 and 7. Hematoxylin and eosin and immunohistochemical staining were performed for local tissues. MMP-9, MMP-2 and TIMP-1 levels and gene expression level were measured by ELISA and reverse transcription-quantitative polymerase chain reaction. Radiological investigation of the rat lower limbs was conducted at weeks 5 and 10 following modeling to observe the occurrence of HO. The incidence of HO for rats in the experimental group was higher compared with the control group. The serum MMP-9 levels of the experimental group were notably higher on postoperative days 5–7 compared with the control group. The MMP-9 gene expression of the experimental group was higher on postoperative days 3–7 compared with the control group. The TIMP-1 gene expression levels were markedly higher compared with the control group at each time point. Thus, an increase in inflammatory response is closely associated with brain injury, in addition to an increase in the number of inflammatory cells with the incidence of HO. The pathological elevation of MMP-9 and the altered dynamic equilibrium between MMP-9 and TIMP-1 contributed to the degradation, remodeling and calcification of the extracellular matrix, resulting in the induction of osteoblast precursor cells in HO. MMP-9 is a predictive marker of HO.
Keywords: heterotopic ossification, brain injury, matrix metalloproteinase-9, matrix metalloproteinase-2, tissue inhibitor of metalloproteinase-1
Introduction
Heterotopic ossification (HO) indicates new bone formation in non-ossifying tissues and can occur in numerous parts of the body following injury. HO is different from calcium deposition and new bone formation in bone healing and leads to abnormal joint motion affecting quality of life and employment prospects of the individual. The occurrence of HO is influenced by a number of factors, including brain injuries and burns (1,2). The incidence rate of HO is 20–25% following spinal injury, 18–35% of which is associated with restricted joint motion (3). The incidence rate of HO is 10–20% following closed trauma to the head, 18–35% of which is associated with restricted joint motion (4).
Rodenberg et al (5) reported that matrix metalloproteinase-9 (MMP-9) was a biomarker of the early reorganization of the extracellular matrix (ECM) and had a specific diagnostic function in the early stage of HO. Oliveira et al (6) proposed that MMPs were involved in bone remodeling and angiogenesis and were considered as a potential biomarker of HO.
The present study investigated rat models of Feeney's freefall-induced brain injury combined with Achilles tendon rupture-induced HO. It analyzed the altered curves of MMP-9, MMP-2 and tissue inhibitor of metalloproteinase-1 (TIMP-1) in addition to the curves of gene expression. It also explored the pathogenesis of HO.
Materials and methods
Experimental animals, main reagents and instruments
A total of 132 male Sprague-Dawley rats aged 4–5 weeks with a mean weight of 135.0±6.5 g, were purchased from Shanghai Laboratory Animal Research Center (Shanghai, China). Housing conditions were controlled for temperature (23±2°C) and humidity (40%), andon a 12 h light/dark cycle (on at 6:00 a.m., off at 6:00 p.m.). The rats were raised in the Animal Center of Institute of Biomedical Sciences of East China Normal University (Shanghai, China) for 1 week. The East China Normal University animal care and use committee approved all experimental protocols. ELISA kits for MMP-9 MMP-2 and TIMP-1 were purchased from Cusabio Biotech Co., Ltd. (Wuhan, China). MMP-9 antibodies (cat. no. ab119906) were purchased from Abcam (Cambridge, MA, USA) and the MMP-2 antibody (cat. no. 10373-2-AP) was from Proteintech (Proteintech Group, Inc., Chicago, IL, USA). TIMP-1 (cat. no. orb195994) was purchased from Biorbyt, Ltd. (Cambridge, UK) and goat anti-rabbit antibody (cat. no. 111-005-045) from Jackson ImmunoResearch Laboratories, Inc. (West Grove, PA, USA). TRIzol was purchased from Invitrogen (Thermo Fisher Scientific, Inc., Waltham, MA, USA) and the reverse transcription kit from Takara Biotechnology Co., Ltd. (Dalian, China). The polymerase chain reaction (PCR) kit (SYBR® Premix Ex Taq™ II) was purchased from Takara Biotechnology Co., Ltd. and the X-ray machine was from Kodak (Rochester, NY, USA). The light microscope was from Olympus Corporation (Tokyo, Japan) and the micro spectrophotometers were from NanoDrop (Thermo Fisher Scientific, Inc., Wilmington, DE, USA).
Animal model building and grouping
Traumatic brain injury model
The rats were anesthetized by a peritoneal injection of chloral hydrate (10%, 0.2–0.3 ml/100 g), followed by the preparation of the skin for surgery. Routine disinfection was conducted using iodine and ethanol. The rats were covered by a piece of scarf with a hole and the scalp was removed using Feeney's freefall-induced method (7). A bone window with a diameter of 5 mm between the anterior and posterior fontanelles on the right parietal lobe of the rat was made using a dental drill, keeping the dura intact. A 20 g weight was loaded onto the free fall instrument and dropped from a height of 35 cm to hit the rat, in order to establish the model of mild traumatic brain injury (MTBI). Amoxicillin (5 mg; Guangzhou Baiyunshan Medicine Co., Ltd., Guangzhou, China) was smeared on the wound following the injury and the incision was closed with a 4–0 silk suture (Fig. 1A). Following the brain injury, neurobehavioral scores were used to categorize the MTBI model.
Figure 1.
(A) Amoxicillin (5 mg) was smeared on the wound following surgery and (B) the incision was closed with a standard 4–0 silk suture.
HO model induced by Achilles tendon ruptures
The rats were anesthetized with a peritoneal injection of chloral hydrate (10%; 0.3–0.35 ml/100 g; Takara Biotechnology Co., Ltd., Dalian, China), followed by the preparation of the skin of the posterolateral right leg for surgery. Iodine and ethanol were used to disinfect the surgical and nearby areas. The Achilles tendon was exposed with a longitudinal incision in the right hind limb and clamped with forceps eight times to create the wound. The Achilles tendon was completely severed at the midpoint without any suture. The incision was closed with a 4–0 silk suture (Fig. 1B).
Trauma control model
The rats were anesthetized with a peritoneal injection of chloral hydrate (0.2–0.3 ml/100 g), followed by the preparation of the skin for surgery. The Achilles tendon was exposed in the posterolateral right hind leg and the incision was closed without any treatment.
Animal model grouping
A total of 132 rats were divided into the experimental and control groups, comprising 66 rats each, 10 rats were randomly selected from each group for observation of gross outcomes.
Observations
Blood was collected from the heart on postoperative days 1, 2, 3, 4, 5, 6 and 7. The rats were anesthetized with injection of chloral hydrate (0.2–0.3 ml/100 g) and subsequently euthanized by cervical dislocation. The Achilles tendon and surrounding soft tissues were dissected. The Achilles tendon and surrounding soft tissues were separated by dissecting scissors and a record of the general state and extent of ossification of tissue. Histological features and immunohistochemical (IHC) staining were studied in addition to ELISA and reverse transcription-quantitative PCR (RT-qPCR). To comprehensively evaluate HO formation in the 10 rats from the two groups, X-ray examination at postoperative weeks 5 and 10 and histological observation at postoperative week 10 were conducted.
Histological and IHC staining
Two samples of Achilles tendon tissues were collected at each time point and fixed in neutral formalin (10%) for 24 h, followed by decalcification in 15% EDTA for 1 week. Following complete decalcification, dehydration was conducted by a graded ethanol series. The tissues were embedded in paraffin wax and sectioned at 5-µm. Hematoxylin and eosin (H&E) staining was performed on a number of sections for light microscopy, followed by dewaxing, hydration, antigen retrieval, PBS wash, incubation with 3% H2O2 for 30 min at 37°C and a second PBS wash of the remaining sections, conducted successively. Subsequently, the tissues were incubated for 1 h at room temperature with 10% goat serum (Takara Biotechnology Co., Ltd.) and 150 µl of each antibody (1:200) was added. PBS replacing the antibody was used as a control and incubated with the sections at 4°C, followed by an additional PBS wash. The secondary antibody (150 µl; 1:200; cat. no. 111-005-045) from Jackson ImmunoResearch Laboratories, Inc. was added and incubated for 1 h at room temperature, followed by PBS wash. The 3,3′-diaminobenzidine color reaction was performed for 5–10 min followed by a PBS wash. The sections were stained with hematoxylin for 1 min and washed with running water for 15 min. Finally, the sections were dehydrated and mounted for observation under the light microscope.
ELISA detection
Serum MMP-9, MMP-2 and TIMP-1 expression levels in the rats were identified at each time point. Blood samples from the rats were stored at room temperature for 2 h and centrifuged at 4°C for 15 min at 1,000 × g. The supernatant was used to measure the MMP-9, MMP-2 and TIMP-1 expression levels following the protocol of the aforementioned ELISA kits.
RT-qPCR detection
Achilles tendon tissues from the two groups were removed at each time point and treated with 1 ml diethyl-pyrocarbonate. The primers of the MMP-9, MMP-2, TIMP-1 reference genes were synthesized by Sangon Biotech Co., Ltd. (Shanghai, China; Table I). TRIzol was purchased from Invitrogen (Thermo Fisher Scientific, Inc.) and the reverse transcription kit from Takara Biotechnology Co., Ltd. The PCR kit (SYBR® Premix Ex Taq™ II) was purchased from Takara Biotechnology Co., Ltd. Each sample was transferred to a 5 ml Eppendorf (EP) tube and suspended in 1 ml TRIzol. Following homogenization, 200 µl chloroform was added and the sample was centrifuged for at 4°C for 15 min at 10,000 × g, 400 µl supernatant was transferred into another 1.5 ml EP tube, followed by the addition of 400 µl isopropanol and mixing. The sample was stored at −70°C for 30 min and centrifuged at 4°C for 10 min at 10,000 × g. The supernatant was discarded and 1 ml iced 75% ethanol added to the residue. The sample was then centrifuged at 4°C for 5 min at 10,000 × g and allowed to stand for 1–15 min at room temperature to dry the RNA. The RNA was dissolved with 1 µl RNase-free deionized water and quantified. The PCR cycling conditions were as follows: 95°C for 30 sec; followed by 40 cycles at 95°C for 5 sec and 60°C for 31 sec. The relative mRNA quantities of target genes were normalized to the values of 18 ribosomal RNA. The results were expressed as fold changes of threshold cycle value relative to the controls using the 2-ΔΔCq method (8,9). Primers for PCR are presented in Table I.
Table I.
Primer sequences.
| Primer | Sequences 5′-3′ |
|---|---|
| MMP-9 | F: AGGTGCCTCGGATGGTTATCG |
| R: TGCTTGCCCAGGAAGACGAA | |
| MMP-2 | F: AAAGGAGGGCTGCATTGTGAA |
| R: CTGGGGAAGGACGTGAAGAGG | |
| TIMP-1 | F: GGCGAACCGGAAACCTGT |
| R: GCGCCCTTTGCATCTCTGG | |
| 18S | F: AGTCGCCGTGCCTACCAT |
| R: CGGGTCGGGAGTGGGTAAT |
F, forward; R, reverse; MMP-9, matrix metalloproteinase-9; TIMP-1, tissue inhibitor of metalloproteinase-1; 18S, 18 ribosomal RNA.
HO diagnosis
X-ray observation
The rats from the control and experimental groups were anesthetized at postoperative weeks 5 and 10 using the method described above. Lateral right hind limbs were radiologically examined to observe the presence of any highlighted shadow.
Histological observation
Two groups of rats were anesthetized with an injection of chloral hydrate (0.2–0.3 ml/100 g), and subsequently euthanized by cervical dislocation at postoperative week 10. Achilles tendon gross morphology was observed using the original incision. The Achilles tendon tissues were stained by H&E and observed under the light microscope. The HO diagnosis was based on the results of radiological and histological observations: If the radiograph demonstrated a highlighted shadow in the Achilles tendon and the histology indicated the presence of bone tissue, the rats were diagnosed as HO.
Statistical analysis
The data were analyzed using SPSS version 13.0 (SPSS, Inc., Chicago, IL, USA) and presented as the mean ± standard deviation. The independent samples t-test was used for comparisons between the groups. P<0.05 was considered to indicate a statistically significant difference.
Results
Gross observation
All the rats survived the surgery and the incisions healed well. Rats from the experimental and control groups demonstrated symptoms of slow movement, reduced food intake and weight loss. The right lower extremity of the rats from the experimental groups demonstrated reduced activity, which returned to normal after 2–3 weeks.
Histological and IHC staining
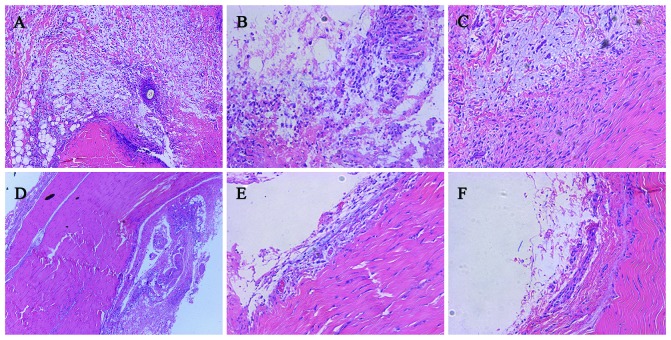
H&E staining
H&E staining of the experimental group demonstrated a large number of inflammatory cells entering tendon tissues from blood vessels. Inflammatory cells infiltrated around the vessels and irregular connective tissues were observed. A large number of irregular connective tissues were observed on postoperative day 4, accompanied by macrophages, neutrophils and other inflammatory cells. On postoperative day 7, increased cartilage cells were observed in the irregular connective tissues. By contrast, in the control group, on postoperative day 1 inflammatory cells gathered around the Achilles tendon tissues and transformed into regular connective tissues. On postoperative day 4, inflammatory cells gradually infiltrated Achilles tendon tissues and became irregular connective tissues. On day 7 inflammatory cells infiltrated the Achilles tendon tissues (Fig. 2).
Figure 2.
Hematoxylin and eosin staining. Experimental group: Postoperative days (A) 1, (B) 3 and (C) 7. Control group: Days (D) 1, (E) 3 and (F) 7. Magnification, ×200.
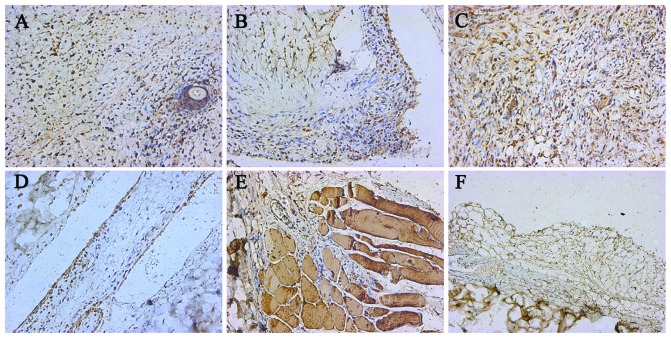
MMP-9 IHC staining
IHC staining of MMP-9 in the experimental group: A large number of inflammatory cells and dark-brown particles infiltrated the tissues on postoperative day 1. A number of dark-brown and inflammatory cells were observed on postoperative days 4 and 7. IHC staining of MMP-9 from control group: Yellow particles and inflammatory cells accumulated around the Achilles tendon tissues on postoperative day 1. On postoperative days 4 and 7, an increasing number of yellow particles and inflammatory cells gradually infiltrated the muscle tissues (Fig. 3).
Figure 3.
MMP-9 immunohistochemical staining. Experimental group: Postoperative days (A) 1, (B) 3 and (C) 7. Control group: Days (D) 1, (E) 3 and (F) 7. Magnification, ×200. MMP, matrix metalloproteinase.
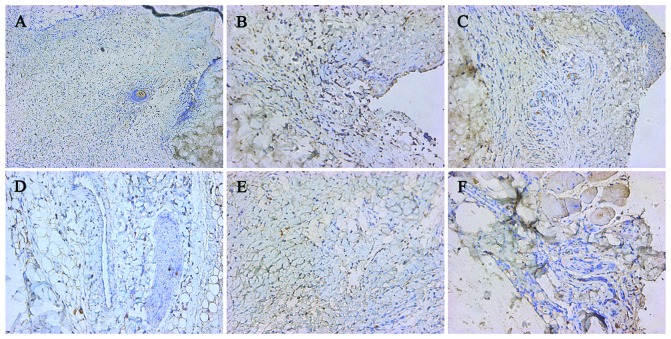
MMP-2 IHC staining
Experimental group: A large number of inflammatory cells infiltrated the tissues at each time point following surgery and a few light-yellow particles were observed. Control group: The number of inflammatory cells increased gradually at each time point following surgery and a few light-yellow particles were observed (Fig. 4).
Figure 4.
MMP-2 immunohistochemical staining. Experimental group: Postoperative days (A) 1, (B) 3 and (C) 7. Control group: Days (D) 1, (E) 3 and (F) 7. Magnification, ×200. MMP, matrix metalloproteinase.
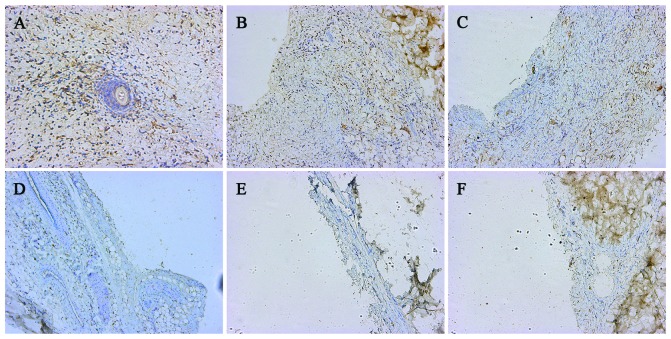
TIMP-1 IHC staining
Experimental group; on postoperative day 1, a large number of inflammatory cells were secreted into the surrounding tissues from the blood vessels and yellow particles infiltrated the tissues. On postoperative days 4 and 7, yellow particle infiltration was also observed in the tissues. Control group; the number of inflammatory cells increased gradually at each time point and light-yellow particles were observed (Fig. 5).
Figure 5.
TIMP-1 immunohistochemical staining. Experimental group: Postoperative days (A) 1, (B) 3 and (C) 7. Control group: Days (D) 1, (E) 3 and (F) 7. Magnification, ×200. TIMP-1, tissue inhibitor of metalloproteinase-1.
Detection of MMP-9, MMP-2 and TIMP-1 expression
The differences in serum protein and gene expression of MMP-9, MMP-2 and TIMP-1 between rats sustaining brain injury combined with Achilles tendon clamp and brain injury alone were compared. A significantly elevated MMP-9 expression in the experimental group postoperative days 5–7 compared with the control group was observed (P<0.05). However, no significant differences in the MMP-2 and TIMP-1 levels were observed between the experimental and control groups at each time point (P≥0.05). It was identified that the TIMP-1 gene expression in the experimental group was significantly higher compared with the control group (P<0.05). A similar finding was obtained with MMP-9 gene expression at postoperative days 3–7. However, MMP-2 gene expression in experimental group was not significantly different from control group at each time point (P≥0.05; Fig. 6).
Figure 6.
(A) Protein and (B) gene expression of MMP-9, MMP-2 and TIMP-1. MMP, matrix metalloproteinase; TIMP-1, tissue inhibitor of metalloproteinase-1; PCR, polymerase chain reaction.
HO diagnosis
Highlighted shadow areas were observed in all the rats in the experimental group (10/10) by postoperative week 5 and similar shadows by week 10. By contrast, only 40% of the rats in the control group exhibited highlighted shadow areas by postoperative week 5 and 60% by week 10. Histological observations after week 10 revealed mature bone tissues and bone trabecula in the experimental and control groups, which corresponded to the shadows on the X-rays. The ossification area in the experimental group was larger compared with the control group. According to the radiological and histological observations, all of the rats in the experimental group manifested HO by postoperative week 10. By contrast, only 60% of the rats in the control group had HO under the same conditions (Fig. 7).
Figure 7.
Diagnosis of heterotopic ossification. X-ray observation, radiographs of lateral right hind limbs; experimental group, postoperative weeks (A) 5, (B) 10 and (C) 5; (D) control group, week 10. Achilles tendon tissues stained by hematoxylin and eosin, (E) Experimental group week 10 and (F) control group week 10. Magnification, ×200.
Discussion
A rat brain injury model was induced by free fall. By adjusting the weight and height, mild, moderate or severe brain injury was created (7). Pathophysiological changes and mechanisms of mechanical impact caused by Feeney's freefall-induced rat brain injury were similar to focal cerebral contusions. The direct hit on the endocranium avoided anomalies associated with the variation in animal hair and skull thickness (10). HO was induced via Achilles tendon rupture. The morphology and imaging of this model were similar to the HO caused by surgical trauma and the model had good repeatability (11,12). Following the cutting of the Achilles tendon, the macrophages accumulated during tissue repair. The released inflammatory mediators stimulated the mesenchymal stem cells to differentiate into chondrocytes or osteoblasts. Chondrocyte proliferation and hypertrophy were followed by calcification in the ECM. New blood vessels grew into the calcified tissue and osteoclasts and osteoblasts rebuilt the tissues. The bone tissues were formed by cartilage (13).
The disease incidence of HO at postoperative week 5 was 100 percent in the experimental group compared with only 40% at week 5 and 60% at week 10 in the control group. Evidence suggested that the combined brain injury increased the rate and degree of osteogenesis. In the control group, the degree of local tissue trauma failed to induce HO. However, the combined brain injury resulted in a 60% disease incidence of HO at postoperative week 10. The model indicated that brain injury had a close association with HO, suggesting that HO in the traumatic area was not correlated with HO severity.
MMP-9 is an important component of gelatinase, degrading and denaturing collagen types I, II and III. It also breaks down the small molecules and ECM components including collagen types IV, V, VII, IX, XI, elastin and gelatin (14). MMP-2, also known as gelatinase A, is expressed in the cytoplasm of osteoblasts and certain osteoclasts. Additionally, MMP-2 can cause the degradation of bone matrix, the inhibition of bone resorption and increased bone reconstruction (15). Changes in the levels of MMP-2 secreted from osteoblasts reflect bone metabolism (16). TIMPs are widely distributed in the body fluids and tissues and the specificity and dynamic balance are maintained between MMPs and TIMPs (17). Under pathological conditions, this dynamic balance was disturbed and led to the excessive decomposition of the ECM and pathological changes (18).
The present study indicated that MMP-9 and MMP-2 levels increased in postoperative days 1–3, in contrast to the gene expression of MMP-9 and MMP-2. On postoperative day 3, the MMP-9 and MMP-2 expression levels decreased, suggesting a close association with combined brain injury. Wang et al (19) identified that intrinsic brain cells secreted MMPs following brain injury and that astrocytes were the major source of MMP-9. Following mechanical brain injury, the extracellular regulated kinases P38 and MMP-9 were mutually regulated, resulting in an increase in MMPs. MMP-9 damaged the close association between the microvascular cells of blood brain barrier and the cerebral vascular matrix and the integrity of blood brain barrier was thus destroyed (20). MMPs increased in the peripheral blood following brain injury and the increased number of neutrophils aggravated the inflammatory response.
The present study hypothesized that the increase in inflammatory response caused by brain injury and inflammatory cells had a close association with HO incidence. A comparison of the two groups of rats revealed that serum MMP-9 increased in postoperative days 5–7 although the MMP-2 and TIMP-1 expression was not significantly altered. MMP-9 expression was associated with the HO incidence and osteogenic amount. It was hypothesized that serum MMP-9 may be proportional to the severity of HO and was an early biomarker of HO. In a previous study (21), mesenchymal stem cells were identified as having a vital role in the HO process and being the precursors of chondrocytes. Extracellular microenvironment is important for cartilage cell differentiation and maturation (22). MMP-9-mediated ECM degradation and reconstruction may be closely associated with HO bone formation and remodeling to create an appropriate osteogenic environment.
It was demonstrated that MMP-9 expression in the experimental group was higher compared with the control group in postoperative days 3–7, which confirmed the hypothesis of the present study. In the early stage of HO, the MMP-9 gene exhibited high expression in local tissues. No significant difference was observed in MMP-2 gene expression between the two groups, although the role of MMP-2 in the subsequent pathogenesis of HO cannot be excluded. The present study demonstrated that TIMP-1 gene expression was higher in the experimental group compared with the control group at each time point but no statistical difference was observed in serum TIMP-1 levels between the two groups. Therefore, it was assumed that the change of TIMP-1 gene expression may be associated with the degree of trauma. The results of the present study suggested that TIMPs inhibited the MMPs activation by forming a stable complex with proMMPs. TIMPs may bind the activated MMPs non-covalently, thus decreasing MMP activity. This type of binding is irreversible and stable (23,24). The increase of TIMP-1 gene expression in the experimental group may have protected local tissues. The H&E staining results demonstrated that rats from the two groups suffered from inflammatory cell infiltration. A number of regular and dense connective tissues became regular and thick collagen fibers interweaved in a three-dimensional manner. In the experimental group, inflammatory cells infiltrated local tissues sooner and the chondrocytes appeared in the early stage of HO. In the control group, the Achilles tendon tissues demonstrated less damage; the infiltration of local tissues around the Achilles tendon by inflammatory cells and the change from regular connective tissues to irregular connective tissues was slower. No chondrocytes or cartilage matrix were observed. It was hypothesized that in the early stage of HO, inflammatory factors were important in the local tissues. The large infiltration area and rapidity of inflammatory response resulted in severe HO of the Achilles tendon. Staining of the local tissues identified that MMP-9 was secreted by macrophages and neutrophils (23). The altered MMP-9 levels in local tissues were consistent with serum MMP-9, suggesting that MMP-9 mediated the ECM remodeling. MMP-9 may be considered as an early biomarker and a predictor of the degree of severity of HO. Similarly, MMP-2 was also secreted from macrophages and neutrophils. H&E staining indicated that MMP-2 was not significantly expressed in the local tissues. Therefore, MMP-9 possessed higher sensitivity in the early stage of HO compared with MMP-2. TIMP-1 was secreted from inflammatory cells and served a function in the local tissues. TIMP-1 expression in the local tissues of the experimental group was higher compared with the control group. It was hypothesized that TIMP-1 was associated with the degree of local damage and protected the local tissue.
A previous study (25) proposed three criteria for induction of osteogenesis in the soft tissues: Osteogenic precursor cells, osteogenic inducible factor and proper environment. Achilles tendon tissues were infiltrated by inflammatory cells in the early stage of HO. MMP-9, secreted from macrophages and neutrophils, mediated cell migration and ECM degradation and remodeling, which created a suitable environment and induced the osteoblast precursor cells. In the experimental group, the irregular and dense connective tissues appeared in the Achilles tendon and large numbers of inflammatory cells infiltrated continuously, also secreting MMP-9. The MMP-9 gene was inducible by cytokines, hormones and growth factors (26,27). Therefore, specific growth factors (vascular endothelial growth factor and bone morphogenetic proteins) demonstrated continuous and higher expression in the Achilles tendon tissues and thus mesenchymal stem cells were transformed into chondrocytes, osteoblasts and osteoclasts, leading to pathological bone tissues in the local tissue.
Acknowledgements
The present study was supported by the Shanghai Municipal Commission of Health and Family Planning (grant no. 20134204).
References
- 1.Chen HC, Yang JY, Chuang SS, Huang CY, Yang SY. Heterotopic ossification in burns: Our experience and literature reviews. Burns. 2009;35:857–862. doi: 10.1016/j.burns.2008.03.002. [DOI] [PubMed] [Google Scholar]
- 2.Reznik JE, Biros E, Marshall R, Jelbart M, Milanese S, Gordon S, Galea MP. Prevalence and risk-factors of neurogenic heterotopic ossification in traumatic spinal cord and traumatic brain injured patients admitted to specialised units in Australia. J Musculoskelet Neuronal Interact. 2014;14:19–28. [PubMed] [Google Scholar]
- 3.Naraghi FF, DeCoster TA, Moneim MS, Miller RA, Rivero D. Heterotopic ossification. Orthopedics. 1996;19:145–151. doi: 10.3928/0147-7447-19960201-10. [DOI] [PubMed] [Google Scholar]
- 4.Evans EB. Heterotopic bone formation in thermal burns. Clin Orthop Relat Res. 1991:94–101. [PubMed] [Google Scholar]
- 5.Rodenberg E, Azhdarinia A, Lazard ZW, Hall M, Kwon SK, Wilganowski N, Salisbury EA, Merched-Sauvage M, Olmsted-Davis EA, Sevick-Muraca EM, Davis AR. Matrix metalloproteinase-9 is a diagnostic marker of heterotopic ossification in a murine model. Tissue Eng Part A. 2011;17:2487–2496. doi: 10.1089/ten.tea.2011.0007. [DOI] [PubMed] [Google Scholar]
- 6.Oliveira CO, Ikuta N, Regner A. Outcome biomarkers following severe traumatic brain injury. Rev Bras Ter Intensiva. 2008;20:411–421. [PubMed] [Google Scholar]
- 7.Feeney DM, Boyeson MG, Linn RT, Murray HM, Dail WG. Responses to cortical injury: I. Methodology and local effects of contusions in the rat. Brain Res. 1981;211:67–77. doi: 10.1016/0006-8993(81)90067-6. [DOI] [PubMed] [Google Scholar]
- 8.Nolan T, Hands RE, Bustin SA. Quantification of mRNA using real-time RT-PCR. Nat Protoc. 2006;1:1559–1582. doi: 10.1038/nprot.2006.236. [DOI] [PubMed] [Google Scholar]
- 9.Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(−Delta Delta C(T)) Methods. 2001;25:402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 10.Lomnitski L, Kohen R, Chen Y, Shohami E, Trembovler V, Vogel T, Michaelson DM. Reduced levels of antioxidants in brains of apolipoprotein E-deficient mice following closed head injury. Pharmacol Biochem Behav. 1997;56:669–673. doi: 10.1016/S0091-3057(96)00412-1. [DOI] [PubMed] [Google Scholar]
- 11.Lin L, Shen Q, Xue T, Duan X, Fu X, Yu C. Sonic hedgehog improves redifferentiation of dedifferentiated chondrocytes for articular cartilage repair. PloS One. 2014;9:e88550. doi: 10.1371/journal.pone.0088550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Xu JC, Wu T, Wu GH, Zhong ZM, Tang YZ, Chen JT. Leptin expression by heterotopic ossification-isolated tissue in rats with Achilles' tenotomy. Saudi Med J. 2009;30:605–610. [PubMed] [Google Scholar]
- 13.Hong CC, Yu PB. Applications of small molecule BMP inhibitors in physiology and disease. Cytokine Growth Factor Rev. 2009;20:409–418. doi: 10.1016/j.cytogfr.2009.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gupta K, Shukla M, Cowland JB, Malemud CJ, Haqqi TM. Neutrophil gelatinase-associated lipocalin is expressed in osteoarthritis and forms a complex with matrix metalloproteinase 9. Arthritis Rheum. 2007;56:3326–3335. doi: 10.1002/art.22879. [DOI] [PubMed] [Google Scholar]
- 15.Hill PA, Murphy G, Docherty AJ, Hembry RM, Millican TA, Reynolds JJ, Meikle MC. The effects of selective inhibitors of matrix metalloproteinases (MMPs) on bone resorption and the identification of MMPs and TIMP-1 in isolated osteoclasts. J Cell Sci. 1994;107:3055–3064. doi: 10.1242/jcs.107.11.3055. [DOI] [PubMed] [Google Scholar]
- 16.Baker AH, Zaltsman AB, George SJ, Newby AC. Divergent effects of tissue inhibitor of metalloproteinase-1, −2, or −3 overexpression on rat vascular smooth muscle cell invasion, proliferation and death in vitro. TIMP-3 promotes apoptosis. J Clin Invest. 1998;101:1478–1487. doi: 10.1172/JCI1584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Böhmer AE, Oses JP, Schmidt AP, Perón CS, Krebs CL, Oppitz PP, D'Avila TT, Souza DO, Portela LV, Stefani MA. Neuron-specific enolase, S100B and glial fibrillary acidic protein levels as outcome predictors in patients with severe traumatic brain injury. Neurosurgery. 2011;68:1624–1631. doi: 10.1227/NEU.0b013e318214a81f. [DOI] [PubMed] [Google Scholar]
- 18.Dimopoulou I, Korfias S, Dafni U, Anthi A, Psachoulia C, Jullien G, Sakas DE, Roussos C. Protein S-100b serum levels in trauma-induced brain death. Neurology. 2003;60:947–951. doi: 10.1212/01.WNL.0000049931.77887.7F. [DOI] [PubMed] [Google Scholar]
- 19.Wang X, Mori T, Jung JC, Fini ME, Lo EH. Secretion of matrix metalloproteinase-2 and −9 after mechanical trauma injury in rat cortical cultures and involvement of MAP kinase. J Neurotrauma. 2002;19:615–625. doi: 10.1089/089771502753754082. [DOI] [PubMed] [Google Scholar]
- 20.Caron A, Desrosiers RR, Langlois S, Béliveau R. Ischemia-reperfusion injury stimulates gelatinase expression and activity in kidney glomeruli. Can J Physiol Pharmacol. 2005;83:287–300. doi: 10.1139/y05-011. [DOI] [PubMed] [Google Scholar]
- 21.Nagase H, Visse R, Murphy G. Structure and function of matrix metalloproteinases and TIMPs. Cardiovasc Res. 2006;69:562–573. doi: 10.1016/j.cardiores.2005.12.002. [DOI] [PubMed] [Google Scholar]
- 22.Sternlicht MD, Werb Z. How matrix metalloproteinases regulate cell behavior. Annu Rev Cell Dev Biol. 2001;17:463–516. doi: 10.1146/annurev.cellbio.17.1.463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hess K, Ushmorov A, Fiedler J, Brenner RE, Wirth T. TNFalpha promotes osteogenic differentiation of human mesenchymal stem cells by triggering the NF-kappaB signaling pathway. Bone. 2009;45:367–376. doi: 10.1016/j.bone.2009.04.252. [DOI] [PubMed] [Google Scholar]
- 24.Ortega N, Wang K, Ferrara N, Werb Z, Vu TH. Complementary interplay between matrix metalloproteinase-9, vascular endothelial growth factor and osteoclast function drives endochondral bone formation. Dis Model Mech. 2010;3:224–235. doi: 10.1242/dmm.004226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kaplan FS, Glaser DL, Hebela N, Shore EM. Heterotopic ossification. J Am Acad Orthop Surg. 2004;12:116–125. doi: 10.5435/00124635-200403000-00007. [DOI] [PubMed] [Google Scholar]
- 26.Chakraborti S, Mandal M, Das S, Mandal A, Chakraborti T. Regulation of matrix metalloproteinases: An overview. Mol Cell Biochem. 2003;253:269–285. doi: 10.1023/A:1026028303196. [DOI] [PubMed] [Google Scholar]
- 27.Li DQ, Lokeshwar BL, Solomon A, Monroy D, Ji Z, Pflugfelder SC. Regulation of MMP-9 production by human corneal epithelial cells. Exp Eye Res. 2001;73:449–459. doi: 10.1006/exer.2001.1054. [DOI] [PubMed] [Google Scholar]