Abstract
Objective
To evaluate the usefulness of skin ultrasound and acoustic radiation force impulse (ARFI) quantification in diffuse cutaneous systemic sclerosis (dcSSc).
Patients and methods
28 patients with dcSSc, and 15 age gender matched normal controls were recruited. Skin echogenicity, thickness, and ARFI quantification were measured by ultrasound at 17 sites corresponding to the modified Rodnan skin score (mRSS) in each participant. Compared with controls, skin echogenicity of dcSSc patients was classified into isoechoic, hypoechoic, and hyperechoic. The skin thickness, ARFI quantification and mRSS were compared between isoechoic, hypoechoic, hyperechoic and controls.
Results
In patients with dcSSc, the skin thickness increased as the echogenicity changed on the order of isoechoic, hypoechoic and hyperechoic. ARFI quantification was significantly higher in hyperechoic than isoechoic (p<0.001). The mRSS were significantly higher in hyperechoic and/or hypoechoic than isoechoic. For isoechoic patients and healthy controls, the skin echogenicity or thickness was no significant different, however, the ARFI quantification was significantly higher in isoechoic than controls.
Conclusion
Skin ultrasound is feasible for assessing the skin involvement in dcSSc. Skin echogenicity correlates with skin thickness, stiffness, and mRSS. ARFI quantification may be more sensitive to detect skin changes, compared with skin echogenicity and thickness.
Introduction
Systemic sclerosis (SSc) is a heterogeneous autoimmune disorder of unknown aetiology, which may involve the skin and internal organs to varying degrees and with different courses. The extent of skin involvement correlates with survival and prognosis [1, 2]. Ultrasound has been demonstrated to be a reliable tool to measure skin thickness, echogenicity, and stiffness, and it is increasing employed in SSc. Skin thickness increased in SSc patients compared with healthy controls [3], and was significant different between edematous, fibrotic, and atrophic phases [4, 5]. Echographic images of SSc patients skin differed from healthy controls [6]. The degree of skin echogenicity correlated with the amount of sclerosis on histologic examination [7]. During the oedematous phase, skin echogenicity was low and skin thickness was high. When the oedematous phase was replaced by the indurative phase, skin echogenicity increased and skin thickness decreased [8]. Skin stiffness of SSc patients is more recent and less investigated [9–11]. The principle of this technique is the reduced skin elasticity caused by excessive dermal deposition of collagenous and non-collagenous extracellular matrix mediated fibrosis [12]. Increased skin stiffness, shown by specific color or higher ARFI quantification, was reported in SSc patients compared with healthy controls [9–11]. To our knowledge, the correlations between ultrasound measured skin thickness, echogenicty, and stiffness have not been fully conducted. The purpose of this study was therefore to investigate the correlations between them, and explore the usefulness of ultrasound, with the main focus on skin echogenicity and stiffness, in SSc patients.
Patients and methods
Patients
28 patients with dcSSc and 15 age gender matched controls were prospectively recruited from the rheumatology department of Peking union medical college hospital. The patients, who all met the American College of Rheumatology 1980 criteria [13] or American College of Rheumatology/European League Against Rheumatism 2013 criteria [14] for the classification of scleroderma and dcSSc [15], underwent clinical and serological assessment at entry. The disease duration was calculated from the onset of Raynaud’s phenomenon. An experienced physician assigned each patient mRSS on 0–3 ordinal scale over 17 anatomical sites according to Moore et al seventeen point dermal ultrasound scoring system [16]. The physician was trained at the European League Against Rheumatism Scleroderma Trials and Research group course and blinded to the result of the ultrasound assessment. The 17 sites were bilateral middle finger, hand dorsum, forearm, upper arm, thigh, lower leg, foot dorsum, forehead, anterior chest, and anterior abdomen. The ethics committee of Peking Union Medical College Hospital approved the study (No. S-191), and all participants signed informed consent.
Ultrasound examination and image analysis
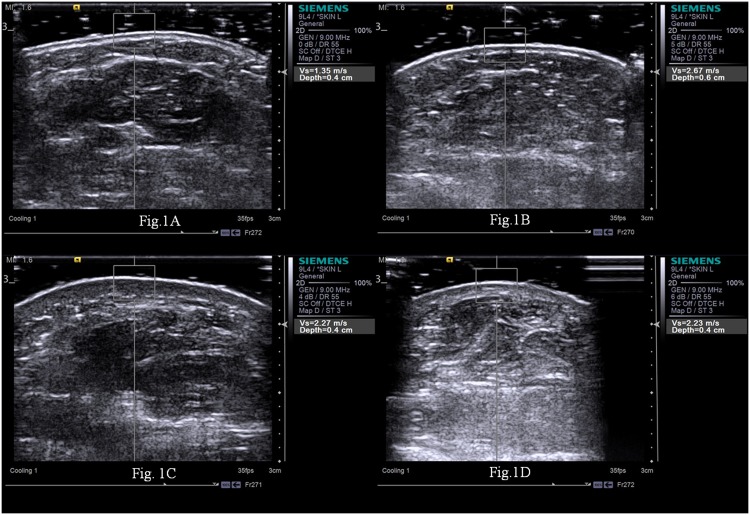
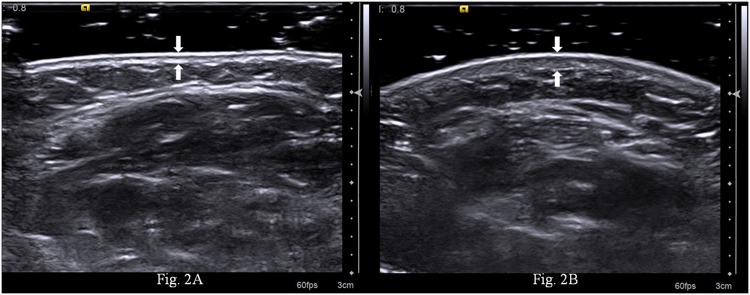
Ultrasound and ARFI quantification were performed over the 17 sites corresponding to mRSS by an experienced ultrasound physician, who was engaged in superficial organ examination for more than 18 years and unaware of the patients’ clinical data. A Siemens S2000 ultrasound system (S2000; Siemens Medical Solutions, Inc. Siemens Healthcare, Erlangen, Germany) fitted with a 9L4 MHz linear probe was used. To increase the accuracy of the measurements, the probe was placed perpendicularly to the skin, and a layer of gel was applied to minimize the compression from the transducer to the skin. The ultrasound image was adopted when the epidermis, dermis, and subcutis were clearly visualized and the interfaces between them were parallel and distinct. The skin stiffness was measured by ARFI quantification. With ARFI technique in the form of Virtual Touch Quantification (VTQ), transducers are used to mechanically excite tissue with short-duration acoustic radiation forces, leading to shear waves propagation away from the region of excitation [9, 17]. The stiffer the tissue, the faster the shear waves propagate. Thus, the shear wave velocity measured by ARFI quantification gives tissue stiffness information of the region of interest (ROI). The ROI box had a preset size of 6mm (width) × 5mm (depth). Five trials of ARFI quantification was performed at each site. When “X” displayed on the screen, the measurements were interpreted as invalid. The five consecutive ARFI quantification measurements with no “X” were taken and the results were averaged. All static ultrasound images were stored and later analyzed by the other three independent outside ultrasound physicians with more than 20 years experience in superficial organs examination. Two ultrasound physicians evaluated all images independently and blinded to the patients’ clinical information. In cases in which there was a discrepancy between the two reviewers, a third ultrasound physician served as a blinded expert. They discussed to reach a consensus for classifying the patient’s skin echogenicity. The patient’s skin echogenicity of each site was compared with site matched normal skin in healthy controls (Fig 1A), and classified into isoechogenic (Fig 1B), hypoechogenic (Fig 1C), and hyperechogenic (Fig 1D). The skin thickness, the combined epidermis and dermis, was determined (Fig 2).
Fig 1. Ultrasound findings of the dcSSc patients and the control’s right forearm skin.
The echogenicity was determined as compared with site-matched, normal skin in healthy controls (Fig 1A), and was classified into isoechogenic (Fig 1B), hypoechogenic (Fig 1C), and hyperechogenic (Fig 1D).
Fig 2. Ultrasound measured skin thickness of the dcSSc patients and the control’s right forearm.
The skin thickness was 0.6mm (between arrows) for controls (Fig 2A), and 1.0mm (between arrows) for patients (Fig 2B).
Statistical analysis
SPSS software version 14.0 was used for statistical analysis, with p<0.05 considered statistically significant. Data were expressed as median (lower quartile, upper quartile). The intraclass correlation coefficient (ICC) was calculated to examine the inter-observer reliability of skin echogenicity classification. Differences in skin thickness, ARFI quantification and mRSS between isoechogenic, hypoechogenic, hyperechogenic and controls were assessed by Kruskal-Wallis test with Bonferroni multiple testing correction.
Results
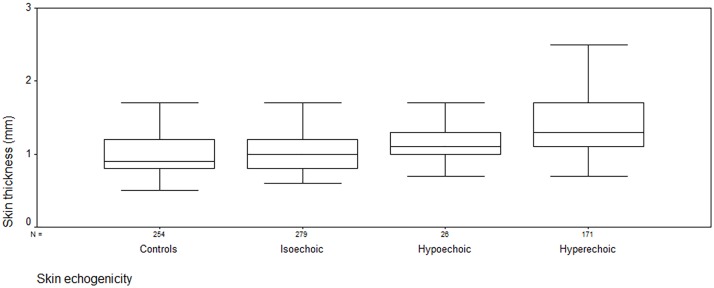
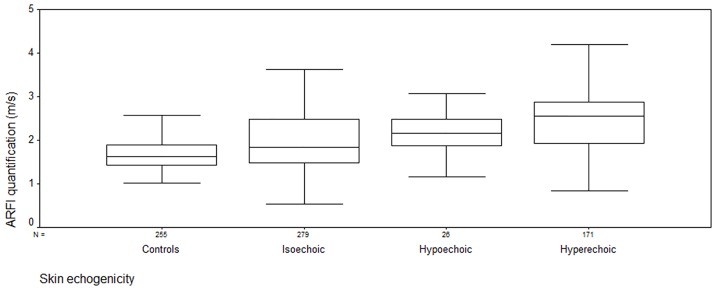
Table 1 showed the clinical data of the patients. Table 2 showed the skin thickness, ARFI, and mRSS of dcSSc patients and controls. ICC of two reviewers’ skin echogenicity classification was 0.608 (p<0.001). In patients with dcSSc, the skin thickness was 1.0 (0.8, 1.2) mm, 1.1 (1.0, 1.3) mm, 1.3 (1.1, 1.7) mm for isoechoic, hypoechoic and hyperechoic respectively. The thickness increased as the echogenicity changed on the order of isoechoic, hypoechoic and hyperechoic (p<0.001) (Fig 3). ARFI quantification was 1.83 (1.48, 2.48) m/s, 2.16 (1.86, 2.49) m/s, 2.55 (1.92, 2.88) m/s for isoechoic, hypoechoic and hyperechoic respectively. The quantification was significantly higher in hyperechoic than isoechoic (p<0.001), no significant difference was found between hyperechoic and hypoechoic, or between hypoechoic and isoechoic (p = 0.117) (Fig 4). The local mRSS was expressed as median (lower quartile, upper quartile) for the three groups (isoechoic, hypoechoic and hyperechoic) respectively, and it was 0 (0, 1), 1 (0, 1), 1(0, 2) for isoechoic, hypoechoic and hyperechoic respectively. The mRSS was significantly higher in hyperechoic and/or hypoechoic than isoechoic (p<0.001), no significant difference was found between hyperechoic and hypoechoic (p = 0.600).
Table 1. Clinical data of 28 patients with dcSSc.
| Characteristic | Patients | Controls |
|---|---|---|
| Age (years) | 50.5 (19–65) | 43 (21–72) |
| Sex, female: male | 22: 6 | 13: 2 |
| Disease duration, median (range) months | 36 (4–204) | |
| Anti-topoisomerase antibodies(+/−) | 17/11 | |
| Anti-centromere antibodies(+/−) | 0/28 | |
| ANA(+/−) | 26/2 | |
| mRSS, median (range) | 10 (4–23) |
Table 2. Skin thickness, ARFI, and mRSS of dcSSc patients and controls.
| Patients | Controls | ||||
|---|---|---|---|---|---|
| Site | Skin thickness(mm) | ARFI(m/s) | mRSS | Skin thickness(mm) | ARFI(m/s) |
| Right middle finger | 1.1(1.0,1.3) | 2.1(1.35,2.58) | 1(0,1) | 0.6(0.4,0.8) | 1.0(0.8,1.34) |
| Right hand dorsum | 1.2(1.0,1.6) | 2.5(1.83,2.83) | 1(1,2) | 0.6(0.5,0.8) | 1.0(0.8,1.28) |
| Right forearm | 1.2(0.9,1.4) | 2.6(2.3,2.89) | 1(1,2) | 0.6(0.4,0.7) | 0.8(0.7,1.1) |
| Right upper arm | 0.9(0.7,1.1) | 1.57(1.35,1.87) | 1(0,1) | 0.5(0.5,0.8) | 0.9(0.8,1.42) |
| Left middle finger | 1.1(1.0,1.2) | 2.49(1.91,2.81) | 1(0,1) | 0.5(0.4,0.7) | 1.0(0.7,1.44) |
| Left hand dorsum | 1.2(1.1,1.3) | 2.4(1.8,2.84) | 1(1,2) | 0.7(0.4,0.8) | 1.0(0.8,1.19) |
| Left forearm | 1.1(0.9,1.4) | 2.55(2.26,2.88) | 1(1,2) | 0.6(0.5,0.7) | 1.0(0.8,1.48) |
| Left upper arm | 0.9(0.8,1.2) | 1.47(1.32,1.83) | 1(0,1) | 0.5(0.4,0.6) | 1.0(0.8,1.41) |
| Forehead | 0.9(0.8,1.1) | 1.59(1.33,1.97) | 1(1,1) | 0.9(0.6,1.0) | 1.2(0.9,1.38) |
| Anterior chest | 1.4(1.1,1.6) | 2.56(1.84,2.97) | 1(0,1) | 1.1(0.8,1.4) | 1.4(1.3,1.59) |
| Anterior abdomen | 1.5(1.1,2.1) | 2.32(1.47,2.73) | 0(0,1) | 1.5(1.1,2.0) | 1.71(1.4,2.0) |
| Right thigh | 1.2(1.0,1.6) | 2.21(1.8,2.64) | 0(0,0) | 1.0(0.6,1.4) | 1.6(0.8,1.9) |
| Right lower leg | 1.1(1.0,1.3) | 2.02(1.63,2.55) | 0(0,0) | 0.8(0.6,1.0) | 1.4(1.0,1.5) |
| Right foot dorsum | 0.8(0.7,1.3) | 1.91(1.33,2.46) | 0(0,0) | 0.5(0.4,0.7) | 0.6(0.8,1.24) |
| Left thigh | 1.2(1.1,1.7) | 2.15(1.85,2.72) | 0(0,0) | 1.0(0.8,1.5) | 1.4(1.1,1.9) |
| Left lower leg | 1.1(0.9,1.3) | 2.25(1.82,2.69) | 0(0,0) | 0.8(0.6,1.1) | 1.2(1.0,1.5) |
| Left foot dorsum | 0.8(0.7,1.1) | 1.54(1.34,1.92) | 0(0,0) | 0.5(0.4,0.6) | 0.8(0.7,1.45) |
Fig 3. The skin thickness of dcSSc patients and controls.
Box plots represent the 25 and 75th percentile of measures, the median (line in box) and the minimum and maximum values (whiskers). The thickness increased as the echogenicity changed on the order of isoechoic, hypoechoic and hyperechoic (p<0.001). No significant difference was found between isoechoic patients and healthy controls (p = 0.142).
Fig 4. The ARFI quantification of dcSSc patients and controls.
Box plots represent the 25 and 75th percentile of measures, the median (line in box) and the minimum and maximum values (whiskers). The ARFI quantification was significantly higher in hyperechoic than isoechoic (p<0.001), no significant difference was found between hyperechoic and hypoechoic, or between hypoechoic and isoechoic (p = 0.117). The ARFI quantification was significantly higher in isoechoic than controls (p<0.001).
Between isoechoic patients and healthy controls, the skin thickness was no significant different (1.0 (0.8, 1.2) mm v.s. 0.7(0.5, 0.9) mm, p = 0.142), however, the ARFI quantification was significantly higher in isoechoic than controls (1.83(1.48, 2.48) m/s v.s. 1.1(0.8, 1.49) m/s, p<0.001).
Discussion
Our study showed that skin echogenicity correlated with skin thickness and local mRSS. The thickness increased as the echogenicity changed on the order of isoechoic, hypoechoic and hyperechoic. The mRSS was significantly higher in hyperechoic and/or hypoechoic than isoechoic. We hypothesized that isoechogenicity in our study may be associated with very early disease or atrophy, while hypoechogenicity and hyperechogenicity may correlate with edema and sclerosis. Our results indicate that ultrasound measured skin thickness is more sensitive than mRSS to detect skin changes, which is in accordance with previous studies [2, 18, 19]. Ultrasound role is becoming more and more relevant in systemic sclerosis. The majority of articles reported the use of thickness for skin involvement assessment, only a few studied skin echogenicity [3, 4, 7, 8, 12]. Hesselstrand et al [8] reported the inverse relationship between skin echogenicity and thickness in SSc patients with short disease duration (<2 years). Over the five examined sites (finger, hand dorsum, forearm, leg, and chest), Hesselstrand et al found a mild-to-moderate positive correlation between local skin thickness and the local/total mRSS (spearman correlation coefficient +0.36 ~ +0.72), while a mild negative correlation between local skin echogenicity and the local/total mRSS (spearman correlation coefficient -0.18 ~ -0.47). Hesselstrand et al [8] used an arbitrary score of 0–255 to measure the mean echogenicity of a selected region. A low value represents high water content and a high value represents low water content. It’s difficult to obtain site-matched, unaffected skin for comparison in patients with dcSSc. Therefore, we determined echogenicity compared to site-matched normal skin in healthy controls. The theoretical basis for this is the previous findings that skin echo structure of SSc patients differed from healthy controls [6], and skin thickness and echogenicity was no significant different in healthy controls with regards to gender (male and female) and age (15–70 years old), except anatomical sites [20, 21].
Imaging of the elastic properties of skin using ARFI quantification has become the subject of increasing research in patients with SSc [10, 11]. Our pilot article showed increased ARFI quantification in dcSSc patients compared with healthy controls, and ARFI quantification was more sensitive than mRSS. In this study ARFI quantification was significantly higher in hyperechoic than isoechoic, suggesting higher grades of fibrosis in hyperechoic lesions. Moreover, ARFI quantification, instead of skin echogenicity or thickness, was significant different between isoechoic and controls, indicating ARFI quantification may be more sensitive than skin echogenicity and thickness to detect subtle skin changes. The results are similar to Kissin et al [18] and our previous study that demonstrated higher skin stiffness in so-called uninvolved skin as compared with healthy control skin, due to the abnormal endothelial activation and procollagen production [8, 22].
Our study is limited by the relatively small number of patients and controls included, single centre design and lack of information about ultrasound validity to detect change in patients’ follow up and clinical trial. These preliminary findings need to be confirmed in large studies.
In conclusion, skin ultrasound is feasible for assessing the skin involvement in dcSSc. Skin echogenicity correlates with skin thickness, stiffness, and mRSS. ARFI quantification may be more sensitive to detect skin changes, compared with skin echogenicity and thickness.
Supporting information
(JPG)
(PDF)
(DOC)
(XLSX)
Acknowledgments
We thank Dr. Haiyu Pang for the assistance in data analysis.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
YH received the funding, the National Natural Science Foundation of China (81671614), the website: www.nsfc.gov.cn/. YH contributed in the study design, data collection and analysis, decision to publish, and preparation of the manuscript.
References
- 1.Steen VD, Medsger TA Jr. Improvement in skin thickening in systemic sclerosis associated with improved survival. Arthritis Rheum. 2001; 44: 2828–35. [DOI] [PubMed] [Google Scholar]
- 2.Clements PJ, Hurwitz EL,Wong WK, Seibold JR, Mayes M, White B, et al. Skin thickness score as a predictor and correlate of outcome in systemic sclerosis: high dose versus low-dose penicillamine trial. Arthritis Rheum. 2000; 43: 2445–54. [DOI] [PubMed] [Google Scholar]
- 3.Akesson A, Forsberg L, Hederstrom E, Wollheim F. Ultrasound examination of skin thickness in patients with progressive systemic sclerosis (scleroderma). Acta radiologica: diagnosis. 1986; 27: 91–4. [DOI] [PubMed] [Google Scholar]
- 4.Kaloudi O, Bandinelli F, Filippucci E, Conforti ML, Miniati I, Guiducci S, et al. High frequency ultrasound measurement of digital dermal thickness in systemic sclerosis. Ann Rheum Dis. 2010; 69: 1140–43. 10.1136/ard.2009.114843 [DOI] [PubMed] [Google Scholar]
- 5.Sedky MM, Fawzy SM, El Baki NA, El Eishi NH, El Bohy Ael M. Systemic sclerosis: an ultrasonographic study of skin and subcutaneous tissue in relation to clinical findings. Skin Res Technol. 2013; 19: 78–84. [DOI] [PubMed] [Google Scholar]
- 6.Seidenari S, Belletti B, Conti A. A quantitative description of echographic images of sclerotic skin in patients with systemic sclerosis, as assessed by computerized image analysis on 20 MHz B-scan recordings. Acta Derm Venereol. 1996; 76: 361–4. [DOI] [PubMed] [Google Scholar]
- 7.Nezafati KA, Cayce RL, Susa JS, Setiawan AT, Tirkes T, Bendeck SE, et al. 14-MHz ultrasonography as an outcome measure in morphea (localized scleroderma). Arch Dermatol. 2011; 147: 1112–5. 10.1001/archdermatol.2011.243 [DOI] [PubMed] [Google Scholar]
- 8.Hesselstrand R, Scheja A, Wildt M, Akesson A. High-frequency ultrasound of skin involvement in systemic sclerosis reflects oedema, extension and severity in early disease. Rheumatology (Oxford). 2008; 47: 84–7. [DOI] [PubMed] [Google Scholar]
- 9.Iagnocco A, Kaloudi O, Perella C, Bandinelli F, Riccieri V, Vasile M, et al. Ultrasound elastography assessment of skin involvement in systemic sclerosis: Lights and shadows. J Rheumatol. 2010; 37: 1688–91. 10.3899/jrheum.090974 [DOI] [PubMed] [Google Scholar]
- 10.Hou Y, Zhu QL, Liu H, Jiang YX, Wang L, Xu D, et al. A preliminary study of acoustic radiation force impulse quantification for the assessment of skin indiffuse cutaneous systemic sclerosis. J Rheumatol. 2015; 42: 449–55. 10.3899/jrheum.140873 [DOI] [PubMed] [Google Scholar]
- 11.Santiago T, Alcacer-Pitarch B, Salvador MJ, Del Galdo F, Redmond AC, da Silva JA. A preliminary study using virtual touch imaging and quantification for the assessment of skin stiffness in systemic sclerosis. Clin Exp Rheumatol. 2016; 34 Suppl 100: 137–41. [PubMed] [Google Scholar]
- 12.Abignano G, DelGaldo F. Quantitating skin fibrosis: innovative strategies and their clinical implications. Curr Rheumatol Rep. 2014; 16: 404 10.1007/s11926-013-0404-5 [DOI] [PubMed] [Google Scholar]
- 13.Anonymous. Preliminary criteria for the classification of systemic sclerosis (scleroderma). Subcommittee for scleroderma criteria of the American Rheumatism Association Diagnostic and Therapeutic Criteria Committee. Arthritis Rheum. 1980; 23: 581–90. [DOI] [PubMed] [Google Scholar]
- 14.Van den Hoogen F, Khanna D, Fransen J, Johnson SR, Baron M, Tyndall A, et al. 2013 classification criteria for systemic sclerosis: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Ann Rheum Dis. 2013; 72: 1747–55. 10.1136/annrheumdis-2013-204424 [DOI] [PubMed] [Google Scholar]
- 15.LeRoy EC, Black C, Fleischmajer R, Jablonska S, Krieg T, Medsger TA Jr, et al. Scleroderma (systemic sclerosis): classification, subsets and pathogenesis. J Rheumatol. 1988; 15: 202–5. [PubMed] [Google Scholar]
- 16.Moore TL, Lunt M, McManus B, Anderson ME, Herrick AL. Seventeen-point dermal ultrasound scoring system-a reliable measure of skin thickness in patients with systemic sclerosis. Rheumatology (Oxford). 2003; 42: 1559–63. [DOI] [PubMed] [Google Scholar]
- 17.Lupsor M, Badea R, Stefanescu H, Sparchez Z, Branda H, Serban A, et al. Performance of a new elastographic method (ARFI technology) compared to unidimensional transient elastography in the noninvasive assessment of chronic hepatitis C. Preliminary results. J Gastrointestin Liver Dis. 2009; 18: 303–10. [PubMed] [Google Scholar]
- 18.Kissin EY, Schiller AM, Gelbard RB, Anderson JJ, Falanga V, Simms RW,et al. Durometry for the assessment of skin disease in systemic sclerosis. Arthritis Rheum. 2006; 55: 603–9. 10.1002/art.22093 [DOI] [PubMed] [Google Scholar]
- 19.Merkel PA, Clements PJ, Reveille JD, Suarez-Almazor ME, Valentini G, Furst DE. Current status of outcome measure development for clinical trials in systemic sclerosis: report from OMERACT 6. J Rheumatol. 2003; 30: 1630–47. [PubMed] [Google Scholar]
- 20.Akesson A, Hesselstrand R, Scheja A, Wildt M. Longitudinal development of skin involvement and reliability of high frequency ultrasound in systemic sclerosis. Ann Rheum Dis. 2004; 63: 791–6. 10.1136/ard.2003.012146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.de Rigal J, Escoffier C, Querleux B, Faivre B, Agache P, Lévêque JL. Assessment of aging of the human skin by in vivo ultrasonic imaging. J Invest Dermatol. 1989; 93: 621–5. [DOI] [PubMed] [Google Scholar]
- 22.Claman HN, Giorno RC, Seibold JR. Endothelial and fibroblastic activation inscleroderma: the myth of the “uninvolved skin”. Arthritis Rheum. 1991; 34: 1495–501. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(JPG)
(PDF)
(DOC)
(XLSX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.