Abstract
Background
There is a paucity of data regarding HF incidence among low-income and minority populations. Our objective was to investigate HF incidence and post-HF survival by race and sex among low-income adults in the southeastern US.
Methods and Results
Participants were 27,078 white and black men and women enrolled during 2002–2009 in the Southern Community Cohort Study (SCCS) who had no history of HF and were receiving Centers for Medicare or Medicaid services (CMS). Incident HF diagnoses through December 31, 2010 were ascertained using ICD-9 codes 428.x via linkage with CMS research files. Most participants were black (68.8%), women (62.6%) and earned < $15,000/year (69.7%); mean age was 55.5 (10.4) years. Risk factors for HF were common: hypertension (62.5%), diabetes (26.5%), myocardial infarction (8.6%) and obesity (44.8%). Over a median follow-up of 5.2 years, 4,341 participants were diagnosed with HF. The age-standardized incidence rates were 34.8, 37.3, 34.9 and 35.6 PY/1000 in white women, white men, black men and black women, respectively, remarkably higher than previously reported. Among HF cases, 952 deaths occurred over a median follow-up 2.3 years. Men had lower survival; hazard ratios and 95% confidence intervals were 1.63 (1.27–2.08), 1.38 (1.11–1.72) and 0.90 (0.73–1.12) for white men, black men and black women compared with white women.
Conclusions
In this low-income population, HF incidence was higher for all race-sex groups than previously reported in other cohorts. The SCCS is a unique resource to investigate determinants of HF risk in a segment of the population underrepresented in other existing cohorts.
Keywords: heart failure, incidence, survival, race, epidemiology
Journal Subject Terms: Heart Failure, Epidemiology, Race and Ethnicity
There are over 26 million persons living with heart failure (HF) worldwide.1 In the US, over 5.7 million adults (≈ 2.5% of the US adult population) are estimated to have HF.2 About half of persons diagnosed with HF die within 5 years and the estimated total costs of HF in the US exceeded $30 billion in 2012.3,4 Several established cardiovascular disease (CVD) cohorts have investigated HF incidence and mortality, including the Framingham Heart Study (FHS), Cardiovascular Health Study (CHS), Multi-ethnic Study of Atherosclerosis (MESA) and Atherosclerosis Risk in Communities (ARIC).5–8 The FHS included predominantly white individuals. Other cohorts, including CHS, MESA, and ARIC, enrolled multi-ethnic middle-class populations from select communities and their relatively small sample sizes limited assessment of differential risk patterns between demographic groups defined by both race and sex.
While data from these previous cohorts suggest differences in HF incidence rates and post-HF survival between population subgroups, knowledge gaps persist regarding the magnitude and direction of these differences, particularly in multi-ethnic low income populations with high burden of CVD risk factors. The prospective Southern Community Cohort Study (SCCS) provided a valuable opportunity to investigate differences in the incidence of HF as well as in post-HF survival between groups defined by race and sex: white women, black women, white men and black men.9
Methods
Study sample
The SCCS is a prospective cohort study designed to investigate the incidence of cancer and other chronic diseases, including differential patterns by race and sex, in a low-income under-insured population underrepresented in previous studies. Between 2002 and 2009, the SCCS enrolled approximately 86,000 adults (≈ two-thirds black) aged 40–79 living in 12 southeastern states to investigate various chronic disease outcomes.9 Approximately 86% of participants were recruited at community health centers (CHC), which provide primary health and preventive care services for low-income populations so that the cohort is made up of a segment of society (minority, poor, rural) seldom included in sizeable numbers in previous cohort studies; particularly those investigating CVD.9, 10 The remaining 14% were recruited via mail-based general population sampling. Data on socioeconomic, demographic (including self-reported race), lifestyle, and anthropometric characteristics, as well as personal medical history, were ascertained at cohort enrollment via standardized computer-assisted personal interviews for CHC participants, and via self-administered mailed questionnaire for general population participants. Detailed description of SCCS methods has been previously published.9, 10
SCCS participants (n = 27,078) included in the current analyses were individuals aged ≥ 65 years (n = 7001) at cohort enrollment, or persons < 65 years (n = 20,077) at enrollment who: a) reported being covered by Medicaid (which provides medical benefits to low-income adults and uninsured persons) on the baseline questionnaire; or b) reported being covered by Medicare (the primary health insurance program for persons aged ≥ 65) on the baseline questionnaire; or c) did not report Medicare or Medicaid on the baseline questionnaire but had a Centers for Medicare and Medicaid Services (CMS) claim within 90 days of being enrolled in SCCS. The restriction to these groups ensures that participants would likely have continuous coverage in Medicare and/or Medicaid from the time of SCCS enrollment to the end of the follow-up period (December 31st, 2010), for the ascertainment of incident HF events. Analyses were restricted to self-reported African American or black and non-Hispanic white SCCS participants, since too few persons in other racial groups were available for stable statistical analysis.
Outcome ascertainment
Heart failure events were ascertained via linkage of the SCCS cohort with CMS Research Identifiable Files (which include Medicare institutional and non-institutional files, and the Medicaid Analytic Extract files). Incident HF was defined as the first occurrence of a medical claim with an International Classification of Diseases, 9th revision, discharge code of 428.x (428.0 to 428.9) within the Medicare institutional (Medicare Provider Analysis and Review, MEDPAR, which includes inpatient, outpatient and skilled nursing facility base files), Part B carrier (includes non-institutional physician services and durable medical equipment), or outpatient-based claims files or the Medicaid Analytic Extract (MAX) Inpatient and Other Services claims files, from the date of SCCS enrollment through December 31st, 2010. Detailed description of the CMS research files are published elsewhere. 11
Deaths, including dates and causes of death, were ascertained via linkage of the SCCS cohort with both the Social Security Administration (SSA) vital status service for epidemiologic researchers and the National Death Index (NDI) through December 31st, 2010. Both NDI and SSA are well-established and reliable means of identifying deaths in the US, and are expected to capture nearly all deaths.12–14
Statistical Analysis
Descriptive statistics (means and standard deviations for continuous variables and counts and percentages for categorical variables) were computed for all study participants by race and sex.
To investigate the incidence of HF, duration of follow-up was computed from date of entry into the SCCS until the date of the first diagnosis of HF, date of death, or December 31st, 2010, whichever occurred first. Incidence rates (IR) of heart failure were calculated for white women, black women, white men and black men by dividing the number of HF cases by person-time of follow-up, presented per 1,000 person-years. The 95% confidence intervals (CI) were calculated using the quadratic approximation to the Poisson log likelihood for the log-rate parameter.15 To account for age differences between the demographic categories, age-standardized rates were computed using the overall age distribution of the SCCS participants.
Multivariable Cox models were utilized to test whether differences in crude IRs between categories defined by race and sex persisted after adjustment for baseline covariates. Three models were constructed, with white women as the referent category: model 1 included indicator variables for white men, black women and black men and age (restricted cubic splines with 4 knots); model 2 additionally adjusted for body mass index (restricted cubic splines with 4 knots), and history of diabetes, hypertension, high cholesterol, MI/CABG or stroke (all yes/no); model 3 additionally adjusted for the following covariates: annual household income (<$15,000; $15,000–$24,999; ≥$25,000); education (< high school, high school/vocational training/junior college, college degree or higher), smoking (never, former, current <19.5 pack-years, current ≥ 19.5 pack-years, 19.5 being the median pack-years among current smokers), alcohol intake (linear and quadratic term), marital status (married/living as married with partner, separated/divorced, widowed, single/never married) and enrollment source (community health centers vs general population). Knots were placed at quantiles of covariate distributions, equally spaced in sample size.16
For analyses of post-HF survival among those with a diagnosis of incident HF, follow-up time was defined as time from HF diagnosis to death or December 31st 2010 whichever occurred first. When date of death was coincident with date of HF diagnosis, follow-up time was set to 0.5 days. We computed cumulative mortality for both HF cases and non-cases using contingency tables. Age-adjusted estimates of the survivor functions (adjusted to the mean age of SCCS participants diagnosed with HF) were obtained from a stratified Cox model fit and plotted for all race-sex groups. Cox models were used to investigate differences in cumulative hazard for death (all-cause mortality) using white women as the referent group. Model 1 comprised indicator variables for white men, black women and black men and age (restricted cubic splines with 4 knots). Variables included in models 2 and 3 are the same as described previously. P-values for race-by-sex interaction were computed in models for HF incidence and post-HF survival; and a p-value < 0.05 was considered statistically significant. Model assumptions were verified using Schoenfeld residuals and log (−log) plots.
All analyses were performed using STATA (version 12.1, Stata Corp, College Station, Texas, USA) and the ‘rms’ package for R version 3.1.1 (R Core Team 2014).16, 17
Ethics statement
SCCS participants provided written informed consent, and protocols were approved by the Institutional Review Boards of Vanderbilt University Medical Center and Meharry Medical College.
Results
Among the 27,078 SCCS participants included in this study, 68.8% were black, 62.6% were women, 69.7% had annual household income < $15,000 and 38.4% had less than a high school education. The mean (SD) age at enrollment was 55.5 (10.4) years. At baseline, risk factors for HF were common: hypertension (62.5%); diabetes (26.5%); myocardial infarction (8.6%); and obesity, BMI ≥ 30 kg/m2 (44.8%) (Table 1).
Table 1.
Comparison* of baseline characteristics of 27, 078 SCCS participants who were receiving Medicare or Medicaid during follow-up between 2002 and 2010, according to race and sex.
| Overall N = 27,078 | White Women n = 5,252 | White Men n = 3,202 | Black Women n = 11,688 | Black Men n = 6,936 | |
|---|---|---|---|---|---|
| Age (SD), years | 55.5 (10.4) | 57.7 (10.6) | 58.7 (10.5) | 54.4 (10.4) | 54.3 (9.5) |
| Age Categories % | |||||
| 40–54 | 51.2 | 41.9 | 38.0 | 56.1 | 56.1 |
| 55–64 | 22.9 | 23.6 | 22.7 | 21.5 | 24.9 |
| ≥ 65 | 25.9 | 34.5 | 39.3 | 22.4 | 18.9 |
| BMI (kg/m2) (SD) | 30.4 (7.8) | 30.7 (8.2) | 28.7 (6.4) | 32.4 (8.2) | 27.7 (6.1) |
| BMI Categories % | |||||
| < 18.5 | 1.7 | 2.2 | 1.1 | 1.4 | 2.0 |
| 18.5 – < 25.0 | 24.0 | 23.6 | 28.2 | 16.5 | 35.0 |
| 25 – < 30.0 | 29.5 | 28.0 | 36.4 | 25.4 | 34.3 |
| ≥ 30.0 | 44.8 | 46.2 | 34.3 | 56.7 | 28.8 |
| History of MI % | 8.6 | 8.6 | 17.7 | 6.1 | 8.6 |
| History of Stroke % | 9.6 | 10.0 | 10.8 | 9.1 | 9.4 |
| Diabetes % | 26.5 | 24.3 | 23.8 | 29.8 | 23.8 |
| Hypertension % | 62.5 | 57.0 | 56.7 | 67.6 | 60.5 |
| High Cholesterol % | 39.5 | 49.5 | 47.1 | 38.0 | 31.0 |
| Education % | |||||
| < High school (HS) | 38.4 | 32.0 | 29.0 | 40.4 | 44.2 |
| HS/Junior college/VT | 53.1 | 58.7 | 53.1 | 52.1 | 49.0 |
| ≥ College degree | 8.5 | 9.4 | 17.9 | 6.5 | 6.8 |
| Annual Income < $15,000, % | 69.7 | 65.9 | 53.4 | 74.5 | 71.8 |
| Smoking % | |||||
| Never | 34.7 | 37.0 | 21.7 | 45.1 | 21.3 |
| Former | 25.3 | 26.8 | 40.4 | 20.5 | 25.3 |
| Current | 40.1 | 36.2 | 37.9 | 34.5 | 53.4 |
| Alcohol Intake % | |||||
| 0 drink per day | 54.9 | 66.8 | 48.8 | 61.0 | 38.5 |
| >0–2 drinks per day | 33.2 | 29.7 | 35.6 | 31.4 | 37.6 |
| >2 drinks per day | 11.9 | 3.5 | 15.6 | 7.5 | 23.9 |
All comparisons between demographic groups were significant (p=0.02 for stroke; p<0.0001 for all other baseline variables).
VT: Vocational Training; MI: Myocardial Infarction; SD: Standard Deviation
Overall, white men were older and had the highest prevalence of MI and stroke at baseline (Table 1). In contrast, black women were more likely to be obese at baseline and report a history of diabetes and hypertension.
HF incidence
Over a median (25th, 75th percentile) follow-up time of 5.2 (3.1, 6.7) years, 4,341 participants (16%) developed incident HF (IR: 32.8/1000 person-years; 95% CI: 31.8–33.8). White men had the highest age-standardized IR, 37.3/1000 PY, compared with 34.8, 34.9 and 35.6 in white women, black men and black women, respectively (Table 2).
Table 2.
Risk of incident heart failure among participants in the Southern Community Cohort Study, overall and stratified by race and sex.
| Overall N = 27,078 | White Women n = 5,252 | White Men n = 3,202 | Black Women n = 11,688 | Black Men n = 6,936 | |
|---|---|---|---|---|---|
| Incident HF cases (n) | 4,341 | 801 | 511 | 1,940 | 1,089 |
| Person-Years (PY) | 132,500 | 23,339 | 13,934 | 60,639 | 34,589 |
| Cumulative Incidence (%) | 16.0 | 15.3 | 16.0 | 16.6 | 15.7 |
| Incidence Rate/1000PY (95% CI) | |||||
| Crude | 32.8 (31.8, 33.8) | 34.3 (32.0, 36.8) | 36.7 (33.6, 40.0) | 32.0 (30.6, 33.4) | 31.5 (29.7, 33.4) |
| Age-adjusted | 35.1 (34.1, 36.2) | 34.8 (32.4, 37.2) | 37.3 (34.0, 40.6) | 35.6 (33.9, 37.2) | 34.9 (32.7, 37.1) |
| Hazard Ratio (95% CI) | |||||
| Model 1 | 1.00 | 1.04 (0.93, 1.16) | 1.02 (0.94, 1.11) | 0.99 (0.91, 1.09) | |
| Model 2 | 1.00 | 1.02 (0.91, 1.14) | 0.91 (0.83, 0.99) | 1.06 (0.97, 1.17) | |
| Model 3 | 1.00 | 1.09 (0.97, 1.23) | 0.89 (0.82, 0.98) | 1.04 (0.94, 1.15) | |
Model 1: Includes age (restricted cubic splines with 4 knots), race and sex. Model 2: Model 1 + BMI (restricted cubic splines with 4 knots), history of diabetes, hypertension, high cholesterol, MI and stroke (all yes/no). Model 3: Model 2 + annual household income (<$15000, $15000–$24999 & ≥$25000), education (< high school, high school/vocational training/junior college, college degree or higher), smoking (never, former, current < 19.5 pack-years, current ≥ 19.5 pack-years) and alcohol intake (linear and quadratic term), marital status (married/living as married with partner, separated/divorced, widowed, single/never married) and enrollment source (community health centers vs general population). P-value for race×sex interaction = 0.22.
CI: Confidence Interval
In models adjusted for age and other risk factors for HF, black women had a significantly lower risk of HF when compared with white women [HR=0.89; 95% CI: 0.82–0.98]. The risk of HF was similar among white men (HR=1.09; 95% CI: 0.97–1.23) and black men (HR=1.04; 95% CI: 0.94–1.15) compared with white women (Table 2). There was no evidence of race-by-sex interaction [p = 0.22].
Post-HF survival
Among the 4,341 individuals who developed incident HF, 952 died (cumulative mortality = 21.9%) over a median (25th, 75th percentile) post-HF follow-up time of 2.3 (0.9, 4.2) years (Table 3). Men had higher percent mortality than women (29% vs. 18%), with little difference by race. In persons without HF (n= 22,737), there were 1,929 deaths, corresponding to a percent mortality of 8.5%.
Table 3.
Percent mortality of SCCS participants according to heart failure status, overall and stratified by race and sex
| Overall N = 4,341 | White Women n = 801 | White Men n = 511 | Black Women n = 1,940 | Black Men n = 1,089 | |
|---|---|---|---|---|---|
| Deaths (n) | 952 | 144 | 152 | 343 | 313 |
| Percent Mortality (%) | 21.9 | 18.0 | 29.7 | 17.7 | 28.7 |
| Risk of death: Hazard ratio (95% CI) | |||||
| Model 1 | 1.00 (ref) | 1.73 (1.37, 2.17) | 0.91 (0.75, 1.10) | 1.61 (1.32, 1.96) | |
| Model 2 | 1.00 (ref) | 1.60 (1.27, 2.02) | 0.89 (0.73, 1.09) | 1.35 (1.09, 1.65) | |
| Model 3 | 1.00 (ref) | 1.63 (1.27, 2.08) | 0.90 (0.73, 1.12) | 1.38 (1.11, 1.72) | |
Model 1: Includes age (restricted cubic splines with 4 knots); race and sex. Model 2: Model 1 + BMI (restricted cubic splines with 4 knots), history of diabetes, hypertension, high cholesterol, MI and stroke (all yes/no). Model 3: Model 2 + annual household income (<$15000, $15000–$24999 & ≥$25000); education (< high school, high school/vocational training/junior college, college degree or higher), smoking (never, former, current < 19.5 pack-years, current ≥ 19.5 pack-years) and alcohol intake (linear and quadratic term), marital status (married/living as married with partner, separated/divorced, widowed, single/never married) and enrollment source (community health centers vs general population). P-value for race×sex interaction = 0.92.
CI: Confidence Interval
Figure 1 shows age-adjusted survival curves for persons diagnosed with HF stratified by race and sex. The 5-year post-HF survival probability was significantly lower among white men (0.55; 95% CI: 0.49–0.61) and black men (0.64; 95% CI: 0.60–0.67) compared with white women (0.73; 95% CI: 0.69–0.78) and black women (0.77; 95% CI: 0.74–0.79), respectively [p < 0.0001]. Racial differences within sex groups were not statistically significant. Similar patterns were observed for 1-year and 3-year survival probabilities.
Figure 1.
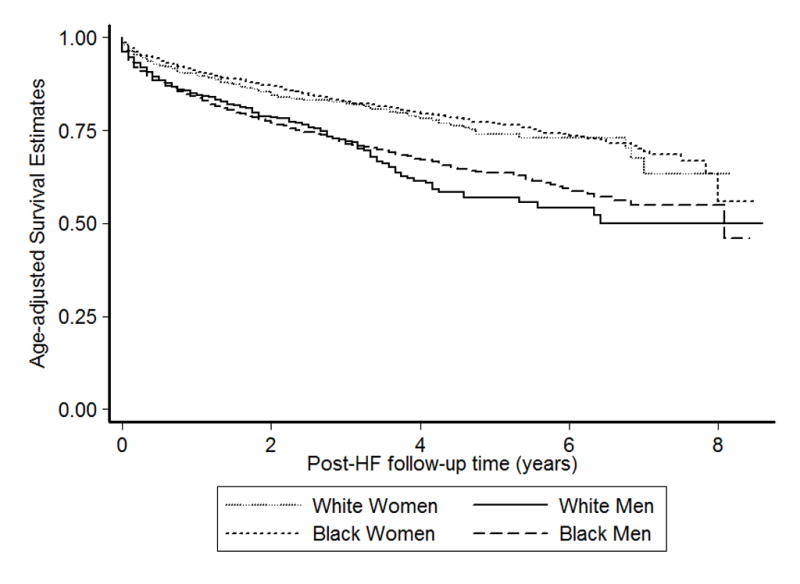
Age-adjusted Survival curves for SCCS participants diagnosed with HF stratified by race and sex. The adjusted survival estimates were computed at the mean age (58 years) of all participants with HF (n = 4341). Compared with white women and black women, white men and black men had significantly lower survival (p<0.0001). The 1-year, 3-year and 5-year age-adjusted survival estimates were (0.91, 0.83, 0.77); (0.90, 0.82, 0.74); (0.84, 0.71, 0.64) and (0.85, 0.73, 0.58) for black women, white women, black men and white men respectively.
Compared with white women, the risk of death was 60% (95% CI: 27%–202%) higher in white men and 35% (95%CI: 9%–65%) higher in black men in analyses adjusted for age, BMI, hypertension, diabetes, high cholesterol, past history of MI/CABG and stroke (Table 3). These findings were robust to further adjustment for lifestyle factors and enrollment source. In contrast, comparisons between black women and white women suggested minimal non-significant relative differences in risk by race in all models. The race-sex interaction term was not statistically significant [p = 0.92].
Discussion
We investigated heart failure incidence and post-HF mortality in a large multi-ethnic low-income sample from the southeastern United States. Our principal findings are: 1) the incidence rate for HF was remarkably high across all race and sex groups in the SCCS, 2) there was no significant difference in age-adjusted incidence rates across groups defined by race and sex but after full adjustment for socioeconomic status and traditional cardiovascular risk factors black women had the lowest risk of HF, and 3) higher post-HF mortality among men with no significant racial differences.
The incidence rates for heart failure in the SCCS exceeded those previously reported from established CVD cohorts (Table 4). In CHS (n = 5,888; age range: ≥ 65 years) for example, the age-standardized HF incidence rates after 10 years of follow-up among white men, black men, white women and black women were 30.2, 19.2, 27.5 and 22.6 per 1000 PY respectively.5 In ARIC (n = 14,933; age range: 45–64), Loehr et al found IRs of 6.0, 9.1, 3.4 and 3.8 per 1000 PY, respectively, in these race-sex groups.8 The FHS and MESA reported even lower IRs (7.2 and 4.2 per 1000 PY in men and women in FHS and 3.1 per 1000 PY overall in MESA).6, 7 The higher SCCS HF incidence could be explained in part by notably higher prevalence of CVD risk factors (in particular hypertension, diabetes, obesity, prior history of MI) in the SCCS study sample at baseline compared with ARIC, CHS, FHS and MESA (Table 5). In addition, SCCS participants were largely of low socioeconomic status, with over two-thirds having annual household income <$15,000. Prior evidence suggests a strong independent association between socioeconomic status and HF risk; 18–21 thus participants in SCCS may be at higher risk of unfavorable societal stressors and an elevated risk of adverse cardiovascular outcomes including HF.
Table 4.
Comparison of heart failure incidence between SCCS, ARIC, MESA and CHS cohorts.
| HF Incidence Rates (IR) per 1000 PY | ||||||||
|---|---|---|---|---|---|---|---|---|
| SCCS* 45–64 yrs |
ARIC8 45–64 yrs |
SCCS* 65–79 yrs |
CHS5† ≥ 65 yrs |
SCCS* 40–79 yrs |
MESA6 45–84 yrs |
|||
| n = 15,321 | n = 14,933 | n = 7,001 | n = 5,888 | n = 27,078 | n = 6,814 | |||
| 5-yr | 10-yr | |||||||
| Overall | 35.8 | 5.7 | 39.5 | 19.3 | 24.0 | Overall | 33.7 | 3.4 |
| White Women | 38.3 | 3.4 | 34.6 | 14.5 | 19.2 | |||
| White Men | 39.7 | 6.0 | 38.3 | 24.9 | 30.2 | Whites | 34.3 | 2.4 |
| Black Women | 35.1 | 8.1 | 42.4 | 19.6 | 22.6 | |||
| Black Men | 34.0 | 9.1 | 41.9 | 23.5 | 27.5 | Blacks | 33.4 | 4.6 |
Incidence rates computed for SCCS participants aged 45–64, 65–79 and 40–79 for comparability with the ARIC, CHS and MESA cohorts respectively. In addition, the rates are standardized to the age distribution of the SCCS study participants within these age ranges.
The tabulated values are computed from values presented in Arnold et al5 and standardized to the age distribution of CHS participants.
ARIC: Atherosclerosis Risk in Communities; CHS: Cardiovascular Health Study; MESA: Multi-ethnic Study of Atherosclerosis; SCCS: Southern Community Cohort Study.
Table 5.
Comparison of baseline characteristics of SCCS, MESA, ARIC and CHS participants
| SCCS (n= 27,078) | ARIC8 (n= 14,993) | CHS5 (n= 5,888) | MESA6 (n = 5,923)† | FHS7 (n=9,405)‡ | |
|---|---|---|---|---|---|
| Age (years)* | 55.5 (10.4) | 54 (6) | 72.8 (5.6) | 61.8 (10.3) | 41 (10) |
| Women (%) | 62.6 | 54 | 57.6 | 53 | 53 |
| Blacks (%) | 68.8 | 27 | 15.7 | 26.1 | ≈ 0 |
| Education (<high school) (%) | 38.4 | 24 | 29.5 | 16 | 56§ |
| BMI (kg/m2)* | 30.4 (7.8) | 27.3 (5.1) | 26.7 (4.7) | 28.0 (5.4) | 24.9 (3.8)|| |
| Obese (BMI > 30) % | 44.8 | 26 | 19 | 32 | 10.8|| |
| Diabetes (%) | 26.5 | 11 | 16.4 | 11.6 | 4.1 |
| Hypertension (%) | 62.5 | 33 | 57.7 | 42 | 7 |
| Myocardial infarction (%) | 8.6 | 4 | 9.6 | n/a | 1.6# |
| Stroke (%) | 9.6 | 1.4 | 4.2 | n/a | 0.5** |
| Ever smoked cigarettes (%) | 65.3 | 58.2 | 53.5 | 49 | 57.3§ |
Tabulated values are mean (SD). n/a = not applicable.
By design, participants enrolled in MESA were free of CVD at baseline so the prevalence of MI and stroke at baseline in this cohort may be best described as not applicable.
The baseline data for the FHS pertains whenever available to both the original cohort and the offspring cohort given this larger sample was utilized to compute HF incidence rates referenced in the manuscript. In the absence of such data, we have presented data from the original cohort (or subsamples thereof) as a proxy and indicated so in each case.
Obtained from a subsample of the parental FHS cohort data (n=1037, 45–62yrs and CHD-free at baseline).
Obtained from a subsample of the parental FHS cohort data (n=2922, 30–62yrs and CHD-free at baseline).
Obtained from the parental FHS cohort data (n=5209) and pertains to the composite of MI, CHD-related sudden death and angina pectoris.
Obtained from the parental FHS cohort data (n=5209).
ARIC: Atherosclerosis Risk in Communities; CHS: Cardiovascular Health Study; SCCS: Southern Community Cohort Study; MESA: Multi-ethnic Study of Atherosclerosis; FHS: Framingham Heart Study.
White men had the highest crude incidence rate of HF in the SCCS, consistent with findings from the CHS. However, minimal differences in age-adjusted incidence rates and HF risk between groups after adjustment for CVD risk factors (except for black women who had significantly lower risk) suggest homogeneity of HF risk profile. Similarly, in ARIC, crude racial and sex differences in incidence density were attenuated by adjustment for CVD risk factors.8
Overall, the 5-year post-HF survival in SCCS was higher than the 52% previously reported (data from the Olmsted county study).3 This may be due in part to the fact that SCCS participants had shorter post-HF follow-up time, were younger at baseline (55.5 vs 74 years) and temporal trends suggesting improved post-HF survival 3 related to recent improvements in therapeutic options. In addition, participants in the Olmsted county study were mostly non-Hispanic Whites who may be at higher risk of HF with reduced ejection fraction (HFrEF), which has a less favorable prognosis compared with heart failure with preserved ejection fraction (HFpEF).22, 23
The relative patterns of post-HF survival for the four demographic subgroups in SCCS were substantially different from those seen in ARIC and CHS. In ARIC, compared with white men and women, black men and women had the lowest survival probability following admission for HF. The 5-year case fatality for white women, white men, black women and black men were 35.8%, 41.2%, 46.1% and 51.8%, respectively. The racial differences were significant, with black men having the highest all-cause mortality following admission, but the differences by sex were non-significant. In CHS, the mortality rate in white women, white men, black women and black men were 35.5, 40.5, 33.6 and 44.4 per 100 PY respectively. After full adjustment for covariates there were no significant racial differences, but women had a 15% lower risk of all-cause mortality [HR: 0.85; 95% CI: 0.73, 0.99].13 In SCCS, white men had the lowest 5-year survival post-HF diagnosis; but after full adjustment, there were mainly sex-differences in post-HF mortality with higher risk of death among men and no significant racial differences. This could be explained in part by the higher prevalence of MI among men. MI is associated with greater risk for the development of HFrEF which is known to have a worse prognosis compared with HFpEF.22, 23 However, MI does not fully account for the higher risk of post HF mortality among men, as this risk persisted even after full adjustment for relevant baseline covariates (including history of MI).
Limitations of our study should be noted. Our study sample may not be representative of the background population of the Southeastern states as the recruitment and sampling scheme utilized by the SCCS was tailored towards low-income, rural and under-insured populations not often included in sizeable numbers in other cohorts investigating chronic disease outcomes. Also, HF was ascertained via linkage with CMS Research Identifiable Files using ICD-9 codes 428.x, rather than independent physician adjudication. However, the diagnosis codes (ICD-9 428.x) algorithm for identification of HF used in this study has been previously validated and utilized in other cohorts.24–26 A review of the detection of HF in administrative claims data that included eight studies conducted among Medicare beneficiaries reported positive predictive values (PPVs) between 76% and 99%, with the majority of the studies reporting PPVs over 90%.24 These codes have also been used with high specificity in a number of studies 25, 26 even though no independent validation was conducted by the SCCS investigators. An over-representation of groups with elevated HF risk (persons > 65 and persons < 65 receiving Medicare) in our SCCS sub-cohort compared with the SCCS base population, may have contributed to higher HF incidence rates than would be expected for the total SCCS cohort. However with the mean age of the total cohort being ≈ 52.6 years27 versus 55.5 years for our sub-cohort, the small age difference between both populations may have had less than dramatic effects on the HF incidence. In addition, with studies suggesting that the sensitivity of ICD-9 code 428.x for HF ascertainment varies between 62.8 and 89%24, 28, it is plausible that we may have underestimated the incidence rate of HF in our sub-cohort. Also, when contrasting the incidence rates between our study and previous CVD cohorts (like ARIC and CHS) we used data for comparable age groups between studies (Table 4). However, the fact that HF represents a myriad of clinical conditions, the lack of universality in the definition of HF and the heterogeneity in the methods for HF ascertainment between studies makes head-to-head comparisons between studies difficult. Our analyses required assumptions regarding the continuous coverage in CMS of persons less than 65 years, raising the possibility of incomplete capturing of HF events in this age stratum of the SCCS cohort. However, we found that over 81.9% of persons aged < 65 who reported CMS coverage at baseline had a claim for any condition within 90 days of being enrolled in SCCS. This suggests that an even greater proportion of participants included in this study filed at least one claim at some point during follow-up from 2002 to 2010 and thus any HF event would likely have been captured if it occurred. Data on baseline covariates (including anthropometric and cardiovascular risk factors) were based on self-report of a physician diagnosis and use of medications (diabetes and hypertension). While self-report may be susceptible to recall and misclassification bias, these methods have been successfully used and validated in large epidemiologic cohorts, including the SCCS. Many of the questions on the SCCS questionnaire were adapted from questionnaires used and validated in other settings; and a series of independent validation studies using biomarkers, repeat interviews or medical records have demonstrated the reliability of the questionnaire within the SCCS population for variables such as smoking status, self-reported diseases including diabetes, height and weight.9
The SCCS cohort is comprised of a substantial number of individuals from minority and low-income populations who are traditionally under-represented in most studies investigating CVD and heart failure in particular. The incidence rates for HF in the SCCS exceeded that of most existing cardiovascular cohorts. Therefore, the SCCS provides an unparalleled opportunity to investigate patterns in HF incidence and mortality among the highest risk individuals. In addition, both black and white participants included in this cohort had minor differences in income and education levels thereby curtailing confounding by socioeconomic differences. The availability of a large sample of participants and HF cases provided the opportunity to adequately explore differential patterns across sex and racial categories. Also, linkage with the NDI and SSA allowed for robust ascertainment of all-cause mortality.
In conclusion, in this low-income multiethnic population, we found higher incidence rates for HF in all race-sex groups than previously reported in other CVD cohorts which was paralleled by high prevalence of CVD risk factors at baseline. This suggests that SCCS can be a unique resource to investigate determinants of HF risk in a segment of the population underrepresented in other existing cohorts.
Clinical Perspective.
Heart failure (HF) is a major public health problem. Most of the epidemiologic data regarding the incidence, prevalence, and survival in HF is derived from cardiovascular disease (CVD) cohorts that enrolled mostly middle-class individuals and with relatively low representation of black individuals. However, the greatest burden of HF risk factors resides within individuals of lower socioeconomic status, particularly within the southeastern United States. Therefore, we investigated HF incidence and post-HF survival by race and sex among 27,078 low-income individuals enrolled in the Southern Community Cohort Study (SCCS). Over a median follow-up of 5.2 years, 4,341 participants were diagnosed with HF. The age-standardized incidence rates were 34.8, 37.3, 34.9 and 35.6 PY/1000 in white women, white men, black men and black women, respectively, which are approximately two to ten times higher than previously reported from cohorts such as the Cardiovascular Health Study (CHS), Atherosclerosis Risk in Communities (ARIC), and the Multi-Ethnic Study of Atherosclerosis (MESA). Among incident HF cases in the SCCS, 952 deaths occurred over a median follow-up of 2.3 years. Compared with women, men had lower post-HF survival; hazard ratios and 95% confidence intervals were 1.63 (1.27–2.08), 1.38 (1.11–1.72) and 0.90 (0.73–1.12) for white men, black men and black women compared with white women. Individuals of lower socioeconomic status in the southeastern United States are at particularly high risk for the development of HF. In order to curb the HF epidemic, population and individual level resources should be directed toward this high risk segment of the population.
Acknowledgments
The authors would like to thank all the participants of the Southern Community Cohort Study, the research team of the SCCS as well as the entire team of the International Epidemiology Institute.
Sources of Funding: The Southern Community Cohort Study was supported by the National Cancer Institute (grant R01 CA 092447) and supplemental funding from the American Recovery and Reinvestment Act (3R01 CA029447-0851).
Footnotes
Disclosures: None.
References
- 1.Ambrosy AP, Fonarow GC, Butler J, Chioncel O, Greene SJ, Vaduganathan M, Nodari S, Lam CS, Sato N, Shah AN, Gheorghiade M. The global health and economic burden of hospitalizations for heart failure: lessons learned from hospitalized heart failure registries. J Am Coll Cardiol. 2014;63:1123–1133. doi: 10.1016/j.jacc.2013.11.053. [DOI] [PubMed] [Google Scholar]
- 2.Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, Das SR, de Ferranti S, Despres JP, Fullerton HJ, Howard VJ, Huffman MD, Isasi CR, Jimenez MC, Judd SE, Kissela BM, Lichtman JH, Lisabeth LD, Liu S, Mackey RH, Magid DJ, McGuire DK, Mohler ER, 3rd, Moy CS, Muntner P, Mussolino ME, Nasir K, Neumar RW, Nichol G, Palaniappan L, Pandey DK, Reeves MJ, Rodriguez CJ, Rosamond W, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Woo D, Yeh RW, Turner MB. Heart Disease and Stroke Statistics-2016 Update: A Report From the American Heart Association. Circulation. 2016;133:e38–360. doi: 10.1161/CIR.0000000000000350. [DOI] [PubMed] [Google Scholar]
- 3.Roger VL, Weston SA, Redfield MM, Hellermann-Homan JP, Killian J, Yawn BP, Jacobsen SJ. Trends in heart failure incidence and survival in a community-based population. JAMA. 2004;292:344–350. doi: 10.1001/jama.292.3.344. [DOI] [PubMed] [Google Scholar]
- 4.Heidenreich PA, Albert NM, Allen LA, Bluemke DA, Butler J, Fonarow GC, Ikonomidis JS, Khavjou O, Konstam MA, Maddox TM, Nichol G, Pham M, Pina IL, Trogdon JG American Heart Association Advocacy Coordinating C, Council on Arteriosclerosis T, Vascular B, Council on Cardiovascular R, Intervention, Council on Clinical C, Council on E, Prevention and Stroke C. Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circ Heart Fail. 2013;6:606–619. doi: 10.1161/HHF.0b013e318291329a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Arnold AM, Psaty BM, Kuller LH, Burke GL, Manolio TA, Fried LP, Robbins JA, Kronmal RA. Incidence of cardiovascular disease in older Americans: the cardiovascular health study. J Am Geriatr Soc. 2005;53:211–218. doi: 10.1111/j.1532-5415.2005.53105.x. [DOI] [PubMed] [Google Scholar]
- 6.Bahrami H, Kronmal R, Bluemke DA, Olson J, Shea S, Liu K, Burke GL, Lima JA. Differences in the incidence of congestive heart failure by ethnicity: the multi-ethnic study of atherosclerosis. Arch Intern Med. 2008;168:2138–2145. doi: 10.1001/archinte.168.19.2138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ho KK, Pinsky JL, Kannel WB, Levy D. The epidemiology of heart failure: the Framingham Study. J Am Coll Cardiol. 1993;22:6A–13A. doi: 10.1016/0735-1097(93)90455-a. [DOI] [PubMed] [Google Scholar]
- 8.Loehr LR, Rosamond WD, Chang PP, Folsom AR, Chambless LE. Heart failure incidence and survival (from the Atherosclerosis Risk in Communities study) Am J Cardiol. 2008;101:1016–1022. doi: 10.1016/j.amjcard.2007.11.061. [DOI] [PubMed] [Google Scholar]
- 9.Signorello LB, Hargreaves MK, Blot WJ. The Southern Community Cohort Study: investigating health disparities. J Health Care Poor Underserved. 21:26–37. doi: 10.1353/hpu.0.0245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lipworth L, Mumma MT, Cavanaugh KL, Edwards TL, Ikizler TA, Tarone RE, McLaughlin JK, Blot WJ. Incidence and predictors of end stage renal disease among low-income blacks and whites. PLoS One. 7:e48407. doi: 10.1371/journal.pone.0048407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chronic Conditions Data Warehouse. [Accessed November 15, 2016];Centers for Medicare and Medicaid Services (CMS) research data. Available online at https://www.ccwdata.org/web/guest/technical-guidance-documentation.
- 12.Agarwal SK, Chambless LE, Ballantyne CM, Astor B, Bertoni AG, Chang PP, Folsom AR, He M, Hoogeveen RC, Ni H, Quibrera PM, Rosamond WD, Russell SD, Shahar E, Heiss G. Prediction of incident heart failure in general practice: the Atherosclerosis Risk in Communities (ARIC) Study. Circ Heart Fail. 5:422–429. doi: 10.1161/CIRCHEARTFAILURE.111.964841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Parashar S, Katz R, Smith NL, Arnold AM, Vaccarino V, Wenger NK, Gottdiener JS. Race, gender, and mortality in adults > or =65 years of age with incident heart failure (from the Cardiovascular Health Study) Am J Cardiol. 2009;103:1120–1127. doi: 10.1016/j.amjcard.2008.12.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sathiakumar N, Delzell E, Abdalla O. Using the National Death Index to obtain underlying cause of death codes. J Occup Environ Med. 1998;40:808–813. doi: 10.1097/00043764-199809000-00010. [DOI] [PubMed] [Google Scholar]
- 15.StataCorp. Stata Survival Analysis and Epidemiological Tables Reference Manual. College Station, TX: Stata Press; 2013. Release 13. [Google Scholar]
- 16.Harrell FE., Jr . Regression Modelling Strategies with Applications to Linear Models, Logistic and Ordinal Regression, and Survival Analysis. 2. New York: Springer; 2015. [Google Scholar]
- 17.R Development Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing; Vienna, Austria: 2014. http://www.R-project.org. [computer program] [Google Scholar]
- 18.Gottdiener JS, Arnold AM, Aurigemma GP, Polak JF, Tracy RP, Kitzman DW, Gardin JM, Rutledge JE, Boineau RC. Predictors of congestive heart failure in the elderly: the Cardiovascular Health Study. J Am Coll Cardiol. 2000;35:1628–1637. doi: 10.1016/s0735-1097(00)00582-9. [DOI] [PubMed] [Google Scholar]
- 19.Roberts CB, Couper DJ, Chang PP, James SA, Rosamond WD, Heiss G. Influence of life-course socioeconomic position on incident heart failure in blacks and whites: the Atherosclerosis Risk in Communities Study. Am J Epidemiol. 172:717–727. doi: 10.1093/aje/kwq193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.He J, Ogden LG, Bazzano LA, Vupputuri S, Loria C, Whelton PK. Risk factors for congestive heart failure in US men and women: NHANES I epidemiologic follow-up study. Arch Intern Med. 2001;161:996–1002. doi: 10.1001/archinte.161.7.996. [DOI] [PubMed] [Google Scholar]
- 21.Ingelsson E, Lind L, Arnlov J, Sundstrom J. Socioeconomic factors as predictors of incident heart failure. J Card Fail. 2006;12:540–545. doi: 10.1016/j.cardfail.2006.05.010. [DOI] [PubMed] [Google Scholar]
- 22.Writing Committee M; Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE, Jr, Drazner MH, Fonarow GC, Geraci SA, Horwich T, Januzzi JL, Johnson MR, Kasper EK, Levy WC, Masoudi FA, McBride PE, McMurray JJ, Mitchell JE, Peterson PN, Riegel B, Sam F, Stevenson LW, Tang WH, Tsai EJ, Wilkoff BL American College of Cardiology Foundation/American Heart Association Task Force on Practice G. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013;128:e240–327. doi: 10.1161/CIR.0b013e31829e8776. [DOI] [PubMed] [Google Scholar]
- 23.Fonarow GC, Stough WG, Abraham WT, Albert NM, Gheorghiade M, Greenberg BH, O’Connor CM, Sun JL, Yancy CW, Young JB Investigators O-H and Hospitals. Characteristics, treatments, and outcomes of patients with preserved systolic function hospitalized for heart failure: a report from the OPTIMIZE-HF Registry. J Am Coll Cardiol. 2007;50:768–777. doi: 10.1016/j.jacc.2007.04.064. [DOI] [PubMed] [Google Scholar]
- 24.Goff DC, Jr, Pandey DK, Chan FA, Ortiz C, Nichaman MZ. Congestive heart failure in the United States: is there more than meets the I(CD code)? The Corpus Christi Heart Project. Arch Intern Med. 2000;160:197–202. doi: 10.1001/archinte.160.2.197. [DOI] [PubMed] [Google Scholar]
- 25.Rector TS, Wickstrom SL, Shah M, Thomas Greeenlee N, Rheault P, Rogowski J, Freedman V, Adams J, Escarce JJ. Specificity and sensitivity of claims-based algorithms for identifying members of Medicare+Choice health plans that have chronic medical conditions. Health Serv Res. 2004;39:1839–1857. doi: 10.1111/j.1475-6773.2004.00321.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Saczynski JS, Andrade SE, Harrold LR, Tjia J, Cutrona SL, Dodd KS, Goldberg RJ, Gurwitz JH. A systematic review of validated methods for identifying heart failure using administrative data. Pharmacoepidemiol Drug Saf. 21(Suppl 1):129–40. doi: 10.1002/pds.2313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cohen SS, Signorello LB, Cope EL, McLaughlin JK, Hargreaves MK, Zheng W, Blot WJ. Obesity and all-cause mortality among black adults and white adults. Am J Epidemiol. 2012;176:431–442. doi: 10.1093/aje/kws032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fisher ES, Whaley FS, Krushat WM, Malenka DJ, Fleming C, Baron JA, Hsia DC. The accuracy of Medicare’s hospital claims data: progress has been made, but problems remain. Am J Publ Health. 1992;82:243–248. doi: 10.2105/ajph.82.2.243. [DOI] [PMC free article] [PubMed] [Google Scholar]


