Abstract
Objective
Proximal junctional kyphosis (PJK) is radiologic finding, and is defined as kyphosis of >10° at the proximal end of a construct. The aim of this study is to identify factors associated with PJK after segmental spinal instrumented fusion in adults with spinal deformity with a minimum follow-up of 2 years.
Methods
A total of 49 cases of adult spinal deformity treated by segmental spinal instrumented fusion at two university hospitals from 2004 to 2011 were enrolled in this study. All enrolled cases included at least 4 or more levels from L5 or the sacral level. The patients were divided into two groups based on the presence of PJK during follow-up, and these two groups were compared to identify factors related to PJK.
Results
PJK was observed in 16 of the 49 cases. Age, sex and mean follow-up duration were not statistically different between two groups. However, mean bone marrow density (BMD) and mean back muscle volume at the T10 to L2 level was significantly lower in the PJK group. Preoperatively, the distance between the C7 plumb line and uppermost instrumented vertebra (UIV) were no different in the two groups, but at final follow-up a significant intergroup difference was observed. Interestingly, spinal instrumentation factors, such as, receipt of a revision operation, the use of a cross-link, and screw fracture were no different in the two groups at final follow-up.
Conclusion
Preoperative BMD, sagittal imbalance at UIV, and thoracolumbar muscle volume were found to be strongly associated with the presence of PJK.
Keywords: Proximal junctional kyphosis, Adult spinal deformity, Complication, Back muscle, Osteoporosis, Sarcopenia
INTRODUCTION
Proximal junctional kyphosis (PJK) is traditionally defined as a proximal junctional sagittal Cobb angle change of ≥10° versus the preoperative value. Although no consensus has been reached, the majority of authors have used kyphosis of ≥10° between the lower endplate of the uppermost instrumented vertebra (UIV) and the upper endplate of the two supra-adjacent vertebrae as a definition5). PJK is a post-surgical radiographic status observed in the sagittal plane following multi-level fusion surgery for spinal deformity. In a broader sense, PJK is a type of adjacent segment disease associated with spinal fusion and often occurs after deformity correction. Furthermore, PJK results in poor surgical results due to pain, deformity, instability, motion difficulties, and potential neurologic deficits.
To minimize PJK, it is important that associated risk factors be identified. To date, several such factors have been described in the literature, namely, older age, inadequate restoration of global sagittal balance, combined anterior-posterior surgery, fusion to the sacrum, posterior only spinal fusion rather than anterior instrumentation, and low bone mineral density (BMD)9,10,12,15,19).
Skeletal muscles, including flexor and extensors, produce movements of the trunk and maintain body balance, and degeneration and atrophy of thoracolumbar extensor muscles lead to fatty replacement and back kyphosis as manifested by lumbar degenerative kyphosis or flat back syndrome. Furthermore, sarcopenia may affect skeletal stability or surgical outcome, but the impact of thoracolumbar muscle volume on PJK has not been previously evaluated. The aim of this study was to identify the factors responsible for PJK after spinal instrumented fusion in adult spinal deformity with a minimum follow-up of 2 years.
MATERIALS AND METHODS
This study was conducted by retrospectively reviewing the medical charts and radiologic data of 49 patients with spinal deformity, including lumbar degenerative kyphosis, diffuse lumbar scoliosis, and post-operative flat-back syndrome, that underwent posterior fusion with instrumentation from January 2004 to December 2011 at two university hospitals. Those with infection or malignancy were excluded. The minimum follow-up was 2 years and mean follow-up was 3.6 years. All 49 patients underwent multi-level fusion surgery at more than 4 levels from L5 or the sacral level. No complication occurred in any patient during the year following surgery.
Radiographic PJK was defined as angle change of >10° on dynamic plain radiographs at the proximal end of a construct14). Preoperative evaluations included plain radiographic examinations and magnetic resonance imaging (MRI), a postoperative radiograph examination was conducted before discharge (early postop, EP), and then annually. Postoperative radiographs included standing antero-posterior, lateral whole spine, and dynamic flexion/extension views, and were used to determine the presence or not of PJK at proximal adjacent level from instrumentation. The 49 patients were divided in terms of two groups (PJK and non-PJK groups) based on the presence of PJK at final follow-up. These two groups were compared with respect to demographic factors, BMD, sagittal plane angle parameter, pelvic parameter, instrumentation factor, surgical approach, and the back muscle volume of thoracolumbar junction. Group BMD values were compared using T scores determined by Dual energy X-ray absorptiometry.
Sagittal plane angle parameters17)
C7PL was defined distance between C7 plumb line which is the vertical line originating the center of the C7 vertebral body and the posterior superior corner of S1, and its length was measured preoperatively and at final follow-up. Distance from the center of the upper instrumented vertebra (UIV) to C7PL was also measured at early postoperatively and final follow-up (Fig. 1).
Fig. 1.
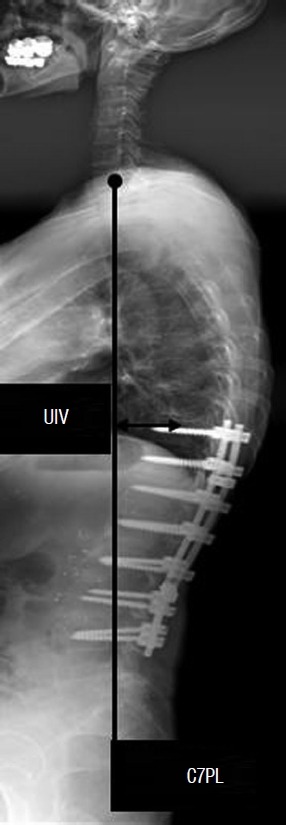
C7PL was defined distance between C7 plumb line which is the vertical line originating the center of the C7 vertebral body and the posterior superior corner of S1, and its length was measured preoperatively and at ÿnal follow-up. The distance between the center of the UIV and C7PL was also measured early postoperatively and at final follow-up. C7PL: C7 plumb line, UIV: uppermost instrumented vertebra.
Pelvic parameters13)
Pelvic incidence (PI) is defined as the angle between the perpendicular to the sacral plate at its midpoint and the line connecting this point to the middle axis of the femoral head. Sacral slope (SS) is the angle between the superior endplate of S1 and the horizontal line. Pelvic tilt (PT) is the angle between the line connecting the midpoint of the sacral plate to center of the axis of femoral heads, and the vertical line.
Surgical approach and instrumentation factors
Data related to surgical procedures, including surgical approach (concomitant anterior-posterior or not), cross-link usage, whether screws and rods were fractured or not, and UIV level, were also analyzed.
Thoracolumbar junction back muscle volume1)
Contiguous T2-weighted MRI scans were acquired in 5-mm slices using a 1.5-Tesla GE (General Electric, Milwaukee, WI, USA) twin-speed scanner from T10 to L2. Patients were positioned supine on the imaging table and numbers of scan slices were adjusted to include the anatomic extent of muscles of interest.
Cross-section areas were calculated using software installed in the MRI unit in the following way. After choosing a region of interest in the axial plane, the range of interest (ROI) was enlarged on a monitor screen as much as necessary and subjected to planimetry. All measurements were obtained using a Picture Archiving and Communication System and its software (PACS, INFINITT, Seoul, Korea) (Fig. 2).
Fig. 2.

Thoracolumbar back muscle volumes were measured from T10 to L2 in T2 weighted magnetic resonance images.
Statistical analysis
Data were analyzed using SPSS for Windows (version 14.0; SPSS Inc., Chicago, IL, USA), and statistical significance was accepted for p values<0.05.
RESULTS
Demographic factors
The PJK group and non-PJK group contained 16 and 33 patients, respectively. Women dominated in both groups – 2 men and 14 women in PJK group and 4 men and 29 women in non-PJK group. Mean overall age was 62.5 in PJK group (range of 56–69) and 61.9 in non-PJK group. Sexual distributions and ages were non-significantly different (Table 1).
Table 1.
Patient demographics
| Variable | Group A (n=16) | Group B (n=33) | p-value |
|---|---|---|---|
| PJK | Non-PJK | ||
| Sex (male: female) | 2: 14 | 4: 29 | 0.104 |
| Age (mean, years) | 62.5 (56–69) | 61.9 (54–69) | 0.408 |
| Mean follow up period (months) | 47.7±23.4 | 45.6±25.6 | 0.392 |
| BMD (T score) | −2.30±0.85 | −1.01±0.67 | 0.027 |
| C7PL in Pre-Op (mm) | 89.85±51.60 | 58.97±66.98 | 0.111 |
| C7PL in FF (mm) | 71.96±58.04 | 55.83±37.00 | 0.423 |
| UIV distance to C7PL in EP (mm) | 1.9±6.0 | 0.5±3.0 | 0.444 |
| UIV distance to C7PL in FF (mm) | −5.5±5.4 | −2.5±3.4 | 0.019 |
| SS in Pre-OP (°) | 15.38±5.88 | 16.91±6.59 | 0.433 |
| PT in Pre-Op (°) | 42.06±12.00 | 41.21±9.16 | 0.785 |
| PI in Pre-Op (°) | 57.94±12.70 | 58.45±8.37 | 0.865 |
| Anterior-posterior | 6 (37.5) | 16 (48.4) | 0.468 |
| Use of cross-links | 13 (81.2) | 26 (78.8) | 0.841 |
| Screw & rod fracture | 5 (31.2) | 10 (30.0) | 0.946 |
| UIV Level (T10) | 2 (12.5) | 5 (15.1) | 0.804 |
| UIV Level (T11) | 3 (18.8) | 4 (12.2) | 0.534 |
| UIV Level (T12) | 5 (31.2) | 12 (36.3) | 0.724 |
| UIV Level (L1) | 4 (25.0) | 6 (18.2) | 0.579 |
| UIV Level (L2) | 2 (12.5) | 6 (18.2) | 0.614 |
| Muscle volume, T10 (mm2) | 1042±149 | 1315±143 | <0.001 |
| Muscle volume, T11 (mm2) | 1113±101 | 1445±176 | <0.001 |
| Muscle volume, T12 (mm2) | 1227±111 | 1603±230 | <0.001 |
| Muscle volume, L1 (mm2) | 1333±99 | 1783±326 | <0.001 |
| Muscle volume, L2 (mm2) | 1443±175 | 1905±303 | <0.001 |
Values are presented as number (%) or mean±standard deviation. PJK: proximal junctional kyphosis, BMD: bone mineral density, UIV: upper instrumented vertebra, C7PL: C7 plumb line, EP: early post-op, FF: final follow-up, SS: sacral slope, PT: pelvic tilt, PI: pelvic incidence
Bone mineral density
Mean T score was −2.30±0.85 in PJK group and −1.01±0.67 in non-PJK group. BMD was significantly lower in the PJK group than in the non-PJK group (p=0.027) (Table 1).
Sagittal plane angle parameters
Mean C7PL before surgery was 89.95±51.60 mm in PJK group and 58.97±66.98 mm in non-PJK group, and mean C7PL at final follow-up was 71.96±58.04 mm in PJK group and 55.83±37.00 mm in non-PJK group. Mean distance from UIV to C7PL before surgery was 1.9±6.0 mm in PJK group and 0.5±3.0 mm in non-PJK group, and mean distance from UIV to C7PL at final follow-up was −5.5±5.4 mm in PJK group and −2.5±3.4 mm in non-PJK group. No intergroup difference was observed for mean C7PL at pre-op or at final follow-up and for mean UIV distance to C7PL distance at early post-op. However, mean UIV distance to C7PL distance at final follow-up was significantly greater in PJK group (p=0.019) (Table 1).
Pelvic parameters
Mean preoperative PI was 57.94±12.70° in PJK group and 58.45±8.37° in non-PJK group, and mean preoperative SS was 15.38±5.88° in PJK group and 16.91±6.59° in non-PJK group. Mean preoperative PT was 42.06±12.00° in PJK group and 41.21±9.16° in non-PJK group. Pre-op mean PI, SS, and PT were not significantly different in the two groups (Table 1).
Surgical approach and instrumentation factors
Concomitant anterior-posterior surgery was performed in 6 of 16 (37.5%) in PJK group and in 16 of 33 (48.4%) in non-PJK group. Cross-linkages were used in 13 of 16 (81.2%) in PJK group and in 26 of 33 (78.8%) in non-PJK group. Instrument fractures occurred in 5 of 16 (31.2%) in PJK group and in 10 of 33 (30.0%) in non-PJK group. In PJK group, number of UIV levels were 2 of 16 (T10, 12.5%), 3 of 16 (T11, 18.8%), 5 of 16 (T12, 31.2%), 4 of 16 (L1, 25.0%), and 2 of 16 (L2, 12.5%), and in non-PJK group were 5 of 33 (T10, 15.1%), 4 of 33 (T11, 12.2%), 12 of 33 (T12, 36.3%), 6 of 33 (L1, 18.2%), and 6 of 33 (L2, 18.2%). Surgical approaches, cross-link-usage, instrument fracture, and UIV level were non-significantly different in the two groups (Table 1).
Thoracolumbar junction back muscle volume
Mean thoracolumbar junction back muscle volumes in PJK and non-PJK group were 1042±149 and 1315±143 mm2, respectively, at T10, 1113±101 and 1445±176 mm2 at T11, 1227±111 and 1603±230 mm2 at T12, 1333±99 and 1783±326 mm2 at L1, and 1443±175 and 1905±303 mm2, respectively, at L2. Thoracolumbar junction back muscle volume was significant lower in the PJK group than in the non-PJK group (p<0.001) (Table 1, Fig. 3). The correlation of thoracolumbar junction back muscle volume and preoperative sagittal imbalance in overall group was also evaluated. The mean muscle volume of T10 to L2 showed negative correlation with mean C7PL before surgery in the overall group. But the correlation was not strong with Pearson correlation −0.313 (p=0.029) (Fig. 4).
Fig. 3.
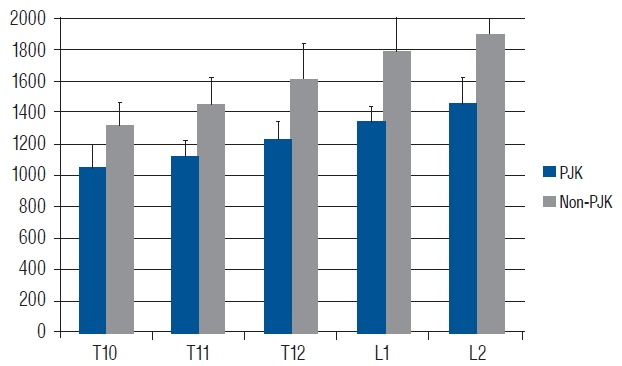
Di°erences in muscle volume (mm2) of two study groups. PJK: proximal junctional kyphosis.
Fig. 4.
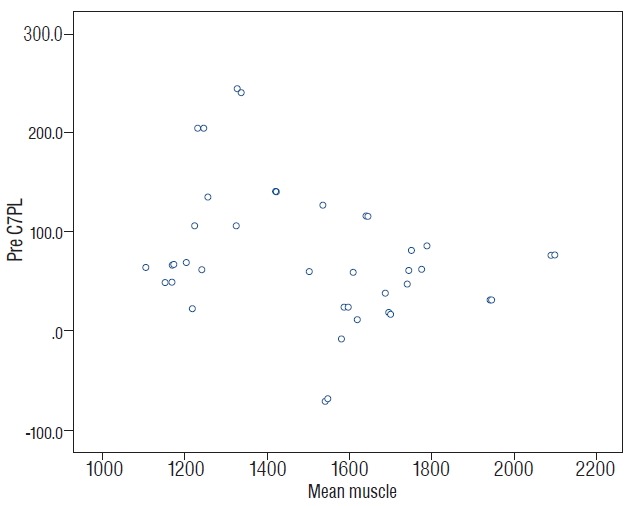
Scatter plot showed correlation between preoperative C7PL (mm) and mean muscle volume (mm2).
DISCUSSION
The present study confirms preoperative BMD and thoracolumbar back muscle volume are related to the presence of PJK after segmental spinal instrumented fusion in adults with spinal deformity, and that although sagittal balance is achieved immediately after surgery, newly developed sagittal imbalance after deformity surgery is associated with increased PJK at final follow-up.
PJK is a major potential complication of adult spinal deformity surgery5,6,10). Many studies have identified risk factors of the postoperative development of PJK3,5,6,9,10,12,15,19), such as, patient age, bone quality, and inadequate restoration of global sagittal balance requiring substantial correction to restore global alignment. Furthermore, UIV level may play a role because the UIV in many deformity cases ends at the thoracolumbar junction, a transition zone between the mobile lumbar spine and the less mobile thoracic spine and rib cage. It is also possible that body mass index contributes to the development of PJK as the UIV may be biomechanically stressed in larger patients.
Paraspinal muscles including flexor and extensors produce trunk movements and maintain body balance. Takemitsu et al. measured the cross-sectional areas of paraspinal muscles in patients with lumbar degenerative kyphosis, which lumbar extensor muscles overwork to maintain secure balance by CT, and weakness of spinal extensors is caused by definite atrophy, which may produce round back kyphosis and more fatty replacement as compared with normal individuals8,18). Trunk muscular effort is directly linked to posture of trunk and pelvis4,7). Harrison et al. showed that anterior trunk translation in standing subjects increases extensor muscle activity and loads and stresses acting on intervertebral discs in the lower thoracic and lumbar regions7). It has been established altered biomechanical stresses on an intervertebral disc may cause adjacent segment degeneration. In the present study, thoracolumbar back muscle volume was smaller in the PJK group than in the non-PJK group. We could know relation between preoperative thoracolumbar back muscle volume and PJK, even if this result could not answer what is the preceding between two factors.
Osteoporosis is a characterized by reduced bone strength, increased skeletal fragility, and fracture susceptibility. Furthermore, a weak bone/screw interface is a known risk factor of screw pull-out after a spinal instrumentation procedure, and numerous studies have concluded low bone mineral density is a risk factor for adjacent segment disease after spinal fusion. Terracciano et al.2) showed muscle atrophy is prominent in osteoporosis and preferentially affects type II muscle fibers with little or no impact on type I fibers, and that this atrophy is associated with BMD, which suggests disease severity plays a central role in the pathogenesis of osteoporosis-related muscle atrophy. In the present study, patients allocated to two groups based on the presence of absence of PJK. Group comparisons showed bone quality and muscle mass were poor in the PJK group. Osteoporosis and sarcopenia are aging related, but in the present study age was not found to be related with PJK. Decreased skeletal muscle volume increases axial loading during the maintenance of skeletal stability, and osteoporotic bone cannot sufficiently support skeletal loading, which means back muscles are exposed and a vicious cycle is initiated. Furthermore, reduced screw pull-out strength imposes a heavy burden on back muscles and causes micro-motion of proximal instrumentation. Resultantly, lower BMD in combination reduced thoracolumbar back muscle volume might in combination induce skeletal instability and facilitate proximal junctional kyphosis.
Line of gravity and center of gravity have been studied by several authors11,16). In a stabilized standing position, the C7 plumb line is located behind the gravity line in the sagittal plane. However, in most pathological situations, the center of gravity is too far forward with a mechanical axis located in front of the femoral heads, and this imbalance will induce body reactions. The present study shows UIV distance from the C7 plumb line was greater in the PJK group. Furthermore, center of gravity is located more frontally for greater UIV distances and stress loading on proximal instrumentation might be dependent on UIV distance, and thus, when compensatory mechanisms, such as, thoracic kyphosis, hip or knee bending cannot tolerate a critical point, PJK might occur.
The present study has some limitations that require consideration. First it is limited by its retrospective design and sample size. Second, fat volume could not be excluded from muscle mass measurements because of technical limitations. Third, we did not examine the effects of bone fusion. Accordingly, we suggest a well designed prospective study be performed to identify more precisely factors that contribute to PJK, and that a biomechanical study be undertaken to confirm our results. Nevertheless, the study provides surgeons with information useful for deciding on instrumentation level and surgical approach.
CONCLUSION
The incidence of PJK following multi-level fusion surgery was higher related to preoperative lower BMD, thoracolumbar back muscle volume, and insufficient postoperative sagittal balance. Surgeons should make treatment plan carefully to prevent PJK after multi-level fusion surgery, especially in cases of osteoporosis and sarcopenia. We believe the result of this study will be useful for preventing PJK after surgery, but more studies with long-term follow-up and more subjects are also needed in the future.
Acknowledgements
This work was supported by INHA UNIVERSITY Research Grant.
References
- 1.Beneke R, Neuerburg J, Bohndorf K. Muscle cross-section measurement by magnetic resonance imaging. Eur J Appl Physiol Occup Physiol. 1991;63:424–429. doi: 10.1007/BF00868073. [DOI] [PubMed] [Google Scholar]
- 2.Terracciano C, Celi M, Lecce D, Baldi J, Rastelli E, Lena E, et al. Differential features of muscle fiber atrophy in osteoporosis and osteoarthritis. Osteoporos Int. 2013;24:1095–1100. doi: 10.1007/s00198-012-1990-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cho SK, Shin JI, Kim YJ. Proximal junctional kyphosis following adult spinal deformity surgery. Eur Spine J. 2014;23:2726–2736. doi: 10.1007/s00586-014-3531-4. [DOI] [PubMed] [Google Scholar]
- 4.Cholewicki J, Panjabi MM, Khachatryan A. Stabilizing function of trunk flexor-extensor muscles around a neutral spine posture. Spine (Phila Pa 1976) 1997;22:2207–2212. doi: 10.1097/00007632-199710010-00003. [DOI] [PubMed] [Google Scholar]
- 5.Glattes RC, Bridwell KH, Lenke LG, Kim YJ, Rinella A, Edwards C., 2nd Proximal junctional kyphosis in adult spinal deformity following long instrumented posterior spinal fusion: incidence, outcomes, and risk factor analysis. Spine (Phila Pa 1976) 2005;30:1643–1649. doi: 10.1097/01.brs.0000169451.76359.49. [DOI] [PubMed] [Google Scholar]
- 6.Hyun SJ, Rhim SC. Clinical outcomes and complications after pedicle subtraction osteotomy for fixed sagittal imbalance patients: a long-term follow-up data. J Korean Neurosurg Soc. 2010;47:95–101. doi: 10.3340/jkns.2010.47.2.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Harrison DE, Colloca CJ, Harrison DD, Janik TJ, Haas JW, Keller TS. Anterior thoracic posture increases thoracolumbar disc loading. Eur Spine J. 2005;14:234–242. doi: 10.1007/s00586-004-0734-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kang CH, Shin MJ, Kim SM, Lee SH, Lee CS. MRI of paraspinal muscles in lumbar degenerative kyphosis patients and control patients with chronic low back pain. Clin Radiol. 2007;62:479–486. doi: 10.1016/j.crad.2006.12.002. [DOI] [PubMed] [Google Scholar]
- 9.Kim HJ, Bridwell KH, Lenke LG, Park MS, Ahmad A, Song KS, et al. Proximal junctional kyphosis results in inferior SRS pain subscores in adult deformity patients. Spine (Phila Pa 1976) 2013;38:896–901. doi: 10.1097/BRS.0b013e3182815b42. [DOI] [PubMed] [Google Scholar]
- 10.Kim YJ, Bridwell KH, Lenke LG, Glattes CR, Rhim S, Cheh G. Proximal junctional kyphosis in adult spinal deformity after segmental posterior spinal instrumentation and fusion: minimum five-year follow-up. Spine (Phila Pa 1976) 2008;33:2179–2184. doi: 10.1097/BRS.0b013e31817c0428. [DOI] [PubMed] [Google Scholar]
- 11.Le Huec JC, Saddiki R, Franke J, Rigal J, Aunoble S. Equilibrium of the human body and the gravity line: the basics. Eur Spine J. 2011;20(Suppl 5):558–563. doi: 10.1007/s00586-011-1939-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee GA, Betz RR, Clements DH, 3rd, Huss GK. Proximal kyphosis after posterior spinal fusion in patients with idiopathic scoliosis. Spine (Phila Pa 1976) 1999;24:795–799. doi: 10.1097/00007632-199904150-00011. [DOI] [PubMed] [Google Scholar]
- 13.Legaye J, Duval-Beaupère G, Hecquet J, Marty C. Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J. 1998;7:99–103. doi: 10.1007/s005860050038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lonner BS, Newton P, Betz R, Scharf C, O’Brien M, Sponseller P, et al. Operative management of Scheuermann’s kyphosis in 78 patients: radiographic outcomes, complications, and technique. Spine (Phila Pa 1976) 2007;32:2644–2652. doi: 10.1097/BRS.0b013e31815a5238. [DOI] [PubMed] [Google Scholar]
- 15.Maruo K, Ha Y, Inoue S, Samuel S, Okada E, Hu SS, et al. Predictive factors for proximal junctional kyphosis in long fusions to the sacrum in adult spinal deformity. Spine (Phila Pa 1976) 2013;38:E1469–E1476. doi: 10.1097/BRS.0b013e3182a51d43. [DOI] [PubMed] [Google Scholar]
- 16.Roussouly P, Gollogly S, Noseda O, Berthonnaud E, Dimnet J. The vertical projection of the sum of the ground reactive forces of a standing patient is not the same as the C7 plumb line: a radiographic study of the sagittal alignment of 153 asymptomatic volunteers. Spine (Phila Pa 1976) 2006;31:E320–E325. doi: 10.1097/01.brs.0000218263.58642.ff. [DOI] [PubMed] [Google Scholar]
- 17.Roussouly P, Pinheiro-Franco JL. Sagittal parameters of the spine: biomechanical approach. Eur Spine J. 2011;20(Suppl 5):578–585. doi: 10.1007/s00586-011-1924-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Takemitsu Y, Harada Y, Iwahara T, Miyamoto M, Miyatake Y. Lumbar degenerative kyphosis. Clinical, radiological and epidemiological studies. Spine (Phila Pa 1976) 1988;13:1317–1326. [PubMed] [Google Scholar]
- 19.Yagi M, King AB, Boachie-Adjei O. Incidence, risk factors, and natural course of proximal junctional kyphosis: surgical outcomes review of adult idiopathic scoliosis. Minimum 5 years of follow-up. Spine (Phila Pa 1976) 2012;37:1479–1489. doi: 10.1097/BRS.0b013e31824e4888. [DOI] [PubMed] [Google Scholar]


