Abstract
The number of revision total knee arthroplasty procedures performed annually is increasing and, subsequently, so is the number of patients presenting following a failed revision. Rerevising a total knee arthroplasty after one or more failed revision procedures presents many challenges, including diminished bone stock for prosthetic fixation. “Off the shelf” implants may not offer the best alternative for reconstruction. We present the case of a 55-year-old patient who required a rerevision total knee arthroplasty following multiple failed revisions with severe femoral and tibia bone loss. We describe a novel technique we employed to improve component fixation within the compromised bone stock.
Keywords: Revision TKA, Novel technique, Custom trabecular metal cone, Trabecular metal cone, Interlocking revision stem
Introduction
As the population ages and the use of total knee arthroplasty (TKA) in younger patients expands, we can expect the number of revision TKAs to increase [1]. Unfortunately, revision procedures have a higher rate of failure, and many of these patients present unique challenges for reconstruction of the failed knee arthroplasty, mainly due to compromised bone stock [1], [2]. Options to manage compromised bone stock in these cases include bulk allografts, impaction grafting, metallic augmentation, and porous metal cones/sleeves; however, there are situations in which these described techniques do not provide the best alternative for component fixation.
We report the case of a 55-year-old patient who required a rerevision TKA with severely compromised left distal femoral and proximal tibial bone stock following four prior arthroplasty procedures and who suffered a diaphyseal periprosthetic tibia fracture while awaiting revision. To address both issues; we developed a custom tantalum cone for the femur reconstruction and used a custom tibial stem with distal interlocking locking screws and a standard trabecular metal cone for management of proximal tibia bone deficiency and the unexpected periprosthetic fracture.
Case history
A 55-year-old female with a history of left primary TKA (1986) and 3 revision TKAs for arthrofibrosis and periprosthetic infection (1993, 2007, and 2011) presented to our facility for consultation with progressive activity-related left knee and thigh pain. The patient rated her pain as a 10/10 and stated that it severely interfered with her activities of daily living.
On physical examination, her knee showed a midline scar consistent with previous surgeries. The range of motion was restricted and painful from 0˚ to 90˚. Her hip and ankle examination was unremarkable.
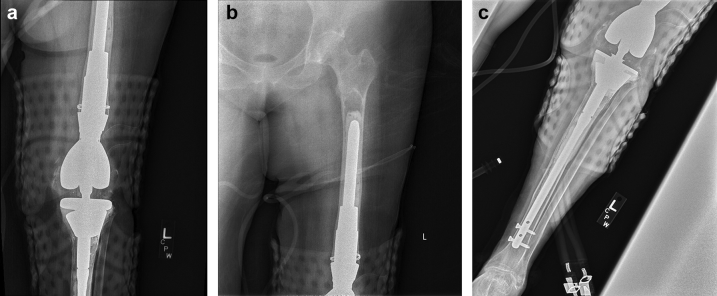
Plain film radiographs taken at her initial visit (Fig. 1) revealed a hinged distal femoral replacement with long cemented tibial and femoral stems. There was evidence of continuous radiolucencies in the cement-bone interface in the femur and tibia consistent with loosening, as well as Anderson Orthopaedic Research Institute type III femoral and tibial bone loss. There was posterolateal migration of the long tibial stem tip with impending fracture.
Figure 1.
(a) Preoperative anteroposterior femur radiograph. (b) Preoperative anteroposterior tibia radiograph. (c) Preoperative lateral femur radiograph. (d) Preoperative lateral tibia radiograph.
Serology was within normal limits, including a C-reactive protein (1.7 mg/L; range 0.0-4.9 mg/L) and erythrocyte sedimentation rate (8 mm/h; range 0-40 mm/h). An arthrocentesis showed a white blood cell count of less than 2000/mL and no microorganism growth for 14 days.
Due to the amount of bone loss and failure of the prior cemented revisions, surgical options were limited on the femoral side. Options considered included total femoral arthroplasty and femoral impaction grafting. Total femoral arthroplasty has been proven successful in patients who have failed previous total knee revisions and have insufficient bone stock for prosthesis implantation [3]. However, total femoral replacement can lead to suboptimal functional outcomes, diminished implant survivorship, and increased morbidity [3], [4]. Although impaction grafting has been proven successful in restoring adequate bone stock before revision TKA [5], [6], it is technically demanding with reported high implant failure rate [5], [7]. In addition, we have minimal experience with this highly technical procedure.
Therefore, we entertained the creation of a custom tantalum cone as an alternative that would provide an adequate cementation surface in the already compromised patulous femur. The concept was to obtain bone ingrowth between the femur and cone and cement a femoral stem supporting a distal femoral replacement into the porous metal. This concept has been successful with readily available implants in revision TKAs [2], [8].
In coordination with industry engineers, a surgical plan was developed following a lower extremity computed tomography (CT) scan. The custom tantalum cone was designed using the parameters measured on the CT scan. The outer diameter (38 mm) of the trabecular metal cone was designed to obtain scratch fit into the femoral canal and the inner diameter (22.5 mm) to allow for a predetermined 15-mm diameter stem passage and fixation with an appropriate cement mantle. The length of the trabecular metal cone provided over 7.5 cm of scratch fit for potential bone ingrowth and improved surface area for cementation of a 15 mm × 190 mm stem. Furthermore, the cone was designed with a geometry to facilitate bone preparation and implantation with a standard size B ZMR (Zimmer) proximal body reamer.
During the design process, the patient sustained a fall for which she requested further evaluation due to increased pain. Plain film radiographs (Fig. 2) revealed an acute Felix and Associates type IIB [9] periprosthetic diaphyseal tibia fracture with posterior cortical penetration of the tibial stem. The surgical plan and radiology workup were adjusted to include a CT-based design of a custom tibial stem that would bypass the tibial fracture and allow for distal interlocking screws. The designed stem would distribute load away from the deficient proximal bone and facilitate fracture healing by stabilizing the bone to axial, rotational, and torsional forces. In concordance with engineers, a 12 mm × 200 mm tibial stem was designed to have an appropriate length to bypass the fracture as well as proper diameter and distal interlocking screw options for fracture stabilization.
Figure 2.
(a) Preoperative (post fall) anteroposterior tibia radiograph. (b) Preoperative (post fall) lateral tibia radiograph.
The patient underwent revision TKA according to preoperative plan (Figure 3, Figure 4, Figure 5). An “off the shelf” tantalum cone was utilized in the proximal tibia to manage the deficient bone. Excellent stability of each component was achieved following impaction. Intraoperative fluoroscopy and postoperative radiographs confirmed adequate cement mantle and alignment (Fig. 6).
Figure 3.

Photograph of custom tantalum cone.
Figure 4.
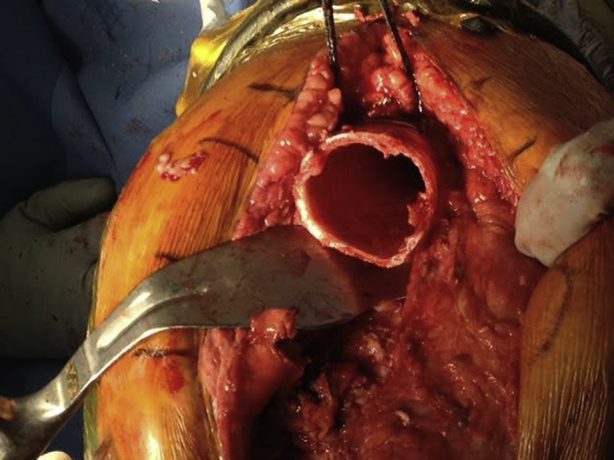
Intraoperative photograph of distal femur after removal of prior implant.
Figure 5.

Custom tantalum cone inserted.
Figure 6.
(a) Postoperative anteroposterior knee radiograph. (b) Postoperative anteroposterior femur radiograph. (c) Postoperative anteroposterior tibia radiograph.
Postoperatively, the patient was made toe-touch weight bearing for 6 weeks, mainly to protect the tibia fracture. The patient successfully completed physical therapy and was subsequently able to return to her activities of daily living. At her 2-year follow-up, the patient was reporting no pain, and her physical examination revealed a painless range of motion of her left knee from 0˚ to 100˚. Images taken at this follow-up demonstrated well-aligned and well-fixed components with tibial fracture union and no signs of loosening (Fig. 7).
Figure 7.

Two-year postoperative anteroposterior knee radiograph.
Discussion
Rerevision TKAs are complex procedures, fraught with obstacles including compromised femoral and tibial bone stock. Common techniques to address these patients include impaction grafting, bulk allograft, metal augments, and more recently, porous metal cones. In our patient's case, her previous failed cemented revisions and significant bone loss, compounded by a tibial shaft fracture, required a unique approach.
A custom trabecular metal cone was designed to address the femoral bone deficiency and provide support for a femoral component to be cemented. Metaphyseal cones have previously been employed in revision TKAs to achieve good initial fixation, improve rotational stability, and bear a portion of the axial load [10]. Radiographic studies also confirm that cones can achieve osteointegration in both the short term and midterm [10], [11], [12]. These cones can provide an adequate surface for cement interdigitation while obtaining osseous integration with potential long-term survivorship. In our case, standard “off the shelf” cones would have not provided a reliable option to manage the femoral side, hence, the development of the custom implant. The case was further complicated by the periprosthetic diaphyseal tibia fracture which required a tibial stem with interlocking distal screws for rotational stability.
Chalkin and Minter [13] reported a case in which a custom trabecular metal sleeve was used during salvage total hip arthroplasty for a patient with segmental bone loss [13]. An added challenge to their case was the need for soft-tissue reattachment via ingrowth into this implant [13]. Satisfactory clinical results were recorded at the 2-year follow-up, and adequate osteointegration was noted on postoperative radiographic evaluations [13]. The 2-year follow-up radiograph did show unexpected distal femur bone resorption surrounding the tantalum implant (Fig. 7). Despite tantalum being isoelastic with bone which would minimize stress shielding; the size of the implant, rigidity of the cement construct along with the previously compromised cortices could have contributed to this phenomenon and continues to be monitored.
Summary
Rerevision TKAs present unique challenges including severely compromised bone stock and fractures. Although most can be handled with readily available implants, some unique cases can benefit from custom implants that can simplify surgery and potentially improve survivorship. This particular case highlights the importance and value of proper surgical planning.
Footnotes
One or more of the authors of this paper have disclosed potential or pertinent conflicts of interest, which may include receipt of payment, either direct or indirect, institutional support, or association with an entity in the biomedical field which may be perceived to have potential conflict of interest with this work. For full disclosure statements refer to http://dx.doi.org/10.1016/j.artd.2016.08.003.
Appendix A. Supplementary data
References
- 1.Leta T., Lygre S., Skredderstuen A., Hallan G., Furnes O. Failure of aseptic revision total knee arthroplasties. Acta Orthop. 2015:48. doi: 10.3109/17453674.2014.964097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ponzio D., Austin M. Metaphyseal bone loss in revision knee arthroplasty. Curr Rev Musculoskelet Med. 2015;8(4):361. doi: 10.1007/s12178-015-9291-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Steinbrink K., Engelbrecht E., Fenelon G. The total femoral prosthesis. J Bone Joint Surg Br. 1982;64(3):305. doi: 10.1302/0301-620X.64B3.7096396. [DOI] [PubMed] [Google Scholar]
- 4.Nakamura S., Kusuzaki K., Murata H. More than 10 years of follow-up of two patients after total femur replacement for malignant bone tumor. Int Orthop. 2000;24:176. doi: 10.1007/s002640000145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rudert M., Holzapfel B., Rottkay E., Holzapfel D., Noeth U. Impaction bone grafting for the reconstruction of large bone defects in revision knee arthroplasty. Oper Orthop Traumatol. 2015;27(1):35. doi: 10.1007/s00064-014-0330-3. [DOI] [PubMed] [Google Scholar]
- 6.Naim S., Toms A. Impaction bone grafting for tibial defects in knee replacement surgery. Results at two years. Acta Orthop Belg. 2013;79(2):205. [PubMed] [Google Scholar]
- 7.Hilgen V., Citak M., Vettorazzi E. 10-year results following impaction bone grafting of major bone defects in 29 rotational and hinged knee revision arthroplasties. Acta Orthop. 2013;84(4):387. doi: 10.3109/17453674.2013.814012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tischler E., Hansen E., Austin M. A custom trabecular metal implant in revision total hip replacement with a paprosky type-iv femoral defect: a case report. JBJS Case Connector. 2014;4(4):e103. doi: 10.2106/JBJS.CC.N.00018. [DOI] [PubMed] [Google Scholar]
- 9.Felix N.A., Stuart M.J., Hanssen A.D. Periprosthetic fractures of the tibia associated with total knee arthroplasty. Clin Orthop Relat Res. 1997;(345):113. [PubMed] [Google Scholar]
- 10.Haidukewych G., Hanssen A., Jones R. Metaphyseal fixation in revision total knee arthroplasty: indications and techniques. J Am Acad Orthop Surg. 2011;19(6):311. doi: 10.5435/00124635-201106000-00001. [DOI] [PubMed] [Google Scholar]
- 11.Jones R., Skedros J., Chan A., Beauchamp D., Harkins P. Total knee arthroplasty using the S-ROM mobile-bearing hinge prosthesis. J Arthroplasty. 2001;16(3):279. doi: 10.1054/arth.2001.21498. [DOI] [PubMed] [Google Scholar]
- 12.Jones R., Barrack R., Skedros J. Modular, mobile-bearing hinge total knee arthroplasty. Clin Orthop Relat Res. 2001;(392):306. doi: 10.1097/00003086-200111000-00040. [DOI] [PubMed] [Google Scholar]
- 13.Chalkin B., Minter J. Limb salvage and abductor reattachment using a custom prosthesis with porous tantalum components. J Arthroplasty. 2005;20(1):127. doi: 10.1016/j.arth.2004.09.029. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.