ABSTRACT
Based upon knowledge of the hydrolytic profile of major β-lactamases found in Gram-negative bacteria, we tested the efficacy of the combination of ceftazidime-avibactam (CAZ-AVI) with aztreonam (ATM) against carbapenem-resistant enteric bacteria possessing metallo-β-lactamases (MBLs). Disk diffusion and agar-based antimicrobial susceptibility testing were initially performed to determine the in vitro efficacy of a unique combination of CAZ-AVI and ATM against 21 representative Enterobacteriaceae isolates with a complex molecular background that included blaIMP, blaNDM, blaOXA-48, blaCTX-M, blaAmpC, and combinations thereof. Time-kill assays were conducted, and the in vivo efficacy of this combination was assessed in a murine neutropenic thigh infection model. By disk diffusion assay, all 21 isolates were resistant to CAZ-AVI alone, and 19/21 were resistant to ATM. The in vitro activity of CAZ-AVI in combination with ATM against diverse Enterobacteriaceae possessing MBLs was demonstrated in 17/21 isolates, where the zone of inhibition was ≥21 mm. All isolates demonstrated a reduction in CAZ-AVI agar dilution MICs with the addition of ATM. At 2 h, time-kill assays demonstrated a ≥4-log10-CFU decrease for all groups that had CAZ-AVI with ATM (8 μg/ml) added, compared to the group treated with CAZ-AVI alone. In the murine neutropenic thigh infection model, an almost 4-log10-CFU reduction was noted at 24 h for CAZ-AVI (32 mg/kg every 8 h [q8h]) plus ATM (32 mg/kg q8h) versus CAZ-AVI (32 mg/kg q8h) alone. The data presented herein require us to carefully consider this new therapeutic combination to treat infections caused by MBL-producing Enterobacteriaceae.
KEYWORDS: ceftazidime, avibactam, aztreonam, disk diffusion, metallo-β-lactamases
INTRODUCTION
As a consequence of the threat of rising antibiotic resistance, the Infectious Diseases Society of America has challenged the pharmaceutical industry to develop novel antibiotics (the “10 × 20 Initiative”; http://www.idsociety.org/10x20/). Of particular importance are carbapenem-resistant strains of bacteria, which are typically resistant to most or all commonly used therapeutic options and cause high morbidity and mortality (1). In response, the “antibiotic pipeline” has delivered an important β-lactam–β-lactamase inhibitor combination, ceftazidime-avibactam (CAZ-AVI) (2).
Avibactam (AVI) is a novel diazabicyclooctane (DBO) β-lactamase inhibitor with in vitro activity against serine enzymes, such as the class A extended-spectrum β-lactamases (ESBLs) and Klebsiella pneumoniae carbapenemases (KPCs), as well as the class D OXA-48 found in Enterobacteriaceae and the class C cephalosporinases present in enteric bacteria and Pseudomonas aeruginosa. AVI restores the activity of CAZ against a broad array of resistance threats, making CAZ-AVI a welcome addition to the antibiotic armamentarium against Gram-negative bacteria. However, CAZ-AVI is not active against strains bearing class B metallo-β-lactamases (MBLs) such as NDM, VIM, and IMP. The monobactam antibiotic aztreonam (ATM) remains stable against MBLs but is not a therapeutic option in many cases because it is inactivated by ESBLs, KPCs, and other cephalosporinases frequently found in the background of MBL-producing bacteria (2, 3).
Even before widespread clinical use of CAZ-AVI, case reports appeared that described resistance to this novel inhibitor combination (4). As a result of these findings, we now know that CAZ-AVI MICs may be elevated in the setting of unfavorable genetic backgrounds that include resistance determinants that control entry and egress of antibiotics (5). Recent reports have also described clinical isolates bearing KPC-3 that are resistant to the combination CAZ-AVI as a result of amino acid substitutions in the Ω loop. Additionally, MBLs are a worldwide problem, with outbreaks reported in the United States in numbers that were previously unanticipated (6, 7).
Knowing that ATM is stable against hydrolysis by MBLs, we hypothesized that addition of ATM to the CAZ-AVI combination would result in enhanced activity by “protecting” ATM from the “attack” of ESBLs and other cephalosporinases. Therefore (i) we tested the in vitro activity of the combination of CAZ-AVI plus ATM against 21 carbapenem-resistant, MBL-producing Enterobacteriaceae isolates containing blaNDM or blaIMP genes and a pan-susceptible control, (ii) we evaluated the in vivo antibacterial efficacy of CAZ-AVI with ATM in a mouse thigh infection model using an MBL-producing K. pneumoniae strain, and finally (iii) we report a case of infection caused by an Enterobacter cloacae strain containing an MBL treated with ATM in combination with CAZ-AVI. Our findings encourage further study of CAZ-AVI with ATM under experimental and clinical circumstances when therapeutic options against MBL-producing strains are limited.
RESULTS AND DISCUSSION
As established by current and previous molecular testing (8), each of the isolates possessed an MBL, with the exception of Escherichia coli DH10B, which served as a negative control. In Table 1, we show that isolates containing an MBL were resistant to CAZ (21/21 isolates), ATM (19/21 isolates), and CAZ-AVI (21/21 isolates) by disk diffusion (9). The combination of CAZ-AVI and ATM produced an inhibition zone of ≥21 mm, suggesting susceptibility in 17 of the 21 MBL-producing strains that were tested (i.e., ≥21 mm is the susceptibility (S) zone diameter for CAZ-AVI alone), with the measured zones being larger than with CAZ-AVI or ATM alone: 10 to 15 mm larger for 9 isolates and 4 to 9 mm larger for 5 isolates (Table 1). In 3 cases where an increase in the inhibition zone was not found with the combination of CAZ-AVI and ATM, there was already a significant zone of susceptibility to ATM observed.
TABLE 1.
Evaluation of in vitro activities of CAZ-AVI plus ATM, by both disk diffusion and agar MIC testinga
| Isolate | Known bla gene(s) | Disk diffusion assay inhibition zone diam (mm) |
MIC (μg/ml) by agar MIC test |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 30 μg CAZ (CLSI S ≥ 21, I = 18–20, R ≤ 17 mm) | 30 μg ATM (CLSI S ≥ 21, I = 18–20, R ≤ 17 mm) | 30 μg CAZ–20 μg AVI (FDA S ≥ 21, R ≤20 mm) | CAZ-AVI with ATMb | CAZ (CLSI S ≤ 4, I = 8, R ≥ 16 μg/ml) | ATM (CLSI S ≤ 4, I = 8, R ≥ 16 μg/ml) | CAZ with ATM at 16 μg/ml | CAZ-AVI (FDA S ≤ 8/4, R ≥ 16/4 μg/ml) | CAZ-AVI with ATM at constant concn of: |
|||||
| 8 μg/ml | 16 μg/ml | 32 μg/ml | 64 μg/ml | ||||||||||
| E. coli DH10B | None | 33 | 35 | 35 | 40 (5) | 0.125 | 0.25 | <0.0625 | 0.25 | <0.0625 | <0.0625 | ||
| E. cloacae 6.31 | NDM-1, CTX-M-15, ACT/MIR, OXA-48 | 6 | 6 | 14 | 26 (12) | >512 | >>512 | >512 | 64 | 0.5 | 0.5 | ||
| E. cloacae 6.43 | NDM-1, CTX-M-15, ACT/MIR | 6 | 6 | 17 | 25 (8) | >512 | >512 | >512 | 128 | 0.5 | 0.25 | ||
| E. cloacae joint infection | NDM-1, CTX-M, TEM-1, AmpCc | 6 | 6 | 18 | 28 (10) | >512 | 256 | >512 | 128 | 0.5 | 0.25 | ||
| E. coli 8.68 | NDM-1, CTX-M-15, CMY-2, TEM | 6 | 6 | 19 | 21 (2) | >512 | >512 | >512 | 64 | 16 | 16 | 8 | 1 |
| E. coli 8.69 | NDM-1, CTX-M-15, CMY-2, SHV-5 | 6 | 6 | 17 | 24 (7) | >512 | >512 | >512 | 64 | 8 | 4 | ||
| E. coli 8.70 | NDM-1, CTX-M-15, CMY-2, TEM, SHV-5 | 6 | 6 | 20 | 22 (2) | >512 | 512 | >512 | 64 | 16 | 4 | 0.5 | 0.25 |
| E. coli 8.71 | NDM-1, CTX-M-15, CMY-2, TEM | 6 | 6 | 17 | 20 (3) | >512 | >512 | >512 | 64 | 32 | 8 | 1 | 0.25 |
| E. coli 8.72 | NDM-1, CTX-M-15, CMY-2, TEM | 6 | 6 | 18 | 23 (5) | >512 | >512 | >512 | 64 | 8 | 2 | ||
| E. coli 8.73 | NDM-1, CTX-M-15, CMY-2, TEM | 6 | 6 | 17 | 20 (3) | >512 | >512 | >512 | 32 | 8 | 2 | ||
| E. coli 8.74 | NDM-1, TEM | 6 | 6 | 20 | 27 (7) | >512 | 2 | <0.0625 | 64 | 0.0625 | <0.0625 | ||
| E. coli 6728 | NDM-1 | 6 | 15 | 18 | 18 (0) | >512 | 32 | >512 | 64 | 16 | 4 | 0.125 | 0.06 |
| K. pneumoniae 1.41 | NDM-1, CTX-M-15, DHA, SHV, TEM | 6 | 6 | 17 | 32 (15) | >512 | 128 | >512 | 64 | 1 | 0.5 | ||
| K. pneumoniae 1.42 | NDM-1, CTX-M-15, SHV-12 | 6 | 6 | 17 | 27 (10) | >512 | >512 | >512 | 64 | 1 | 0.5 | ||
| K. pneumoniae 1.44 | NDM-1, CTX-M-15, CMY-2, DHA, SHV, TEM | 6 | 6 | 15 | 25 (10) | >512 | >512 | >512 | 128 | 16 | 8 | 8 | 4 |
| K. pneumoniae 1.50 | NDM-1, CTX-M-15, SHV | 6 | 6 | 20 | 30 (10) | >512 | >512 | >512 | 128 | 0.25 | 0.25 | ||
| K. pneumoniae 1.63 | NDM-1, CTX-M-15, CMY-2, SHV, TEM | 6 | 6 | 15 | 30 (15) | >512 | 512 | >512 | 256 | 1 | 0.125 | ||
| K. pneumoniae 6913 | IMP, SHV | 6 | 28 | 17 | 28 (0) | 256 | 0.5 | 0.0625 | 128 | <0.0625 | <0.0625 | ||
| K. pneumoniae 11-01-13 | NDM-1, CTX-M-15, SHV | 6 | 6 | 17 | 30 (13) | >512 | 512 | >512 | 128 | 1 | 0.5 | ||
| Providencia rettgeri 6384 | NDM-1, SHV | 6 | 37 | 6 | 34 (−3) | 512 | 0.0625 | <0.0625 | 256 | <0.0625 | <0.0625 | ||
| P. rettgeri 1.27 | NDM-1, CMY-2, DHA | 6 | 14 | 10 | 20 (6) | >512 | 64 | >512 | >512 | 32 | 16 | ||
| Morganella morganii 1.39 | NDM-1, CTX-M-15, DHA | 6 | 12 | 10 | 25 (13) | >512 | 256 | >512 | 512 | 0.125 | <0.0625 | ||
Shown are the genetic background of isolates and inhibition zone diameters of disks with CAZ, ATM, or CAZ-AVI and CAZ-AVI disks to which ATM was added. Isolates in this table were available from the laboratories of the authors and characterized previously (8). Interpretative criteria for CAZ and ATM MICs were according to the Clinical and Laboratory Standards Institute (CLSI) guidelines (9). For CAZ-AVI, MICs were interpreted according to FDA guidelines from the package insert. For CAZ, suceptible (S), intermediate (I), and resistant (R) are ≤4, 8, and ≥16 μg/ml, respectively. For ATM, S, I, and R are ≤4, 8, and ≥16 μg/ml, respectively. For CAZ-AVI, S and R are ≤8/4 and ≥16/4 μg/ml, respectively. The values reported for CAZ-AVI reflect the concentration of the CAZ in the 4:1 ratio formulation.
The data presented represent the zone diameter of the CAZ-AVI disk to which ATM was added. In parentheses is the difference between this zone size and the zone of inhibition of either CAZ-AVI or ATM alone—whichever of the two was greater.
Presumed AmpC.
For the agar dilution MIC determinations, we used a series of doubling dilutions of CAZ-AVI in the ratio that is found in the commercial preparation (Avycaz) intended for patient use. This was a deliberate decision as we feel these dilutions reflect doses of CAZ-AVI that patients receive. The commercial preparation is formulated in a 4:1 ratio (CAZ at 2 g and AVI at 0.5 g/per vial). The values reported for CAZ-AVI in Table 1 reflect the concentration of the CAZ in the 4:1 ratio formulation. For MIC determinations, where the efficacy of ATM addition was assessed, ATM was kept at a fixed concentration of 8, 16, 32, or 64 μg/ml and CAZ-AVI was added in doubling dilutions. These concentrations of ATM were chosen as they represent the expected serum concentrations of the monobactam when delivered in 1- and 2-g doses throughout the dosing interval, particularly the 8- and 16-μg/ml doses. Single 30-min intravenous infusions of 1- and 2-g doses of ATM produce peak serum levels immediately after administration of 54 and 90 μg/ml and 3 and 6 μg/ml at 8 h (the end of the dosing interval), respectively (Azactam package insert).
All 21 isolates were resistant to CAZ and CAZ-AVI alone by agar dilution MIC and disk diffusion assay, and all demonstrated a reduction in CAZ-AVI MICs with the addition of ATM (Table 1 and Fig. 1) in a dose-dependent fashion. Notably, one K. pneumoniae isolate and four E. coli isolates demonstrated MIC values that remained at or above the resistance breakpoint for CAZ-AVI alone (≥16/4 μg/ml) after the addition of ATM. However, addition of ATM at higher concentrations of 32 and 64 μg/ml for all 5 isolates brought them into the susceptible MIC range for CAZ-AVI alone (susceptibility, ≤8/4 μg/ml) (Table 1). Remarkably, the results presented herein accurately reflect the genetic backgrounds established in these isolates, and as anticipated, the combination of CAZ-AVI with ATM worked especially well in NDM-producing strains.
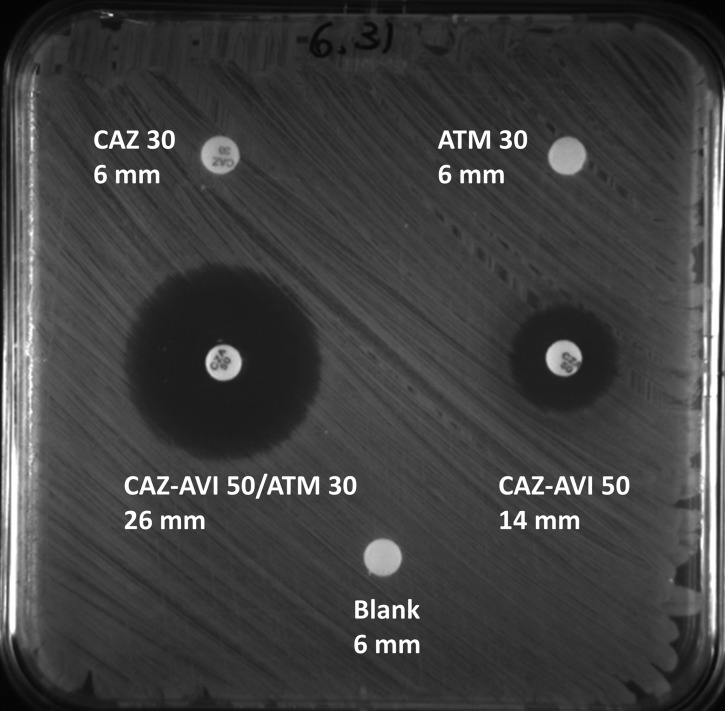
FIG 1.
ATM placed directly on the CAZ-AVI disk to evaluate synergy. E. cloacae isolate 6.31 was used in this assay.
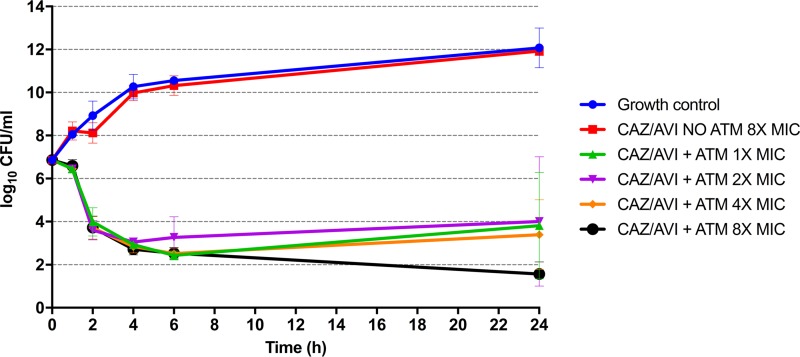
The time-kill curves detail the bactericidal activity of the combination of CAZ-AVI and ATM against the MBL-containing K. pneumoniae 1.41 isolate. ATM at a fixed concentration of 8 μg/ml was added to various sublethal concentrations of CAZ-AVI ranging from 8 μg/ml CAZ plus 2 μg/ml AVI down to 1 μg/ml CAZ plus 0.25 μg/ml AVI; corresponding to 4 different MIC multiples of the CAZ-AVI plus ATM agar MIC of 1 μg/ml. Time-kill kinetics showed a time-dependent decrease in CFU/ml from 1 to 24 h (Fig. 2). A ≥4-log10-CFU decrease was observed by 2 h for all combination concentrations, and by 6 h, approximately 5-log10 reductions were observed, compared to the growth control, to which antibiotics were not added. After 24 h, there was minimal regrowth observed for all combinations, still keeping a 3-log10 decrease compared to time zero, with the exception of the 8× the MIC, which showed approximately a 6-log10 decrease.
FIG 2.
Time-kill curve for K. pneumoniae isolate 1.41. ATM concentrations were held constant at 8 μg/ml for all combinations, with two exceptions: (i) the growth control (no antibiotics added) and (ii) CAZ-AVI with no ATM at 8× the MIC. Various ceftazidime-avibactam (CAZ-AVI) concentrations were added corresponding to 1× (1 μg/ml CAZ plus 0.25 μg/ml AVI), 2× (2 μg/ml CAZ plus 0.5 μg/ml AVI), 4× (4 μg/ml CAZ plus 1 μg/ml AVI), and 8× (8 μg/ml CAZ plus 2 μg/ml AVI) the MIC of the combination CAZ-AVI plus ATM obtained by agar dilution (1 μg/ml). Three replicates were conducted for each of the conditions reported in the time-kill assay.
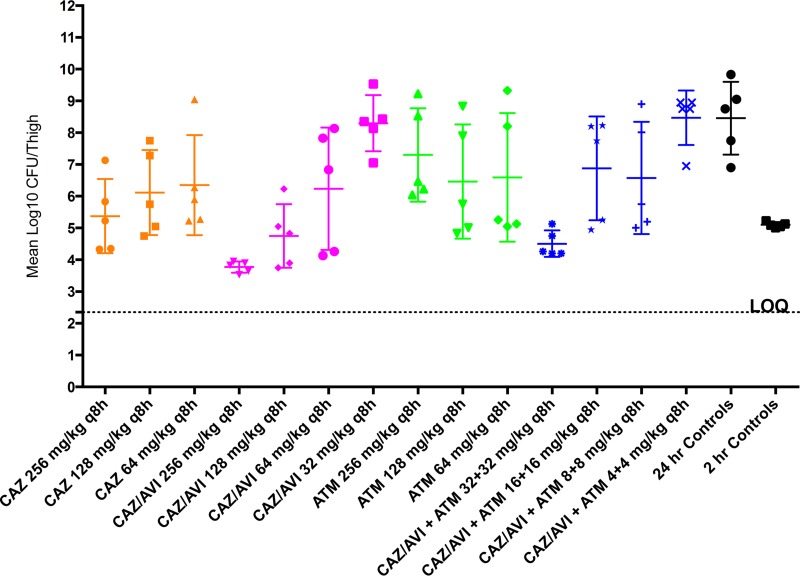
We next evaluated the in vivo antibacterial efficacy of CAZ-AVI in combination with ATM in a mouse thigh infection model using the MBL-producing K. pneumoniae 1.41 isolate. The results are presented in Table 2 and Fig. 3. Both CAZ alone (256 mg/kg) and CAZ-AVI alone (256/64 and 128/32 mg/kg) resulted in 3.1-, 4.7-, and 3.7-log-CFU reductions, respectively, compared to the untreated control group at 24 h. The lower dose of either CAZ or CAZ-AVI was less effective. ATM alone at doses from 64 to 256 mg/kg every 8 h (q8h) exhibited minimal efficacy (a 1.16- to 1.99-log-CFU reduction).
TABLE 2.
Log10 CFU per thigh counts for various antibiotic–β-lactamase inhibitor combinations in the neutropenic thigh infection model for K. pneumoniae 1.41-infected micea
| Treatment | Dose (mg/kg s.c. q8h, 5 mice/treatment) | Mean log10 CFU/thigh ± SD | Change from control at 24 h with no antibiotics (log10 CFU) | Tukey adjusted P value (treatment vs 24-h control) |
|---|---|---|---|---|
| 24-h infection control | NA | 8.46 ± 1.15 | NA | NA |
| CAZ | 256 | 5.37 ± 1.17 | −3.08 | 0.0405 |
| 128 | 6.12 ± 1.34 | −2.34 | 0.3152 | |
| 64 | 6.35 ± 1.57 | −2.11 | 0.4909 | |
| ATM | 256 | 7.30 ± 1.47 | −1.16 | 0.9912 |
| 128 | 6.46 ± 1.80 | −1.99 | 0.5873 | |
| 64 | 6.59 ± 2.02 | −1.86 | 0.6936 | |
| CAZ-AVI | 256/64 | 3.77 ± 0.18 | −4.68 | <0.0001 |
| 128/32 | 4.75 ± 1.00 | −3.70 | 0.0042 | |
| 64/16 | 6.23 ± 1.93 | −2.22 | 0.4018 | |
| 32/8 | 8.30 ± 0.88 | −0.16 | >0.9999 | |
| CAZ-AVI-ATM | 32/8/32 | 4.51 ± 0.42 | −3.95 | 0.0016 |
| 16/4/16 | 6.88 ± 1.63 | −1.58 | 0.8818 | |
| 8/2/8 | 6.57 ± 1.77 | −1.88 | 0.6777 | |
| 4/1/4 | 8.47 ± 0.85 | 0.02 | >0.9999 |
Infection was 5 log10 CFU/mouse with 5 mice per treatment group. Boldface indicates a statistically significant value. NA, not applicable.
FIG 3.
Individual and mean counts of log10 CFU per thigh for various antibiotic–β-lactamase inhibitor combinations in the neutropenic thigh infection model for K. pneumoniae 1.41-infected mice, with 5 log10 CFU/mouse and 5 mice per treatment group. LOQ, limit of quantitation (2.35 log10 CFU/thigh).
Our data in Table 2 show that in this model, the addition of ATM to the CAZ-AVI treatment regimen results in significant enhancement in the reduction of infection as measured by titer in CFU per thigh compared to either agent alone and the untreated controls. Doses of 32/8 mg/kg q8h CAZ-AVI (4:1 ratio) plus 32 mg/kg q8h ATM reduced bacterial thigh titers by 3.95 log CFU below that in the 24-h no-antibiotic controls (P = 0.0016), 3.79 log CFU below those of 32/8 mg/kg q8h CAZ-AVI alone (P = 0.003; data not shown), and 2.08 log CFU below 64 mg/kg ATM alone. Dosages of ≤4/1 mg/kg q8h CAZ-AVI (4:1 ratio) plus 4 mg/kg q8h ATM were unable to reduce the CFU count.
Clinical commentary.
A 72-year-old woman without significant medical history fell and sustained a fractured hip on an excursion. She was treated with a total hip arthroplasty performed in Eastern Europe and returned home within 2 weeks with a painful, red surgical site. The arthroplasty was removed in the United States, and all intraoperative cultures grew carbapenem-resistant Enterobacter cloacae susceptible to colistin, intermediate to tigecycline (FDA breakpoint), and resistant to all other agents tested, including fosfomycin. PCR and sequencing efforts revealed that the Enterobacter cloacae isolate possessed blaNDM-1 (Table 1). The culture also contained an ESBL-producing Klebsiella pneumoniae isolate and Enterococcus faecalis isolate (ampicillin and vancomycin susceptible). A hip spacer was not placed at this time, knowing further debridement would be necessary.
By day 4 of colistimethate sodium (colistin), tigecycline, and meropenem treatment, serum creatinine increased from 0.9 to 2.4 mg/dl. Colistimethate sodium was reduced to 1.5 mg/kg every 36 h, and meropenem was adjusted for declining renal function. The patient underwent repeat washout, with cultures again yielding the carbapenem-resistant E. cloacae and ESBL-producing K. pneumoniae. CAZ-AVI at 1.25 g three times daily was added to the antibiotic regimen; however, CAZ-AVI was discontinued after 4 days as the carbapenem-resistant Enterobacter cloacae isolate demonstrated in vitro resistance by disk diffusion (ATM, 30-μg disk, 6-mm zone size; CAZ-AVI, 50-μg disk, 18-mm zone size). Meropenem was soon discontinued due to lack of evidence of efficacy. With normalization of serum creatinine, the colistimethate sodium dose was increased to 2 mg/kg every 12 h.
Qualitative synergy in the E. cloacae isolate was demonstrated in vitro between CAZ-AVI and ATM. (The inhibition zone of the CAZ-AVI disk was increased from 18 mm to 28 mm upon addition of ATM [Table 1]). Therefore, the treatment regimen was modified so that the final 3 weeks of her 6-week postoperative antibiotic course were comprised of colistimethate sodium, CAZ-AVI (2.5 g every 8 h), ATM (2 g every 8 h), and vancomycin. Six months after completion of antibiotics, the patient underwent successful final reimplantation of a total hip arthroplasty, with extensive inspection and washout. Six cultures were obtained from acetabular and femoral spaces. All were negative for the 3 organisms originally isolated.
Concluding remarks.
Based upon an understanding of the biochemical mechanisms of action of these three agents, we show that the combination of ATM and CAZ-AVI is able to help overcome carbapenem and expanded-spectrum cephalosporin resistance in MBL-producing strains of enteric bacteria. AVI is a very potent β-lactamase inhibitor of class A and C enzymes, and since most strains of Enterobacter spp. possess class C enzymes and possibly some class A ESBLs, we reasoned that AVI would prevent the hydrolysis of CAZ and ATM (10). Although AVI cannot restore susceptibility to MBL-producing strains, ATM is not susceptible to hydrolysis by MBLs. By inhibiting class A and C β-lactamases with AVI and using ATM to “bypass” the class B metallo-β-lactamase, susceptibility can be restored, leading to a successful microbiological and possible clinical outcome. Our clinical observation is supported by evidence from our in vitro investigations.
An unexpected benefit from using CAZ and ATM may arise by the simultaneous inhibition of multiple penicillin-binding proteins (PBPs). CAZ has a high affinity for the penicillin-binding protein 3 (PBP 3) and moderate affinity for the PBP 1a of certain Gram-negative organisms, such as E. coli and P. aeruginosa. Binding to PBPs results in spheroplast formation followed by rapid lysis. Furthermore, AVI and developmental DBO inhibitors can also bind to certain PBPs (11–13). ATM is relatively PBP 3 specific. The combination (CAZ-AVI and ATM) may completely affect the “divisome” of Gram-negative bacteria and have an independent impact on its own. Of note, the use of “double β-lactams” has some precedent in the literature. Overall, the existing data suggest that the potential benefit of this approach against Gram-negative pathogens should be explored carefully, especially given the recent availability of novel inhibitors and β-lactams (14).
There are important limitations that must be considered before uniform application of this promising combination: (i) further animal testing with additional isolates and pharmacokinetic (PK) studies along with trials in humans are required before full endorsement by clinicians, and (ii) results from Enterobacteriaceae should not be extrapolated to nonfermenters without appropriate testing (studies in progress). At present, clinical experience using this combination against Stenotrophomonas maltophilia proved to be successful in a single case (15). Finally, the possibility of cumulative toxicity from “double-β-lactam” combinations must be considered when administering this regimen. However, one major advantage of using ATM is its safety profile. ATM is safe to use in patients with penicillin allergies, can be administered by prolonged or continuous infusion, and is not associated with nephrotoxicity. The data presented here require us to carefully consider CAZ-AVI combined with ATM as a “new therapeutic opportunity” to treat infections caused by MBL-producing strains, while recognizing the ongoing need for new antibiotics.
MATERIALS AND METHODS
Antimicrobial susceptibility testing.
In vitro efficacy of the CAZ-AVI and ATM combination was performed on 21 previously characterized strains of diverse species of Enterobacteriaceae (8). Susceptibility testing was initially performed by disk diffusion. Disks containing CAZ (30 μg) and CAZ-AVI (30/20 μg) were obtained from Becton Dickinson (Sparks, MD) and Actavis (Schaumburg, IL), respectively. ATM (30-μg) disks were made by adding 10 μl of a 3,000-μg/ml stock of ATM (Chem-Impex International, Inc., Wood Dale, IL) solution to blank disks. To test the activity of the combination of CAZ-AVI with ATM, 30 μg of ATM was placed directly on the CAZ-AVI disk and allowed to dry for 30 min before use. Isolates were grown overnight in cation-adjusted Mueller-Hinton broth (CAMHB), diluted to a McFarland 0.5 standard, and inoculated to form a lawn on cation-adjusted Mueller-Hinton agar (MHA) plates. Disks containing CAZ, CAZ-AVI, and ATM were placed onto the plates and then incubated overnight at 37°C. For CAZ and ATM, zones of inhibition were interpreted according to the Clinical and Laboratory Standards Institute (CLSI) guidelines (9). For CAZ-AVI, zones of inhibition were interpreted according to FDA guidelines.
Agar dilution MICs for CAZ, ATM, CAZ-AVI, CAZ-ATM, and the CAZ-AVI-ATM combination were determined in triplicate and performed according to the CLSI protocol (9). Isolates were grown overnight in CAMHB and stamped on MHA plates containing doubling dilutions of CAZ (Sigma Chemical Co., St. Louis, MO), ATM (Chem-Impex, International, Inc., Wood Dale, IL) and CAZ-AVI (2/0.5 g per vial [Avycaz; Allergan]) using a Steers replicator that delivered 104 CFU/spot. The effect of adding a fixed concentration of 8 or 16 μg/ml of ATM to CAZ or to CAZ-AVI was also assessed. Plates were incubated for 18 to 20 h at 37°C, and the antibiotic concentration (µg/ml) at which bacterial growth was no longer observed defined the MIC. A minimum of 3 determinations was done for each susceptibility, with the most frequently observed result reported.
Time-kill assays.
Time-kill assays were performed for K. pneumoniae isolate 1.41 as previously described, with some modifications (16). Briefly, freshly prepared colonies were resuspended in 5 ml CAMHB and incubated overnight in a shaking incubator (37°C, 220 rpm). Cultures were then diluted 1:100 and incubated in a shaking incubator until they reached a 0.5 McFarland standard (approximately 108 CFU/ml). A bacterial suspension was prepared in 50-ml conical tubes containing 10 ml CAMHB so that the starting inoculum was approximately 106 CFU/ml. CAZ-AVI (Avycaz) was added to the prepared bacterial suspensions so that the final concentration was 1×, 2×, 4×, or 8× the agar MIC of the CAZ-AVI-ATM combination (1 μg/ml CAZ–0.25 μg/ml AVI to 8 μg/ml CAZ–2 μg/ml AVI, with ATM held constant at 8 μg/ml). A control consisting of CAZ-AVI alone was diluted in the prepared bacterial suspension at 8× the MIC, and a growth control without antibiotics was also included. The starting inoculum was determined from the growth control tube immediately after dilution and was recorded as the count at time zero. After addition of antibiotics, the starting inoculum was 1 × 106 to 1 × 107 CFU/ml. Tubes were incubated in a shaking incubator (37°C, 180 rpm), and viability counts were performed at 1, 2, 4, 6, and 24 h by removing 200 μl of the culture, diluting as appropriate, and plating 100 μl on MHA. Plates were incubated at 37°C for 18 to 20 h, colonies were counted on plates yielding 30 to 300 colonies per plate, and the results were recorded as the number of CFU per milliliter. Three replicates were conducted for each of the conditions reported in the time-kill assay.
PCR and sequencing.
PCR amplification of blaNDM and other bla genes, in isolates not previously characterized, was achieved using established primers and amplified with a MJ Research gradient cycler model PTC 225 using thermocycling conditions adjusted to the primer melting temperatures (8). Positive controls included well-characterized isolates (in the laboratory of R.A.B.). Amplicons were sequenced at a commercial sequencing facility (MCLAB, San Francisco, CA). Sequence data were analyzed using Lasergene 7.2 software (DNAstar, Madison, WI), and sequences were compared with BLAST online software (http://blast.ncbi.nlm.nih.gov), using the megablast algorithm.
Mouse thigh infection model.
For the thigh infection model, female Hsd:ICR (CD-1) mice from Envigo were rendered neutropenic by intraperitoneal (i.p.) injection of cyclophosphamide (Cytoxan; Baxter Healthcare, Deerfield, IL) as previously described (17). Five mice per 2 control and 14 treatment groups were infected by injecting a prepared inoculum of K. pneumoniae 1.41 at an input CFU of 5.01 log10 CFU/mouse into the right hind thigh muscle contained in a volume of 0.1 ml per animal. At 2 h postinfection, animals were administered subcutaneous doses (q8h) of CAZ (ceftazidime hydrate [Sigma]), CAZ-AVI (AvyCaz), ATM (Azactam for injection [USP]) or CAZ-AVI plus ATM (1:1). All animals were euthanized 24 h postinfection, and thighs were aseptically removed into chilled PBS, homogenized (Kinematica Polytron PT2100 tissue homogenizer), 10-fold serially diluted, plated on brain heart infusion agar plates containing 0.5% activated charcoal, and incubated for the determination of bacterial thigh titers (CFU).
The animal studies were conducted under IACUC-approved protocol 2014/15-09-A04 (approved on 31 October 2014 and to expire on 30 October 2017).
Statistical analysis.
The 24-h log10 CFU counts were compared across all treatment and control groups using a one-way analysis of variance (ANOVA). Post hoc pairwise comparisons were performed across all treatment and control groups, and P values were adjusted according to Tukey's method. All analysis was performed using GraphPad Prism 6.0 software.
ACKNOWLEDGMENTS
We thank C. Lascols and the SMART study for sharing isolates with R.A.B.
This study was supported in part by funds and facilities provided by the Cleveland Department of Veterans Affairs, Veterans Affairs Merit Review Program award no. 1I01BX001974, from the Biomedical Laboratory Research & Development Service of the VA Office of Research and Development and the Geriatric Research Education and Clinical Center VISN 10 to R.A.B. This work was also supported by funds from the National Institute of Allergy and Infectious Diseases of the National Institutes of Health under award no. UM1AI104681, R01AI063517, R01AI072219, and R01AI100560 to R.A.B. The efficacy study in mice was supported by NIAID's Animal Models of Infectious Diseases program under contract HHSN272201500007C awarded to the University of North Texas. Funding organizations were not involved in the design and conduct of the study, collection, management, analysis, and interpretation of the data, and preparation, review, or approval of the manuscript.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the Department of Veterans Affairs.
REFERENCES
- 1.Centers for Disease Control and Prevention. 2013. Vital signs: carbapenem-resistant Enterobacteriaceae. MMWR Morb Mortal Wkly Rep 62:165–170. [PMC free article] [PubMed] [Google Scholar]
- 2.van Duin D, Bonomo RA. 2016. Ceftazidime/avibactam and ceftolozane/tazobactam: second-generation beta-lactam/beta-lactamase inhibitor combinations. Clin Infect Dis 63:234–241. doi: 10.1093/cid/ciw243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Falcone M, Paterson D. 2016. Spotlight on ceftazidime/avibactam: a new option for MDR Gram-negative infections. J Antimicrob Chemother 71:2713–2722. doi: 10.1093/jac/dkw239. [DOI] [PubMed] [Google Scholar]
- 4.Humphries RM, Yang S, Hemarajata P, Ward KW, Hindler JA, Miller SA, Gregson A. 2015. First report of ceftazidime-avibactam resistance in a KPC-3-expressing Klebsiella pneumoniae isolate. Antimicrob Agents Chemother 59:6605–6607. doi: 10.1128/AAC.01165-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pages JM, Peslier S, Keating TA, Lavigne JP, Nichols WW. 2015. The role of the outer membrane and porins in the susceptibility of beta-lactamase-producing Enterobacteriaceae to ceftazidime-avibactam. Antimicrob Agents Chemother 60:1349–1359. doi: 10.1128/AAC.01585-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Castanheira M, Mills JC, Costello SE, Jones RN, Sader HS. 2015. Ceftazidime-avibactam activity tested against Enterobacteriaceae isolates from U.S. hospitals (2011 to 2013) and characterization of beta-lactamase-producing strains. Antimicrob Agents Chemother 59:3509–3517. doi: 10.1128/AAC.00163-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Epstein L, Hunter JC, Arwady MA, Tsai V, Stein L, Gribogiannis M, Frias M, Guh AY, Laufer AS, Black S, Pacilli M, Moulton-Meissner H, Rasheed JK, Avillan JJ, Kitchel B, Limbago BM, MacCannell D, Lonsway D, Noble-Wang J, Conway J, Conover C, Vernon M, Kallen AJ. 2014. New Delhi metallo-beta-lactamase-producing carbapenem-resistant Escherichia coli associated with exposure to duodenoscopes. JAMA 312:1447–1455. doi: 10.1001/jama.2014.12720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lascols C, Hackel M, Marshall SH, Hujer AM, Bouchillon S, Badal R, Hoban D, Bonomo RA. 2011. Increasing prevalence and dissemination of NDM-1 metallo-beta-lactamase in India: data from the SMART study (2009). J Antimicrob Chemother 66:1992–1997. doi: 10.1093/jac/dkr240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.CLSI. 2015. Performance standards for antimicrobial susceptibility testing, 25th informational supplement. Clinical and Laboratory Standards Institute, Wayne, PA. [Google Scholar]
- 10.Drawz SM, Papp-Wallace KM, Bonomo RA. 2014. New beta-lactamase inhibitors: a therapeutic renaissance in an MDR world. Antimicrob Agents Chemother 58:1835–1846. doi: 10.1128/AAC.00826-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alm RA, Johnstone MR, Lahiri SD. 2015. Characterization of Escherichia coli NDM isolates with decreased susceptibility to aztreonam/avibactam: role of a novel insertion in PBP3. J Antimicrob Chemother 70:1420–1428. doi: 10.1093/jac/dku568. [DOI] [PubMed] [Google Scholar]
- 12.Asli A, Brouillette E, Krause KM, Nichols WW, Malouin F. 2016. Distinctive binding of avibactam to penicillin-binding proteins of Gram-negative and Gram-positive bacteria. Antimicrob Agents Chemother 60:752–756. doi: 10.1128/AAC.02102-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.King AM, King DT, French S, Brouillette E, Asli A, Alexander JA, Vuckovic M, Maiti SN, Parr TR Jr, Brown ED, Malouin F, Strynadka NC, Wright GD. 2016. Structural and kinetic characterization of diazabicyclooctanes as dual inhibitors of both serine-beta-lactamases and penicillin-binding proteins. ACS Chem Biol 11:864–868. doi: 10.1021/acschembio.5b00944. [DOI] [PubMed] [Google Scholar]
- 14.Rahme C, Butterfield JM, Nicasio AM, Lodise TP. 2014. Dual beta-lactam therapy for serious Gram-negative infections: is it time to revisit? Diagn Microbiol Infect Dis 80:239–259. doi: 10.1016/j.diagmicrobio.2014.07.007. [DOI] [PubMed] [Google Scholar]
- 15.Mojica MF, Ouellette CP, Leber A, Becknell MB, Ardura MI, Perez F, Shimamura M, Bonomo RA, Aitken SL, Shelburne SA. 2016. Successful treatment of bloodstream infection due to metallo-beta-lactamase-producing Stenotrophomonas maltophilia in a renal transplant patient. Antimicrob Agents Chemother 60:5130–5134. doi: 10.1128/AAC.00264-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Keepers TR, Gomez M, Celeri C, Nichols WW, Krause KM. 2014. Bactericidal activity, absence of serum effect, and time-kill kinetics of ceftazidime-avibactam against beta-lactamase-producing Enterobacteriaceae and Pseudomonas aeruginosa. Antimicrob Agents Chemother 58:5297–5305. doi: 10.1128/AAC.02894-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Endimiani A, Hujer KM, Hujer AM, Pulse ME, Weiss WJ, Bonomo RA. 2011. Evaluation of ceftazidime and NXL104 in two murine models of infection due to KPC-producing Klebsiella pneumoniae. Antimicrob Agents Chemother 55:82–85. doi: 10.1128/AAC.01198-10. [DOI] [PMC free article] [PubMed] [Google Scholar]