Abstract
Background
Breastfeeding is an important public health initiative. Low-income women benefiting from the U.S. Department of Agriculture’s Food and Nutrition Service Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) are a prime population for breastfeeding promotion efforts.
Research aim
This study aims to determine factors associated with increased likelihood of breastfeeding for WIC participants.
Methods
The Preferred Reporting Items for Systematic Reviews and Meta-Analysis statement guided the systematic review of literature. Database searches occurred in September and October 2014 and included studies limited to the previous 10 years. The following search terms were used: low-income; WIC; women, infants, and children; breastfeeding; breast milk; and maternal and child health. The criterion for inclusion was a study sample of women and children enrolled in the WIC program, thereby excluding non-United States–based research.
Results
Factors that increased the likelihood of breastfeeding for WIC participants included sociodemographic and health characteristics (n = 17); environmental and media support (n = 4); government policy (n = 2); intention to breastfeed, breastfeeding in hospital, or previous breastfeeding experience (n = 9); attitudes toward and knowledge of breastfeeding benefits (n = 6); health care provider or social support; and time exposure to WIC services (n = 5).
Conclusion
The complexity of breastfeeding behaviors within this population is clear. Results provide multisectored insight for future research, policies, and practices in support of increasing breastfeeding rates among WIC participants.
Keywords: breastfeeding, breastfeeding promotion, infant nutrition, public health nutrition, Special Supplemental Nutrition Program for Women, Infants, Children
Background
Breastfeeding is a top public health priority due to its unparalleled, favorable health outcomes affecting infants, mothers, and entire communities (American Academy of Pediatrics [AAP], 2012; National WIC Association, 2013; U.S. Department of Health and Human Services [HHS], 2011). For this reason, the AAP recommends that breastfeeding continue for at least 1 year and exclusively for the first 6 months (AAP, 2012). Comprehensive breastfeeding data show that widescale promotion has the potential to reduce health care costs in the United States by $13 billion annually (Bartick & Reinhold, 2010), increase economic input (Victora et al., 2015), and decrease the use of natural and fiscal resources required to produce and use human milk alternatives (HHS, 2011).
The U.S. Department of Agriculture’s (USDA) Food and Nutrition Service Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) continues to be integral to American public health (National WIC Association, 2013). Since pilot initiation in 1972, WIC has supplemented low-income women, infants, and children with nutrition, education, and breastfeeding support to address population-specific health concerns. Today, the reach of WIC is significant, extending to nearly one half of all infants born in the United States (USDA, 2012).
Special Supplemental Nutrition Program for Women, Infants, and Children packages include full, partial, or no breastfeeding, with full breastfeeding inclusive of a greater multitude of food offerings for the mother and less formula issuance overall. A full breastfeeding mother enrolled in WIC is eligible to receive food package offerings up to 1 year after delivery, an incentive not offered to women choosing partial or no breastfeeding. Furthermore, a full breastfeeding package recipient receives $10 vouchers for fresh fruits and vegetables, whereas all other package participants receive $8 (USDA, 2014).
Despite efforts to encourage breastfeeding, mothers participating in WIC continue to display lower rates of breastfeeding on a national scale in comparison with nonparticipants (Deming, Briefel, & Reidy, 2014; Jacknowitz, Novillo, & Tiehen, 2007; Jensen, 2012; Oliveira, 2002; Ponza, Devaney, Ziegler, Reidy, & Squatrito, 2004; Ryan & Zhou, 2006; USDA, 2012; Ziol-Guest, 2010). A recent review highlighted specific barriers to breastfeeding within the WIC population: lack of social and provider support, return to work and worksite barriers, lactation issues, WIC program and policy issues, and social or cultural hindrances (Hedberg, 2013). Another review studied the effect of the recent 2009 WIC food package revisions on participants’ dietary intake, access to healthy food and beverages, and breastfeeding (Schultz, Byker Shanks, & Houghtaling, 2015).
This systematic review of the literature examines factors associated with an increased likelihood of breastfeeding among WIC participants, a scope lacking in the literature. The literature search was narrowed to WIC participants only, as evidence demonstrates demographic differences between those who participate and those who abstain from the WIC program, despite eligibility (USDA, 2012).
Methods
Design
The Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) (Moher, Liberati, Tetzlaff, Altman, & PRISMA Group, 2009) statement guided methodological parameters. Articles in this search were extracted from PubMed, CINAHL, and ScienceDirect. The search for publications was conducted in September and October 2014. The following keywords were used to yield articles: low-income; WIC; women, infants, and children; breastfeeding; breast milk; and maternal and child health. A lack of literature addressing opportunities to breastfeed (as opposed to barriers) prompted authors to include all relevant articles published since January 2004. The year 2004 was selected because WIC initiated the Breastfeeding Peer Counseling initiative that year, a major program shift in support and education for the agency (USDA, 2016).
This review was exempt from institutional review board review; no human participants were involved in the research.
Sample
Articles written in English, based in the United States, observing WIC participants, and focused on breastfeeding practices were included for a review of titles and abstracts. Articles were excluded if a publication focused on a low-income population not exclusively consisting of WIC participants, health outcomes or nutrient analyses related to infant consumption of human milk, or a comparison of WIC populations and non-WIC populations. Furthermore, manuscripts that presented any data about the factors that determined the likelihood of breastfeeding were included. Manuscripts that focused only on barriers to breastfeeding were excluded, as that topic has already been extensively researched and documented in current literature.
See Figure 1 for the PRISMA Flow Diagram demonstrating the search process and article exclusions. Full-text screening resulted in the removal of 70 articles for the following reasons: no data about factors that determine increased likelihood of breastfeeding (n = 55), participant recruitment was vague and implied a sample not exclusively consisting of WIC participants (n = 11), and study primarily assessed the early introduction of solid foods with no focus on breastfeeding (n = 4). Remaining articles (n = 32) were organized into areas of research by emergent themes.
Figure 1.
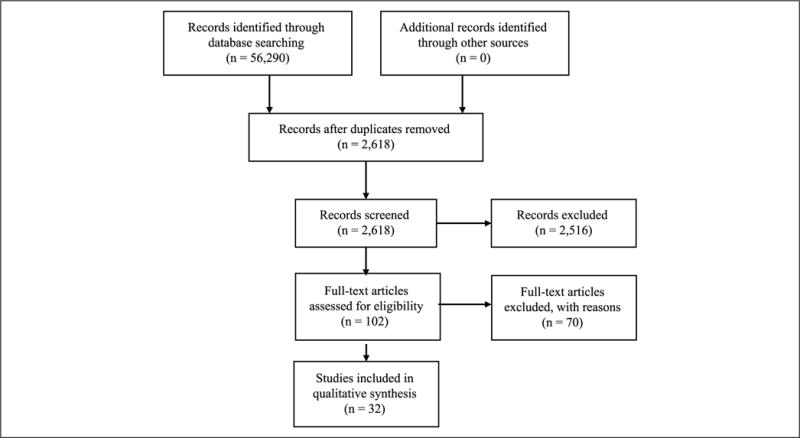
PRISMA 2009 flow diagram.
Data Collection
The Cochrane Collaboration’s tool for assessing risk of bias (Julian et al., 2011) was applied in the following ways: a total of three authors were involved in verification of inclusion versus exclusion criteria for all screened articles, including full-text review; articles were considered appropriate for analysis if all data of interest were specified within the study. Application of the Cochrane tool ensured a comprehensive analysis of resulting studies and ability to compare results across studies. Data of interest extracted from each publication are displayed in tables.
Data Analysis
After data were extracted from each article, authors met to discuss all of the factors identified in the research that support the likelihood of breastfeeding among WIC participants. Authors organized factors into seven themes.
Results
See Table 1 for references supporting each identified theme and Table 2 for characteristics of included studies.
Table 1.
Articles Contributing to Emerged Thematic Results in Systematic Review Assessing Factors Associated With Increased Likelihood of Breastfeeding Among Participants of WIC.
Note. WIC = Special Supplemental Nutrition Program for Women, Infants, and Children. N = 32. In many cases, articles were categorized into multiple research foci, due to the frequency of association with several identified themes (n = 16).
Table 2.
Variables of Included Research for Systematic Review Identifying Predictors of Increased Likelihood of Breastfeeding Within the WIC Population.
| First author, year | Research design | Participant characteristics | State | Study description | Data collection |
|---|---|---|---|---|---|
| Campbell, 2014 | Cross-sectional | WIC participants: no prior breastfeeding experience | TX | Determined PC contact with breastfeeding initiation rates among primiparas and women with no prior breastfeeding experience | Infant Feeding Practices Survey |
| Cricco-Lizza, 2004 | Ethnographic | WIC participants and their relatives or friends | NY | Explored context of infant-feeding decisions in an urban WIC clinic | Participant observation; interviews; key informants |
| Cricco-Lizza, 2005 | Ethnographic | WIC participants and their relatives or friends | NY | Explored context of infant-feeding decisions in an urban WIC clinic | Participant observation; interviews; key informants |
| Cross-Barnet, 2012 | Qualitative | WIC participants: with infants; met at least once with PC | MD | Explored infant-feeding education and support experiences of mothers | Semistructured interviews |
| Darfour-Oduro, 2014 | Cross-sectional | WIC participants: mother–infant dyads; biological mothers | IL | Understanding of mothers’ social environments and well-being in postnatal period, including breastfeeding initiation and duration to 3 months | Survey |
| Dodgson, 2007 | Retrospective | WIC participants: postpartum; initiated breastfeeding | HI | Description of breastfeeding patterns of women who had initiated breastfeeding | WIC participant data |
| Fornasaro-Donahue, 2014 | Mixed methods descriptive | WIC participants: pregnant or nonbreastfeeding women with infant age 1-4 months | RI | Assessed cost of formula as a motivator and deciding factor in breastfeeding decision | Surveys; interviews |
| Gross, 2009 | Cross-sectional | WIC participants | MD | Determined rates of breastfeeding initiation by PC program participation | Electronic data |
| Haughton, 2010 | Retrospective | WIC participants: breastfed at least one child who was younger than 5 | CT | Identification of factors associated with breastfeeding duration | Survey; self-completed or administered |
| Hildebrand, 2014 | Two-part quasi-experimental | WIC participants: parents and caregivers of children (birth–3 years); WIC clinics | OK | Changes in physical and social environment in four WIC clinics determined perception of WIC experience and breastfeeding initiation | Computerized survey; secondary breastfeeding data |
| Hurley, 2008 | Cross-sectional | WIC participants | MD | Examined how breastfeeding behaviors, perceptions, and experiences vary by race/ethnicity in the United States | Telephone survey |
| Jacobson, 2015 | Cross-sectional | WIC participants | KS | Sought insight into maternal characteristics associated with breastfeeding among urban and rural women | Pregnancy Nutrition Surveillance System data set |
| Joyce, 2008 | Cross-sectional | WIC participants: enrolled during pregnancy and continued enrollment postpartum | FL, GA, IN, MI, MO, NJ, NC, OH, VA | Tested exposure to WIC and associated outcomes with smoking, weight gain during pregnancy, birth outcomes, and likelihood of breastfeeding | Pregnancy Nutrition Surveillance System data set |
| Langellier, 2012 | Cross-sectional | WIC participants: biological mother of child in WIC | CA | Measured effect of in-hospital breastfeeding, receiving of formula discharge pack, and maternal return to work on breastfeed duration | Survey data from 2008; telephone interview |
| Langellier, 2014 | Cross-sectional; pre/post design | WIC participants: English or Spanish speaking | CA | Effect of 2009 WIC changes on breastfeeding outcomes | Survey questionnaire; interview |
| Lovera, 2010 | Cohort; intervention | WIC participants: mothers and spouses; initiated breastfeeding | TX | Pilot Peer Dad Program based on theory of planned behavior aimed toward fathers to promote support of breastfeeding through peer counseling | Structured interviews |
| Ma, 2012 | Cross-sectional | WIC participants: first-time mothers | LA | Application of positive deviance concept to explore characteristics of positive deviants for breastfeeding | LaPRAMS from 2000–2004 |
| McKechnie, 2009 | Retrospective | WIC participants | WI | Examined exclusive versus partial breastfeeding relating to breastfeeding duration and determined association of demographic characteristics | Maternal records from existing database |
| Meehan, 2008 | Cross-sectional; pre/post design | WIC participants: English or Spanish speaking | CA | Electric pump loan program determined facility of breastfeeding for mothers returning to work | Survey questionnaire; interview |
| Metallinos-Katsaras, 2015 | Longitudinal | WIC participants: prenatal and postpartum; singleton live births | MA | Association between length of exposure to WIC and breastfeeding initiation and duration | WIC breastfeeding data |
| Mickens, 2009 | Cross-sectional | WIC participants: any stage of pregnancy | CA | Identification of effect factors for low-income women’s infant-feeding decisions | Structured survey questionnaire |
| Mistry, 2007 | Quantitative | WIC participants | CA | Breastfeeding PC used the theory of planned behavior to assess intentions, attitudes, and norms toward breastfeeding | Structured survey questionnaire |
| Murimi, 2010 | Cross-sectional | WIC participants: rural residency | LA | Determined factors that have largest effect on breastfeeding and effect of formula provision by WIC on breastfeeding | Validated questionnaire, adapted |
| Olson, 2010 | Quasi-experimental | WIC participants | MI | Examined effectiveness of a PC program | Administrative and survey-based sources |
| Reeder, 2014 | Stratified, randomized | WIC participants: indicated intention or indecisiveness to breastfeed | OR | Effectiveness of a telephone PC program for increased breastfeeding initiation, duration, and exclusivity | Data retrieved from OR WIC Information System Tracker (TWIST) |
| Sayegh, 2007 | Pre/post intervention | WIC participants: rural; expectant or new mothers | TX | Pilot media breastfeeding outreach campaign (posters, billboard, radio, TV, newspaper, magazine ads, community presentations, gift basket distribution) | Interviews |
| Stremler, 2004 | Intervention | WIC participants: fathers of enrolled infants and children | TX | Father peer support program development from documented success from PC and research identifying father’s attitude as important influence on breastfeeding | Exit interviews |
| Tender, 2009 | Retrospective | WIC participants | DC | Identified reasons that breastfeeding mothers begin inhospital formula supplementation and risk factors associated with supplementation | Orally administered survey |
| Tenfelde, 2011 | Cross-sectional | WIC participants: initiated breastfeeding and responded to a question on breastfeeding exclusivity | IL | Examined predictors of breastfeeding exclusivity in hospital in an urban area | Clinical and administrative data |
| Vaaler, 2010 | Cross-sectional | WIC participants: mothers of young children | TX | Influences of demographic characteristics, breastfeeding in public, attitudes to infant feeding, and use of formula on breastfeeding | Infant Feeding Practices Survey |
| Whaley, 2012 | Pre/post data analysis | WIC participants | CA | Effect of 2009 WIC food package changes with increased staff training and education on breastfeeding package issuance rates | WIC data on breastfeeding and infant-feeding packages issued |
| Yun, 2010 | Cross-sectional | WIC participant data: all 118 WIC agencies | MO | Effectiveness of PC programs on breastfeeding initiation and identification of factors to facilitate breastfeeding initiation | 2006 Pregnancy Nutrition Surveillance System, birth certificate data |
Note. PC = peer counselor; WIC = Special Supplemental Nutrition Program for Women, Infants, and Children. N = 32.
Sociodemographic and Health Characteristics
Seventeen studies found specific sociodemographic and health characteristics that predicted the likelihood of breastfeeding (see Table 3), including absence of depression (n = 1), age (n = 8), decreased body mass index (n = 2), decreased time spent in the United States (n = 3), delayed return to work (n = 1), increased income (n = 2), larger weight infants (n = 1), geographic location (n = 1), cohabitation with child’s father (n = 1), lower birth-weight infants (n = 1), marriage (n = 2), more years of education (n = 6), not receiving food stamps (n = 1), nonsmoking (n = 1), number of prior children (n = 3), planned pregnancies (n = 1), prenatal care (n = 1), Spanish speaking (n = 4), taking multivitamins (n = 1), unemployed or working part-time (n = 1), and urban residency (n = 2).
Table 3.
Sociodemographic and Health Characteristics as a Predictor of Increased Likelihood of Breastfeeding Within the WIC Population.
| First author, year | Results indicating increased likelihood of breastfeeding |
|---|---|
| Campbell, 2014a | More than a high school education; Hispanic women; first-time pregnant women when compared with women who did not breastfeed in prior pregnancies |
| Darfour-Oduro, 2014 | Married mothers 3.47 times more likely to initiate breastfeeding and 4.08 times more likely to continue through 3 months. Not receiving food stamps; not diagnosed with postpartum depression or not depressed (not statistically significant) |
| Dodgson, 2007a | Multiparous; older age (not significant) |
| Gross, 2009a | Hispanic participants had highest breastfeeding rates in all categories; larger infants in comparison with low-birth-weight infants |
| Haughton, 2010a | Additional year of maternal age, less time spent in United States associated with breastfeeding at 6 months; planned pregnancies 2 times as likely to breastfeed for at least 6 months |
| Hildebrand, 2014a | White women more likely to breastfeed compared with American Indians/Alaska Natives; women with one child in comparison with women with two or more children; age 28 or older |
| Hurley, 2008 | Hispanic mothers more likely (91%) than African American (65%) or white (61%) to initiate; maternal age; decreased infant age; more than high school education |
| Jacobson, 2015a | Urban women: Hispanic; 18–19 years old; more than a high school education; earning more than $10,000 per year; prenatal care early in pregnancy; nonsmoking; use of multivitamins. Not variable within rural population (age, income, prenatal care, WIC enrollment timing not statistically significant predictors) |
| Langellier, 2012a | Non-Hispanic white mothers had 2.9 times the odds of Hispanic mothers to breastfeed exclusively at 6 months; foreign-born mothers more likely to breastfeed at 6 and 12 months; Spanish-speaking mothers more likely to breastfeed at 6, 12, and 24 months; mothers living with child’s parent 21% increased odds of breastfeeding at 6 months and 31% increased odds at 12 months; mothers returning to work after 7 months postpartum more likely to breastfeed at 6, 12, and 24 months |
| Langellier, 2014a | Latinas in comparison with blacks more likely to initiate breastfeeding but less likely to exclusively breastfeed at 6 months; white mothers more likely than Latinas to exclusively breastfeed at 3 and 6 months; children’s age, mother’s education, foreign nativity, and Spanish speaking |
| Ma, 2012a | White: increased breastfeeding initiation by maternal age and education, more likely to initiate breastfeeding when compared with black mothers. Black: married, 13 years or more of education, urban residence, and low-birth-weight infants. Positive deviants were more likely to have a job prior to delivery |
| McKechnie, 2009 | Exclusive breastfeeding associated with older mothers and mothers with lower body mass index |
| Mickens, 2009a | Income greater than $18,000 |
| Murimi, 2010a | White; unemployed or part-time work; married |
| Reeder, 2014a | Nonexclusive breastfeeding duration greater at 6 months for Spanish speakers only; likelihood of exclusive breastfeeding cessation less among Spanish speakers |
| Tenfelde, 2011a | Women not classified as overweight or obese 50% more likely |
| Vaaler, 2010a | Higher education; older age; Spanish-speaking Hispanic; metropolitan residence; not living near the Texas–Mexico border |
Note. WIC = Special Supplemental Nutrition Program for Women, Infants, and Children. n = 17.
Data are also displayed in other table(s).
In addition, white or Hispanic women were documented as being more likely to breastfeed than non-Hispanic black or American Indians/Alaska Natives (n = 10).
Environmental and Media Support
Four articles targeted the WIC participant’s environment (n = 3) and media promotion (n = 1) (see Table 4).
Table 4.
Environmental and Media Support as a Predictor of Increasing the Likelihood of Breastfeeding Within the WIC Population
| First author, year | Results indicating increased likelihood of breastfeeding |
|---|---|
| Cricco-Lizza, 2005a | Clinic environment with culturally appropriate posters with relevant messages potentially influential of infant-feeding decisions; encouraged women to breastfeed or think about breastfeeding more |
| Hildebrand, 2014a | Women 1.5 times more likely to initiate breastfeeding in influence model when compared with traditional services |
| Meehan, 2008 | Mothers receiving pump as soon as requested did not request formula supplementation until 8.8 months on average and 5.5 times more likely to not request formula at 6 months |
| Sayegh, 2007 | Postcampaign, providers reported more breastfeeding-specific questions being asked; intention to breastfeed |
Note. WIC = Special Supplemental Nutrition Program for Women, Infants, and Children. n = 4.
Data are also displayed in other table(s).
One study focused on changing the normative formula-feeding method for urban black women enrolled in WIC. Posters that promoted breastfeeding were influential overall and persuasive to one WIC participant who chose breastfeeding. In addition, positive social interactions between WIC staff and participants facilitated breastfeeding discussion and increased breastfeeding initiation.
Another study found that changing the social and physical WIC clinic environment promoted breastfeeding efforts. Intervention tactics included staff training to align communication styles to WIC principles and increased visual promotion efforts of breastfeeding. Furthermore, visual and audio breastfeeding advertisements through a media campaign in rural Texas resulted in increased inquiries about breastfeeding practices to health care providers. Last, one study associated ease of access to breast pumps in the WIC participant’s environment with longer breastfeeding duration of WIC participants.
Government Policy
Recent changes in policy regarding the WIC food package contents positively influenced participant breastfeeding rates (see Table 5). One study compared pre-2009 and post-2009 revision package choices. More participants chose full breastfeeding packages postrevision and extended the duration of exclusive breastfeeding, although regional differences were observed.
Table 5.
Government Policy as a Predictor of Increasing the Likelihood of Breastfeeding Within the WIC Population.
| First author, year | Results indicating increased likelihood of breastfeeding |
|---|---|
| Langellier, 2014a | Participants receiving new food package had 2.2 times the odds of breastfeeding initiation, 1.7 times the odds of exclusive breastfeeding at 3 months, and 3.1 times the odds of exclusive breastfeeding through 6 months |
| Whaley, 2012a | Full breastfeeding package issuance increased by 86%; increase of exclusive breastfeeding at 2 and 6 months |
Note. WIC = Special Supplemental Nutrition Program for Women, Infants, and Children. n = 2.
Data are also displayed in other table(s).
Another study increased staff training and participant education at various WIC agencies in order to promote the full breastfeeding package option corresponding with 6 months pre-implementation of 2009 WIC food package content changes. These efforts increased initiation and duration of breastfeeding measured at 2 and 6 months, with an additional increase postimplementation of food package revisions.
Intention to Breastfeed
Nine articles indicated intention to breastfeed as a predictor of breastfeeding (see Table 6). Three studies specifically identified intention to breastfeed as being predictive of exclusive breastfeeding and one identified increased odds of longer duration to 3 and 6 months. Breastfeeding in hospital and previous breastfeeding experience were defined as intent to breastfeed, based on the conclusion of two studies within this data set.
Table 6.
Intention to Breastfeed, Breastfeeding in Hospital, or Previous Breastfeeding Experience as a Predictor of Increasing the Likelihood of Breastfeeding Within the WIC Population.
| First author, year | Results indicating increased likelihood of breastfeeding |
|---|---|
| Dodgson, 2007a | Mothers exclusively breastfed at initiation weaned significantly later and more likely to breastfeed for 6 months |
| Langellier, 2012a | Exclusive breastfeeding in hospital 9.9 times more likely to breastfeed for 6 months, 8 times the odds of breastfeeding at 12 months, and 5.7 times the odds of breastfeeding at 24 months; mothers reporting prenatal intention to breastfeed had 3.6 times the odds of breastfeeding at 6 months with 7.4 times the odds of exclusive breastfeeding |
| Langellier, 2014a | Intention to breastfeed: 12 times the odds of initiation, 3 or more times the odds of any breastfeeding at 3 and 6 months, and 4 or more times the odds of exclusive breastfeeding at 3 and 6 months. Exclusive breastfeeding in hospital: about 10 times the odds of any breastfeeding at 3 months and at least 6 times the odds at 6 months |
| Lovera, 2010a | Mothers who previously breastfed 2 times more likely to breastfeed for 6 months or longer |
| McKechnie, 2009 | Those who initiated exclusive breastfeeding and continued past 6 weeks breastfed significantly longer |
| Mickens, 2009a | Previous breastfeeding experience related to increased intent to breastfeed |
| Murimi, 2010a | Mothers breastfed as infants more likely to breastfeed their infants |
| Tender, 2009 | Participation in prenatal breastfeeding class sole factor significantly associated with exclusive breastfeeding in hospital |
| Tenfelde, 2011a | Women intending to breastfeed (determined by prenatal visit) about 4 times more likely to breastfeed exclusively |
Note. WIC = Special Supplemental Nutrition Program for Women, Infants, and Children. n = 9.
Data are also displayed in other table(s).
One study identified participation in a prenatal breastfeeding education class as influential on exclusive breastfeeding in hospital. Exclusive breastfeeding initiation in the hospital led to higher breastfeeding duration rates for WIC participants to at least 6 (n = 4), 12 (n = 1), and 24 months (n = 1).
Knowledge and Attitudes Toward Breastfeeding
Six articles noted the positive effect of knowledge of breastfeeding and its benefits (see Table 7) on likelihood of breastfeeding. Informed decision making based on increased knowledge of mother and infant health benefits (n = 4) and bonding with child through breastfeeding (n = 1) were important factors influencing the decision to breastfeed for WIC mothers. In addition, stronger beliefs about breastfeeding’s benefits (n = 2) and positive attitudes toward breastfeeding a child and breastfeeding in public were important determinants (n = 1).
Table 7.
Attitudes Toward and Knowledge of Breastfeeding Benefits as a Predictor of Increasing the Likelihood of Breastfeeding Within the WIC Population.
| First author, year | Results indicating increased likelihood of breastfeeding |
|---|---|
| Cricco-Lizza, 2004 | Women who chose breastfeeding reported that health benefits, advantages of breastfeeding, and close bond with baby are what interested them in the process |
| Fornasaro-Donahue, 2014 | Primary reason to choose breastfeeding was health benefits to infant; cost of formula not influential on breastfeeding decision, but considered additional motivation for women who chose breastfeeding |
| Mickens, 2009a | Knowledge of breastfeeding and fewer negative beliefs of breastfeeding |
| Mistry, 2007 | Stronger beliefs supporting breastfeeding |
| Murimi, 2010a | 39% of breastfeeding women reported breastfeeding benefits for baby as most important reason for breastfeeding; 96% of participants reported that breastfeeding benefits given at WIC were clear and helped in decision to breastfeed |
| Vaaler, 2010a | Positive attitudes to breastfeeding benefits and breastfeeding in public more likely to breastfeed exclusively for 1 year |
Note. WIC = Special Supplemental Nutrition Program for Women, Infants, and Children. n = 6.
Data are also displayed in other table(s).
Health Care Provider and Social Support
Fifteen studies contributed to the theme of health care provider and social support (see Table 8). Support from health care professionals (n = 6), peer counseling (n = 6), and family support (n = 2) increased the likelihood of breastfeeding.
Table 8.
Health Care Provider or Social Support as a Predictor of Increasing the Likelihood of Breastfeeding Within the WIC Population.
| First author, year | Results indicating increased likelihood of breastfeeding |
|---|---|
| Campbell, 2014a | PC contact during pregnancy or after delivery more likely to initiate breastfeeding; receiving PC contacts during pregnancy and hospitalization highest percentage of breastfeeding initiation |
| Cricco-Lizza, 2005a | Attentiveness, kindness, and empathy of WIC staff in culturally appropriate interactions seemed to encourage women to be more open to the promotion of breastfeeding |
| Cross-Barnet, 2012 | One mother in sample reported positive, consistent support and information from health care provider and was only mother who breastfed exclusively for at least 10 months |
| Gross, 2009a | Odds of breastfeeding initiation 21% greater for PC-exposed infants |
| Haughton, 2010a | Women who consulted with lactation consultants or WIC staff with breastfeeding issues |
| Hildebrand, 2014a | Women 1.5 times more likely to initiate breastfeeding in influence model when compared with traditional services |
| Langellier, 2012a | Mothers not receiving discharge formula pack more likely to breastfeed exclusively for 6 months |
| Lovera, 2010a | Peer Dad Program participation resulted in 63.4% of women breastfeeding for 6 months or longer compared with 54.6% of nonprogram participants (not statistically significant) |
| Ma, 2012a | Positive deviants more likely to have received information about breastfeeding from staff |
| Mickens, 2009a | Regardless of breastfeeding knowledge or beliefs, women who attended support group 2 or more times more likely to intend to breastfeed |
| Olson, 2010 | Estimated PC increased breastfeeding initiation by 27% and increased mean duration of breastfeeding by 3.6 weeks. |
| Reeder, 2014a | Treatment group breastfeeding nonexclusively for at least 3 months was 22% greater than control. |
| Stremler, 2004 | Initiation of breastfeeding increased at clinics employing peer dads |
| Yun, 2010a | Breastfeeding initiation rate in PC agencies 2.3% higher than non-PC agencies. Increased breastfeeding initiation rates: agencies with more years of PC experience; PC who had other positions within organization; PC coordinator as Breastfeeding PC Task Force member |
| Whaley, 2012a | Staff training and participant education (WIC changes and breastfeeding decisions) increased full breastfeeding package rates and exclusive breastfeeding to 2 and 6 months before policy change |
Note. PC = peer counselor; WIC = Special Supplemental Nutrition Program for Women, Infants, and Children. n = 15.
Data are also displayed in other table(s).
Health care professional support varied among the following: conveying feelings of empathy (n = 2); positive, consistent interactions with clients (n = 1); utilization of WIC staff or lactation consultants for breastfeeding barriers (n = 1); providing any breastfeeding information (n = 1); and increased staff training on 2009 WIC food package changes for breastfeeding promotion (n = 1).
Group support through peer counseling had a greater effect than education efforts in breastfeeding (n = 1). Overall, any involvement in a peer counseling group had positive outcomes for breastfeeding (n = 3), with implications of prenatal involvement or in-hospital peer counselor support being even more beneficial to the likelihood of breastfeeding (n = 1). A telephone-based counseling support network primarily for Spanish-speaking participants was successful in increasing likelihood of breastfeeding. Furthermore, two studies focused on peer dad interventions in Texas with a primarily Hispanic population.
Time Exposure to WIC
Five articles are associated with the theme of time exposure to WIC (see Table 9). Participants enrolled in WIC during the first (n = 2) and second trimesters (n = 3) are more likely to breastfeed than participants enrolled later.
Table 9.
Time Exposed to WIC Services as a Predictor of Increasing the Likelihood of Breastfeeding Within the WIC Population.
| First author, year | Results indicating increased likelihood of breastfeeding |
|---|---|
| Jacobson, 2015a | Urban women enrolling in WIC during first trimester had increased odds of initiating breastfeeding; not statistically significant for rural women |
| Joyce, 2008 | Whites: enrolled in WIC during first trimester (2.2%) and second trimester (1%) more likely to breastfeed when compared with whites enrolled during third trimester. Blacks: enrolled in WIC prenatally (3.1%), during first trimester (3.9%), and during second trimester (3.7%) more likely to breastfeed when compared with blacks enrolled during third trimester. Hispanics: enrolled in WIC prenatally (4.6%), during first trimester (5.7%), and during second trimester (4.7%) more likely to breastfeed when compared with Hispanics enrolled during third trimester |
| Metallinos-Katsaras, 2015 | Women entered into WIC in first trimester more likely to breastfeed for 3 months (15%), 6 months (25%), and 12 months (33%) than women enrolled in third trimester; associations differed upon whether mother had previous live birth |
| Tenfelde, 2011a | Women entering care during first trimester 2 times as likely to exclusively breastfeed |
| Yun, 2010a | Both PC and non-PC agencies: women enrolled in WIC prior to last 3 months antepartum were more likely to initiate breastfeeding; longer duration correlated with time of WIC enrollment |
Note. PC = peer counselor; WIC = Special Supplemental Nutrition Program for Women, Infants, and Children. n = 5.
Data are also displayed in other table(s).
Discussion
To the authors’ knowledge, this systematic review of the literature is the first to highlight positive factors that increase the likelihood of breastfeeding in the WIC population. The review identified 32 articles that described seven distinct factors. Below, we provide guidance on adapting strategies in research or practice with WIC populations to promote breastfeeding. The discussion is based on promoting breastfeeding strategies with the WIC population at the individual, social, environmental, and policy levels around the seven identified factors. A co-interaction of the determined factors is conceptually portrayed in Figure 2.
Figure 2.
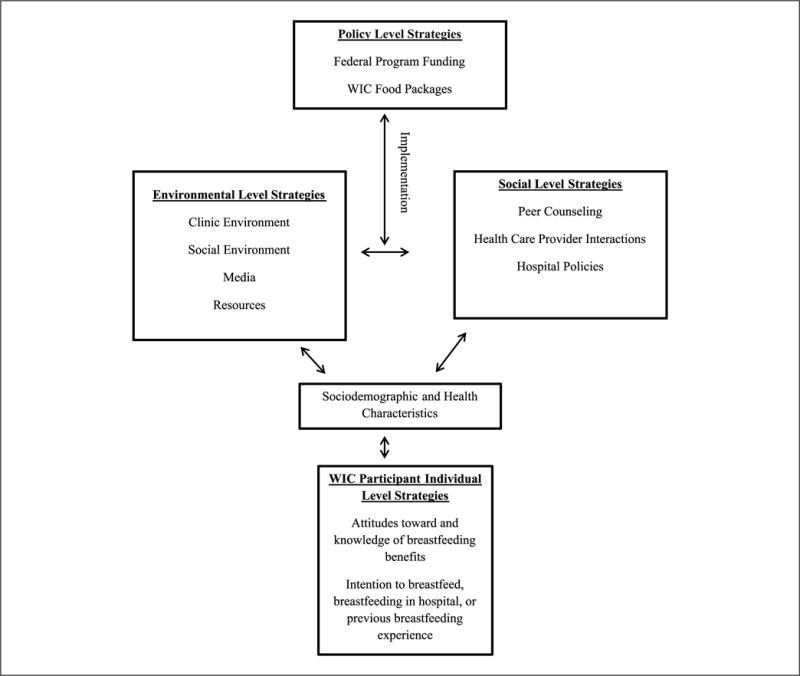
Individual, social, environmental, and policy level strategies based on clientele sociodemographic and health characteristics: Important factors in increasing the likelihood of breastfeeding in the Special Supplemental Nutrition Program for Women, Infants, and Children population.
Individual Level Strategies
Nationally, demographic characteristics such as income, education, and race/ethnicity are well documented as factors increasing the likelihood of breastfeeding (HHS, 2011). Persons classified in lower socioeconomic groups, with less education, or of minority race/ethnicity are often less likely to initiate and sustain breastfeeding (HHS, 2011). Overall, findings provide important information about tailoring WIC services to different sociodemographic audiences with particular health outcomes and behaviors. For example, inclusion of weight management counseling, coping skills, couple counseling, smoking cessation support, workplace breastfeeding, and family planning may be important additions to breastfeeding interventions for specific populations and warrant further research specific to the WIC population.
Breastfeeding science should offer meaningful insights into deeper and more personal barriers to breastfeeding moving forward. For example, lack of depression increased likelihood of breastfeeding (Darfour-Oduro & Kim, 2014). Many low-income women throughout the United States suffer from substance abuse or dependence, domestic violence, and depression (Lawrence, Chau, & Lennon, 2004), which are not listed or studied as barriers to breastfeeding in recent literature. Future research needs to determine the role of the aforementioned factors as potential barriers to breastfeeding among WIC participants.
Resonation of differing education methods should be tested with ethnically and racially diverse WIC mothers and respective educators. The WIC Nutrition Services Standards provide some insight into education requirements of staff members, highlighting multicultural awareness training (USDA, 2001). Likewise, education guides for multicultural WIC communities exist (Food and Research Action Center, 2009). Perhaps, further tailoring of these resources through site-specific, direct feedback from clientele would be helpful moving forward.
The infant-feeding method that the mother determines during pregnancy strongly aligns with the infant-feeding method used when the infant is born (Mistry, 2007), indicating that prenatal intention to breastfeed is predictive of breastfeeding. Considering that 10.1% of WIC participants are prenatal (Johnson et al., 2013), stronger efforts to promote breastfeeding among this group would be beneficial.
Information about breastfeeding and time exposed to the WIC program is conflicting to date. A study including a national representation of WIC participants determined that participation in WIC during the first and second trimesters is associated with decreased likelihood of breastfeeding (Ziol-Guest, 2010). Possibly confounding variables, such as resources allocated and breastfeeding promotion techniques at individual WIC clinics, as evidenced by this review, are more influential on infant-feeding decisions than are time exposure. Perhaps, allocated resources beyond the minimum breastfeeding promotion standards have an increased benefit to breastfeeding when combined with variables such as time exposure to government services.
Social Level Strategies
Social support is strongly related to the likelihood of breastfeeding, and lack thereof is a known barrier to breastfeeding in the WIC population (Hedberg, 2013). A recent publication identified the necessity to offer peer counseling support to every WIC participant, highlighting the limited funding available for such programs (Baumgartel & Spatz, 2013). Allocated WIC resources for formula purchases are 25 times higher than breastfeeding promotion efforts, even when peer support programs supported by WIC are lacking throughout much of the country (Baumgartel & Spatz, 2013).
Peer counseling for WIC fathers and the effectiveness of such an intervention likely rely on cultural appropriateness. One study inclusive of Puerto Rican males demonstrated their willingness to provide support to a woman in the breastfeeding decision (Rivera Alvarado, Vázquez García, Dávila Torres, & Parrilla Rodríguez, 2006). Conversely, ongoing tribal research demonstrates breastfeeding as primarily a woman’s role with limited male support. In this specific research, a greater focus on female family members in providing breastfeeding support is more appropriate (Houghtaling, Byker Shanks, Ahmed, & Rink, in preparation). Translation of peer or partner breastfeeding support across WIC should focus on building different frameworks based on differing cultural contexts.
Partner support in breastfeeding specific to Hispanic fathers of WIC dyads is acknowledged in this review. Culture is influential on behavior and health outcomes (Abraído-Lanza, Chao, & Flórez, 2005). Increased emigrant duration in the United States (acculturation) in recent years has influenced the integration of Americanized beliefs and practices with traditional knowledge (Abraído-Lanza et al., 2005). This transition affects breastfeeding initiation and duration, documented within the Hispanic or Latina populations as having a greater likelihood of breastfeeding when less assimilated (Chapman & Pérez-Escamilla, 2013).
Environmental Level Strategies
Recent public health nutrition research has focused on the potential of environmental factors to contribute to high obesity and chronic disease rates (Glanz, Sallis, Saelens, & Frank, 2007). For example, food environments have the potential to influence health behavior and influence dietary choices (Glanz et al., 2007) and school lunchroom layouts by influencing positive dietary intake (Wansink, 2004; Wansink, Just, Payne, & Klinger, 2012; Wansink, Just, & Smith, 2011). Evidence of how the WIC clinic environment influences breastfeeding behavior is limited in published research.
The WIC Nutrition Services Standards (USDA, 2001) address the need for the clinic’s environment to be conducive to breastfeeding success. Strategies include limiting formula advertisements and being respectful of breastfeeding mothers in the waiting area or providing private accommodations (USDA, 2001). Research is needed to determine the effect of an increasingly supportive WIC environment on breastfeeding rates. Results could guide specific policy guidelines about facility layouts for health promotion. For example, Baby-Friendly Hospital Initiatives provide a framework for extended health care provider support to new mothers (HealthDay News, 2015). Learning from such initiatives and modifying to create optimal WIC environments and provider support networks may increase breastfeeding practices.
Policy Level Strategies
In 2009, the USDA implemented an interim rule adjustment in WIC program policies, recommended by the Institute of Medicine (2006), part of which incentivized breastfeeding for enrolled mothers in promotion of breastfeeding according to the AAP recommendations (AAP, 2012). The new food packages had positive effects for breastfeeding mothers (Langellier, Chaparro, Wang, Koleilat, & Whaley, 2014; Whaley et al., 2012). Issuance rates of full breastfeeding packages increased in a study of 10 states’ WIC administrative records (Wilde, Wolf, Fernandes, & Collins, 2012); however, partial breastfeeding packages also increased and initiation rates of breastfeeding remained largely unchanged, implying no substantive evidence of increased likelihood of breastfeeding (Wilde et al., 2012).
Policy changes can provide guidelines for breastfeeding improvement. Important to consider for success is the method of local implementation and potential regional differences. Further research identifying the weight of differential population and regional factors alongside new policy implementations in support of breastfeeding within the WIC population is justified.
Limitations
Researchers did not include negative or neutral results within the scope of this literature review; this represents a large limitation, as this information is also necessary in informing breastfeeding science and policy. Review parameters were chosen to emphasize positive associations of breastfeeding within the WIC population, as much of the literature to date has focused on barriers that are now well understood. The authors included articles over a 10-year span, since 2004 when a peer support model was introduced to WIC. This is a clear limitation, as changes in breastfeeding practices and WIC policies during this time potentially influenced study results and are not addressed.
Methodological limitations include the following: Terms and databases used for the literature search may not have resulted in a comprehensive list of studies; inclusion of only peer-reviewed articles may have excluded work such as theses, dissertations, or government documents; a lack of specified quality parameters for study inclusion may limit the merit of results with potential for a large variation in quality among included studies; and a limited number of articles per theme necessitates further investigations into each described outcome.
Conclusion
Recent policy reform increased incentives for WIC breastfeeding participation, though the distribution of infant formula remains controversial and a barrier to breastfeeding (Hedberg, 2013). The ability of the WIC program to supplement formula for mothers unable to initiate or continue to breastfeed will likely always be necessary; however, continuing to improve program incentives and federal spending in support of increasing likelihood of breastfeeding is paramount in effecting positive change in maternal and child health among WIC participants.
Key Messages.
Factors influencing the likelihood of breastfeeding within the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) population are important to understand in order to increase breastfeeding rates.
Seven themes were identified to increase the likelihood of breastfeeding within the WIC population, spanning multiple sectors of influence.
Research, policy, and practice applications at the individual, social, environmental, and policy sectors are warranted to increase WIC breastfeeding rates.
Acknowledgments
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Research reported in this publication was partially supported by the National Institute of General Medical Sciences of the National Institutes of Health under Award Number P20GM103474. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
A similar version of this article was accepted in thesis format by Montana State University in November 2015.
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Abraído-Lanza AF, Chao MT, Flórez KR. Do healthy behaviors decline with greater acculturation? Implications for the Latino mortality paradox. Social Science & Medicine. 2005;61(6):1243–1255. doi: 10.1016/j.socs-cimed.2005.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Academy of Pediatrics. Breastfeeding and the use of human milk. Pediatrics. 2012;129(3):E827–E841. doi: 10.1542/peds.2011-3552. [DOI] [PubMed] [Google Scholar]
- Bartick M, Reinhold A. The burden of suboptimal breastfeeding in the United States: A pediatric cost analysis. Pediatrics. 2010;125(5):e1048–e1056. doi: 10.1542/peds.2009-1616. [DOI] [PubMed] [Google Scholar]
- Baumgartel KL, Spatz DL. WIC (the Special Supplemental Nutrition Program for Women, Infants, and Children): Policy versus practice regarding breastfeeding. Nursing Outlook. 2013;61(6):466–470. doi: 10.1016/j.outlook.2013.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell LA, Wan J, Speck PM, Hartig MT. Women, infant and children (WIC) peer counselor contact with first time breastfeeding mothers. Public Health Nursing. 2014;31(1):3–9. doi: 10.1111/phn.12055. [DOI] [PubMed] [Google Scholar]
- Chapman DJ, Pérez-Escamilla R. Acculturative type is associated with breastfeeding duration among low-income Latinas. Maternal & Child Nutrition. 2013;9(2):188–198. doi: 10.1111/j.1740-8709.2011.00344.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cricco-Lizza R. Infant-feeding beliefs and experiences of black women enrolled in WIC in the New York metropolitan area. Qualitative Health Research. 2004;14(9):1197–1210. doi: 10.1177/1049732304268819. [DOI] [PubMed] [Google Scholar]
- Cricco-Lizza R. The milk of human kindness: Environmental and human interactions in a WIC clinic that influence infant-feeding decisions of black women. Qualitative Health Research. 2005;15(4):525–538. doi: 10.1177/1049732304273030. [DOI] [PubMed] [Google Scholar]
- Cross-Barnet C, Augustyn M, Gross S, Resnik A, Paige D. Long-term breastfeeding support: Failing mothers in need. Maternal and Child Health Journal. 2012;16(9):1926–1932. doi: 10.1007/s10995-011-0939-x. [DOI] [PubMed] [Google Scholar]
- Darfour-Oduro SA, Kim J. WIC mothers’ social environment and postpartum health on breastfeeding initiation and duration. Breastfeeding Medicine. 2014;9(10):524–529. doi: 10.1089/bfm.2014.0067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deming DM, Briefel RR, Reidy KC. Infant feeding practices and food consumption patterns of children participating in WIC. Journal of Nutrition Education and Behavior. 2014;46(3):S29–S37. doi: 10.1016/j.jneb.2014.02.020. [DOI] [PubMed] [Google Scholar]
- Dodgson JE, Codier E, Kaiwi P, Oneha MFM, Pagano I. Breastfeeding patterns in a community of native Hawaiian mothers participating in WIC. Family & Community Health. 2007;30(Suppl. 2):S46–S58. doi: 10.1097/01.FCH.0000264880.96310.9a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Food and Research Action Center. Making WIC work for multicultural communities: Best practices in outreach and nutrition education. Washington, DC: FRAC; 2009. Retrieved from www.frac.org. [Google Scholar]
- Fornasaro-Donahue VM, Tovar A, Sebelia L, Greene GW. Increasing breastfeeding in WIC participants: Cost of formula as a motivator. Journal of Nutrition Education and Behavior. 2014;46(6):560–569. doi: 10.1016/j.jneb.2014.03.003. [DOI] [PubMed] [Google Scholar]
- Glanz K, Sallis JF, Saelens BE, Frank LD. Nutrition Environment Measures Survey in stores (NEMS-S)—development and evaluation. American Journal of Preventative Medicine. 2007;32(4):282–289. doi: 10.1016/j.amepre.2006.12.019. [DOI] [PubMed] [Google Scholar]
- Gross SM, Resnik AK, Cross-Barnet C, Nanda JP, Augustyn M, Paige DM. The differential impact of WIC peer counseling programs on breastfeeding initiation across the state of Maryland. Journal of Human Lactation. 2009;25(4):435–443. doi: 10.1177/0890334409342070. [DOI] [PubMed] [Google Scholar]
- Haughton J, Gregorio D, Perez-Escamilla R. Factors associated with breastfeeding duration among Connecticut Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) participants. Journal of Human Lactation. 2010;26(3):266–273. doi: 10.1177/0890334410365067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HealthDay News. CDC: Hospitals doing better job of promoting breastfeeding. 2015 Retrieved from MPR website: http://www.empr.com/medical-news/cdc-hospitals-doing-better-job-of-promoting-breastfeeding/article/443781/
- Hedberg IC. Barriers to breastfeeding in the WIC population. The American Journal of Maternal/Child Nursing. 2013;38(4):244–249. doi: 10.1097/NMC.0b013e3182836ca2. [DOI] [PubMed] [Google Scholar]
- Hildebrand DA, McCarthy P, Tipton D, Merriman C, Schrank M, Newport M. Innovative use of influential prenatal counseling may improve breastfeeding initiation rates among WIC participants. Journal of Nutrition Education and Behavior. 2014;46(6):458–466. doi: 10.1016/j.jneb.2014.05.005. [DOI] [PubMed] [Google Scholar]
- Houghtaling B, Byker Shanks C, Ahmed S, Rink E. Grandmother and health care professional perspectives on breastfeeding provide opportunities for health promotion in a tribal community. Social Science & Medicine. doi: 10.1016/j.socscimed.2018.05.017. in prepration. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hurley KM, Black MM, Papas MA, Quigg AM. Variation in breastfeeding behaviours, perceptions, and experiences by race/ethnicity among a low-income statewide sample of Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) participants in the United States. Maternal & Child Nutrition. 2008;4(2):95–105. doi: 10.1111/j.1740-8709.2007.00105.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine. WIC food packages: Time for a change. Washington, DC: National Academies Press; 2006. [Google Scholar]
- Jacknowitz A, Novillo D, Tiehen L. Special Supplemental Nutrition Program for Women, Infants, and Children and infant feeding practices. Pediatrics. 2007;119(2):281–289. doi: 10.1542/peds.2006-1486. [DOI] [PubMed] [Google Scholar]
- Jacobson LT, Twumasi-Ankrah P, Redmond ML, Ablah E, Hines RB, Johnston J, Collins TC. Characteristics associated with breastfeeding behaviors among urban versus rural women enrolled in the Kansas WIC program. Maternal and Child Health Journal. 2015;19(4):828–839. doi: 10.1007/s10995-014-1580-2. [DOI] [PubMed] [Google Scholar]
- Jensen E. Participation in the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) and breastfeeding: National, regional, and state level analyses. Maternal and Child Health Journal. 2012;16(3):624–631. doi: 10.1007/s10995-011-0796-7. [DOI] [PubMed] [Google Scholar]
- Johnson B, Thorn B, McGill B, Suchman A, Mendelson M, Patlan KL, Connor P. WIC participant and program characteristics 2012. Alexandria, VA: U.S. Department of Agriculture, Food and Nutrition Service; 2013. (Prepared by Insight Policy Research under Contract No. AG-3198-C-11-0010). [Google Scholar]
- Joyce T, Racine A, Yunzal-Butler C. Reassessing the WIC effect: Evidence from the pregnancy nutrition surveillance system. Journal of Policy Analysis and Management. 2008;27(2):277–303. doi: 10.1002/pam.20325. [DOI] [PubMed] [Google Scholar]
- Julian PTH, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Sterne JAC. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ: British Medical Journal. 2011;343(7829):889–893. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langellier BA, Chaparro MP, Wang MC, Koleilat M, Whaley SE. The new food package and breastfeeding outcomes among women, infants, and children participants in Los Angeles County. American Journal of Public Health. 2014;104(2):S112–S118. doi: 10.2105/AJPH.2013.301330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langellier BA, Chaparro MP, Whaley SE. Social and institutional factors that affect breastfeeding duration among WIC participants in Los Angeles County, California. Maternal and Child Health Journal. 2012;16(9):1887–1895. doi: 10.1007/s10995-011-0937-z. [DOI] [PubMed] [Google Scholar]
- Lawrence S, Chau M, Lennon MC. Depression, substance abuse, and domestic violence: Little is known about co-occurrence and combined effects on low-income families. 2004 Retrieved from National Center for Children in Poverty website: http://nccp.org/publications/pub_546.html.
- Lovera D. Evaluation of a breastfeeding peer support program for fathers of Hispanic participants in a Texas Special Supplemental Nutrition Program for Women, Infants, and Children. Journal of the American Dietetic Association. 2010;110(11):1696–1702. doi: 10.1016/j.jada.2010.08.001. [DOI] [PubMed] [Google Scholar]
- Ma P, Magnus JH. Exploring the concept of positive deviance related to breastfeeding initiation in black and white WIC enrolled first time mothers. Maternal and Child Health Journal. 2012;16(8):1583–1593. doi: 10.1007/s10995-011-0852-3. [DOI] [PubMed] [Google Scholar]
- McKechnie AC, Tluczek A, Henriques JB. Maternal variables influencing duration of breastfeeding among low-income mothers. ICAN: Infant, Child, & Adolescent Nutrition. 2009;1(3):126–132. doi: 10.1177/1941406409334379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meehan K, Harrison GG, Afifi AA, Nickel N, Jenks E, Ramirez A. The association between an electric pump loan program and the timing of requests for formula by working mothers in WIC. Journal of Human Lactation. 2008;24(2):150–158. doi: 10.1177/0890334408316081. [DOI] [PubMed] [Google Scholar]
- Metallinos-Katsaras E, Brown L, Colchamiro R. Maternal WIC participation improves breastfeeding rates: A statewide analysis of WIC participants. Maternal and Child Health Journal. 2015;19(1):136–143. doi: 10.1007/s10995-014-1504-1. [DOI] [PubMed] [Google Scholar]
- Mickens AD, Modeste N, Montgomery S, Taylor M. Peer support and breastfeeding intentions among black WIC participants. Journal of Human Lactation. 2009;25(2):157–162. doi: 10.1177/0890334409332438. [DOI] [PubMed] [Google Scholar]
- Mistry Y. P21: Infant feeding practices of Vietnamese American women. Journal of Nutrition Education and Behavior. 2007;39(4):S84. doi: 10.1016/j.jneb.2007.04.216. [DOI] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Annals of Internal Medicine. 2009;151(4):264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- Murimi M. Factors that influence breastfeeding decisions among Special Supplemental Nutrition Program for Women, Infants, and Children participants from Central Louisiana. Journal of the American Dietetic Association. 2010;110(4):624–627. doi: 10.1016/j.jada.2009.12.019. [DOI] [PubMed] [Google Scholar]
- National WIC Association. The role of WIC in public health. 2013 Retrieved from https://www.nwica.org/position-papers.
- Oliveira VJ. The WIC program: Background, trends, and issues. Washington, DC: Government Printing Office; 2002. (Food Assistance and Nutrition Research Report No. 27). [Google Scholar]
- Olson BH, Haider SJ, Vangjel L, Bolton TA, Gold JG. A quasi-experimental evaluation of a breastfeeding support program for low income women in Michigan. Maternal and Child Health Journal. 2010;14(1):86–93. doi: 10.1007/s10995-008-0430-5. [DOI] [PubMed] [Google Scholar]
- Ponza M, Devaney B, Ziegler P, Reidy K, Squatrito C. Nutrient intakes and food choices of infants and toddlers participating in WIC. Journal of the American Dietetic Association. 2004;104(1):71–79. doi: 10.1016/j.jada.2003.10.018. [DOI] [PubMed] [Google Scholar]
- Reeder JA, Joyce T, Sibley K, Arnold D, Altindag O. Telephone peer counseling of breastfeeding among WIC participants: A randomized controlled trial. Pediatrics. 2014;134(3):E700–E709. doi: 10.1542/peds.2013-4146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rivera Alvarado I, Vázquez García V, Dávila Torres RR, Parrilla Rodríguez AM. Exploratory study: Breastfeeding knowledge, attitudes towards sexuality and breastfeeding, and disposition towards supporting breastfeeding in future Puerto Rican male parents. Puerto Rico Health Sciences Journal. 2006;25(4):337. [PubMed] [Google Scholar]
- Ryan AS, Zhou W. Lower breastfeeding rates persist among the Special Supplemental Nutrition Program for Women, Infants, and Children participants, 1978–2003. Pediatrics. 2006;117(4):1136–1146. doi: 10.1542/peds.2005-1555. [DOI] [PubMed] [Google Scholar]
- Sayegh MA, Erickson T, Fortenberry FD, Castrucci B. The case study of a breastfeeding outreach campaign on rural young adult adolescent African American women. Journal of Adolescent Health. 2007;40(2):S28–S29. [Google Scholar]
- Schultz DJ, Byker Shanks C, Houghtaling B. The impact of the 2009 Special Supplemental Nutrition Program for Women, Infants, and Children food package revisions on participants: A systematic review. Journal of the Academy of Nutrition and Dietetics. 2015;115(11):1832–1846. doi: 10.1016/j.jand.2015.06.381. [DOI] [PubMed] [Google Scholar]
- Stremler J, Lovera D. Insight from a breastfeeding peer support pilot program for husbands and fathers of Texas WIC participants. Journal of Human Lactation. 2004;20(4):417–422. doi: 10.1177/0890334404267182. [DOI] [PubMed] [Google Scholar]
- Tender JAF, Janakiram J, Arce E, Mason R, Jordan T, Marsh J, Moon RY. Reasons for in-hospital formula supplementation of breastfed infants from low-income families. Journal of Human Lactation. 2009;25(1):11–17. doi: 10.1177/0890334408325821. [DOI] [PubMed] [Google Scholar]
- Tenfelde S, Finnegan L, Hill PD. Predictors of breastfeeding exclusivity in a WIC sample. Journal of Obstetric, Gynecologic & Neonatal Nursing. 2011;40(2):179–189. doi: 10.1111/j.1552-6909.2011.01224.x. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Agriculture. WIC nutrition services standards. Washington, DC: Government Printing Office; 2001. [Google Scholar]
- U.S. Department of Agriculture. Effects of the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC): A review of recent research. Washington, DC: Government Printing Office; 2012. [Google Scholar]
- U.S. Department of Agriculture. Special Supplemental Nutrition Program for Women, Infants and Children (WIC) revisions in the WIC food packages; final rule. Washington, DC: Government Printing Office; 2014. [Google Scholar]
- U.S. Department of Agriculture. About WIC breastfeeding peer counseling. 2016 Retrieved from https://lovingsupport.fns.usda.gov/content/about-wic-breastfeeding-peer-counseling.
- U.S. Department of Health and Human Services. The surgeon general’s call to action to support breastfeeding. Washington, DC: U.S. Department of Health and Human Services, Office of the Surgeon General; 2011. [Google Scholar]
- Vaaler ML, Stagg J, Parks SE, Erickson T, Castrucci BC. Breast-feeding attitudes and behavior among WIC mothers in Texas. Journal of Nutrition Education and Behavior. 2010;42(3):S30–S38. doi: 10.1016/j.jneb.2010.02.001. [DOI] [PubMed] [Google Scholar]
- Victora CG, Horta BL, de Mola CL, Quevedo L, Pinheiro RT, Gigante DP, Barros FC. Association between breastfeeding and intelligence, educational attainment, and income at 30 years of age: A prospective birth cohort study from Brazil. Lancet Global Health. 2015;3(4):E199–E205. doi: 10.1016/S2214-109X(15)70002-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wansink B. Environmental factors that increase the food intake and consumption volume of unknowing consumers. Annual Review of Nutrition. 2004;24(1):455–479. doi: 10.1146/annurev.nutr.24.012003.132140. [DOI] [PubMed] [Google Scholar]
- Wansink B, Just DR, Payne CR, Klinger MZ. Attractive names sustain increased vegetable intake in schools. Preventive Medicine. 2012;55(4):330–332. doi: 10.1016/j.ypmed.2012.07.012. [DOI] [PubMed] [Google Scholar]
- Wansink B, Just D, Smith L. Move the fruit: Putting fruit in new bowls and new places doubles lunchroom sales. Journal of Nutrition Education and Behavior. 2011;43(4):S1. doi: 10.1016/j.jneb.2011.03.013. [DOI] [Google Scholar]
- Whaley SE, Koleilat M, Whaley M, Gomez J, Meehan K, Saluja K. Impact of policy changes on infant feeding decisions among low-income women participating in the Special Supplemental Nutrition Program for Women, Infants, and Children. American Journal of Public Health. 2012;102(12):2269–2273. doi: 10.2105/AJPH.2012.300770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilde P, Wolf A, Fernandes M, Collins A. Food-package assignments and breastfeeding initiation before and after a change in the Special Supplemental Nutrition Program for Women, Infants, and Children. American Journal of Clinical Nutrition. 2012;96(3):560–566. doi: 10.3945/ajcn.112.037622. [DOI] [PubMed] [Google Scholar]
- Yun S, Liu Q, Mertzlufft K, Kruse C, White M, Fuller P, Zhu BP. Evaluation of the Missouri WIC (Special Supplemental Nutrition Program for Women, Infants, and Children) breast-feeding peer counselling programme. Public Health Nutrition. 2010;13(2):229–237. doi: 10.1017/S1368980009990668. [DOI] [PubMed] [Google Scholar]
- Ziol-Guest KM. First- and second-trimester WIC participation is associated with lower rates of breastfeeding and early introduction of cow’s milk during infancy. Journal of the American Dietetic Association. 2010;110(5):702–709. doi: 10.1016/j.jada.2010.02.013. [DOI] [PubMed] [Google Scholar]


