Abstract
Background: The reduction of sugar-sweetened beverage (SSB) intake may be beneficial for weight management and other related health conditions; however, to our knowledge, no data exist regarding the spontaneous changes in other dietary components or the overall dietary quality after an SSB-reduction intervention.
Objectives: We explored longitudinal changes within and between an SSB-reduction intervention (SIPsmartER) and a physical activity intervention (MoveMore) with respect to spontaneous changes in 1) energy intake and macronutrients and micronutrients, 2) dietary quality [Healthy Eating Index–2010 (HEI)], and 3) beverage categories.
Design: Participants were enrolled in a 6-mo, community-based behavioral trial and randomly assigned into either the SIPsmartER (n = 149) intervention group or the MoveMore (n = 143) matched-contact comparison group. Dietary intake was assessed through a mean of three 24-h dietary recalls at baseline and 6 mo. Dietary recalls were analyzed with the use of nutritional analysis software. A multilevel, mixed-effects linear regression with intention-to-treat analyses is presented.
Results: SIPsmartER participants showed a significant reduction in total SSBs (mean decrease: −366 mL; P ≤ 0.001). Several spontaneous changes occurred within the SIPsmartER group and, compared with the MoveMore group, included significant HEI improvements for empty calorie, total vegetable, and total HEI scores (mean increases: 2.6, 0.3, and 2.6, respectively; all P ≤ 0.01). Additional positive changes were shown, including significant decreases in total energy intake, trans fat, added sugars, and total beverage energy (all P ≤ 0.05). Few dietary changes were noted in the MoveMore group over the 6-mo intervention.
Conclusions: Intervention of the single dietary component SSB resulted in additional spontaneous and beneficial dietary changes. Interventions that target a single dietary change, such as limiting SSB intake to <240 mL/d (<8 fl oz/d), may improve the overall dietary quality health and provide motivation to make additional dietary changes. This trial was registered at clinicaltrials.gov as NCT02193009.
Keywords: added sugar, beverages, dietary quality, sugar-sweetened beverages, dietary intervention
INTRODUCTION
Added-sugar (AS)6 consumption is a key dietary intervention target because evidence has shown that excessive intake is a contributor to obesity (1, 2) and related comorbidities such as type 2 diabetes (3, 4) and cardiovascular disease (2). Because ∼50% of AS consumption is from sugar-sweetened beverages (SSBs) (5), reducing SSB intake is a common objective of AS-reduction interventions (6, 7) and public health policies (8–10). Recently, the US Dietary Guidelines recommended that ≤10% of energy should come from AS and that SSBs should be replaced with water (11).
The reduction of SSB intake may be beneficial for weight management (12, 13) and other related health conditions (14). However, to our knowledge, no data exist that have examined concurrent changes in other dietary components or in the overall dietary quality that results from an intervention that has targeted an SSB reduction. Furthermore, the US Dietary Guidelines has recognized dietary pattern research as a substantial research gap (15) because foods are not consumed in isolation but, rather, in combination with other dietary components (16). With multiple AS recommendations and public policies (e.g., SSB taxation) being implemented (11, 17, 18), a key opportunity is to determine what compensatory dietary changes are occurring when SSB and AS intakes are reduced. The few studies that have examined longitudinal changes in dietary patterns have not specifically explored changes in dietary components or quality when SSB consumption has been reduced (19). Because SSB intake provides a lower satiety value than solid AS intake does, as a result of its liquid form, changes in SSB consumption may play a more substantial role in altering dietary intake and consequently increasing energy intake compared with changes in solid AS intake (20–23).
Alternatively, there has been some evidence to suggest that changes in health behaviors may cluster (24) and that some behaviors may act as a potential gateway to changes in other related health behaviors. For example, in a trial with exercise as the primary behavioral target for weight loss, changes in self-regulation for exercise were related to concurrent changes in self-regulation for dietary intake (25). Other studies have examined the potential of a single health-behavior intervention, primarily exercise, as a gateway for other positive health behavior changes with mixed results (26, 27). There has been some evidence that certain dietary behaviors have the potential to act as a gateway to other dietary behavior changes (24), and research has indicated an association between healthier beverage patterns and healthier dietary patterns (19, 28). However, the existing literature has primarily been cross-sectional with limited investigations of potential behavioral spillover effects within the broad range of dietary behaviors.
These secondary data were from the Talking Health study, which was a randomized controlled trial that targeted adults with low socioeconomic status (7). Participants were randomly assigned to the SIPsmartER intervention (SSB reduction) or to the MoveMore comparison group (physical activity). This analysis extends previously reported dietary changes from the Talking Health trial including an established significant reduction of SSBs and AS in SIPsmartER participants compared with MoveMore participants (29, 30).
The purpose of this analysis was to evaluate longitudinal changes within and between SIPsmartER and MoveMore intervention groups with respect to compensatory changes in 1) energy intake and macronutrients and micronutrients, 2) dietary quality [Healthy Eating Index-2010 (HEI)], and 3) beverage categories. Relative to the MoveMore group, it was hypothesized that the SIPsmartER group would show significant improvements in the overall dietary quality (HEI total and individual component scores, specifically the empty calorie component) and beverage profiles. This trial was registered at clinicaltrials.gov as NCT02193009.
METHODS
Study design and subjects
Guided by concepts in health literacy and the theory of planned behavior (31), the Talking Health study (7) was a 6-mo, community-based, 2-arm, randomized controlled behavioral trial that targeted SSB or physical activity behaviors through 3 small-group educational classes, one live teach-back call, and 11 interactive voice-response telephone calls. Detailed trial information has been presented elsewhere (7, 30). The SIPsmartER group’s primary intervention goal was to reach the recommendation of <240 mL SSBs/d (<8 fl oz SSBs/d) (18, 32), and the MoveMore group’s primary intervention goal was to reach 150 min of moderate-intensity aerobic activity and muscle-strengthening activities on ≥2 d/wk (30).
Participants were recruited from medically-underserved rural regions (Medical Underservice Index score ≤62) (33) in Southwest Virginia for the Talking Health trial (7). Recruitment details have been published elsewhere (7); briefly, participants were recruited from April 2012 to June 2014 through various active recruitment methods (daycare centers, festivals, health and free clinics, health departments, and local extension agents) and passive recruitment methods (targeted mailings, flyers, radio announcements, and newspaper advertisement). Information regarding eligibility and enrollment has been presented elsewhere (7). Briefly, 1056 individuals were screened, 620 of whom were eligible, and 301 subjects were enrolled. To be eligible, participants had to consume ≥200 kcal SSBs/d as assessed with the use of the validated BEVQ-15 (a beverage intake questionnaire) (34–37) before enrollment. In addition, participants had to be English-speaking adults ≥18 y old, have reported no physical activity limitations, and could not be currently enrolled in any other nutrition or physical activity programs. Although pregnancy status was not an exclusion criterion, women who were pregnant at baseline or became pregnant during the 6-mo intervention were excluded from the analysis (n = 5). Participants were randomly assigned to either the SSB intervention group (SIPsmartER: n = 151) or the physical activity group (MoveMore: n = 145) after completing the baseline assessment.
Previous findings
To provide context to the reported changes in dietary intake, several previously published variables are presented here, which include changes in weight status (30), physical activity (30), and δ13C values (29). Within the SIPsmartER group, a significant mean decrease in BMI (in kg/m2) of 0.21 (95% CI: −0.35, −0.06; P ≤ 0.01) was shown relative to a nonsignificant mean increase in BMI of 0.10 (95% CI: −0.23, 0.43; P > 0.05) in the MoveMore group. A significant group-by-time mean difference in BMI of −0.31 (95% CI: −0.55, −0.07; P ≤ 0.05) (30) was also shown. Within the MoveMore group, and compared with the SIPsmartER group, a significant increase in the mean time spent doing moderate-to-vigorous physical activity (15 min; 95% CI: 6, 24 min; P ≤ 0.01) and strength-training physical activity (17 min; 95% CI: 7, 28; P ≤ 0.01) was shown. A significant group-by-time mean difference of 20 min (95% CI: −32, −7 min; P ≤ 0.01) for strength training was noted but not for moderate-to-vigorous physical activity (30). A significant group-by-time mean difference of −0.07‰ in δ13C values was revealed, with the SIPsmartER group δ13C values decreasing by 0.05‰ (95% CI: −0.10‰, 0.01‰; P > 0.05) compared with an increase of 0.02‰ (95% CI: −0.04‰, 0.08‰; P > 0.05) in MoveMore δ13C values (29).
Methods
Participants underwent baseline and 6-mo follow-up assessments of height, which was measured in meters without shoes with the use of a portable stadiometer, and of weight, which was measured in light clothing without shoes to the nearest 0.1 kg with the use of a digital scale (model 310GS; Tanita), and BMI was calculated. The time spent being physically active was collected at baseline and at 6-mo assessments via the Godin Leisure Time Exercise Questionnaire, which measures moderate-to-vigorous and strength-training physical activity over the past 7 d (38).
Participants provided demographic information, and usual dietary intake was collected with the use of three 24-h dietary intake recalls (39, 40). The first 24-h dietary recall was completed in person, and the 2 remaining dietary recalls were completed unannounced via the telephone. Recalls were collected by trained research technicians who were supervised by doctoral-level registered dietitians. One weekend and 2 weekdays were recalled to provide a more-accurate representation of habitual dietary habits. Dietary intake recalls were analyzed with the use of the Nutrition Data System for Research (NDS-R) nutritional analysis software (2011; Nutrition Coordinating Center, University of Minnesota), and the daily mean of completed dietary recalls was used for the analysis. Beverage intake data were extracted from the NDS-R food-group output files. SSBs were defined as calorically sweetened beverages that included regular soft drinks, sweetened fruit drinks, sweetened tea or coffee, and energy or sports drinks (18). HEI scores were calculated with the use of dietary intake recall data. HEI total and subcomponent scores were derived from the NDS-R output on the basis of guidelines that were developed by the NDS-R, and scores were calculated according to a standardized published protocol, which included adjustment for energy intake (15, 41). Possible HEI scores ranged from 0 to 100 (the HEI total score was the sum of all 12 component scores) (41) with higher scores indicating greater adherence to the 2010 Dietary Guidelines for Americans (42). Furthermore, the following beverages were collapsed and analyzed via beverage amounts established by the Beverage Guidance Panel (32): 1) water, 2) unsweetened tea and coffee, 3) low-fat and skim milk, 4) noncalorically sweetened beverages, 5) caloric beverages with some nutrients (including 100% fruit juice, alcohol, and whole milk), and 6) calorically sweetened beverages.
Fingerstick blood samples were collected at baseline and at 6 mo and measured for δ13C values, which are an objective dietary biomarker of SSB consumption. Relative to other dietary items, corn- and cane-sugar plants have a high concentration of 13C compared with 15C; thus, the consumption of these sweeteners is reflected in human tissue samples (29). The time period reflected by δ13C values is relative to the respective turnover time of various tissue samples (43). The fasting whole blood samples were analyzed with the use of natural-abundance stable-isotope mass spectrometry as described elsewhere (29).
Ethics
This study was conducted according to the guidelines of the Declaration of Helsinki of 1975 as revised in 1983, and the Virginia Tech Institutional Review Board approved the study protocol. Participants provided written informed consent before enrollment.
Statistics
For demographic characteristics, descriptive statistics (means ± SDs and frequencies), ANOVA (F) tests (for comparisons of means across conditions), and chi-square tests (for comparisons of proportions across conditions) were performed with the use of SPSS statistical software (version 23, 2015; IBM). Multilevel, mixed-effects, linear regression analyses were performed with the use of Stata software (version 13, 2013; StataCorp LP) to account for the clustering of individuals within cohorts. In addition, time and program indicators and their interactions were included in the models to account for within-individual and between-program variations. Results of the intention-to-treat (baseline-value-carried-forward) analyses are presented (44, 45). Individual baseline characteristics were controlled in accordance with the primary outcome article’s methods (30) including age, sex, race-ethnicity, BMI, income, educational level, health-literacy level, employment status, number of children, and smoking status. Forty-one participants in the SIPsmartER group and 38 participants in the MoveMore group did not return for the 6-mo data collection. In addition, participants with artificial sweetener consumption >3 SDs from the mean were excluded from the analysis (n = 4) because of the suspected substantial misreporting of dietary intake. The final analytic sample included 292 subjects (SIPsmartER: n = 149; MoveMore: n = 143). The significance level was set a priori at P ≤ 0.05.
RESULTS
Included participants (n = 292) were primarily women and Caucasian with a mean age of 42 ± 13 y (range: 18–81 y) (Table 1). The majority of participants were overweight or obese (79%) with a mean BMI of 33 ± 9 (range: 16–72). There were no significant differences in baseline demographic characteristics between the SIPsmartER group (n = 149) and the MoveMore group (n = 143) (P > 0.05). The overall completion rate for dietary recalls at baseline was 89% (75% of subjects had 3 complete days, 16% of subjects had 2 complete days, and 9% of subjects had only 1 complete day). The 6-mo follow-up overall-completion rate for the dietary recalls was 75% (49% of subjects had 3 complete days, 27% of subjects had 2 complete days, and 24% of subjects had only 1 complete day).
TABLE 1.
Baseline sample characteristics by randomly assigned condition
| Characteristic | Total sample (n = 292) | SIPsmartER (n = 149) | MoveMore (n = 143) |
| Age, y | 42.0 ± 13.41 | 41.8 ± 13.4 | 42.3 ± 13.4 |
| Sex, n (%) | |||
| M | 55 (19) | 30 (20) | 25 (17.5) |
| F | 237 (81) | 119 (80) | 118 (82.5) |
| Race, n (%) | |||
| Caucasian | 271 (93) | 135 (90.5) | 136 (95) |
| African American | 13 (4.5) | 10 (7) | 3 (2) |
| Other | 8 (2.5) | 4 (2.5) | 4 (3) |
| Ethnicity, n (%) | |||
| Hispanic or Latino | 3 (1) | 2 (1) | 1 (0.5) |
| Educational level, n (%) | |||
| High school graduate or less | 90 (31) | 48 (32) | 42 (29.5) |
| Some college or greater | 202 (69) | 101 (68) | 101 (70.5) |
| Anthropometric measures | |||
| Weight, kg | 90.6 ± 25.4 | 90.5 ± 26.4 | 90.6 ± 24.4 |
| BMI, kg/m2 | 33.0 ± 9.1 | 33.2 ± 9.3 | 32.8 ± 9.0 |
| Categories (in kg/m2), n (%) | |||
| Underweight (≤18.4) | 5 (1.5) | 3 (2) | 2 (1.5) |
| Normal weight (18.5–24.9) | 58 (20) | 28 (19) | 30 (21) |
| Overweight (25–29.9) | 63 (21.5) | 34 (23) | 29 (20.5) |
| Obese (≥30) | 166 (57) | 86 (56) | 82 (57) |
| Physical activity, min | |||
| Moderate to vigorous | 40 ± 50 | 40 ± 50) | 39 ± 51 |
| Strength training | 10 ± 47 | 13 ± 60 | 7 ± 28 |
| δ13C, ‰ | −18.93 ± 0.68 | −18.92 ± 0.65 | −18.94 ± 0.72 |
Mean ± SD (all such values).
Changes in HEI scores
The empty calorie HEI component and the total HEI score significantly improved in the SIPsmartER group and showed significant group-by-time differences. The total vegetable HEI-component score significantly increased in the SIPsmartER group, and a significant group-by-time difference between SIPsmartER and MoveMore groups was shown (Table 2).
TABLE 2.
Changes in HEI scores from baseline to 6 mo by treatment group with the use of an intention-to-treat analysis1
| HEI variable (possible score) and group | Baseline | 6 mo | Adjusted change from baseline to 6 mo2 | P-group by time |
| Total fruit (0–5) | NS | |||
| SIPsmartER | 1.0 ± 1.43 | 1.1 ± 1.6 | 0.1 (−0.2, 0.4) | |
| MoveMore | 1.5 ± 1.7 | 1.4 ± 1.7 | −0.1 (−0.4, 0.2) | |
| Whole fruit (0–5) | NS | |||
| SIPsmartER | 1.1 ± 1.7 | 1.2 ± 1.8 | 0.1 (−0.3, 0.4) | |
| MoveMore | 1.5 ± 2.0 | 1.4 ± 1.9 | −0.1 (−0.4, 0.3) | |
| Total vegetables (0–5) | ≤0.001 | |||
| SIPsmartER | 2.5 ± 1.5 | 2.8 ± 1.6 | 0.3 (0.1, 0.5)** | |
| MoveMore | 2.8 ± 1.5 | 2.7 ± 1.4 | −0.1 (−0.2, 0.1) | |
| Greens and beans (0–5) | NS | |||
| SIPsmartER | 1.1 ± 1.8 | 1.2 ± 1.9 | 0.1 (−0.3, 0.4) | |
| MoveMore | 1.2 ± 1.7 | 1.2 ± 1.9 | 0.01 (−0.2, 0.2) | |
| Whole grains (0–10) | ≤0.05 | |||
| SIPsmartER | 2.3 ± 3.3 | 2.6 ± 3.6 | 0.3 (−0.4, 1.0) | |
| MoveMore | 2.7 ± 3.2 | 2.3 ± 3.3 | −0.4 (−1.2, 0.4) | |
| Dairy (0–10) | NS | |||
| SIPsmartER | 4.5 ± 2.9 | 4.9 ± 3.3 | 0.4 (−0.2, 1.1) | |
| MoveMore | 4.8 ± 2.9 | 4.6 ± 2.9 | −0.2 (−0.3, −0.01) | |
| Total protein foods (0–5) | NS | |||
| SIPsmartER | 4.2 ± 1.2 | 4.3 ± 1.3 | 0.2 (−0.02, 0.3) | |
| MoveMore | 4.4 ± 1.1 | 4.5 ± 1.1 | 0.1 (−0.1, 0.2) | |
| Seafood and plant proteins (0–5) | NS | |||
| SIPsmartER | 1.7 ± 2.0 | 1.4 ± 2.0 | −0.2 (−0.4, −0.1) | |
| MoveMore | 1.8 ± 2.1 | 1.6 ± 2.1 | −0.2 (−0.5, 0.1) | |
| Fatty acids (0–5) | NS | |||
| SIPsmartER | 4.3 ± 3.1 | 4.0 ± 3.1 | −0.3 (−0.9, 0.4) | |
| MoveMore | 3.9 ± 3.5 | 4.1 ± 3.2 | 0.1 (−0.1, 0.3) | |
| Refined grains (0–10) | NS | |||
| SIPsmartER | 5.9 ± 3.2 | 5.9 ± 3.5 | 0.04 (−0.6, 0.7) | |
| MoveMore | 6.6 ± 3.1 | 6.2 ± 3.4 | −0.4 (−1.0, 0.2) | |
| Sodium (0–10) | NS | |||
| SIPsmartER | 3.9 ± 3.1 | 3.3 ± 3.3 | −0.6 (−1.3, 0.1) | |
| MoveMore | 4.1 ± 3.1 | 3.9 ± 3.3 | −0.1 (−0.6, 0.3) | |
| Empty calories (0–20) | ≤0.001 | |||
| SIPsmartER | 10.0 ± 5.4 | 12.5 ± 5.8 | 2.6 (1.7, 3.5)*** | |
| MoveMore | 10.2 ± 5.9 | 10.8 ± 5.9 | 0.6 (−0.2, 1.3) | |
| Total HEI score (0–100) | ≤0.01 | |||
| SIPsmartER | 42.3 ± 12.4 | 45.0 ± 13.4 | 2.6 (0.9, 4.3)** | |
| MoveMore | 45.4 ± 12.8 | 44.3 ± 13.7 | −1.1 (−2.6, 0.3) |
Analysis was conducted with the use of an ANOVA with intention to treat, which used the baseline-observation-carried-forward imputation procedure. n = 292 (SIPsmartER condition: n = 149; MoveMore condition: n = 143). P values denote the significance between SIPsmartER and MoveMore conditions. HEI, Healthy Eating Index–2010.
All values are means (95% CIs). Values were adjusted for covariates. The model was controlled for baseline covariates including age, sex, race/ethnicity, BMI, income, educational level, health-literacy level, employment status, number of children, and smoking status. **,***Within-group significance: **P ≤ 0.01, ***P ≤ 0.001.
Mean ± SD (all such values). Values were not adjusted for covariates.
Changes in energy and specific macronutrient and micronutrient intakes
Within the SIPsmartER group, and compared with the MoveMore group, significant group-by-time improvements were noted for total energy intake, grams of AS, percentage of kilocalories from AS, and grams of trans fat (Table 3).
TABLE 3.
Changes in energy intake and macronutrient and micronutrient consumption from baseline to 6 mo by treatment group with the use of an intention-to-treat analysis1
| Dietary variable and group | Baseline | 6 mo | Adjusted change from baseline to 6 mo2 | P-group by time |
| Total energy intake, kcal | ≤0.05 | |||
| SIPsmartER | 1975 ± 11003 | 1690 ± 1099 | −285 (−434, −136)*** | |
| MoveMore | 1766 ± 640 | 1723 ± 682 | −44 (−136, 49) | |
| Energy density, kcal/g | NS | |||
| SIPsmartER | 0.8 ± 0.3 | 0.7 ± 0.3 | −0.1 (−0.1, 0.01) | |
| MoveMore | 0.7 ± 0.3 | 0.7 ± 0.3 | −0.02 (−0.07, 0.03) | |
| Carbohydrates, % of kcal | NS | |||
| SIPsmartER | 51.0 ± 10.4 | 47.6 ± 11.3 | −3 (−5, −0.4) | |
| MoveMore | 50.4 ± 9.0 | 48.9 ± 9.9 | −1.5 (−2.5, −0.4) | |
| Added sugar, g | ≤0.001 | |||
| SIPsmartER | 108.0 ± 92.4 | 72.8 ± 88.5 | −35.1 (−47.3, −23.0)*** | |
| MoveMore | 93.0 ± 64.1 | 86.8 ± 68.4 | −6.2 (−14.6, 2.3) | |
| Added sugar, % of kcal | ≤0.001 | |||
| SIPsmartER | 21.6 ± 12.5 | 16.4 ± 12.5 | −5.2 (−7.3, −3.1)*** | |
| MoveMore | 20.7 ± 11.1 | 19.7 ± 11.6 | −1.0 (−2.5, 0.4) | |
| Protein, % of kcal | NS | |||
| SIPsmartER | 14.6 ± 4.2 | 16.4 ± 5.0 | 1.8 (0.9, 2.8) | |
| MoveMore | 15.2 ± 4.3 | 15.9 ± 4.4 | 0.7 (−0.02, 1.4) | |
| Fat, % of kcal | NS | |||
| SIPsmartER | 33.6 ± 7.9 | 35.2 ± 9.4 | 1.6 (0.3, 2.9) | |
| MoveMore | 33.6 ± 6.7 | 34.6 ± 7.9 | 0.9 (−0.1, 1.9) | |
| Saturated fat, g | NS | |||
| SIPsmartER | 27.1 ± 25.5 | 24.1 ± 25.0 | −3.1 (−5.2, −0.9) | |
| MoveMore | 24.0 ± 12.3 | 23.8 ± 13.4 | −0.2 (−1.6, 1.2) | |
| Saturated fat, % of kcal | NS | |||
| SIPsmartER | 11.5 ± 3.4 | 12.1 ± 3.7 | 0.54 (−0.1, 1.2) | |
| MoveMore | 11.7 ± 3.1 | 11.8 ± 3.5 | 0.1 (−0.2, 0.4) | |
| trans Fat, g | ≤0.01 | |||
| SIPsmartER | 3.2 ± 2.7 | 2.8 ± 2.6 | −0.4 (−0.8, −0.1)* | |
| MoveMore | 3.0 ± 2.0 | 3.1 ± 2.2 | 0.1 (−0.3, 0.4) | |
| Alcohol, % of kcal | NS | |||
| SIPsmartER | 0.8 ± 3.4 | 0.8 ± 3.7 | −0.1 (−0.1, 0.03) | |
| MoveMore | 0.8 ± 3.7 | 0.7 ± 3.1 | −0.2 (−0.3, −0.04) | |
| Sodium, mg | NS | |||
| SIPsmartER | 3240 ± 1637 | 2933 ± 1607 | −306 (−582, −30) | |
| MoveMore | 2902 ± 1138 | 2897 ± 1238 | −5 (−219, 209) | |
| Artificial sweetener,4 mg | NS | |||
| SIPsmartER | 101.1 ± 315.2 | 152.2 ± 336.3 | 51.1 (−23.1, 125.4) | |
| MoveMore | 117.3 ± 334.3 | 89.6 ± 274.0 | −27.7 (−68.0, 12.7) |
Analysis was conducted with the use of an ANOVA with intention to treat, which used the baseline-observation-carried-forward imputation procedure. n = 292 (SIPsmartER condition: n = 149; MoveMore condition: n = 143). P values denote the significance between SIPsmartER and MoveMore conditions.
All values are means (95% CIs). Values were adjusted for covariates. The model was controlled for baseline covariates including age, sex, race/ethnicity, BMI, income, educational level, health-literacy level, employment status, number of children, and smoking status. *,***Within-group significance: *P ≤ 0.05, ***P ≤ 0.001.
Mean ± SD (all such values). Values were not adjusted for covariates.
Included saccharin, aspartame, sucralose, and acesulfame K.
Changes in beverage consumption
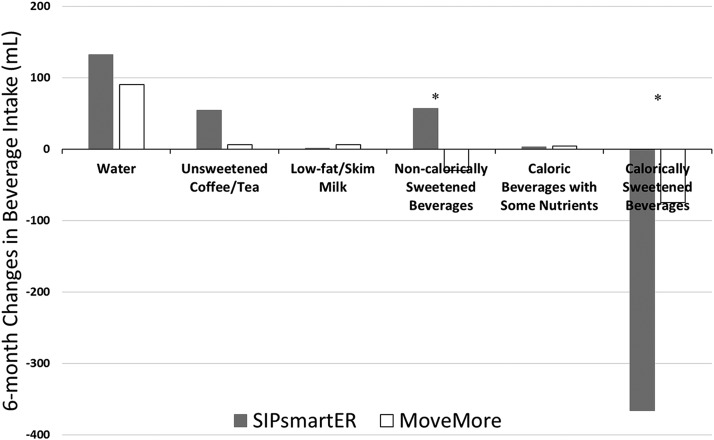
Within the SIPsmartER group, and compared with the MoveMore group, significant improvements in the reported consumption of regular soda, sweetened coffee, total SSBs (milliliters), and total beverage energy were shown. No additional changes in beverage intake were shown within the MoveMore group (Table 4). Similar results were shown when the beverage categories were collapsed into 6 beverage amounts that were established by the Beverage Guidance Panel (32). Figure 1 and Table 5 show intention-to-treat changes in beverage amounts over the 6-mo intervention for both SIPsmartER and MoveMore groups whereby significant group-by-time differences in intakes occurred for noncalorically sweetened beverages (87 mL; 95% CI: 3, 171 mL; P ≤ 0.05) and calorically sweetened beverages (291 mL 95% CI: −419, −165 mL; P ≤ 0.001).
TABLE 4.
Changes in beverage consumption from baseline to 6 mo by treatment group with the use of an intention-to-treat analysis1
| Beverage variable and group | Baseline | 6 mo | Adjusted change from baseline to 6 mo2 | P-group by time |
| Water, mL | NS | |||
| SIPsmartER | 666 ± 7413 | 798 ± 894 | 132 (−6, −180) | |
| MoveMore | 753 ± 789 | 846 ± 804 | 90 (−78, −2340) | |
| 100% fruit juice, mL | NS | |||
| SIPsmartER | 18 ± 54 | 24 ± 69 | 6 (−3, −90) | |
| MoveMore | 30 ± 72 | 42 ± 108 | 9 (−9, −270) | |
| Sweetened juice drink, mL | NS | |||
| SIPsmartER | 48 ± 123 | 33 ± 99 | −12 (−36, −1080) | |
| MoveMore | 36 ± 90 | 36 ± 135 | 0 (−27, −810) | |
| Whole milk, mL | NS | |||
| SIPsmartER | 15 ± 60 | 12 ± 57 | −3 (−15, −450) | |
| MoveMore | 15 ± 42 | 9 ± 48 | −3 (−12, −360) | |
| Reduced-fat milk, mL | NS | |||
| SIPsmartER | 27 ± 72 | 30 ± 87 | 3 (−15, −450) | |
| MoveMore | 39 ± 102 | 21 ± 72 | −18 (−36, −1080) | |
| Fat-free milk, mL | NS | |||
| SIPsmartER | 21 ± 72 | 21 ± 75 | 0 (−9, −270) | |
| MoveMore | 27 ± 102 | 33 ± 180 | 6 (−24, −720) | |
| Regular soft drinks, mL | ≤0.01 | |||
| SIPsmartER | 486 ± 870 | 321 ± 822 | −165 (−258, −7740)*** | |
| MoveMore | 315 ± 432 | 315 ± 441 | 0 (−57, −1710) | |
| Artificially sweetened beverages, mL | ≤0.05 | |||
| SIPsmartER | 114 ± 300 | 171 ± 372 | 57 (−9, −270) | |
| MoveMore | 123 ± 348 | 93 ± 288 | −30 (−66, −1980) | |
| Sweet tea, mL | NS | |||
| SIPsmartER | 141 ± 282 | 78 ± 201 | −63 (−99, −2970) | |
| MoveMore | 198 ± 399 | 159 ± 282 | −39 (−99, −2970) | |
| Sweetened coffee, mL | ≤0.05 | |||
| SIPsmartER | 249 ± 618 | 129 ± 261 | −120 (−213, −6390)** | |
| MoveMore | 147 ± 270 | 123 ± 255 | −27 (−81, −2430) | |
| Black tea or coffee, mL | NS | |||
| SIPsmartER | 105 ± 294 | 159 ± 309 | 54 (−21, −630) | |
| MoveMore | 135 ± 363 | 141 ± 306 | 6 (−39, −1170) | |
| Beer, mL | NS | |||
| SIPsmartER | 57 ± 375 | 63 ± 420 | 6 (−12, −360) | |
| MoveMore | 33 ± 180 | 30 ± 222 | −3 (−21, −630) | |
| Wine, mL | NS | |||
| SIPsmartER | 3 ± 18 | 0 ± 3 | −3 (−6, −180) | |
| MoveMore | 6 ± 42 | 6 ± 42 | 0 (−3, −90) | |
| Energy drinks, mL | NS | |||
| SIPsmartER | 42 ± 120 | 24 ± 96 | −18 (−42, −1260) | |
| MoveMore | 24 ± 102 | 30 ± 117 | 6 (−18, −540) | |
| Sugar-sweetened beverages,4 mL | ≤0.001 | |||
| SIPsmartER | 978 ± 981 | 612 ± 855 | −366 (−498, −14,940)*** | |
| MoveMore | 744 ± 609 | 669 ± 525 | −75 (−150, −4500)* | |
| Total beverages, mL | NS | |||
| SIPsmartER | 2010 ± 1143 | 1887 ± 1131 | −123 (−306, −9180) | |
| MoveMore | 1905 ± 927 | 1887 ± 909 | −18 (−234, −7020) | |
| Total beverages, kcal | ≤0.001 | |||
| SIPsmartER | 459 ± 435 | 325 ± 433 | −134 (−195, −73)*** | |
| MoveMore | 368 ± 243 | 336 ± 252 | −32 (−63, −0.7)* |
Analysis was conducted with the use of an ANOVA with intention to treat, which used the baseline-observation-carried-forward imputation procedure. n = 292 (SIPsmartER condition: n = 149; MoveMore condition: n = 143). P values denote the significance between SIPsmartER and MoveMore conditions.
All values are means; (95% CIs). Values were adjusted for covariates. The model was controlled for baseline covariates including age, sex, race/ethnicity, BMI, income, educational level, health-literacy level, employment status, number of children, and smoking status. *,**,***Within-group significance: **P ≤ 0.05, **P ≤ 0.01, ***P ≤ 0.001.
Mean ± SD (all such values). Values were not adjusted for covariates.
Total sugar-sweetened beverages included regular soda, sweetened juice drinks, sweetened tea and coffee, and energy and sports drinks.
FIGURE 1.
Changes in consumption of beverage categories from baseline to 6 mo between SIPsmartER (n = 149) and MoveMore (n = 143) participants. *Significant between SIPsmartER and MoveMore conditions, P ≤ 0.05 (ANOVA with intention to treat, which used the baseline-observation-carried-forward imputation procedure).
TABLE 5.
Changes in Beverage Guidance Panel recommendations from baseline to 6 mo by treatment group with the use of an intention-to-treat analysis1
| Beverage variable | Beverage Guidance Panel daily recommendation2 | Group | Baseline, mL | 6 mo, mL | Adjusted change from baseline to 6 mo,3 mL | P-group by time |
| Level 1: water | 600–1500 mL | SIPsmartER | 666 ± 7414 | 798 ± 894 | 132 (−6, −180) | NS |
| MoveMore | 753 ± 789 | 846 ± 804 | 90 (−78, −2340) | |||
| Level 2: unsweetened coffee or tea | 0–1200 mL | SIPsmartER | 105 ± 294 | 159 ± 309 | 54 (−21, −630) | NS |
| MoveMore | 135 ± 363 | 141 ± 306 | 6 (−39, −1170) | |||
| Level 3: low-fat and skim milk | 0–480 mL | SIPsmartER | 21 ± 72 | 21 ± 75 | 0 (−9, −270) | NS |
| MoveMore | 27 ± 102 | 33 ± 180 | 6 (−24, −720) | |||
| Level 4: noncalorically sweetened beverages | 0–960 mL | SIPsmartER | 114 ± 300 | 171 ± 372 | 57 (−9, −270) | ≤0.05 |
| MoveMore | 123 ± 348 | 93 ± 288 | −30 (−66, −1980) | |||
| Level 5: caloric beverages with some nutrients | Total, mL | SIPsmartER | 93 ± 380 | 96 ± 423 | 3 (−36, 31) | NS |
| 0–240 mL 100% juice | MoveMore | 83 ± 197 | 87 ± 249 | 4 (−33, 25) | ||
| 0–2 alcoholic drinks5 | ||||||
| 0 mL whole milk | ||||||
| Level 6: calorically sweetened beverages | 0–240 mL | SIPsmartER | 978 ± 981 | 612 ± 855 | −366 (−498, −14,940)*** | ≤0.001 |
| MoveMore | 744 ± 609 | 669 ± 525 | −75 (−150, −4500)* |
Analysis was conducted with the use of an ANOVA with intention to treat, which used the baseline-observation-carried-forward imputation procedure. n = 292 (SIPsmartER condition: n = 149; MoveMore condition: n = 143). P values denote the significance between SIPsmartER and MoveMore conditions.
Popkin et al. (32).
All values are means (95% CIs). Values were adjusted for covariates. The model was controlled for baseline covariates including age, sex, race/ethnicity, BMI, income, educational level, health-literacy level, employment status, number of children, and smoking status. *,***Within-group significance: *P ≤ 0.05, ***P ≤ 0.001.
Mean ± SD (all such values). Values were not adjusted for covariates.
Alcoholic drink intake was defined as 0–1 drinks/d for women and 0–2 drinks/d for men. One drink was equivalent to 360 mL beer, 150 mL wine, or 45 mL liquor.
DISCUSSION
Although previous cross-sectional studies have shown associations between healthier beverage patterns and healthier dietary patterns (19, 28), this is the first behavioral investigation, to our knowledge, to examine changes in dietary components concurrently with a targeted SSB reduction. These findings suggest that SSB reduction may be a promising gateway behavior when targeted with a multicomponent intervention for improvements in the overall dietary quality. These results are particularly relevant for communities who are experiencing health disparities and have limited access to medical resources, where messages that target overall and multiple dietary improvements are difficult because of socioeconomic status and environmental factors.
As hypothesized, compared with the MoveMore group, the SIPsmartER group experienced significant improvements in dietary components beyond a decrease in SSB consumption (including soda and sweetened coffee). Specifically, total energy, beverage energy, AS, and trans-fat consumption were all significantly lower at the 6-mo follow-up. The dietary changes that occurred with the SSB reduction were beneficial in that focusing the intervention on one dietary component (SSB) led to other beneficial dietary changes. These results are congruent with previous literature that has indicated that healthier beverage patterns are associated with healthier dietary patterns (19, 28); specifically, prudent-type dietary patterns have been shown to have negative associations with SSB intake in various US populations (46, 47) and with regular soda consumption in US and international populations (28, 48–51). Previous work has proposed that SSB and AS intakes may be accurate indicators of overall dietary health (52), thereby suggesting that changes in consumption may affect other dietary variables. However, all of these previous associations have been based on cross-sectional studies and have not provided a route for direct comparisons (19).
In addition, these results suggest that improvements in other dietary factors beyond decreased SSB intake may be occurring. Specifically, there was a decrease in total energy intake of 285 kcal from all food and beverages, which was >2-fold the decrease in total energy from beverages alone (134 kcals). However, the AS gram deficit that was accrued from decreasing SSB intake was comparable to the AS gram decrease that was shown by all food and beverages (34 compared with 35 g, respectively). Thus, the loss of AS intake from SSBs was not replaced by other less-healthy dietary items such as sugar-rich foods (53). A similar phenomenon was previously shown by Stookey et al. (54) in which the SSB calories that were lost were not replaced by spontaneous increases in other foods or beverages. However, because the main outcome of that trial was the comparison of weight loss via 4 popular diets, SSB and beverage intakes only represented a small portion of the intervention, which included many other potential confounding factors (54). In addition, although the percentage of kilocalories from AS decreased significantly in the SIPsmartER group, intake did not reach the recommended ≤10% of energy intake, and intake reported by the MoveMore group remained 2-times higher than recommended intake (11).
The current results showed multiple significant changes in the amounts of specific beverages consumed, and although there was also a significant decrease in total beverage energy, no significant changes were reported for total beverage milliliters. We hypothesized that participants replaced their SSBs with healthier beverage options (i.e., water or artificially sweetened beverages) instead of simply decreasing SSB intake (and subsequently total fluid intake). A previous investigation showed that the replacement of SSBs with water or artificially sweetened beverages decreased energy intake (55); however, because the authors did not report the change in total beverage milliliters, it was not possible to determine whether these results are comparable. An additional hypothesis is that, because beverages have a decreased satiety value compared with that of solid foods (20–23), the displaced calories from SSBs were not perceived as a hunger cue. Thus, consequently, they were not replaced with other energy sources as was substantiated by the significant reduction in BMI status within the SIPsmartER group compared with that in the MoveMore group (30). When SIPsmartER beverage intake was compared with recommendations set by the Beverage Guidance Panel, 5 of 6 beverage amounts met the standards with the exception of a minimal amount of whole milk (12 mL). Although SSB consumption significantly decreased, intake did not meet the recommendation of <240 mL/d (<8 fl oz/d) for the sixth beverage intake (calorically sweetened beverages) (Table 5).
The intention-to-treat analyses were discussed in this article because they provided a more conservative approach; however, SIPsmartER participants who were present at follow-up experienced additional alterations in their dietary intakes. For HEI scores, total protein scores improved, whereas sodium scores decreased. Because HEI scores were adjusted for total energy intake, the reduction of carbohydrates and, consequently, that of energy may have caused a higher percentage of energy to come from protein sources. Although absolute sodium intake decreased over the intervention, conversely, the sodium HEI score also decreased. A possible explanation of this outcome may be that decreased energy intake consequently caused an increased ratio of sodium per calorie (56). Also, beneficial changes were shown in respect to the consumption of specific beverages including increased intake of water and decreased intake sweetened-juice drinks.
In the MoveMore group, a significant but minimal decrease in SSB milliliters and total beverage energy occurred, which provided partial support for the potential of exercise as a gateway behavior to some dietary changes (24–27). However, unlike in the SIPsmartER group, no changes were shown for any other dietary variables. Because MoveMore participants were exposed to multiple SSB questions during the baseline and 6-mo assessments, and participants were aware of the other intervention arm, it may be hypothesized that, rather than being a gateway behavior, this exposure contributed to the reported minimal decrease in SSB consumption (75 mL) and, consequently, that of beverage energy (57). The SIPsmartER group did not show improvements in physical activity behaviors, thereby suggesting that, considered in the context of improvements of other dietary indicators of SIPsmartER participants, a reduction of SSB consumption may be a reasonable gateway behavior for the overall dietary quality but likely does not extend this benefit to physical activity or other behaviors. In addition, when changes in dietary quality were examined between the 2 groups over the intervention, SIPsmartER participants improved HEI scores of total and empty calories as well as of total vegetable consumption, but intakes of other dietary quality indicators were unchanged, which suggested that an SSB reduction as a gateway across all aspects of the HEI score is questionable.
A major strength of this investigation is that the Talking Health study was the first randomized controlled trial, to our knowledge, to focus on reducing SSB consumption as the primary outcome. Thus, this aspect facilitated the ability to identify direct associations between SSB reduction and compensatory changes in dietary variables. Several limitations of this investigation should be noted. The first limitation is the reliance on self-reported dietary data, which are subject to reporting errors and a potential bias (40). To help offset the potential bias, a gold-standard dietary recall methodology and state-of the-art nutritional analysis (NDS-R) software were used as was an objective SSB dietary biomarker (29). The reported significant changes in δ13C values provided objective evidence for the actual reduction in SSB consumption. In addition, the low variability in sex (81% female) and race (93% Caucasian) may have made it difficult to generalize these findings beyond rural Southwest Virginia; however, this cohort was representative of the study region with the exception of the male participants (i.e., 95% Caucasian) (7, 58).
In conclusion, a behavioral intervention that focuses solely on SSB reduction leads to significant improvements beyond SSB and AS consumption by also improving the overall dietary quality. Although the SIPsmartER group did not reach the new AS recommendation of ≤10% of energy from AS during the 6-mo intervention (a decrease from 21% to 16%), significant dietary improvements were still achieved. Interventions that target a single dietary recommendation, such as ≤240 mL SSBs/d (≤8 fl oz SSB/d) or ≤10% of calories from AS per day, may improve overall dietary health and provide motivation for individuals to make additional positive dietary changes.
Acknowledgments
The authors’ responsibilities were as follows—VEH, BMD, WY, PAE, and JMZ: were responsible for the study concept and design; VEH, KJP, and JMZ: conducted the research; VEH and WY: analyzed the data and performed the statistical analysis; and all authors: drafted the manuscript, had full access to all study data, took full responsibility for the final content of the manuscript, and read and approved the final manuscript. None of the authors reported a conflict of interest related to the study.
Footnotes
Abbreviations used: AS, added sugar; HEI, Healthy Eating Index-2010; NDS-R, Nutrition Data System for Research; SSB, sugar-sweetened beverage.
REFERENCES
- 1.Hu FB. Resolved: there is sufficient scientific evidence that decreasing sugar-sweetened beverage consumption will reduce the prevalence of obesity and obesity-related diseases. Obes Rev 2013;14:606–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yang Q, Zhang Z, Gregg EW, Flanders WD, Merritt R, Hu FB. Added sugar intake and cardiovascular diseases mortality among US adults. JAMA Intern Med 2014;174:516–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.O’Connor L, Imamura F, Lentjes MA, Khaw KT, Wareham NJ, Forouhi NG. Prospective associations and population impact of sweet beverage intake and type 2 diabetes, and effects of substitutions with alternative beverages. Diabetologia 2015;58:1474–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Malik VS, Popkin BM, Bray GA, Despres JP, Hu FB. Sugar-sweetened beverages, obesity, type 2 diabetes mellitus, and cardiovascular disease risk. Circulation 2010;121:1356–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kit BK, Fakhouri TH, Park S, Nielsen SJ, Ogden CL. Trends in sugar-sweetened beverage consumption among youth and adults in the United States: 1999-2010. Am J Clin Nutr 2013;98:180–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tate DF, Turner-McGrievy G, Lyons E, Stevens J, Erickson K, Polzien K, Diamond M, Wang X, Popkin B. Replacing caloric beverages with water or diet beverages for weight loss in adults: main results of the Choose Healthy Options Consciously Everyday (CHOICE) randomized clinical trial. Am J Clin Nutr 2012;95:555–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zoellner J, Chen Y, Davy B, You W, Hedrick V, Corsi T, Estabrooks P. Talking Health, a pragmatic randomized-controlled health literacy trial targeting sugar-sweetened beverage consumption among adults: rationale, design & methods. Contemp Clin Trials 2014;37:43–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brownell KD, Frieden TR. Ounces of prevention-the public policy case for taxes on sugared beverages. N Engl J Med 2009;360:1805–8. [DOI] [PubMed] [Google Scholar]
- 9.Brownell KD, Farley T, Willett WC, Popkin BM, Chaloupka FJ, Thompson JW, Ludwig DS. The public health and economic benefits of taxing sugar-sweetened beverages. N Engl J Med 2009;361:1599–605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sturm R, Powell LM, Chriqui JF, Chaloupka FJ. Soda taxes, soft drink consumption, and children’s body mass index. Health Aff (Millwood) 2010;29:1052–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.US Department of Health and Human Services (HHS), USDA. Dietary Guidelines for Americans, 2015-2020. 8th ed. Washington (DC): US Government Printing Office; 2015. [Google Scholar]
- 12.Zheng M, Allman-Farinelli M, Heitmann BL, Rangan A. Substitution of sugar-sweetened beverages with other beverage alternatives: a review of long-term health outcomes. J Acad Nutr Diet 2015;115:767–79. [DOI] [PubMed] [Google Scholar]
- 13.Chen L, Appel LJ, Loria C, Lin PH, Champagne CM, Elmer PJ, Ard JD, Mitchell D, Batch BC, Svetkey LP, et al. Reduction in consumption of sugar-sweetened beverages is associated with weight loss: the PREMIER trial. Am J Clin Nutr 2009;89:1299–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chen L, Caballero B, Mitchell DC, Loria C, Lin PH, Champagne CM, Elmer PJ, Ard JD, Batch BC, Anderson CA, et al. Reducing consumption of sugar-sweetened beverages is associated with reduced blood pressure: a prospective study among United States adults. Circulation 2010;121:2398–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Myers EF, Khoo CS, Murphy W, Steiber A, Agarwal S. A critical assessment of research needs identified by the Dietary Guidelines committees from 1980 to 2010. J Acad Nutr Diet 2013;113:957–71.e1. [DOI] [PubMed] [Google Scholar]
- 16.2015 Dietary Guidelines Advisory Committee. Scientific report of the 2015 Dietary Guidelines Advisory Committee (DGAC report) [Internet]. Released 2015 Feb 23 [cited 2015 Aug 5]. Available from: https://health.gov/dietaryguidelines/.
- 17.Novak NL, Brownell KD. Taxation as prevention and as a treatment for obesity: the case of sugar-sweetened beverages. Curr Pharm Des 2011;17:1218–22. [DOI] [PubMed] [Google Scholar]
- 18.Johnson RK, Appel LJ, Brands M, Howard BV, Lefevre M, Lustig RH, Sacks F, Steffen LM, Wylie-Rosett J. Dietary sugars intake and cardiovascular health: a scientific statement from the American Heart Association. Circulation 2009;120:1011–20. [DOI] [PubMed] [Google Scholar]
- 19.Hedrick V, Davy B, Duffey K. Is beverage consumption related to specific dietary pattern intakes. Curr Nutr Rep 2015;4:72–81. [Google Scholar]
- 20.Davy BM, Dennis EA, Dengo AL, Wilson KL, Davy KP. Water consumption reduces energy intake at a breakfast meal in obese older adults. J Am Diet Assoc 2008;108:1236–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dennis EA, Dengo AL, Comber DL, Flack KD, Savla J, Davy KP, Davy BM. Water consumption increases weight loss during a hypocaloric diet intervention in middle-aged and older adults. Obesity (Silver Spring) 2010;18:300–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.DiMeglio DP, Mattes RD. Liquid versus solid carbohydrate: effects on food intake and body weight. Int J Obes Relat Metab Disord 2000;24:794–800. [DOI] [PubMed] [Google Scholar]
- 23.Mattes RD. Dietary compensation by humans for supplemental energy provided as ethanol or carbohydrate in fluids. Physiol Behav 1996;59:179–87. [DOI] [PubMed] [Google Scholar]
- 24.Nigg CR, Burbank PM, Padula C, Dufresne R, Rossi JS, Velicer WF, Laforge RG, Prochaska JO. Stages of change across ten health risk behaviors for older adults. Gerontologist 1999;39:473–82. [DOI] [PubMed] [Google Scholar]
- 25.Mata J, Silva MN, Vieira PN, Carraca EV, Andrade AM, Coutinho SR, Sardinha LB, Teixeira PJ. Motivational “spill-over” during weight control: increased self-determination and exercise intrinsic motivation predict eating self-regulation. Health Psychol 2009;28:709–16. [DOI] [PubMed] [Google Scholar]
- 26.Dutton GR, Napolitano MA, Whiteley JA, Marcus BH. Is physical activity a gateway behavior for diet? Findings from a physical activity trial. Prev Med 2008;46:216–21. [DOI] [PubMed] [Google Scholar]
- 27.Tucker M, Reicks M. Exercise as a gateway behavior for healthful eating among older adults: an exploratory study. J Nutr Educ Behav 2002;34 Suppl 1:S14–9. [DOI] [PubMed] [Google Scholar]
- 28.Duffey KJ, Popkin BM. Adults with healthier dietary patterns have healthier beverage patterns. J Nutr 2006;136:2901–7. [DOI] [PubMed] [Google Scholar]
- 29.Davy BM, Jahren AH, Hedrick VE, You W, Zoellner JM. Influence of an intervention targeting a reduction in sugary beverage intake on the δ13C sugar intake biomarker in a predominantly obese, health-disparate sample. Public Health Nutr 2017;20:25–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zoellner JM, Hedrick VE, You W, Chen Y, Davy BM, Porter KJ, Bailey A, Lane H, Alexander R, Estabrooks PA. Effects of a behavioral and health literacy intervention to reduce sugar-sweetened beverages: a randomized-controlled trial. Int J Behav Nutr Phys Act 2016;13:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process 1991;50:179–211. [Google Scholar]
- 32.Popkin BM, Armstrong LE, Bray GM, Caballero B, Frei B, Willett WC. A new proposed guidance system for beverage consumption in the United States. Am J Clin Nutr 2006;83:529–42. [DOI] [PubMed] [Google Scholar]
- 33. US Department of Health and Human Services and Health Resources and Services Administration [Internet]. Medically underserved areas/populations: guidelines for MUA and MUP designation. 1995 [cited 2014 Oct 2]. Available from: https://bhw.hrsa.gov/shortage-designation/muap.
- 34.Hedrick VE, Comber DL, Estabrooks PA, Savla J, Davy BM. The beverage intake questionnaire: determining initial validity and reliability. J Am Diet Assoc 2010;110:1227–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hedrick VE, Comber DL, Ferguson KE, Estabrooks PA, Savla J, Dietrich AM, Serrano E, Davy BM. A rapid beverage intake questionnaire can detect changes in beverage intake. Eat Behav 2013;14:90–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hedrick VE, Savla J, Comber DL, Flack KD, Estabrooks PA, Nsiah-Kumi PA, Ortmeier S, Davy BM. Development of a brief questionnaire to assess habitual beverage intake (BEVQ-15): sugar-sweetened beverages and total beverage energy intake. J Acad Nutr Diet 2012;112:840–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Riebl SK, Paone AC, Hedrick VE, Zoellner JM, Estabrooks PA, Davy BM. The comparative validity of interactive multimedia questionnaires to paper-administered questionnaires for beverage intake and physical activity: pilot study. JMIR Res Protoc 2013;2:e40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Godin G, Shephard RJ. A simple method to assess exercise behavior in the community. Can J Appl Sport Sci 1985;10:141–6. [PubMed] [Google Scholar]
- 39.Monsen E. Research: successful approaches. 2nd ed. Chicago: American Dietetic Association; 2003. [Google Scholar]
- 40.Willett W, Lenart E. Nutritional epidemiology. 2nd ed. New York: Oxford University Press; 1998. [Google Scholar]
- 41.Guenther PM, Kirkpatrick SI, Reedy J, Krebs-Smith SM, Buckman DW, Dodd KW, Casavale KO, Carroll RJ. The Healthy Eating Index-2010 is a valid and reliable measure of diet quality according to the 2010 Dietary Guidelines for Americans. J Nutr 2014;144:399–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.USDA, US Department of Health and Human Services. Dietary Guidelines for Americans, 2010. Washington (DC): US Government Printing Office; 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hedrick VE, Dietrich AM, Estabrooks PA, Savla J, Serrano E, Davy BM. Dietary biomarkers: advances, limitations and future directions. Nutr J 2012;11:109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Laird NM, Ware JH. Random-effects models for longitudinal data. Biometrics 1982;38:963–74. [PubMed] [Google Scholar]
- 45.Rubin D. Multiple imputations for nonresponse in surveys. New York: John Wiley & Sons Inc.; 1987. [Google Scholar]
- 46.Anderson AL, Harris TB, Tylavsky FA, Perry SE, Houston DK, Lee JS, Kanaya AM, Sahyoun NR. Dietary patterns, insulin sensitivity and inflammation in older adults. Eur J Clin Nutr 2012;66:18–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Steffen LM, Van Horn L, Daviglus ML, Zhou X, Reis JP, Loria CM, Jacobs DR, Duffey KJ. A modified Mediterranean diet score is associated with a lower risk of incident metabolic syndrome over 25 years among young adults: the CARDIA (Coronary Artery Risk Development in Young Adults) study. Br J Nutr 2014;112:1654–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Engeset D, Alsaker E, Ciampi A, Lund E. Dietary patterns and lifestyle factors in the Norwegian EPIC cohort: the Norwegian Women and Cancer (NOWAC) study. Eur J Clin Nutr 2005;59:675–84. [DOI] [PubMed] [Google Scholar]
- 49.Naja F, Nasreddine L, Itani L, Chamieh MC, Adra N, Sibai AM, Hwalla N. Dietary patterns and their association with obesity and sociodemographic factors in a national sample of Lebanese adults. Public Health Nutr 2011;14:1570–8. [DOI] [PubMed] [Google Scholar]
- 50.Sánchez-Villegas A, Toledo E, Bes-Rastrollo M, Martín-Moreno JM, Tortosa A, Martínez-González MA. Association between dietary and beverage consumption patterns in the SUN (Seguimiento Universidad de Navarra) cohort study. Public Health Nutr 2009;12:351–8. [DOI] [PubMed] [Google Scholar]
- 51.Newby PK, Muller D, Hallfrisch J, Andres R, Tucker KL. Food patterns measured by factor analysis and anthropometric changes in adults. Am J Clin Nutr 2004;80:504–13. [DOI] [PubMed] [Google Scholar]
- 52.Hedrick VE, Davy BM, Wilburn GA, Jahren AH, Zoellner JM. Evaluation of a novel biomarker of added sugar intake (delta 13C) compared with self-reported added sugar intake and the Healthy Eating Index-2010 in a community-based, rural US sample. Public Health Nutr 2016;19:429–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kuhnle GG. Nutritional biomarkers for objective dietary assessment. J Sci Food Agric 2012;92:1145–9. [DOI] [PubMed] [Google Scholar]
- 54.Stookey JD, Constant F, Gardner CD, Popkin BM. Replacing sweetened caloric beverages with drinking water is associated with lower energy intake. Obesity (Silver Spring) 2007;15:3013–22. [DOI] [PubMed] [Google Scholar]
- 55.Piernas C, Tate DF, Wang X, Popkin BM. Does diet-beverage intake affect dietary consumption patterns? Results from the Choose Healthy Options Consciously Everyday (CHOICE) randomized clinical trial. Am J Clin Nutr 2013;97:604–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Guenther PM, Casavale KO, Reedy J, Kirkpatrick SI, Hiza HA, Kuczynski KJ, Kahle LL, Krebs-Smith SM. Update of the Healthy Eating Index: HEI-2010. J Acad Nutr Diet 2013;113:569–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Morwitz VG, Johnson E, Schmittlein D. Does measuring intent change behavior? J Consum Res 1993;20:46–61. [Google Scholar]
- 58.US Census Bureau. American FactFinder fact sheet: Lee County, Giles County, Pulaski County, Washington County, Grayson County, Wise County, VA. 2010 [cited 2014 Mar 7]. Available from: http://factfinder2.census.gov.