Since 2012, the Hospital Readmission Reduction Program1 within the Patient Protection and Affordable Care Act2 began holding hospitals accountable for higher-than-expected 30-day readmission rates following hospitalization for certain medical conditions.3, 4 In fiscal year 2015, total knee arthroplasty (TKA) was added to the readmission reduction program. TKA along with total hip replacements are the only conditions in the current program with a high concentrations (87%) of post-acute care use.5 In 2013, the Patient Protection and Affordable Care Act also initiated the Bundled Payments for Care Improvement program.2, 6 This national initiative examines 30-, 60- or 90-day episodes of care and includes all cost of services within the stated time periods.6 Unlike the Bundled Payment program, which is a voluntary participation program, the Centers for Medicare and Medicaid Services (CMS) included joint replacement into the bundling initiative through the Comprehensive Care for Joint Replacement (CJR) model, which was implemented on April 1, 2016.7, 8 These policy changes have resulted in a critical need to examine ways to improve the efficiency of continuity of care among acute and post-acute providers and reducing complications that result in unplanned hospital readmissions.9 It would be helpful to know if the rates and causes of readmission differ based on the patient’s initial post-acute discharge setting.10
More than 600,000 TKA procedures are performed yearly in the United States, making TKA one of the most commonly performed major surgical procedures.11 TKA, both primary and revision procedures, are expected to drastically increase in frequency during the upcoming decades due to the rapidly growing aging population.12 Post-acute care following TKA encompasses several types of health care services at both institutional and community-based settings, all of which aim to provide health and rehabilitative services for recovery and functional restoration.13 Post-acute services are available through skilled nursing facilities (SNF), inpatient rehabilitation facilities (IRF), home health agencies, long term acute care hospitals, and outpatient rehabilitation centers.13 The projected growth, coupled with the inclusion of TKA in several different policy implications (payment bundling, CJR)1,2,5–7 highlights the need to examine the effects of post-acute discharge setting on readmission rates following TKA.14
Previous research indicates that TKA patients who discharge home have lower 30- and 90-day readmission rates than those who discharge to IRF or SNF settings.14–17 Commonly cited reasons for hospital readmission at 30 or 90 days include problems associated with the joint replacement procedure itself (infection or joint stiffness)16, 18–21 or respiratory or cardiovascular events.9, 20 Other reported clinical factors increasing 30- or 90-day readmission include longer hospital length of stay, general anesthesia, blood transfusions, increased comorbidity, rheumatoid arthritis, venous thromboembolism and urinary tract infections.21–23 Overall readmission rates among Medicare beneficiaries regardless of diagnosis are reported to be 19.6% within 30 days and 34.0% within 90 days.3 Readmission following TKA are reported to range from 3.4% to 6.6% over 30 days and 3.5% to 15.6% over 90 days.9, 19–21, 23 However, these results are coming from studies with relatively small samples or did not include all commonly used post-acute settings.14–17
To address these gaps and advance the evidence for readmissions among patients with a TKA, this study has two objectives: first, identify predictors of 30-day unplanned readmission following TKA among Medicare beneficiaries; and second, examine readmission rates and common reasons for readmissions up to 90 days following discharge to the three primary post-acute settings: IRF, SNF and community.
Methods
Study Design
This study was a secondary analysis of Medicare claims data for 2009–2011. We used the Medicare Provider Analysis and Review (MedPAR) files linked with the enrollment indicator files. To examine the number of times a patient was readmitted in the previous year as a covariate, a retrospective observation period of one-year was performed using 2008 data. Further, to examine 90-day readmission following hospitalization discharge, only those patients who received a primary TKA (unilateral or bilateral) and were discharged from an acute care hospital between January 1, 2009 and September 30, 2011 were included. We included only Medicare beneficiaries aged ≥ 66 years at the index hospitalization and those enrolled in a fee-for-service plan. TKA procedures were identified using the International Classification of Diseases, Ninth revision, Clinical Modification (ICD-9-CM) procedure code of 81.54.24 Bilateral procedures were identified using the TKA 81.54 procedure code listed under two surgical procedure code columns for a single stay in the MedPAR files. This study was approved by the University’s Institutional Review Board and a data use agreement was established with the CMS prior to the study.
Sample preparation
In all, 963,438 patients met the initial inclusion criteria. We excluded patients who were enrolled in a Health Maintenance Organization (HMO) at any time during the study period, died during initial hospitalization, had missing data on patient or clinical characteristics, had other than elective or traumatic reasons for admission or were discharged to a setting other than the three post-acute settings (IRF, SNF, and HHA) or community. Following exclusions, 63% of the original sample was included in the univariate analysis, frequencies and reasons for readmission and 90-day survival analysis. An additional 0.1% who died within 30 days of their index stay was excluded in the logistic modeling for 30-day readmission. Figure 1 shows a graphical representation of the study’s inclusions and exclusion criteria and results.
Figure 1.
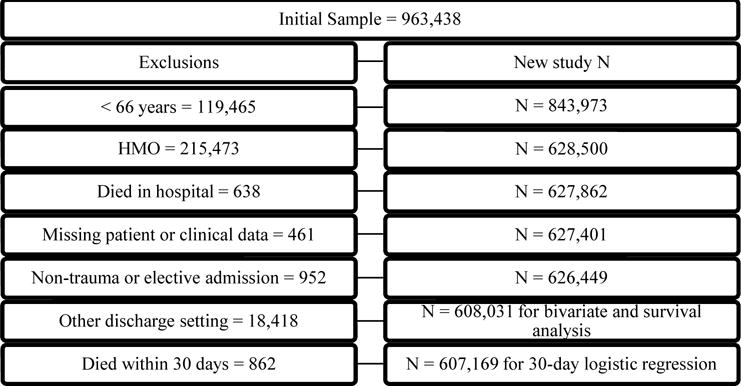
Flow chart representing study inclusions and exclusion criteria.
Outcome Measures
Readmissions were indicated if a patient had a claim for an unplanned acute hospital stay in the MedPAR within the specified timeframes (30, 60 or 90 days) following discharge from the index stay for TKA. Unplanned readmissions were coded using the methodology from CMS’ hospital-wide readmission measure.25 The variable was coded as a dichotomous (yes/no) variable for the 30-day readmission logistic regression analysis. Days to readmission were also recorded and used along with the dichotomous indicator variable for the 90-day readmission survival analysis. Reasons for hospital readmission were obtained using the Medicare Severity-Diagnosis Related Groups (MS-DRG) diagnostic codes in the MedPAR files.
Independent variable
The discharge setting variable included the three post-acute settings following TKA: SNF, IRF and community. Two categories, SNF and IRF, are distinct categories in the discharge setting variable of the MedPAR.26 The community category included home with or without home health care. All other settings were excluded.
Demographic Information
Age and sex were obtained from the MedPAR. Age was categorized (66–70, 71–80, ≥ 81 years) for the descriptive table and used as a continuous variable for the regression modeling. Race/ethnicity was extracted from the enrollment indicator files using the variable developed by the Research Triangle Institute (RTI).27 Non-Hispanic white, non-Hispanic black and Hispanic were coded directly from the original source variable. Individuals listed as Asian/Pacific Islander, American Indian/Alaska Native, Unknown, and Other were re-coded as “other” for the analyses. The original reason for Medicare benefits was also extracted from the enrollment indicator; we coded this as a dichotomous variable indicating disability as the original reason for entitlement or not (yes/no).
Clinical Characteristics
The Charlson Comorbidity Index (CCI) was used to control for comorbidity burden during the hospital stay.28 This index quantifies health status by examining ICD-codes related to 17 medical conditions.28, 29 The comorbidity index was categorized into a 3-level (0, 1, ≥ 2) variable based on the sum of conditions listed for a given patient. Hospital length of stay was categorized (1–2, 3–4, ≥ 5 days) for the descriptive table and maintained as a continuous variable for regression analysis. The number of times a patient was admitted to a hospital over the year prior to the index admission date was also categorized (0, 1, ≥ 2) for the descriptive analysis and used as a continuous variable for the regression analysis. Other clinical variables included in this analysis include number of days (0, ≥ 1) in the intensive care unit (ICU), surgery type (unilateral, bilateral), and admission type (elective, traumatic) for the TKA intervention. Traumatic admissions were coded using the MedPAR variables of emergent, urgent or traumatic.
Facility Volume
Previous studies found associations between facility TKA volume and patient outcomes of functional status, mortality rates and post-operative complication rates.30–33 For this study, hospital-level TKA volumes were aggregated from the annual number of claims in the MedPAR and categorized into quartiles (1–19, 20–58, 59–137, ≥ 138) for analysis.
Statistical Analysis
Demographic, clinical and facility volume were stratified by post-acute discharge setting to highlight the differences in the patient populations. In addition, these characteristics were stratified by 30-day readmission (yes/no) for the entire sample. Differences in readmission rates across categories of patient characteristic variables were assessed via observed rates and estimated 95% confidence intervals (CIs).34 Rates with 95% CIs that did not overlap were considered to be statistically different. Fully adjusted logistic regression was performed in order to assess the independent effects of post-acute discharge setting on 30-day readmission after controlling for age, gender, race/ethnicity, disability entitlement, surgery type, admission type, number of times a patient was admitted to a hospital within the previous year, hospital length of stay, number of ICU days, discharge setting, Charlson Comorbidity Index and hospital TKA volume. Non-readmission was used as the referent category.
Cox proportional hazards models were used to assess the independent effects of discharge setting in predicting time-to-readmission over 90 days following the initial TKA procedure, after controlling for all the covariates. Patients not readmitted within 90 days were censored at the 90-day point. Patients who either died or enrolled in an HMO prior to being readmitted were censored at those respective time points. Kaplan-Meier curves were used to assess the proportion of first time hospital readmissions of patients from each discharge setting at the 30-, 60- and 90-day time points. Groups were compared using a log-rank test with a p < .05 indicating statistical significance.
To examine the reasons for hospital readmission, the top 10 MS-DRGs were identified at the 30-, 60- and 90-day time points and stratified by post-acute discharge setting. Readmissions for TKA, representing a staged bilateral procedure, within the readmission period were not counted as a condition of readmission following the index stay. All analyses were performed using SPSS version 23 (IBM Corp., Armonk, NY).
Results
The mean age of the sample was 74.4 (SD 6.0) years. A majority of the patients were female (64%) and white (89%). A total of 32,226 patients were readmitted within 30 days. Patients with disability entitlement comprised 7.8% of the sample. Unilateral TKA encompassed 96% of the procedures. Over 94% of the patients received an elective TKA procedure. The average number of admissions in the previous year was 0.3 (SD 0.6). The average length of stay in acute hospitals was 3.4 (SD 1.5) days. Most (96%) patients did not have any days in the ICU during their hospitalization. Less than 1% of patients died within 90 days following their initial hospitalization. More than half (56%) of the patients were discharged to the community following TKA with 32% and 12% discharging to SNF and IRF, respectively.
Patient characteristics stratified by hospital discharge setting are shown in Table 1. Older patients with more comorbidities, more prior acute stays and longer lengths of stay were more likely to be discharged to IRF or SNF than to community. In addition, those with bilateral procedures were much more likely to be discharged to IRF than to either SNF or community.
Table 1.
Patient characteristics stratified by hospital discharge setting and overall (95% CI) 30-day readmission rates by patient characteristics.
| DC Setting
|
Total
|
||||
|---|---|---|---|---|---|
| IRF | SNF | Community | N | 30-dayReadmission | |
| N | 71, 741 | 192, 792 | 343, 498 | 608, 031 | 5.3% (5.3%, 5.4%) |
| Age | |||||
| 66–70 yrs | 25.6% | 22.1% | 38.7% | 194, 063 | 4.0% (3.9%, 4.1%) |
| 71–80 yrs | 49.5% | 51.4% | 50.5% | 308, 084 | 5.3% (5.3%, 5.4%) |
| 81+ yrs | 24.9% | 26.5% | 10.8% | 105, 884 | 7.8% (7.6%, 7.9%) |
| Sex | |||||
| Female | 69.3% | 73.0% | 57.7% | 388, 495 | 5.0% (4.9%, 5.1%) |
| Male | 30.7% | 27.0% | 42.3% | 219, 536 | 6.0% (5.9%, 6.1%) |
| Race/ethnicity | |||||
| White | 85.6% | 88.0% | 90.5% | 541, 719 | 5.3% (5.2%, 5.3%) |
| Black | 7.3% | 6.0% | 3.9% | 30, 111 | 6.4% (6.1%, 6.7%) |
| Hispanic | 4.9% | 3.9% | 3.7% | 23, 507 | 5.5% (5.2%, 5.7%) |
| Other | 2.2% | 2.2% | 2.0% | 12, 694 | 5.0% (4.6%, 5.4%) |
| Disability | |||||
| No | 90.8% | 91.2% | 93.0% | 560, 507 | 5.2% (5.1%, 5.2%) |
| Yes | 9.2% | 8.8% | 7.0% | 47, 524 | 7.5% (7.2%, 7.7%) |
| Surgery type | |||||
| Unilateral | 83.6% | 96.6% | 98.5% | 584, 626 | 5.3% (5.2%, 5.4%) |
| Bilateral | 16.4% | 3.4% | 1.5% | 23, 405 | 6.2% (5.9%, 6.5%) |
| Admission type | |||||
| Elective | 93.4% | 94.4% | 94.2% | 572, 532 | 5.3% (5.2%, 5.4%) |
| Traumatic | 6.6% | 5.6% | 5.8% | 35, 499 | 6.0% (5.8%, 6.3%) |
| Prior acute stays | |||||
| 0 stays | 77.2% | 76.2% | 80.7% | 479, 550 | 4.9% (4.8%, 5.0%) |
| 1 stay | 16.8% | 18.2% | 16.3% | 103, 063 | 6.0% (5.9%, 6.1%) |
| 2+ stays | 5.9% | 5.6% | 3.0% | 25, 418 | 10.8% (10.5%, 11.2%) |
| Charlson | |||||
| 0 conditions | 51.6% | 52.5% | 61.1% | 347, 905 | 4.3% (4.3%, 4.4%) |
| 1 condition | 34.7% | 34.1% | 30.4% | 195, 086 | 5.9% (5.8%, 6.0%) |
| 2+ conditions | 13.7% | 13.4% | 8.6% | 65, 040 | 8.9% (8.7%, 9.1%) |
| Length of stay | |||||
| 1–2 days | 12.3% | .4% | 21.4% | 82, 985 | 3.8% (3.7%, 3.9%) |
| 3–4 days | 71.7% | 85.8% | 71.4% | 462, 068 | 5.1% (5.0%, 5.1%) |
| 5+ days | 16.0% | 13.8% | 7.2% | 62, 978 | 9.3% (9.1%, 9.6%) |
| ICU | |||||
| 0 days | 93.5% | 94.8% | 96.8% | 582, 273 | 5.2% (5.1%, 5.2%) |
| 1+ days | 6.5% | 5.2% | 3.2% | 25, 758 | 9.2% (8.8%, 9.5%) |
| Death | |||||
| Survived | 99.4% | 99.5% | 99.8% | 605, 945 | 5.2% (5.1%, 5.2%) |
| 1–30 days | .2% | .2% | .1% | 862 | 56.1% (52.8%, 59.5%) |
| 31–60 days | .2% | .2% | .0% | 643 | 50.7% (46.8%, 54.6%) |
| 61–90 days | .2% | .2% | .0% | 581 | 33.4% (29.6%, 37.2%) |
| TKA volume (Quartiles) | |||||
| 1–19 | 1.5% | 1.7% | 1.8% | 10, 581 | 6.7% (6.2%, 7.2%) |
| 20–58 | 8.9% | 9.0% | 8.2% | 51, 715 | 6.0% (5.8%, 6.2%) |
| 59–137 | 24.9% | 23.9% | 20.6% | 134, 819 | 5.6% (5.5%, 5.7%) |
| >137 | 64.6% | 65.4% | 69.4% | 410, 916 | 5.1% (5.1%, 5.2%) |
Estimated 95% confidence intervals were calculated using the methodology described by Blythe34
Table 1 also shows 30-day readmission rates stratified by patient demographic and clinical characteristics. Using non-overlapping 95% confidence intervals as the criterion, numerous variables were significantly associated with 30-day readmission. Readmission increased with advanced age. Males were more likely to be readmitted than females. Regarding race/ethnicity, black patients experienced the highest readmission rates and were the only group significantly different from whites. Patients with disability entitlement were more likely to be readmitted than those without. Bilateral surgery was associated with higher readmission rates than unilateral. Similarly, traumatic admission was associated with higher rates than the more common elective admission. Patients with ≥ 2 admissions over the prior year were twice as likely to be readmitted as those with no prior stays. Similarly, patients with ≥ 2 Charlson comorbid conditions were twice as likely to be readmitted as those with none. Our length of stay categories (1–2 days, 3–4 days and ≥ 5 days) also demonstrated a significant stepwise increase in readmission risk. Being admitted to the ICU during the hospital stay was also associated with substantially higher readmission rates. Interestingly, more than half (56.1%) of patients who died within 30 days of discharge were readmitted first. Hospital TKA volume demonstrated a stepwise decrease in readmission rates from the lowest quartile to the highest. Discharge setting also demonstrated a discernable gradient in readmission rates from community (4.1%) to SNF (6.9%) to IRF (7.2%).
Table 2 presents the adjusted odds ratios (OR) from the logistic regression analysis for 30-day unplanned readmission using non-readmission as the referent category. Compared to community discharge, patients discharged to IRF or SNF had 44% and 40% higher odds of 30-day readmission, respectively. Figure 2 represents the adjusted predicted probability of 30-day readmission by discharge setting (community, SNF and IRF). Patients discharged to the community had a lower probability of 30-day readmission than those discharged to either SNF or IRF.
Table 2.
Results of logistic regression analysis for 30-day readmission.
| Odds Ratio | 95% CI | |
|---|---|---|
| Discharge setting (Community = reference) | ||
| IRF | 1.44 | 1.39–1.49 |
| SNF | 1.40 | 1.36–1.44 |
| Age | 1.04 | 1.03–1.04 |
| Gender (Female = reference) | ||
| Male | 1.24 | 1.22–1.27 |
| Race/Ethnicity (White = reference) | ||
| Black | 1.12 | 1.07–1.18 |
| Hispanic | 0.99 | 0.93–1.05 |
| Other | 0.95 | 0.88–1.03 |
| Disability entitlement (No = reference) | ||
| Yes | 1.41 | 1.36–1.46 |
| Surgery type (Unilateral = reference) | ||
| Bilateral | 1.10 | 1.03–1.16 |
| Admission type (Elective = reference) | ||
| Traumatic | 1.05 | 1.00–1.10 |
| # Previous admissions | 1.24 | 1.22–1.25 |
| Hospital length of stay | 1.09 | 1.08–1.10 |
| # days in ICU (0 days = reference) | 1.25 | 1.19–1.31 |
| Charlson comorbidities (0 = reference) | ||
| 1 | 1.28 | 1.25–1.31 |
| ≥2 | 1.72 | 1.66–1.78 |
| Hospital TKA volume (≥138 = reference) | ||
| 1–19 | 1.21 | 1.12–1.31 |
| 20–58 | 1.10 | 1.06–1.14 |
| 59–137 | 1.04 | 1.01–1.07 |
Target category for readmission outcome = yes.
Figure 2.
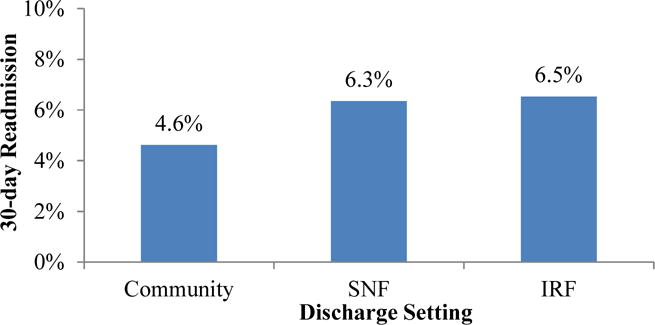
Predicted probability of 30-day readmission by discharge setting.
Table 3 shows the adjusted hazard ratios (HR) for the time to first unplanned readmission within 90 days of hospital discharge. Patients discharged to IRF and SNF had a 48% and 45% higher risk of 90-day readmission, respectively, compared to those discharged to community.
Table 3.
Results of Cox regression model for readmission within 90 days.
| Hazard Ratio | 95% CI | |
|---|---|---|
| Discharge setting (Community = reference) | 1.00 | |
| IRF | 1.48 | 1.44–1.52 |
| SNF | 1.45 | 1.42–1.47 |
| Age | 1.04 | 1.03–1.04 |
| Gender (Female = reference) | 1.00 | |
| Male | 1.17 | 1.15–1.19 |
| Race/Ethnicity (White = reference) | 1.00 | |
| Black | 1.11 | 1.07–1.15 |
| Hispanic | 1.00 | 0.96–1.04 |
| Other | 0.96 | 0.90–1.02 |
| Disability entitlement (No = reference) | 1.00 | |
| Yes | 1.41 | 1.38–1.45 |
| Surgery type (Unilateral = reference) | 1.00 | |
| Bilateral | 1.01 | 0.96–1.05 |
| Admission type (Elective = reference) | 1.00 | |
| Traumatic | 1.06 | 1.03–1.10 |
| # Previous admissions | 1.28 | 1.27–1.29 |
| Hospital length of stay | 1.05 | 1.05–1.06 |
| # days in ICU (0 days = reference) | 1.00 | |
| ≥1 | 1.32 | 1.27–1.36 |
| Charlson comorbidities (0 = reference) | 1.00 | |
| 1 | 1.28 | 1.26–1.30 |
| ≥2 | 1.73 | 1.69–1.77 |
| Hospital TKA volume (≥138 = reference) | 1.00 | |
| 1–19 | 1.18 | 1.12–1.26 |
| 20–58 | 1.09 | 1.06–1.13 |
| 59–137 | 1.04 | 1.03–1.07 |
Figure 3 represents the unadjusted cumulative readmission probabilities for the first unplanned readmission for both the overall sample and by discharge setting. Overall, cumulative readmission rates increased over time and readmissions were lower in community discharges than for IRF or SNF in each time period. The largest increase in readmissions occurred within 30 days of hospital discharge in each discharge setting. A significant difference (p < .0001) was found across discharge settings.
Figure 3.
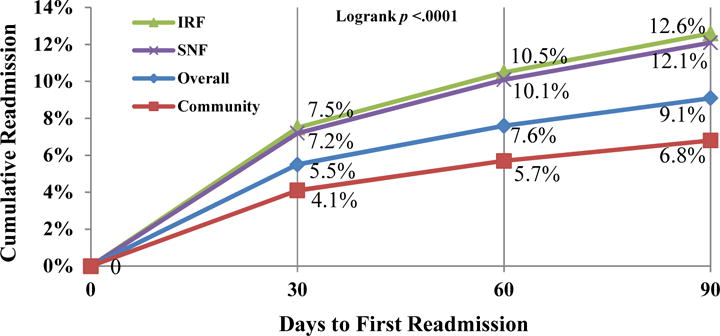
Probability of readmission over time stratified by discharge setting
Appendices A, B and C present the 10 most common reasons (MS-DRG) for hospital readmission within each of the three time periods, by discharge setting. Similar MS-DRGs are observed for all three discharge settings and time categories. In the early (1–30 day) category, MS-DRG 863 (post-operative or traumatic infections) was the most frequent readmission diagnosis in all three discharge settings. Other reasons at 1–30 days included MS-DRGs 603 (cellulitis), 392 (esophagitis, gastroenteritis and miscellaneous digestive disorders), 176 (pulmonary embolus), 309–310 (cardiac arrhythmias) and 641 (miscellaneous disorders of nutrition, metabolism, fluids, or electrolytes). At 31–60 days, MS-DRG 863 (post-operative or traumatic infections) remained in the top 5–7 reasons for readmission in all three settings; however, it did not appear in the 61–90 day period. Reasons for readmission at 31–60 and 61–90 days showed several other similarities. The primary reason for readmission at 31–60 and 61–90 days was MS-DRG 392 (esophagitis, gastroenteritis and miscellaneous digestive disorders) in all settings, except for IRF at 61–90 days, where it was second to MS-DRG 690 (kidney & urinary tract infections). Other codes included MS-DRG 603 (cellulitis), 312 (syncope and collapse) and other cardiac related or miscellaneous diagnoses.
Discussion
Healthcare reform has led to policy changes that hold hospitals responsible for quality measures, such as 30-day readmission following TKA.1–4 In addition, for lower extremity joint replacements, CMS is currently implementing the concept of “payment bundling,” through the CJR initiative, which would cover all acute and post-acute services within 90 days of the initial TKA procedure.2, 6–8 These changes, coupled with the growing trend of individuals undergoing TKA, highlight a critical need to examine ways to reduce healthcare costs and improve quality of care for these patients.12, 9, 14
A previous study using 2003–2004 Medicare data found that 20% of all beneficiaries were readmitted within 30 days and 34% within 90 days following their index hospitalization.3 Also, 10% of those receiving combined knee or hip surgery were readmitted back into the hospital within 30 days. However, that study did not define which surgical procedures specifically made up the surgery cohort.3 Based on 100% Medicare data from 1991–2010, Cram et al. reported that all-cause 30-day readmission following TKA increased from 4% in 1991–1994 to 5% in 2007–2010.11 Using the 100% Medicare data from 2009–2011, our study examined several patient demographic and clinical characteristics as well as hospital volume to predict 30-day hospital readmission. Unlike previous studies, our study emphasized readmission rates and reasons for readmission based on the three most common post-acute discharge settings following TKA: community, SNF and IRF. We also examined cumulative rates and the most common reasons for readmission within 90 days.
Using logistic regression, we found 44% and 40% higher odds of 30-day readmission in patients discharged to IRF or SNF, respectively, compared to those discharged to community. Few prior studies have examined the effect of post-acute discharge setting on 30-day hospital readmission. Ramos et al. found no significant trend in greater 30-day unplanned readmission in those sent to IRF compared to a combined variable of SNF or community.14 Bini et al. examined 90-day hospital readmission using hospital level data and found that those discharged to a SNF had higher odds of readmission compared to those sent home.15 A recent study by Kurtz et al. reported that Medicare beneficiaries discharged home had 25% less risk for 30-day all-cause hospital readmission than those discharged to inpatient post-acute settings.17 Nonetheless, these studies only provide partial information regarding the most prevalent discharge settings following TKA and their impact on hospital readmission, particularly 30-day unplanned readmission in Medicare beneficiaries, which is the primary quality indicator of the readmission reduction program.1
When looking at cumulative rates over 90 days we found 5.5% (30-day), 7.6% (60-day) and 9.1% (90-day) overall unplanned readmission rates, similar to other recent rates reported using the Medicare population.17 We also found lower readmission rates for community than for IRF or SNF at each time point. Other studies examining readmission using non-Medicare data found overall 3.1% to 4.0% 30-day and 3.5% to 8.0% 90-day unplanned readmission rates.15, 16, 18 These lower rates may be explained by these studies having a younger patient population (< 65 years), compared to our study of the Medicare population.
Our time-to-event analysis indicated that those discharged to IRF and SNF had a 48% and 45% greater risk for unplanned hospital readmission up to 90 days, respectively, compared to those discharged to community. Literature is limited related to 90-day readmission by discharge settings. Schairer et al. found, in their all-payer sample, that patients who received either a primary or a revision TKA and were discharged to SNF had a 62% increase in risk of 90-day unplanned readmission when compared to those discharged to all other settings combined.18 The higher rate reported by these authors could be due to the inclusion of revision TKA in their sample and their use of a combined discharge setting variable of IRF and community.18 In addition, those findings were obtained from a single facility, which may vary from our nationally representative sample of more than 608, 000 patients in 2,500 acute hospitals.
A secondary objective of this study was to examine the top 10 reasons for readmission by discharge setting at each (30-, 60- 90-day) time point. Previous literature indicates that surgical- related infections, cardiovascular events and wound or joint problems are common reasons for readmission following joint replacement surgery.16, 18 Commonly cited reasons for hospital readmission at 30 or 90 days include problems associated with the joint replacement procedure itself (infection or stiffness)16, 18–21 or respiratory or cardiovascular events.9, 20 Kurtz et al. recently showed that a majority of both 30- and 90-day readmissions occur for similar reasons: wound or deep infections, atrial fibrillation, cellulitis and abscess, or pulmonary embolism.17 Our study stratified the 10 most prevalent MS-DRGs by discharge setting (IRF, SNF and community) and found commonalities at all three discharge settings and time categories. Gastrointestinal and cardiovascular conditions were observed for all three time periods and settings. We also found that post-operative infections were most common within in the first 30 days; however, the prevalence decreased during days 31–60 and was no longer present at days 61–90. As episodic (bundled) payment programs and shared accountability initiatives continue to replace the current fee-for-service payment systems, providers will certainly want to know the common reasons for future hospital admissions among patient subgroups in order to align the appropriate resources and personnel to minimize that risk.
This study builds on the current body of knowledge on the rates and causes of readmission following TKA. The advantages of our study over previous studies include our large and representative sample from the 100% Medicare files, the use of a standardized comorbidity index which include 17 conditions,28 and the inclusion of the three most common post-acute discharge settings following TKA to determine the relationships between settings and hospital readmission. This study investigated patient, clinical and facility level variables for their impact on recent policy changes affecting TKA beneficiaries such as the hospital readmission reduction program1 and the CJR model.7, 8
We also acknowledge several limitations in our study. Study findings are only generalizable to Medicare Fee-for-Service beneficiaries 66 years and older. Another limitation is the potential for coding errors in claims data, which can lead to misdiagnosis, false identification of complications and comorbidities, or under-reporting of comorbid conditions.35–37 While we accounted for comorbidity as an aggregate variable, we did not account for or examine specific comorbidities or their effect on hospital readmission. We differentiated planned from unplanned readmissions using established criteria in the hospital-wide readmission measure, but we did not try to distinguish potentially preventable from non-preventable readmissions, which would better reflect opportunities for quality improvement. Our community outcome variable combines patients discharged with and without home health recommendations, and does not capture outpatient rehabilitation services. Lastly, we do not have information on other community based services or the quality of family support, which may help older adults remain in the community and avoiding re-hospitalization.
This study adds to our understanding of the rates of and reasons for hospital readmission following TKA in the Medicare population, specifically the influence of post-acute discharge setting on readmission. We found community discharge following TKA is associated with lower odds of 30-day readmission and lower risk of readmission up to 90 days. Also, IRF and SNF show similarly higher trends of readmission. We know from previous literature that differences in patient functional status, comorbidity and support systems following TKA38–40 can influence post-acute discharge setting. In turn, these factors are also associated with readmission risk. Therefore, as the number of TKA procedures continues to grow12 and with current initiatives to reduce hospital readmissions and costs associated with TKA in the Medicare population,1, 6 more information on the potential influences of initial discharge setting on reducing readmission risks is needed. Further studies on functional status, different combinations of comorbidities, and living situation and/or support systems may improve our ability to identify high-risk patients prior to discharge. Our current findings can be useful to help healthcare practitioners, hospital administrators, payers and patients better understand what factors are associated with hospital readmission following TKA, so as to target modifications to reduce risk.
Acknowledgments
This study was supported in part by grants from the National Institutes of Health (XXX) and the National Institute on Disability, Independent Living, and Rehabilitation Research (XXX). The content is solely the responsibility of the authors and does not necessarily represent the views of the funding agencies. The agencies did not influence the design, analysis or interpretation of the study results.
Funding: This study was supported in part by grants from the National Institutes of Health (P2C HD065702; R01 HD069443; K01 HD086290) and the National Institute on Disability, Independent Living, and Rehabilitation Research (90IF0071).
Appendix A.
Top 10 MS-DRG codes for hospital readmission between 1–30 days by discharge setting.
| DRG | N | % | Label | |
|---|---|---|---|---|
| Community | 863 | 879 | 6.12% | Postoperative & post-traumatic infections w/o mcc |
| 176 | 644 | 4.48% | Pulmonary embolism w/o mcc | |
| 392 | 560 | 3.90% | Esophagitis, gastrointestinal & miscellaneous digestive disorders w/o mcc | |
| 603 | 455 | 3.17% | Cellulitis w/o mcc | |
| 560 | 392 | 2.73% | Aftercare, musculoskeletal system & connective tissue w cc | |
| 310 | 378 | 2.63% | Cardiac arrhythmia & conduction disorders w/o cc/mcc | |
| 641 | 366 | 2.55% | Miscellaneous disorders of nutrition, metabolism, fluids/electrolytes w/o mcc | |
| 312 | 334 | 2.33% | Syncope & collapse | |
| 378 | 329 | 2.29% | Gastrointestinal hemorrhage w cc | |
| 300 | 302 | 2.10% | Peripheral vascular disorders w cc | |
|
| ||||
| SNF | 863 | 707 | 5.09% | Postoperative & post-traumatic infections w/o mcc |
| 603 | 448 | 3.22% | Cellulitis w/o mcc | |
| 392 | 438 | 3.15% | Esophagitis, gastrointestinal & miscellaneous digestive disorders w/o mcc | |
| 812 | 427 | 3.07% | Red blood cell disorders w/o mcc | |
| 176 | 352 | 2.53% | Pulmonary embolism w/o mcc | |
| 378 | 343 | 2.47% | Gastrointestinal hemorrhage w cc | |
| 641 | 297 | 2.14% | Miscellaneous disorders of nutrition, metabolism, fluids/electrolytes w/o mcc | |
| 560 | 292 | 2.10% | Aftercare, musculoskeletal system & connective tissue w cc | |
| 871 | 290 | 2.09% | Septicemia or severe sepsis w/o mv 96+ hours w mcc | |
| 310 | 288 | 2.07% | Cardiac arrhythmia & conduction disorders w/o cc/mcc | |
|
| ||||
| IRF | 863 | 205 | 3.81% | Postoperative & post-traumatic infections w/o mcc |
| 310 | 190 | 3.53% | Cardiac arrhythmia & conduction disorders w/o cc/mcc | |
| 176 | 170 | 3.16% | Pulmonary embolism w/o mcc | |
| 392 | 166 | 3.08% | Esophagitis, gastrointestinal & miscellaneous digestive disorders w/o mcc | |
| 603 | 141 | 2.62% | Cellulitis w/o mcc | |
| 309 | 135 | 2.51% | Cardiac arrhythmia & conduction disorders w cc | |
| 641 | 129 | 2.40% | Miscellaneous disorders of nutrition, metabolism, fluids/electrolytes w/o mcc | |
| 312 | 117 | 2.17% | Syncope & collapse | |
| 378 | 102 | 1.90% | Gastrointestinal hemorrhage w cc | |
| 812 | 96 | 1.78% | Red blood cell disorders w/o mcc | |
W, With; W/O, Without; CC, Complicating or Comorbid Condition; MCC, Major Complicating or Comorbid Condition; MV, Mechanical Ventilation.
Appendix B.
Top 10 MS-DRG codes for hospital readmission between 31–60 days by discharge setting.
| DRG | N | % | Label | |
|---|---|---|---|---|
| Community | 392 | 298 | 5.51% | Esophagitis, gastrointestinal & miscellaneous digest disorders w/o mcc |
| 310 | 157 | 2.90% | Cardiac arrhythmia & conduction disorders w/o cc/mcc | |
| 176 | 124 | 2.29% | Pulmonary embolism w/o mcc | |
| 603 | 121 | 2.24% | Cellulitis w/o mcc | |
| 863 | 114 | 2.11% | Postoperative & post-traumatic infections w/o mcc | |
| 378 | 106 | 1.96% | Gastrointestinal hemorrhage w cc | |
| 554 | 106 | 1.96% | Bone diseases & arthropathies w/o mcc | |
| 312 | 100 | 1.85% | Syncope & collapse | |
| 561 | 100 | 1.85% | Aftercare, musculoskeletal system & connective tissue w/o cc/mcc | |
| 641 | 99 | 1.83% | Miscellaneous disorders of nutrition, metabolism, fluids/electrolytes w/o mcc | |
|
| ||||
| SNF | 392 | 317 | 4.72% | Esophagitis, gastrointestinal & miscellaneous digest disorders w/o mcc |
| 603 | 190 | 2.84% | Cellulitis w/o mcc | |
| 690 | 178 | 2.65% | Kidney & urinary tract infections w/o mcc | |
| 641 | 159 | 2.37% | Miscellaneous disorders of nutrition, metabolism, fluids/electrolytes w/o mcc | |
| 871 | 144 | 2.14% | Septicemia or severe sepsis w/o mv 96+ hours w mcc | |
| 863 | 129 | 1.92% | Postoperative & post-traumatic infections w/o mcc | |
| 310 | 128 | 1.90% | Cardiac arrhythmia & conduction disorders w/o cc/mcc | |
| 372 | 127 | 1.89% | Major gastrointestinal disorders & peritoneal infections w cc | |
| 176 | 126 | 1.87% | Pulmonary embolism w/o mcc | |
| 312 | 118 | 1.76% | Syncope & collapse | |
|
| ||||
| IRF | 392 | 119 | 4.58% | Esophagitis, gastrointestinal & miscellaneous digest disorders w/o mcc |
| 603 | 72 | 2.77% | Cellulitis w/o mcc | |
| 310 | 58 | 2.23% | Cardiac arrhythmia & conduction disorders w/o cc/mcc | |
| 312 | 56 | 2.16% | Syncope & collapse | |
| 690 | 55 | 2.12% | Kidney & urinary tract infections w/o mcc | |
| 292 | 52 | 2.00% | Heart failure & shock w cc | |
| 863 | 52 | 2.00% | Postoperative & post-traumatic infections w/o mcc | |
| 641 | 51 | 1.96% | Miscellaneous disorders of nutrition, metabolism, fluids/electrolytes w/o mcc | |
| 871 | 47 | 1.81% | Septicemia or severe sepsis w/o mv 96+ hours w mcc | |
| 309 | 45 | 1.73% | Cardiac arrhythmia & conduction disorders w cc | |
W, With; W/O, Without; CC, Complicating or Comorbid Condition; MCC, Major Complicating or Comorbid Condition; MV, Mechanical Ventilation.
Appendix C.
Top 10 MS-DRG codes for hospital readmission between 61–90 days by discharge setting.
| DRG | N | % | Label | |
|---|---|---|---|---|
| Community | 392 | 155 | 3.86% | Esophagitis, gastrointestinal & miscellaneous digest disorders w/o mcc |
| 310 | 105 | 2.61% | Cardiac arrhythmia & conduction disorders w/o cc/mcc | |
| 378 | 88 | 2.19% | Gastrointestinal hemorrhage w cc | |
| 176 | 82 | 2.04% | Pulmonary embolism w/o mcc | |
| 603 | 74 | 1.84% | Cellulitis w/o mcc | |
| 292 | 68 | 1.69% | Heart failure & shock w cc | |
| 312 | 65 | 1.62% | Syncope & collapse | |
| 690 | 61 | 1.52% | Kidney & urinary tract infections w/o mcc | |
| 287 | 60 | 1.49% | Circulatory disorders except acute myocardial infarction, w cardiac catheterization w/o mcc | |
| 641 | 60 | 1.49% | Miscellaneous disorders of nutrition, metabolism, fluids/electrolytes w/o mcc | |
|
| ||||
| SNF | 392 | 178 | 3.67% | Esophagitis, gastrointestinal & miscellaneous digest disorders w/o mcc |
| 871 | 127 | 2.62% | Septicemia or severe sepsis w/o mv 96+ hours w mcc | |
| 603 | 125 | 2.58% | Cellulitis w/o mcc | |
| 690 | 120 | 2.47% | Kidney & urinary tract infections w/o mcc | |
| 292 | 110 | 2.27% | Heart failure & shock w cc | |
| 310 | 84 | 1.73% | Cardiac arrhythmia & conduction disorders w/o cc/mcc | |
| 641 | 82 | 1.69% | Miscellaneous disorders of nutrition, metabolism, fluids/electrolytes w/o mcc | |
| 312 | 80 | 1.65% | Syncope & collapse | |
| 552 | 77 | 1.59% | Medical back problems w/o mcc | |
| 293 | 71 | 1.46% | Heart failure & shock w/o cc/mcc | |
|
| ||||
| IRF | 690 | 48 | 2.59% | Kidney & urinary tract infections w/o mcc |
| 392 | 46 | 2.48% | Esophagitis, gastrointestinal & miscellaneous digest disorders w/o mcc | |
| 312 | 40 | 2.16% | Syncope & collapse | |
| 603 | 38 | 2.05% | Cellulitis w/o mcc | |
| 292 | 34 | 1.83% | Heart failure & shock w cc | |
| 293 | 34 | 1.83% | Heart failure & shock w/o cc/mcc | |
| 481 | 31 | 1.67% | Hip & femur procedures except major joint w cc | |
| 310 | 29 | 1.57% | Cardiac arrhythmia & conduction disorders w/o cc/mcc | |
| 313 | 29 | 1.57% | Chest pain | |
| 871 | 29 | 1.57% | Septicemia or severe sepsis w/o mv 96+ hours w mcc | |
W, With; W/O, Without; CC, Complicating or Comorbid Condition; MCC, Major Complicating or Comorbid Condition; MV, Mechanical Ventilation.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors report no conflicts of interest.
Contributor Information
Rodney Laine Welsh, Assistant Professor, University of Texas Medical Branch – Occupational Therapy, 301 University Blvd, Galveston, Tx. 77555-1142, (409) 772-3060 (office), (409) 747-1615 (fax).
James Graham, Associate Professor, University of Texas Medical Branch – Rehabilitation Sciences, 301 University Blvd, Galveston, Tx. 77555 – 1137, (409) 747-1637.
Amol Karmarkar, Assistant Professor, University of Texas Medical Branch – Rehabilitation Sciences.
Natalie Leland, Assistant Professor, University of South California – Occupational Science & Occupational Therapy.
Jacques G. Baillargeon, Professor, University of Texas Medical Branch – Preventative Medicine & Community Health.
Dana Wild, Associate Professor, University of Texas Medical Branch – Physical Therapy.
Kenneth Ottenbacher, Professor, University of Texas Medical Branch – Rehabilitation Sciences.
References
- 1.Centers for Medicare & Medicaid Services. Readmissions Reduction Program. Available at: https://www.cms.gov/medicare/medicare-fee-for-service-payment/acuteinpatientpps/readmissions-reduction-program.html. Accessed September 4, 2015.
- 2.HR 3590 - 111th Congress: Patient Protection and Affordable Care Act. 2009 Available at: https://www.congress.gov/bill/111th-congress/house-bill/3590. Accessed August 15, 2014.
- 3.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360(14):1418–28. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 4.Schmidt PL. Medicare and the Patient Protection and Affordable Care Act Health Care Issues, Costs, and Access. Hauppauge, NY: Nova Science Publishers; 2011. [Google Scholar]
- 5.Gage B, Morley M, Spain P, Ingber M. Examining post acute care relationships in an integrated hospital system. Washington (DC): Centers for Medicare & Medicaid Services, Department of Health and Human Services; 2009. p. 118. [Google Scholar]
- 6.Centers for Medicare & Medicaid Services. Bundled Payments for Care Improvement (BPCI) Initiative: General Information. Available at: https://innovation.cms.gov/initiatives/bundled-payments. Accessed September 6, 2015.
- 7.Centers for Medicare & Medicaid Services. Comprehensive care for joint replacement model. doi: 10.3928/01477447-20170302-03. Available at: https://innovation.cms.gov/initiatives/ccjr. Accessed September 12, 2015. [DOI] [PubMed]
- 8.Centers for Medicare and Medicaid Services. Medicare Program: Comprehensive care for joint replacement payment model for acute care hospitals furnishing lower extremity joint replacement services. Federal Register. 2015 Jul 14; Available at: https://www.federalregister.gov/articles/2015/07/14/2015-17190/medicare-program-comprehensive-care-for-joint-replacement-payment-model-for-acute-care-hospitals. Accessed September 12, 2015. [PubMed]
- 9.Vorhies JS, Wang Y, Herndon JH, et al. Decreased length of stay after TKA is not associated with increased readmission rates in a national Medicare sample. Clin Orthop Relat Res. 2012;470(1):166–71. doi: 10.1007/s11999-011-1957-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ottenbacher KJ, Graham JE, Ottenbacher AJ, et al. Hospital readmission in persons with stroke following postacute inpatient rehabilitation. J Gerontol A Biol Sci Med Sci. 2012;67(8):875–81. doi: 10.1093/gerona/glr247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cram P, Lu X, Kates SL, et al. Total knee arthroplasty volume, utilization, and outcomes among Medicare beneficiaries, 1991–2010. JAMA. 2012;308(12):1227–36. doi: 10.1001/2012.jama.11153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kurtz SM, Lau E, Ong K, et al. Future young patient demand for primary and revision joint replacement: national projections from 2010 to 2030. Clin Orthop Relat Res. 2009;467(10):2606–12. doi: 10.1007/s11999-009-0834-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Buntin MB. Access to postacute rehabilitation. Arch Phys Med Rehabil. 2007;88(11):1488–93. doi: 10.1016/j.apmr.2007.07.023. [DOI] [PubMed] [Google Scholar]
- 14.Ramos NL, Karia RJ, Hutzler LH, et al. The effect of discharge disposition on 30-day readmission rates after total joint arthroplasty. J Arthroplasty. 2014;29(4):674–7. doi: 10.1016/j.arth.2013.09.010. [DOI] [PubMed] [Google Scholar]
- 15.Bini SA, Fithian DC, Paxton LW, et al. Does discharge disposition after primary total joint arthroplasty affect readmission rates? J Arthroplasty. 2010;25(1):114–7. doi: 10.1016/j.arth.2008.11.007. [DOI] [PubMed] [Google Scholar]
- 16.Zmistowski B, Restrepo C, Hess J, et al. Unplanned readmission after total joint arthroplasty: rates, reasons, and risk factors. J Bone Joint Surg Am. 2013;95(20):1869–76. doi: 10.2106/JBJS.L.00679. [DOI] [PubMed] [Google Scholar]
- 17.Kurtz SM, Lau EC, Ong KL, et al. Which hospital and clinical factors drive 30- and 90-day readmission after TKA? J Arthroplasty. 2016 doi: 10.1016/j.arth.2016.03.045. [DOI] [PubMed] [Google Scholar]
- 18.Schairer WW, Vail TP, Bozic KJ. What are the rates and causes of hospital readmission after total knee arthroplasty? Clin Orthop Relat Res. 2014;472(1):181–7. doi: 10.1007/s11999-013-3030-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Saucedo JM, Marecek GS, Wanke TR, et al. Understanding readmission after primary total hip and knee arthroplasty: who’s at risk? J Arthroplasty. 2014;29(2):256–60. doi: 10.1016/j.arth.2013.06.003. [DOI] [PubMed] [Google Scholar]
- 20.Pugely AJ, Callaghan JJ, Martin CT, et al. Incidence of and risk factors for 30-day readmission following elective primary total joint arthroplasty: analysis from the ACS-NSQIP. J Arthroplasty. 2013;28(9):1499–504. doi: 10.1016/j.arth.2013.06.032. [DOI] [PubMed] [Google Scholar]
- 21.Raines BT, Ponce BA, Reed RD, et al. Hospital acquired conditions are the strongest predictor for early readmission: an analysis of 26,710 arthroplasties. J Arthroplasty. 2015;30(8):1299–307. doi: 10.1016/j.arth.2015.02.024. [DOI] [PubMed] [Google Scholar]
- 22.Mesko NW, Bachmann KR, Kovacevic D, et al. Thirty-day readmission following total hip and knee arthroplasty - a preliminary single institution predictive model. J Arthroplasty. 2014;29(8):1532–8. doi: 10.1016/j.arth.2014.02.030. [DOI] [PubMed] [Google Scholar]
- 23.Singh JA, Inacio MC, Namba RS, Paxton EW. Rheumatoid arthritis is associated with higher ninety-day hospital readmission rates compared to osteoarthritis after hip or knee arthroplasty: a cohort study. Arthritis Care Res. 2015;67(5):718–24. doi: 10.1002/acr.22497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Centers for Disease Control and Prevention, National Center for Health Statistics. International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) 6th. Los Angeles: Practice Management Information Corporation; 2000. [Google Scholar]
- 25.Yale New Haven Health Services Corporation, Center for Outcomes Research & Evaluation. Measure Updates and Specifications Report Hospital-Wide All-Cause Unplanned Readmission – Version 3.0. 2014 Available at: altarum.org/sites/default/files/uploaded-publication-files/Rdmsn_Msr_Updts_HWR_0714_0.pdf. Accessed November 5, 2015. [Google Scholar]
- 26.Research Data Distribution Center. Medicare Provider Analysis And Review (MEDPAR) Record, Data Dictionary For SAS and CSV Datasets. Available at: http://ftp.cdc.gov/pub/Health_Statistics/NCHS/datalinkage/medpar%20(edited).pdf. Accessed March 2, 2015.
- 27.Agency for Healthcare Research and Quality, Rockville, MD. Creation of New Race-Ethnicity Codes and Socioeconomic Status (SES) Indicators for Medicare Beneficiaries. 2014 Dec; Available at: http://www.ahrq.gov/research/findings/final-reports/medicareindicators/index.html. Assessed August 19, 2015.
- 28.Charlson ME, Pompei P, Ales KL, Mackenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J Chronic Dis. 1987;40(5):373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 29.Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43(11):1130–1139. doi: 10.1097/01.mlr.0000182534.19832.83. [DOI] [PubMed] [Google Scholar]
- 30.Losina E, Walensky R, Kessler C, et al. Cost-effectiveness of total knee arthroplasty in the United States: patient risk and hospital volume. Arch Intern Med. 2009;169(12):1113–21. doi: 10.1001/archinternmed.2009.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Katz JN, Barrett J, Mahomed NN, et al. Association between hospital and surgeon procedure volume and the outcomes of total knee replacement. J Bone Joint Surgery Am. 2004;86(9):1909–16. doi: 10.2106/00004623-200409000-00008. [DOI] [PubMed] [Google Scholar]
- 32.Taylor HD, Dennis DA, Crane HS. Relationship between mortality rates and hospital patient volume for medicare patients undergoing major orthopaedic surgery of the hip, knee, spine, and femur. J Arthroplasty. 1997;12(3):235–42. doi: 10.1016/s0883-5403(97)90018-8. [DOI] [PubMed] [Google Scholar]
- 33.Katz JN, Mahomed NN, Baron JA, et al. Association of hospital and surgeon procedur volume with patient-centered outcomes of total knee replacement in a population-based cohort of patients age 65 years and older. Arthritis Rheum. 2007;56(2):568–74. doi: 10.1002/art.22333. [DOI] [PubMed] [Google Scholar]
- 34.Blyth C, Still H. Binomial confidence intervals. J Am Stat Assoc. 1983;78(381):108–16. [Google Scholar]
- 35.Cram P, Cai X, Lu X, et al. Total knee arthroplasty outcomes in top-ranked and non-top-ranked orthopedic hospitals: an analysis of Medicare administrative data. Mayo Clin Proc. 2012;87(4):341–8. doi: 10.1016/j.mayocp.2011.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Menendez M, Neuhaus V, van Dijk CN, Ring D. The Elixhauser comorbidity method outperforms the Charlson index in predicting inpatient death after orthopaedic surgery. Clin Orthop Relat Res. 2014;472(9):2878–86. doi: 10.1007/s11999-014-3686-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Keeney JA, Adelani MA, Nunley RM, et al. Assessing readmission databases: how reliable is the information? J Arthroplasty. 2012;27(8, Suppl):72–6. doi: 10.1016/j.arth.2012.03.032. [DOI] [PubMed] [Google Scholar]
- 38.Barsoum WK, Murray TG, Klika AK, et al. Predicting patient discharge disposition after total joint arthroplasty in the United States. J Arthroplasty. 2010;25(6):885–92. doi: 10.1016/j.arth.2009.06.022. [DOI] [PubMed] [Google Scholar]
- 39.Munin MC, Kwoh CK, Glynn N, et al. Predicting discharge outcome after elective hip and knee arthoplasty. Am J Phys Med Rehabil. 1995;74(4):294–301. doi: 10.1097/00002060-199507000-00006. [DOI] [PubMed] [Google Scholar]
- 40.Oldmeadow LB, McBurney H, Robertson VJ, et al. Targeted postoperative care improves discharge outcome after hip or knee arthroplasty. Arch Phys Med Rehabil. 2004;85(9):1424–7. doi: 10.1016/j.apmr.2003.12.028. [DOI] [PubMed] [Google Scholar]


