Abstract
Aims
This paper examined longitudinal marijuana use trajectories among drug-using youth presenting to the ED to inform intervention development.
Methods
Given interest in substance use and violence, this study oversampled those presenting with assault injuries. Assault-injured youth (ages 14-24) endorsing past 6-month drug use (n=349), and a sex and age proportionally-sampled comparison group (n=250) endorsing drug use, completed a baseline assessment and follow-ups at 6, 12, 18, and 24 months. Latent class trajectory analyses examined days of marijuana use over 2 years. Multinomial regression analyses examined baseline, 12-month and 24-month factors associated with substance use trajectory groups.
Results
Trajectory analyses identified 5 groups: Low (Low; 28.2%; n=169); Intermittent (INT; 16.2%; n=97); Moderate Decline (MD; 12.0%; n=72); High decline (HD, 13.2%; n=79) and Chronic (C; 30.4%; n=182). At baseline, as compared to the Low group, the other trajectory groups were more likely to be male and have greater levels of physical aggression. At 12- and 24-months, negative and positive peer influences, incarceration and community violence were additional characteristics associated with the greater marijuana use trajectories (as compared to the Low group).
Conclusions
Interventions for drug-using youth presenting to the urban ED should address peer influences, physical aggression and community violence exposure, given the association between these characteristics and greater marijuana use trajectories.
Keywords: marijuana use, youth, violence, latent class trajectory analysis, peer influence
1.0 Introduction
There is a critical need to understand marijuana use trajectories among youth residing in socio-economically disadvantaged communities. Marijuana is the most commonly used illicit drug used during adolescence (Substance Abuse and Mental Health Service Administration, 2014b), with use adversely affecting neuromaturation of the vulnerable adolescent brain (Gruber et al., 2012; Lopez-Larson et al., 2011; Schepis et al., 2011). Marijuana use during adolescence places youth at increased risk for motor vehicle crash (Maxwell, 2012; Naimi et al., 2003; Quinlan et al., 2005; Wilhelmi and Cohen, 2012), and other drug use (Center for Disease Control and Prevention, 2012; Center for Lawful Access and Abuse Deterrence, 2011; Schillie et al., 2009; Substance Abuse and Mental Health Service Administration, 2013; White et al., 2013a) The emergency department (ED) provides a useful setting to identify at-risk youth and initiate substance use interventions (Cunningham et al., 2009).
Based on social ecological and resiliency theories (Bronfrenbrenner, 1998; Garmezy, 1991; Rutter, 1987; Stokols et al., 1996), marijuana use during adolescence and emerging adulthood is associated with evolving interactions between individual and social risk and promotive factors that can decrease or accelerate problem trajectories (Abadi et al., 2011; Bernstein et al., 2011; Brown et al., 2008; Cadoret et al., 1995; Cleveland and Wiebe, 2008; Fowler et al., 2007; Henry and Thornberry, 2010; Hussong et al., 2008; Mrug et al., 2010; Wagner, 2008; Windle et al., 2008; Zucker et al., 2000; Zucker et al., 2008). For example, violence is associated with substance use, particularly among those residing in socio-economically disadvantaged communities (Goldstick et al., 2015; Goldstick et al., 2016; Walton et al., 2009; White et al., 2009), likely due to shared risk and promotive factors for some substances (e.g., marijuana), and/or acute pharmacological effects of substances (e.g., alcohol) (Chermack and Giancola, 1997; White et al., 2009). Although parental influences are important during younger ages, peers are the most robust influence for substance use during the transition to adulthood (Abadi et al., 2011; Allen et al., 2012; Brechwald and Prinstein, 2011; Burk et al., 2012; Chein et al., 2011; Dziak et al., 2014; Simons-Morton and Farhat, 2010; Wolfe et al., 2012), increasing exposure to deviant social contexts and distancing youth from protective influences.
Latent trajectory analysis is a useful approach to identifying heterogeneity in trajectories of substance use (Nagin and Tremblay, 2005; Skardhamar, 2010), with groupings providing an opportunity to examine characteristics that can inform interventions (Brame et al., 2012). Prior research examining marijuana use trajectories are relatively rare. For example, a longitudinal study of youth from a socio-economically disadvantaged community (Brook et al., 2011) found four groups of marijuana users (low users, decreasing, increasing, and chronic), whereas Schulenberg and colleagues (2005) used Monitoring the Future (MTF) data to identify six marijuana use trajectory groups (i.e., chronic, decreased, increased, fling, rare, and abstain). Chronic users are more likely to be male, with the greatest constellation of risk factors including externalizing (e.g., delinquency, impulsivity, and substance use) and internalizing problems (Brook et al., 2011; Chassin et al., 2004; Jackson et al., 2008; Meier et al., 2013). Baseline factors that distinguish chronic users from decreasing or late onset users are less evident, with one study finding greater negative affect among the late onset group (Brook et al., 2011; Meier et al., 2013). Other researchers find that decreasing users are initially similar to chronic users, but over time had less substance use, delinquency and peers who used marijuana (Schulenberg et al., 2005); in contrast, increasing users are most likely to use other substances, use marijuana to cope, have drug-using friends, and report delinquency (Schulenberg et al., 2005). Although aggression is related to alcohol use during adolescence (White et al., 2013b; White et al., 2009), few studies have examined marijuana use in relation to violence, with one study finding that increasing users show more persistent physical aggression (Schulenberg et al., 2005). It is unclear how these findings generalize to youth presenting to urban EDs, with generally much lower socio-economic status and greater minority representation.
The current study examined longitudinal marijuana use trajectories among youth presenting for care at an urban ED. The ED is an important contact point for medical care for youth at high risk for substance use and violence, especially the underinsured and uninsured, with ED patients over-representing socially disadvantaged minority groups (Albert and McCaig, 2014). Further, the ED provides a location to access adolescents, who are often missed in school-based studies because of poor attendance (Grove et al., 2000; Ramirez et al., 2012; Wilson and Klein, 2000). Most patients (>90%) seeking ED care are treated and released (Albert and McCaig, 2014), which is consistent with studies demonstrating the receptivity of patients to ED-based interventions (Walton et al., 2012; Cunningham et al., 2015).
The purpose of this study was to examine factors associated with greater marijuana use trajectories to inform intervention development for drug-using youth presenting to urban EDs, with this study enrolling patients with past 6 month drug use, oversampling those presenting with assault injuries (Bohnert et al., 2015). Prior papers showed that assault-injured youth had increased rates of ED visits for violent injury, which was related to having a drug use disorder (Cunningham et al., 2015). First, this paper presents findings from latent trajectory analysis to identify subgroups of marijuana users two-years post-ED visit. Second, we characterize risk and promotive factors associated with these groupings at baseline, and at 12- and 24-months to inform interventions. For example, if the relationship between time-varying factors is consistent over time, then baseline screening could indicate the need for initiating interventions in the ED, with extended interventions addressing influences over time. In contrast, if the factors associated with trajectories varied over time, then adaptive interventions may be indicated to address these changing factors (Lei et al., 2012; Rich et al., 2014). Hypothesized factors associated with greater marijuana use trajectories included: male gender and older age; greater involvement with violence (assault injury, physical aggression, physical victimization, community violence) and negative peer influences; less involvement with positive peers, substance use treatment, and the criminal justice system. Also, we hypothesized that greater marijuana use trajectories would be: consistently related to peer influences over time, reflecting their importance during adolescence and emerging adulthood, and community violence, reflecting the urban setting in which youth likely remain; less strongly associated with interpersonal violence (aggression and victimization) over time, reflecting developmental trends for decreased involvement with violence during the transition to emerging adulthood; and, inconsistently related to incarceration and drug treatment over time, particularly given expected low rates of receipt of treatment services.
2.0 Material and Methods
2.1 Design
Data were collected for the Flint Youth Injury Study (Bohnert et al., 2015; Cunningham et al., 2015; Cunningham et al., 2014), which is a longitudinal study with assessments during the ED visit and over 24-months. Flint, Michigan has similar crime rates to other urban centers (Federal Bureau of Investigation, 2011). Youth presenting for an assault injury were oversampled (n=349), and proportionally balanced by age (ages 14-17; 18-20; 21-24) and sex with youth presenting for other reasons (n=250). The study was approved by university and hospital IRBs; a NIH Certificate of Confidentiality was obtained.
2.2 Setting and Sample
Following written assent/consent (parental consent if age <18 years), patients (ages 14-24) presenting to the ED for an assault injury, and a proportionally sampled group presenting for other reasons self-administered a computerized survey (assault patients admitted to the hospital were recruited if they stabilized within 72 hours). Exclusions were presentation for acute sexual assault, child maltreatment, suicidal ideation/attempt, or inability to provide consent (e.g., altered mental status).
2.3 Procedures
Youth reporting past six-month drug use on the Alcohol, Smoking, and Substance use Involvement Screening Test [ASSIST; marijuana, other illicit drugs (i.e., cocaine, inhalants, Sent to street opioids, other) or non-medical use of prescription drugs (i.e., opioids, sedative, stimulants)](Humeniuk et al., 2008; National Institute on Drug Abuse, 2010; WHO ASSIST Working Group, 2002) were eligible for the study. Alcohol and tobacco use were not inclusion criteria. Eligible youth provided assent/consent (parental consent if age <18 years), and completed a ∼90-minute baseline assessment ($20 remuneration, plus $5 for urine sample for drug testing). In-person follow-up assessments were conducted at 6-, 12-, 18-, and 24-months [remuneration: $35, $40, $40, and $50 respectively, including urine samples).
2.4 Measures
2.4.1 Demographics
Age, sex, race, education, marital status, school drop-out (past 6-month not in school or complete high school) and past 6-month self/family receipt of public assistance were collected (Cunningham et al., 2014).
2.4.2 Substance Use
Substance use was assessed using the Time Line Follow Back (TLFB) (Chermack et al., 2010; Epstein-Ngo et al., 2013; Hjorthoj et al., 2012; Sobell et al., 1988) for the past 30 days at baseline and for the past 90 days at follow-ups. For latent trajectory analyses, the number of days of marijuana use was summed for each assessment.
2.4.3 Violence
Past 6-month violence was assessed using a modified version of the physical assault scale of the Conflict Tactics Scale 2 (Straus et al., 1996), assessing: a) frequency of moderate and severe physical victimization (someone did to you); and, b) physical aggression (you did to someone else). Aggression and victimization were assessed separately for dating partners (e.g., girlfriend/boyfriend, husband/wife) and peers (e.g., non-partners: friend, stranger, acquaintance, etc.); responses ranged from 0 (never) to 6 (20 times or more). Peer and dating items were summed for a total score (physical aggression α = .0.90; physical victimization α = .0.93). Community violence exposure in the past 6 months included five items assessing frequency of witnessed neighborhood behaviors (e.g., heard gun shots, saw drug deals, had their homes broken into, saw gangs in the neighborhood, saw someone getting stabbed or shot) (Richters and Martinez, 1992), ranging from “never” (0) to “many times” (3) (range 0 -15; α = .0.73).
2.4.4 Drug Treatment Criminal Justice Involvement
Participants were asked the number of days they were incarcerated in the past 6 months (McLellan et al., 1992). Similarly, past 6-month substance use treatment was assessed with a single item (McLellan et al., 1992).
2.4.5 Other Risk and Promotive Factors
Negative peer influences assessed how many of their friends were currently involved in negative activities (e.g., use substances, sell drugs, fight, carry weapons, shoplifting/busted for burglary/robbery) (Ostaszewski and Zimmerman, 2006) (range 7-35; α = 0.81). Positive peer influences assessed how many of their friends were currently involved in positive activities (e.g., good grades, attend church, school clubs or community activities, plans to go to college; range 4-20; α = 0.75).
2.5 Data Analyses
Data were analyzed with R version 3.2.3. Using the R package flexmix (Grun and Leisch, 2008; Leisch, 2004), we modeled marijuana use days across the five time points using latent trajectory analysis. Because the outcome variable is a count, we specified a Poisson distribution for the outcome; an offset for the log of the number of days in the substance use calendar was used, to account for different follow-back periods at baseline (past 30 days) vs. follow-ups (past 90 days at each assessment); thus, the fitted model is effectively equivalent to modeling the % of use days (i.e., number of use days per days assessed). A cubic polynomial was used to model the time-varying rate on the log scale. This specification is capable of capturing most plausible patterns of change over five time points, and uses fewer parameters than estimating separate coefficients for each time point. Following convention (Nylund et al., 2007), we used the Bayesian information criterion (BIC), in conjunction with considerations of parsimony and interpretability, to select the number of groups. To ensure a parsimonious solution that does not over fit the data, as well as ensuring large enough groups to make between-group comparisons, we imposed the constraint that each group must have a prior probability of at least 0.10 (corresponding to 60 individuals); this constraint operated within the fitting process so that, for a given number of input classes, the fitted model is that which maximizes the likelihood subject to the aforementioned constraint; in some cases the optimal solution may have fewer than the nominal number of input classes. To guard against model convergence to local maximums, the model was re-fit from 200 random starting values for each number of input classes and the model corresponding to the maximum converged likelihood was saved. To evaluate class separation, we calculated the relative entropy of the posterior probability distribution, with a value of 0.8 indicating acceptable separation between classes (Ram and Grimm, 2009). After assigning participants to the group in which they had the greatest posterior probability of membership, we compared the model-estimated rates with the empirical rates in each group to verify acceptable within-group fit.
We used regression analyses to examine the associations between trajectory membership and factors assessed at baseline, 12, and 24 months, with descriptive data also provided to aid with interpretation of regression models. We included time invariant measures of age, sex, and assault injury in regression analyses; we included all other time-varying variables in regression analyses except physical victimization (which was highly correlated with physical aggression at baseline; r=0.66), prioritizing variables that would inform interventions in terms of sample (i.e., assault injury) and content (i.e., physical aggression, community violence). The outcome, predicted trajectory class, is not changing across the baseline, 12- and 24-month analyses; however, time-invariant associations (e.g., age, male) vary across the models due to differences in the time-varying factors and participants that are simultaneously included (i.e., n=599 at baseline; n=502 at 12-months; n=512 at 24-months). While we have ascribed labels to the groups identified, we want to emphasize latent trajectory analysis as a model-based tool for detecting, and describing, heterogeneity in trajectories of marijuana use over the study period, rather than as an immutable typology of individuals (Nagin and Tremblay, 2005; Skardhamar, 2010). This descriptive, rather than endogenous, interpretation of the groupings partially justifies our examination of 12- and 24-month correlates of trajectory groups, which may inform interventions aims at disrupting a deleterious trajectory (Brame et al., 2012).
3.0 Results
3.1 Descriptive Characteristics
At baseline, 58.8% were male, the mean age was 20.1 (standard deviation=2.4), 28% were living with a partner, 40% had at least one child, most received public assistance (73.0%), and were African-American (58.3%; 32.5% Caucasian, 9.3% other); 5.8% reported Hispanic ethnicity. Follow-up rates were: 85.3% (6-months), 83.7% (12-months), 84.2% (18-months) and 85.3% (24-months).
3.2 Marijuana Use Trajectory Groups
Examination of the BIC scores resulted in strong evidence in support of a five-group model [1 group BIC= 111537.30; 2 group= 63993.41; 3 group= 54853.51; 4 group=47800.53; 5 group= 43637.72]: Low (Low; 28.2%; n=169); Moderate decline (MD; 12.0%; n=72); Intermittent (INT; 16.2%; n=97); High decline (HD, 13.2%; n=79) and Chronic (C; 30.4%; n=182). Based on 200 replications from random starting values, the maximum likelihood estimator for the (at most) 6-class model, subject to the group size constraint, had 5-classes in 100% of replications; thus no admissible 6-class model was found, in light of our constraint. The relative entropy for the 5-class solution was 0.94, indicating very good separation between classes. The very close agreement between the model-estimated rates shown in Figure 1 and the observed proportion of substance use days for each group and time point shown in Table 1 indicate good within-group model fit.
Figure 1. Marijuana use trajectory groups.
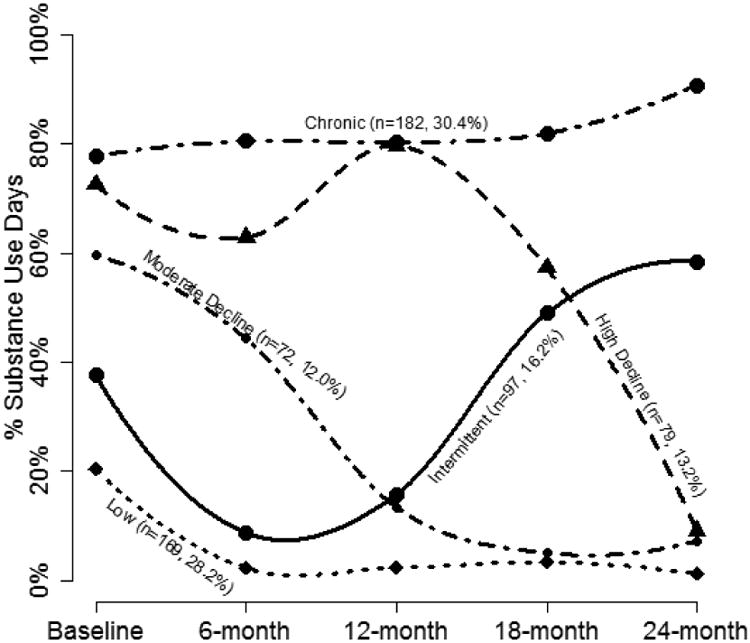
Table 1. Mean marijuana use days at baseline, 6-, 12-, 18-, and 24-month follow-ups based on trajectory group membership.
| Assessment | Low (n=169, 28.2%) | Intermittent (n=97, 16.2%) | Moderate Decline (n=72, 12.0%) | High Decline (n=79, 13.2%) | Chronic (n=182, 30.4%) |
|---|---|---|---|---|---|
| Baseline Cannabis | 18.3 (25.1) | 34.8 (33.7) | 51.8 (32.9) | 60.9 (32.4) | 71.0 (29.5) |
| 6-month Cannabis | 2.2 (3.2) | 6.8 (8.1) | 41.7 (26.7) | 61.3 (32.6) | 71.8 (26.0) |
| 12-month Cannabis | 1.8 (3.5) | 16.0 (18.8) | 8.9 (11.5) | 64.0 (31.2) | 73.4 (27.1) |
| 18-month Cannabis | 3.2 (6.5) | 43.0 (34.8) | 6.4 (7.9) | 56.0 (33.9) | 73.0 (28.5) |
| 24-month Cannabis | 1.1 (2.2) | 53.1 (31.4) | 6.1 (9.8) | 6.9 (9.9) | 81.9 (16.3) |
Note: Values are Mean (SD). Because marijuana use was measured for the past 30 days at baseline, and the past 90 days at each follow-up, the value for baseline days was multiplied by 3 to standardize the days presented for descriptive purposes; n= 599 (baseline), n=512 (6-month), n=502 (12-month), n=505 (18-month) and n=512 (24 month).
3.3 Characteristics of Trajectory Groups
Table 2 shows descriptive characteristics based on marijuana use trajectory group. Age and assault injury appeared similar across the groups, whereas females appeared to be most likely in Low group. Physical aggression and victimization decreased over time. Rates of drug treatment were generally low across the groups. Rates of incarceration were higher at baseline for all groups. The Low group had the lowest negative peer influences and community violence, and the greatest positive peer influences.
Table 2. Descriptive characteristics based on marijuana use trajectory group membership.
| Variables | Low (n =169, 8.2%) | Intermittent (n=97, 16.2%) | Moderate Decline (n=72, 12.0%) | High Decline (n=79, 13.2%) | Chronic (n=182, 30.4%) |
|---|---|---|---|---|---|
| Age | |||||
| Baseline | 20.0 (2.4) | 19.6 (2.7) | 19.9 (2.5) | 20.3 (2.1) | 20.3 (2.4) |
| 12-Month | 20.9 (2.3) | 20.5 (2.8) | 20.9 (2.5) | 21.4 (2.1) | 21.2 (2.4) |
| 24-Month | 22.0 (2.4) | 21.3 (2.7) | 22.0 (2.5) | 22.3 (2.2) | 22.2 (2.3) |
| Male | |||||
| Baseline | 46.2% | 61.9% | 66.7% | 63.3% | 63.7% |
| 12-Month | 42.5% | 58.8% | 66.1% | 61.1% | 64.1% |
| 24-Month | 43.5% | 55.7% | 64.1% | 63.5% | 62.6% |
| Assault Injury Group | |||||
| Baseline | 57.4% | 63.9% | 63.9% | 54.4% | 55.5% |
| 12-Month | 57.5% | 66.3% | 69.4% | 51.4% | 54.9% |
| 24-Month | 58.1% | 65.8% | 65.6% | 54.1% | 53.1% |
| Physical Aggression | |||||
| Baseline | 6.3 (8.5) | 9.5 (15.6) | 11.1 (12.1) | 12.4 (14.7) | 11.4 (15.6) |
| 12-Month | 2.8 (7.3) | 2.9 (5.9) | 3.6 (7.4) | 7.2 (15.2) | 7.5 (13.8) |
| 24-Month | 1.7 (5.4) | 4.2 (11.1) | 2.0 (4.9) | 4.3 (12.0) | 3.2 (10.0) |
| Physical Victimization | |||||
| Baseline | 13.0 (17.7) | 14.3 (18.9) | 13.7 (14.1) | 14.2 (16.0) | 13.6 (17.0) |
| 12-Month | 3.3 (7.1) | 3.5 (8.1) | 4.7 (8.1) | 6.9 (12.4) | 8.2 (14.0) |
| 24-Month | 1.7 (5.1) | 5.8 (15.5) | 1.3 (2.8) | 4.1 (10.2) | 3.8 (10.3) |
| Drug Treatment | |||||
| Baseline | 10.7% | 8.3% | 5.6% | 8.9% | 8.2% |
| 12-Month | 5.2% | 8.8% | 11.3% | 8.3% | 5.9% |
| 24-Month | 6.1% | 11.4% | 10.9% | 8.1% | 4.1% |
| Incarceration | |||||
| Baseline | 18.3% | 20.6% | 27.8% | 30.4% | 24.7% |
| 12-Month | 3.7% | 7.5% | 17.7% | 2.8% | 7.2% |
| 24-Month | 9.5% | 8.9% | 17.2% | 23.0% | 7.5% |
| Negative Peer Influences | |||||
| Baseline | 13.5 (4.8) | 13.6 (4.8) | 14.0 (4.0) | 14.6 (4.4) | 15.6 (5.1) |
| 12-Month | 12.1 (3.9) | 12.9 (4.0) | 13.2 (4.7) | 14.1 (4.4) | 15.4 (5.0) |
| 24-Month | 11.6 (3.9) | 14.1 (5.3) | 12.5 (3.6) | 13.2 (4.8) | 14.6 (4.8) |
| Positive Peer Influences | |||||
| Baseline | 9.0 (3.3) | 8.9 (3.0) | 9.0 (2.7) | 8.9 (3.0) | 8.3 (2.7) |
| 12-Month | 8.9 (3.2) | 8.5 (2.9) | 8.5 (2.4) | 8.5 (2.6) | 8.1 (2.9) |
| 24-Month | 8.6 (2.8) | 8.3 (3.2) | 8.8 (2.6) | 7.8 (2.9) | 7.7 (2.8) |
| Community Violence | |||||
| Baseline | 5.7 (3.4) | 6.4 (3.8) | 6.5 (3.7) | 7.6 (3.5) | 7.3 (3.5) |
| 12-Month | 4.8 (3.9) | 5.6 (3.7) | 5.5 (3.7) | 6.8 (4.1) | 6.8 (3.6) |
| 24-Month | 4.0 (3.6) | 6.0 (4.2) | 4.7 (3.4) | 5.1(4.0) | 6.0 (3.7) |
Note: Values are Mean (SD) or %.
3.3.1 Baseline
At baseline (Table 3), males were more likely to be in the INT, MD, HD, and Chronic groups than in the Low group. Physical aggression was greater among those in the INT, MD, HD, and Chronic groups than in the Low group. In contrast, community violence was greater among those in the HD group than the Low group. Finally, the Chronic group reported less positive peer influences than the Low group.
Table 3. Multinomial regression findings for baseline, 12-month, and 24-month variables associated with marijuana use trajectory group membership.
| Variables | Intermittent RRR (CI) | Moderate Decline RRR (CI) | High Decline RRR (CI) | Chronic RRR (CI) |
|---|---|---|---|---|
| Baseline | ||||
| Age | 0.94 (0.84-1.05) | 0.99 (0.88-1.12) | 1.04 (0.93-1.17) | 1.04 (0.95-1.14) |
| Male | 2.16 (1.24-3.76)** | 2.72 (1.45-5.12)** | 2.15 (1.17-3.98)* | 2.26 (1.40-3.65)** |
| Assault Injury Group | 1.13 (0.66-1.92) | 1.07 (0.59-1.93) | 0.69 (0.39-1.21) | 0.78 (0.49-1.22) |
| Physical Aggression | 1.04 (1.01-1.06)* | 1.05 (1.02-1.08)** | 1.04 (1.02-1.08)** | 1.04 (1.01-1.06)** |
| Drug Treatment | 0.70 (0.28-1.74) | 0.38 (0.12-1.21) | 0.57 (0.21-1.53) | 0.50 (0.23-1.10) |
| Incarceration | 0.96 (0.49-1.91) | 1.36 (0.67-2.78) | 1.48 (0.74-2.96) | 0.99 (0.55-1.77) |
| Negative Peer Influences | 0.97 (0.91-1.04) | 0.98 (0.91-1.05) | 0.98 (0.91-1.05) | 1.05 (0.99-1.05) |
| Positive Peer Influences | 0.99 (0.91-1.07) | 1.00 (0.91-1.10) | 1.01 (0.92-1.10) | 0.92 (0.85-0.99)* |
| Community Violence | 1.03 (0.95-1.12) | 1.02 (0.93-1.12) | 1.12 (1.03-1.22)* | 1.07 (1.00-1.15) |
| 12-Months | ||||
| Age | 0.93 (0.83- 1.05) | 1.01 (0.89-1.15) | 1.11 (0.97-1.26) | 1.06 (0.95-1.17) |
| Male | 1.76 (0.98-3.16) | 2.17 (1.12-4.20)* | 2.28 (1.23-4.23)* | 2.46 (1.46-4.12)** |
| Assault Injury Group | 1.30 (0.72-2.34) | 1.47 (0.76-2.85) | 0.63 (0.35-1.16) | 0.68 (0.41-1.13) |
| Physical Aggression | 0.99 (0.95-1.04) | 1.01 (0.97-1.05) | 1.04 (1.01-1.08)* | 1.04 (1.01-1.07)* |
| Drug Treatment | 1.39 (0.45-4.32) | 1.45 (0.45-4.70) | 1.39 (0.42-4.63) | 0.83 (0.28-2.48) |
| Incarceration | 1.41 (0.39-5.10) | 3.38 (1.04-11.0)* | 0.38 (0.07-2.15) | 0.84 (0.26-2.77) |
| Negative Peer Influences | 1.03 (0.95-1.11) | 1.03 (0.95-1.12) | 1.07 (0.99-1.16) | 1.14 (1.06-1.22)** |
| Positive Peer Influences | 0.94 (0.86-1.04) | 0.96 (0.86-1.06) | 0.92 (0.83-1.02) | 0.88 (0.80-0.96)** |
| Community Violence | 1.05 (0.97-1.14) | 1.04 (0.94-1.14) | 1.10 (1.01-1.20)* | 1.08 (1.00-1.16)* |
| 24-Months | ||||
| Age | 0.88 (0.79- 1.00)* | 1.00 (0.88-1.13) | 1.04 (0.92-1.17) | 1.03 (0.93-1.14) |
| Male | 1.69 (0.94-3.01) | 2.20 (1.16-4.17)* | 2.07 (1.11-3.86)* | 2.34 (1.40-3.92)** |
| Assault Injury Group | 1.30 (0.72-2.36) | 1.27 (0.68-2.38) | 0.68 (0.38-1.23) | 0.80 (0.48-1.32) |
| Physical Aggression | 1.02 (0.98-1.06) | 1.00 (0.96-1.05) | 1.03 (0.99-1.07) | 1.01 (0.98-1.05) |
| Drug Treatment | 1.64 (0.58-4.68) | 1.50 (0.51-4.41) | 0.81 (0.25-2.57) | 0.51 (0.16-1.59) |
| Incarceration | 0.40 (0.14-1.14) | 1.17 (0.46-2.97) | 1.79 (0.75-4.28) | 0.32 (0.13-0.84)* |
| Negative Peer Influences | 1.10 (1.02-1.19)* | 1.02 (0.94-1.11) | 1.06 (0.98-1.15) | 1.15 (1.08-1.23)*** |
| Positive Peer Influences | 0.92 (0.83-1.02) | 1.01 (0.91-1.11) | 0.89 (0.81-0.99)* | 0.85 (0.77-0.93)** |
| Community Violence | 1.11 (1.02-1.21)* | 1.04 (0.96-1.14) | 1.05 (0.96-1.14) | 1.11 (1.03-1.19)** |
Note: Low is the reference group. RRR=Relative Risk Ratios
p<.05,
p<.01,
p<.001.
3.3.2 12-months
At 12-months (Table 3), males were more likely to be assigned to the MD, HD, and Chronic groups than in the Low group. The Low and INT groups did not differ on any variables examined. The MD group was significantly more likely to be incarcerated than the Low group. The HD reported greater physical aggression and community violence than the Low group. Finally, the Chronic group reported more physical aggression, negative peer influences and community violence, and less positive peer influences than the Low group.
3.3.3 24-months
At 24-months (Table 3), the INT group was younger than the Low group. Males were more likely to be in the MD, HD, and Chronic groups than in the Low group. The INT group reported greater negative peer influences and community violence than the Low group. With the exception of sex, the MD group did not differ from the Low group. The HD had less positive friend influences than the Low group. As compared to the Low group, the Chronic group was less likely to be incarcerated and have positive peer influences, and had more negative peer influences and community violence.
4.0 Discussion
This study presents novel data regarding marijuana use trajectories among youth from socioeconomically disadvantaged communities who present to the ED for care. Specifically, 30.4% of youth were chronic users, reporting almost daily use of marijuana over time. Conversely, 28.2% of youth showed low rates of marijuana use at baseline, with almost no days of use two years later. Similar to increasing or late onset groups in other studies, 16.2% were intermittent users, with marijuana use increasing at 24-months. The moderate and high decline groups comprised 25.2% of the sample, showing decreases in marijuana use. Note that the trajectory groups identified represent statistical probabilities of group membership, as opposed to definitive individual outcomes (Nagin and Tremblay, 2005; Skardhamar, 2010); nonetheless, this grouping is useful for understanding characteristics associated with greater marijuana use to inform ED-based intervention efforts (Brame et al., 2012).
Consistent with prior studies, males were more likely than females to be in the greater marijuana use groups (Brook et al., 2011; Schulenberg et al., 2005). Overall, age did not distinguish trajectory groups; however, the limited numbers of adolescents could have precluded detection of effects found in other studies (White et al., 2013b; White et al., 2009). For example, it could be that the moderate declining group may mature into the high declining group. Although prior analysis from the screening sample of this study among drug-users and non-drug users showed that youth presenting with assault injuries had higher rates of substance use than those presenting for other reasons (Cunningham et al., 2014), when examining drug using youth, assault injury (as compared to other reason) was not related to substance use trajectory groups. These findings support the notion of universal screening and initiation of substance use interventions in the ED regardless of chief presenting complaint. The baseline factor consistently associated with greater marijuana use trajectories was physical aggression, which is consistent with findings for externalizing behaviors (Brook et al., 2011; Chassin et al., 2004; Jackson et al., 2008; Schulenberg et al., 2005), likely due to shared risk and promotive factors (e.g., peer influences) and/or exposure to situations that increase aggression (e.g., community violence). The relationship between greater marijuana use and aggression was also observed at 12-months post-ED visit, but dissipated by 24 months, likely reflecting developmental maturation of the sample.
Together, these findings suggest that ED-based interventions should address both substance use and violence, among youth reporting these multiple risk behaviors. Prior studies examining brief interventions for marijuana use are sparse, with a handful of studies showing positive outcomes among youth (D'Amico et al., 2008; Walton et al., 2013; Walton et al., 2014; Woolard et al., 2013), whereas adult studies show null findings (Blow et al., under review; Bogenschutz et al., 2014; Roy-Byrne et al., 2014; Saitz et al., 2014; Woodruff et al., 2014). These interventions, however, have not addressed violence. Similarly, although violence interventions have shown promise among assault injured youth (Becker et al., 2004; Cheng et al., 2008a; Cheng et al., 2008b; Cooper et al., 2006; De Vos et al., 1996; Dicker, 2005; Fein et al., 2013; Karraker et al., 2011; Zun et al., 2006; Zun et al., 2003), these approaches do not typically address substance use. Given that a motivational interviewing (Miller and Rollnick, 2002; Miller and Rollnick, 2012) based brief intervention addressing alcohol and violence showed sustained though modest effects (Cunningham et al., 2012; Walton et al., 2010), interventions may need to be extended, adapting to address increasing and decreasing risk and promotive factors for marijuana use over time (Lei et al., 2012; Rich et al., 2014).
Findings from this study suggest that such adaptive substance use interventions approaches consider also addressing negative peer influences and community violence, which were associated with greater marijuana use trajectories over time. For example, the chronic group showed less positive peer influences at all time points, and more negative peer influences and community violence at 12- and 24-months than the low group. Corresponding to increasing rates of marijuana use, the intermittent group reported greater negative peer influences and community violence at 24-months. Caution is required, however, when making causal conclusions, as the direction of this relationship can't be fully ascertained in this study; in fact, it is likely that these relationships are reciprocal. For example, greater exposure to community violence could lead to greater marijuana use to cope with negative affect, and/or greater marijuana use could lead to greater exposure to situations where violence is likely (e.g., buying and selling drugs). In this regard, multi-level interventions may be beneficial, including individual approaches that facilitate connections with pro-social peers, activities, and services potentially using technology (e.g., text messaging, remote therapy) to reduce barriers, in concert with community-level approaches (Hawkins et al., 2012).
Participation in substance use treatment was not related to marijuana use trajectories, likely because access to treatment services is generally low for youth, particularly in resource poor environments (Center for Behavioral Health Statistics and Quality, 2015), which is reflected in low rates of treatment utilization in this sample despite nearly daily use of marijuana in the chronic group. Next, incarceration was not a useful correlate of marijuana use trajectories, with the exception that the moderate decline group was more likely (at 12 months) to be incarcerated and the chronic group was less likely (at 24 months) to be incarcerated than the low group. Given data showing disproportionate rates of incarceration among African-American youth, with substance use being a salient risk factor for incarceration, early interventions are needed to reduce these health disparities (Mukku et al., 2012; Substance Abuse and Mental Health Service Administration, 2014a).
4.1. Limitations
Although data collected from youth residing in socio-economically disadvantaged communities is an important contribution to the literature, data from a single emergency department setting may not generalize to other samples (e.g., Hispanics). Given findings that self-reported community violence exposure was related to greater marijuana use trajectories, future studies are needed examining geospatial influences on substance use and violence. Our study examined trajectories following an event, namely an ED visit, as opposed to focusing on developmental trajectories among a specific age group, which is why our sample contained a wide age range (14-24 years) of youth with recent drug use. It is likely findings for classes would have differed if non-drug using youth presenting to ED had been included (e.g., abstainers, early initiators, later initiators). Replication of study findings among ED studies taking an age-specific sampling approach would provide further evidence for characteristics associated with marijuana use trajectories across the key developmental transition from adolescence to young adulthood.
5.0 Conclusions
Findings underscore the need for interventions to interrupt marijuana use trajectories among youth residing in urban communities, with a third of youth likely remaining chronic users of marijuana. Interventions for marijuana-using youth should be initiated at the point of the ED visit, particularly among those involved with physical aggression and/or exposed to community violence, which are associated with greater marijuana use. Peer influences are particularly important in distinguishing marijuana use trajectory groups over time, suggesting that interventions are needed to help young people increase involvement with positive peers, activities, and services, adapting to evolving needs over time.
Highlights.
Five marijuana use trajectory groups were identified among drug-using youth.
Aggression and male gender were baseline markers of more severe use trajectories.
Peer influences distinguished marijuana use trajectories over time.
Acknowledgments
We would like to acknowledge the critical assistance of Lynn Massey and Kaneesha Wallace for data collection and Linping Duan for statistical support. Finally, special thanks are owed to the patients and medical staff at Hurley Medical Center for their support of this project.
Role of Funding Source: This project was supported by a grant from the National Institute on Drug Abuse (NIDA DA024646); the work was also supported partly by grants from the CDC (R49CE002099 and U01 CE001957) and the National Institute on Alcohol Abuse and Alcoholism (K23AA022641). The funding agencies did not have direct involvement in the design, collection, analysis and interpretation of data, writing of the paper, or in the decision to submit the paper for publication.
Footnotes
Conflict of Interest: The authors do not have any conflicts of interest to declare.
Contributors: The final manuscript has been reviewed and approved by all authors. Dr. Cunningham was the principal investigator on the grant that funded this work. Drs. Walton, Cunningham, and Epstein-Ngo initiated the development of this paper. Dr. Walton wrote an initial draft of the manuscript, with writing assistance from Drs. Epstein-Ngo, Cunningham and Carter. Drs. Walton, Zimmerman, and Blow were co-investigators on the grant that funded this work; they designed the study including measurements, and with Dr. Buu, provided critical feedback on the focus of this manuscript. Dr. Goldstick assisted with analyses and refinement of the results section and tables. All authors reviewed/edited the manuscript multiple times, approving this final version of the manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Abadi MH, Shamblen SR, Thompson K, Collins DA, Johnson K. Influence of risk and protective factors on substance use outcomes across developmental periods: A comparison of youth and young adults. Subst Use Misuse. 2011;46:1604–1612. doi: 10.3109/10826084.2011.598598. [DOI] [PubMed] [Google Scholar]
- Albert M, McCaig LF. Injury-related emergency department visits by children and adolescents: United States, 2009-2010 NCHS data brief. National Center for Health Statistics; Hyattsville, MD: 2014. [PubMed] [Google Scholar]
- Allen JP, Chango J, Szwedo D, Schad M, Marston E. Predictors of susceptibility to peer influence regarding substance use in adolescence. Child Dev. 2012;83:337–350. doi: 10.1111/j.1467-8624.2011.01682.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker MG, Hall JS, Ursic CM, Jain S, Calhoun D. Caught in the Crossfire: the effects of a peer-based intervention program for violently injured youth. J Adolesc Health. 2004;34:177–183. doi: 10.1016/j.jadohealth.2003.04.001. [DOI] [PubMed] [Google Scholar]
- Bernstein J, Graczyk A, Lawrence D, Bernstein E, Strunin L. Determinants of drinking trajectories among minority youth and young adults the interaction of risk and resilience. Youth Soc. 2011;43:1199–1219. [Google Scholar]
- Blow FC, Walton MA, Bohnert ASB, Ignacio RV, Chermack S, Cunningham RM, Booth BM, Ilgen M, Barry KL. Brief interventions for drug use among adults in an inner city emergency department: A randomized controlled trial. JAMA under review. [Google Scholar]
- Bogenschutz MP, Donovan DM, Mandler RN, Perl HI, Forcehimes AA, Crandall C, Lindblad R, Oden NL, Sharma G, Metsch L, Lyons MS, McCormack R, Konstantopoulos WM, Douaihy A. Brief intervention for patients with problematic drug use presenting in emergency departments: A randomized clinical trial. JAMA Intern Med. 2014;174:1736–1745. doi: 10.1001/jamainternmed.2014.4052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bohnert KM, Walton MA, Ranney M, Bonar EE, Blow FC, Zimmerman MA, Booth BM, Cunningham RM. Understanding the service needs of assault-injured, drug-using youth presenting for care in an urban emergency department. Addict Behav. 2015;41:97–105. doi: 10.1016/j.addbeh.2014.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brame R, Paternoster R, Piquero AR. Thoughts on the analysis of group-based developmental trajectories in criminology. Justice Q. 2012;29:469–490. [Google Scholar]
- Brechwald WA, Prinstein MJ. Beyond homophily: A decade of advances in understanding peer influence processes. J Res Adolesc. 2011;21:166–179. doi: 10.1111/j.1532-7795.2010.00721.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bronfrenbrenner U. The ecology of developmental processes. In: Damon W, Lerner RM, editors. Handbook of Child Psychology; Vol 1: Theoretical models of human development. John Wiley and Sons, Inc; New York: 1998. pp. 993–1023. [Google Scholar]
- Brook JS, Lee JY, Brown EN, Finch SJ, Brook DW. Developmental trajectories of marijuana use from adolescence to adulthood: Personality and social role outcomes. Psychol Rep. 2011;108:339–357. doi: 10.2466/10.18.PR0.108.2.339-357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown SA, McGue M, Maggs J, Schulenberg J, Hingson R, Swartzwelder S, Martin C, Chung T, Tapert SF, Sher K, Winters KC, Lowman C, Murphy S. A developmental perspective on alcohol and youths 16 to 20 years of age. Pediatrics. 2008;121:S290–S310. doi: 10.1542/peds.2007-2243D. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burk WJ, Van der Vorst H, Kerr M, Stattin H. Alcohol use and friendship dynamics: Selection and socialization in early-, middle-, and late-adolescent peer networks. J Stud Alcohol Drugs. 2012;73:89–98. doi: 10.15288/jsad.2012.73.89. [DOI] [PubMed] [Google Scholar]
- Cadoret RJ, Yates WR, Troughton E, Woodworth G, Stewart MA. Adoption study demonstrating two genetic pathways to drug abuse. Arch Gen Psychiatry. 1995;52:42–52. doi: 10.1001/archpsyc.1995.03950130042005. [DOI] [PubMed] [Google Scholar]
- Center for Behavioral Health Statistics and Quality. Behavioral health trends in the United States: Results from the 2014 National Survey on Drug Use and Health 2015 [Google Scholar]
- Center for Disease Control and Prevention. Youth Risk Behavior Surveillance – United States, 2011. Morbidity & Mortality Weekly Report. 2012:61. [PubMed] [Google Scholar]
- Center for Lawful Access and Abuse Deterrence. The National Prescription Drug Abuse Prevention Strategy: 2011-2012 Update. Arlington: 2011. [Google Scholar]
- Chassin L, Fora DB, King KM. Trajectories of alcohol and drug use and dependence from adolescence to adulthood: The effects of familial alcoholism and personality. J Abnorm Psychol. 2004;113:483–498. doi: 10.1037/0021-843X.113.4.483. [DOI] [PubMed] [Google Scholar]
- Chein J, Albert D, O'Brien L, Uckert K, Steinberg L. Peers increase adolescent risk taking by enhancing activity in the brain's reward circuitry. Dev Sci. 2011;14 doi: 10.1111/j.1467-7687.2010.01035.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng TL, Haynie D, Brenner R, Wright JL, Chung SE, Simons-Morton B. Effectiveness of a mentor-implemented, violence prevention intervention for assault-injured youths presenting to the emergency department: Results of a randomized trial. Pediatrics. 2008a;122:938–946. doi: 10.1542/peds.2007-2096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng TL, Wright JL, Markakis D, Copeland-Linder N, Menvielle E. Randomized trial of a case management program for assault-injured youth: Impact on service utilization and risk for reinjury. Pediatr Emerg Care. 2008b;24:130–136. doi: 10.1097/PEC.0b013e3181666f72. [DOI] [PubMed] [Google Scholar]
- Chermack ST, Giancola PR. The relation between alcohol and aggression: An integrated biopsychosocial conceptualization. Clin Psychol Rev. 1997;17:621–649. doi: 10.1016/s0272-7358(97)00038-x. [DOI] [PubMed] [Google Scholar]
- Chermack ST, Grogan-Kaylor A, Perron BE, Murray RL, De Chavez P, Walton MA. Violence among men and women in substance use disorder treatment: A multi-level event-based analysis. Drug Alcohol Depend. 2010;112:194–200. doi: 10.1016/j.drugalcdep.2010.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cleveland HH, Wiebe RP. Understanding the association between adolescent marijuana use and later serious drug use: Gateway effect or developmental trajectory? Dev Psychopathol. 2008;20:615–632. doi: 10.1017/S0954579408000308. [DOI] [PubMed] [Google Scholar]
- Cooper C, Eslinger DM, Stolley PD. Hospital-based violence intervention programs work. J Trauma. 2006;61:534–537. doi: 10.1097/01.ta.0000236576.81860.8c. discussion 537-540. [DOI] [PubMed] [Google Scholar]
- Cunningham RM, Bernstein SL, Walton MA, Broderick K, Vaca F, Woolard B, Bernstein E, Blow FC, D'Onofrio G. Alcohol, tobacco, and other drugs: Future directions for screening and intervention in the emergency department. Acad Emerg Med. 2009;16:1078–1088. doi: 10.1111/j.1553-2712.2009.00552.x. [DOI] [PubMed] [Google Scholar]
- Cunningham RM, Carter PM, Ranney M, Zimmerman MA, Blow FC, Booth BM, Goldstick J, Walton MA. Violent reinjury and mortality among youth seeking emergency department care for assault-related injury: a 2-year prospective cohort study. JAMA Pediatr. 2015;169:63–70. doi: 10.1001/jamapediatrics.2014.1900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham RM, Chermack ST, Zimmerman MA, Shope JT, Bingham CR, Blow FC, Walton MA. Brief motivational interviewing intervention for peer violence and alcohol use in teens: One-year follow-up. Pediatrics. 2012;129:1083–1090. doi: 10.1542/peds.2011-3419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham RM, Ranney M, Newton M, Woodhull W, Zimmerman M, Walton MA. Characteristics of youth seeking emergency care for assault injuries. Pediatrics. 2014;133:e96–e105. doi: 10.1542/peds.2013-1864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D'Amico EJ, Miles JN, Stern SA, Meredith LS. Brief motivational interviewing for teens at risk of substance use consequences: A randomized pilot study in a primary care clinic. J Subst Abuse Treat. 2008;35:53–61. doi: 10.1016/j.jsat.2007.08.008. [DOI] [PubMed] [Google Scholar]
- De Vos E, Stone DA, Goetz MA, Dahlberg LL. Evaluation of a hospital-based youth violence intervention. Am J Prev Med. 1996;12:101–108. [PubMed] [Google Scholar]
- Dicker R. Violence prevention for trauma centers: A feasible start [Poster 2901] Injury and Violence In America, Denver, CO 2005 [Google Scholar]
- Dziak JJ, Li R, Zimmerman MA, Buu A. Time- varying effect models for ordinal responses with applications in substance abuse research. Stat Med. 2014;33:5126–5137. doi: 10.1002/sim.6303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epstein-Ngo QM, Cunningham RM, Whiteside LK, Chermack ST, Booth BM, Zimmerman MA, Walton MA. A daily calendar analysis of substance use and dating violence among high risk urban youth. Drug Alcohol Depend. 2013;1:1–3. doi: 10.1016/j.drugalcdep.2012.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Federal Bureau of Investigation. Preliminary Annual Uniform Crime Report, January - December, 2010. Federal Bureau of Investigation; Washington, DC: 2011. [Google Scholar]
- Fein JA, Mollen CJ, Greene MB. The assault-injured youth and the emergency medical system: What can we do? Clin Pediatr Emerg Med. 2013;14:47–55. [Google Scholar]
- Fowler T, Lifford K, Shelton K, Rice F, Thapar A, Neale MC, McBride A, Van den Bree MB. Exploring the relationship between genetic and environmental influence on initiation and progression of substance use. Addiction. 2007;101:413–422. doi: 10.1111/j.1360-0443.2006.01694.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garmezy N. Resilience in children's adaptation to negative life events and stressed environments. Pediatr Ann. 1991;20:459–460. 463–456. doi: 10.3928/0090-4481-19910901-05. [DOI] [PubMed] [Google Scholar]
- Goldstick JE, Lipton RI, Carter P, Stoddard SA, Newton MF, Reischl T, Walton M, Zimmerman MA, Cunningham RM. The effect of neighborhood context on the relationship between substance misuse and weapons aggression in urban adolescents seeking ED care. Subst Use Misuse. 2015;50:674–684. doi: 10.3109/10826084.2014.998235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstick JE, Stoddard SA, Carter PM, Zimmerman MA, Walton MA, Cunningham RM. Characteristic substance misuse profiles among youth entering an urban emergency department: neighborhood correlates and behavioral comorbidities. Am J Drug Alcohol Abuse. 2016:1–11. doi: 10.1080/00952990.2016.1174707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grove DD, Lazebnik R, Petrack EM. Urban emergency department utilization by adolescents. Clin Pediatr (Phila) 2000;39:479–483. doi: 10.1177/000992280003900806. [DOI] [PubMed] [Google Scholar]
- Gruber SA, Dahlgren MK, Sagar KA, Gönenc A, Killgore WDS. Age of onset of marijuana use impacts inhibitory processing. Neurosci Lett. 2012;511:89–94. doi: 10.1016/j.neulet.2012.01.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grun B, Leisch F. FlexMix version 2: Finite mixtures with concomitant variables and varying and constant parameters. J Stat Softw. 2008;28:1–35. [Google Scholar]
- Hawkins JD, Oesterle S, Brown EC, Monahan KC, Abbott RD, Arthur MW, Catalano RF. Sustained decreases in risk exposure and youth problem behaviors after installation of the Communities That Care prevention system in a randomized trial. Arch Pediatr Adolesc Med. 2012;166:141–148. doi: 10.1001/archpediatrics.2011.183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henry KL, Thornberry TP. Truancy and escalation of substance use during adolescence. J Stud Alcohol Drugs. 2010;71:115–124. doi: 10.15288/jsad.2010.71.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hjorthoj CR, Hjorthoj AR, Nordentoft M. Validity of Timeline Follow-Back for self-reported use of cannabis and other illicit substances--systematic review and meta-analysis. Addict Behav. 2012;37:225–233. doi: 10.1016/j.addbeh.2011.11.025. [DOI] [PubMed] [Google Scholar]
- Humeniuk R, Ali R, Babor TF, Farrell M, Formigoni ML, Jittiwutikarn J, de Lacerda RB, Ling W, Marsden J, Monteiro M, Nhiwatiwa S, Pal H, Poznyak V, Simon S. Validation of the Alcohol, Smoking And Substance Involvement Screening Test (ASSIST) Addiction. 2008;103:1039–1047. doi: 10.1111/j.1360-0443.2007.02114.x. [DOI] [PubMed] [Google Scholar]
- Hussong A, Bauer D, Chassin L. Telescoped trajectories from alcohol initiation to disorder in children of alcoholic parents. J Abnorm Psychol. 2008;117:63–78. doi: 10.1037/0021-843X.117.1.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson KM, Sher KJ, Schulenberg JE. Conjoint developmental trajectories of young adult substance use. Alcohol Clin Exp Res. 2008;23:723–737. doi: 10.1111/j.1530-0277.2008.00643.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karraker N, Cunningham RM, Becker MG, Fein JA, Knox LM. Violence is Preventable: A Best Practices Guide for Launching & Sustaining a Hospital-based Program to Break the Cycle of Violence. 2011 http://www.ncdsv.org/images/NNHVIP-YouthAlive_ViolenceIsPreventable_2011.pdf.
- Lei H, Nahum-Shani I, Lynch K, Oslin D, Murphy SA. A “SMART” design for building individualized treatment sequences. Annu Rev Clin Psychol. 2012;8:21–48. doi: 10.1146/annurev-clinpsy-032511-143152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leisch F. Flexmix: A general framework for finite mixture models and latent class regression in R. J Stat Softw. 2004;11:1–18. [Google Scholar]
- Lopez-Larson MP, Bogorodzki P, Rogowska J, McGlade E, King JB, Terry J, Yurgelun-Todd D. Altered prefrontal and insular cortical thickness in adolescent marijuana users. Behav Brain Res. 2011;220:164–172. doi: 10.1016/j.bbr.2011.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maxwell JC. Drunk versus drugged: How different are the drivers? Drug Alcohol Depend. 2012;121:68–72. doi: 10.1016/j.drugalcdep.2011.08.009. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Kushner H, Metzger D, Peters R, Smith I, Grissom G, Pettinati H, Argeriou M. The fifth edition of the addiction severity index. J Subst Abuse Treat. 1992;9:199–213. doi: 10.1016/0740-5472(92)90062-s. [DOI] [PubMed] [Google Scholar]
- Meier MH, Caspi A, Houts R, Slutske WS, Harrington H, Jackson KM, Belsky DW, Poulton R, Moffitt TE. Prospective developmental subtypes of alcohol dependence from age 18 to 32 years: Implications for nosology, etiology, and intervention. Dev Psychopathol. 2013;25:785–800. doi: 10.1017/S0954579413000175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR, Rollnick S. Motivational Interviewing: Preparing People for Change. The Guilford Press; New York, NY: 2002. [Google Scholar]
- Miller WR, Rollnick S. Motivational Interviewing: Helping People Change. The Guilford Press; New York: 2012. [Google Scholar]
- Mrug S, Gaines J, Su W, Windle M. School-level substance use: Effects on early adolescents' alcohol, tobacco, and mairjuana use. J Stud Alcohol Drugs. 2010;71:488–495. doi: 10.15288/jsad.2010.71.488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mukku VK, Benson TG, Alam F, Richie WD, Bailey RK. Overview of substance use disorders and incarceration of African American males. Front Psychiatry. 2012:3. doi: 10.3389/fpsyt.2012.00098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagin DS, Tremblay RE. Developmental trajectory groups: Fact or a useful statistical fiction? Criminology. 2005;43:873–904. [Google Scholar]
- Naimi TS, Brewer RD, Mokdad A, Denny C, Serdula MK, Marks JS. Binge drinking among US adults. JAMA. 2003;289:70–75. doi: 10.1001/jama.289.1.70. [DOI] [PubMed] [Google Scholar]
- National Institute on Drug Abuse. NIDA-Modified ASSIST-Prescreen V1.0. [Accessed on July 20, 2010];2010 http://www.drugabuse.gov/nidamed/screening/nmassist.pdf.
- Nylund KL, Asparouhov T, Muthén BO. Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Struct Equ Modeling. 2007;14:535–569. [Google Scholar]
- Ostaszewski K, Zimmerman MA. The effects of cumulative risks and promotive factors on urban adolescent alcohol and other drug use: A longitudinal study of resiliency. Am J Community Psychol. 2006;38:237–249. doi: 10.1007/s10464-006-9076-x. [DOI] [PubMed] [Google Scholar]
- Quinlan KP, Brewer RD, Siegel P, Sleet DA, Mokdad AH, Shults RA, Flowers N. Alcohol-impaired driving among U.S. adults, 1993-2002. Am J Prev Med. 2005;28:346–350. doi: 10.1016/j.amepre.2005.01.006. [DOI] [PubMed] [Google Scholar]
- Ram N, Grimm KJ. Methods and measures: Growth mixture modeling: A method for identifying differences in longitudinal change among unobserved groups. Int J Behav Dev. 2009;33:565–576. doi: 10.1177/0165025409343765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramirez M, Wu Y, Kataoka S, Wong M, Yang J, Peek-Asa C, Stein B. Youth violence across multiple dimensions: A study of violence, absenteeism, and suspensions among middle school children. J Pediatr. 2012;161:542–546. e542. doi: 10.1016/j.jpeds.2012.03.014. [DOI] [PubMed] [Google Scholar]
- Rich B, Moodie EE, Stephens DA. Simulating sequential multiple assignment randomized trials to generate optimal personalized warfarin dosing strategies. Clin Trials. 2014;11:435–444. doi: 10.1177/1740774513517063. [DOI] [PubMed] [Google Scholar]
- Richters JE, Martinez P. In: Things I Have Seen and Heard: A structured interview for assessing young children's violence exposure. National Institute of Mental Health, editor. Rockville, MD: 1992. [Google Scholar]
- Roy-Byrne P, Bumgardner K, Krupski A, Dunn C, Ries R, Donovan D, West II, Maynard C, Atkins DC, Graves MC, Joesch JM, Zarkin GA. Brief intervention for problem drug use in safety-net primary care settings: a randomized clinical trial. JAMA. 2014;312:492–501. doi: 10.1001/jama.2014.7860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutter M. Psychosocial resilience and protective mechanisms. Am J Orthopsychiatry. 1987;57:316–331. doi: 10.1111/j.1939-0025.1987.tb03541.x. [DOI] [PubMed] [Google Scholar]
- Saitz R, Palfai TP, Cheng DM, Alford DP, Bernstein JA, Lloyd-Travaglini CA, Meli SM, Chaisson CE, Samet JH. Screening and brief intervention for drug use in primary care: the ASPIRE randomized clinical trial. JAMA. 2014;312:502–513. doi: 10.1001/jama.2014.7862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schepis TS, Desai RA, Cavallo DA, Smith AE, McFetridge A, Liss TB, Potenza MN, Krishnan-Sarin S. Gender differences in adolescent marijuana use and associated psychosocial characteristics. J Addict Med. 2011;5:65–73. doi: 10.1097/ADM.0b013e3181d8dc62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schillie SF, Shehab N, Thomas KE, Budnitz DS. Medication overdoses leading to emergency department visits among children. Am J Prev Med. 2009;37:181–187. doi: 10.1016/j.amepre.2009.05.018. [DOI] [PubMed] [Google Scholar]
- Schulenberg JE, Merline AC, Johnston LD, O'Malley PM, Bachman JG, Laetz VB. Trajectories of marijuana use during the transition to adulthood: The big picture based on national panel data. J Drug Issues. 2005;35:255–280. doi: 10.1177/002204260503500203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simons-Morton B, Farhat T. Recent findings on peer group influences on adolescent smoking. J Prim Prev. 2010;31:191–208. doi: 10.1007/s10935-010-0220-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skardhamar T. Distinguishing facts and artifacts in group- based modeling. Criminology. 2010;48:295–320. [Google Scholar]
- Sobell LC, Sobell MB, Leo GI, Cancilla A. Reliability of a timeline method: assessing normal drinkers' reports of recent drinking and a comparative evaluation across several populations. Br J Addict. 1988;83:393–402. doi: 10.1111/j.1360-0443.1988.tb00485.x. [DOI] [PubMed] [Google Scholar]
- Stokols D, Allen J, Bellingham L. The social ecology for health promotion: Implications for research and practice. Am J Health Promot. 1996;10:247–251. doi: 10.4278/0890-1171-10.4.247. [DOI] [PubMed] [Google Scholar]
- Straus MA, Hamby SL, Boney-McCoy S, Sugarman DB. The Revised Conflict Tactics Scales (CTS2) J Fam Issues. 1996;17:283–316. [Google Scholar]
- Substance Abuse and Mental Health Service Administration. Results from the 2012 National Survey on Drug Use and Health: Summary of National Findings NSDUH Series H-46. Substance Abuse and Mental Health Services Administration; Rockville: 2013. [Google Scholar]
- Substance Abuse and Mental Health Service Administration. Health Disparities. [Accessed on October 19, 2016];2014a http://www.samhsa.gov/health-disparities.
- Substance Abuse and Mental Health Service Administration. Results from the 2013 National Survey on Drug Use and Health: Detailed Tables. Substance Abuse and Mental Health Services Administration; Rockville, MD: 2014b. [Google Scholar]
- Wagner EF. Developmentally informed research on the effectiveness of clinical trials: A primer for assessing how developmental issues may influence treatment responses among adolescents with alcohol use problems. Pediatrics. 2008;121:S337–S347. doi: 10.1542/peds.2007-2243F. [DOI] [PubMed] [Google Scholar]
- Walton MA, Bohnert K, Resko S, Barry KL, Chermack ST, Zucker RA, Zimmerman MA, Booth BM, Blow FC. Computer and therapist based brief interventions among cannabis-using adolescents presenting to primary care: One year outcomes. Drug Alcohol Depend. 2013;132:646–653. doi: 10.1016/j.drugalcdep.2013.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walton MA, Chermack ST, Shope JT, Bingham CR, Zimmerman MA, Blow FC, Cunningham RM. Effects of a brief intervention for reducing violence and alcohol misuse among adolescents: a randomized controlled trial. JAMA. 2010;304:527–535. doi: 10.1001/jama.2010.1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walton MA, Cunningham RM, Goldstein AL, Chermack ST, Zimmerman MA, Bingham CR, Shope JT, Stanley R, Blow FC. Rates and correlates of violent behaviors among adolescents treated in an urban emergency department. J Adolesc Health. 2009;45:77–83. doi: 10.1016/j.jadohealth.2008.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walton MA, Resko S, Barry KL, Chermack ST, Zucker RA, Zimmerman MA, Booth BM, Blow FC. A randomized controlled trial testing the efficacy of a brief cannabis universal prevention program among adolescents in primary care. Addiction. 2014;109:786–797. doi: 10.1111/add.12469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White AM, MacInnes E, Hingson RW, Pan I. Hospitalizations for suicide-related drug poisonings and co-occuring alcohol overdoses in adolsescents (ages 12-17) and young adults (ages 18-24) in the United States, 1999-2008: Results from the Nationwide Inpatient Sample. Suicide Life Threat Behav. 2013a;43:198–212. doi: 10.1111/sltb.12008. [DOI] [PubMed] [Google Scholar]
- White HR, Fite P, Pardini D, Mun EY, Loeber R. Moderators of the dynamic link between alcohol use and aggressive behavior among adolescent males. J Abnorm Child Psychol. 2013b;41:211–222. doi: 10.1007/s10802-012-9673-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White HR, Jackson KM, Loeber R. Handbook on crime and deviance. Springer; 2009. Developmental sequences and comorbidity of substance use and violence; pp. 433–468. [Google Scholar]
- WHO ASSIST Working Group. The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): Development, reliability and feasibility. Addiction. 2002;97:1183–1194. doi: 10.1046/j.1360-0443.2002.00185.x. [DOI] [PubMed] [Google Scholar]
- Wilhelmi BG, Cohen SP. A framework for “driving under the influence of drugs” policy for the opioid using driver. Pain Physician. 2012;15:215–230. [PubMed] [Google Scholar]
- Wilson KM, Klein JD. Adolescents who use the emergency department as their usual source of care. Arch Pediatr Adolesc Med. 2000;154:361–365. doi: 10.1001/archpedi.154.4.361. [DOI] [PubMed] [Google Scholar]
- Windle M, Spear LP, Fuligni AJ, Angold A, Brown JD, Pine D, Smith GT, Giedd J, Dahl RE. Transitions into underage and problem drinking: developmental processes and mechanisms between 10 and 15 years of age. Pediatrics. 2008;121(4):S273–289. doi: 10.1542/peds.2007-2243C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolfe DA, Crooks CV, Chiodo D, Hughes R, Ellis W. Observations of adolescent peer resistance skills following a classroom-based healthy relationship program: A post-intervention comparison. Prev Sci. 2012;13:196–205. doi: 10.1007/s11121-011-0256-z. [DOI] [PubMed] [Google Scholar]
- Woodruff SI, Clapp JD, Eisenberg K, McCabe C, Hohman M, Shillington AM, Sise CB, Castillo EM, Chan TC, Sise MJ, Gareri J. Randomized clinical trial of the effects of screening and brief intervention for illicit drug use: the Life Shift/Shift Gears study. Addict Sci Clin Pract. 2014;9:8. doi: 10.1186/1940-0640-9-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woolard R, Baird J, Longabaugh R, Nirenberg T, Lee CS, Mello MJ, Becker B. Project reduce: reducing alcohol and marijuana misuse: effects of a brief intervention in the emergency department. Addict Behav. 2013;38:1732–1739. doi: 10.1016/j.addbeh.2012.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zucker RA, Chermack ST, Curran GM. Alcoholism: A lifespan perspective on etiology and course. In: Sameroff AJ, Lewis M, Miller R, editors. Handbook of Developmental Psychopathology. Plenum; New York: 2000. pp. 569–587. [Google Scholar]
- Zucker RA, Donovan JE, Masten AS, Mattson ME, Moss HB. Early developmental processes and the continuity of risk for underage drinking and problem drinking. Pediatrics. 2008;121(4):S252–272. doi: 10.1542/peds.2007-2243B. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zun LS, Downey L, Rosen J. The effectiveness of an ED-based violence prevention program. Am J Emerg Med. 2006;24:8–13. doi: 10.1016/j.ajem.2005.05.009. [DOI] [PubMed] [Google Scholar]
- Zun LS, Downey LV, Rosen J. Violence prevention in the ED: linkage of the ED to a social service agency. Am J Emerg Med. 2003;21:454–457. doi: 10.1016/s0735-6757(03)00102-5. [DOI] [PubMed] [Google Scholar]


