Abstract
Background:
Massive rotator cuff tears pose a difficult and complex challenge even for the experienced surgeon; inability to repair these tears by conventional means designates them as irreparable, while management becomes quite taxing. Several operative options have been suggested for the management of such lesions with varying degrees of success, while it is imperative to match patient demands and expectations to the predicted outcome.
Methods:
Research articles are examined and key concepts are discussed, in order to provide an evidence based review of the available literature. The anatomy and pathomechanics along with the indications, contraindications and surgical techniques are reported.
Results:
Transfer of the Latissimus dorsi has been used with success to restore shoulder function in deficits of the posterior rotator cuff. Although it can be used in a variety of settings, the ideal patient for a Latissimus dorsi tendon transfer is a young and active individual, with no glenohumeral osteoarthritis that has a severe disability and weakness related to an irreparable posterior cuff tear.
Conclusion:
Tendon transfers have proved to be a successful treatment option in salvaging this difficult problem, providing pain relief and restoring shoulder function. Despite the excellent functional outcomes and pain suppression following operation, a variety of factors may affect the outcome; thus making indications and preoperative assessment a valuable component.
Keywords: Irreparable rotator cuff tears, Latissimus dorsi, Massive rotator cuff tears, Shoulder surgery, Tendon, Transfer
INTRODUCTION
Rotator cuff tears constitute a significant cause of pain and loss of upper limb function, an incident reflected in the increasing number of operations recorded per annum [1]. An estimated 10- 40% of all rotator cuff tears reported are massive [2-4] and may lead to even more severe impairment of shoulder function, as they are associated with persistent defects, weakness and poor outcomes [5]. The resulting symptomatology is deficit related; presenting in patients suffering from posterosuperior cuff tears as a decrease or loss of active external rotation and anterior elevation, resulting in spatial ataxia of the upper extremity [6].
A variety of classifications for massive rotator cuff tears has been proposed, although they are currently mostly defined the detachment of two or more tendons [7]. Several authors defined massive tears as those with an anteroposterior dimension greater than 5cm [8] whereas others have determined the size by measuring the amount of the exposed humeral head [9]. In addition massive tears may be characterized by their anatomic pattern to anterosuperior and posterosuperior [10]; the first concerns tears of the supraspinatus and subscapularis tendons, while the second is associated with tears of the supraspinatus and infraspinatus which may be combined with a compromised teres minor tendon.
Typically massive tears are chronic lesions characterized by gradual progression, and mostly affect older patients, while they only rarely occur as an acute injury secondary to trauma. Nevertheless chronic lesions may be complicated by acute injury and are often regarded as acute on chronic. Chronicity of these lesions may lead to muscle atrophy [11], tendon retraction [12-14] and fatty infiltration [15], posing a serious challenge even for the experienced shoulder surgeon in comparison to smaller tears; and despite of the technical difficulties encountered many of these are repairable [16].
Abnormal shoulder kinematics and joint forces consequent of a massive tear may conclusively lead to arthritic degeneration due to eccentric loading. Tears that cannot be repaired by conventional techniques on the rotator cuff footprint are deemed irreparable. Reported incidence ranges from 6.5%- 22.4% [17] and can be as high as 30% [18]. Reparability is affected by a variety of factors. An increased failure probability, has been correlated to an acromio-humeral distance of <7mm in a standard AP radiograph [3, 19] along with advanced fatty infiltration [19, 20] of the muscles above Goutallier stage 2 [15, 21]. Other factors that predispose to failure include the size of the defect and poor tendon quality [5, 22, 23].
A variety of treatment options has been proposed ranging from non-operative treatment to simple debridement, partial cuff repair with or without graft augmentation, tendon transfers and reverse total shoulder arthroplasty. Debridement with or without biceps tenotomy [24] has been proven to be effective, providing satisfactory functional outcomes and pain relief [25] despite the inability to restore strength [26]; nevertheless results may deteriorate with time and pain may reappear [24, 27]. Partial repair of the cuff on the other hand has been associated with the ability to restore normal function [28] providing strength improvement and satisfactory outcomes [29, 30]. Augmenting the tendons with allografts despite providing the ability to bridge the defect [31], has been associated with poor outcomes [32] and high failure rates [17, 33].
Reverse arthroplasty has been proven effective for older patients when significant joint degeneration is present. It provides the ability to restore active elevation [34-37], but in the setting of a posterior cuff deficiency it is not able to restore active external rotation; in which case it may be coupled with a latissimus dorsi (LD) tendon transfer to restore function [38-40]. Nevertheless it has been suggested recently in a study combining LD and teres major with reverse that it should be limited in patients with major disability and high grades of fatty infiltration, due to a high rate of complications [41].
Latissimus dorsi transfer has been first proposed in 1988 by Gerber for irreparable posterior cuff tears [23] as a means to restore active shoulder external rotation and has been used ever since with success [42-47].
The purpose of restoration of active external rotation has also been achieved by other tendon transfers such as the lower trapezius transfer to the infraspinatus tendon or insertion [48-50]; nonetheless LD still remains the most studied and reported transfer [23, 42, 51-55].
PATHOMECHANICS
Normal shoulder kinematics and function is the result of the synergistic action of the muscles of the rotator cuff and the deltoid. These muscles act as a dynamic stabilizer by providing a centralizing force in the glenohumeral joint and allow for normal shoulder function [56]. The centralizing forces that are exerted into the glenohumeral joint act in couples and are present into the coronal and transverse planes [57]. The coronal plane balance is maintained by a force couple involving the deltoid and the inferior cuff, while balance in the transverse plane is maintained by the subscapularis anteriorly and infraspinatus-teres minor complex posteriorly [58-60]. In this setting any imbalance in the balancing force couples may result in abnormal shoulder kinematics and subsequently loss of function. Thus it is obvious that tears in the anterior cuff involving the subscapularis or posterior cuff involving the infraspinatus may result in uncoupling of the normal balance and produce abnormal forces and affect motion [57-60].
ANATOMY-BIOMECHANICS
The latissimus dorsi is a triangular shaped muscle that originates from the posterior part of the iliac crest, the lumbar fascia, the T7-T12 vertebrae, the lower 3 or 4 ribs and several times with a few muscle fibers from the inferior scapular angle; and is inserted into the floor of the bicipital groove of the humerus. It is innervated by the thoracodorsal nerve, and its original function is extension, adduction and internal rotation of the arm [61].
The purpose behind LD tendon transfer is to restore active shoulder external rotation and normal shoulder function in the setting of an imbalance caused by a posterior cuff deficient force couple [62]. The hypothesis behind restoration of external rotation following LD tendon transfer was supported as early as 1936 by L’Episcopo [63] who used it for obstetrical plexus paralysis, followed by Gerber et al. who successfully used it to treat massive and irreparable RC tears [23, 42]. Transfer of the LD provides the ability in the context of a massive irreparable posterior cuff tear, to bridge the defect and provide an external rotation force thus restoring the force couple and improve shoulder motion [64]. With the transfer procedure the function of LD changes from an internal rotator to an external rotator [61]; this is achieved by either a true muscular activity or a tenodesis effect exerting a passive force that balances the force couple [65].
Muscular activity has been recorded in several EMG studies following transfer procedures, and has been exhibited that LD activates synergistically and contributes besides external rotation to both adduction [66] and abduction [67, 68]. Furthermore the LD tendon acts as a depressor of humerus resisting cranial migration, which in turn allows for more effective deltoid function during abduction and forward flexion [55, 65]. Nevertheless, despite the marked functional improvement reported with LD transfers in posterior irreparable tears, the normal rotator cuff function cannot be fully restored; owing mostly to abnormal forces exerted on the glenohumeral joint relative to the inferior LD anatomic position in regards to infraspinatus and teres minor [62].
INDICATIONS-CONTRAINDICATION FOR LD TRANSFER
In the absence of a perfect solution, treatment of massive irreparable posterior RC lesions has proven to be quite challenging, adding to the surgeon’s dilemma regarding the choice of patient and treatment option. Tendon transfers have proven to be a valuable asset in restoring function and improving outcomes in the setting of an irreparable cuff tear. However a multitude of elements may influence the outcome and effectiveness of such operations, limiting their use to selected patients; and rendering the use of indications and contraindications, an essential component (Table 1).
Table 1.
Indications, contraindications and complications of latissimus dorsi tendon transfer.
| Indications | Contraindications | Complications |
|---|---|---|
|
Patients • Young age, active individuals • Older patients with increased functional • demands, bodily active Clinical • Severe functional disability due to • Weakness and loss of motion • Severe pain caused by a massive • Irreparable cuff tear Compliance • Patients that will comply with long •rehabilitation Imaging and intraoperative • Fatty infiltration – retraction • Not amenable to repair |
Absolute |
• Postoperative hematoma • Infection • Late / secondary tendon rupture • Anchor pull out • Nerve palsies |
| • Advanced age • Comorbidities (infection etc) • Severe joint degeneration (Hamada ≥ stage 2, Samilson ≥ stage 1) • Compromised Coracoacromial arch • Anterosuperior subluxation • Subscapularis deficiency – atrophy – fatty degeneration • Deltoid deficiency – detachment • Nerve injuries • Inability to comply with long rehabilitation | ||
| Relative | ||
| • Subscapularis partial tears • Advanced fatty degeneration of the teres minor • Acromio- humeral distance < 7 mm • Moderate joint degeneration (Hamada – Stage 1-2) • Preoperative weakness - pseudoparalysis |
Preoperative assessment must take into consideration a variety of factors, including age, pain, disability, functional demands and patient expectations; additionally the patient must be educated on anticipated functional outcomes. Other factors that may affect operative outcomes must be considered as well, such as medical comorbidities, subscapularis and deltoid function, coraco-acromial arch integrity the presence of arthritic changes and the degree to which a patient is obliged and will comply with extended rehabilitation.
The principal complaints on presentation in patients with symptomatic massive RC tears are usually pain, weakness and loss of motion. The cause of pain must be determined during physical examination and distinguished from other causes of shoulder pathology [69]. Massive irreparable RC tears are common causes of severe pain and are often extremely disabling minimizing in this context the choice on other treatment modalities.
Typically patients with posterosuperior cuff tears present with reduced forward flexion and abduction and are unable to actively externally rotate the arm [70, 71]. A positive external rotation lag sign and a positive hornblower’s sign are indicative of posterior cuff deficits and external rotation inability [72, 73]. Moreover a positive hornblower’s sign has been associated with irreparable teres minor tears [73] and advanced fatty infiltration [7, 14] and is related to poor outcomes in tendon transfers [74]. This has been highlighted in the studies of Gerber et al. [55] and Costouros et al. [74] who reported lower outcome scores and decreased external rotation in patients with advanced fatty degeneration. However Nové-Josserand et al. found that patients with severe atrophy had greater increments in functional outcome scores than patients with moderate atrophy or without atrophy and bigger gains in active external rotation during abduction; suggesting that the transferred LD compensates the deficient teres minor [75]. The positive influence an intact teres minor may have on LD tendon transfer may be partially explained by the fact that it has a greater excursion in comparison to the other rotator cuff muscles; not impending thereby the excursion of the LD [74, 76].
Weakness may present with varying degrees ultimately leading to pseudoparalysis; referring to the inability of active external rotation or forward flexion in the absence of nerve lesions or unhindered passive motion. It has been suggested that pseudoparalysis is a contraindication to LD transfer [77], and it is related to poor outcomes [65]; as it does not provide the required strength to overcome a pseudoparalytic shoulder and achieve elevation not present preoperatively [65]. However recent evidence suggests that in patients with an intact subscapularis it may not be a contraindication as it may provide good functional results in that particular group, although further studies may be required to provide additional data for that matter [78]. Nevertheless despite the fact that there is no consensus regarding the degrees of anteflexion for a shoulder to be considered pseudoparalytic, in a recent study [79] patients with mobility lower than 80° exhibited bigger increments in anteflexion than patients with greater range of motion; suggesting that these patients still gain from LD tendon transfers. A finding confirmed by a study by Nové-Josserand et al. who reported on five pseudoparalytic patients that gained mobility postoperatively and overcame the pseudoparalytic state [75].
Furthermore patient observation may reveal the status of the periscapular muscles, revealing atrophies and possible deficiencies as the detachment of deltoid muscle origin. Subscapularis and deltoid muscles must be intact for a successful LD transfer as deficiencies may cause imbalances in the force couples subsequently causing instabilities in both planes [47]. Poor outcomes have been reported by many authors for LD transfer in patients with subscapularis tears, rendering it a definitive contraindication [23, 43, 44, 46, 61, 80]. However several studies reported good results with no impact on final outcomes following repair of partial upper third subscapularis tears [47, 65, 75, 79, 81].
Imaging studies play a critical role in preoperative assessment and evaluation of the defects. Plain film radiographs are useful in determining the morphology and status of the glenohumeral joint. Osteoarthritic changes of the glenohumeral joint are evident in simple radiographs and the degree of glenoid erosion can be easily assessed [82, 83]. The presence of severe osteoarthritis is coupled with inferior outcomes in the setting of LD tendon transfer [84] while furthermore in patients of young age that are not candidates for a total shoulder arthroplasty, LD transfer may potentially restore function and slow arthritic progression [55]. A decreased acromiohumeral distance <7 mm may also be exhibited which is correlated to the size of the RC tear, tendon irreparability and varying degrees of fatty infiltration [85]. Typically an acromiohumeral distance <7mm is associated with superior migration of the humeral head and indicates tears of the infraspinatus that mainly acts in lowering the humeral head [86-89]. The integrity of the coracoacromial arch may be assessed as well, an important structure that stabilizes anterosuperior movement when there is a tear of the supraspinatus and any other tendon [18, 90, 91]. This is due to the loss of joint compressive forces in the setting of a massive irreparable tear, that are unable to be compensated by the remaining muscles; leading to an imbalance between a deficient rotator cuff and a strong deltoid with subsequent anterosuperior subluxation [92, 93]. In this context an intact arch remains the only passive restraint against superior subluxation, which when severely compromised will have an impact on overhead function [94].
Computed tomography scans were successfully used to evaluate the degree of rotator cuff atrophy and the degree of fatty infiltration, although MRI studies are more effective in the study of soft tissue deficits and are used more often. Muscle belly atrophy can be determined effectively [95] and is correlated to poor functional outcomes following repair [96]. The size of the defect can be easily assessed in MRI studies, as well as tendon quality [5, 22, 23] two factors that directly affect the reparability of a tear. Tendon retraction [97] can be evaluated as well, along with muscular fatty infiltration, an indicator of chronicity that is coupled to the probability of a failed repair when above Goutallier stage 2 [15, 96].
Ultrasonographic reports of soft tissue deficiencies seem to correlate with MRI findings in up to 85% of the cases [98, 99] although the outcome and repeatability is directly related to the experience of the technician.
SURGICAL TECHNIQUES
Latissimus dorsi tendon transfer has become a valuable choice for reconstruction of irreparable posterosuperior rotator cuff tears. Since its inception, several modifications of the original technique have been suggested, while other considerations have risen such as the method and site of fixation. Variable means of fixation have been used by several authors such as transosseous sutures [23, 47], classic anchors [45, 81, 100] and interference screw [101]. A common mode of repair failure has been discussed by several authors [102, 103] and involves splitting of the transferred tendon by sutures mainly due to its reduced thickness [104]. A recent biomechanical study supports this finding by reporting that the weakest element was the tendon itself and not the anchor – suture construct [103]; while they conclude that interference screw fixation presents higher or similar biomechanical properties to anchor fixation whereas tubularization of the tendon which is performed in conjunction, may address the reduced thickness variable [103]. Regarding this matter, other authors suggested harvesting the tendon with a small bone chip may help alleviate this issue [54].
Several authors agree with the hypothesis, that lower thickness of the transferred tendon is responsible for secondary failures [75, 84, 105, 106]. The incidence of late LD tendon rupture has been reported to occur in 20-30% of the cases while it has been suggested that augmentation may help to overcome this issue [18]. A number of materials have been used for enhancing LD structural integrity at the insertion point including, synthetic biomaterials autografts and allografts. Vicryl mesh [84] has been used with success suggesting that the material provides strong fixation points at the insertion site [84]. Absorbable PDS reinforcement [75] has also been recommended, suggesting an enhanced tenodesis effect due to the ability for the transplant to be placed under tension; coming to agreement with Aoki et al. regarding augmentation with a Teflon felt [107]. Other authors reported the use of Achilles tendon or double looped semitendinosus allografts, which in addition to reinforcing the insertion site they may allow for lengthening of the tendon if required [108]. Further options include tensor fascia lata [106] and teres major augmentation.
The combined use of LD and teres major has been studied extensively. It has been used initially by L’Episcopo for restoring external rotation secondary to obstetric brachial plexus paralysis and later by Hoffer [109]. The role in massive irreparable cuff tears is providing tissue for coverage and enhancing strength of the tendon complex [110]. Isolated LD transfers versus combined LD and teres major transfers have been reported to have lower gains in strength postoperatively [72, 110]. Biomechanical studies have shown that isolated teres major transfers are more efficient in restoring normal shoulder function versus isolated LD transfers or a combination of them [67, 111]. Nevertheless it has been demonstrated [110] that the use of isolated LD transfer provides better external rotation and forward flexion, while joint degeneration progresses slower and patient satisfaction remains high [43-45, 47, 65, 81, 112]. Moreover isolated teres major transfer remains difficult to perform due to a short excursion [76, 113].
The site of tendon fixation remains controversial. Several authors support attachment to the superior facet of the greater tuberosity or the subscapularis or the stump of the supraspinatus in order to obtain a more anterior fixation [45, 65, 68, 69, 76, 77, 111]; gaining thereby a supplementary tenodesis effect. Other authors [114, 115] recommended fixing the tendon at the infraspinatus insertion site on the middle or inferior facet in order to achieve better external rotation. Furthermore a recent biomechanical finite element study suggested that the best option for restoration of external rotation and anterior elevation is fixation at the insertion of the infraspinatus tendon [67, 111]. In regards to operative technique, LD transfer may be accomplished either by open technique, or in combination with arthroscopy.
SINGLE INCISION
The opportunity to perform the LD tendon transfer via a single incision thereby avoiding deltoid injury, was made possible by translating the site of fixation posteriorly and inferiorly [45, 75]. In this context Habermayer et al. [45] suggested a single incision axillary approach and reported comparable clinical results to the standard double incision [23, 42, 81, 116]. Boileau et al. [115] used a modification of the deltopectoral approach described by L’Episcopo. The single incision according to Habermayer [45] is performed in a lateral decubitus position. Exposure is achieved through a triangular incision from the lateral border of the scapula to the inferior scapular angle and from the axillary pouch to its apex. Identification and separation of the LD from the teres major follows. Detachment of the tendon occurs. The infraspinatus is approached through the plane between deltoid and teres minor. The arm in 90° of abduction and external rotation helps identify the greater tuberosity. The tendon is then inserted and attached at the site of the infraspinatus insertion.
DOUBLE INCISION
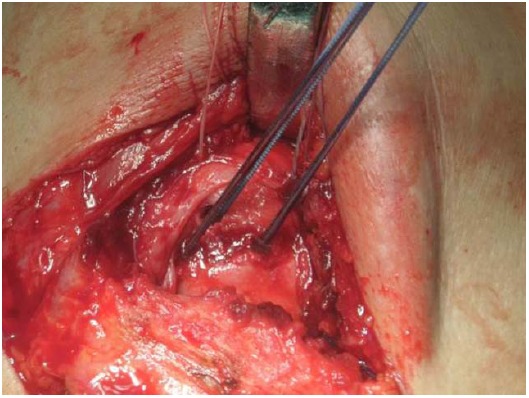
The original technique suggested by Gerber et al. in 1988 [23] involved a double incision, via the axilla and superiorly via the deltoid [42]. This technique has been popularized by other authors and reported good results in the absence of a subscapularis tear [47, 81, 117]. The operation is performed in a lateral decubitus position. A superior approach is performed with an incision lateral to the acromioclavicular joint, allowing for exposure of the rotator cuff through a deltoid split (Fig. 1). The axillary approach is performed through an incision on the lateral border of the LD (Fig. 2). The muscle is released from the humerus and separated from teres major (Fig. 3). Following exploration of the neurovascular bundle the muscle is transferred through the interval between the deltoid and infraspinatus and teres minor. Attachment of the tendon follows at the supraspinatus insertion with anchors while attachment of the remaining rotator cuff to the medial edge of the muscle is performed (Fig. 4) [62]. In addition a more anterior fixation may be achieved with suturing on the superior border of the subscapularis.
Fig. (1).

Superior approach with an incision 1 cm medial to the lateral border of the acromion.
Fig. (2).

Axillary approach on the lateral border of the latissimus dorsi.
Fig. (3).

Dissection of the pedicle and separation of the latissimus dorsi tendon.
Fig. (4).
Preparation of the denuded supraspinatus footprint for fixation of latissimus dorsi with anchors.
ARTHROSCOPICALLY ASSISTED
Arthroscopically assisted techniques are technically demanding procedures, while they permit for reduced muscle damage in contrast to open surgery. Injury of the deltoid muscle may occur during open transfer [118] an incident that is related to poor clinical outcomes [10, 43, 65, 74], while it has been exhibited that following open surgery it is unable to regain strength [61]. Therefore arthroscopically assisted procedures may potentially help avoid such issues. The procedure typically involves dissection and preparation of the LD through an axillary approach while the glenohumeral joint is initially inspected via arthroscopy through a posterior portal [108]. The insertion site is prepared arthroscopically by decorticating the infraspinatus and supraspinatus footprint. A subdeltoid tunnel is created by blunt dissection through the interval of the deltoid- teres minor. The tendon is then passed under the acromion by pulling the sutures through the anterior portal (Fig 5). Fixation of the tendon follows with the suture anchors and once secured the anterior edge is fixed to the subscapularis (Fig 6).
Fig. (5).
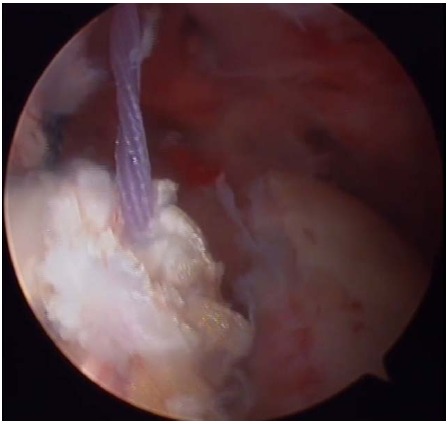
Transfer of the latissimus dorsi tendon by pulling the sutures through an anterior portal.
Fig. (6).
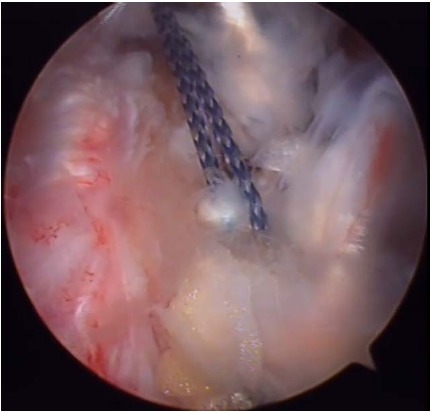
Anchor fixation of the latissimus dorsi over the supraspinatus footprint.
Recently a mini-open approach has been introduced for LD harvesting to be used in combination with arthroscopy for transfer and fixation [101]. A small axillary incision around 5 cm for preparation of the LD is achieved with the use of an ultrasound Doppler. Preoperative identification of the pedicle using ultrasonography, allows for accurate placement of the incision and straightforward dissection while minimizing incision length. Fixation of the tendon follows by means of arthroscopy.
REVERSE SHOULDER ARTHROPLASTY AND LD TRANSFER
Massive rotator cuff tears are frequently linked with superior humeral head migration [119-122] which without appropriate treatment may lead to degenerative changes of the glenohumeral joint. Cuff tear arthropathy usually presents with loss of active elevation, although a subset of patients may present with severe dysfunction due to a combined loss of elevation and external rotation [38]. Reverse shoulder arthroplasty has been used with success in treating cuff tear arthropathies and restore active elevation [34-37]; it does not however restore active external rotation and may lead to reduced functional results [34, 123, 124]. Pseudoparalysis of external rotation has been mainly attributed to deficiency of the teres minor [72, 73, 125], relative to chronicity with ensuing atrophy or fatty infiltration [7, 126]. In this context, extending indications of LD tendon transfer to be performed in conjunction with reverse shoulder arthroplasty has provided a solution; as it has been demonstrated to increase external rotation and provide a better control of the arm in space [38-40].
OUTCOMES
Latissimus dorsi tendon transfers have been associated with satisfactory results [43, 45, 55, 65, 75, 81, 84, 105]. Table 2 Reported pain, range of motion and function have been shown to improve postoperatively [43, 45, 55, 65, 75, 81, 84, 105]. Patient satisfaction following operation remains high [32, 43-45, 47, 81, 112], while a high percentage of patients has been reported to be willing to undergo the operation again [42, 78, 84]. Operative outcomes have been demonstrated to be sustained in the long term, preserving pain relief and range of motion [55, 127]. There are some reports however, demonstrating deterioration of results with time and reemergence of pain [24, 27]. Recently Gerber et al. [55] associated poor outcomes following operation, with a large critical shoulder angle [128]. They noted significantly better outcomes in the low angle group (≤36°) in regards to flexion, abduction and mean relative constant score; while abduction strength and external rotation were comparable. These findings were attributed to better stability in abduction and flexion, theoretically resulting from a deltoid force vector that is centered in the glenoid in shoulders with a low critical angle [55]. Thus they suggested correction of a large critical angle >36° to be taken into consideration.
Table 2.
Functional outcome scores following LD tendon transfer (CS: Constant Score, SSV: Subjective Shoulder Value, SSI: Shoulder Score Index).
| Authors | Journal | Year | No. of patients | Technique | Age | Follow up | Preoperative functional measurements | Postoperative functional measurements |
|---|---|---|---|---|---|---|---|---|
| El-Azab et al. | J bone Joint Surg Am | 2015 | 93 | Gerber | 56 years (40-72) | 111,6 months (79,2-132) | 44% relative CS 30 ASES score |
71% relative CS 70 ASES score |
| De casa et al. | J Orth Surg Res | 2014 | 14 | Arthroscopy assisted | 59 years (52-66) | 52 months (36-77) | 33 CS | 59 CS |
| Castricini et al. | J bone Joint Surg Am | 2014 | 27 | Arthroscopy assisted | 60 years (46-67) | 27 months (24-36) | 36 CS | 74 CS |
| Villacis et al. | Arthrosc Tech | 2013 | 8 | Arthroscopy assisted | 54 years (49- 60) | Mean 14 months | 63 SSI | 70 SSI |
| Gerber et al. | J bone Joint Surg Am | 2013 | 45 | Gerber | 56 years (37-67) | 146.6 months (122-184) | 47,3 CS 29% SSV |
63,8 CS 70,1% SSV |
| Debeer et al. | Acta Orthop Belg | 2010 | 26 | Gerber | 56,5 years (42-66) | 43,3 months (13-124) | 39 CS | 60 CS |
| Weening et al. | Int Orthop | 2010 | 16 | Gerber | 60 years (49-71) | 26 months (7-73) | 32,5 CS | 50,3 CS |
| Moursy et al. | J bone Joint Surg Am | 2009 | 42 | Gerber (n =22) Bone chip (n=20) |
58 years (50-75) | Mean 47 months | 43,4 (Gerber technique) 40,2 (bone chip) |
64,8 ASES score 74,2 ASES score |
| Nové – Josserand et al. | Orthop Traumatol Surg Res | 2009 | 26 | Gerber | 55,5 years (36-71) | 34 months (24-62) | 50 CS | 74 CS |
| Habermayer et al. | J bone Joint Surg Br | 2006 | 14 | Single incision | 61 years (47- 76) | 32 months (19-42) | 46,5 CS | 74,6 CS |
| Gerber et al. | J bone Joint Surg Am | 2006 | 69 | Gerber | 61 years (49- 72) | 59 months (24 – 126) | 55% CS | 73% CS |
| Ianotti et al. | J bone Joint Surg Am | 2006 | 20 | Gerber | 54,8 years (44-68) | 39 months (24- 85) | 40 PENN score | 66 PENN score |
| Miniaci et al. | J bone Joint Surg Am | 1999 | 17 | Gerber | 55 years (32-77) | 51 months (24-72) | 6,8 UCLA score | 16,4 UCLA score |
| Aoki et al. | J bone Joint Surg Br | 1996 | 12 | Gerber | 64 years (48- 82) | 35,6 months (26-42) | 11,8 UCLA score | 28 UCLA score |
Despite the important improvements noted on range of motion and pain relief, strength gains following the tendon transfer are low. Gerber et al. [55] noted an approximately 40% strength gain in women and 25% in men in relation to preoperative levels. In a recent systematic review which included 10 studies the authors indicated that a 70% gain in abduction strength can be expected [64]. Possible causes of low strength gains suggested include, the inability of LD to center the humeral head [61]. The noted strength gains however, do not seem to influence daily living activities [61]. Furthermore another factor that may influence postoperative outcomes is the compliance and adherence of the patient to a strict physiotherapy regime, that is required in order to develop the neuromuscular control to recruit the LD as an external rotator instead of an internal rotator [129].
Joint degenerative changes has been recorded in several studies and results were quite controversial. Gerber et al. [55] noted structural deterioration comparable to non-operative management, although progression was reported slower. The described osteoarthritic changes were commonly restricted in 1 or 2 stages of the Hamada classification [82], while another group [130] reported significant osteoarthritic changes with time. However, it has been reported that radiologic findings regarding arthritic degeneration are not related to the clinical outcomes [43, 54, 117]. Nevertheless joint degeneration is anticipated [43, 75, 117] due to degradation of the tenodesis effect over time [131], a finding evident in several studies that demonstrated a decrease in acromiohumeral distance in the mid [130] and long term [55, 127] in comparison to the initial postoperative outcome. It has been suggested however, that potentially LD tendon transfer may prolong the time till arthroplasty [131].
Primary operations have been reported to obtain better results than revision operations [43, 44, 47, 54, 75, 79, 84, 117]. In addition several investigators noted better outcomes in younger patients [127]. Arthroscopically assisted techniques have been reported to obtain results comparable to the open transfers [103, 108]. Moreover a recent clinical study reported significant improvements regarding strength and functional outcome scores in patients treated with arthroscopically assisted LD tendon transfer in comparison to patients treated with arthroscopic partial repair [132]. Regarding the approach, there are no studies in the literature with strong statistical data to provide a valid comparison between single and double incision; although it has been reported that results from single incision are comparable to the standard double incision technique [81, 116]. Complications reported include, the formation of hematoma [84, 105, 117] in up to 14,3% of the patients, and the appearance of infection [61, 84, 105, 117] in up to 7,7% of the patients. Late transferred tendon rupture [44, 47, 54, 80, 105, 117] has been recorded ranging from 5,5% up to 44%. Nerve palsies following operation have been reported as well although in most cases were transient [43, 54, 117].
CONCLUSION
Latissimus dorsi tendon transfer for the treatment of irreparable posterior cuff tears is a demanding and complex procedure that may restore shoulder function and provide pain relief. In addition it may help restore strength to some extent, but this improvement should not be expected to be significant. Outcome results may vary and directly rely on careful patient selection while underlying pathology must be taken into consideration. Patients should be able to withstand and comply with long rehabilitation protocols, as well as be informed on the benefits expected following operation. In this context patient expectations should match anticipated results.
ACKNOWLEDGEMENTS
Declared none.
LIST OF ABBREVIATIONS
- AP
= Anteroposterior
- ASES
= American Shoulder and Elbow Surgeons
- CS
= Constant Score
- EMG
= Electromyographic
- LD
= Latissimus Dorsi
- MRI
= Magnetic Resonance Imaging
- PDS
= Polydioxanone Sutures
- RC
= Rotator Cuff
- SSI
= Shoulder Score Index
- SSV
= Subjective Shoulder Value
- UCLA
= University of California at Los Angeles
AUTHOR'S CONTRIBUTION
Panagiotis P. Anastasopoulos
Contributed in conception, design, and acquisition of data as well as drafting the manual and revising it.
George Alexiadis
Contributed in conception, design, and acquisition of data as well as drafting the manual and revising it.
Sarantis Spyridonos
Contributed in conception of the manuscript and in revising it.
Emmanouil Fandridis
Contributed in conception, design, and acquisition of data as well as drafting the manual and revising it.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
REFERENCES
- 1.Yamaguchi K. New guideline on rotator cuff problems. Rosemount, USA: AAOS Now; 2011. [Google Scholar]
- 2.Habermeyer P, Krieter C, Tang KL, Lichtenberg S, Magosch P. A new arthroscopic classification of articular-sided supraspinatus footprint lesions: a prospective comparison with Snyder's and Ellman's classification. J Shoulder Elbow Surg. 2008. [DOI] [PubMed]
- 3.Ellman H., Hanker G., Bayer M. Repair of the rotator cuff. End-result study of factors influencing reconstruction. J. Bone Joint Surg. Am. 1986;68(8):1136–1144. [PubMed] [Google Scholar]
- 4.Ellman H, Kay SP, Wirth M. Arthroscopic treatment of full-thickness rotator cuff tears: 2- to 7-year follow-up study. Arthroscopy. 1993;9(2):195–200. doi: 10.1016/s0749-8063(05)80374-3. [DOI] [PubMed] [Google Scholar]
- 5.Harryman D.T., II, Mack L.A., Wang K.Y., Jackins S.E., Richardson M.L., Matsen F.A., III Repairs of the rotator cuff. Correlation of functional results with integrity of the cuff. J. Bone Joint Surg. Am. 1991;73(7):982–989. [PubMed] [Google Scholar]
- 6.Jost B., Pfirrmann C.W., Gerber C., Switzerland Z. Clinical outcome after structural failure of rotator cuff repairs. J. Bone Joint Surg. Am. 2000;82(3):304–314. doi: 10.2106/00004623-200003000-00002. [DOI] [PubMed] [Google Scholar]
- 7.Gerber C., Fuchs B., Hodler J. The results of repair of massive tears of the rotator cuff. J. Bone Joint Surg. Am. 2000;82(4):505–515. doi: 10.2106/00004623-200004000-00006. [DOI] [PubMed] [Google Scholar]
- 8.Cofield R.H. Rotator cuff disease of the shoulder. J. Bone Joint Surg. Am. 1985;67(6):974–979. [PubMed] [Google Scholar]
- 9.Nobuhara K., Hata Y., Komai M. Surgical procedure and results of repair of massive tears of the rotator cuff. Clin. Orthop. Relat. Res. 1994;(304):54–59. [PubMed] [Google Scholar]
- 10.Warner J.J. Treatment of massive rotator cuff tears: posterior-superior and anterior-superior. In: Iannotti J.P., editor. The rotator cuff: current concepts and complex problems. Rosemont, Illinois: American Academy of Orthopedic Surgeons; 1998. pp. 59–94. [Google Scholar]
- 11.Thomazeau H., Boukobza E., Morcet N., Chaperon J., Langlais F. Prediction of rotator cuff repair results by magnetic resonance imaging. Clin. Orthop. Relat. Res. 1997;(344):275–283. [PubMed] [Google Scholar]
- 12.Meyer D.C., Lajtai G., von Rechenberg B., Pfirrmann C.W., Gerber C. Tendon retracts more than muscle in experimental chronic tears of the rotator cuff. J. Bone Joint Surg. Br. 2006;88(11):1533–1538. doi: 10.1302/0301-620X.88B11.17791. [DOI] [PubMed] [Google Scholar]
- 13.Zingg P.O., Jost B., Sukthankar A., Buhler M., Pfirrmann C.W., Gerber C. Clinical and structural outcomes of nonoperative management of massive rotator cuff tears. J. Bone Joint Surg. Am. 2007;89(9):1928–1934. doi: 10.2106/JBJS.F.01073. [DOI] [PubMed] [Google Scholar]
- 14.Zumstein M.A., Jost B., Hempel J., Hodler J., Gerber C. The clinical and structural long-term results of open repair of massive tears of the rotator cuff. J. Bone Joint Surg. Am. 2008;90(11):2423–2431. doi: 10.2106/JBJS.G.00677. [DOI] [PubMed] [Google Scholar]
- 15.Goutallier D., Postel J.M., Bernageau J., Lavau L., Voisin M.C. Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin. Orthop. Relat. Res. 1994;(304):78–83. [PubMed] [Google Scholar]
- 16.Lo IK, Burkhart SS. Arthroscopic repair of massive, contracted, immobile rotator cuff tears using single and double interval slides: technique and preliminary results. Arthroscopy. 2004;20(1):22–33. doi: 10.1016/j.arthro.2003.11.013. [DOI] [PubMed] [Google Scholar]
- 17.Moore D.R., Cain E.L., Schwartz M.L., Clancy W.G., Jr Allograft reconstruction for massive, irreparable rotator cuff tears. Am. J. Sports Med. 2006;34(3):392–396. doi: 10.1177/0363546505281237. [DOI] [PubMed] [Google Scholar]
- 18.Warner J.J. Management of massive irreparable rotator cuff tears: the role of tendon transfer. Instr. Course Lect. 2001;50:63–71. [PubMed] [Google Scholar]
- 19.Gerber C, Wirth SH, Farshad M. Treatment options for massive rotator cuff tears. J Shoulder Elbow Surg. 2011;20(2 Suppl):S20–9. doi: 10.1016/j.jse.2010.11.028. [DOI] [PubMed] [Google Scholar]
- 20.Goutallier D, Postel JM, Gleyze P, Leguilloux P, Van Driessche S. Influence of cuff muscle fatty degeneration on anatomic and functional outcomes after simple suture of full-thickness tears. J Shoulder Elbow Surg. 2003. [DOI] [PubMed]
- 21.Goutallier D., Postel J.M., Lavau L., Bernageau J. Impact of fatty degeneration of the suparspinatus and infraspinatus msucles on the prognosis of surgical repair of the rotator cuff. Rev. Chir. Orthop Repar. Appar. Mot. 1999;85(7):668–676. [PubMed] [Google Scholar]
- 22.Gazielly D.F., Gleyze P., Montagnon C. Functional and anatomical results after rotator cuff repair. Clin. Orthop. Relat. Res. 1994;(304):43–53. [PubMed] [Google Scholar]
- 23.Gerber C., Vinh T.S., Hertel R., Hess C.W. Latissimus dorsi transfer for the treatment of massive tears of the rotator cuff. A preliminary report. Clin. Orthop. Relat. Res. 1988;(232):51–61. [PubMed] [Google Scholar]
- 24.Walch G, Edwards TB, Boulahia A, Nove-Josserand L, Neyton L, Szabo I. Arthroscopic tenotomy of the long head of the biceps in the treatment of rotator cuff tears: clinical and radiographic results of 307 cases. J Shoulder Elbow Surg. 2005;14(3):238–46. doi: 10.1016/j.jse.2004.07.008. [DOI] [PubMed] [Google Scholar]
- 25.Kempf JF, Gleyze P, Bonnomet F, et al. A multicenter study of 210 rotator cuff tears treated by arthroscopic acromioplasty. Arthroscopy. 1999;15(1):56–66. doi: 10.1053/ar.1999.v15.015005. [DOI] [PubMed] [Google Scholar]
- 26.Rockwood C.A., Jr, Williams G.R., Jr, Burkhead W.Z., Jr Débridement of degenerative, irreparable lesions of the rotator cuff. J. Bone Joint Surg. Am. 1995;77(6):857–866. doi: 10.2106/00004623-199506000-00006. [DOI] [PubMed] [Google Scholar]
- 27.Melillo A.S., Savoie F.H., III, Field L.D. Massive rotator cuff tears: debridement versus repair. Orthop. Clin. North Am. 1997;28(1):117–124. doi: 10.1016/S0030-5898(05)70269-8. [DOI] [PubMed] [Google Scholar]
- 28.Burkhart S.S. Partial repair of massive rotator cuff tears: the evolution of a concept. Orthop. Clin. North Am. 1997;28(1):125–132. doi: 10.1016/S0030-5898(05)70270-4. [DOI] [PubMed] [Google Scholar]
- 29.Burkhart SS, Nottage WM, Ogilvie-Harris DJ, Kohn HS, Pachelli A. Partial repair of irreparable rotator cuff tears. Arthroscopy. 1994. [DOI] [PubMed]
- 30.Duralde XA, Bair B. Massive rotator cuff tears: the result of partial rotator cuff repair. J Shoulder Elbow Surg. 2005;14(2):121–7. doi: 10.1016/j.jse.2004.06.015. [DOI] [PubMed] [Google Scholar]
- 31.Neviaser JS. Ruptures of the rotator cuff of the shoulder. Arch Surg. 1971;102(5):483–5. doi: 10.1001/archsurg.1971.01350050049015. [DOI] [PubMed] [Google Scholar]
- 32.Iannotti J.P., Codsi M.J., Kwon Y.W., Derwin K., Ciccone J., Brems J.J. Porcine small intestine submucosa augmentation of surgical repair of chronic two-tendon rotator cuff tears. A randomized, controlled trial. J. Bone Joint Surg. Am. 2006;88(6):1238–1244. doi: 10.2106/JBJS.E.00524. [DOI] [PubMed] [Google Scholar]
- 33.Sclamberg SG, Tibone JE, Itamura JM, Kasraeian S. Six-month magnetic resonance imaging follow-up of large and massive rotator cuff repairs reinforced with porcine small intestinal submucosa. J Shoulder Elbow Surg. 2004. [DOI] [PubMed]
- 34.Boileau P, Watkinson DJ, Hatzidakis AM, Balg F. Grammont reverse prosthesis: design, rationale, and biomechanics. J Shoulder Elbow Surg. 2005. [DOI] [PubMed]
- 35.Werner C.M., Steinmann P.A., Gilbart M., Gerber C. Treatment of painful pseudoparesis due to irreparable rotator cuff dysfunction with the Delta III reverse-ball-and-socket total shoulder prosthesis. J. Bone Joint Surg. Am. 2005;87(7):1476–1486. doi: 10.2106/JBJS.D.02342. [DOI] [PubMed] [Google Scholar]
- 36.Valenti P.H., Boutens D., Nerot C. Delta 3 reversed prosthesis for osteoarthritis with massive rotator cuff tear: Long term results (>5 years). In: G. Walch, P. Boileau, D. Mole Eds. 2000 Shoulder Prosthesis Two to Ten Year Follow-Up. Sauramps Medical, Montpellier, France. 2001; pp. 253–9. [Google Scholar]
- 37.Sirveaux F., Favard L., Oudet D., Huguet D., Lautman S. Grammont inverted total shoulder arthroplasty in the treatment of glenohumeral osteoarthritis with massive and non repairable cuff rupture. In: Walch G., Boileau P., Mole D., editors. 2000 Shoulder prosthesis … two to ten year follow-up. Montpellier, France: Sauramps Medical; 2001. pp. 247–52. [Google Scholar]
- 38.Boileau P., Chuinard C., Roussanne Y., Bicknell R.T., Rochet N., Trojani C. Reverse shoulder arthroplasty combined with a modified latissimus dorsi and teres major tendon transfer for shoulder pseudoparalysis associated with dropping arm. Clin. Orthop. Relat. Res. 2008;466(3):584–593. doi: 10.1007/s11999-008-0114-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Boughebri O., Kilinc A., Valenti P. Reverse shoulder arthroplasty combined with a latissimus dorsi and teres major transfer for a deficit of both active elevation and external rotation. Results of 15 cases with a minimum of 2-year follow-up. Orthop. Traumatol. Surg. Res. 2013;99(2):131–137. doi: 10.1016/j.otsr.2012.11.014. [DOI] [PubMed] [Google Scholar]
- 40.Puskas GJ, Catanzaro S, Gerber C. Clinical outcome of reverse total shoulder arthroplasty combined with latissimus dorsi transfer for the treatment of chronic combined pseudoparesis of elevation and external rotation of the shoulder. J Shoulder Elbow Surg. 2014;23(1):49–57. doi: 10.1016/j.jse.2013.04.008. [DOI] [PubMed] [Google Scholar]
- 41.Shi L.L., Cahill K.E., Ek E.T., Tompson J.D., Higgins L.D., Warner J.J. Latissimus dorsi and teres major transfer with reverse shoulder arthroplasty restores active motion and reduces pain for posterosuperior cuff dysfunction. Clin. Orthop. Relat. Res. 2015;473(10):3212–3217. doi: 10.1007/s11999-015-4433-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gerber C. Latissimus dorsi transfer for the treatment of irreparable tears of the rotator cuff. Clin. Orthop. Relat. Res. 1992;(275):152–160. [PubMed] [Google Scholar]
- 43.Gerber C., Maquieira G., Espinosa N. Latissimus dorsi transfer for the treatment of irreparable rotator cuff tears. J. Bone Joint Surg. Am. 2006;88(1):113–120. doi: 10.2106/JBJS.E.00282. [DOI] [PubMed] [Google Scholar]
- 44.Aoki M., Okamura K., Fukushima S., Takahashi T., Ogino T. Transfer of latissimus dorsi for irreparable rotator-cuff tears. J. Bone Joint Surg. Br. 1996;78(5):761–766. [PubMed] [Google Scholar]
- 45.Habermeyer P., Magosch P., Rudolph T., Lichtenberg S., Liem D. Transfer of the tendon of latissimus dorsi for the treatment of massive tears of the rotator cuff: a new single-incision technique. J. Bone Joint Surg. Br. 2006;88(2):208–212. doi: 10.1302/0301-620X.88B2.16830. [DOI] [PubMed] [Google Scholar]
- 46.Werner CM, Zingg PO, Lie D, Jacob HA, Gerber C. The biomechanical role of the subscapularis in latissimus dorsi transfer for the treatment of irreparable rotator cuff tears. J Shoulder Elbow Surg. 2006;15(6):736–42. doi: 10.1016/j.jse.2005.11.002. [DOI] [PubMed] [Google Scholar]
- 47.Warner JJ, Parsons IMt. Latissimus dorsi tendon transfer: a comparative analysis of primary and salvage reconstruction of massive, irreparable rotator cuff tears. J Shoulder Elbow Surg. 2001;10(6):514–21. doi: 10.1067/mse.2001.118629. [DOI] [PubMed] [Google Scholar]
- 48.Elhassan BT, Wagner ER, Bishop AT. Feasibility of contralateral trapezius transfer to restore shoulder external rotation: part I. J Shoulder Elbow Surg. 2012;21(10):1363–9. doi: 10.1016/j.jse.2011.10.031. [DOI] [PubMed] [Google Scholar]
- 49.Elhassan B. Lower trapezius transfer for shoulder external rotation in patients with paralytic shoulder. J. Hand Surg. Am. 2014;39(3):556–562. doi: 10.1016/j.jhsa.2013.12.016. [DOI] [PubMed] [Google Scholar]
- 50.Elhassan B., Bishop A., Shin A. Trapezius transfer to restore external rotation in a patient with a brachial plexus injury. A case report. J. Bone Joint Surg. Am. 2009;91(4):939–944. doi: 10.2106/JBJS.H.00745. [DOI] [PubMed] [Google Scholar]
- 51.Elhassan B., Bishop A., Shin A., Spinner R. Shoulder tendon transfer options for adult patients with brachial plexus injury. J. Hand Surg. Am. 2010;35(7):1211–1219. doi: 10.1016/j.jhsa.2010.05.001. [DOI] [PubMed] [Google Scholar]
- 52.Cleeman E, Hazrati Y, Auerbach JD, Shubin Stein K, Hausman M, Flatow EL. Latissimus dorsi tendon transfer for massive rotator cuff tears: a cadaveric study. J Shoulder Elbow Surg. 2003;12(6):539–43. doi: 10.1016/S1058-2746(03)00206-4. [DOI] [PubMed] [Google Scholar]
- 53.Waters P.M. Update on management of pediatric brachial plexus palsy. J. Pediatr. Orthop. 2005;25(1):116–126. doi: 10.1097/00004694-200501000-00025. [DOI] [PubMed] [Google Scholar]
- 54.Moursy M., Forstner R., Koller H., Resch H., Tauber M. Latissimus dorsi tendon transfer for irreparable rotator cuff tears: a modified technique to improve tendon transfer integrity. J. Bone Joint Surg. Am. 2009;91(8):1924–1931. doi: 10.2106/JBJS.H.00515. [DOI] [PubMed] [Google Scholar]
- 55.Gerber C., Rahm S.A., Catanzaro S., Farshad M., Moor B.K. Latissimus dorsi tendon transfer for treatment of irreparable posterosuperior rotator cuff tears: long-term results at a minimum follow-up of ten years. J. Bone Joint Surg. Am. 2013;95(21):1920–1926. doi: 10.2106/JBJS.M.00122. [DOI] [PubMed] [Google Scholar]
- 56.Lippitt S., Matsen F. Mechanisms of glenohumeral joint stability. Clin. Orthop. Relat. Res. 1993;(291):20–28. [PubMed] [Google Scholar]
- 57.Burkhart S.S. Fluoroscopic comparison of kinematic patterns in massive rotator cuff tears. A suspension bridge model. Clin. Orthop. Relat. Res. 1992;(284):144–152. [PubMed] [Google Scholar]
- 58.Burkhart S.S. Arthroscopic treatment of massive rotator cuff tears. Clinical results and biomechanical rationale. Clin. Orthop. Relat. Res. 1991;(267):45–56. [PubMed] [Google Scholar]
- 59.Ahmad C.S., Kleweno C., Jacir A.M., Bell J.E., Gardner T.R., Levine W.N., Bigliani L.U. Biomechanical performance of rotator cuff repairs with humeral rotation: a new rotator cuff repair failure model. Am. J. Sports Med. 2008;36(5):888–892. doi: 10.1177/0363546508316285. [DOI] [PubMed] [Google Scholar]
- 60.Thompson W.O., Debski R.E., Boardman N.D., III, Taskiran E., Warner J.J., Fu F.H., Woo S.L. A biomechanical analysis of rotator cuff deficiency in a cadaveric model. Am. J. Sports Med. 1996;24(3):286–292. doi: 10.1177/036354659602400307. [DOI] [PubMed] [Google Scholar]
- 61.Weening A.A., Willems W.J. Latissimus dorsi transfer for treatment of irreparable rotator cuff tears. Int. Orthop. 2010;34(8):1239–1244. doi: 10.1007/s00264-010-0970-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Omid R., Lee B. Tendon transfers for irreparable rotator cuff tears. J. Am. Acad. Orthop. Surg. 2013;21(8):492–501. doi: 10.5435/JAAOS-21-08-492. [DOI] [PubMed] [Google Scholar]
- 63.L'Episcopo J.B. Tendon transplantation in obstetrical paralysis. Am. J. Surg. 1934;25(1):122–125. doi: 10.1016/S0002-9610(34)90143-4. [DOI] [Google Scholar]
- 64.Namdari S., Voleti P., Baldwin K., Glaser D., Huffman G.R. Latissimus dorsi tendon transfer for irreparable rotator cuff tears: a systematic review. J. Bone Joint Surg. Am. 2012;94(10):891–898. doi: 10.2106/JBJS.K.00841. [DOI] [PubMed] [Google Scholar]
- 65.Iannotti J.P., Hennigan S., Herzog R., Kella S., Kelley M., Leggin B., Williams G.R. Latissimus dorsi tendon transfer for irreparable posterosuperior rotator cuff tears. Factors affecting outcome. J. Bone Joint Surg. Am. 2006;88(2):342–348. doi: 10.2106/JBJS.D.02996. [DOI] [PubMed] [Google Scholar]
- 66.Henseler JF, Nagels J, Nelissen RG, de Groot JH. Does the latissimus dorsi tendon transfer for massive rotator cuff tears remain active postoperatively and restore active external rotation? J Shoulder Elbow Surg. 2014;23(4):553–60. doi: 10.1016/j.jse.2013.07.055. [DOI] [PubMed] [Google Scholar]
- 67.Magermans D.J., Chadwick E.K., Veeger H.E., van der Helm F.C., Rozing P.M. Biomechanical analysis of tendon transfers for massive rotator cuff tears. Clin. Biomech. (Bristol, Avon) 2004;19(4):350–357. doi: 10.1016/j.clinbiomech.2003.11.013. [DOI] [PubMed] [Google Scholar]
- 68.Steenbrink F., de Groot J.H., Veeger H.E., van der Helm F.C., Rozing P.M. Glenohumeral stability in simulated rotator cuff tears. J. Biomech. 2009;42(11):1740–1745. doi: 10.1016/j.jbiomech.2009.04.011. [DOI] [PubMed] [Google Scholar]
- 69.Gerber C, Galantay RV, Hersche O. The pattern of pain produced by irritation of the acromioclavicular joint and the subacromial space. J Shoulder Elbow Surg. 1998;7(4):352–5. doi: 10.1016/S1058-2746(98)90022-2. [DOI] [PubMed] [Google Scholar]
- 70.Boes M.T., McCann P.D., Dines D.M. Diagnosis and management of massive rotator cuff tears: the surgeon’s dilemma. Instr. Course Lect. 2006;55:45–57. [PubMed] [Google Scholar]
- 71.Gerber C, Blumenthal S, Curt A, Werner CM. Effect of selective experimental suprascapular nerve block on abduction and external rotation strength of the shoulder. J Shoulder Elbow Surg. 2007;16(6):815–20. doi: 10.1016/j.jse.2007.02.120. [DOI] [PubMed] [Google Scholar]
- 72.Hertel R, Ballmer FT, Lombert SM, Gerber C. Lag signs in the diagnosis of rotator cuff rupture. J Shoulder Elbow Surg. 1996;5(4):307–13. doi: 10.1016/S1058-2746(96)80058-9. [DOI] [PubMed] [Google Scholar]
- 73.Walch G., Boulahia A., Calderone S., Robinson A.H. The ‘dropping’ and ‘hornblower’s’ signs in evaluation of rotator-cuff tears. J. Bone Joint Surg. Br. 1998;80(4):624–628. doi: 10.1302/0301-620X.80B4.8651. [DOI] [PubMed] [Google Scholar]
- 74.Costouros JG, Espinosa N, Schmid MR, Gerber C. Teres minor integrity predicts outcome of latissimus dorsi tendon transfer for irreparable rotator cuff tears. J Shoulder Elbow Surg. 2007;16(6):727–34. doi: 10.1016/j.jse.2007.02.128. [DOI] [PubMed] [Google Scholar]
- 75.Nové-Josserand L., Costa P., Liotard J.P., Safar J.F., Walch G., Zilber S. Results of latissimus dorsi tendon transfer for irreparable cuff tears. Orthop. Traumatol. Surg. Res. 2009;95(2):108–113. doi: 10.1016/j.otsr.2008.10.002. [DOI] [PubMed] [Google Scholar]
- 76.Herzberg G, Urien JP, Dimnet J. Potential excursion and relative tension of muscles in the shoulder girdle: relevance to tendon transfers. J Shoulder Elbow Surg. 1999;8(5):430–7. doi: 10.1016/S1058-2746(99)90072-1. [DOI] [PubMed] [Google Scholar]
- 77.Codsi M.J., Hennigan S., Herzog R., Kella S., Kelley M., Leggin B., Williams G.R., Iannotti J.P. Latissimus dorsi tendon transfer for irreparable posterosuperior rotator cuff tears. Surgical technique. J. Bone Joint Surg. Am. 2007;89(Suppl. 2 Pt.1):1–9. doi: 10.2106/JBJS.F.01160. [DOI] [PubMed] [Google Scholar]
- 78.De Casas R., Lois M., Cidoncha M., Valadron M. Clinic and electromyographic results of latissimus dorsi transfer for irreparable posterosuperior rotator cuff tears. J. Orthop. Surg. 2014;9:83. doi: 10.1186/s13018-014-0083-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Valenti P., Kalouche I., Diaz L.C., Kaouar A., Kilinc A. Results of latissimus dorsi tendon transfer in primary or salvage reconstruction of irreparable rotator cuff tears. Orthop. Traumatol. Surg. Res. 2010;96(2):133–138. doi: 10.1016/j.otsr.2009.11.003. [DOI] [PubMed] [Google Scholar]
- 80.Lehmann L.J., Mauerman E., Strube T., Laibacher K., Scharf H.P. Modified minimally invasive latissimus dorsi transfer in the treatment of massive rotator cuff tears: a two-year follow-up of 26 consecutive patients. Int. Orthop. 2010;34(3):377–383. doi: 10.1007/s00264-009-0782-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Miniaci A., MacLeod M. Transfer of the latissimus dorsi muscle after failed repair of a massive tear of the rotator cuff. A two to five-year review. J. Bone Joint Surg. Am. 1999;81(8):1120–1127. doi: 10.2106/00004623-199908000-00007. [DOI] [PubMed] [Google Scholar]
- 82.Hamada K., Fukuda H., Mikasa M., Kobayashi Y. Roentgenographic findings in massive rotator cuff tears. A long-term observation. Clin. Orthop. Relat. Res. 1990;(254):92–96. [PubMed] [Google Scholar]
- 83.Samilson R.L., Prieto V. Dislocation arthropathy of the shoulder. J. Bone Joint Surg. Am. 1983;65(4):456–460. [PubMed] [Google Scholar]
- 84.Debeer P., De Smet L. Outcome of latissimus dorsi transfer for irreparable rotator cuff tears. Acta Orthop. Belg. 2010;76(4):449–455. [PubMed] [Google Scholar]
- 85.Werner CM, Conrad SJ, Meyer DC, Keller A, Hodler J, Gerber C. Intermethod agreement and interobserver correlation of radiologic acromiohumeral distance measurements. J Shoulder Elbow Surg. 2008;17(2):237–40. doi: 10.1016/j.jse.2007.06.002. [DOI] [PubMed] [Google Scholar]
- 86.Nové-Josserand L., Edwards T.B., O’Connor D.P., Walch G. The acromiohumeral and coracohumeral intervals are abnormal in rotator cuff tears with muscular fatty degeneration. Clin. Orthop. Relat. Res. 2005;(433):90–96. doi: 10.1097/01.blo.0000151441.05180.0e. [DOI] [PubMed] [Google Scholar]
- 87.Nove-Josserand L., Levigne C., Noel E., Walch G. The acromio-humeral interval. A study of the factors influencing its height. Rev. Chir. Orthop Repar. Appar. Mot. 1996;82(5):379–385. [PubMed] [Google Scholar]
- 88.Comtet J.J., Auffray Y. Physiology of the elevator muscles of the shoulder. Rev. Chir. Orthop Repar. Appar. Mot. 1970;56(2):105–117. [PubMed] [Google Scholar]
- 89.Goutallier D., Le Guilloux P., Postel J.M., Radier C., Bernageau J., Zilber S. Acromio humeral distance less than six millimeter: its meaning in full-thickness rotator cuff tear. Orthop. Traumatol. Surg. Res. 2011;97(3):246–251. doi: 10.1016/j.otsr.2011.01.010. [DOI] [PubMed] [Google Scholar]
- 90.Hersche O, Gerber C. Passive tension in the supraspinatus musculotendinous unit after long-standing rupture of its tendon: a preliminary report. J Shoulder Elbow Surg. 1998;7(4):393–6. doi: 10.1016/S1058-2746(98)90030-1. [DOI] [PubMed] [Google Scholar]
- 91.Flatow E.L., Raimondo R.A., Kelkar R., Wang W.M., et al. Active and passive restraints against superior humeral translation: the contributions of the rotator cuff the biceps tendon and the coracoacromial arch. J Shoulder Elbow Surg. 1996;5(2):111. doi: 10.1016/S1058-2746(96)80475-7. [DOI] [Google Scholar]
- 92.Parsons I.M., Apreleva M., Fu F.H., Woo S.L. The effect of rotator cuff tears on reaction forces at the glenohumeral joint. J. Orthop. Res. 2002;20(3):439–446. doi: 10.1016/S0736-0266(01)00137-1. [DOI] [PubMed] [Google Scholar]
- 93.Karduna A.R., Williams G.R., Williams J.L., Iannotti J.P. Kinematics of the glenohumeral joint: influences of muscle forces, ligamentous constraints, and articular geometry. J. Orthop. Res. 1996;14(6):986–993. doi: 10.1002/jor.1100140620. [DOI] [PubMed] [Google Scholar]
- 94.Wiley A.M. Superior humeral dislocation. A complication following decompression and debridement for rotator cuff tears. Clin. Orthop. Relat. Res. 1991;(263):135–141. [PubMed] [Google Scholar]
- 95.Thomazeau H., Rolland Y., Lucas C., Duval J.M., Langlais F. Atrophy of the supraspinatus belly. Assessment by MRI in 55 patients with rotator cuff pathology. Acta Orthop. Scand. 1996;67(3):264–268. doi: 10.3109/17453679608994685. [DOI] [PubMed] [Google Scholar]
- 96.Gladstone J.N., Bishop J.Y., Lo I.K., Flatow E.L. Fatty infiltration and atrophy of the rotator cuff do not improve after rotator cuff repair and correlate with poor functional outcome. Am. J. Sports Med. 2007;35(5):719–728. doi: 10.1177/0363546506297539. [DOI] [PubMed] [Google Scholar]
- 97.Iannotti J.P., Zlatkin M.B., Esterhai J.L., Kressel H.Y., Dalinka M.K., Spindler K.P. Magnetic resonance imaging of the shoulder. Sensitivity, specificity, and predictive value. J. Bone Joint Surg. Am. 1991;73(1):17–29. [PubMed] [Google Scholar]
- 98.Alavekios DA, Dionysian E, Sodl J, Contreras R, Cho Y, Yian EH. Longitudinal analysis of effects of operator experience on accuracy for ultrasound detection of supraspinatus tears. J Shoulder Elbow Surg. 2013;22(3):375–80. doi: 10.1016/j.jse.2012.09.017. [DOI] [PubMed] [Google Scholar]
- 99.Codsi MJ, Rodeo SA, Scalise JJ, Moorehead TM, Ma CB. Assessment of rotator cuff repair integrity using ultrasound and magnetic resonance imaging in a multicenter study. J Shoulder Elbow Surg. 2014;23(10):1468–72. doi: 10.1016/j.jse.2014.01.045. [DOI] [PubMed] [Google Scholar]
- 100.Millett P.J., Yen Y-M., Huang M.J. Arthroscopically assisted latissimus dorsi transfer for irreparable rotator cuff tears. Tech. Shoulder Elbow Surg. 2008;9(2):76–79. doi: 10.1097/BTE.0b013e318169e991. [DOI] [Google Scholar]
- 101.Kany J., Kumar H.A., Chang V.K., Grimberg J., Garret J., Valenti P. Mini invasive axillary approach and arthroscopic humeral head interference screw fixation for latissimus dorsi transfer in massive and irreparable posterosuperior rotator cuff tears. Tech. Shoulder Elbow Surg. 2010;11(1):8–14. doi: 10.1097/BTE.0b013e3181cabdab. [DOI] [Google Scholar]
- 102.Gervasi E, Causero A, Parodi PC, Raimondo D, Tancredi G. Arthroscopic latissimus dorsi transfer. Arthroscopy. 2007;23(11):1243.e1–1243.e4. doi: 10.1016/j.arthro.2006.12.021. [DOI] [PubMed] [Google Scholar]
- 103.Diop A., Maurel N., Chang V.K., Kany J., Duranthon L.D., Grimberg J. Tendon fixation in arthroscopic latissimus dorsi transfer for irreparable posterosuperior cuff tears: an in vitro biomechanical comparison of interference screw and suture anchors. Clin. Biomech. (Bristol, Avon) 2011;26(9):904–909. doi: 10.1016/j.clinbiomech.2011.05.011. [DOI] [PubMed] [Google Scholar]
- 104.Buijze G.A., Keereweer S., Jennings G., Vorster W., Debeer J. Musculotendinous transfer as a treatment option for irreparable posterosuperior rotator cuff tears: teres major or latissimus dorsi? Clin. Anat. 2007;20(8):919–923. doi: 10.1002/ca.20547. [DOI] [PubMed] [Google Scholar]
- 105.Zafra M., Carpintero P., Carrasco C. Latissimus dorsi transfer for the treatment of massive tears of the rotator cuff. Int. Orthop. 2009;33(2):457–462. doi: 10.1007/s00264-008-0536-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Pearsall A.W., IV, Madanagopal S.G., Karas S.G. Transfer of the latissimus dorsi as a salvage procedure for failed debridement and attempted repair of massive rotator cuff tears. Orthopedics. 2007;30(11):943–949. doi: 10.3928/01477447-20071101-19. [DOI] [PubMed] [Google Scholar]
- 107.Aoki M, Fukushima S, Okamura K, Yamada Y, Yamakoshi K. Mechanical strength of latissimus dorsi tendon transfer with Teflon felt augmentation. 1997. [DOI] [PubMed]
- 108.Villacis D., Merriman J., Wong K., Rick Hatch G.F., III Latissimus dorsi tendon transfer for irreparable rotator cuff tears: a modified technique using arthroscopy. Arthrosc. Tech. 2013;2(1):e27–e30. doi: 10.1016/j.eats.2012.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Hoffer M.M., Wickenden R., Roper B. Brachial plexus birth palsies. Results of tendon transfers to the rotator cuff. J. Bone Joint Surg. Am. 1978;60(5):691–695. [PubMed] [Google Scholar]
- 110.Lichtenberg S, Magosch P, Habermeyer P. Are there advantages of the combined latissimus-dorsi transfer according to L'Episcopo compared to the isolated latissimus-dorsi transfer according to Herzberg after a mean follow-up of 6 years? A matched-pair analysis. J Shoulder Elbow Surgery. 2012;21(11):1499–507. doi: 10.1016/j.jse.2012.01.002. [DOI] [PubMed] [Google Scholar]
- 111.Magermans D.J., Chadwick E.K., Veeger H.E., Rozing P.M., van der Helm F.C. Effectiveness of tendon transfers for massive rotator cuff tears: a simulation study. Clin. Biomech. (Bristol, Avon) 2004;19(2):116–122. doi: 10.1016/j.clinbiomech.2003.09.008. [DOI] [PubMed] [Google Scholar]
- 112.Aldridge JM, 3rd, Atkinson TS, Mallon WJ. Combined pectoralis major and latissimus dorsi tendon transfer for massive rotator cuff deficiency. J Shoulder Elbow Surg. 2004;13(6):621–9. doi: 10.1016/j.jse.2004.04.003. [DOI] [PubMed] [Google Scholar]
- 113.Henry PD, Dwyer T, McKee MD, Schemitsch EH. Latissimus dorsi tendon transfer for irreparable tears of the rotator cuff: An anatomical study to assess the neurovascular hazards and ways of improving tendon excursion. Bone Joint J. 2013;95-b(4):517–22. doi: 10.1302/0301-620X.95B4.30839. [DOI] [PubMed] [Google Scholar]
- 114.Schoierer O., Herzberg G., Berthonnaud E., Dimnet J., Aswad R., Morin A. Anatomical basis of latissimus dorsi and teres major transfers in rotator cuff tear surgery with particular reference to the neurovascular pedicles. Surg. Radiol. Anat. 2001;23(2):75–80. doi: 10.1007/s00276-001-0075-1. [DOI] [PubMed] [Google Scholar]
- 115.Boileau P, Chuinard C, Roussanne Y, Neyton L, Trojani C. Modified latissimus dorsi and teres major transfer through a single delto-pectoral approach for external rotation deficit of the shoulder: as an isolated procedure or with a reverse arthroplasty. J Shoulder Elbow Surg. 2007;16(6):671–82. doi: 10.1016/j.jse.2007.02.127. [DOI] [PubMed] [Google Scholar]
- 116.Kessler M.A., Lichtenberg S., Habermeyer P. Reconstruction of big rotator cuff ruptures. A new technique of tendon refixation with the corkscrew suture anchor system. Unfallchirurg. 2003;106(10):826–833. doi: 10.1007/s00113-003-0662-1. [DOI] [PubMed] [Google Scholar]
- 117.Irlenbusch U, Bracht M, Gansen HK, Lorenz U, Thiel J. Latissimus dorsi transfer for irreparable rotator cuff tears: a longitudinal study. J Shoulder Elbow Surg. 2008;17(4):527–34. doi: 10.1016/j.jse.2007.11.022. [DOI] [PubMed] [Google Scholar]
- 118.Groh GI, Simoni M, Rolla P, Rockwood CA. Loss of the deltoid after shoulder operations: An operative disaster. J Shoulder Elbow Surgery. 1994;3(4):243–53. doi: 10.1016/S1058-2746(09)80042-6. [DOI] [PubMed] [Google Scholar]
- 119.Feeley BT, Gallo RA, Craig EV. Cuff tear arthropathy: current trends in diagnosis and surgical management. J Shoulder Elbow Surgery. 2009;18(3):484–94. doi: 10.1016/j.jse.2008.11.003. [DOI] [PubMed] [Google Scholar]
- 120.Jensen K.L., Williams G.R., Jr, Russell I.J., Rockwood C.A., Jr Rotator cuff tear arthropathy. J. Bone Joint Surg. Am. 1999;81(9):1312–1324. doi: 10.2106/00004623-199909000-00013. [DOI] [PubMed] [Google Scholar]
- 121.Macaulay A.A., Greiwe R.M., Bigliani L.U. Rotator cuff deficient arthritis of the glenohumeral joint. Clin. Orthop. Surg. 2010;2(4):196–202. doi: 10.4055/cios.2010.2.4.196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Hamada K., Yamanaka K., Uchiyama Y., Mikasa T., Mikasa M. A radiographic classification of massive rotator cuff tear arthritis. Clin. Orthop. Relat. Res. 2011;469(9):2452–2460. doi: 10.1007/s11999-011-1896-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Boileau P, Watkinson D, Hatzidakis AM, Hovorka I. Neer Award 2005: The Grammont reverse shoulder prosthesis: results in cuff tear arthritis, fracture sequelae, and revision arthroplasty. J Shoulder Elbow Surgery. 2006;15(5):527–40. doi: 10.1016/j.jse.2006.01.003. [DOI] [PubMed] [Google Scholar]
- 124.Boulahia A., Edwards T.B., Walch G., Baratta R.V. Early results of a reverse design prosthesis in the treatment of arthritis of the shoulder in elderly patients with a large rotator cuff tear. Orthopedics. 2002;25(2):129–133. doi: 10.3928/0147-7447-20020201-16. [DOI] [PubMed] [Google Scholar]
- 125.Hurschler C, Wulker N, Windhagen H, Hellmers N, Plumhoff P. Evaluation of the lag sign tests for external rotator function of the shoulder. J Shoulder Elbow Surgery. 2004;13(3):298–304. doi: 10.1016/j.jse.2004.01.021. [DOI] [PubMed] [Google Scholar]
- 126.Fuchs B, Weishaupt D, Zanetti M, Hodler J, Gerber C. Fatty degeneration of the muscles of the rotator cuff: assessment by computed tomography versus magnetic resonance imaging. J Shoulder Elbow Surgery. 1999;8(6):599–605. doi: 10.1016/S1058-2746(99)90097-6. [DOI] [PubMed] [Google Scholar]
- 127.El-Azab H.M., Rott O., Irlenbusch U. Long-term follow-up after latissimus dorsi transfer for irreparable posterosuperior rotator cuff tears. J. Bone Joint Surg. Am. 2015;97(6):462–469. doi: 10.2106/JBJS.M.00235. [DOI] [PubMed] [Google Scholar]
- 128.Moor BK, Bouaicha S, Rothenfluh DA, Sukthankar A, Gerber C. Is there an association between the individual anatomy of the scapula and the development of rotator cuff tears or osteoarthritis of the glenohumeral joint?: A radiological study of the critical shoulder angle. Bone Joint J. 2013;95-b(7):935–41. doi: 10.1302/0301-620X.95B7.31028. [DOI] [PubMed] [Google Scholar]
- 129.Donaldson J., Pandit A., Noorani A., Douglas T., Falworth M., Lambert S. Latissimus dorsi tendon transfers for rotator cuff deficiency. Int. J. Shoulder Surg. 2011;5(4):95–100. doi: 10.4103/0973-6042.91002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Gerhardt C., Lehmann L., Lichtenberg S., Magosch P., Habermeyer P. Modified L’Episcopo tendon transfers for irreparable rotator cuff tears: 5-year follow-up. Clin. Orthop. Relat. Res. 2010;468(6):1572–1577. doi: 10.1007/s11999-009-1030-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Erşen A., Ozben H., Demirhan M., Atalar A.C., Kapıcıoğlu M. Time-dependent changes after latissimus dorsi transfer: tenodesis or tendon transfer? Clin. Orthop. Relat. Res. 2014;472(12):3880–3888. doi: 10.1007/s11999-014-3770-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Paribelli G., Boschi S., Randelli P., Compagnoni R., Leonardi F., Cassarino A.M. Clinical outcome of latissimus dorsi tendon transfer and partial cuff repair in irreparable postero-superior rotator cuff tear. Musculoskelet. Surg. 2015;99(2):127–132. doi: 10.1007/s12306-015-0353-4. [DOI] [PubMed] [Google Scholar]


