Abstract
Ischemic heart diseases are the leading cause of morbidity and mortality worldwide. Reperfusion of an ischemic heart is necessary to regain the normal functioning of the heart. However, abrupt reperfusion of an ischemic heart elicits a cascade of adverse events that leads to injury of the myocardium, i.e., ischemia–reperfusion injury. An endogenous powerful strategy to protect the ischemic heart is ischemic preconditioning, in which the myocardium is subjected to short periods of sublethal ischemia and reperfusion before the prolonged ischemic insult. However, it should be noted that the cardioprotective effect of preconditioning is attenuated in some pathological conditions. The aim of this article is to review present knowledge on how menopause and some metabolic disorders such as diabetes and hyperlipidemia affect myocardial ischemic preconditioning and the mechanisms involved.
Keywords: Diabetes, Hyperlipidemia, Ischemic preconditioning, Menopause
Abbreviations
- I/R
ischemia/reperfusion
- IPC
ischemic preconditioing
- ROS/RNS
reactive oxygen or nitrogen species
- PI3K
phosphatidylinositol 3-kinase
- PIP3
phosphatidyl-inositol 3,4,5-triphosphate
- PIP2
phosphatidyl inositol 3,4-biphosphate
- PDK
phosphoinositide-dependent kinase
- Akt
protein kinase B
- PKC
protein kinase C
- GSK3β
glycogen synthase kinase-3β
- NO
nitric oxide
- mitoKATP
mitochondrial ATP-sensitive potassium channels
- DAG
diacylglycerol
- IP3
inositol triphosphate
- ROS
reactive oxygen species
- MAPK
mitogen activated protein kinases
- ERK
extracellular signal-regulated kinases
- mPTP
mitochondrial permeability transition pore
- ATP
adenosine triphosphate
- eNOS
endothelial nitric oxide synthase
- RISK
reperfusion injury salvage kinase
- GSH
glutathione
- iNOS
inducible nitric oxide synthase
- MMP
matrix metalloproteinases
- STZ
streptozotocin
- TNF
tumour necrosis factor
- NADPH
nicotinamide adenine dinucleotide phosphate
- ER
estrogen receptor
- AR
adrenergic receptor
Introduction
Coronary heart disease is a leading and growing problem in most of the developing regions of the world and the most common mode of cardiovascular death is ischemic heart disease and stroke [1]. Myocardial ischemia occurs when there is insufficient blood supply to the myocardium [2]. Although early reperfusion protects the myocardium from damage, reperfusion after a prolonged ischemic insult causes tissue injury, i.e., ischemia–reperfusion (I/R) injury [3], [4]. It is characterized by a cascade of adverse events—local inflammatory responses, metabolic disorder, and cell death—leading to myocardial ultrastructural changes and subsequently myocardial systolic and diastolic dysfunction [5], [6], [7]. Some experimental studies suggest that reactive oxygen species (ROS) or reactive nitrogen species, including superoxide radicals, hydrogen peroxide, hydroxyl radicals, singlet oxygen and peroxynitrite (ONOO−) are mainly responsible for myocardial I/R injury [8], [9].
Ischemic preconditioning and its molecular mechanism
The strategy to prevent I/R injury was given by Murry and coworkers [10] in 1986. They showed that brief intermittent periods of sublethal ischemia followed by reperfusion have a protective effect on myocardial tissue against prolonged ischemic insult; this is called ischemic preconditioning (IPC) [10], [11]. IPC is found to be a biphasic phenomenon: an early phase that starts within minutes and wanes off gradually within 2–3 hours, called classical preconditioning [12], [13]; and the late phase, which is delayed to 12–24 hours after the ischemic stress and lasts up to 3–4 days, and is called late-phase preconditioning or second window of protection [14], [15]. The early phase of IPC protects only against the myocardial infarction but the late-phase IPC also protects against myocardial stunning [16], [17].
Preconditioning results in the generation and release of various endogenous ligands, thus leading to activation of their corresponding receptors [18]. The endogenous ligands generated and released during ischemia and reperfusion are adenosine [19], bradykinin [20], [21], opioids [22] norepinephrine [23], and acetylcholine [24]. They bind to their respective G-protein coupled receptors and initiate a cascade of signal transduction, which leads to activation of phosphatidylinositol 3-kinase (PI3K) [25] and phospholipase C [26].
Activated PI3K generates phosphatidyl-inositol 3,4,5-triphosphate from cell membrane lipid phosphatidyl inositol 3,4-biphosphate leading to activation of phosphoinositide-dependent kinase 1 (PDK1) and subsequent activation of protein kinase B (Akt) and p70S6-kinase [27], [28]. PI3K/Akt activation upregulates protein kinase C (PKC) [29], phosphorylation of glycogen synthase kinase-3β (GSK3β) [30], generation of nitric oxide (NO) [29], and activates the mitochondrial adenosine triphosphate-sensitive potassium channels (mitoKATP) [31], [32].
The activated phospholipase C leads to generation of two second messengers (diacylglycerol and inositol triphosphate) by hydrolysis of phosphatidyl inositol 3,4-biphosphate. Diacylglycerol activates protein kinase C by translocating it from cytosol to the perinuclear membrane [33], [34]. PKC activation has been shown to be important in the opening of mitoKATP [35]. PKCε and PKCδ have been demonstrated to mimic preconditioning due to opening of mitoKATP [36]. As potassium enters the mitochondria, it causes them to release free radicals, known as ROS [37]. ROS generation during preconditioning also activates PKC [38], [39]. Although a large burst of ROS leads to cell damage, a moderate release during nonlethal short episodes of ischemia plays a significant triggering role in the signal transduction pathways of IPC [40]. PKCε also forms a complex with mitochondrial permeability transition pore (mPTP) [41], [42], which leads to a decrease in the release of cytochrome C and apoptotic cell death [43], [44]. In addition, IPC also activates extracellular signal-regulated kinase (ERK)1/2 during the preconditioning phase as well as the reperfusion phase, which mediates the inhibition of mPTP opening through various mechanisms [45].
More recent interest has focused on GSK-3β, phosphorylated (and hence inactivated) by other kinases, including Akt and p42/p44 ERK1/2 mitogen activated protein kinase [30], [46]. GSK-3β plays a crucial role in apoptosis and necrosis of cardiomyocytes [47]. Experimental studies have reported that GSK-3β confers cardioprotective effects through its potential mitochondrial effects including inhibition of mPTPs opening and control of mitochondrial adenine nucleotide transport through the outer mitochondrial membrane [48], [49], [50].
Although IPC provides a remarkable cardioprotection, its effectiveness is attenuated in animal models of some diseases, including hyperlipidemia, diabetes, nitrate tolerance, heart failure, menopause in women, and aging due to alteration in intracellular signaling relevant to cytoprotection and thus myocardial responses to IPC [51], [52].
Methods
Relevant studies were identified through electronic searches of Pubmed, Medline, Scopus, and Google scholar. The search used the terms “ischemia reperfusion,” “ischemia reperfusion injury,” or “ischemic preconditioning,” paired with “diabetes mellitus,” “hyperlipidemia,” “hypercholesterolemia,” “postmenopause,” and “ovariectomized,”. In addition, we searched the bibliographies of relevant studies, reviews, and editorial letters between 1983 and 2016 for articles in English.
Diabetes mellitus
Diabetes mellitus is a disorder of carbohydrate, protein, and lipid metabolism affecting many organs, which ultimately leads to severe acute and chronic complications [53]. Hyperglycemia has been reported to impair coronary microvascular responses to ischemia [54], reduces the availability of nitric oxide [55], and enhances the oxygen derived free radical production [56].
I/R injury in the diabetic heart
Ischemic heart disease is significantly more common and severe in patients with diabetes than in nondiabetics [57]. However, it is unclear whether resistance to ischemia is greater or lower in diabetic hearts [58], [59]. Moreover, in patients with diabetes, the mortality rate after an acute myocardial infarction or coronary bypass surgery is almost double that of nondiabetics [60].
Insulin modulates the glucose transport, glycogen synthesis, glycolysis, protein synthesis, lipid metabolism, growth, contractility, and apoptosis in cardiomyocytes. Thus the reduction of these insulin-stimulated effects may be responsible for the increased myocardial injury during ischemia and reperfusion in diabetic patients [61], [62]. Diabetes mellitus also disturbs the function of cardiac subcellular organelles, including the sarcolemma, sarcoplasmic reticulum, and mitochondria [63]. The lower glycolytic rates and impaired oxidation result in loss of ATP [64], altered expression of adenosine receptors [65], and impairment of KATP channels [66], which worsen the I/R induced myocardial injury.
In contrast, some experimental studies showed that the diabetic heart is resistant to I/R injury [67], [68], [69], which may be due to elevated antioxidant defenses [70], [71], depressed sarcoplasmic reticulum calcium pump activities [72], depressed sodium–calcium exchange [73], decreased sensitivity of β-adrenergic stimulation [74], [75], upregulation of PKC [76], and release of protective calcitonin gene related peptide [77].
Impact of diabetes on IPC and mechanisms involved
It has been documented that IPC-induced cardioprotection is attenuated or eliminated in rats with spontaneous Type 2 diabetes [78] and the myocardium from patients with diabetes cannot be protected by preconditioning [79]. Unfortunately, however, research on whether the diabetic myocardium can be protected by IPC is in conflict [80]; some studies have reported that diabetic hearts can be protected by IPC [81], [82], and the majority have reported fewer or no protective effects [82], [83], [84].
It has been suggested that KATP channels in the myocytes of streptozotocin-induced diabetic rats open at higher intracellular ATP levels than do KATP channels in normal control rats [85], which may be one hurdle in IPC-induced cardioprotection in the diabetic heart. One reason of failure to precondition the diabetic myocardium that has been also reported is dysfunction in mitochondrial superoxide production [86], which is an important element of the signal transduction pathway of preconditioning [87]. Diabetes also alters the function of vascular and myocardial KATP channels [85], [88]. In addition to this, channel density also appears to be diminished in diabetic hearts [89], and this may be one reason for IPC not developing in diabetic hearts.
It has been observed in that attenuation of the cardioprotective effect of IPC in diabetic rat heart is due to some defect in the caveolin–endothelial nitric oxide synthase (eNOS) complex in diabetic heart, which leads to a decrease in the availability of NO and the consequent decreased activation of mitoKATP channels [90]. Moreover, the loss of preconditioning is also observed in the presence of sulfonylurea drugs [91], [92], and the mechanism of this has been found to be inhibition of KATP channels present in both pancreatic β cells [93] and cardiac myocytes [94].
Tsang and coworkers [95] for the first time reported that the Type2 diabetic myocardium can be protected by IPC, but the threshold required to achieve this protection is greater than that required for nondiabetic hearts, and this elevated threshold is required to achieve sufficient phosphorylation of Akt to execute the IPC protective signal. By contrast, Tatsumi and coworkers [81] found less cumulative creatine kinase release in preconditioned diabetic hearts than in normal hearts, and thus concluded that, in the diabetic myocardium, preconditioning may offer greater protection than in the normal myocardium. Further, hyperglycemia may lead to upregulation of endogenous stress protein, i.e., hsp-27 in Type 1 diabetic mice, which has a potential role in cardioprotection and compensates for detrimental effects of hyperglycemia [96].
However, whether diabetes eliminates IPC mediated myocardial protection depends on IPC times or the periods of diabetes. For instance, Ting and co-workers [97] showed that mice with diabetes for 4 weeks showed tolerance to I/R induced damage comparable to normal rats and partial IPC-induced myocardial protection, while mice with diabetes for 8 weeks showed low tolerance to I/R-induced damage compared to normal rats and no evidence of IPC induced myocardial protection. In another study on streptozotocin-induced diabetic rat heart, it was reported that the 2-week diabetic heart was resistant to I/R injury, but the protection was not shown in 4-week and 6-week diabetic hearts, and there is a worse outcome of I/R in 8-week diabetic hearts [84].
Furthermore, it has been demonstrated that diabetes-induced activation of GSK-3β and impairment of the reperfusion injury salvage kinase pathway play important roles in diabetes-induced myocardial oxidative damage [98]. It is well known that IPC produces myocardial protection by phosphorylation and thus inactivation of GSK-3β that inhibits the opening of mPTP, but the activity of GSK-3β was found to be elevated during diabetes [99], [47], [100]. In our laboratory, Yadav and coworkers [101] investigated the role of GSK-3β in attenuating the cardioprotective effect of IPC using a Type-1 diabetic rat model and found that the cardioprotective effect of IPC was significantly attenuated in diabetic rats compared to normal rats. At the same time, they found that GSK-3β inhibitors, including lithium chloride, indirubin-3 monooxime, and SB216763, significantly reduced the myocardial damage and decreased infarct size in diabetic rat myocardium. This study suggests that diabetes-induced attenuation of myocardial protection mediated by IPC involves the activation of GSK-3β.
Emerging evidence indicates that IPC-mediated myocardial protection is predominantly mediated by stimulating PI3K/Akt and the associated GSK-3β pathway while diabetes-mediated pathogenic effects are found to be mediated by inhibiting this pathway. Therefore, we may activate PI3K/Akt indirectly to inactivate the GSK-3β pathway or use the GSK-3β inactivator directly to inactivate the GSK-3β pathway to preserve IPC-mediated myocardial protection under diabetic conditions. However, further studies are required to observe the involvement of proposed mechanisms in attenuation of IPC-mediated myocardial protection in hyperglycemic patients. The possible mechanisms involved in hyperglycemia-induced attenuation of cardioprotective effect of IPC are shown in Fig. 1.
Fig. 1.
Mechanisms involved in hyperglycemia induced attenuation of cardioprotective effect of preconditioning. eNOS = endothelial nitric oxide synthase; GSK3β = glycogen synthase kinase-3β; KATP = adenosine triphosphate-sensitive potassium channels; NO = nitric oxide.
Hyperlipidemia/hypercholesterolemia
Hyperlipidemia is a well-known risk factor in development of cardiovascular diseases, as it contributes to the formation of atherosclerotic plaques in coronary vessel [102]. Although many of the studies have shown that hyperlipidemia attenuates the IPC-induced cardioprotection, there is a controversy as to whether hyperlipidemia interferes with the infarct size-limiting effect of preconditioning [52]. This may be attributed to differences in hyperlipidemia models (species, duration of hyperlipidemic diet, presence of significant coronary sclerosis).
I/R injury in hyperlipidemic heart
Some experimental studies have reported that hypercholesterolemia increases the myocardial infarct size in rabbits subjected to I/R after exposure to short-term (2–3 weeks) cholesterol diet compared to rabbits fed a long-term (5–16 weeks) cholesterol diet or a normal diet [103]. Golino and coworkers [104] reported that the myocardial infarct size was dramatically increased in rabbits subjected to ischemia and reperfusion after only a 3-day cholesterol diet. In mice, however, short-term high cholesterol diet does not influence the infarct size in wild-type animals, although it markedly increases the infarct size in low-density lipoprotein receptor deficient animals [105]. However, long-term (>6 weeks) high cholesterol diet protects the myocardium from I/R injury in rabbits [106] and in wild-type and low-density lipoprotein receptor deficient mice [105]. These opposing findings may be attributed to reduction of myocardial glutathione levels after a 2-week cholesterol diet but increased glutathione levels after 12 weeks [105]. It has also been reported that hyperlipidemia prevents the normal reduction of myocardial ischemia on repeated balloon inflations during angioplasty in humans [107].
Impact of hyperlipidemia on ischemic preconditioning and mechanisms involved
Hypercholesterolemia, irrespective of the development of atherosclerosis, interferes with the cardioprotective mechanisms of IPC [108]. This loss of preconditioning was further confirmed in isolated hearts of rat with chronic exposure to cholesterol diet [109]. It has been well documented by means of a beat-to-beat analysis of ST segments that hypercholesterolemia attenuates the IPC-induced anti-ischemic effect, accelerates the evolution of myocardial ischemia, and delays the reperfusion recovery from ischemia in humans [110].
Researchers were able to induce late preconditioning in hyperlipidemic rabbits only when the numbers of IPC cycles was increased compared to that applied in normolipidemic rats to induce late preconditioning [111], which suggests that the threshold to trigger cardioprotection is increased in experimental hyperlipidema. Hypercholesterolemia abrogates the late preconditioning, possibly by preventing upregulation of tetrahydrobiopterin synthesis, an essential cofactor for inducible NO synthase [112].
Hypercholesterolemia causes oxidative/nitrosative stress leading to myocardial dysfunction [113]. It has been observed that the reduced NO release from rabbit aorta in hypercholesterolemia [114] and the high cholesterol concentrations in endothelial cell membranes caused downregulation of NO synthase [115]. Reduced vascular NO release in hyperlipidemia has been also shown as a consequence of increased release of superoxide, which then reacts with NO to form ONOO− [116], [117].
It has been established that cholesterol-enriched diet-induced hyperlipidemia leads to increase in cardiac ONOO− formation and a decrease in the NO bioavailability which leads to the deterioration of cardiac performance and further cardiac pathologies [118]. This peroxynitrite is also responsible for rapidly increasing the release of a large family of zinc endopeptidases, matrix metalloproteinases (MMPs) in coronary effluent via a nonproteolytic oxidative mechanism resulting in fully active proenzymes [119], [120]. Moreover, hyperlipidemia has been shown to diminish IPC-induced inhibition of myocardial MMP-2 activation and release in to the coronary perfusate [121]. This MMP-2 promotes vasoconstriction in rat mesenteric arteries [122], and ischemia-induced activation and release of MMP-2 contributes to acute mechanical dysfunction after I/R in rat hearts [123], [124].
One study suggested that in hyperlipidemia, there is an alteration in one of the main signal transduction elements, i.e., distribution of the intracellular localization of Connexin 43 in the heart that takes part in gap junction formation and thus in electrical and chemical coupling of cardiomyocytes, and in that study the protective effect of preconditioning was found to be lost in hyperlipidemia [125]. In addition, hyperlipidemia has been shown to suppress the opening of mitoKATP channels in the rabbit heart subjected to I/R [126].
The antihyperlipidemic drugs, statins increase the half-life of NO synthase mRNA in human saphenous vein endothelial cells [127], increase PI3K activity in cultured human umbilical vein endothelial cells and bovine aortic endothelial cells [128] and adenosine production in SV40-transfected aortic rat endothelial cells [129], showing the cardioprotective effect independently of cholesterol-lowering effects. Thus, it seems a possible explanation that cholesterol-enriched diet-induced hypercholesterolemia increases nicotinamide adenine dinucleotide phosphate oxidase and cardiac superoxide, thereby leading to increased peroxynitrite production, resulting in activation of MMPs that ultimately leads to cardiac dysfunction. Thus lowering of serum cholesterol, targeting ONOO− with pharmacological tools, and pharmacological inhibition of MMP-2 may be new strategies to protect the heart and the vasculature in hyperlipidemia. Taken together, further studies are requisite to elucidate the interference of hyperlipidemia with the infarct size-limiting effect of preconditioning. Possible mechanisms involved in hyperlipidemia induced attenuation of cardioprotective effect of preconditioning are shown in Fig. 2.
Fig. 2.
Mechanisms involved in hyperlipidemia induced attenuation of cardioprotective effect of preconditioning. mitoKATP = mitochondrial adenosine triphosphate-sensitive potassium channels; MMP = matrix metalloproteinases; NO = nitric oxide.
Postmenopause
The incidence of coronary heart disease is relatively low among premenopausal women and increases sharply with the occurrence of menopause [130], which indicates that the female sex hormones, particularly estrogen, play a crucial role in reducing the risk of ischemic heart diseases [131], [132]. Although animal models with surgical menopause (ovariectomy) indicate the cardioprotective effect of estrogen replacement [133], [134], some clinical trials failed to demonstrate any cardioprotection from such estrogen replacement therapy [135], [136]. In fact, the incidence of ischemic heart disease was increased in women receiving estrogen compared to those receiving placebo [136].
I/R injury in postmenopausal heart
Cardiomyocytes from female hearts are more resistant to I/R injury than those from male hearts [137]. There are sex differences in the myocardial response to acute I/R injury, and the increased phosphorylated Akt and phosphorylated PKCε levels in female hearts are responsible for these sex-related differences in heart susceptibility to I/R and play an important role in cardioprotection against I/R injury in female hearts [138].
Cardiac myocytes and some other cardiac cells produce tumor necrosis factor (TNF)-α [139], and the increased TNF-α levels after an ischemic event contribute to myocardial injury [140]. Estrogen deficiency and menopause are associated with increased TNF-α levels, which may lead to increased myocardial injury after menopause [141]. In another study, it is reported that decreased mitochondrial respiration and increased mPTP opening with aging are responsible for necrotic cell death associated with I/R injury in aged female rats [142].
Impact of menopause on ischemic preconditioning and mechanisms involved
Shinmura and coworkers [143] demonstrated that the cardioprotective effect of IPC is lost in ovariectomized (surgical menopause) rats, which is partly due to impaired translocation of PKCε to the membranous fraction and phosphorylation of PKCε and PDK1. However, estrogen replacement or selective activation of PKCε-mediated signaling can fully restore the IPC effect, the translocation and phosphorylation of PKCε, and the phosphorylation of PDK1 [143]. It has been well documented by our laboratory that ovariectomy reduces the activity of eNOS in cardiac tissue due to upregulation of its inhibitory protein caveolin [144], but the chronic estrogen treatment accompanies restoration of normal activity of myocardial eNOS [145].
Endogenous and exogenous estrogen in pre- and postmenopausal women, respectively, protects against the cardiovascular disease [146], [147]. Estrogen acts as a vasoprotective molecule by increasing bioavailability of NO [148], [149]. Estrogen upregulates eNOS and downregulates its inhibitory protein, caveolin-1 [150], [151]. The effect of estrogen on eNOS expression is mediated via estrogen receptor (ER)α and ERβ, which are present on endothelial cells [152]. Activation of eNOS by estrogen has been reported to occur through the ERK-1/2 [153] pathway as well as via the PI3K/Akt pathway [154], [155], [156]. The recruitment of the latter cascade depends on the ligand dependent association of ERα with PI3K [154]. Akt can be activated by estrogen [157], which further activates eNOS by phosphorylating it at serine 1177 residue [158], [159]. This phosphorylation not only activates eNOS but also increases the efficiency of activation by Ca++/calmodulin [160]. Thus estrogen increases the bioavailability of NO and thus results in decrease in myocardial injury. In addition, 17β-estradiol has been shown to reduce myocardial necrosis in rabbits after I/R [161] and improve recovery of mechanical function following global ischemia in isolated rat hearts [162], [163]. The cardioprotective effects of estrogen are in part mediated by regulation of TNFα levels in the ischemic heart [164].
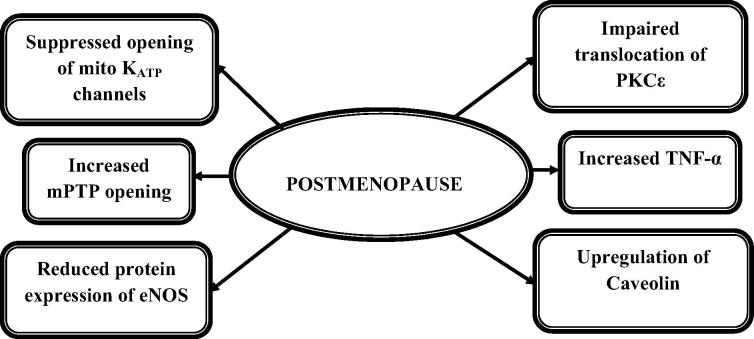
It has been found that the development of cardiovascular diseases after menopause is not only due to the decrease in estrogen but also due to the decrease in androgen [165]. Furthermore, it has been reported that testosterone enhances estradiol’s cardioprotection in ovariectomized rats, estradiol and testosterone combination protects cardiomyocytes against I/R injury, and the protective effects are at least partly mediated by β2-adrenergic receptor [166]. These findings illustrate the need for better understanding of changes contributing to impaired ischemic tolerance in the postmenopausal heart and for finding the alternative therapeutics to reduce injury during myocardial infarction in postmenopausal women. The possible mechanisms involved in menopause-induced attenuation of the cardioprotective effect of IPC are shown in Fig. 3.
Fig. 3.
Mechanisms involved in menopause-induced attenuation of cardioprotective effect of preconditioning. eNOS = endothelial nitric oxide synthase; mitoKATP = mitochondrial adenosine triphosphate-sensitive potassium channels; mPTP = mitochondrial permeability transition pore; PKC = protein kinase C; TNF = tumor necrosis factor.
Conclusion
The cardioprotective potential of IPC is well established, but it is lost in various clinical conditions such as hyperglycemia, hypercholesterolemia, and menopause. In these conditions the outcome of I/R injury worsens and the infarct size-limiting effect of IPC is blunted. This may affect the clinical application of IPC in patients undergoing cardiac surgery who also have the above mentioned clinical conditions. Therefore, there is a need to explore the underlying mechanisms of altered IPC-induced cardioprotection in various clinical conditions in order to identify the rational approaches for the protection of hyperglycemic, hyperlipidemic, and postmenopausal heart.
Acknowledgments
We are grateful to Mr Narayan Das Agrawal, Chancellor, GLA University, Dr Pradeep Mishra, Director, Institute of Pharmaceutical Research, GLA University, and Dr Anoop Kumar Gupta, Director, Institute of Applied Sciences and Humanities, GLA University, Mathura, Uttar Pradesh, India for their praiseworthy inspiration and constant support for this study.
Disclosure: Authors have nothing to disclose with regard to commercial support.
Footnotes
Peer review under responsibility of King Saud University.
References
- 1.Gersh B.J., Sliwa K., Mayosi B.M., Yusuf S. The epidemic of cardiovascular disease in the developing world: global implications. Eur Heart J. 2010;31:642–648. doi: 10.1093/eurheartj/ehq030. [DOI] [PubMed] [Google Scholar]
- 2.Gasser R., Schafhalter I., Wolff P., Schwarz T., Fürschuss W., Klein W. Experimental models and definitions of myocardial ischemia: a review. Int J Angiol. 1994;3:154–156. [Google Scholar]
- 3.Kloner R.A. Does reperfusion injury exist in humans? J Am Coll Cardiol. 1993;21:537–545. doi: 10.1016/0735-1097(93)90700-b. [DOI] [PubMed] [Google Scholar]
- 4.Collard C.D., Gelman S. Pathophysiology, clinical manifestation and prevention of ischemia reperfusion injury. Anesthesiology. 2001;94:1133–1138. doi: 10.1097/00000542-200106000-00030. [DOI] [PubMed] [Google Scholar]
- 5.Matsumura K., Jeremy R.W., Schaper J., Becker L.C. Progression of myocardial necrosis during reperfusion of ischemic myocardium. Circulation. 1998;97:795–804. doi: 10.1161/01.cir.97.8.795. [DOI] [PubMed] [Google Scholar]
- 6.Frangogiannis N.G., Smith C.W., Entman M.L. The inflammatory response in myocardial infarction. Cardiovasc Res. 2002;53:31–47. doi: 10.1016/s0008-6363(01)00434-5. [DOI] [PubMed] [Google Scholar]
- 7.Zhao Z.Q., Corvera J.S., Halkos M.E., Kerendi F., Wang N.P., Guyton R.A. Inhibition of myocardial injury by ischemic postconditioning during reperfusion comparison with ischemic preconditioning. Am J Physiol Heart Circ Physiol. 2003;285:H579–H588. doi: 10.1152/ajpheart.01064.2002. [DOI] [PubMed] [Google Scholar]
- 8.Park J.L., Lucchesi B.R. Mechanisms of myocardial reperfusion injury. Ann Thorac Surg. 1999;68:1905–1912. doi: 10.1016/s0003-4975(99)01073-5. [DOI] [PubMed] [Google Scholar]
- 9.Rosano G.M.C., Fini M., Caminiti G., Barbaro G. Cardiac metabolism in myocardial ischemia. Curr Pharm Des. 2008;14:2551–2562. doi: 10.2174/138161208786071317. [DOI] [PubMed] [Google Scholar]
- 10.Murry C.E., Jennings R.B., Reimer K.A. Preconditioning with ischemia: a delay of lethal cell injury in ischemic myocardium. Circulation. 1986;74:1124–1136. doi: 10.1161/01.cir.74.5.1124. [DOI] [PubMed] [Google Scholar]
- 11.Tomai F., Crea F., Chiariello L., Gioffre P.A. Ischemic preconditioning in humans: models, mediators, clinical relevance. Circulation. 1999;100:559–563. doi: 10.1161/01.cir.100.5.559. [DOI] [PubMed] [Google Scholar]
- 12.Downey M., Cohen M.V. Preconditioning: what it is and how it works. Dial Cardiovasc Med. 1997;2:179–196. [Google Scholar]
- 13.Yellon D.M., Downey J.M. Preconditioning the myocardium: from cellular physiology to clinical cardiology. Physiol Res. 2003;83:1113–1115. doi: 10.1152/physrev.00009.2003. [DOI] [PubMed] [Google Scholar]
- 14.Kuzuya T., Hoshida S., Yamashita N., Fuji H., Oe H., Hori M. Delayed effects of sublethal ischemia on the acquisition of tolerance to ischemia. Circ Res. 1993;72:1293–1299. doi: 10.1161/01.res.72.6.1293. [DOI] [PubMed] [Google Scholar]
- 15.Marber M.S., Latchman D.S., Walker J.M., Yellon D.M. Cardiac stress protein elevation 24 hours after brief ischemia or heat stress is associated with resistance to myocardial infarction. Circulation. 1993;88:1264–1272. doi: 10.1161/01.cir.88.3.1264. [DOI] [PubMed] [Google Scholar]
- 16.Bolli R. The early and late phases of preconditioning against myocardial stunning and the essential role of oxyradicals in the late phase: an overview. Basic Res Cardiol. 1996;91:57–63. doi: 10.1007/BF00788866. [DOI] [PubMed] [Google Scholar]
- 17.Sisakiyan H. Pathophysiology, clinical significance and possibilities of cardioprotection in myocardial stunning, hibernation and preconditioning. New Am Med J. 2008;2:28–34. [Google Scholar]
- 18.Murphy E. Primary and secondary signaling pathways in early preconditioning that converge on the mitochondria to produce cardioprotection. Circ Res. 2004;94:7–16. doi: 10.1161/01.RES.0000108082.76667.F4. [DOI] [PubMed] [Google Scholar]
- 19.Liu G.S., Thornton J., Van Winkle D.M., Stanley A.W., Olsson R.A., Downey J.M. Protection against infarction afforded by preconditioning is mediated by A1 adenosine receptors in rabbit heart. Circulation. 1991;84:350–356. doi: 10.1161/01.cir.84.1.350. [DOI] [PubMed] [Google Scholar]
- 20.Goto M., Liu Y., Yang X.M., Ardell J.L., Cohen M.V., Downey J.M. Role of bradykinin in protection of ischemic preconditioning in rabbit hearts. Circ Res. 1995;77:611–621. doi: 10.1161/01.res.77.3.611. [DOI] [PubMed] [Google Scholar]
- 21.Cohen M.V., Philipp S., Krieg T., Cui L., Kuno A., Solodushko V. Preconditioning mimetics bradykinin and DADLE activate PI3K through divergent pathways. J Mol Cell Cardiol. 2007;42:842–851. doi: 10.1016/j.yjmcc.2007.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schultz J.E., Rose E., Yao Z., Gross G.J. Evidence for involvement of opioid receptors in ischemic preconditioning in rat hearts. Am J Physiol. 1995;268:H2157–H2161. doi: 10.1152/ajpheart.1995.268.5.H2157. [DOI] [PubMed] [Google Scholar]
- 23.Banerjee A., Locke-Winter C., Rogers K.B., Mitchell M.B., Brew E.C., Cairns C.B. Preconditioning against myocardial dysfunction after ischemia and reperfusion by an alpha 1-adrenergic mechanism. Circ Res. 1993;73:656–670. doi: 10.1161/01.res.73.4.656. [DOI] [PubMed] [Google Scholar]
- 24.Yao Z., Gross G.J. Role of nitric oxide, muscarinic receptors, and the ATP-sensitive K+ channel in mediating the effects of acetylcholine to mimic preconditioning in dogs. Circ Res. 1993;73:1193–1201. doi: 10.1161/01.res.73.6.1193. [DOI] [PubMed] [Google Scholar]
- 25.Mocanu M.M., Bell R.M., Yellon D.M. PI3K and not p42/p44 appears to be implicated in the protection conferred by ischemic preconditioning. J Mol Cell Cardiol. 2002;34:661–668. doi: 10.1006/jmcc.2002.2006. [DOI] [PubMed] [Google Scholar]
- 26.Tyagi P., Tayal G. Ischemic preconditioning of myocardium. Acta Pharmacol Sin. 2002;23:865–870. [PubMed] [Google Scholar]
- 27.Jonassen A.K., Mjos O.D., Sack M.N. P70S6 kinase is a functional target of insulin activated Akt cell-survival signaling. Biochem Biophys Res Commun. 2004;315:160–165. doi: 10.1016/j.bbrc.2004.01.029. [DOI] [PubMed] [Google Scholar]
- 28.Kis A., Yellon D.M., Baxter G.F. Second window of protection following myocardial preconditioning: an essential role for PI3 kinase and p70S6 kinase. J Mol Cell Cardiol. 2003;35:1063–1071. doi: 10.1016/s0022-2828(03)00208-6. [DOI] [PubMed] [Google Scholar]
- 29.Tong H., Chen W., Steenbergen C., Murphy E. Ischemic preconditioning activates phosphatidylinositol-3-kinase upstream of protein kinase C. Circ Res. 2000;87:309–315. doi: 10.1161/01.res.87.4.309. [DOI] [PubMed] [Google Scholar]
- 30.Tong H., Imahashi K., Steenbergen C., Murphy E. Phosphorylation of glycogen synthase kinase-3β during preconditioning through a phosphatidylinositol-3-kinase–dependent pathway is cardioprotective. Circ Res. 2002;90:377–379. doi: 10.1161/01.res.0000012567.95445.55. [DOI] [PubMed] [Google Scholar]
- 31.Oldenburg O., Qin Q., Sharma A.R., Cohen M.V., Downey J.M., Benoit J.N. Acetylcholine leads to free radical production dependent on KATP channels, Gi proteins, phosphatidylinositol 3-kinase and tyrosine kinase. Cardiovasc Res. 2002;55:544–552. doi: 10.1016/s0008-6363(02)00332-2. [DOI] [PubMed] [Google Scholar]
- 32.Garlid K.D., Paucek P., Yarov-Yarovoy V., Murray H.N., Darbenzio R.B., D’Alonzo A.J. Cardioprotective effect of diazoxide and its interaction with mitochondrial ATP-sensitive KATP channels: possible mechanism of cardioprotection. Circ Res. 1997;81:1072–1082. doi: 10.1161/01.res.81.6.1072. [DOI] [PubMed] [Google Scholar]
- 33.Mitchell M.B., Meng X., Ao L., Brown J.M., Harken A.H., Banerjee A. Preconditioning of isolated rat heart is mediated by protein kinase C. Circ Res. 1995;76:73–81. doi: 10.1161/01.res.76.1.73. [DOI] [PubMed] [Google Scholar]
- 34.Tong H., Rockman H.A., Koch W.J., Steenbergen C., Murphy E. G protein coupled receptor internalization signaling is required for cardioprotection in ischaemic preconditioning. Circ Physiol. 2004;283:H61–H68. doi: 10.1161/01.RES.0000126048.32383.6B. [DOI] [PubMed] [Google Scholar]
- 35.Sato T., O’Rourke B., Marbán E. Modulation of mitochondrial ATP dependent K+ channels by protein kinase C. Circ Res. 1998;83:110–114. doi: 10.1161/01.res.83.1.110. [DOI] [PubMed] [Google Scholar]
- 36.Dreixler J.C., Shaikh A.R., Shenoy S.K., Steven Y.S. Protein kinase C subtypes and retinal ischemic preconditioning. Exp Eye Res. 2008;87:300–311. doi: 10.1016/j.exer.2008.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Downey J.M., Cohen M.V. Reducing infarct size in the setting of acute myocardial infarction. Prog Cardiovasc Dis. 2006;48:363–371. doi: 10.1016/j.pcad.2006.02.005. [DOI] [PubMed] [Google Scholar]
- 38.Penna C., Mancardi D., Rastaldo R., Pagliaro P. Cardioprotection: a radical view. Free radicals in pre and postconditioning. Biochim Biophys Acta. 2009;1787:781–793. doi: 10.1016/j.bbabio.2009.02.008. [DOI] [PubMed] [Google Scholar]
- 39.Baines C.P. Oxygen radicals released during ischaemic preconditioning contribute to cardioprotection in the rabbit myocardium. J Mol Cell Cardiol. 1997;29:207–216. doi: 10.1006/jmcc.1996.0265. [DOI] [PubMed] [Google Scholar]
- 40.Vanden Hoek T.L., Becker L.B., Shao Z., Li C., Schumacker P.T. Reactive oxygen species released from mitochondria during brief hypoxia induce preconditioning in cardiomyocytes. J Biol Chem. 1998;273:18092–18098. doi: 10.1074/jbc.273.29.18092. [DOI] [PubMed] [Google Scholar]
- 41.Baines C.P., Song C.X., Zheng Y.T., Wang G.W., Zhang J., Wang O.L. Protein kinase C interacts with and inhibits the permeability transition pore in cardiac mitochondria. Circ Res. 2003;92:873–880. doi: 10.1161/01.RES.0000069215.36389.8D. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zoratti M., De Marchi U., Gulbins E., Szabò I. Novel channels of the inner mitochondrial membrane. Biochim Biophys Acta. 2009;1787:351–363. doi: 10.1016/j.bbabio.2008.11.015. [DOI] [PubMed] [Google Scholar]
- 43.Kroemer G., Dallaporta B., Resche-Rigon M. The mitochondrial death/life regulator in apoptosis and necrosis. Annu Rev Physiol. 1998;60:619–642. doi: 10.1146/annurev.physiol.60.1.619. [DOI] [PubMed] [Google Scholar]
- 44.Hausenloy D.J., Tsang A., Mani-Babu S., Duchen M.R. Preconditioning protects by inhibiting the mitochondrial permeability transition. Am J Physiol Heart Circ Physiol. 2004;287:H841–H849. doi: 10.1152/ajpheart.00678.2003. [DOI] [PubMed] [Google Scholar]
- 45.Hausenloy D.J., Yellon D.M. Preconditioning and postconditioning: united at reperfusion. Pharmacol Ther. 2007;116:173–191. doi: 10.1016/j.pharmthera.2007.06.005. [DOI] [PubMed] [Google Scholar]
- 46.Juhaszova M., Zorov D.B., Kimet S.H., Pepe S., Fu Q., Fishbein K.W., Ziman B.D. Glycogen synthase kinase-3β mediates convergence of protection signalling to inhibit the mitochondrial permeability transition pore. J Clin Invest. 2004;113:1535–1549. doi: 10.1172/JCI19906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Miura T., Miki T. GSK-3β, a therapeutic target for cardiomyocyte protection. Circ J. 2009;73:1184–1192. doi: 10.1253/circj.cj-09-0284. [DOI] [PubMed] [Google Scholar]
- 48.Javador S.A., Clarke S., Das M., Griffiths E.J., Lim K.H.H., Halestrap A.P. Ischaemic preconditioning inhibits opening of mitochondrial permeability transition pores in the reperfused rat heart. J Physiol. 2003;549:513–524. doi: 10.1113/jphysiol.2003.034231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Tsang A., Hausenloy D.J., Mocanu M.M., Yellon D.M. Postconditioning: a form of “modified reperfusion” protects the myocardium by activating the phosphatidylinositol 3- kinase-Akt pathway. Circ Res. 2004;95:230–232. doi: 10.1161/01.RES.0000138303.76488.fe. [DOI] [PubMed] [Google Scholar]
- 50.Gomez L., Paillard M., Thibault H., Derumeaux G., Ovize M. Inhibition of GSK3β by postconditioning is required to prevent opening of the mitochondrial permeability transition pore during reperfusion. Circulation. 2008;117:2761–2768. doi: 10.1161/CIRCULATIONAHA.107.755066. [DOI] [PubMed] [Google Scholar]
- 51.Ferdinandy P., Szilvassy Z., Baxter G.F. Adaptation to myocardial stress in disease states: is preconditioning a healthy heart phenomenon? Trends Pharmacol Sci. 1998;19:223–229. doi: 10.1016/s0165-6147(98)01212-7. [DOI] [PubMed] [Google Scholar]
- 52.Ferdinandy P. Myocardial ischaemia/reperfusion injury and preconditioning: effects of hypercholesterolaemia/hyperlipidaemia. Br J Pharmacol. 2003;138:283–285. doi: 10.1038/sj.bjp.0705097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Mahgoub M.A., Abd-Elfattah S. Diabetes mellitus and cardiac function. Mol Cell Biochem. 1998;180:59–64. [PubMed] [Google Scholar]
- 54.Kersten J.R., Brooks L.A., Dellsperger K.C. Impaired microvascular response to graded coronary occlusion in diabetic and hyperglycaemic dogs. Am J Physiol Heart Circ Physiol. 1995;268:H1667–H1674. doi: 10.1152/ajpheart.1995.268.4.H1667. [DOI] [PubMed] [Google Scholar]
- 55.Giugliano D., Marfella R., Coppola L., Verrazzo G., Acampora R., Giunta R. Vascular effects of acute hyperglycemia in humans are reversed by L-arginine. Evidence for reduced availability of nitric oxide during hyperglycemia. Circulation. 1997;95:1783–1790. doi: 10.1161/01.cir.95.7.1783. [DOI] [PubMed] [Google Scholar]
- 56.Yang Z., Laubach V.E., French B.A., Kron I.L. Acute hyperglycemia enhances oxidative stress and exacerbates myocardial infarction by activating nicotinamide adenine dinucleotide phosphate oxidase during reperfusion. J Thorac Cardiovasc Surg. 2009;137:723–729. doi: 10.1016/j.jtcvs.2008.08.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Jaffe A.S., Spadaro J.J., Schechtman K., Roberts R., Geltman E.M., Sobel B.E. Increased congestive heart failure after myocardial infarction of modest extent in patients with diabetes mellitus. Am Heart J. 1984;108:31–37. doi: 10.1016/0002-8703(84)90541-6. [DOI] [PubMed] [Google Scholar]
- 58.Tani M., Neely J.R. Hearts from diabetic rats are more resistant to in vitro ischemia: possible role of altered Ca2+ metabolism. Circ Res. 1988;62:931–940. doi: 10.1161/01.res.62.5.931. [DOI] [PubMed] [Google Scholar]
- 59.Gamble J., Lopaschuk G.D. Glycolysis and glucose oxidation during reperfusion of ischemic hearts from diabetic rats. Biochem Biophys Acta. 1994;1225:191–199. doi: 10.1016/0925-4439(94)90078-7. [DOI] [PubMed] [Google Scholar]
- 60.Herlitz J., Wognsen G.B., Emanuelsson H., Haglid M., Karlson B.W., Karlsson T. Mortality and morbidity in diabetic and nondiabetic patients during a 2-year period after coronary artery bypass grafting. Diabetes Care. 1996;19:698–703. doi: 10.2337/diacare.19.7.698. [DOI] [PubMed] [Google Scholar]
- 61.Abel E.D. Insulin signalling in heart muscle: lessons from genetically engineered mouse models. Curr Hypertens Rep. 2004;6:416–423. doi: 10.1007/s11906-004-0034-4. [DOI] [PubMed] [Google Scholar]
- 62.Abel E.D. Myocardial insulin resistance and cardiac complications of diabetes. Curr Drug Targets Immune Endocr Metabol Disord. 2005;5:219–226. doi: 10.2174/1568008054064869. [DOI] [PubMed] [Google Scholar]
- 63.Fein S.F., Sonnenblick E.H. Diabetic cardiomyopathy. Cardiovascular stress in disease states: is preconditioning a healthy heart phenomenon? Drugs Ther. 1994;8:65–73. doi: 10.1007/BF00877091. [DOI] [PubMed] [Google Scholar]
- 64.Ravingerova T., Stetka R., Volkovova K., Pancza D., Dzurba A., Ziegelhoffer A. Acute diabetes modulates response to ischemia in isolated rat heart. Mol Cell Biochem. 2000;210:143–151. doi: 10.1023/a:1007129708262. [DOI] [PubMed] [Google Scholar]
- 65.Greden M., Podgorska M., Szutowicz A., Pawelcyzk T. Altered expression of adenosine receptors in heart of diabetic rat. J Physiol Pharmacol. 2005;56:587–597. [PubMed] [Google Scholar]
- 66.Kersten J.R., Montgomery M.W., Ghassemi T., Gross E.R., Toller W.G., Pagel P.S. Diabetes and hyperglycemia impair activation of mitochondrial KATP channel. Am J Physiol Heart Circ Physiol. 2001;280:H1744–H1750. doi: 10.1152/ajpheart.2001.280.4.H1744. [DOI] [PubMed] [Google Scholar]
- 67.Liu Y., Thornton J.D., Cohen M.V., Downey J.M., Schaffer S.W. Streptozotocin induced non-insulin-dependent diabetes protects the heart from infarction. Circulation. 1993;88:1273–1278. doi: 10.1161/01.cir.88.3.1273. [DOI] [PubMed] [Google Scholar]
- 68.Kusama Y., Hearse D.J., Avkiran M. Diabetes and susceptibility to reperfusion-induced ventricular arrhythmias. J Mol Cell Cardiol. 1992;24:411–421. doi: 10.1016/0022-2828(92)93195-p. [DOI] [PubMed] [Google Scholar]
- 69.Otani H. Ischemic preconditioning: from molecular mechanism to therapeutic opportunities. Antioxid Redox Signal. 2008;10:207–247. doi: 10.1089/ars.2007.1679. [DOI] [PubMed] [Google Scholar]
- 70.Wohaieb S.A., Godin D.V. Alterations in free radical tissue-defense mechanisms in streptozotocin-induced diabetes in rat. Effects of insulin treatment. Diabetes. 1987;36:1014–1018. doi: 10.2337/diab.36.9.1014. [DOI] [PubMed] [Google Scholar]
- 71.Matejikova J., Kucharska J., Pancza D., Ravingerova T. The effect of antioxidant treatment and nos inhibition on the incidence of ischemia-induced arrhythmias in the diabetic rat heart. Physiol Res. 2008;57:S55–S60. doi: 10.33549/physiolres.931552. [DOI] [PubMed] [Google Scholar]
- 72.Ganguly P.K., Pierce G.N., Dhalla K.S., Dhalla N.S. Defective sarcoplasmic reticular calcium transport in diabetic cardiomyopathy. Am J Physiol. 1983;244:E528–E535. doi: 10.1152/ajpendo.1983.244.6.E528. [DOI] [PubMed] [Google Scholar]
- 73.Allo S.N., Lincoln T.M., Wilson G.L., Green F.J., Watanabe A.M., Schaffer S.W. Non-insulin-dependent diabetes-induced defects in cardiac cellular calcium regulation. Am J Physiol. 1991;260:C1165–C1171. doi: 10.1152/ajpcell.1991.260.6.C1165. [DOI] [PubMed] [Google Scholar]
- 74.Atkins F.L., Dowell R.T., Love S. β-adrenergic receptors, adenylate cyclise activity and cardiac dysfunction in the diabetic rats. J Cardiovasc Pharmacol. 1985;7:66–70. doi: 10.1097/00005344-198501000-00011. [DOI] [PubMed] [Google Scholar]
- 75.Schaffer S. Cardiomyopathy associated with noninsulin-dependent diabetes. Mol Cell Biochem. 1991;107:1–20. doi: 10.1007/BF02424571. [DOI] [PubMed] [Google Scholar]
- 76.Moon C.H., Jung Y.S., Lee S.H., Baik E.J. Protein kinase C inhibitors abolish the increased resistance of the diabetic rat heart to ischemia-reperfusion injury. Jpn J Physiol. 1999;49:409–415. doi: 10.2170/jjphysiol.49.409. [DOI] [PubMed] [Google Scholar]
- 77.Lu R., Hu C.P., Peng J., Deng H.W., Li Y.J. Role of calcitonin gene-related peptide in ischemic preconditioning in diabetic rat hearts. Clin Exp Pharmacol Physiol. 2001;28:392–396. doi: 10.1046/j.1440-1681.2001.03467.x. [DOI] [PubMed] [Google Scholar]
- 78.Mori C., Ogawa K., Takatsuka H., Anzawa R. Cardioprotective effect of ischemic preconditioning on ischemia/reperfusion injury in spontaneously type 2 diabetic rat heart. Jikeikai Med J. 2006;53:69–79. [Google Scholar]
- 79.Ghosh S., Standen N.B., Galinanes M. Failure to precondition pathological human myocardium. J Am Coll Cardiol. 2001;37:711–718. doi: 10.1016/s0735-1097(00)01161-x. [DOI] [PubMed] [Google Scholar]
- 80.Paulson D.J. The diabetic heart is more sensitive to ischemic injury. Cardiovasc Res. 1997;34:104–112. doi: 10.1016/s0008-6363(97)00018-7. [DOI] [PubMed] [Google Scholar]
- 81.Tatsumi T., Matoba S., Kobara M., Keira N., Kawahara A., Tsuruyama K. Energy metabolism after ischemic preconditioning in streptozotocin-induced diabetic rat heart. JACC. 1998;31:707–715. doi: 10.1016/s0735-1097(97)00556-1. [DOI] [PubMed] [Google Scholar]
- 82.Ravingerová T., Stetka R., Pancza D., Ulicná O., Ziegelhöffer A., Styk J. Susceptibility to ischemia-induced arrhythmias and the effect of preconditioning in the diabetic rat heart. Physiol Res. 2000;49:607–616. [PubMed] [Google Scholar]
- 83.Charan K., Goyal A., Gupta J.K., Yadav H.N. Role of atrial natriuretic peptide in ischemic preconditioning induced cardioprotection in diabetic rat heart. J Surg Res. 2016;201:272–278. doi: 10.1016/j.jss.2015.10.045. [DOI] [PubMed] [Google Scholar]
- 84.Tosaki A., Engelman D.T., Engelman R.M., Das D.K. The evolution of diabetic response to ischemia/reperfusion and preconditioning in isolated working rat hearts. Cardiovasc Res. 1996;31:526–536. [PubMed] [Google Scholar]
- 85.Smith J.M., Wahler G.M. ATP-sensitive potassium channels are altered in ventricular myocytes from diabetic rats. Mol Cell Biochem. 1996;158:43–51. doi: 10.1007/BF00225881. [DOI] [PubMed] [Google Scholar]
- 86.Hassouna A., Loubani M., Matata B.M., Fowler A., Standen N.B., Galinanes M. Mitochondrial dysfunction as the cause of the failure to precondition the diabetic human myocardium. Cardiovasc Res. 2006;69:450–458. doi: 10.1016/j.cardiores.2005.11.004. [DOI] [PubMed] [Google Scholar]
- 87.Baines C.P., Goto M., Downey J.M. Oxygen radicals released during ischemic preconditioning contribute to cardioprotection in the rabbit myocardium. J Mol Cell Cardiol. 1997;29:207–216. doi: 10.1006/jmcc.1996.0265. [DOI] [PubMed] [Google Scholar]
- 88.Miura H., Breu M., Gutterman D.D. Diabetes mellitus impairs ATP-sensitive potassium channel function of human coronary arterioles. Circulation. 1997;96:1–17. doi: 10.1161/01.res.0000052671.53256.49. [DOI] [PubMed] [Google Scholar]
- 89.Magyar J., Rusznak Z., Szentesi P., Szucs G., Kovacs L. Action potential and potassium currents in rat ventricular muscle during experimental diabetes. J Mol Cell Cardiol. 1992;24:841–853. doi: 10.1016/0022-2828(92)91098-p. [DOI] [PubMed] [Google Scholar]
- 90.Ajmani P., Yadav H.N., Singh M., Sharma P.L. Possible involvement of caveolin in attenuation of cardioprotective effect of ischemic preconditioning in diabetic rat heart. BMC Cardiovasc Disord. 2011;11:43. doi: 10.1186/1471-2261-11-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Engler R.L., Yellon D.M. Sulfonylurea KATP blockade in type II diabetes and preconditioning in cardiovascular disease: time for reconsideration. Circulation. 1996;94:2297–2301. doi: 10.1161/01.cir.94.9.2297. [DOI] [PubMed] [Google Scholar]
- 92.Cleveland J.C., Jr, Meldrum D.R., Cain B.S., Banerjee A., Harken A.H. Oral sulfonylurea hypoglycemic agents prevent ischemic preconditioning in human myocardium: two paradoxes revisited. Circulation. 1997;96:29–32. doi: 10.1161/01.cir.96.1.29. [DOI] [PubMed] [Google Scholar]
- 93.Ashcroft S.J., Ashcroft F.M. The sulfonylurea receptor. Biochim Biophys Acta. 1992;1175:45–59. doi: 10.1016/0167-4889(92)90008-y. [DOI] [PubMed] [Google Scholar]
- 94.Terzic A., Jahangir A., Kurachi Y. Cardiac ATP-sensitive K channels: Regulation by intracellular nucleotides and K channel-opening drugs. Am J Physiol. 1995;269:C525–C545. doi: 10.1152/ajpcell.1995.269.3.C525. [DOI] [PubMed] [Google Scholar]
- 95.Tsang A., Hausenloy D.J., Mocanu M.M., Carr R.D., Yellon D.M. Preconditioning the diabetic heart: the importance of Akt phosphorylation. Diabetes. 2005;54:2360–2364. doi: 10.2337/diabetes.54.8.2360. [DOI] [PubMed] [Google Scholar]
- 96.Chen H., Wu X.J., Lu X.Y., Zhu L., Wang L.P., Yang H.T. Phosphorylated heat shock protein 27 is involved in enhanced heart tolerance to ischemia in short-term type1 diabetic rats. Acta Pharmacol Sin. 2005;26:806–812. doi: 10.1111/j.1745-7254.2005.00113.x. [DOI] [PubMed] [Google Scholar]
- 97.Ting W.S., Hua X.M., Ting C.W., Hou G.F., Ying G.Z. Study on tolerance to ischemia-reperfusion injury and protection of ischemic preconditioning of type diabetes rat heart. Biomed Aging Pathol. 2011;1:56–60. [Google Scholar]
- 98.Ghaboura N., Tamareille S., Ducluzeau P.H., Grimaud L., Loufrani L., Croué A. Diabetes mellitus abrogates erythropoietin-induced cardioprotection against ischemic-reperfusion injury by alteration of the RISK/GSK-3β signalling. Basic Res Cardiol. 2011;106:147–162. doi: 10.1007/s00395-010-0130-3. [DOI] [PubMed] [Google Scholar]
- 99.Juhaszova M., Zorov D.B., Kimet S.H. Glycogen synthase kinase-3β mediates convergence of protection signalling to inhibit the mitochondrial permeability transition pore. J Clin Invest. 2004;113:1535–1549. doi: 10.1172/JCI19906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Wang Y., Feng W., Xue W., Tan Y., Hein D.W., Li X.K. Inactivation of GSK-3β by metallothionein prevents diabetes-related changes in cardiac energy metabolism, inflammation, nitrosative damage, and remodeling. Diabetes. 2009;58:1391–1402. doi: 10.2337/db08-1697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Yadav H.N., Singh M., Sharma P.L. Involvement of GSK-3β in attenuation of the cardioprotective effect of ischemic preconditioning in diabetic rat heart. Mol Cell Biochem. 2010;343:75–81. doi: 10.1007/s11010-010-0500-z. [DOI] [PubMed] [Google Scholar]
- 102.Goldstein J.L., Hazzard W.R., Schrott H.G., Bierman E.L., Motulsky A.G. Hyperlipidemia in coronary heart disease. I. Lipid levels in 500 survivors of myocardial infarction. J Clin Invest. 1973;52:1533–1543. doi: 10.1172/JCI107331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Tilton R.G., Cole P.A., Zions J.D., Daugherty A., Larson K.B., Sutera S.P. Increased ischemia–reperfusion injury to the heart associated with short-term, diet-induced hypercholesterolemia in rabbits. Circ Res. 1987;60:551–559. doi: 10.1161/01.res.60.4.551. [DOI] [PubMed] [Google Scholar]
- 104.Golino P., Maroko P.R., Carew T.E. The effect of acute hypercholesterolaemia on myocardial infarct size and the no-reflow phenomenon during coronary occlusion–reperfusion. Circulation. 1987;75:292–298. doi: 10.1161/01.cir.75.1.292. [DOI] [PubMed] [Google Scholar]
- 105.Girod W.G., Jones S.P., Sieber N., Aw T.Y., Lefer D.J. Effects of hypercholesterolemia on myocardial ischemia-reperfusion injury in LDL receptor-deficient mice. Arterioscler Thromb Vasc Biol. 1999;19:2776–2781. doi: 10.1161/01.atv.19.11.2776. [DOI] [PubMed] [Google Scholar]
- 106.Le G.B., Vié B., Fauré P., Degryse A.D., Mouillard P., John G.W. Increased resistance to ischaemic injury in the isolated perfused atherosclerotic heart of the cholesterol-fed rabbit. Cardiovasc Res. 1995;30:689–696. doi: 10.1016/0008-6363(95)00076-3. [DOI] [PubMed] [Google Scholar]
- 107.Kyriakides Z.S., Psychar S. Hyperlipidemia prevents the expected reduction of myocardial ischemia on repeated balloon inflations during angioplasty. Chest. 2002;121:1211–1215. doi: 10.1378/chest.121.4.1211. [DOI] [PubMed] [Google Scholar]
- 108.Szilvassy Z., Ferdinandy P., Szilvassy J., Nagy I., Karcsu S., Lonovics J. The loss of pacing-induced preconditioning in atherosclerotic rabbits: role of hypercholesterolemia. J Mol Cell Cardiol. 1995;27:2559–2569. doi: 10.1006/jmcc.1995.0043. [DOI] [PubMed] [Google Scholar]
- 109.Ferdinandy P., Szilvassy Z., Horvath L.I., Csont T., Csonka C., Nagy E. Loss of pacing-induced preconditioning in rat hearts: role of nitric oxide and cholesterol-enriched diet. J Mol Cell Cardiol. 1997;29:3321–3333. doi: 10.1006/jmcc.1997.0557. [DOI] [PubMed] [Google Scholar]
- 110.Ungi I., Ungi T., Ruzsa Z., Nagy E., Zimmermann Z., Csont T. Hypercholesterolemia attenuates the anti-ischemic effect of preconditioning during coronary angioplasty. Chest. 2005;128:1623–1628. doi: 10.1378/chest.128.3.1623. [DOI] [PubMed] [Google Scholar]
- 111.Szekeres L., Szilvássy Z., Ferdinandy P., Nagy I., Karcsu S., Csáti S. Delayed cardiac protection against harmful consequences of stress can be induced in experimental atherosclerosis in rabbits. J Mol Cell Cardiol. 1997;29:1977–1983. doi: 10.1006/jmcc.1997.0418. [DOI] [PubMed] [Google Scholar]
- 112.Tang X.L., Takano H., Xuan Y.T., Sato H., Kodani E., Dawn B. Hypercholesterolemia abrogates late preconditioning via a tetrahydrobiopterin-dependent mechanism in conscious rabbits. Circulation. 2005;112:2149–2156. doi: 10.1161/CIRCULATIONAHA.105.566190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Csont T., Bereczki E., Bencsik P., Fodor G., Görbe A., Zvara A. Hypercholesterolemia increases myocardial oxidative and nitrosative stress thereby leading to cardiac dysfunction in apoB-100 transgenic mice. Cardiovasc Res. 2007;76:100–109. doi: 10.1016/j.cardiores.2007.06.006. [DOI] [PubMed] [Google Scholar]
- 114.Lefer A.M., Ma X.L. Decreased basal nitric oxide release in hypercholesterolemia increases neutrophil adherence to rabbit coronary artery endothelium. Arterioscler Thromb. 1993;13:771–776. doi: 10.1161/01.atv.13.6.771. [DOI] [PubMed] [Google Scholar]
- 115.Deliconstantinos G., Villiotou V., Stavrides J.C. Modulation of particulate nitric oxide synthase activity and peroxynitrite synthesis in cholesterol enriched endothelial cell membranes. Biochem Pharmacol. 1995;49:1589–1600. doi: 10.1016/0006-2952(95)00094-g. [DOI] [PubMed] [Google Scholar]
- 116.White C.R., Brock T.A., Chang L.Y., Crapo J., Briscoe P., Ku D. Superoxide and peroxynitrite in atherosclerosis. Proc Natl Acad Sci USA. 1994;91:1044–1048. doi: 10.1073/pnas.91.3.1044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Szilvássy Z., Csont T., Páli T., Droy-Lefaix M.T., Ferdinandy P. Nitric oxide, peroxynitrite and cGMP in atherosclerosis-induced hypertension in rabbits: beneficial effects of cicletanine. J Vasc Res. 2001;38:39–46. doi: 10.1159/000051028. [DOI] [PubMed] [Google Scholar]
- 118.Onody A., Csonka C., Giricz Z., Ferdinandy P. Hyperlipidemia induced by a cholesterol-rich diet leads to enhanced peroxynitrite formation in rat hearts. Cardiovasc Res. 2003;58:663–670. doi: 10.1016/s0008-6363(03)00330-4. [DOI] [PubMed] [Google Scholar]
- 119.Okamoto T., Akaike T., Sawa T., Miyamoto Y., Van der Vleit A., Maeda H. Activation of matrix metalloproteinases by peroxynitrite-induced protein S glutathiolation via disulfide S-oxide formation. J Biol Chem. 2001;276:29596–29602. doi: 10.1074/jbc.M102417200. [DOI] [PubMed] [Google Scholar]
- 120.Wang W., Sawicki G., Schulz R. Peroxynitrite-induced myocardial injury is mediated through matrix metalloproteinase-2. Cardiovasc Res. 2002;53:165–174. doi: 10.1016/s0008-6363(01)00445-x. [DOI] [PubMed] [Google Scholar]
- 121.Giricz Z., Lalu M.M., Csonka C., Bencsik P., Schulz R., Ferdinandy P. Hyperlipidemia attenuates the infarct size-limiting effect of ischemic preconditioning: role of matrix metalloproteinase-2 inhibition. J Pharmacol Exp Ther. 2006;316:154–161. doi: 10.1124/jpet.105.091140. [DOI] [PubMed] [Google Scholar]
- 122.Hao L., Du M., Lopez-Campistrous A., Fernandez-Patron C. Agonist-induced activation of matrix metalloproteinase-7 promotes vasoconstriction through the epidermal growth factor-receptor pathway. Circ Res. 2004;94:68–76. doi: 10.1161/01.RES.0000109413.57726.91. [DOI] [PubMed] [Google Scholar]
- 123.Cheung P.Y., Sawicki G., Wozniak M., Wang W., Radomski M.W., Schulz R. Matrix metalloproteinase-2 contributes to ischemia-reperfusion injury in the heart. Circulation. 2000;101:1833–1839. doi: 10.1161/01.cir.101.15.1833. [DOI] [PubMed] [Google Scholar]
- 124.Lalu M.M., Pasini E., Schulze C.J., Ferrari-Vivaldi M., Ferrari-Vivaldi G., Bachetti T. Ischaemia–reperfusion injury activates matrix metalloproteinases in the human heart. Eur Heart J. 2005;26:27–35. doi: 10.1093/eurheartj/ehi007. [DOI] [PubMed] [Google Scholar]
- 125.Görbe A., Varga Z.V., Kupai K., Bencsik P., Kocsis G.F., Csont T. Cholesterol diet leads to attenuation of ischemic preconditioning-induced cardiac protection: the role of connexin 43. Am J Physiol Heart Circ Physiol. 2011;300:H1907–H1913. doi: 10.1152/ajpheart.01242.2010. [DOI] [PubMed] [Google Scholar]
- 126.Genda S., Miura T., Miki T., Ichikawa Y., Shimamoto K. KATP channel opening is an endogenous mechanism of protection against the no-reflow phenomenon but its function is compromised by hypercholesterolemia. J Am Coll Cardiol. 2002;40:1339–1346. doi: 10.1016/s0735-1097(02)02156-3. [DOI] [PubMed] [Google Scholar]
- 127.Laufs U., La Fata V., Plutzky J., Lioa J.K. Upregulation of endothelial nitric oxide synthase by HMG CoA reductase inhibitors. Circulation. 1998;97:1129–1135. doi: 10.1161/01.cir.97.12.1129. [DOI] [PubMed] [Google Scholar]
- 128.Kureishi Y., Luo Z., Shiojima I., Bialik A., Fulton D., Lefer D.J. The HMG-CoA reductase inhibitor simvastatin activates the protein kinase Akt and promotes angiogenesis in normocholesterolemic animals. Nat Med. 2000;6:1004–1010. doi: 10.1038/79510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Ledoux S., Laouari D., Essig M., Runembert I., Trugnan G., Michel J.B. Lovastatin enhances ecto-5′-nucleotidase activity and cell surface expression in endothelial cells: implication of rho-family GTPases. Circ Res. 2002;90:420–427. doi: 10.1161/hh0402.105668. [DOI] [PubMed] [Google Scholar]
- 130.Barrett-Connor E. Sex differences in coronary heart disease: why are women so superior? The 1995 Ancel Keys Lecture. Circulation. 1997;95:252–264. doi: 10.1161/01.cir.95.1.252. [DOI] [PubMed] [Google Scholar]
- 131.Sullivan J.M., Vander Zwaag R., Lemp G.F. Postmenopausal estrogen use and coronary atherosclerosis. Ann Intern Med. 1998;108:358–363. doi: 10.7326/0003-4819-108-3-358. [DOI] [PubMed] [Google Scholar]
- 132.Grodstein F., Stampfer M. The epidemiology of coronary heart disease and estrogen replacement in postmenopausal women. Prog Cardiovasc Dis. 1995;38:199–210. doi: 10.1016/s0033-0620(95)80012-3. [DOI] [PubMed] [Google Scholar]
- 133.Delyani J.A., Murohara T., Nossuli T.O., Lefer A.M. Protection from a myocardial reperfusion injury by acute administration of 17β-estradiol. J Mol Cell Cardiol. 1996;28:1001–1008. doi: 10.1006/jmcc.1996.0093. [DOI] [PubMed] [Google Scholar]
- 134.Beer S., Reincke M., Kral M., Lie S.Z., Steinhauer S., Schmidt H.H. Susceptibility to cardiac ischemia/reperfusion injury is modulated by chronic estrogen status. J Cardiovasc Pharmacol. 2002;40:420–428. doi: 10.1097/00005344-200209000-00011. [DOI] [PubMed] [Google Scholar]
- 135.Barrett-Connor E., Stuenkel C. Hormones and heart disease in women: heart and estrogen/progestin replacement study in perspective. J Clin Endocrinol Metab. 1999;84:1848–1853. doi: 10.1210/jcem.84.6.5667. [DOI] [PubMed] [Google Scholar]
- 136.Rossouw J.E., Anderson G.L., Prentice R.L., LaCroix A.Z., Kooperberg C., Stefanick M.L. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results from the Women’s Health Initiative randomized controlled trial. JAMA. 2002;288:321–333. doi: 10.1001/jama.288.3.321. [DOI] [PubMed] [Google Scholar]
- 137.Ranki H.J., Budas G.R., Crawford R.M. Gender-specific difference in cardiac ATP-sensitive K+ channels. J Am Coll Cardiol. 2001;38:906–915. doi: 10.1016/s0735-1097(01)01428-0. [DOI] [PubMed] [Google Scholar]
- 138.Bae S., Zhang L. Gender differences in cardioprotection against ischemia/reperfusion injury in adult rat hearts and protein kinase C signalling. J Pharmacol Exp Ther. 2005;315:1125–1135. doi: 10.1124/jpet.105.090803. [DOI] [PubMed] [Google Scholar]
- 139.Kapadia S., Lee J., Torre-Amione G., Birdsall H.H., Ma T.S., Mann D.L. Tumor necrosis factor-alpha gene and protein expression in adult feline myocardium after endotoxin administration. J Clin Invest. 1995;96:1042–1052. doi: 10.1172/JCI118090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Hirschl M.M., Gwechenberger M., Binder T., Binder M., Graf S., Stefenelli T. Assessment of myocardial injury by serum tumour necrosis factor alpha measurements in acute myocardial infarction. Eur Heart J. 1996;17:1852–1859. doi: 10.1093/oxfordjournals.eurheartj.a014803. [DOI] [PubMed] [Google Scholar]
- 141.Liao S.L., Chen W.Y., Chen C.J. Estrogen attenuates tumor necrosis factor-alpha expression to provide ischemic neuroprotection in female rats. Neurosci Lett. 2002;330:159–162. doi: 10.1016/s0304-3940(02)00754-1. [DOI] [PubMed] [Google Scholar]
- 142.Machikas A.M., Hunter J.C., Lopez V., Korzick D.H. Increased mitochondrial permeability transition pore opening dominates ischemia–reperfusion injury in the aged female rat heart. Circ Res. 2012;111:A342. [Google Scholar]
- 143.Shinmura K., Nagai M., Tamaki K., Roberto B. Loss of ischaemic preconditioning in ovariectomized rat hearts: Possible involvement of impaired protein kinase C€ phosphorylation. Cardiovasc Res. 2008;79:387–394. doi: 10.1093/cvr/cvn086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Goyal A., Semwal B.C., Yadav H.N. Abrogate cardioprotective effect of ischemic preconditioning in ovariectomized rat heart. Hum Exp Toxicol. 2015;35:644–653. doi: 10.1177/0960327115597980. [DOI] [PubMed] [Google Scholar]
- 145.Wang X., Abdel-Rahman A.A. Estrogen modulation of eNOS activity and its association with caveolin-3 and calmodulin in rat hearts. Am J Physiol Heart Circ Physiol. 2002;282:H2309–H2315. doi: 10.1152/ajpheart.00772.2001. [DOI] [PubMed] [Google Scholar]
- 146.Stampfer M.J., Colditz G.A., Willett W.C., Manson J.E., Rosner B., Speizer F.E. Postmenopausal estrogen therapy and cardiovascular disease: ten-year follow-up from the nurses’ health study. N Engl J Med. 1991;325:756–762. doi: 10.1056/NEJM199109123251102. [DOI] [PubMed] [Google Scholar]
- 147.Grady D., Rubin S.M., Petitti D.B., Fox C.S., Black D., Ettinger B. Hormone therapy to prevent disease and prolong life in a postmenopausal women. Ann Intern Med. 1992;117:1016–1037. doi: 10.7326/0003-4819-117-12-1016. [DOI] [PubMed] [Google Scholar]
- 148.Best P.J., Berger P.B., Miller V.M., Lerman A. The effect of estrogen a replacement therapy on plasma nitric oxide and endothelin-1 levels in postmenopausal women. Ann Intern Med. 1998;128:285–288. doi: 10.7326/0003-4819-128-4-199802150-00006. [DOI] [PubMed] [Google Scholar]
- 149.Levin R.E. Integration of the extranuclear and nuclear actions of estrogen. Mol Endocrinol. 2005;19:1951–1959. doi: 10.1210/me.2004-0390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Hishikawa K., Nakaki T., Marumo T., Suzuki H., Kato R., Saruta T. Up regulation of nitric oxide synthase by estradiol in human aortic endothelial cells. FEBS Lett. 1995;360:291–293. doi: 10.1016/0014-5793(95)00124-r. [DOI] [PubMed] [Google Scholar]
- 151.Michel J.B., Feron O., Sacks D., Michel T. Reciprocol regulation of endothelial nitric oxide synthatase by Ca2+ calmodulin and caveolin. J Biol Chem. 1997;272:15583–15586. doi: 10.1074/jbc.272.25.15583. [DOI] [PubMed] [Google Scholar]
- 152.Gavin K.M., Seals D.R., Silver A.E., Moreau K.L. Vascular endothelial estrogen receptor α is modulated by estrogen status and related to endothelial function and endothelial nitric oxide synthase in healthy women. J Clin Endocrinol Metab. 2009;94:3513–3520. doi: 10.1210/jc.2009-0278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Chen Z., Yuhanna I.S., Galcheva-Gargova Z., Karas R.H., Mendelsohn M.E., Shaul P.W. Estrogen receptor mediates the nongenomic activation of endothelial nitric oxide synthase by estrogen. J Clin Invest. 1999;103:401–406. doi: 10.1172/JCI5347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Simoncini T., Hafezi-Moghadam A., Brazil D. Interaction of oestrogen receptor with the regulatory subunit of phosphatidylinositol-3-OH kinase. Nature. 2000;407:538–541. doi: 10.1038/35035131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Hisamoto K., Ohmichi M., Kurachi H. Estrogen induces the Akt dependent activation of endothelial nitric-oxide synthase in vascular endothelial cells. J Biol Chem. 2001;276:3459–3467. doi: 10.1074/jbc.M005036200. [DOI] [PubMed] [Google Scholar]
- 156.Haynes M.P., Sinha D., Russell K.S. Membrane estrogen receptor engagement activates endothelial nitric oxide synthase via the PI3-kinase-Akt pathway in human endothelial cells. Circ Res. 2000;87:677–682. doi: 10.1161/01.res.87.8.677. [DOI] [PubMed] [Google Scholar]
- 157.Camper-Kirby D., Welch S., Walker A., Shiraishi I., Setchell K.D., Schaefer E. Myocardial Akt activation and gender: increased nuclear activity in females versus males. Circ Res. 2001;88:1020–1027. doi: 10.1161/hh1001.090858. [DOI] [PubMed] [Google Scholar]
- 158.Fulton D., Gratton J.P., McCabe T.J., Fontana J., Fujio Y., Walsh K. Regulation of endothelium-derived nitric oxide production by the protein kinase Akt. Nature. 1999;399:597–601. doi: 10.1038/21218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Dimmeler S., Fleming I., Fisslthaler B., Hermann C., Busse R., Zeiher A.M. Activation of nitric oxide synthase in endothelial cells by Akt-dependent phosphorylation. Nature. 1999;399:601–605. doi: 10.1038/21224. [DOI] [PubMed] [Google Scholar]
- 160.McCabe T.J., Fulton D., Roman L.J., Sessa W.C. Enhanced electron flux and reduced calmodulin dissociation may explain “calcium-independent” eNOS activation by phosphorylation. J Biol Chem. 2000;275:6123–6128. doi: 10.1074/jbc.275.9.6123. [DOI] [PubMed] [Google Scholar]
- 161.Hale S.L., Birnbaum Y., Kloner R.A. Beta-estradiol, but not alpha-estradiol, reduced myocardial necrosis in rabbits after ischemia and reperfusion. Am Heart J. 1996;132:258–262. doi: 10.1016/s0002-8703(96)90419-6. [DOI] [PubMed] [Google Scholar]
- 162.Kolodgie F.D., Farb A., Litovsky S.H., Narula J., Jeffers L.A., Lee S.J. Myocardial protection of contractile function after global ischemia by physiologic estrogen replacement in the ovariectomized rat. J Mol Cell Cardiol. 1997;29:2403–2414. doi: 10.1006/jmcc.1997.0476. [DOI] [PubMed] [Google Scholar]
- 163.Fraser H., Davidge S.T., Clanachan A.S. Enhancement of post-ischemic myocardial function by chronic 17β-estradiol treatment: role of alterations in glucose metabolism. J Mol Cell Cardiol. 1999;31:1539–1549. doi: 10.1006/jmcc.1999.0986. [DOI] [PubMed] [Google Scholar]
- 164.Xu Y., Arenas I.A., Armstrong S.J., Plahta W.C., Xu H., Davidge T. Estrogen improves cardiac recovery after ischemia/reperfusion by decreasing tumor necrosis factor-α. Cardiovasc Res. 2006;69:836–844. doi: 10.1016/j.cardiores.2005.11.031. [DOI] [PubMed] [Google Scholar]
- 165.Montalcini T., Gorgone G., Gazzaruso C., Sesti G., Perticone F., Pujia A. Endogenous testosterone and endothelial function in postmenopausal women. Coron Artery Dis. 2007;1:9–13. doi: 10.1097/01.mca.0000236290.79306.d1. [DOI] [PubMed] [Google Scholar]
- 166.Liu A., Gao L., Kang S., Liu Y., Xu C., Sun H. Testosterone enhances estradiols cardioprotection in ovariectomized rats. J Endocrinal. 2011;11:61–69. doi: 10.1530/JOE-11-0181. [DOI] [PubMed] [Google Scholar]