Highlights
-
•
Synovial chrondroma is a rare condition of which the aetiology remains unclear. Large palpable lesions represent an atypical presentation.
-
•
The diagnosis is often not immediately apparent. However it is usually suggested by radiologic investigation and confirmed on histology.
-
•
Disease recurrence is not infrequent after excision (15–23%) and patients should be counselled regarding this.
-
•
Malignant transformation whilst uncommon has been described. At present no definite criteria exist in order to make the diagnosis of malignancy.
-
•
Due to the above risks of recurrence and malignancy, long term follow up of affected patients is advised.
Keywords: Orthopaedics, Chrondromatosis, Knee, Case report
Abstract
Introduction
Synovial chrondomatosis is a rare disorder characterised by the development of hyaline cartilage from the synovial membrane. Large isolated lesions in the Hoffa's fat pad are an uncommon entity.
Presentation of case
A 33 year old gentleman presented complaining of progressive knee pain associated with an enlarging lesion on the anterior aspect of the right knee, with associated locking and giving way. Examination revealed a firm 4 × 5 cm lesion adjacent to the patellar tendon.
Subsequent CT and MRI demonstrated a lesion in the inferior aspect of Hoffa’s fat pad, with a second lesion adjacent to the proximal tibiofibular joint, in addition to advanced degenerative changes and a meniscal tear.
He proceeded to excisional biopsy. Histological analysis was consistent with a solitary synovial osteochondroma. There were no atypical features suggestive of malignancy.
Discussion
Synovial chondromatosis is a rare disorder affecting the synovial joints. The underlying pathophysiology is thought to be metaplastic change of the synovium to hyaline cartilaginous tissue. Transformation to malignancy has been described but is uncommon with an estimated risk of 5%. It is 1.5–2 times as prevalent in males versus females. Symptoms which patients may complain of include pain;locking and giving way; and palpable masses.
The management usually entails removal of the mass lesion with or without accompanying synovectomy. Recurrence of disease may occur in up to 15–23% of patients.
Conclusion
Synovial chrondromatosis is a rare but well recognised condition. Long term follow up is advised in view of the risk of recurrence and malignant transformation.
1. Introduction
Synovial chrondomatosis is a rare disorder characterised by the development of hyaline cartilage from the synovial membrane. It typically presents as a monoarthropathy, with the knee being the most frequently involved joint. It is thought to arise from a metaplastic process of the synovium. This cartilage may form loose bodies in the joint and cause patients to become symptomatic. Malignant transformation to chondrosarcoma has been described but is uncommon. Large isolated lesions in the Hoffa’s fat pad are a rare entity.
2. Presentation of case
A 33 year old male presented to our service with a 6 month history of worsening knee pain associated with a progressively enlarging mass on the anterior aspect of the right knee. He denied systemic symptoms of anorexia, unintentional weight loss or night sweats. No other joints were affected. He had no past medical history of note.
His background was significant for chronic right knee pain ongoing for the past 10 years, with associated symptoms of locking and giving way. He had undergone 2 previous arthroscopies at 10 and 2 years previously. The most recent arthoscopy demonstrated advanced degeneration of the articular cartilage, with no other abnormalities noted.
Examination of the joint revealed a 4 × 5 cm firm mass lesion on the anterolateral aspect of the right knee adjacent to the patellar tendon. The patient had full range of motion of the knee although deep flexion aggravated the pain. Examination was otherwise unremarkable. His inflammatory markers were normal.
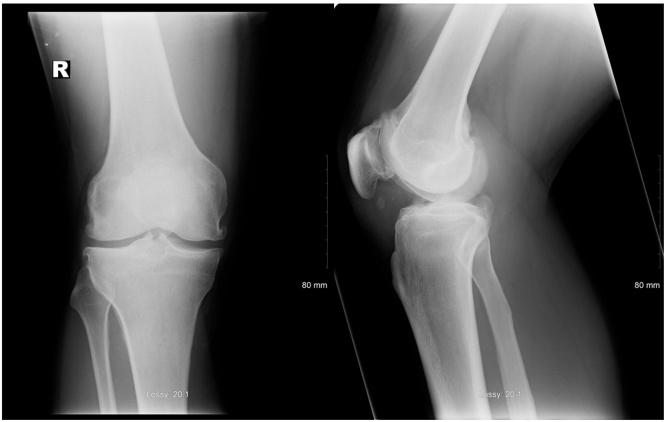
Plain films and CT imaging of the right knee demonstrated advanced degenerative changes with intraarticular loose bodies (Fig. 1). It showed a large non homogenous lesion adjacent to the patellar tendon and second one near the proximal tibiofibular joint.
Fig. 1.
Plain films of knee prior to excision of lesion (AP and lateral, right knee).
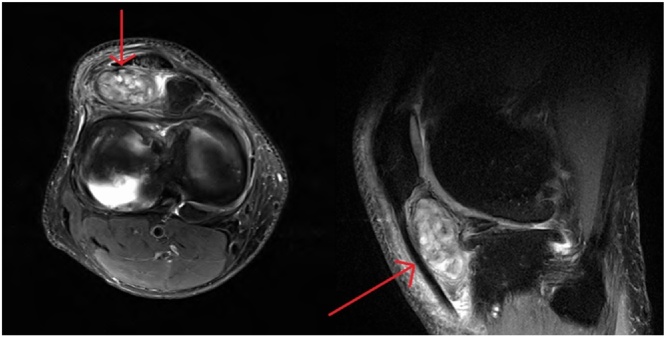
Subsequent MRI of the knee showed a well circumscribed 4.2 × 2.6 cm lesion in the inferior aspect of Hoffa’s fat pad, with a second similar lesion adjacent to the proximal tibiofibular joint. It filled the fat pad almost completely with subsequent tenting of the patellar tendon (Fig. 2). A lateral meniscal tear and advanced degenerative disease was also noted.
Fig. 2.
MRI of knee prior to excision of lesion (coronal and sagittal sections, right knee).
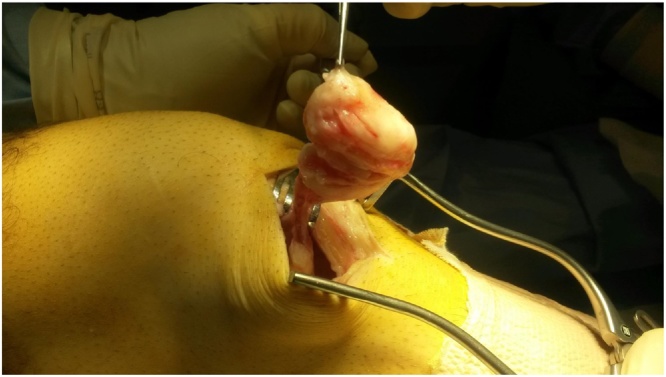
We proceeded to an excision biopsy of the larger lesion under general anaesthetic as a day case, performed by the consultant surgeon. The lesion was completely excised. His postoperative course was uncomplicated and he made a rapid recovery (Fig. 3).
Fig. 3.
Macroscopic appearance of lesion on excision.
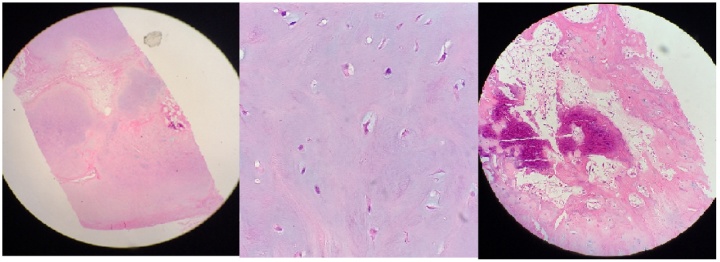
Histologic analysis revealed lobulated, predominantly cartilaginous tissue, with foci of ossification and vascular proliferation consistent with a solitary synovial osteochondroma. There were no atypical features suggestive of malignancy.
At 2 weeks, his wound was healed. At his six week review his knee was pain free and no further episodes of locking or instability were reported (Fig. 4).
Fig. 4.
Microscopic appearance on histopathological analysis.
3. Discussion
Synovial chondromatosis is a rare disorder affecting the synovial joints. The underlying pathophysiology is thought to be metaplastic change of the synovium to foci of hyaline cartilaginous tissue. Transformation to malignancy has been described but is thought to be uncommon with an estimated risk of 5% [1], [2], [3]. Three phases of disease were described in a case series by Milgram in 1977; an early phase, characterised by active intrasynovial disease with no loose bodies; a transitional phase with active disease and loose bodies; and a late phase without intrasynovial disease but with multiple loose bodies [4]. Large isolated chondroma as seen in our case is a rare ocurrence [13].
It is approximately 1.5–2 times as prevalent in males comparative to females and usually presents in the 3rd to 6th decade of life [1]. It typically presents as a monoarthopathy, with the knee joint most commonly involved (43–68% of cases). Subsequent sites of involvement in order of decreasing frequency are the hip, shoulder, elbow, ankle and wrist joints [3], [4]. Of those patients who have knee involvement, 10% have bilateral disease [2]. Symptoms which patients may complain of include pain and swelling in the affected joint; clicking, locking and giving way; and palpable masses. Mass lesions may also be detected on examination, in addition to crepitus of the joint.
Although some lesions may undergo calcification and become radioopaque, plain radiographs are frequently normal [5]. CT or MRI allows better characterisation of lesions and can often be diagnostic. Non- calcified and calcified lesions may be differentiated on MRI, in which non-mineralised chondromata are isointense on T1 but hyperintense on T2 weighted sequences; whereas mineralised lesions are hypointense on all sequences [6]. The differential diagnosis includes Hoffa’s disease, para-articular osteochondroma and primary chondrosarcoma.
On histologic examination, hypercellular lobules of hyaline cartilage arising from synovium are found. Nuclear atypia is common. Benign synovial chondromata can be difficult to differentiate histologically from low grade chondrosarcoma; some features more suggestive of malignancy include myxoid changes, cartilaginous cells in sheets rather than clusters and the presence of necrosis [1], [2], [3]. However, no definitive criteria for the diagnosis of malignancy exist. In our case no definite malignant features were detected.
Management of synovial chondroma usually entails open or arthoscopic removal of mass lesion and intraarticular loose bodies if present, with or without accompanying synovectomy [7], [8], [9], [10]. Recurrence of disease may occur in up to 15–23% of patients, and usually occurs within the first 18 months after resection [3], [11]. As with skeletal chondrosarcomas, synovial chondrosarcomas arising in benign chondromata mandate excision with wide margins, occasionally necessitating amputation [1]. Long term follow up is recommended in view of the high frequency of recurrence and risk of malignant transformation [12].
4. Conclusion
-
•
Synovial chrondromatosis is a rare but well recognised condition of which the exact aetiology remains unclear. Large isolated palpable lesions are an atypical presentation of the disease.
-
•
Due to the rarity of the condition, particularly in combination with an atypical presentation, the diagnosis is often not immediately apparent. However it is usually suggested by radiologic investigation, particularly MRI, and subsequently confirmed on histologic analysis.
-
•
Disease recurrence is not infrequent after excision (15–23%) and patients should be counselled regarding this.
-
•
Malignant transformation whilst uncommon has been described, with the risk standing at approximately 5%. At present no definite criteria exist in order to make the diagnosis of malignancy.
-
•
Due to the above risks of recurrence and malignancy, long term follow up of affected patients is advised.
Consent and conflict of interest
The authors declare that no actual or potential conflict of interest exists.
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
This work has been reported in line with the SCARE guidelines for surgical case reports [14].
Funding
No sources of funding provided.
Ethical approval
Not applicable.
Author contribution
O’Connell L, Memon A, Kenny P. – Data collection and writing of paper.
Foran P – Review of radiological images.
Leen E – Review of histopathology.
Guarantor
Lauren O’Connell, Adeel Memon.
References
- 1.Campanacci M. 2nd ed. Springer; New York: 1999. Bone and Soft Tissue Tumours. [Google Scholar]
- 2.Kransdorf M., Meis J. Extraskeletal osseous and cartilaginous tumours of the extremities. Radiographics. 1993;13(4):853–884. doi: 10.1148/radiographics.13.4.8356273. [DOI] [PubMed] [Google Scholar]
- 3.Davis R.I., Hamilton A., Biggart J.D. Primary synovial chondromatosis: a clinicopathological review and assessment of malignant potential. Hum. Pathol. 1998;29(7):683–688. doi: 10.1016/s0046-8177(98)90276-3. [DOI] [PubMed] [Google Scholar]
- 4.Milgram J.W. Synovial osteochondromatosis. J. Bone Joint Surg. 1977;59A:792. [PubMed] [Google Scholar]
- 5.Christensen J.H., Poulsen J.O. Synovial chondromatosis. Acta Orthop. Scand. 1975;46:919. doi: 10.3109/17453677508989279. [DOI] [PubMed] [Google Scholar]
- 6.Sheldon P., Forreste D., Learch T. Imaging of intraarticular masses. Radiographics. 2005;25(1):105–119. doi: 10.1148/rg.251045050. [DOI] [PubMed] [Google Scholar]
- 7.Coolican M.R., Dandy D.J. Arthoscopic management of synovial chondromatosis of the knee. Findings and results in 18 cases. J. Bone Joint Surg. 1989;71B:498. doi: 10.1302/0301-620X.71B3.2722947. [DOI] [PubMed] [Google Scholar]
- 8.Gilbert S.R., Lacheiwicz P.F. Primary synovial osteochondromatosis of the hip: report of two cases with long-term follow-up after synovectomy and a review of the literature. Am. J. Orthop. 1997;26:555. [PubMed] [Google Scholar]
- 9.Ogilvie-Harris D.J., Saleh K. Generalised synovial chondromatosis of the knee: a comparison of removal of the loose bodies alone with arthoscopic synovectomy. Arthroscopy. 1994;10:166. doi: 10.1016/s0749-8063(05)80088-x. [DOI] [PubMed] [Google Scholar]
- 10.Shpitzer T., Ganel A., Engelberg S. Surgery for synovial chrondromatosis. 26 cases followed up for 6 years. Acta Orthop. Scand. 1990;61:567. doi: 10.3109/17453679008993585. [DOI] [PubMed] [Google Scholar]
- 11.Roulet E., Le Viet D. Primary synovial osteochondromatosis of the hand and wrist; report of a series of 21 cases and literature review. Rev. Rheum. Engl. Ed. 1999;66:256–266. [PubMed] [Google Scholar]
- 12.Bashaireh K.M. Patellar subluxation with early-phase synovial chondromatosis of the knee. Orthopedics. 2016;39(1):176–179. doi: 10.3928/01477447-20151222-16. [DOI] [PubMed] [Google Scholar]
- 13.Steiner G.C., Meusher N., Norman A., Present D. Intracapsular and paraarticular chondromas. Clin. Orthop. Relat. Res. 1994;303:231–236. [PubMed] [Google Scholar]
- 14.Agha R.A., Fowler A.J., Saeta A., Borai I., Rajmohan S., Orgill D.P. SCARE group: the SCARE statement: consensus based surgical report guidelines. Int. J. Surg. 2016;34:180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]