Abstract
Background:
Astigmatism is the leading complication in visual recovery after penetrating keratoplasty (PKP) and deep anterior lamellar keratoplasty (DALK); in this study, we evaluated the outcome of femtosecond laser arcuate keratotomy (FLAK) after DALK and PKP in Iranian keratoconic patients.
Materials and Methods:
In this prospective interventional case series, refractive and keratometric predictability, efficacy, and complications of FLAK for postkeratoplasty astigmatism in keratoconus were evaluated; 23 eyes of 23 consecutive patients (mean age of 32.43 ± 9.11 years) with high astigmatism were enrolled. The femtosecond laser performed paired 90°-angled arcuate incisions.
Results:
Mean logarithm of the minimum angle of resolution of corrected and uncorrected visual acuity improved from preoperative values of 0.30 ± 0.18 and 0.85 ± 0.32 to 6-month values of 0.19 ± 0.17 and 0.65 ± 0.33, respectively (P < 0.05). Mean subjective astigmatism was 7.79 ± 2.64 diopter (D) preoperatively and 3.69 ± 2.25D at 6-month after surgery (P < 0.05). Surgically induced astigmatism was 9.27 ± 5.00D. Mean refractive spherical equivalent showed no significant (P = 0.69) hyperopic shift from − 4.21 ± 4.84D preoperatively to − 2.16 ± 6.09D postoperatively. Two (8.7%) microperforations were observed.
Conclusion:
FLAK is a relatively safe and effective method for the treatment of postkeratoplasty astigmatism.
Keywords: Astigmatic keratotomy, deep anterior lamellar keratoplasty, femtosecond laser, keratoconus, keratoplasty, penetrating keratoplasty
INTRODUCTION
Astigmatism is the leading complication in visual recovery after penetrating keratoplasty (PKP) and deep anterior lamellar keratoplasty (DALK) to the extent of more than five diopters (D) in up to 38% of cases.[1,2,3] About 8%–20% of postkeratoplasty patients have intolerable astigmatism that makes surgical interventions inevitable.[4]
Manual astigmatic keratotomy (AK) has poor reliability and predictability to reduce astigmatism and may be complicated with perforation, infection, gaping of the incision, and irregular astigmatism.[1] Hence, femtosecond laser arcuate keratotomy (FLAK) has become a reasonable alternative to mechanical techniques for its higher precision of the incisions with enhanced reproducibility and improved accuracy and safety profile.[5,6,7]
There are some reports regarding the refractive results of this new technology worldwide; however, outcomes of this technology in our country, Iran, are not reported. In this study, we evaluated the outcomes of FLAK after DALK and PKP in Iranian keratoconic patients.
MATERIALS AND METHODS
Study design and participants
The study was a prospective interventional case series. Informed written consent was obtained from all patients, and our institutional review board approved the study protocol. Patients with at least 4.5 diopters of regular astigmatism were included in the study. Furthermore, the interval between the primary keatoplasty and FLAK was at least 18 months and all sutures should hadc been removed at the time of surgery. Patients who failed to attend study visits were excluded from the study. FLAK was performed in 23 consecutive patients (11 males and 12 females with a mean age of 32.43 ± 9.11 years) who had been referred to our center for postkeratoplasty high astigmatism. The case series included 15 (65.2%) PKPs and 8 (34.8%) DALKs performed with big-bubble technique for keratoconus.
Procedures and variables assessment
The diameter of all grafts was 7.25–8.25 mm. The preoperative evaluation included slit lamp examination of anterior and posterior segment, refraction, logarithm of the minimum angle of resolution (logMAR) of uncorrected visual acuity (UCVA) and best spectacle-corrected visual acuity (BSCVA), corneal topography, and pachymetry with Pentacam (Oculus Optikgeräte, Wetzlar, Germany) and javal keratometry.
The graft thickness in the intended site of incision (1 mm inside the graft-host interface) was measured using a full pachymetry map of the Pentacam. Incision depth was set at 85% of the local corneal thickness. Based on previously published procedures,[2,4] steep and flat semimeridians were identified in the axial topographic maps of each patient and the surgical plan was drawn superimposed on it. The length of the relaxing arcuate incisions was determined ranged from 40° to 90°;[4,7] 40°–60° for up to 6 diopters, 65°–75° for 6–10 diopters, and 90° for >10 diopters of astigmatism.
Patients underwent paired AKs with the Femtec femtosecond laser (FSL) (20/10 perfect vision, Heidelberg, Germany). Then, under surgical microscope, a blunt spatula was used to separate eventual stromal tissue. At the end of surgery, all patients were administered with soft contact lenses; topical levofloxacin 5 mg/ml for 1 week; and topical betamethasone 0.1% for 4 weeks. UCVA and BSCVA in logMAR, automated keratometric and subjective refraction, and astigmatism were determined in all eyes at 6 months, postoperatively. In addition, we performed a power vector analysis (Kaye and Patterson method) of the astigmatic changes from baseline to 6 months, postoperatively.[8,9]
Statistics
Statistical analysis was performed using SPSS software version 13.0 (SPSS Inc., Chicago, Illinois, USA). Data were expressed as means ± standard deviation and a P < 0.05 was considered statistically significant. Paired t-test was used to assess the difference between pre- and post-operative values.
RESULTS
All patients completed the 6-month follow-up period. The mean interval from keratoplasty to AK was 50.65 ± 5.12 months. Pre- and post-operative crude details of series as regards, age, spherical equivalent (D), astigmatic dioptric power, axis (degrees), UCVA, and BSCVA are summarized in Table 1. Comparison of pre- and post-operative astigmatism and its reductions by three methods of refractive, autorefractive, and javal keratometry are summarized in Table 2.
Table 1.
Pre- and post-operative refractive astigmatism and visual acuity
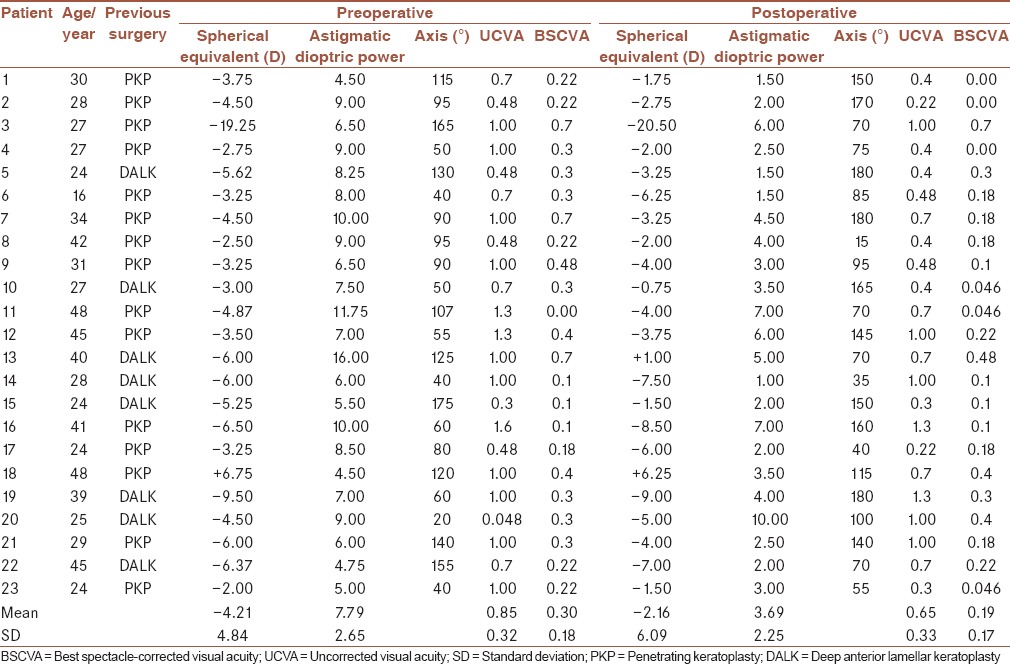
Table 2.
Pre- and post-operative astigmatism
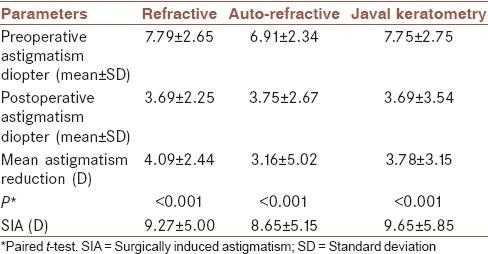
UCVA improved significantly from 0.85 ± 0.32, preoperatively to 0.65 ± 0.33, postoperatively (P = 0.003, paired t-test). BSCVA improved significantly from 0.3 ± 0.18, preoperatively to 0.19 ± 0.17, postoperatively (P = 0.002). Mean sphere significantly increased from − 0.85 ± 4.35D, preoperatively to − 2.41 ± 4.79D, postoperatively (P = 0.001). However, mean refractive spherical equivalent showed no significant (P = 0.692) hyperopic shift from − 4.21 ± 4.84D, preoperatively to − 2.16 ± 6.09D, postoperatively. Preoperative mean absolute refractive¸ autorefractometric, and keratometric astigmatisms were reduced from 7.79 ± 2.65, 6.91 ± 2.34, and 7.75 ± 2.76 to 3.69 ± 2.25, 3.75 ± 2.67, and 3.96 ± 3.54D, respectively, after 6 months (P < 0.001). The mean astigmatic reduction as regards the three aforementioned items was 4.09D, 3.16D, and 3.78D, respectively. Surgically induced astigmatisms were 9.27 ± 5.00, 8.65 ± 5.15, and 9.65 ± 5.85 with refraction, autorefractometery, and javal keratometry, respectively [Table 2].
Complications
Overcorrection occurred in 10 (43.5%) patients; four of which were in DALK (50% of DALK eyes) and 6 in PKP (40% of PKP eyes). Microperforation happened in one of two cuts in 2 patients (1 PKP eye and 1 DALK eye). Perforations were self-sealing neither requiring suturing nor being eventful. No keratitis or rejection occurred in our patients during 6 months of follow-up.
DISCUSSION
FSL is able to create quality arcuate incisions with precise length, depth, radius, and symmetry that were previously hard to achieve by manual techniques.[1,7,10] Furthermore, AK spares the visual axis and yields rapid visual rehabilitation.[11]
In our study, after FLAK, mean refractive, autorefractometric, and javal keratometric astigmatism was significantly reduced. Such reductions are comparable to recent reports.[2,6,7,10,11,12] Furthermore, improvement of UCVA and BSCVA after FLAK was documented in our study in line with what Kumar et al. found in their study.[7] Meanwhile, Hoffart et al. reported no significant improvement in UCVA and BCVA in spite of increase of ≥1 line of visual acuity in 70% of their patients; this could be probably due to the preoperative irregular corneal astigmatism in all of their cases.[6]
In this study, no meaningful hyperopic shift was seen (P = 0.69); some authors reported myopic shift[1,5,6,13] while others found hyperopic shift.[2,3,7,10,12] The main explanation for the absence of such changes may be that medium length incisions (30°–90°) may yield a coupling ratio of about one and no change in the spherical equivalent. Shorter incisions cause more flattening than steepening, whereas longer incisions reverse this ratio.[4]
In our study, overcorrection was seen in 10 eyes (43.5%); Four DALK and six PKP eyes. These results are comparable with two similar studies.[10,7] In a study, overcorrection occurred in 24% of patients.[7] Two-thirds of the overcorrected eyes had originally undergone PK for keratoconus. Same as they discussed, it is conceivable that ecstatic eyes are at great risk of overcorrection and all of our cases were keratoconic. In spite of conservative treatment regimen for FLAK, we observed high rate of overcorrection; hence, it seems mandatory to adjust a treatment nomogram in future studies.
This study is among the few ones in which Pentacam full pachymetry maps were used to assess the preoperative thickness and to plan the meridians for incisions. Buzzonetti et al. also used Pentacam for preoperative corneal thickness assessment.[12] Theoretically, this method may be of more accuracy than ultrasound pachymetry in evaluation of graft periphery, which may be confounded by the probe positioning.[2]
Two cases in our series (8.7%) experienced microperforation in one of the paired AKs, but they were self-sealing, requiring neither suturing nor being eventful. The reported perforation rate of AK with the Hanna arcitome, ranges from 2.5% to 4.5%,[2] which is lower than what we found; this can be explained by the notion that manual keratome blades are set at 75% of the graft thickness[2] while FLAK incisions are set at 85% in our cases. We postulate that our two microperforations could be due to the mechanical stress induced by Sinskey hook in separating tissue bridges within the margins of the cut rather than the incidence of primary full-thickness FSL cut. Low rate of microperforations in our study supports the usefulness of Pentacam full pachymetry in preoperative assessment of corneal thickness though further studies are warranted to clarify this issue.
One of the limitations of our study was inadequate sample size (DALK in eight eyes and PKP in 15 eyes). Further investigations with larger sample sizes in comparative randomized trials are mandatory to evaluate the optimal size, depth and location of AKs, and consequent clinical and topographic outcomes.
CONCLUSION
FLAK is a relatively safe and effective method for treatment of postkeratoplasty astigmatism. Further work is needed to develop newer nomograms for better prediction of this surgical modality.
Financial support and sponsorship
This project was funded by the Tehran University of Medical Sciences.
Conflicts of interest
There are no conflicts of interest.
AUTHORS’ CONTRIBUTIONS
MNH, HO and MM contributed in the conception and design of the work, conducting the study, drafting and revising the draft, approval of the final version of the manuscript and agreed for all aspects of the work.
MJ, FR, MAA, MM And SHA contributed in conducting the study, drafting and revising the draft, approval of the final version of the manuscript and agreed for all aspects of the work.
REFERENCES
- 1.Cleary C, Tang M, Ahmed H, Fox M, Huang D. Beveled femtosecond laser astigmatic keratotomy for the treatment of high astigmatism post-penetrating keratoplasty. Cornea. 2013;32:54–62. doi: 10.1097/ICO.0b013e31825ea2e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nubile M, Carpineto P, Lanzini M, Calienno R, Agnifili L, Ciancaglini M, et al. Femtosecond laser arcuate keratotomy for the correction of high astigmatism after keratoplasty. Ophthalmology. 2009;116:1083–92. doi: 10.1016/j.ophtha.2009.01.013. [DOI] [PubMed] [Google Scholar]
- 3.Kubaloglu A, Coskun E, Sari ES, Gunes AS, Cinar Y, Piñero DP, et al. Comparison of astigmatic keratotomy results in deep anterior lamellar keratoplasty and penetrating keratoplasty in keratoconus. Am J Ophthalmol. 2011;151:637–43.e1. doi: 10.1016/j.ajo.2010.10.029. [DOI] [PubMed] [Google Scholar]
- 4.Wu E. Femtosecond-assisted astigmatic keratotomy. Int Ophthalmol Clin. 2011;51:77–85. doi: 10.1097/IIO.0b013e31820f26cd. [DOI] [PubMed] [Google Scholar]
- 5.Rückl T, Dexl AK, Bachernegg A, Reischl V, Riha W, Ruckhofer J, et al. Femtosecond laser-assisted intrastromal arcuate keratotomy to reduce corneal astigmatism. J Cataract Refract Surg. 2013;39:528–38. doi: 10.1016/j.jcrs.2012.10.043. [DOI] [PubMed] [Google Scholar]
- 6.Hoffart L, Proust H, Matonti F, Conrath J, Ridings B. Correction of postkeratoplasty astigmatism by femtosecond laser compared with mechanized astigmatic keratotomy. Am J Ophthalmol. 2009;147:779–87. doi: 10.1016/j.ajo.2008.12.017. 787.e1. [DOI] [PubMed] [Google Scholar]
- 7.Kumar NL, Kaiserman I, Shehadeh-Mashor R, Sansanayudh W, Ritenour R, Rootman DS. IntraLase-enabled astigmatic keratotomy for post-keratoplasty astigmatism: On-axis vector analysis. Ophthalmology. 2010;117:1228–35.e1. doi: 10.1016/j.ophtha.2009.10.041. [DOI] [PubMed] [Google Scholar]
- 8.Kaye SB, Patterson A. Analyzing refractive changes after anterior segment surgery. J Cataract Refract Surg. 2001;27:50–60. doi: 10.1016/s0886-3350(00)00801-4. [DOI] [PubMed] [Google Scholar]
- 9.Zare MA, Hosseini Tehrani M, Gohari M. Management of corneal astigmatism by limbal relaxing incisions during cataract surgery. Iran J Ophthalmol. 2010;22:15–20. [Google Scholar]
- 10.Bahar I, Levinger E, Kaiserman I, Sansanayudh W, Rootman DS. IntraLase-enabled astigmatic keratotomy for postkeratoplasty astigmatism. Am J Ophthalmol. 2008;146:897–904.e1. doi: 10.1016/j.ajo.2008.07.004. [DOI] [PubMed] [Google Scholar]
- 11.Fares U, Sarhan AR, Dua HS. Management of post-keratoplasty astigmatism. J Cataract Refract Surg. 2012;38:2029–39. doi: 10.1016/j.jcrs.2012.09.002. [DOI] [PubMed] [Google Scholar]
- 12.Buzzonetti L, Petrocelli G, Laborante A, Mazzilli E, Gaspari M, Valente P. Arcuate keratotomy for high postoperative keratoplasty astigmatism performed with the intralase femtosecond laser. J Refract Surg. 2009;25:709–14. doi: 10.3928/1081597X-20090707-05. [DOI] [PubMed] [Google Scholar]
- 13.Bochmann F, Schipper I. Correction of post-keratoplasty astigmatism with keratotomies in the host cornea. J Cataract Refract Surg. 2006;32:923–8. doi: 10.1016/j.jcrs.2006.02.013. [DOI] [PubMed] [Google Scholar]


