Abstract
Background:
Osteonecrosis of the femoral head (ONFH) is a common disease with high disability rate. However, a few studies investigate the etiology and clinical characteristics of nontraumatic ONFH patients in China. Therefore, we conducted this cross-sectional study.
Materials and Methods:
Totally, information of 7268 nontraumatic ONFH patients treated between August 2005 and August 2015 was extracted from the medical records. The extracted information included the age, gender, diagnostic criteria, cause of nontraumatic ONFH, types of steroid use, and types of alcohol.
Results:
Among these included patients, there were 5126 (70.5%) male patients with average age of 44.5 years and 2142 (29.5%) female patients with average age of 47.6 years (P = 0.54). The number of steroid-, alcohol-, steroid/alcohol-, and idiopathic-induced nontraumatic ONFH men patients was 1684, 2310, 364, and 768, respectively, and nontraumatic ONFH women patients was 1058, 482, 140, and 462, respectively. Meanwhile, we found that both the levels of triglycerides (P = 0.03) and low-density lipoprotein (P = 0.02) were significantly changed in the idiopathic-induced nontraumatic ONFH patients.
Conclusion:
These results indicated the earlier onset of nontraumatic ONFH in male patients than in female patients, different main etiology for male (alcohol consumption) and female (steroid use) patients, and close relationship between the lipid metabolism and idiopathic-induced nontraumatic ONFH. Our findings could be helpful for researchers to investigate the pathogenesis of ONFH and aid the clinicians in the early prevention and diagnosis of nontraumatic ONFH.
Keywords: Alcohols, idiopathic, osteonecrosis, steroid
INTRODUCTION
Osteonecrosis of the femoral head (ONFH) is a pathological state with multiple possible etiologies and characterized by the bone marrow and death of osteocytes. It could lead to progressive destruction of the hip joint. ONFH could be divided into traumatic ONFH and nontraumatic ONFH. Nontraumatic ONFH, as the main type of ONFH, is characterized by the substantial morbidity and frequently total hip arthroplasty. A previous study reported that in the United States, the incidence of nontraumatic ONFH could be up to 20,000 cases per year.[1] Another study reported that the total number of nontraumatic ONFH patients in China was between 500 and 700 million.[2]
Recently, more and more researchers investigate this disease in the worldwide. In South Korea, an epidemiologic study showed that the prevalence of ONFH was estimated to 28.91/100,000.[3] In Japan, the prevalence of ONFH was about 8.93/100,000 in 2004.[4] Each year, there are 2500–3000 new cases in Japan,[4] 15,000–20,000 new cases in the United States,[5] and 100,000–200,000 new cases in China.[6] Moreover, these numbers are rising in the recent years. Up to now, the most consistent findings across studies about ONFH might be the disproportionately prevalent in men. Men are more vulnerable to experience this disease. The Japan study reported that the men-to-women ratio of ONFH was about 3:2.[4] Moreover, the South Korea study reported that the ratio was about 7:3.[3]
Although the etiology of ONFH has not been definitely demonstrated, risk factors include alcohol consumption, corticosteroid use, and coagulation abnormalities. Previous study reported that the nontraumatic ONFH patients accounted for over 70% of the whole ONFH patients.[7] Most of these cases are caused by alcohol consumption and steroid use. The rest of these cases are viewed as the idiopathic-induced ONFH patients with unclear etiologies, such as slipped capital femoral epiphysis, systemic lupus erythematosus, HIV infection, and hyperlipidemia.[8,9,10] Among the several common etiologies, Fukushima et al. reported that the steroid use (51%) was the main etiology in Japanese,[4] but Kang et al. reported that the most of nontraumatic ONFH patients belonged to idiopathic ONFH patients (51.4%) in South Korean.[3] These inconsistent results might be caused by the geographical difference and indicate that it is needed to conduct an epidemiological study to investigate the main etiology in Chinese people with nontraumatic ONFH.
MATERIALS AND METHODS
Nontraumatic osteonecrosis of the femoral head patients
This study was a cross-sectional study. Nontraumatic ONFH patients treated in the following hospitals between August 2005 and August 2015 were the candidates: the Affiliated Hospital of Zunyi Medical College, The Fifth Affiliated Hospital of Zunyi Medical College, and The Affiliated Zhongshan Hospital of Dalian University. This study was reviewed and approved by the Ethics Committee (Institutional Review Board) of Zunyi Medical College. Moreover, the methods were conducted according to the relevant guidelines and regulations. Two experienced clinicians who studied and treated nontraumatic ONFH for several years were in-charge of the patients’ recruiting.
Nontraumatic ONFH patients were diagnosed based on the criteria that were proposed by Mont and Hungerford in 1995.[11] The Association Research Circulation Osseous (ARCO) stage was used to assess the severity of ONFH.[12] Candidates met one of the following criteria were excluded: (1) patients with hip tuberculosis, a disease that could result in the defect and collapse of unilateral or bilateral femoral head; (2) patients with hip disease that was caused by infection, which might also result in the defect and collapse of unilateral or bilateral femoral head; (3) patients with congenital hip dysplasia; (4) patients with hemophilic arthritis; (5) patients with Kaschin–Beck disease; (6) patients who were <18 years old.
Etiologies judgment
Nontraumatic ONFH could be divided into three main types: nontraumatic ONFH caused by alcohol consumption, nontraumatic ONFH caused by steroid use, and idiopathic nontraumatic ONFH. Nontraumatic ONFH patients with clear history of long-term steroid use in the medical records were assigned into the steroid-induced nontraumatic ONFH group. Nontraumatic ONFH patients with clear history of long-term habitual alcohol consumption were assigned into the alcohol-induced nontraumatic ONFH group. Nontraumatic ONFH patients with clear history of long-term steroid use and habitual alcohol consumption in the medical record were assigned into the steroid/alcohol-induced nontraumatic ONFH group. Nontraumatic ONFH patients with no obvious causes in the medical records were assigned into the idiopathic-induced nontraumatic ONFH group.
Data collection
Two authors in this study independently screened all potential patients by the aforementioned criteria and completed the data abstraction. Any disagreement between the two authors was resolved by consensus, and if needed, a third one was consulted. Data retrieved from the medical records were collected in a structured fashion as follows: gender, age, ethnic, body mass index (BMI), age of disease onset, ARCO stage, diagnostic criteria (X-ray, magnetic resonance imaging, computed tomography or pathology), cause of ONFH (steroid, alcohol, or unclear etiologies), type and reason of steroid use, and type of alcohol.
Statistical analyses
Normal assumption was checked, and if not, the nonparametric method was used. Data were shown as the mean ± standard deviation or percentage. One-way analysis of variance, Chi-square test, multivariate logistic regression analysis, or Student's t-test was used when appropriate. If a significant difference was found, the Bonferroni or Tamhane's T2 post hoc test was further conducted to determine which two groups had significant difference. SPSS 19.0 software (IBM, New York) was used here to conduct analyses. The P < 0.05 was considered significantly different.
RESULTS
Included patients
First, there were 9048 candidates in these three hospitals. After screening with the aforementioned criteria, 1780 patients were excluded. Finally, 7268 nontraumatic ONFH patients with complete medical records were included in this study. Among these patients, there were 3042 (men: 1984; women: 1058) steroid-induced nontraumatic ONFH patients, 2492 (men: 2010; women: 482) alcohol-induced nontraumatic ONFH patients, 504 (men: 364; women: 140) steroid/alcohol-induced nontraumatic ONFH patients, and 1230 (men: 768; women: 462) idiopathic-induced nontraumatic ONFH patients. To analyze the risk factors of idiopathic ONFH, we selected 850 age- and gender-matched congenital hip dysplasia patients with total hip replacement surgery. The value of kappa was 0.928, which indicated that the extracted data between the two authors were highly consistent.
Age distribution
For male patients, the age of these patients ranged from 18 to 88 years. The average age was 44.8 ± 12.5, 45.5 ± 10.3, 43.2 ± 13.7, and 44.3 ± 12.8 years in the steroid-, alcohol-, steroid/alcohol-, and idiopathic-induced nontraumatic ONFH patients, respectively. Significant difference on the average age was not found here (P = 0.67). The major age distributions were 30–50 years. The peak age distributions were 30–40 years in both steroid- and steroid/alcohol-induced nontraumatic ONFH patients and 40–50 years in both alcohol- and idiopathic-induced nontraumatic ONFH patients. The detailed age distribution is described in Figure 1.
Figure 1.
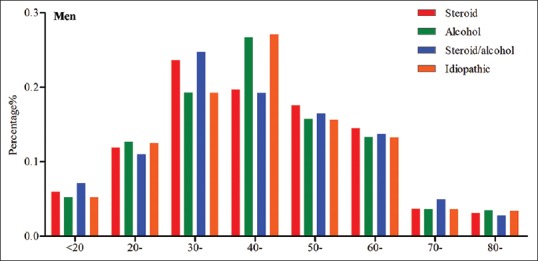
Age distribution in male patients with nontraumatic osteonecrosis of the femoral head
For female patients, the age of these patients ranged from 18 to 90 years. The average age was 47.2 ± 11.9, 48.9 ± 12.1, 46.1 ± 13.3, and 48.2 ± 10.8 years in the steroid-, alcohol-, steroid/alcohol-, and idiopathic-induced nontraumatic ONFH patients, respectively. Significant difference on the average age was not found here (P = 0.73). The major age distributions were 40–60 years. The peak age distributions were 40–50 years in both steroid- and steroid/alcohol-induced nontraumatic ONFH patients and 50–60 years in both alcohol- and idiopathic-induced nontraumatic ONFH patients. The detailed age distribution is described in Figure 2.
Figure 2.
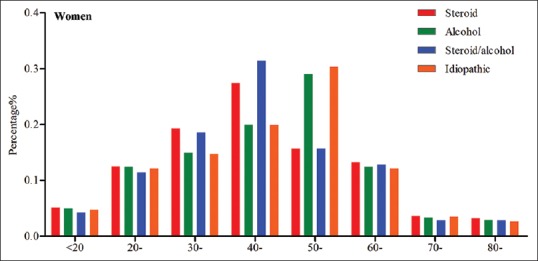
Age distribution in female patients with nontraumatic osteonecrosis of the femoral head
Etiologies composition
Totally, there were 5126 male patients and 2142 female patients. The male-to-female ratio was about 5:2. Among the male patients, the number of alcohol-induced ONFH patients was highest (2310 patients). There were also 1684 steroid-induced ONFH patients, 364 steroid/alcohol-induced ONFH patients, and 768 idiopathic-induced ONFH patients [Figure 3]. Among the female patients, the number of steroid-induced ONFH patients was highest (1058 patients). There were also 482 alcohol-induced ONFH patients, 140 steroid/alcohol-induced ONFH patients, and 462 idiopathic-induced ONFH patients [Figure 3].
Figure 3.
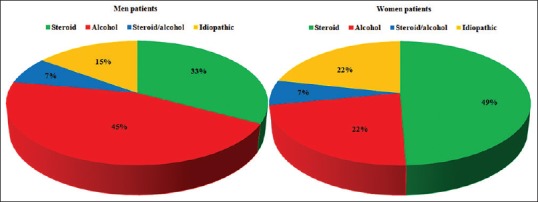
Etiologies composition in male and female patients with nontraumatic osteonecrosis of the femoral head
Steroid use
Among the 2742 steroid-induced nontraumatic ONFH patients, most of the patients (47.4%) used steroids because of autoimmune diseases [Figure 4]. The rest of patients used steroids because of skin diseases, respiratory diseases, kidney diseases, nervous system diseases, trauma/surgery, eye diseases, organ transplantation, inappropriate use of medicines, hematological system diseases, allergic diseases, and others. The type of steroid use included hydrocortisone, prednisone, prednisolone, dexamethasone, and fluocinonide. Among the 1299 patients used steroids, there were 658 patients (50.6%) using dexamethasone and 405 patients (31.2%) using prednisone. The glucocorticoids and prednisone were the most used steroids in China.
Figure 4.
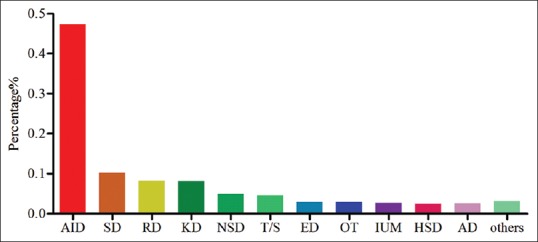
Different disease treated by steroid in nontraumatic osteonecrosis of the femoral head patients
Risk factors
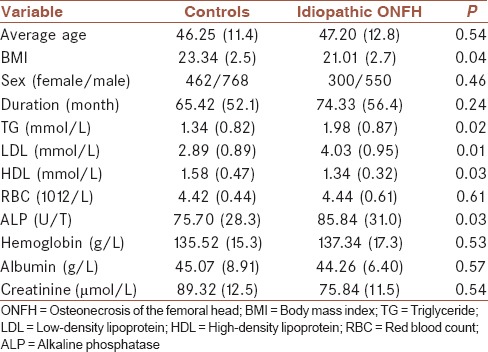
The following factors were used to analyze the risk factors of idiopathic ONFH: average age, BMI, sex ratio, duration of ONFH, triglycerides (TGs), low-density lipoprotein (LDL), high-density lipoprotein (HDL), alkaline phosphatase (ALP), red blood count, hemoglobin, albumin, and creatinine [Table 1]. Univariate analysis showed that these five factors were contributed to the idiopathic ONFH, including BMI (P = 0.04), TG (P = 0.02), LDL (P = 0.01), HDL (P = 0.03), and ALP (P = 0.03). However, the multivariate logistic regression analysis showed that only TG (P = 0.03) and LDL (P = 0.02) had a negative relationship with idiopathic ONFH.
Table 1.
Characteristics of the osteonecrosis of the femoral head patients and controls
DISCUSSION
ONFH is a common disease with high disability rate, which often occurs in the hips of patients. In the recent years, researchers have made remarkable progress in the ability to diagnose and to treat ONFH. There are many researchers investigating the etiology and clinical characteristics in patients with nontraumatic ONFH.[3,4,13] However, similar studies investigating the etiology and clinical characteristics of nontraumatic ONFH patients in China are still rare. Therefore, we conducted this study. As far as we know, this is the first study to investigate the etiology and clinical characteristics in Chinese patients with nontraumatic ONFH.
In this study, we found that among the included patients, there were 5126 (70.5%) male patients with average age of 44.5 years and 2142 (29.5%) female patients with average age of 47.6 years. The average age of female patients was 3.1 years greater than that of male patients, which indicated the earlier onset of nontraumatic ONFH in male patients. In analyzing the etiologies of nontraumatic ONFH, we observed that the steroid use and alcohol consumption were responsible for 77.9% of the male cases and 71.9% of the female cases. However, the main etiology was different between male and female patients. For men, the alcohol consumption (45.1%) was the main etiology; however, for women, the steroid use (49.4%) was the main etiology. Our findings were inconsistent with the previously published studies,[3,4] which might be caused by two reasons: (1) the studied patients were from the different countries and belonged to the different races; (2) our study took sex-based differences into consideration and separately studied the etiologies composition of male and female patients.
Our study found that the most used steroids were the glucocorticoids and prednisolone. Similarly, previous studies reported that the glucocorticoids could affect the metabolism of bone marrow stromal cells and induce adipogenesis in these cells, which finally led to nontraumatic ONFH.[14,15] Another study indicated that the actual time of onset of osteonecrosis in systemic lupus erythematosus patients was within the 1st month of high-dose corticosteroid treatment.[16] As for prednisone, Chernetsky et al. reported that the continuous prednisolone treatment (20 mg/day, 3 months; 60 mg/day, 1 month) could result in nontraumatic ONFH.[17]
Alcohol could cause the marrow necrosis, proliferation and hypertrophy of fat cells, diminished hematopoiesis, thinner and sparse trabeculae, and increased empty osteocyte lacunae, which all could found in the ONFH patients.[18] Wang et al. used 9.2 g/kg/day ethanol to induce osteonecrosis in rabbits,[18] and Broulík et al. used 7.22 g/kg/day ethanol to induce disturbances in bone metabolism in rats.[19] These animal studies showed a close relationship between the alcohol consumption and ONFH. Here, we found that the alcohol consumption was the main etiology in nontraumatic ONFH male patients. One study reported that the continuous alcohol consumption (400 ml/week) could obvious increase the risk of ONFH.[20] However, the exact quantity of alcohol that is needed to cause nontraumatic ONFH in human is still unclear.
In addition, we found that the level of TG and LDL were significantly changed in the idiopathic-induced nontraumatic ONFH patients. This finding matches up with the hypothesis that the ONFH might have a close relationship with the lipid metabolism.[21] The disturbed lipid metabolism might increase the risk of ONFH by the following ways. On the one hand, it might lead to the blood coagulation tendency in the tiny blood vessels of the femoral head and even the formation of lipid emboli on the inside of vessels. These phenomena could affect the blood supply and at last result in ONFH. On the other hand, it might cause the increase of fat cells in the bone marrow cavity and adipose tissue accumulation, which leads to the increase in marrow cavity pressure. Then, the blood supply is affected, and at last, the ONFH emerges.
This study had several limitations: (1) most of the recruited patients were from the same place, which might limit the applicability of our findings;[22] (2) as an epidemiological study, we only studied the etiology and clinical characteristics in patients with nontraumatic ONFH, but not explored its pathogenesis; (3) there were similar studies in other countries, but the geographical difference might result in the different conclusions;[3,4] our study found the different main etiology for male patients (alcohol consumption) and female patients (steroid use).
CONCLUSION
We found in this study that the male patients had the earlier onset of nontraumatic ONFH than female patients, the main etiology for male (alcohol consumption) and female (steroid use) patients was different, and there might be a close relationship between the lipid metabolism and idiopathic-induced nontraumatic ONFH. Our findings could be helpful for the investigation of etiology and pathogenesis of nontraumatic ONFH and aid the clinicians in the early prevention and diagnosis of nontraumatic ONFH.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
AUTHORS’ CONTRIBUTION
FL and DWZ designed the experiments, interpreted the data, and revised the manuscript. WW, LY, and BJW collected the data. JCW and WFC conducted the statistical analyses. All authors made a significant contribution to and approved the final manuscript.
Acknowledgments
We sincerely thank all the researchers and co-medical staff in our department for their excellent work.
REFERENCES
- 1.Koo KH, Kim R, Ko GH, Song HR, Jeong ST, Cho SH. Preventing collapse in early osteonecrosis of the femoral head. A randomised clinical trial of core decompression. J Bone Joint Surg Br. 1995;77:870–4. [PubMed] [Google Scholar]
- 2.Liu TG, Chen WH. Research progress of epidemiology about nontraumatic osteonecrosis of the femoral head. Med Recapitulate. 2009;15:2637–9. [Google Scholar]
- 3.Kang JS, Park S, Song JH, Jung YY, Cho MR, Rhyu KH. Prevalence of osteonecrosis of the femoral head: A nationwide epidemiologic analysis in Korea. J Arthroplasty. 2009;24:1178–83. doi: 10.1016/j.arth.2009.05.022. [DOI] [PubMed] [Google Scholar]
- 4.Fukushima W, Fujioka M, Kubo T, Tamakoshi A, Nagai M, Hirota Y. Nationwide epidemiologic survey of idiopathic osteonecrosis of the femoral head. Clin Orthop Relat Res. 2010;468:2715–24. doi: 10.1007/s11999-010-1292-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mont MA, Zywiel MG, Marker DR, McGrath MS, Delanois RE. The natural history of untreated asymptomatic osteonecrosis of the femoral head: A systematic literature review. J Bone Joint Surg Am. 2010;92:2165–70. doi: 10.2106/JBJS.I.00575. [DOI] [PubMed] [Google Scholar]
- 6.Liu LY. Analysis of osteonecrosis of the femoral head. Chin J Convalescent Med. 2007;16:447–8. [Google Scholar]
- 7.Wang FY, Ma ZS, Ma SY, Su BC, Chen SL, Li RJ, et al. Seroepidemiological survey and study on ischemic necrosis of femoral head. China J Orthop Traumatol. 2001;14:25–6. [Google Scholar]
- 8.Malizos KN, Karantanas AH, Varitimidis SE, Dailiana ZH, Bargiotas K, Maris T. Osteonecrosis of the femoral head: Etiology, imaging and treatment. Eur J Radiol. 2007;63:16–28. doi: 10.1016/j.ejrad.2007.03.019. [DOI] [PubMed] [Google Scholar]
- 9.Larson AN, McIntosh AL, Trousdale RT, Lewallen DG. Avascular necrosis most common indication for hip arthroplasty in patients with slipped capital femoral epiphysis. J Pediatr Orthop. 2010;30:767–73. doi: 10.1097/BPO.0b013e3181fbe912. [DOI] [PubMed] [Google Scholar]
- 10.Morse CG, Mican JM, Jones EC, Joe GO, Rick ME, Formentini E, et al. The incidence and natural history of osteonecrosis in HIV-infected adults. Clin Infect Dis. 2007;44:739–48. doi: 10.1086/511683. [DOI] [PubMed] [Google Scholar]
- 11.Mont MA, Hungerford DS. Non-traumatic avascular necrosis of the femoral head. J Bone Joint Surg Am. 1995;77:459–74. doi: 10.2106/00004623-199503000-00018. [DOI] [PubMed] [Google Scholar]
- 12.Choi HR, Steinberg ME, Y Cheng E. Osteonecrosis of the femoral head: Diagnosis and classification systems. Curr Rev Musculoskelet Med. 2015;8:210–20. doi: 10.1007/s12178-015-9278-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mont MA, Jones LC, Hungerford DS. Nontraumatic osteonecrosis of the femoral head: Ten years later. J Bone Joint Surg Am. 2006;88:1117–32. doi: 10.2106/JBJS.E.01041. [DOI] [PubMed] [Google Scholar]
- 14.Tan G, Kang PD, Pei FX. Glucocorticoids affect the metabolism of bone marrow stromal cells and lead to osteonecrosis of the femoral head: A review. Chin Med J (Engl) 2012;125:134–9. [PubMed] [Google Scholar]
- 15.Yin L, Li YB, Wang YS. Dexamethasone-induced adipogenesis in primary marrow stromal cell cultures: Mechanism of steroid-induced osteonecrosis. Chin Med J (Engl) 2006;119:581–8. [PubMed] [Google Scholar]
- 16.Oinuma K, Harada Y, Nawata Y, Takabayashi K, Abe I, Kamikawa K, et al. Osteonecrosis in patients with systemic lupus erythematosus develops very early after starting high dose corticosteroid treatment. Ann Rheum Dis. 2001;60:1145–8. doi: 10.1136/ard.60.12.1145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chernetsky SG, Mont MA, LaPorte DM, Jones LC, Hungerford DS, McCarthy EF. Pathologic features in steroid and nonsteroid associated osteonecrosis. Clin Orthop Relat Res. 1999;368:149–61. [PubMed] [Google Scholar]
- 18.Wang Y, Yin L, Li Y, Liu P, Cui Q. Preventive effects of puerarin on alcohol-induced osteonecrosis. Clin Orthop Relat Res. 2008;466:1059–67. doi: 10.1007/s11999-008-0178-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Broulík PD, Vondrová J, Ruzicka P, Sedlácek R, Zíma T. The effect of chronic alcohol administration on bone mineral content and bone strength in male rats. Physiol Res. 2010;59:599–604. [PubMed] [Google Scholar]
- 20.Hirota Y, Hirohata T, Fukuda K, Mori M, Yanagawa H, Ohno Y, et al. Association of alcohol intake, cigarette smoking, and occupational status with the risk of idiopathic osteonecrosis of the femoral head. Am J Epidemiol. 1993;137:530–8. doi: 10.1093/oxfordjournals.aje.a116706. [DOI] [PubMed] [Google Scholar]
- 21.Ke H, Yujin T. Experiment study on intervention effects of pravastatin on alcoholic osteonecrosis of femoral head. Chongqing Med. 2013;9:6. [Google Scholar]
- 22.Chen JJ, Zhou CJ, Liu Z, Fu YY, Zheng P, Yang DY, et al. Divergent urinary metabolic phenotypes between major depressive disorder and bipolar disorder identified by a combined GC-MS and NMR spectroscopic metabonomic approach. J Proteome Res. 2015;14:3382–9. doi: 10.1021/acs.jproteome.5b00434. [DOI] [PubMed] [Google Scholar]


