Abstract
Lung cancer is a common fatal malignancy in both men and women. Xuanwei, Yunnan has the highest incidence of lung cancer in China. The area has a specific risk factor in the domestic combustion of bituminous coal, and lung cancer patients from this area tend to be resistant to platinum-based treatments. However, little is known about the mechanism of platinum resistance in patients from Xuanwei. Herein, we used lentiviral infection with shRNA to silence expression of the DNA repair enzyme ERCC1 in XWLC05 both in its RNA and protein expression level, a lung adenoma cell line derived from a patient from Xuanwei. ERCC1 expression in this cell line is high and contributes to its resistance to cisplatin. Suppression of ERCC1 decreased XWLC05 proliferation in vitro (IC50 of cisplatin 1.34 µM for shRNA-infected cells vs. 4.54 µM for control cells) and increased the apoptotic rate after treatment with cisplatin (81.2% shRNA cells vs. 58% control cells, P<0.05). Progression-free survival was longer in ERCC1-negative lung adenoma patients than those with high ERCC1 levels (30 vs. 11 months, P<0.0001). ERCC1 expression was identified as a prognostic marker for overall survival in the patient cohort with operable lesions. Taken together, our data identify ERCC1 as a disease marker in lung adenoma patients from Xuanwei and confirm the significance of resection for the subsequent effect of platinum treatment in these patients. Additional studies are needed to determine the mechanism of ERCC1-induced platinum resistance in lung adenoma patients from Xuanwei.
Keywords: cisplatin, ERCC1, lung adenoma, XWLC05, Xuanwei patients
Introduction
Lung cancer is a common malignancy in China. In 2015, the incidence was approximately 733 per 100,000 people and the age-standardized mortality rate was approximately 610 per 100,000. Lung cancer is one of the top five most diagnosed cancers in both genders, and there is a significant upward trend in the age-standardized incidence rates in females (1). Xuanwei, Yunnan is well known for its high incidence of lung cancer (2). Domestic combustion of bituminous coal (referred to as ‘smoky’ coal) is the most important risk factor for lung cancer, rather than tobacco exposure (3). The highest incidence of lung cancer in Xuanwei occurs among farmers, and the most common histological type is adenocarcinoma. Women living in this area are also more susceptible to lung cancer (4–6). Therefore, lung adenoma patients in Xuanwei appear to differ from those in other areas.
Platinum-based chemotherapy has been standard treatment for lung cancer for decades. However, the efficacy of platinum therapies can be seriously hindered by drug resistance, especially to cisplatin (7,8). Cisplatin binds to DNA to create platinum-DNA adducts that can induce covalent cross-linking between DNA strands. In turn, this activates the apoptotic pathway, resulting in cell death (9). Mismatch repair and nucleotide excision repair (NER) are particularly important mechanisms in the effects of platinum-based agents. NER is a highly conserved DNA repair pathway that acts by altering the helical structure of the DNA molecule and excising damaged DNA fragments. This pathway involves three important steps: recognition of DNA damage, formation of a complex that unwinds and excises the damaged portion, and finally, resynthesis of the damaged sequence and ligation (10). The excision repair cross-complementation group 1 (ERCC1) enzyme, which recognizes and removes cisplatin-induced DNA adducts (11–13), plays a rate-limiting role in the NER pathway. High ERCC1 expression in solid tumors predicts poor prognosis and suggests a higher possibility of resistance to platinum treatments (14–20). This is also true for lung cancer patients, and low ERCC1 expression is beneficial in non-small cell lung cancer patients (8,21–24).
In our previous study (25), we showed that ERCC1 expression is significantly higher in Xuanwei lung adenocarcinoma patients before treatment than patients from other areas. However, it is not known how the high ERCC1 levels affect the prognosis of this patient population. Herein, we hypothesize that high ERCC1 expression may be related to the response to platinum-based chemotherapy and may predict poor prognosis in lung adenoma patients from Xuanwei.
Materials and methods
Cell lines and cell culture
The established human lung adenocarcinoma cell line XWLC05 was obtained from No. 1 Affiliated Hospital of Kunming Medical University. Cells were maintained in RPMI-1640 medium (HyClone, Thermo Scientific, Waltham, MA, USA) supplemented with 10% fetal bovine serum (Gibco Life Technologies, Carlsbad, CA, USA), 100 U/ml penicillin (Biowest, Nuaillé, France), and 100 U/ml streptomycin (Biowest) and incubated at 37°C in a humidified 5% CO2 atmosphere.
Viral infection
A lentiviral vector carrying ERCC1 shRNA was designed and constructed by GeneChem Co., Ltd. (Shanghai, China). Cells were infected with the lentivirus twice for 2 days each and positive clones were selected with puromycin (200 ng/ml) for 7–10 days. Control cell lines were generated by infecting with viruses containing the empty vector, following the same protocol.
Real-time PCR
For each cell line, total RNA from 3×106 cells was isolated using TRIzol reagent (Invitrogen, Carlsbad, CA, USA). RNAs were then reverse transcribed into cDNAs for Real-time PCR analysis using an ExScript RT-PCR kit (Takara, Shiga, Japan). Oligonucleotide primers for ERCC1 were 5′-CGTGCTGTACCTCTCGC-3′ (forward primer) and 5′-CTGAGGAACGGTTCCTG-3′ (reverse primer), and primers for glyceraldehyde 3-phosphate dehydrogenase (GAPDH) were 5′-GGCCTCCAAGGAGTAAGACC-3′ (forward primer) and 5′-CAAGGGGTCTACATGGCAAC-3′ (reverse primer). Amplification and detection were carried out in the Applied Biosystems Prism 7900 system (Applied Biosystems, Foster City, CA, USA) using an ExScript SYBR Green QPCR kit (Takara) and the following conditions: 95°C for 10 sec; 40 cycles of 95°C for 5 sec, 62°C for 31 sec; followed by a 30-min melting curve analysis to verify the primer dimers. Statistical analysis was performed using the 2−∆∆CT relative quantification method.
CCK-8 proliferation assay
Cell proliferation was measured using a CCK-8 assay kit (Dojindo, Japan) according to the manufacturer's protocol. Cells were seeded in 96-well plates (2×103 cells/well) and 10 µl CCK-8 solution was added to each well on days 0, 1, 2, 3, 4, and 5. The plates were incubated at 37°C in 5% CO2 for 1 h, and the absorbance of each sample at 450 nm was measured using a microplate reader. Three independent experiments were required for this assay.
Colony-forming assay
A total of 500 cells were seeded at single-cell density in 6-well plates with fresh medium with or without cisplatin and allowed to grow for at least a week. Colonies with more than 50 cells were then stained with gentian violet (Solarbio) and counted.
Western blot analysis
Western blot analysis was performed to determine protein expression levels. The cells were harvested, washed with cold phosphate-buffered saline (PBS), lysed with RIPA lysis buffer (Beyotime) for 30 min on ice, and then centrifuged at 12,000 × g for 15 min at 4°C. The total protein concentration in the supernatant was determined using a BCA protein assay kit (Beyotime). Equal amounts (30 µg per lane) of protein were separated by SDS-PAGE and transferred to polyvinylidene fluoride membranes (Millipore). The membranes were blocked with 10% non-fat milk, incubated with primary antibodies, and then incubated with secondary antibodies conjugated to horseradish peroxidase. The protein bands were revealed by incubation with chemiluminescent reagents (Millipore). Antibodies to ERCC1 were from Proteintech. The antibody to β-actin was purchased from Sigma-Aldrich (St. Louis, MO, USA). Three independent protein samples were harvested and tested to make sure that ERCC1 gene has been successfully silenced.
Drugs
Cisplatin was purchased from Sigma-Aldrich and stored at a concentration of 5 mM in dimethyl sulfoxide (DMSO). XWLC05 cells were incubated with cisplatin at a concentration of 1 µM unless otherwise specified.
Cell apoptosis assay
Cells were incubated with various concentrations of cisplatin or DMSO for 48 h and then harvested, washed twice with cold PBS, and resuspended in 200 µl binding buffer at a density of 1×105 cells/ml. The cells were stained with 5 µl Annexin V and propidium iodide (PI) (BD Biosciences) for 15 min in the dark at room temperature and then analyzed by flow cytometry (Cytomics FC 500 MPL, Beckman Coulter). Early- and late-stage apoptosis was determined by the percentage of Annexin V+/PI− and Annexin V+/PI+ cells, respectively. The results are expressed as the mean values from three independent determinations.
Animal experiments
The animal experiments were approved by the Institutional Animal Care and Use Committee of Kunming Medical University and were performed following Institutional guidelines and protocols. XWL05 cells stably expressing ERCC1 shRNA were generated by retroviral infection. Tumors were induced by injecting 5×106 cells of each cell line subcutaneously into 4- to 6-week-old BALB/c female athymic nude mice (Department of Laboratory Animals, Kunming Medical University). Each cell type was injected into seven mice, respectively. Mice were treated with 5 mg/kg cisplatin by intraperitoneal injection every 3 days for 2 weeks (five injections) starting immediately after injection of tumor cells. Control mice received injections of PBS. One week after the last cisplatin injection, the mice were sacrificed and the tumors were weighed. The longest diameter ‘a’ and the shortest diameter ‘b’ of the tumors were measured and the tumor volumes were calculated using the following formula: volume (in mm3) = a × b2 × 0.52, where 0.52 is a constant to calculate the volume of an ellipsoid. Three tumors per cell line were excised, fixed in 10% formalin overnight, and subjected to routine histological examination by investigators who were blinded to the tumor status. Animal experiments were repeated twice.
Immunohistochemical staining
Samples from the mouse tumor xenografts and lung tumor tissue from patients were subjected to immunohistochemical (IHC) staining to detect ERCC1 expression. Antibodies to ERCC1 were from Maixin (Fuzhou, China, mouse clone 8F1). Paraffin-embedded sections were pre-treated and stained with antibodies as previously reported (26). Secondary antibodies against mouse or rabbit IgG were supplied in an IHC kit (#CW2069) from Beijing Cowin Bioscience Co. Ltd (Beijing, China).
IHC scoring
Differentiated degree of these tissue samples collected from our patients were classified into well differentiated or poor differentiated according to the pathological evaluation system of our hospital. The stained tissue sections were scored separately by two pathologists blinded to the clinical parameters. The staining intensity was scored as 0 (negative), 1 (weak), 2 (medium), or 3 (strong). The staining extent was scored as the percentage of positively stained area compared with the entire carcinoma area and was scored as 0 (<5%), 1 (5–25%), 2 (26–50%), 3 (51–75%), and 4 (>75%). Scores for the staining intensity and extent were multiplied to generate an immunoreactivity score for each sample. Tissues with a total immunoreactivity score of <4, 4, 6, and ≥8 were expressed as -, +, ++, and +++, respectively. In our research, IHC score ≥6 was defined as high ERCC1 expression and IHC score ≤4 was low expression.
Patient information
Sections of lung adenoma tissue were obtained from 106 operable patients who were staged based on the 7th edition of the AJCC Cancer Staging Manual and graded based on WHO criteria. The patients had undergone radical surgery at the Department of Thoracic Surgery of No. 3 Affiliated Hospital of Kunming Medical University (Yunnan Provincial Tumor Hospital) between January 2009 and September 2011. Each patient provided written informed consent, and the study was approved by the ethics committee of No. 3 Affiliated Hospital of Kunming Medical University (Yunnan Provincial Tumor Hospital). We explored the relationship between ERCC1 expression levels and patient survival by IHC staining of ERCC1 in sections from the 106 patients, who had received cisplatin, carboplatin, gemcitabine, or vinorelbine as first-line chemotherapy between December 2008 and April 2012 in No. 3 Affiliated Hospital of Kunming Medical University (Yunnan Provincial Tumor Hospital). Complete follow-up information was available.
Statistical analysis
SPSS software (version 18.0) was used for statistical analysis. Student's t-test or ANOVA were used to compare quantitative data and Chi-square or Kruskal-Wallis tests were used to assess qualitative data. A P-value of <0.05 (two tailed) was considered statistically significant. The median progression-free survival (PFS) and overall survival (OS) were estimated by the Kaplan-Meier method and compared using a log-rank test.
Results
ERCC1 silencing reverses XWLC05 cell cisplatin resistance
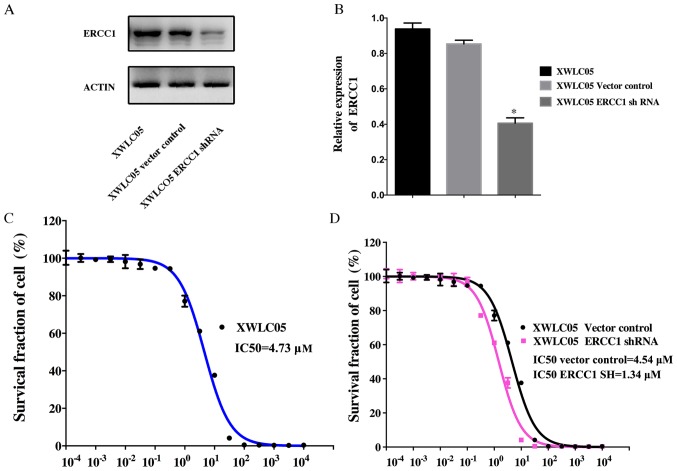
Expression of ERCC1 was examined in cultured unmanipulated XWLC05 cells and cells expressing empty vector (Vector Control) or ERCC1 shRNA (Fig. 1A and B). The level of ERCC1 in XWLC05-ERCC1-shRNA cells was significantly lower than that in XWLC05 and Vector Control cells.
Figure 1.
Cisplatin IC50 of ERCC1 silencing XWLC05 cell line decreased significantly. (A and B) Efficiently ERCC1 silencing XWLC05 cell line and its control were verified by immunoblotting and real-time PCR. (C) Cisplatin IC50 of XWLC05 was 4.73 µM. (D) Cisplatin IC50 of XWLC05 ERCC1-shRNA cell line and its control were 4.54 and 1.34 µM, respectively.
To evaluate the anticancer effect of cisplatin, XWLC05, Vector Control, and XWLC05-ERCC1-shRNA cells were treated with concentrations of cisplatin ranging from 1×10−4 to 1×104 µM. A dose-dependent cytotoxic effect of cisplatin was observed in these cell lines (Fig. 1C and D). The half-maximal inhibitory concentration (IC50) for XWLC05, Vector Control, and XWLC05-ERCC1-shRNA cells was 4.73, 4.54, and 1.31 µM, respectively (P<0.05).
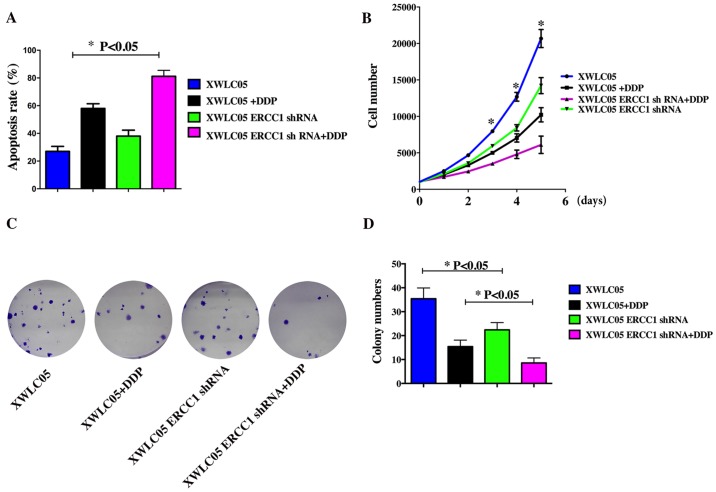
ERCC1 silencing increases apoptosis and inhibits proliferation of cisplatin-treated cancer cells in vitro
We studied the effect of cisplatin treatment on apoptosis in the cell lines. After 24 h treatment with cisplatin at 1 µM, XWLC05, Vector Control, and XWLC05-ERCC1-shRNA cells were double-stained with Annexin V and PI and subjected to flow cytometry to quantify apoptosis (Fig. 2A). Cisplatin induced apoptosis in all cell lines; however, XWLC05-ERCC1-shRNA cells showed a higher apoptotic rate than Vector Control cells after incubation with or without cisplatin.
Figure 2.
ERCC1 silencing increased cisplatin sensitivity of XWLC05 cell line in vitro. (A) Quantitative analysis of apoptotic cells under the treatment of cisplatin (1 µM) in ERCC1 silencing cell line and its controls (P<0.05). Error bar 95% Confidence intervals (Cis). (B) The proliferous capacity of XWLC05 ERCC1-shRNA cell line and its control with or without the treatment of cisplatin (1 µM) by CCK8 kit (P<0.05). Error bars 95% CIs. (C and D) Detection of colony formation ability of XWLC05 ERCC1-shRNA cell line and its control with or without the treatment of cisplatin (1 µM) and quantitative analysis of colony formation (P<0.05). Error bars 95% CIs.
The CCK-8 assay showed that cell proliferation was significantly suppressed in XWLC05-ERCC1-shRNA cells compared with control cells treated with the same cisplatin concentration (Fig. 2B). Moreover, ERCC1 silencing also significantly inhibited the colony-forming ability of XWLC05 cells (Fig. 2C and D).
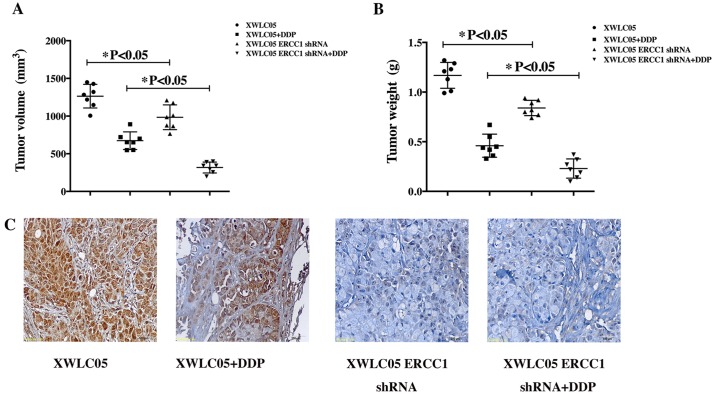
ERCC1 silencing inhibits proliferation and increases cisplatin sensitivity of XWLC05 cells in vivo
The effect of ERCC1 on XWLC05 cells in vivo was investigated by injecting XWLC05-ERCC1-shRNA cells and the corresponding Vector Control cells subcutaneously into nude mice and then treating the mice with vehicle or cisplatin (5 mg/kg) for 2 weeks. Tumor sizes were measured every 7 days. The mean volumes of tumors formed by XWL05 control cells and XWLC05-ERCC1-shRNA cells at day 35 were 1264 and 984 mm3, respectively (Fig. 3A, P<0.05). After cisplatin treatment, the mean tumor volumes at day 35 were 674 and 317 mm3, respectively (Fig. 3A, P<0.05). Thus, the growth of XWLC05-ERCC1-shRNA cells was most significantly inhibited by cisplatin in vivo. The tumor weights from the four mouse groups showed similar results (Fig. 3B). The mean weight of tumors formed by XWL05 control cells and XWLC05-ERCC1-shRNA cells at day 35 were 1.16 g and 0.84 g, respectively (P<0.05). After cisplatin treatment, the mean tumor weight at day 35 were 0.46 g and 0.23 g, respectively. We confirmed that expression of ERCC1 was efficiently inhibited in the xenograft mouse model by performing IHC analysis of tumor sections from each experimental group (Fig. 3C).
Figure 3.
XWLC05 ERCC1-shRNA cell line and its control xenograft tumor burden in mice with or without the treatment of cisplatin. (A and B) In vivo tumorigenesis examined by animal assay and subcutaneous tumor growth from mice injected with XWLC05 ERCC1-shRNA cell line and its control with or without the treatment of cisplatin (n=7 for each group, P<0.05 in XWLC05 ERCC1-shRNA groups). Error bars 95% CIs. Images show tumor volume and tumor weight of mice at the end of observation. (C) Immunohistochemical staining of xenograft tumor tissues. Tissues were stained with rabbit anti-ERCC1 antibody and visualized with goat anti-rabbit secondary antibody (magnification of ×400).
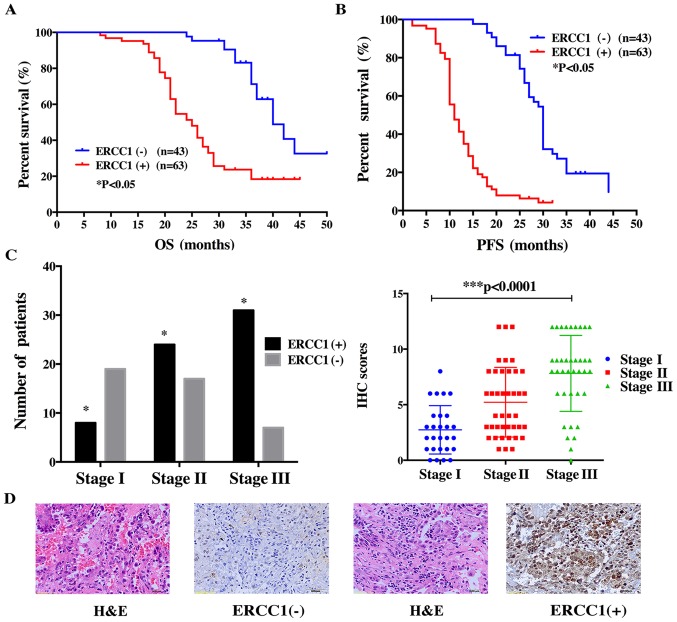
ERCC1 expression predicts poor prognosis in lung adenoma patients
The mean age of the 106 patients in the study was 62.7 years (range 30–79 years) (Table I). The surgical disease stage was 27 (25.4%) stage I, 41 (38.8%) stage II, and 38 (35.8%) stage III. There were 31 (29.2%) patients with well-differentiated (low-grade) tumors and 75 (70.8%) patients with poorly differentiated (high-grade) tumors. Among the 106 patients, 90 (84.9%) received adjuvant chemotherapy and 40 (37.7%) received radiotherapy. The mean follow-up interval was 30 months (range 2–55 months). At the last follow-up, 93 (87.7%) patients had progressive disease after first-line chemotherapy and 64 (60.4%) patients had died. The median PFS was 17 months (range, 2–44 months) and the median OS was 30 months (range, 8–50 months).
Table I.
Clinical characteristics of this cohort.
| Characteristics | N (%) |
|---|---|
| Age at diagnosis (years) | |
| Mean ± SD | 62.7±11.3 |
| Gender | |
| Male | 44 (41.5) |
| Female | 62 (58.5) |
| Smoking status | |
| Yes | 50 (47.2) |
| No | 56 (52.8) |
| TNM stage | |
| I | 27 (25.5) |
| II | 41 (38.7) |
| III | 38 (35.8) |
| Pathology grading | |
| Well-differentiated | 33 (31.1) |
| Poor-differentiated | 73 (68.9) |
| Receive chemotherapy | |
| Yes | 92 (86.8) |
| No | 14 (13.2) |
| Receive radiotherapy | |
| Yes | 55 (51.9) |
| No | 51 (48.1) |
To confirm the relationship between the expression level of ERCC1 and the survival of lung adenoma patients, we performed IHC in the 106 patients with operable stage disease (Ia-IIIa). The results showed that positive ERCC1 staining was significantly associated with poor OS and PFS (Fig. 4A and B). In this patient cohort, we found that ERCC1 positivity correlated with disease progression. Lung adenoma samples were positive for ERCC1 in only 8 of 27 stage I patients but in 31 of 38 patients with stage III disease (Fig. 4C). This trend was also observed in the IHC score (Fig. 4D). For stage I patients, the IHC score was 2.74±0.42, increasing significantly to 5.22±0.48 in stage II patients and to 7.62±0.62 in stage III patients. These data suggest that as the disease progresses, lung adenoma tissues become increasingly positive for ERCC1.
Figure 4.
Correlation of ERCC1 expression in operable Xuanwei lung adenoma patient samples and the association of ERCC1 with patient survival. (A and B) Favorable overall survival and progression-free survival were associated with negative nuclear accumulation of ERCC1 (P<0.05). (C) The number of ERCC1 positive patients and IHC score of each case in the different stage groups. Increasingly more patients were detected as ERCC1-positive as the disease progressed (Chi-square test was applied for the analysis of ERCC1 positive rate. P<0.05). Stage IIIa patients had the highest IHC score. (Kruskal-Wallis test was applied for the analysis of IHC score of protein expression *P<0.05). (D) Typical patient samples of ERCC1 expression. Slides were stained with rabbit anti-ERCC1 antibody and visualized with goat anti-rabbit secondary antibody (magnification of ×400).
Discussion
In this study, we constructed a lentiviral vector encoding ERCC1-specific short hairpin RNA (shRNA) and transfected it into the lung adenocarcinoma cell line XWLC05, established from a patient from Xuanwei. Western blotting and quantitative PCR analysis confirmed the silencing efficiency of the ERCC1 shRNA construct. ERCC1 silencing increased XWL05 sensitivity to cisplatin, as reflected by the significant decrease in cisplatin IC50 values. Flow cytometric analysis showed that ERCC1 shRNA-infected cancer cells treated with cisplatin had a significantly higher rate of apoptosis compared with control cells. In vivo, the volume of tumors derived from XWLC05-ERCC1-shRNA cells was significantly lower after cisplatin treatment compared with tumors grown from control cells, which was consistent with the data from in vitro experiments. In a clinical cohort study of Xuanwei patients, we evaluated ERCC1 expression by IHC staining of tissue sections from 106 patients with operable lung adenoma. ERCC1 expression was predictive of worse prognosis, as reflected by the higher number of ERCC1-positive patients with advanced disease. This may be related to the active rate of cancer cell division in the advanced stage of disease, since DNA damage repair pathways are critical for cell division.
Drug resistance is associated with worse prognosis in cancer. Given the mechanism of platinum drug-induced killing of cancer cells and the involvement of ERCC1 in DNA damage repair, it is reasonable to assume that higher ERCC1 levels would be associated with worse prognosis. Our research confirms previous studies in this regard (27–32). Higher ERCC1 expression results in a lower mutational load in lung cancer patients (33) since ERCC1 repairs mismatch during DNA replication. Lower mutational load is related to the poor response to immunotherapy and body immunity of cancer patients, likely because it reduces the number of antigenic tumor epitopes available for detection by the immune system (34,35). Our research confirms the ERCC1 expression status of Xuanwei lung adenoma patients and suggests that ERCC1 could be a predictive marker for identifying patients suitable for immunotherapy. Thus, positive ERCC1 expression may predict a poor response to immunotherapy. Further studies will be needed to establish the role of ERCC1 in the immune response of Xuanwei adenoma patients.
Previous studies (36,37) suggested that lower ERCC1 RNA expression might be related to shorter survival of lung cancer patients and commercial ERCC1 IHC test was not practical in the prospective evaluation of chemotherapy resistance of lung cancer patients, which contrasts with the results observed here. One explanation for this discrepancy is that many factors are involved in platinum resistance. In addition to ERCC1, many other genes, such as YAP (38) and NEAT1 (39), play important roles in the complicated biological events underlying the resistance process. ERCC1 expression level and function can be affected by post-transcriptional modifications.
Many other aspects of treatment, including the platinum dose, subsequent radiotherapy, and combination therapy with agents such as tyrosine kinase inhibitors (TKI) for patients with mutated epidermal growth factor receptor (EGFR), may also be related to the OS and PFS of lung cancer patients. As for ERCC1 IHC commercial tests, it could be a much more complicated problem. Different antibody with different clone number from different company may lead to confused conclusion of lung cancer patients with ERCC1 expression, so more studies are urgently needed. There is an urgent need for a more appropriate antibody, better and more mature detecting methods instead of totally declining the possibility to predict chemotherapy response of lung cancer patients. We should emphasize that the clone number of antibody we used in our research was the same as that in IALT Bio study (27) (mouse, 8F1).
In this study, negative ERCC1 expression did benefit lung cancer patients who were administered with cisplatin based chemotherapy. Thus, we can make some deduction: positive ERCC1 expression may be a negative factor for lung cancer patients who were administered with cisplatin based chemotherapy. In addition, accumulating evidence indicates ERCC1 is a good marker for cellular or clinical resistance to cisplatin, carboplatin, and oxaliplatin (7,40,41). ERCC1 is still a good predictive marker for chemotherapy.
Our study enrolled 106 patients from Xuanwei with operable cancer. These patients were positive for ERCC1 before administration of platinum-based chemotherapy, and the proportion of ERCC1-positive patients increased as the disease progressed. ERCC1 expression has been shown to predict the response to platinum-based therapy in advanced NSCLC patients (42). These observations serve as reminders of the significance of surgery in managing Xuanwei lung adenoma patients. Radical resection of lesions can reduce the ERCC1-positive tumor load in these patients, which is important for post-operative adjuvant therapy. Xuanwei lung adenoma patients diagnosed at an early disease stage may benefit from relatively complete resection of ERCC1-positive tumor tissue, thus ensuring a better response to adjuvant platinum-based chemotherapy.
There are some limitations to our study. All of the samples analyzed here were from Xuanwei lung adenoma patients. Most patients in this cohort did not undergo gene analysis for detection of EGFR mutant status and did not accept TKI treatment for economic reasons. The potential effects of these clinical factors on our study are unknown. In addition, patients with advanced lung adenoma (stage IIIb-IV) were not included in this study. We should also pay attention to the in vitro experiment because only one cell line was applied. In animal experiments, XWLC05-ERCC1-shRNA cells and control cells were injected subcutaneously, and the microenvironment in this location is quite different from that in human lung.
This study is the first to investigate ERCC1 expression in residents of Western China, which has a high incidence of lung adenoma. We examined ERCC1 gene-modified XWLC05 cells, originating from a Xuanwei lung adenoma patient, in vitro and in vivo. Our findings indicate that ERCC1 may play a critical role in the treatment of Xuanwei patients with platinum-based therapy and may have a significant effect on prognosis. Our research could thus be a good reference for further study of Xuanwei lung adenoma patients.
Acknowledgements
This study was supported by Yunnan Provincial Science and Technology Agency/Kunming Medical University Joint Project (2013FB164, 201501UH00557) to W.W.
References
- 1.Chen W, Zheng R, Baade PD, Zhang S, Zeng H, Bray F, Jemal A, Yu XQ, He J. Cancer statistics in China, 2015. CA Cancer J Clin. 2016;66:115–132. doi: 10.3322/caac.21338. [DOI] [PubMed] [Google Scholar]
- 2.Downward GS, Hu W, Large D, Veld H, Xu J, Reiss B, Wu G, Wei F, Chapman RS, Rothman N, et al. Heterogeneity in coal composition and implications for lung cancer risk in Xuanwei and Fuyuan counties, China. Environ Int. 2014;68:94–104. doi: 10.1016/j.envint.2014.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Liu ZY, He XZ, Chapman RS. Smoking and other risk factors for lung cancer in Xuanwei, China. Int J Epidemiol. 1991;20:26–31. doi: 10.1093/ije/20.1.26. [DOI] [PubMed] [Google Scholar]
- 4.Shen M, Chapman RS, He X, Liu LZ, Lai H, Chen W, Lan Q. Dietary factors, food contamination and lung cancer risk in Xuanwei, China. Lung Cancer. 2008;61:275–282. doi: 10.1016/j.lungcan.2007.12.024. [DOI] [PubMed] [Google Scholar]
- 5.Lan Q, Chapman RS, Schreinemachers DM, Tian L, He X. Household stove improvement and risk of lung cancer in Xuanwei, China. J Natl Cancer Inst. 2002;94:826–835. doi: 10.1093/jnci/94.11.826. [DOI] [PubMed] [Google Scholar]
- 6.Kim C, Chapman RS, Hu W, He X, Hosgood HD, Liu LZ, Lai H, Chen W, Silverman DT, Vermeulen R, et al. Smoky coal, tobacco smoking, and lung cancer risk in Xuanwei, China. Lung Cancer. 2014;84:31–35. doi: 10.1016/j.lungcan.2014.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Reed E. ERCC1 and clinical resistance to platinum-based therapy. Clin Cancer Res. 2005;11:6100–6102. doi: 10.1158/1078-0432.CCR-05-1083. [DOI] [PubMed] [Google Scholar]
- 8.Sodja E, Knez L, Kern I, Ovčariček T, Sadikov A, Cufer T. Impact of ERCC1 expression on treatment outcome in small-cell lung cancer patients treated with platinum-based chemotherapy. Eur J Cancer. 2012;48:3378–3385. doi: 10.1016/j.ejca.2012.06.011. [DOI] [PubMed] [Google Scholar]
- 9.Siddik ZH. Cisplatin: Mode of cytotoxic action and molecular basis of resistance. Oncogene. 2003;22:7265–7279. doi: 10.1038/sj.onc.1206933. [DOI] [PubMed] [Google Scholar]
- 10.Martin LP, Hamilton TC, Schilder RJ. Platinum resistance: The role of DNA repair pathways. Clin Cancer Res. 2008;14:1291–1295. doi: 10.1158/1078-0432.CCR-07-2238. [DOI] [PubMed] [Google Scholar]
- 11.Zamble DB, Mu D, Reardon JT, Sancar A, Lippard SJ. Repair of cisplatin - DNA adducts by the mammalian excision nuclease. Biochemistry. 1996;35:10004–10013. doi: 10.1021/bi960453+. [DOI] [PubMed] [Google Scholar]
- 12.Selby CP, Sancar A. Mechanisms of transcription-repair coupling and mutation frequency decline. Microbiol Rev. 1994;58:317–329. doi: 10.1128/mr.58.3.317-329.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mu D, Hsu DS, Sancar A. Reaction mechanism of human DNA repair excision nuclease. J Biol Chem. 1996;271:8285–8294. doi: 10.1074/jbc.271.14.8285. [DOI] [PubMed] [Google Scholar]
- 14.Smith S, Su D, de la Rigault Longrais IA, Schwartz P, Puopolo M, Rutherford TJ, Mor G, Yu H, Katsaros D. ERCC1 genotype and phenotype in epithelial ovarian cancer identify patients likely to benefit from paclitaxel treatment in addition to platinum-based therapy. J Clin Oncol. 2007;25:5172–5179. doi: 10.1200/JCO.2007.11.8547. [DOI] [PubMed] [Google Scholar]
- 15.Krivak TC, Darcy KM, Tian C, Armstrong D, Baysal BE, Gallion H, Ambrosone CB, DeLoia JA. Gynecologic Oncology Group Phase III Trial: Relationship between ERCC1 polymorphisms, disease progression, and survival in the Gynecologic Oncology Group Phase III Trial of intraperitoneal versus intravenous cisplatin and paclitaxel for stage III epithelial ovarian cancer. J Clin Oncol. 2008;26:3598–3606. doi: 10.1200/JCO.2008.16.1323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yamada Y, Boku N, Nishina T, Yamaguchi K, Denda T, Tsuji A, Hamamoto Y, Konishi K, Tsuji Y, Amagai K, et al. Impact of excision repair cross-complementing gene 1 (ERCC1) on the outcomes of patients with advanced gastric cancer: Correlative study in Japan Clinical Oncology Group Trial JCOG9912. Ann Oncol. 2013;24:2560–2565. doi: 10.1093/annonc/mdt238. [DOI] [PubMed] [Google Scholar]
- 17.Squires MH, III, Fisher SB, Fisher KE, Patel SH, Kooby DA, El-Rayes BF, Staley CA, III, Farris AB, III, Maithel SK. Differential expression and prognostic value of ERCC1 and thymidylate synthase in resected gastric adenocarcinoma. Cancer. 2013;119:3242–3250. doi: 10.1002/cncr.28175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kuhlmann JD, Wimberger P, Bankfalvi A, Keller T, Schöler S, Aktas B, Buderath P, Hauch S, Otterbach F, Kimmig R, et al. ERCC1-positive circulating tumor cells in the blood of ovarian cancer patients as a predictive biomarker for platinum resistance. Clin Chem. 2014;60:1282–1289. doi: 10.1373/clinchem.2014.224808. [DOI] [PubMed] [Google Scholar]
- 19.Hatch SB, Swift LP, Caporali S, Carter R, Hill EJ, MacGregor TP, D'Atri S, Middleton MR, McHugh PJ, Sharma RA. XPF protein levels determine sensitivity of malignant melanoma cells to oxaliplatin chemotherapy: Suitability as a biomarker for patient selection. Int J Cancer. 2014;134:1495–1503. doi: 10.1002/ijc.28454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bauman JE, Austin MC, Schmidt R, Kurland BF, Vaezi A, Hayes DN, Mendez E, Parvathaneni U, Chai X, Sampath S, et al. ERCC1 is a prognostic biomarker in locally advanced head and neck cancer: Results from a randomised, phase II trial. Br J Cancer. 2013;109:2096–2105. doi: 10.1038/bjc.2013.576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cecere F, Bria E, Rosell R. DNA repair by ERCC1 in non-small-cell lung cancer. N Engl J Med. 2006;355:2590–2591. doi: 10.1056/NEJMc062783. author reply 2591. [DOI] [PubMed] [Google Scholar]
- 22.Bepler G, Williams C, Schell MJ, Chen W, Zheng Z, Simon G, Gadgeel S, Zhao X, Schreiber F, Brahmer J, et al. Randomized international phase III trial of ERCC1 and RRM1 expression-based chemotherapy versus gemcitabine/carboplatin in advanced non-small-cell lung cancer. J Clin Oncol. 2013;31:2404–2412. doi: 10.1200/JCO.2012.46.9783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Soria JC. ERCC1-tailored chemotherapy in lung cancer: The first prospective randomized trial. J Clin Oncol. 2007;25:2648–2649. doi: 10.1200/JCO.2007.11.3167. [DOI] [PubMed] [Google Scholar]
- 24.Shiraishi K, Kohno T, Tanai C, Goto Y, Kuchiba A, Yamamoto S, Tsuta K, Nokihara H, Yamamoto N, Sekine I, et al. Association of DNA repair gene polymorphisms with response to platinum-based doublet chemotherapy in patients with non-small-cell lung cancer. J Clin Oncol. 2010;28:4945–4952. doi: 10.1200/JCO.2010.30.5334. [DOI] [PubMed] [Google Scholar]
- 25.Weiwei W, Zaoxiu H, Deguang W, Yong Z. Comparison of ERCC1 expression in lung adenoma tissue from Xuanwei of Yunnan province and other areas. Shangdong Med. 2016;22:67–68. [Google Scholar]
- 26.Rubatt JM, Darcy KM, Tian C, Muggia F, Dhir R, Armstrong DK, Bookman MA, Niedernhofer LJ, Deloia J, Birrer M, et al. Pre-treatment tumor expression of ERCC1 in women with advanced stage epithelial ovarian cancer is not predictive of clinical outcomes: A Gynecologic Oncology Group study. Gynecol Oncol. 2012;125:421–426. doi: 10.1016/j.ygyno.2012.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Olaussen KA, Dunant A, Fouret P, Brambilla E, André F, Haddad V, Taranchon E, Filipits M, Pirker R, Popper HH, et al. IALT Bio Investigators: DNA repair by ERCC1 in non-small-cell lung cancer and cisplatin-based adjuvant chemotherapy. N Engl J Med. 2006;355:983–991. doi: 10.1056/NEJMoa060570. [DOI] [PubMed] [Google Scholar]
- 28.Wang X, Zhao J, Yang L, Mao L, An T, Bai H, Wang S, Liu X, Feng G, Wang J. Positive expression of ERCC1 predicts a poorer platinum-based treatment outcome in Chinese patients with advanced non-small-cell lung cancer. Med Oncol. 2010;27:484–490. doi: 10.1007/s12032-009-9239-3. [DOI] [PubMed] [Google Scholar]
- 29.Ota S, Ishii G, Goto K, Kubota K, Kim YH, Kojika M, Murata Y, Yamazaki M, Nishiwaki Y, Eguchi K, et al. Immunohistochemical expression of BCRP and ERCC1 in biopsy specimen predicts survival in advanced non-small-cell lung cancer treated with cisplatin-based chemotherapy. Lung Cancer. 2009;64:98–104. doi: 10.1016/j.lungcan.2008.07.014. [DOI] [PubMed] [Google Scholar]
- 30.Lee HW, Choi YW, Han JH, Kim JH, Jung JH, Jeong SH, Kang SY, Choi JH, Oh YT, Park KJ, et al. Expression of excision repair cross-complementation group 1 protein predicts poor outcome in advanced non-small cell lung cancer patients treated with platinum-based doublet chemotherapy. Lung Cancer. 2009;65:377–382. doi: 10.1016/j.lungcan.2008.12.005. [DOI] [PubMed] [Google Scholar]
- 31.Holm B, Mellemgaard A, Skov T, Skov BG. Different impact of excision repair cross-complementation group 1 on survival in male and female patients with inoperable non-small-cell lung cancer treated with carboplatin and gemcitabine. J Clin Oncol. 2009;27:4254–4259. doi: 10.1200/JCO.2008.18.8631. [DOI] [PubMed] [Google Scholar]
- 32.Azuma K, Komohara Y, Sasada T, Terazaki Y, Ikeda J, Hoshino T, Itoh K, Yamada A, Aizawa H. Excision repair cross-complementation group 1 predicts progression-free and overall survival in non-small cell lung cancer patients treated with platinum-based chemotherapy. Cancer Sci. 2007;98:1336–1343. doi: 10.1111/j.1349-7006.2007.00557.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yu D, Zhang X, Liu J, Yuan P, Tan W, Guo Y, Sun T, Zhao D, Yang M, Liu J, et al. Characterization of functional excision repair cross-complementation group 1 variants and their association with lung cancer risk and prognosis. Clin Cancer Res. 2008;14:2878–2886. doi: 10.1158/1078-0432.CCR-07-1612. [DOI] [PubMed] [Google Scholar]
- 34.Snyder A, Makarov V, Merghoub T, Yuan J, Zaretsky JM, Desrichard A, Walsh LA, Postow MA, Wong P, Ho TS, et al. Genetic basis for clinical response to CTLA-4 blockade in melanoma. N Engl J Med. 2014;371:2189–2199. doi: 10.1056/NEJMoa1406498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rizvi NA, Hellmann MD, Snyder A, Kvistborg P, Makarov V, Havel JJ, Lee W, Yuan J, Wong P, Ho TS, et al. Cancer immunology. Mutational landscape determines sensitivity to PD-1 blockade in non-small cell lung cancer. Science. 2015;348:124–128. doi: 10.1126/science.aaa1348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Simon GR, Sharma S, Cantor A, Smith P, Bepler G. ERCC1 expression is a predictor of survival in resected patients with non-small cell lung cancer. Chest. 2005;127:978–983. doi: 10.1378/chest.127.3.978. [DOI] [PubMed] [Google Scholar]
- 37.Schneider JG, Farhadfar N, Sivapiragasam A, Geller M, Islam S, Selbs E. Commercial laboratory testing of excision repair cross-complementation group 1 expression in non-small cell lung cancer. Oncologist. 2014;19:459–465. doi: 10.1634/theoncologist.2013-0311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cheng H, Zhang Z, Rodriguez-Barrueco R, Borczuk A, Liu H, Yu J, Silva JM, Cheng SK, Perez-Soler R, Halmos B. Functional genomics screen identifies YAP1 as a key determinant to enhance treatment sensitivity in lung cancer cells. Oncotarget. 2016;7:28976–28988. doi: 10.18632/oncotarget.6721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jiang P, Wu X, Wang X, Huang W, Feng Q. NEAT1 upregulates EGCG-induced CTR1 to enhance cisplatin sensitivity in lung cancer cells. Oncotarget. 2016;7:43337–43351. doi: 10.18632/oncotarget.9712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Reed E. Nucleotide excision repair and anti-cancer chemotherapy. Cytotechnology. 1998;27:187–201. doi: 10.1023/A:1008016922425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Olaussen KA, Postel-Vinay S. Predictors of chemotherapy efficacy in non-small-cell lung cancer: A challenging landscape. Ann Oncol. 2016;27:2004–2016. doi: 10.1093/annonc/mdw321. [DOI] [PubMed] [Google Scholar]
- 42.Cobo M, Isla D, Massuti B, Montes A, Sanchez JM, Provencio M, Viñolas N, Paz-Ares L, Lopez-Vivanco G, Muñoz MA, et al. Customizing cisplatin based on quantitative excision repair cross-complementing 1 mRNA expression: A phase III trial in non-small-cell lung cancer. J Clin Oncol. 2007;25:2747–2754. doi: 10.1200/JCO.2006.09.7915. [DOI] [PubMed] [Google Scholar]