Abstract
Th22 cells are a major source of IL-22 and have been found at sites of infection and in a range of inflammatory diseases. However, their molecular characteristics and functional roles remain largely unknown due to our inability to generate and isolate pure populations. We developed a novel Th22 differentiation assay and generated dual IL-22/IL-17A reporter mice to isolate and compare pure populations of cultured Th22 and Th17 cells. Il17a fate-mapping and transcriptional profiling provide evidence that these Th22 cells have never expressed IL-17A, suggesting that they are potentially a distinct cell lineage from Th17 cells under in vitro culture conditions. Interestingly, Th22 cells also expressed granzymes, IL-13 and increased levels of Tbet. Using transcription factor-deficient cells, we demonstrate that RORγt and Tbet act as positive and negative regulators of Th22 differentiation, respectively. Furthermore, under Th1 culture conditions in vitro, as well as in an IFN-γ-rich inflammatory environment in vivo, Th22 cells displayed marked plasticity towards IFN-γ production. Th22 cells also displayed plasticity under Th2 conditions in vitro by up-regulating IL-13 expression. Our work has identified conditions to generate and characterize Th22 cells in vitro. Further, it provides evidence that Th22 cells develop independently of the Th17 lineage, whilst demonstrating plasticity towards both Th1 and Th2 type cells.
Keywords: IL-22, IL-17, Th1, Th17, Th22, Tbet, Plasticity
Introduction
The identification and characterization of CD4+ Th cell subsets and defining their immunological function has significantly advanced our understanding of adaptive immunity and the regulation of infectious and inflammatory diseases 1. It is now recognized that naïve Th cells differentiate into multiple distinct subsets, including Th-1, -2, -17 and regulatory T cells (Treg). More recently, Th9 and Th22 cells have also been identified, so-named for their predominant expression of IL-9 and IL-22, respectively 1,2. For many Th subsets (Th1, Th2, and Th17), the signals required for differentiation, the master regulators of transcription, secreted cytokines and the immune responses they regulate are well characterized. By contrast, we are just beginning to understand the contribution of Th9 and Th22 cells to immunity and inflammatory diseases, and the factors that regulate their development.
Th17 cells are defined by the production of IL-17A in association with IL-17F, IL-21 and IL-22. Th17 cells are increased in patients with psoriasis, inflammatory bowel disease (IBD), multiple sclerosis and rheumatoid arthritis, and are known to play pathogenic roles in animal models of these inflammatory disorders 3–8. The expression and function of T cell-derived IL-22 was previously linked to Th17 cells. However, IL-22 is now recognized to be produced by both Th17 and Th22 subsets, and the highest IL-22 levels are present in Th22 cells. Unlike Th17 cells, which produce IL-17A either alone or concomitantly with IL-22, the Th22 subset completely lacks expression of IL-17A 9,10. Furthermore, the presence of Th17 cells can be dissociated from Th22 cells at sites of inflammation, suggesting divergent roles for these effector cells 5,11–14. Th22 cells were first identified in psoriatic lesions, as phenotypically distinct from Th17 cells and other Th cell subsets, with high levels of IL-22 production 9. Although these cells have been repeatedly identified in various human diseases and mouse models, characterization of their gene expression and function has remained incomplete.
IL-22 can be produced during both innate and adaptive phases of immune responses by a range of cells (e.g. NK cells, ILCs, Th17 cells and Th22 cells). The function of IL-22 appears to be influenced by the type of inflammatory response, its cellular source, and the surrounding cytokine milieu, and IL-22 can be pro-inflammatory and/or tissue protective 15,16. These apparently dichotomous roles may depend on concomitant expression of IL-17A. For example, in the presence of IL-17A, IL-22 contributes to bleomycin-mediated inflammation, whereas when IL-17A is absent (in Il17a-/- mice), IL-22 is tissue protective 15. Studies in various tissues including the skin, lung and gastrointestinal tract (GIT) have also demonstrated evidence for very divergent functions of IL-22 and IL-17A 5,11–14. For example, the expression of IL-22 in asthma and atopic dermatitis patients has been largely dissociated from Th17 cells. In these patients, IL-22 is predominantly expressed in Th22 cells, and increased frequency correlates with disease severity, suggesting that these cells are important together with Th2 cells in regulating inflammation 9,11,12,17. Although this remains incompletely understood, it suggests that characterization of the cellular source of IL-22 may be as important as assessing IL-22 alone. Recently, Basu et al. demonstrated contrasting roles for Th22 cells (IL-22+IL-17A-CD4+ T cells) and Th17 cells (IL-22+IL-17A+ or IL-22-IL-17A+CD4+ T cells) in the clearance of Citrobacter rodentium from the GIT 18. Although this study did not employ pure populations of these cell subsets, it does provide further evidence to suggest functional differences between Th17 and Th22 cells in vivo.
Although the characterization of IL-22 is well advanced, and Th22 cells have been identified in normal and disease states, there is very little known about the precise function of Th22 cells. Delineation of the role of Th22 cells has been limited, due to our inability to characterize these cells directly in vitro or in vivo. This is primarily because of the limited knowledge of the factors regulating differentiation of Th22 cells and a lack of specific tools to isolate pure populations, which precludes their phenotypic and functional characterization. Current strategies to generate Th22 cells in vitro yield relatively low numbers of IL-22+ cells and these cultures are significantly contaminated with Th17 cells and other Th cell subsets, which prevents the definitive characterization of the phenotype and function of Th22 cells. Thus, it is vitally important to develop a way to study pure Th22 cells, independently of other IL-22-producing cells such as Th17 cells. In this investigation, by employing cells from IL-22/IL-17A dual reporter mice and Il17a fate-mapping mice we identify the factors required to induce optimal differentiation of Th22 cells and demonstrate that these cells may be a separate lineage from Th17 cells in vitro. Transcriptional profiling of isolated pure Th22 and Th17 cells further highlighted differences in cellular identity, transcriptional regulation and potential immunological roles. Notably, the differential Th22 transcriptional signature includes pronounced expression of Tbx21, cell death-inducing granzymes (particularly Gzmb) and Il13. Furthermore, we have identified that the transcription factors RORγt and Tbet act as positive and negative regulators of Th22 differentiation, respectively.
Material and Methods
Mice
Specific pathogen-free WT (C57BL/6), CD45.1 (B6.SJL-PtprcaPep3b/BoyJARC), Rorc(γt)-/- (B6.129P2(Cg)-Rorctm2Litt/J) and Tbx21-/- (B6.129S6-Tbx21tm1Glm/J) mice were obtained from Australian Bioresources (Moss Vale, Australia). Il17aCreR26FP635 (IL-17A tracer) fate mapping reporter mice were provided by Dr Brigitta Stockinger and Dr Mark Wilson. Il17aeGFP reporter mice (C57BL/6-Il17atm1Bcgen/J) and OT-II TCR-transgenic mice (specific for chicken ovalbumin323-339; B6.Cg-Tg(TcraTcrb)425Cbn/J) were purchased from Jackson laboratories. Il22tdTomato BAC transgenic reporter mice (C57BL/6-IL22promTdtomato) were generated by Dr. S.K. Durum (National Institutes of Health). Dual reporter mice (C57BL/6-Il17atm1Bcgen/J x IL22promTdtomato BAC transgenic reporter) and B6.Cg-Tg(TcraTcrb)425Cbn/J x C57BL/6-Il17atm1Bcgen/J x C57BL/6-IL22promTdtomato transgenic reporter mice on the C57BL/6 background (6-8 weeks old) were maintained and housed in individually ventilated cages in approved containment facilities within the Bioresources Facility, Hunter Medical Research Institute (Newcastle, Australia). Mice were provided with water and food ad libitum and acclimatized for one week prior to experimentation. All experiments were approved by the Animal Care and Ethics Committee of the University of Newcastle.
Purification of naïve Th cells and generation of Th cell subsets
CD4+ Th cells were purified from total splenocytes by magnetic cell separation followed by FACS sorting on a FACSAria III cell sorter (BD Pharmingen) for CD4+, CD44- and CD25- surface marker expression. The purity of sorted, naïve Th cells was routinely >99%. For the generation of effector Th cell subsets, purified naïve Th cells were stimulated in complete media (IMDM, 10% FCS, 2 mM L-glutamine, 50 µM β-mercaptoethanol, 100U/ml Penicillin-Streptomycin; Invitrogen) with plate-bound anti-CD3ε (1 μg/ml; Clone 145-2C11; BD Pharmingen) and soluble anti-CD28 (4 μg/ml; Clone 37.51; BD Pharmingen) for 3 days under polarizing conditions for Th0 cells (media alone), Th1 cells (10 ng/ml IL-12, 10 ng/ml IL-2, 10 μg/ml anti-IL-4), Th2 (10 ng/ml IL-4, 10 ng/ml IL-2, 10 μg/ml anti-IFN-γ), Th17 cells (10 ng/ml IL-1β, 30 ng/ml IL-6, 1 ng/ml TGF-β, 10 μg/ml anti-IL-4, 10 μg/ml anti-IFN-γ) or Th22 cells (10 ng/ml IL-1β, 30 ng/ml IL-6, 20ng/ml IL-23, 400nM FICZ, 10 μM Galunisertib (LY2157299), 10 μg/ml anti-IL-4, 10 μg/ml anti-IFN-γ) and 5 μg/ml anti-TGF-β1/2/3 (Clone 1D11, RnDSystems) and 10 ng/ml TNF-α were added where indicated.
Influenza infection with adoptive Th cell transfer
CD45.1 mice were infected with 1.4 x 104 pfu of ovalbumin323–339 peptide-expressing influenza A virus (strain A/HK/x31; H3N2, kindly provided by Stephen Turner from the University of Melbourne) 19. At day 3 of infection, 4 x 105 FACS-purified TCR-transgenic Th17 or Th22 cells (OT-II background) were transferred via intravenous injection. At day 8 of infection, lungs were collected and homogenates prepared for FACS analysis.
Isolation of total RNA and microarray profiling
For the extraction of total RNA, Trizol (Invitrogen) was used according to manufacturer’s protocol. Total RNA was quantified and quality was assessed using a 2100 Bioanalyzer Instrument (Agilent Technologies). RNA samples with RIN values >9 were used for microarray analysis. Mouse whole transcriptome microarrays (Gene array 2.1 ST from Affymetrix) were performed according to the manufacturer’s protocol by the Ramaciotti Centre for Gene Function Analysis (University of New South Wales, Sydney, Australia). The mRNA microarray data have been made publicly available at NCBI (GEO accession number GSE92610; https://www.ncbi.nlm.nih.gov/geo/).
RT-PCR analysis of gene expression and protein quantification
cDNA was generated from RNA using Superscript III with dNTPs and random hexamer primers according to manufacturer’s instructions (Invitrogen). Diluted cDNA (2 μl) was added to 6 μl of PCR mastermix (PCR Supermix-UDG with ROX [Invitrogen] with gene-specific forward and reverse primers [Table I] and water according to manufacturer’s protocol). The mixture was incubated at 95°C for 3 minutes followed by 40 PCR cycles (95°C for 15 seconds and 60°C for 60 seconds) on a ViiA7 real-time PCR analyzer (LifeTechnologies). The expression level of each individual RNA of interest was normalized to the house-keeping RNA Hprt.
Table I. Nucleotide sequence of primers used for gene expression analysis (5’ – 3’).
| Gene | Forward primer | Reverse primer |
|---|---|---|
| Ahr | GACCAGATTACATCATCGCCACTC | GTTGCTTTTGGTGCGTATTGGTAG |
| Bnc2 | GGAGTCCTAGCCTCCTTGCT | AAGCAGAAATGCAAGGCTGT |
| Foxo4 | ATCTCCCCATTCCTTGCTCT | CCCTTCTCCTGCTGACAAAG |
| Foxp3 | GGCGAAAGTGGCAGAGAGGTATT | GGCATTGGGTTCTTGTCAGAGG |
| Gata3 | AGAACCGGCCCCTTATGAA | AGTTCGCGCAGGATGTCC |
| Gzmb | ATGAAGATCCTCCTGCTACTGCT | CTTGATCGAAAGTAAGGCCATGT |
| Hprt | AGGCCAGACTTTGTTGGATTTGAA | CAACTTGCGCTCATCTTAGGCTTT |
| Ifng | TCTTGAAAGACAATCAGGCCATCA | GAATCAGCAGCGACTCCTTTTCC |
| Il13 | AGCTGAGCAACATCACACAAGACC | TGGGCTACTTCGATTTTGGTATCG |
| Il17a | CAAACATGAGTCCAGGGAGAGCTT | ACTGAGCTTCCCAGATCACAGAGG |
| Il17f | GAAGAAGCAGCCATTGGAGAAAC | AAGTCCCAACATCAACAGTAGCA |
| Il22 | GGTGACGACCAGAACATCCAGA | AGAGACATAAACAGCAGGTCCAGT |
| Il5 | TGTTGACAAGCAATGAGACGATGA | AATAGCATTTCCACAGTACCCCCA |
| Maf | AGGGACGCCTACAAGGAGAAAT | CCCACGGAGCATTTAACAAGGT |
| Rorc | CCGCTGAGAGGGCTTCAC | TGCAGGAGTAGGCCACATTACA |
| Tbx21 | TCAACCAGCACCAGACAGAGATG | CACCAAGACCACATCCACAAACA |
Protein concentration of IL-13, IL-17A, IL-17F and IL-22 in culture supernatants was determined by cytometric bead assays or ELISA according to manufacturer’s protocol (Legendplex, BioLegend).
FACS analysis
Surface staining
Cells were washed twice in FACS buffer (PBS + 1% FCS + 2 mM EDTA) and incubated with anti-mouse CD16/32 (Fc receptor block) followed by relevant antibodies (BD Pharmingen, BioLegend) and washed twice in FACS buffer. 7-AAD or SytoxBlue (Life Technologies) was used to exclude dead cells. Cells were analyzed immediately or fixed in 0.5% formaldehyde for later analysis. Analysis was performed on a FACSCanto analyzer (BD Pharmingen).
Intracellular cytokine staining
Cells were stimulated with PMA (50 ng/ml) and ionomycin (1 μg/ml) for 5 hours. Brefeldin A (5 μg/ml) was added for the final 4 hours of incubation. Following stimulation, cells were washed twice in PBS then resuspended either in ZombieYellow Fixable Viability Kit (BioLegend) or Fixable Viability Stain 780 (BD Pharmingen) for the exclusion of dead cells and stained according to manufacturer’s protocols. Fc receptor block was added followed by cell surface antibodies (Pharmingen, BioLegend). Cells were washed twice in FACS buffer and then resuspended in 4% paraformaldehyde and incubated on ice. Cells were washed twice in FACS buffer and permeabilized and stained according to manufacturer’s protocol using BD Perm/Wash buffer (BD Pharmingen). Cells were analyzed immediately or fixed in 0.5% buffered fixative and stored at 4°C in the dark until assayed. Analysis was performed on a FACSAriaIII analyzer (BD Pharmingen).
Statistical analysis
All experimental results are presented as mean ± standard error of the mean. Results were analyzed by one-way ANOVA, followed by a Bonferroni post-test for statistical significance or two-tailed Student's unpaired t-test. One-way ANOVA was used when comparing mean difference between more than two treatment groups. Student’s unpaired t-test was used where there are only two treatment groups. Analysis was performed with Prism v6.0 (GraphPad Software). The p values < 0.05 were considered statistically significant.
Results
Th22 cells are generated as a distinct lineage from Th17 cells in vitro
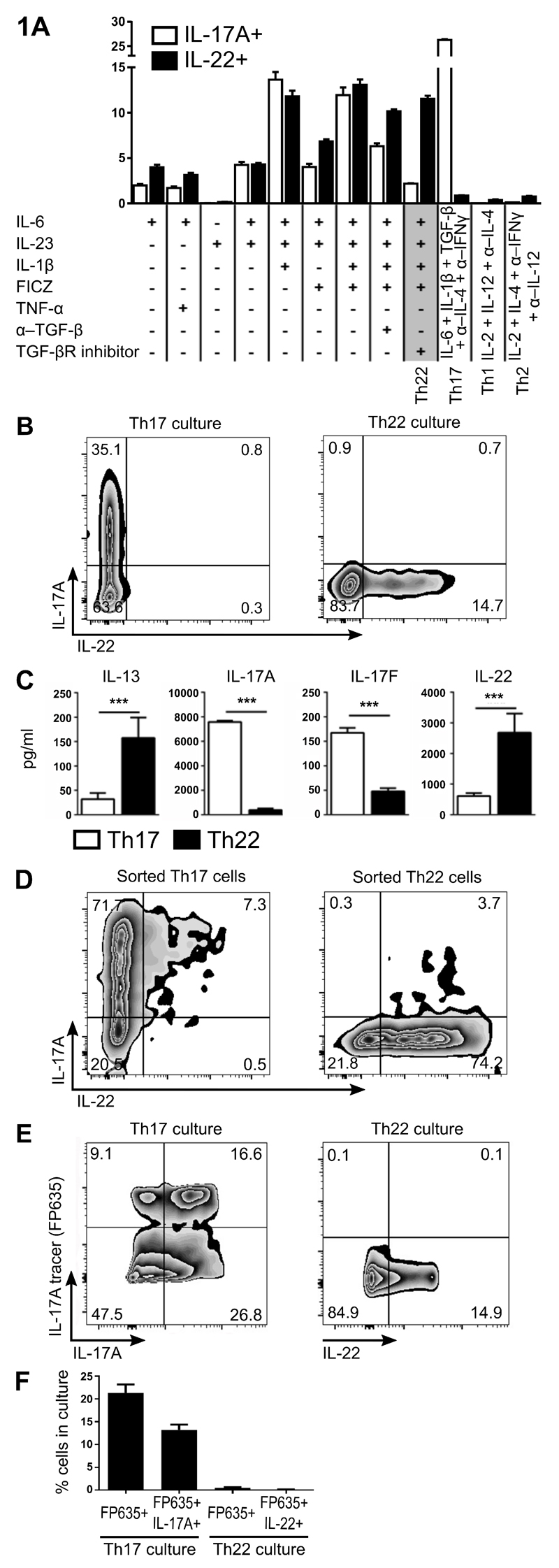
To study Th22 cells, and compare them to Th17 cells, we generated a dual-reporter mouse strain containing an IL-22 promoter-driven tdTomato 20 and an IL-17A-driven IRES eGFP reporter 21. This mouse enabled us to characterize IL-17A/IL-22 expression patterns in live cells and sort purified Th22 and Th17 cells both in vitro and in vivo. We initially sought to optimize culture conditions to produce Th22 cells from naïve murine CD4+ T cells, to determine whether this cell lineage may be distinct from Th17 cells. To do this, we assessed combinations of factors known to induce IL-22 transcription for their ability to differentiate naïve CD4+ T cells into Th22 cells. We trialed multiple combinations of factors on naïve CD4 T cells from our dual-reporter mice and assessed the impact on both IL-22 and IL-17A production (Fig. 1A). As a control, Th1, Th2, and Th17 cells were generated under standard published conditions in vitro and produced minimal amounts of IL-22. As previously reported 18,22,23, IL-6 alone induced IL-22 expression (Fig. 1A). However, induction was relatively weak and was not enhanced by the addition of TNF-α (Fig. 1A). Optimal IL-22 induction was achieved by a combination of four factors (IL-6, IL-23, IL-1β, FICZ; Fig. 1A). However, these conditions also induced substantial IL-17A production (~10% IL-17A+ cells), albeit at lower levels than observed under standard Th17 culture conditions. Further addition of an anti-TGF-β antibody partially suppressed IL-17A production, while addition of a small molecule inhibitor of TGF-β receptor signaling (TGF-βR inhibitor; galunisertib)24 almost completely abrogated IL-17A production, without inhibiting IL-22 production (Fig. 1A). Based on these findings, in further experiments, we defined “Th22 differentiation conditions” as IL-6, IL-23, IL-1β, FICZ and Galunisertib (highlighted as Th22 in Fig. 1A). Assessment of cytokine protein levels in culture supernatants confirmed dichotomous levels of IL-17A/F and IL-22 protein in Th17 and Th22 conditions, respectively (Fig. 1C). Further, IL-13 (Fig. 1C) and granzyme B (data not shown) protein levels were also increased in Th22 culture conditions compared to Th17, which was confirmed by quantitative PCR analysis (Supplemental Fig. 1). In Th22 cultures, we included anti-IL-4 and anti-IFN-γ to limit potential Th2 and Th1 differentiation induced by endogenous cytokine production, as is standard for Th17 polarization. Administration of recombinant IL-4 (without anti-IL-4) during differentiation under Th22 conditions reduced IL-22 expression and increased IL-13 expression (Supplemental Fig. 2A). Similarly, administration of recombinant IL-12 (without anti-IFN-γ) reduced IL-22 expression and increased IFN-γ expression (Supplemental Fig. 2A).
Figure 1. Generation of Th22 cells that appears to be a distinct lineage to Th17 cells.
Determination of optimal culture conditions for Th22 cells (IL-1β, IL-6, IL-23, FICZ and TGF-βR inhibitor/Galunisertib, with anti-IL-4/IFNγ). Percentage of IL-17A+ and IL-22+ cells after culturing naïve Th cells under various polarizing conditions are graphed (A). Representative plots of naïve Th cells stimulated for 3 d under optimal Th17 conditions or Th22 conditions (B). Cytokine protein levels in culture SN from naïve Th cells stimulated for 3 d under optimal Th17 conditions or Th22 conditions (C). Naïve Th cells from IL-17eGFP x IL-22tdTomato reporter mice were differentiated with Th17 or Th22 conditions then FACS sorted to purify Th17 or Th22, respectively. Representative plots of FACS-sorted Th17 and Th22 cells re-stimulated for 3 d under Th0 conditions (D). Representative plots (E), and percentage quantitation (F) of IL-17A fate mapping reporter (IL-17A tracer: Il17aFP635) expression versus IL-17A or IL-22 protein expression in naïve Th cells differentiated for 3 d under optimal Th17 or Th22 conditions. Cell populations in FACS plots are pre-gated on CD4+CD44+ and viable cells. Error bars represent SEM (n=6 per group from three independent experiments). ***p<0.001.
To assess the stability of our in vitro generated cells, we initially sorted Th22 (tdTomato+eGFP-) and Th17 (eGFP+) cells from their respective enriched cultures, and then re-cultured them in neutral conditions with anti-CD3/CD28 for a further 3 days (Fig. 1D). Under these conditions, Th22 and Th17 cells maintained their respective expression patterns. To assess whether Th22 cells ever transition through a Th17 differentiation pathway, we employed a fate reporter mouse (Il17aFP635; IL-17A tracer) 25, in which IL-17A expression results in the permanent expression of the red fluorescent protein FP635. As expected, Th17 cells co-expressed IL-17A protein and Il17aFP635 fate reporter, and a subset of cells under Th17 conditions expressed Il17aFP635, but no longer expressed IL-17A (Fig. 1E and F). By contrast, IL-22-producing cells generated under Th22 culture conditions did not express FP635/IL-17A tracer, indicating that they had not transitioned through an IL-17-expression stage (Fig. 1E and F).
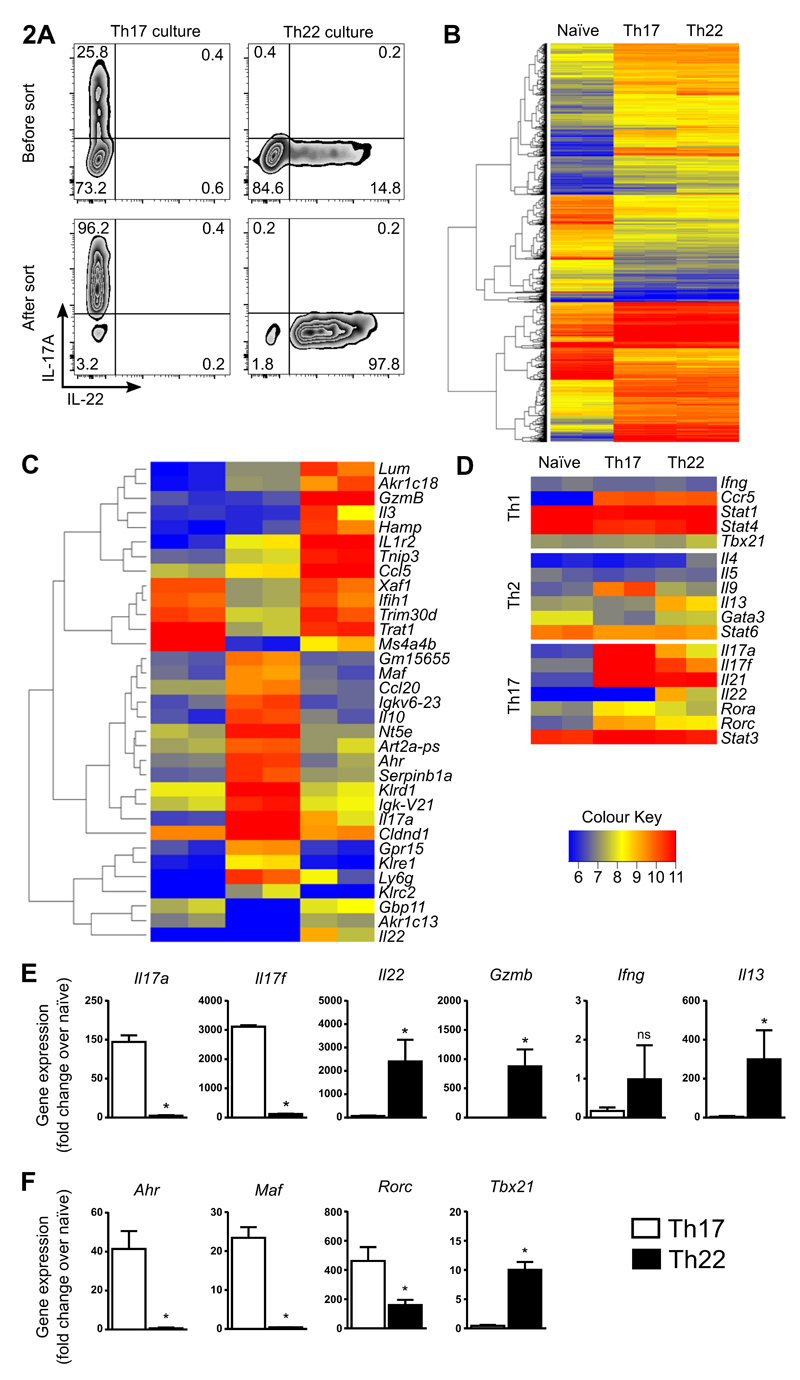
Transcriptional profiling reveals differences between Th17 and Th22 cells
We next sought to profile gene expression in Th17 and Th22 cells, using cells from our dual reporter mice. We initially purified Th17 (IL-17A+) and Th22 (IL-22+IL-17A-) cell populations generated in vitro (Fig. 2A, sorting strategy). We then performed whole-genome microarray analysis and compared mRNA expression profiles of naïve CD4+ T cells, to sorted Th17 cells and Th22 cells. Comparable numbers of differentially expressed genes were identified when comparing Th17 or Th22 cells to naïve CD4+ T cells (2524 and 2383 respectively, > 2-fold difference, p<0.05) (Fig. 2B). Comparison between Th22 and Th17 cells identified 287 genes as differentially regulated (>2-fold difference, p<0.05) (Supplemental Table I). Th17 signature genes, including Il17a, Il17f, Il21, Rora and Rorc were increased in Th17 cells, compared to Th22 cells (Fig. 2D). Among Th1 and Th2 signature genes, only Il9 expression was increased in Th17 cells and Il13 expression was increased in Th22 cells.
Figure 2. Transcription profiling in sorted pure Th17 and Th22 cells.
Cultures of enriched Th17 and Th22 cells were generated from IL-17eGFP x IL-22tdTomato reporter mice using optimal polarizing conditions for the first 3 d, and cells sorted on day 4 for Th17 cells (CD4+CD44+IL-17eGFP+) or Th22 cells (CD4+CD44+IL-17eGFP-IL-22tdTomato+). RNA was extracted from sorted cells and mRNA analysis performed. Th17 and Th22 enriched cultures before FACS, and resulting populations after cell sorting (viable cells shown) (A). Overview heatmap showing differentially expressed mRNAs in sorted naïve Th, Th17 and Th22 cells (B). Heatmap with 33 differentially regulated genes between Th22 and Th17 cells (>6-fold) shown for naïve Th, Th17 and Th22 cells (C). Th cell signature genes (Th1, Th2 and Th17) shown for naïve Th, Th17 and Th22 cells (D). RT-PCR confirmation of cytokine expression (E) and transcription factors (F) in sorted Th17 and Th22 cells (expression is normalized to naïve T cells). Error bars represent SEM (n=6 per group from three independent experiments). *p < 0.05.
Interestingly, some of the most differentially expressed genes between Th17 and Th22 cells were transcription factors and Th signaling molecules, such as Ahr, Maf, Rorc and Tbx21 (Fig. 2C, D, F). Neither Maf nor Foxp3 were induced in Th22 cells. Th22 cells had significantly lower Rorc and significantly higher expression of Tbx21, when compared to Th17 cells. qRT-PCR analysis confirmed differential expression of Th cell signature genes between purified populations of Th17 and Th22 cells (Fig. 2E), with increased expression of Il17a/f, Ahr, Maf and Rorc in Th17 cells and increased Il22, Tbx21, granzymes (particularly Gzmb) and Il13 in Th22 cells (Fig. 2E, F). As Th cells exert much of their function through secretion of modulatory proteins, we also performed an analysis of genes differentially expressed between Th22 and Th17 cells for genes predicted to produce secreted proteins (Supplemental Table II). This analysis identified increased expression of Il17a/f, Il9, Il10 and 16 additional genes in Th17 cells (>2-fold difference, p<0.05; Supplemental Table II). Il22, Il13, Gzmb/a and 24 additional genes were increased in Th22 cells over Th17 (>2-fold difference, p<0.05; Supplemental Table II).
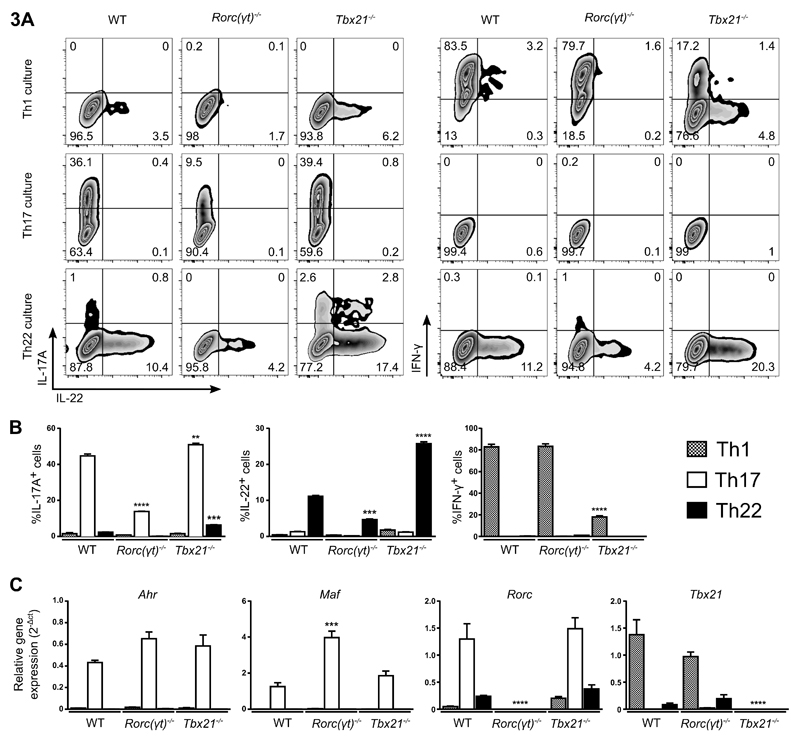
Th22 cell differentiation is partially dependent on RORγt and is negatively regulated by Tbet
We next sought to determine the transcriptional requirements for Th22 cell differentiation. As the transcription factors RORγt and Tbet were differentially expressed between Th22, Th17 and naïve CD4+ T cells, we purified and differentiated naïve CD4+ T cells from Rorc(γt)- and Tbx21- deficient mice and evaluated the effect on Th cell differentiation. As expected, IL-17A expression in Th17 culture conditions and IFN-γ expression in Th1 culture conditions was dramatically diminished in the absence of RORγt and Tbet, respectively (Fig. 3A, 3B). Loss of Rorc(γt) partially reduced IL-22 expression under Th22 culture conditions (Fig. 3A, 3B), suggesting that RORγt is required for IL-22 production and/or Th22 cell differentiation, albeit to a lesser degree than in Th17 cells. Critically, culturing Tbx21-deficient cells under Th22-inducing conditions resulted in a >2-fold increase in CD4+IL-22+ cell numbers, compared to wildtype cells (Fig. 3A, 3B), suggesting that Tbet expression strongly suppresses IL-22 production during Th22 differentiation. By contrast, Th17 cells were unaffected by the loss of Tbet expression and developed normally under Th17 conditions (Fig. 3B). This was supported by the observation that Tbet deletion had no impact on Ahr, Maf or Rorc levels in Th17 cells (Fig. 3C). Tbx21-deficiency did not alter the levels of the transcription factors Ahr, Maf, or Rorc in Th22 cells, and Tbx21-deficiency induced only a small increase in Rorc expression in Th1 cells (Fig. 3C). This data suggests that Tbet plays a critical role in Th22, but not Th17 cell differentiation.
Figure 3. Transcription factor control of Th17 and Th22 cell differentiation.
Representative plots of WT, Rorc(γt)-/- and Tbx21-/- Th cells differentiated in each Th condition (Th1, Th17 and Th22) (A). Cell populations in FACS plots are pre-gated on CD4+CD44+ and viable cells. Quantitation of IL-17+, IL-22+ and IFN-γ+ cells under each Th condition (Th1, Th17 and Th22) for WT, Rorc(γt)-/- and Tbx21-/- cells (B) and differential transcription factor expression assessed by RT-PCR, normalized to the housekeeping gene Hprt (C). Error bars represent SEM (n=6 per group from three independent experiments). **p < 0.01, ***p < 0.001, ****p < 0.0001.
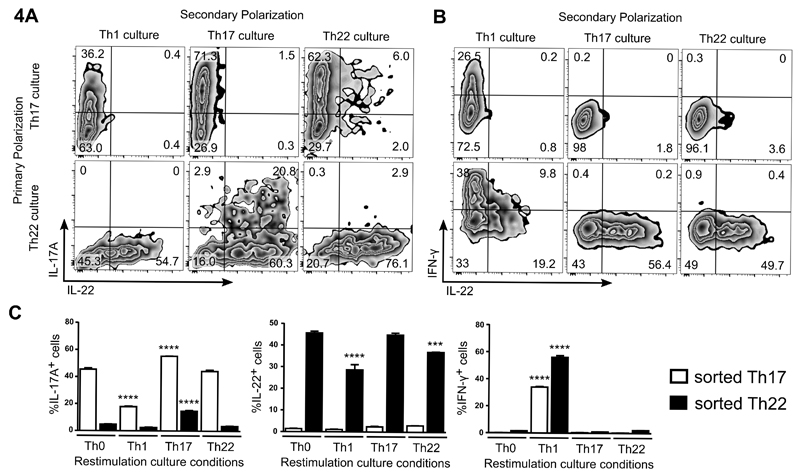
Th22 cells demonstrate plasticity to Th1 or Th2-like cells in vitro
To investigate the potential plasticity of differentiated Th22 cells, we again FACS-sorted dual-reporter cells from enriched cultures, and re-exposed them to Th polarizing conditions in vitro. Naïve CD4+ T cells were initially activated in the presence of Th22-polarising conditions (IL-1β, IL-6, IL-23, FICZ and Galunisertib) or Th17-polarising conditions (IL-6, IL-1β, and TGF-β), rested, and sorted for IL-17A+ (eGFP+;Th17 cells) or IL-22+/IL-17A- (tdTomato+/eGFP-;Th22 cells), respectively. Each cell population was then re-stimulated under Th0, Th1, Th17 or Th22 conditions for 3 days and assessed for reporter expression and levels of intracellular cytokines. Th17 and Th22 cells maintained their phenotype when re-stimulated under Th0, Th17 or Th22 conditions, as indicated by their reporter expression levels (Fig. 4A-C). A small increase in IL-17A production was observed in Th22 cells after re-stimulation in Th17 conditions, although IL-22 levels were unaffected (Fig. 4A, 4C). Interestingly, under Th1 conditions (known to induce Tbet expression 26), both differentiated Th17 and Th22 cells dramatically increased IFN-γ expression (~30-50% IFN-γ+, respectively), with respective decreases in IL-17A and IL-22 production (Fig. 4A-C). In separate experiments, cultures of differentiated Th22 cells were purified and re-stimulated under Th2 culture conditions leading to increased IL-13 expression, and decreased IL-22 expression (Supplemental Fig. 2B-D). Cultures of Th17 cells purified and re-stimulated under Th2 conditions induced a much lower level of IL-13 expression (Supplemental Fig. 2B-D).
Figure 4. In vitro plasticity of sorted Th22 cells re-stimulated under Th1, Th17 and Th22 conditions.
Cultures of enriched Th17 and Th22 cells were generated from IL-17eGFP x IL-22tdTomato reporter mice, using optimal polarizing conditions for the first 3 d, and cells sorted on day 4 for Th17 cells (CD4+CD44+IL-17eGFP+) or Th22 cells (CD4+CD44+IL-17eGFP-IL-22tdTomato+). Purified Th17 and Th22 cells were re-stimulated under Th1, Th17 and Th22 conditions for a further 3 d and the expression of IL-17A, IL-22 and IFN-γ determined. Representative plots of IL-17eGFP and IL-22tdTomato expression in re-stimulated, unfixed Th17 and Th22 cells are shown (A). Representative plots of IL-17eGFP, IL-22tdTomato, and IFN-γ expression in re-stimulated, fixed Th17 and Th22 cells are shown (B). Cell populations in FACS plots are pre-gated on CD4+CD44+ and viable cells. Quantification of IL-17eGFP+, IL-22tdTomato+ and IFN-γ+ cells in sorted Th17 and Th22 populations re-stimulated under Th0, Th1, Th17 and Th22 conditions (C). Note that paraformaldehyde fixation interferes with fluorescence from the tdTomato protein and likely explains the observed decrease in tdTomato signal following intracellular staining (Figure 4B/C). Error bars represent SEM (n=6 per group from three independent experiments). ***p < 0.001, ****p < 0.0001.
Th22 cells transition to produce IFN-γ in an antiviral Th1-environment in vivo
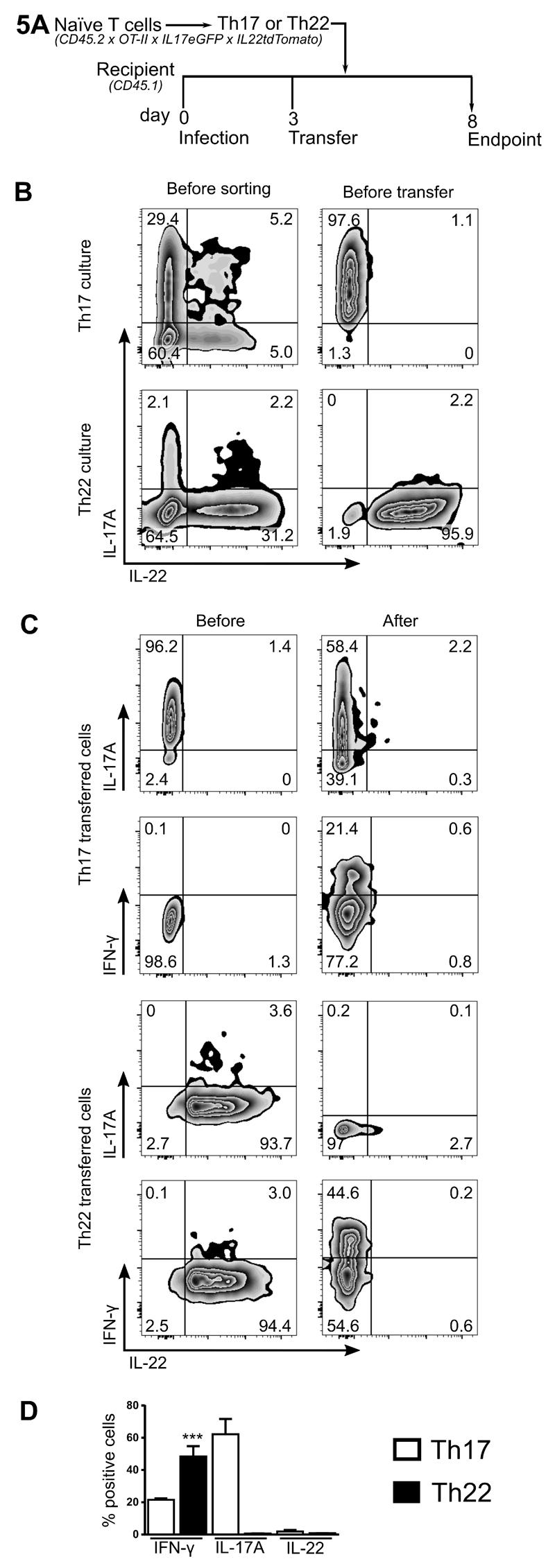
Given the negative regulation of Th22 cells by Tbet and demonstrable plasticity under Th1 conditions in vitro, we next assessed whether similar plasticity occurs in vivo. For this purpose, we bred Il17aeGFP x Il22tdTomato reporter mice onto an OT-II TCR-transgenic background (CD45.2) to enable the generation of antigen (chicken ovalbumin323-339 (OVA))-specific Th22 and Th17 cells in vitro. FACS-purified Th17 or Th22 cells specific for OVA323–339 peptide were then transferred into naive CD45.1 recipients. Wild-type CD45.1 recipients, rather than Rag-deficient mice, were chosen to avoid the complicating effects of homeostatic proliferation of transferred T cells. Three days prior to the cell transfer, recipient mice were infected with OVA323–339-expressing influenza A (Fig. 5A), to create a strong Th1-inducing antiviral environment in the presence of OVA Ag. At the peak of inflammation (day 8), lung cells were isolated to assess the fate of the transferred CD45.2+ Th17 and Th22 cells. Th17 cells largely maintained IL-17A expression in this IFN-γ-high environment, with low levels of IFN-γ expression (Fig. 5B-D). By contrast, transferred Th22 cells completely lost all IL-22 production and approximately half of these cells expressed high levels of IFN-γ (but not IL-17A) (Fig. 5B-D).
Figure 5. In vivo plasticity of Th22 cells in a high IFN/Th1-inflammatory environment.
Naïve Th cells from IL-17eGFP x IL-22tdTomato x OT-II TCR-transgenic (CD45.2) mice were used to differentiate antigen-specific (ovalbumin323–339) Th17 and Th22 cells. OVA-specific Th17 and Th22 cells were purified by FACS-sorting before being transferred into recipient mice (CD45.1) on day 3. Recipient animals were infected with Influenza A (1.4 x 104 pfu of ovalbumin323–339 peptide-expressing influenza A virus; A/HK/x31; H3N2) 3 d before transfer. Endpoint analysis was performed 5 d after cell transfer. Model schematic (A). Representative plots of IL-17eGFP and IL-22tdTomato expression in CD45.2+ Th17 and Th22 enriched cultures before sorting, before adoptive transfer on day 3 (i.e. sorted Th17 and Th22 cells) (B). Representative plots of IL-17eGFP, IL-22tdTomato, and IFN-γ expression in CD45.2+ Th17 and Th22 cells before transfer, and in those cells isolated from the lungs 5 d after transfer into Influenza A-infected recipient mice (C). All cell populations in FACS plots are pre-gated on viable cells and after adoptive transfer additionally with CD4+CD45.2+. Quantitation of IL-17eGFP, IL-22tdTomato, and IFN-γ expression in CD45.2+ Th17 and Th22 cells 5 d after transfer into Influenza A-infected recipient mice (D). Error bars represent SEM (n=6 per group from three independent experiments). ***p<0.001.
Discussion
Th22 cells have been identified in humans and mice and their presence is associated with a variety of diseases 9,18,27. However, conditions that allow for the in vitro generation and isolation of Th22 cells, in order to study their individual function, molecular phenotype, and distinction from Th17 cells have not been specifically defined. Many factors have been suggested to induce the expression of IL-22 in activated CD4+ T cells, including IL-1β, IL-6, IL-21, IL-23, TNF-α and aryl hydrocarbon receptor (AhR) ligands such as FICZ 18,22,28. However, these factors induce low levels of IL-22 and low frequencies of IL-22-producing Th cells or also induce expression of IL-17A in the same cell (Th17 cells). Furthermore, it has been suggested that IL-22 production can be inhibited by only trace amounts of recombinant TGF-β, a critical cytokine for the generation of Th17 cells 23. Thus we inhibited TGF-β using a small molecule inhibitor of TGF-β receptor signaling to suppress Th17 differentiation, in combination with factors that promote IL-22 production in our culture system. Our data demonstrate that optimal induction of enriched Th22 cells (IL-22+IL-17A-) without contaminating Th17 cells (IL-17A+IL-22+/-) can be achieved through simultaneous stimulation with IL-6, IL-23, IL-1β, FICZ and the TGF-βR inhibitor Galunsertib (Th22 culture conditions), in the presence of anti-IL-4/IFN-γ. Our findings provide novel culture conditions that enrich for Th22 cells. Importantly, the IL-22-producing cells generated in our Th22 enriched culture system displayed no IL-17A tracer (Il17aFP635) expression, indicating that they were not originally derived from, nor did they transit through, an IL-17A-producing cell type in vitro. Taken together, this data suggests that Th22 cells may be generated as a potentially distinct lineage from Th17 cells. Our use of dual IL-22/IL-17A reporter mice allows for accurate identification and isolation of live purified Th22 cells, without contaminating Th17 cells. These dual-reporter mice will also be useful for the characterization of Th22 cells in vivo in different tissues and under varying inflammatory conditions, as well as characterization of IL-22-producing cells beyond the Th22 lineage.
We identified major differences in the expression of transcription factors and Th signaling molecules between Th17 and Th22 cells. Maf, a potent inhibitor of IL-22 expression known to be increased in Th17 cells 22, was induced in Th17 but not Th22 cells. TGF-β-induced suppression of IL-22 expression is thought to be mediated through the induction of Maf 22 and likely explains the low expression of IL-22 in the cultured Th17 cells. Interestingly, BATF, a transcription factor required for the differentiation of IL-17A-producing Th17 cells 29, was not different between Th17 and Th22 cells (data not shown). Th22 cells had significantly lower Rorc and significantly higher expression of Tbx21, when compared to Th17 cells. We also assessed Bnc2 and Foxo4 expression in our cultures, as these factors have been reported in isolated human Th22 cells 9. Expression of these factors was variable across varying IL-22-inducing conditions (Supplemental Fig. 1A). Taken together, these results identify significant transcriptional differences between Th17 and Th22 cells across a broad range of T cell signature genes including key transcription factors. In addition, we identified many other interesting genes, such as the cell death-inducing granzymes, Gpr15, and Il13 that further distinguish Th22 cells from Th17 cells. In particular, it would be of future interest to determine whether the cytotoxic molecule Granzyme B, which was absent in naïve and Th17 but highly expressed in Th22 cells, plays a role in the immune function of Th22 cells.
In functional experiments, deletion of Tbx21 in our enriched cultures of Th17 and Th22 cells revealed that IL-22/Th22, but not IL-17A/Th17, were inhibited by Tbet expression. These results contrast with that of Basu et al., who suggested that Tbet actually amplifies IL-22 production 18. The explanation for this may lie in the fact that our in vitro cultures are enriched for Th22 cells with minimal contamination with Th17. In addition, we have directly studied the function of Th22 on an individual cell basis rather than total production of IL-22 or IL-17A by ELISA, this avoids the issue of dual cytokine producers in mixed cultures. Finally, our results indicating an inhibitory role of Tbet on Th22 are strongly supported by the observations, both in vitro and in vivo, that IFN-γ high conditions, which are known to induce Tbet, leads to loss of IL-22 expression. Our data suggests that Tbet acts as a negative regulator of Th22 cell differentiation, potentially controlling the switch between Th22 and Th1 cells depending on the local inflammatory cytokine milieu.
Studies suggest that Th cell subsets can exhibit plasticity in response to local inflammatory environments 26. For example, transfer of virus-specific Th2 cells into a strong IFN-γ environment induced by chronic virus infection induces these cells to adopt a Th1-like phenotype 30. This plasticity of the Th subsets appears to be dependent on the regulation of transcription factors that function as master regulators (e.g. Th1/Tbet, Th2/GATA3, Th17/RORγt, and Treg/Foxp3)2. Whether or not Th22 cells possess plasticity, and if so, how this might be regulated by a signature transcription factor remains unknown. Our data reveals plasticity of Th22 cells in vitro, with decreased expression of IL-22 and increased IFN-γ under Th1-polarising conditions and increased IL-13 expression under Th2-polarising conditions. It also reinforces the importance of Tbet expression in Th22 cells. We observed a similar effect in vivo in an antiviral IFN-rich environment, where we found Th22 cells were plastic and transitioned to an IFN-γ-producing Th1 cell phenotype, completely lacking either IL-17A or IL-22 expression. This effect was much less apparent for Th17 cells, suggesting that Th22 cells may have a unique propensity for plasticity to Th1. This is supported by other studies that provide evidence that IL-22-producing Th cells may potentially be plastic 20,31.
In conclusion, we have identified culture conditions that induce the differentiation of murine Th22 cells, with minimal contaminating Th17 cells. Molecular profiling provides insight into the specific identity of Th22 cells, and suggests that Th22 cells may potentially form a distinct lineage from Th17 cells. We do note that our IL-17A tracing experiments are limited to in vitro studies. Further studies are required to demonstrate whether Th22 cells can differentiate from an IL-17-producing population in different tissues or under differing inflammatory conditions in vivo. The transcription factor RORγt is necessary for Th22 differentiation, whilst Tbet acts as a negative regulator of development in vitro. Interestingly, Th22 cells expressed granzyme B and IL-13, factors associated with host defense and remodeling of tissue. Furthermore, under Th1-promoting conditions in vitro as well as in an IFN-γ-rich inflammatory environment in vivo, Th22 cells displayed marked plasticity towards the production of IFN-γ, further supporting an important role for Tbet in Th22 cell function. Th22 cells also exhibited plasticity under Th2 culture conditions in vitro, with increased IL-13 expression. We have identified conditions to generate and characterize Th22 cells in vitro that suggest that Th22 cells may develop independently of the Th17 lineage whilst demonstrating plasticity towards Th1 and Th2 type cells.
Supplementary Material
Acknowledgments
1 This work was supported by the National Health and Medical Research Council of Australia under project grant APP1061413 and the Australian Respiratory Council under the Harry Windsor Research Grants Scheme. MP is the recipient of a European Respiratory Society Fellowship (STRTF 2015).
References
- 1.Kara EE, Comerford I, Fenix KA, Bastow CR, Gregor CE, McKenzie DR, McColl SR. Tailored immune responses: novel effector helper T cell subsets in protective immunity. PLoS pathogens. 2014;10(2):e1003905. doi: 10.1371/journal.ppat.1003905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Li P, Spolski R, Liao W, Leonard WJ. Complex interactions of transcription factors in mediating cytokine biology in T cells. Immunological reviews. 2014;261(1):141–156. doi: 10.1111/imr.12199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chung Y, Yang X, Chang SH, Ma L, Tian Q, Dong C. Expression and regulation of IL-22 in the IL-17-producing CD4+ T lymphocytes. Cell Res. 2006;16(11):902–907. doi: 10.1038/sj.cr.7310106. [DOI] [PubMed] [Google Scholar]
- 4.Liang SC, Tan XY, Luxenberg DP, Karim R, Dunussi-Joannopoulos K, Collins M, Fouser LA. Interleukin (IL)-22 and IL-17 are coexpressed by Th17 cells and cooperatively enhance expression of antimicrobial peptides. J Exp Med. 2006;203(10):2271–2279. doi: 10.1084/jem.20061308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zenewicz LA, Yancopoulos GD, Valenzuela DM, Murphy AJ, Stevens S, Flavell RA. Innate and adaptive interleukin-22 protects mice from inflammatory bowel disease. Immunity. 2008;29(6):947–957. doi: 10.1016/j.immuni.2008.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hirota K, Hashimoto M, Yoshitomi H, Tanaka H, Nomura T, Yamaguchi T, Iwakura Y, Sakaguchi N, Sakaguchi S. T cell self-reactivity forms a cytokine milieu for spontaneous development of IL-17+ Th cells that cause autoimmune arthritis. J Exp Med. 2007;204(1):41–47. doi: 10.1084/jem.20062259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.van der Fits L, Mourits S, Voerman JS, Kant M, Boon L, Laman JD, Cornelissen F, Mus AM, Florencia E, Prens EP, Lubberts E. Imiquimod-induced psoriasis-like skin inflammation in mice is mediated via the IL-23/IL-17 axis. J Immunol. 2009;182(9):5836–5845. doi: 10.4049/jimmunol.0802999. [DOI] [PubMed] [Google Scholar]
- 8.Veldhoen M, Hocking RJ, Flavell RA, Stockinger B. Signals mediated by transforming growth factor-beta initiate autoimmune encephalomyelitis, but chronic inflammation is needed to sustain disease. Nat Immunol. 2006;7(11):1151–1156. doi: 10.1038/ni1391. [DOI] [PubMed] [Google Scholar]
- 9.Eyerich S, Eyerich K, Pennino D, Carbone T, Nasorri F, Pallotta S, Cianfarani F, Odorisio T, Traidl-Hoffmann C, Behrendt H, Durham SR, et al. Th22 cells represent a distinct human T cell subset involved in epidermal immunity and remodeling. J Clin Invest. 2009;119(12):3573–3585. doi: 10.1172/JCI40202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fujita H, Nograles KE, Kikuchi T, Gonzalez J, Carucci JA, Krueger JG. Human Langerhans cells induce distinct IL-22-producing CD4+ T cells lacking IL-17 production. Proc Natl Acad Sci U S A. 2009;106(51):21795–21800. doi: 10.1073/pnas.0911472106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Duhen T, Geiger R, Jarrossay D, Lanzavecchia A, Sallusto F. Production of interleukin 22 but not interleukin 17 by a subset of human skin-homing memory T cells. Nat Immunol. 2009;10(8):857–863. doi: 10.1038/ni.1767. [DOI] [PubMed] [Google Scholar]
- 12.Trifari S, Kaplan CD, Tran EH, Crellin NK, Spits H. Identification of a human helper T cell population that has abundant production of interleukin 22 and is distinct from T(H)-17, T(H)1 and T(H)2 cells. Nat Immunol. 2009;10(8):864–871. doi: 10.1038/ni.1770. [DOI] [PubMed] [Google Scholar]
- 13.Volpe E, Touzot M, Servant N, Marloie-Provost MA, Hupe P, Barillot E, Soumelis V. Multiparametric analysis of cytokine-driven human Th17 differentiation reveals a differential regulation of IL-17 and IL-22 production. Blood. 2009;114(17):3610–3614. doi: 10.1182/blood-2009-05-223768. [DOI] [PubMed] [Google Scholar]
- 14.Zenewicz LA, Yancopoulos GD, Valenzuela DM, Murphy AJ, Karow M, Flavell RA. Interleukin-22 but not interleukin-17 provides protection to hepatocytes during acute liver inflammation. Immunity. 2007;27(4):647–659. doi: 10.1016/j.immuni.2007.07.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sonnenberg GF, Nair MG, Kirn TJ, Zaph C, Fouser LA, Artis D. Pathological versus protective functions of IL-22 in airway inflammation are regulated by IL-17A. J Exp Med. 2010;207(6):1293–1305. doi: 10.1084/jem.20092054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Besnard AG, Sabat R, Dumoutier L, Renauld JC, Willart M, Lambrecht B, Teixeira MM, Charron S, Fick L, Erard F, Warszawska K, et al. Dual Role of IL-22 in allergic airway inflammation and its cross-talk with IL-17A. Am J Respir Crit Care Med. 2011;183(9):1153–1163. doi: 10.1164/rccm.201008-1383OC. [DOI] [PubMed] [Google Scholar]
- 17.Pennino D, Bhavsar PK, Effner R, Avitabile S, Venn P, Quaranta M, Marzaioli V, Cifuentes L, Durham SR, Cavani A, Eyerich K, et al. IL-22 suppresses IFN-gamma-mediated lung inflammation in asthmatic patients. J Allergy Clin Immunol. 2013;131(2):562–570. doi: 10.1016/j.jaci.2012.09.036. [DOI] [PubMed] [Google Scholar]
- 18.Basu R, O'Quinn DB, Silberger DJ, Schoeb TR, Fouser L, Ouyang W, Hatton RD, Weaver CT. Th22 cells are an important source of IL-22 for host protection against enteropathogenic bacteria. Immunity. 2012;37(6):1061–1075. doi: 10.1016/j.immuni.2012.08.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Olson MR, Seah SG, Cullen J, Greyer M, Edenborough K, Doherty PC, Bedoui S, Lew AM, Turner SJ. Helping themselves: optimal virus-specific CD4 T cell responses require help via CD4 T cell licensing of dendritic cells. J Immunol. 2014;193(11):5420–5433. doi: 10.4049/jimmunol.1303359. [DOI] [PubMed] [Google Scholar]
- 20.Shen W, Hixon JA, McLean MH, Li WQ, Durum SK. IL-22-Expressing Murine Lymphocytes Display Plasticity and Pathogenicity in Reporter Mice. Front Immunol. 2015;6:662. doi: 10.3389/fimmu.2015.00662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lee Y, Awasthi A, Yosef N, Quintana FJ, Xiao S, Peters A, Wu C, Kleinewietfeld M, Kunder S, Hafler DA, Sobel RA, et al. Induction and molecular signature of pathogenic TH17 cells. Nat Immunol. 2012;13(10):991–999. doi: 10.1038/ni.2416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rutz S, Noubade R, Eidenschenk C, Ota N, Zeng W, Zheng Y, Hackney J, Ding J, Singh H, Ouyang W. Transcription factor c-Maf mediates the TGF-beta-dependent suppression of IL-22 production in T(H)17 cells. Nat Immunol. 2011;12(12):1238–1245. doi: 10.1038/ni.2134. [DOI] [PubMed] [Google Scholar]
- 23.Zheng Y, Danilenko DM, Valdez P, Kasman I, Eastham-Anderson J, Wu J, Ouyang W. Interleukin-22, a T(H)17 cytokine, mediates IL-23-induced dermal inflammation and acanthosis. Nature. 2007;445(7128):648–651. doi: 10.1038/nature05505. [DOI] [PubMed] [Google Scholar]
- 24.Herbertz S, Sawyer JS, Stauber AJ, Gueorguieva I, Driscoll KE, Estrem ST, Cleverly AL, Desaiah D, Guba SC, Benhadji KA, Slapak CA, et al. Clinical development of galunisertib (LY2157299 monohydrate), a small molecule inhibitor of transforming growth factor-beta signaling pathway. Drug Des Devel Ther. 2015;9:4479–4499. doi: 10.2147/DDDT.S86621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Coomes SM, Pelly VS, Kannan Y, Okoye IS, Czieso S, Entwistle LJ, Perez-Lloret J, Nikolov N, Potocnik AJ, Biro J, Langhorne J, et al. IFNgamma and IL-12 Restrict Th2 Responses during Helminth/Plasmodium Co-Infection and Promote IFNgamma from Th2 Cells. PLoS pathogens. 2015;11(7):e1004994. doi: 10.1371/journal.ppat.1004994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Geginat J, Paroni M, Maglie S, Alfen JS, Kastirr I, Gruarin P, De Simone M, Pagani M, Abrignani S. Plasticity of human CD4 T cell subsets. Front Immunol. 2014;5:630. doi: 10.3389/fimmu.2014.00630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cheuk S, Wiken M, Blomqvist L, Nylen S, Talme T, Stahle M, Eidsmo L. Epidermal Th22 and Tc17 cells form a localized disease memory in clinically healed psoriasis. J Immunol. 2014;192(7):3111–3120. doi: 10.4049/jimmunol.1302313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yeste A, Mascanfroni ID, Nadeau M, Burns EJ, Tukpah AM, Santiago A, Wu C, Patel B, Kumar D, Quintana FJ. IL-21 induces IL-22 production in CD4+ T cells. Nature communications. 2014;5:3753. doi: 10.1038/ncomms4753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schraml BU, Hildner K, Ise W, Lee WL, Smith WA, Solomon B, Sahota G, Sim J, Mukasa R, Cemerski S, Hatton RD, et al. The AP-1 transcription factor Batf controls T(H)17 differentiation. Nature. 2009;460(7253):405–409. doi: 10.1038/nature08114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hegazy AN, Peine M, Helmstetter C, Panse I, Frohlich A, Bergthaler A, Flatz L, Pinschewer DD, Radbruch A, Lohning M. Interferons direct Th2 cell reprogramming to generate a stable GATA-3(+)T-bet(+) cell subset with combined Th2 and Th1 cell functions. Immunity. 2010;32(1):116–128. doi: 10.1016/j.immuni.2009.12.004. [DOI] [PubMed] [Google Scholar]
- 31.Ahlfors H, Morrison PJ, Duarte JH, Li Y, Biro J, Tolaini M, Di Meglio P, Potocnik AJ, Stockinger B. IL-22 fate reporter reveals origin and control of IL-22 production in homeostasis and infection. J Immunol. 2014;193(9):4602–4613. doi: 10.4049/jimmunol.1401244. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.